Abstract
The epidemiology of cardiovascular diseases in sub-Saharan Africa is unique among world regions, with about half of cardiovascular diseases (CVDs) due to causes other than atherosclerosis. CVD epidemiology data are sparse and of uneven quality in sub-Saharan Africa. Using the available data, the Global Burden of Diseases, Risk Factors, and Injuries (GBD) 2010 Study estimated CVD mortality and burden of disease in sub-Saharan Africa in 1990 and 2010. The leading CVD cause of death and disability in 2010 in sub-Saharan Africa was stroke; the largest relative increases in CVD burden between 1990 and 2010 were in atrial fibrillation and peripheral arterial disease. CVD deaths constituted only 8.8% of all deaths and 3.5% of all disability-adjusted life years (DALYs) in sub-Sahara Africa, less than a quarter of the proportion of deaths and burden attributed to CVD in high income regions. However, CVD deaths in sub-Saharan Africa occur at younger ages on average than in the rest of the world. It remains uncertain if increased urbanization and life expectancy in some parts of sub-Saharan African nations will transition the region to higher CVD burden in future years.
Keywords: Cardiovascular disease, Sub-Saharan Africa, Mortality, Burden of disease, Global health
The major CVDs vary in terms of underlying pathology (atherosclerosis, hypertensive target organ damage, infection, inflammation, anatomic deformities), interaction with other organ systems (pulmonary, immune, endocrine, neurologic, hematologic), and segment of the population affected. The prevalence pattern of the CVDs is distinctly different in sub-Saharan Africa compared with the rest of the world: infectious and inflammatory causes are relatively more common and atherosclerosis relatively less common. The past pattern of sub-Saharan African CVD epidemiology is not necessarily permanent, however. As parts of Sub-Saharan Africa urbanize and life expectancy increases, a larger share of the population may develop higher CVD rates, along with persistence of the lower CVD rates in poorer rural areas.1 CVD epidemiology studies have been scarce in the region, and complete vital registration of deaths by cause and burden of disease assessments have been completed by only a handful of sub-Saharan African nations.2 We therefore have an incomplete picture of CVD epidemiology in sub-Saharan Africa. In this review, we present the data on sub-Saharan Africa based on the Global Burden of Diseases, Injuries, and Risk Factor (GBD 2010) Study and discuss the strengths and limitations of study findings for sub-Saharan Africa.
The objective of the GBD 2010 Study was to estimate the epidemiology of 291 major diseases and injuries in 21 epidemiologic regions, including four sub-Saharan Africa regions (sub-Saharan Africa East, West, Central and South; Table 1).3 The GBD 2010 included substantially more source data on fatal and nonfatal CVD outcomes and more advanced estimation methods than prior versions of the GBD.4 Despite these advances, the problem of scarcity and uneven quality of data on CVD in Sub-Saharan Africa persists and is discussed in the section on study limitations.
Table 1.
Sub-Saharan countries and GBD regions.
| Central: Angola, Central African Republic, Congo, Democratic Republic of Congo, Equatorial Guinea, Gabon East: Burundi, Comoros, Djibouti, Eritrea, Ethiopia, Kenya, Madagascar, Malawi, Mauritius, Mozambique, Rwanda, Seychelles, Somalia, Sudan, Tanzania, Uganda, Zambia South Botswana, Lesotho, Namibia, South Africa, Swaziland, Zimbabwe West: Benin, Burkina Faso, Cameroon, Cape Verde, Chad, Cote d'Ivoire, Gambia, Ghana, Guinea, Guinea-Bisub, Liberia, Mali, Mauritania, Niger, Nigeria, Sao Tome and Principe, Senegal, Sierra Leone, Togo |
Methods
The core summary measurement of population health in the GBD 2010 Study was disability-adjusted life years (DALYs) in the years 1990 and 2010. DALYs represent the “health gap” between a population's actual health and an ideal standard. DALYs are composed of years of life lost (YLL) to premature deaths and years lived with non-fatal disease disability (YLD).3 Ten major CVD cause categories were defined based on International Classification of Disease (ICD) classifications: stroke, ischemic heart disease, cardiomyopathy, rheumatic heart disease, hypertensive heart disease, endocarditis, atrial fibrillation, aortic aneurysm, peripheral arterial disease and “other cardiovascular and circulatory”. The last “other” category included cardiopulmonary disease (ICD-10 I27, I28), non-rheumatic valvular disease (I34, I35, I36, I37), disorders of the arteries, capillaries or veins (I72, I77, I78, I83, I84, I87, I88, I89), venous embolism and thrombosis (I82), hypotension (I95), post-procedural disorders (I97), and cardiovascular disorders in syphilis and other diseases (I98). For mortality and YLL estimates, the GBD 2010 Study assembled a global cause-of-death data base. Mortality data were mapped to GBD cause categories and distribution of deaths to CVD and other causes and regional mortality and temporal trends were estimated using the cause of death ensemble modeling (CODEm) approach.5 The cause of death correct (CoDCorrect) algorithm estimated total CVDs as a proportion of all deaths, after which the component CVD causes were fit into the total CVD mortality envelope. Non-fatal CVD prevalence was estimated from data gathered in systematic reviews of epidemiologic data using a Bayesian meta-regression method (DisMod-MR).6 Disability from each case of nonfatal CVDs and other diseases or injuries was estimated in a household survey of lay people in Bangladesh, Indonesia, Peru, Tanzania, and the U.S.A., and an international web-based survey of health professionals.7 Because heart failure is not defined as an underlying cause of death in the International Classification of Diseases (ICD), separate methods were developed in order to distribute heart failure deaths to upstream CVDs and other causes of heart failure.8
Cause-of-death data from sub-Saharan Africa were usually not from standard vital registration, but were predominantly gathered from verbal autopsy studies, police reports, sibling histories, and burial and mortuary reports.5 With the exception of a few higher quality studies,9–11 most data on CVD in sub-Saharan Africa are from small community surveys and hospital-based registries.12 The GBD dealt with the problem of absent or low quality epidemiologic data from sub-Saharan Africa by 1) incorporating covariates (CVD risk factors, national income, differences in measurement method) and “borrowing strength” from nearby regions and years of observation in CODEm and DisMod-MR models, and 2) using standard assumptions about the relationship between disease-specific incidence, prevalence, case fatality, and mortality in DisMod-MR models.3,6,8
Results
Compared with all other world regions, the sub-Saharan Africa region had the smallest proportion of disease burden attributed to CVD in 2010: 8.8% of total deaths, 3.9 % of years of life lost, and 3.5% of DALYs (“tree plot” visualization of cause proportions, by region, available at http://viz.healthmetricsandevaluation.org/gbd-compare/). The corresponding CVD proportions for combined high-income regions were 35.7%, 27.2%, and 16.4%. Within sub-Saharan Africa, the Southern region had the highest proportional CVD burden and the Western region the lowest. The overall all-ages age-standardized sub-Saharan Africa 2010 CVD mortality rate was 892 deaths per 100,000 persons, and combined fatal and non-fatal burden of disease was 18,825 DALYs per 100,000 persons (Table 2; also by sub-Saharan Africa region, with uncertainty intervals, Table 1). Cerebrovascular disease had the highest death and disability rate of the top 10 CVDs in sub-Saharan Africa. Stroke mortality rates in 2010 ranged from 85 per 100,000 persons (95% CI 72–101) in Western sub-Saharan Africa to 126 per 100,000 person-years (95% CI 105–166) in Central sub-Saharan Africa. Age-adjusted DALYs ranged from 1665 per 100,000 persons (95% CI 1377–1968) in Western sub-Saharan Africa to 2434 per 100,000 persons (95% CI 2040–3041) in Central sub-Saharan Africa. Hemorrhagic and other non-ischemic stroke burden dominated over ischemic stroke burden across all regions of sub-Saharan Africa. Hemorrhagic and other non-ischemic stroke was the cause of 55% of stroke deaths and 64% of stroke DALYs.
Table 2.
Age-standardized mortality and DALYs per 100,000 people, 2010, all sub-Saharan African regions combined, the GBD 2010 Study.
| Cause | All Sub-Saharan Africa Regions Combined | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Males | Females | Both Sexes | ||||
|
|
|
|
||||
| DALYs | Deaths | DALYs | Deaths | DALYs | Deaths | |
| All cardiovascular and circulatory diseases | 20,270.10 | 926.28 | 17,563.61 | 858.36 | 18,824.98 | 891.53 |
| Rheumatic heart disease | 731.48 | 24.21 | 883.81 | 26.28 | 807.43 | 25.30 |
| Ischemic heart disease | 6859.08 | 311.88 | 4689.42 | 240.01 | 5700.08 | 272.80 |
| Cerebrovascular disease | 7955.06 | 401.89 | 7203.56 | 393.29 | 7568.48 | 399.03 |
| Ischemic stroke | 2810.70 | 172.24 | 2682.43 | 181.49 | 2749.08 | 178.43 |
| Hemorrhagic and other non-ischemic stroke | 5144.35 | 229.65 | 4521.14 | 211.79 | 4819.40 | 220.60 |
| Hypertensive heart disease | 1272.43 | 60.24 | 2025.35 | 105.09 | 1682.73 | 85.69 |
| Cardiomyopathy and myocarditis | 1420.36 | 54.34 | 968.39 | 37.60 | 1177.39 | 45.09 |
| Atrial fibrillation and flutter | 256.40 | 3.14 | 184.57 | 3.56 | 215.83 | 3.36 |
| Aortic aneurysm | 172.88 | 9.23 | 98.61 | 5.38 | 131.18 | 6.98 |
| Peripheral arterial disease | 105.04 | 3.82 | 56.97 | 1.58 | 77.91 | 2.52 |
| Endocarditis | 105.52 | 2.89 | 101.47 | 2.61 | 103.03 | 2.74 |
| Other cardiovascular and circulatory diseases | 1391.84 | 54.61 | 1351.45 | 42.94 | 1360.91 | 48.00 |
In sub-Saharan Africa there were more women living with peripheral arterial disease in 2010 than there were men (9.85 versus 4.39 million). Compared to Europe and North America where the bulk of people with peripheral arterial disease is above 55 years, most PAD cases in sub-Saharan Africa were noted amongst younger people (<55 years). For atrial fibrillation, 2010 DALYs were higher for men compared to women (Table 2). However, mortality associated with atrial fibrillation was higher in women compared to men (Table 2). All non-atherosclerotic CVDs (all CVDs excepting ischemic heart disease, thrombotic ischemic stroke, and peripheral arterial disease) were responsible for about half of all CVD mortality and DALYs in sub-Saharan Africa.
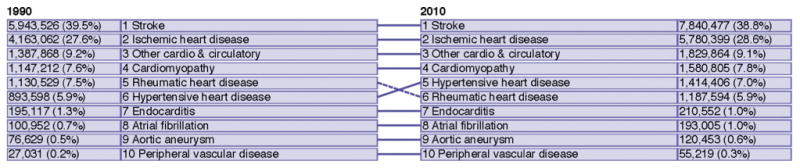
Rank of CVDs by proportion of CVD DALYs changed little in sub-Saharan Africa between 1990 and 2010, though absolute DALYs increased for all CVDs (Fig 1). Of the 20-year, 34% increase in DALYs in sub-Saharan Africa between 1990 and 2010, 65% of the DALY increase was due to population growth, 4% due to aging of the population, and the increase was attenuated by a 35% decrease in age-standardized CVD DALYs per capita population (decrease in disease rates). While absolute DALYs changed little between 1990 and 2010 for causes like endocarditis, DALYs about doubled for CVDs more common in older adults, like peripheral arterial disease and atrial fibrillation. While age-standardized DALY rates decreased for most CVDs in sub-Saharan Africa, age-standardized rates actually increased 16% for atrial fibrillation and 27% for peripheral arterial disease.
Fig 1. Leading causes of cardiovascular disease burden, sub-Saharan Africa, 1990 and 2010.
Because adults in sub-Saharan Africa are more likely to die from a non-CVD cause compared with the rest of the world, sub-Saharan Africa has the lowest years of life lost due to CVD (Table 3). At the same time, for persons dying of CVD, mean age of death in sub-Saharan Africa is the lowest in the world [64.9 years (95% uncertainty interval, 64.4–65.4)].
Table 3.
Average age at CVD death and years of life lost (YLL) due to CVD death per capita, 2010, the GBD 2010 Study.
| Super Region | Age at Death | YLL Per Capita |
|---|---|---|
| Sub-Saharan Africa | 64.9 (64.4–65.4) | 0.0216 (0.0191–0.0245) |
| East Asia/Pacific | 72.6 (72.2–72.9) | 0.0401 (0.0366–0.0421) |
| Eastern Europe/Central Asia | 75.5 (75.3–75.7) | 0.1084 (0.1050–0.1112) |
| High Income | 81.2 (81.0–81.6) | 0.0368 (0.0354–0.0396) |
| Latin America/Caribbean | 73.6 (73.3–73.9) | 0.0294 (0.0279–0.0315) |
| North Africa/Middle East | 68.6 (68.3–68.9) | 0.0442 (0.0406–0.0461) |
| South Asia | 67.6 (66.9–68.2) | 0.0352 (0.0299–0.0385) |
Discussion
The epidemiology of CVDs in sub-Saharan Africa is distinct because atherosclerosis causes only about half of CVDs. The GBD 2010 Study estimated that absolute CVD burden has increased in sub-Saharan Africa since 1990, with the largest relative increases in burden being atrial fibrillation and peripheral arterial disease—CVDs occurring most often in the elderly. Cerebrovascular disease, particularly hemorrhagic and other non-ischemic stroke, was the dominant source of CVD burden in the region. Because of the high burden of human immune deficiency virus (HIV), malaria, neonatal, and other non-CVD causes in sub-Saharan Africa, relatively few lives are lost due to CVD. On the other hand, the average age at CVD death in sub-Saharan Africa is the youngest in the world (Table 3).
Consistent with conclusions of systematic review studies, cerebrovascular disease, and particularly hemorrhagic and other non-ischemic stroke, emerged as the leading cause of CVD burden in sub-Saharan Africa.12,13 Our data on the relatively high rates of stroke mortality in sub-Saharan Africa compared with developed countries can be attributed to the higher stroke severity (for example, hemorrhagic strokes are clinically more severe than non-hemorrhagic strokes and have significantly greater case-fatality)14 and less than optimal acute stroke management in the region. The proportionally greater burden of hemorrhagic and other non-ischemic stroke compared with ischemic stroke burden is likely to be attributed to the relatively low prevalence of atherosclerosis (major cause of ischemic stroke) and high prevalence of hypertension (major cause of hemorrhagic stroke) in sub-Saharan Africa, as it was suggested for countries at the initial stages of epidemiological transition from communicable to non-communicable disorders.15 While there was no substantial variation in stroke burden across Eastern, Southern and Western regions of sub-Saharan Africa, stroke burden in Central sub-Saharan Africa was higher than in other regions of sub-Saharan Africa. This observation may be related to the more advanced stage of epidemiological transition currently observed in Central sub-Saharan Africa compared with other regions of sub-Saharan Africa. However, further good quality stroke epidemiological studies are required in sub-Saharan Africa to reliably address causes of the very high stroke burden in the region and develop culturally appropriate strategies for stroke prevention.
Among the CVDs, the largest relative increase in burden of disease for sub-Saharan Africa between 1990 and 2010 was observed for atrial fibrillation. Since atrial fibrillation is far more common in men, the 2010 DALYs were predictably higher in men compared to women. However, the higher mortality associated with atrial fibrillation in women is an unexpected finding and clearly needs further detailed investigation. Given the established association between atrial fibrillation and stroke, it is possible that the former is contributing to continued high burden of the latter. Atrial fibrillation burden was not assessed in the first GBD project. However an overall increase in both atrial fibrillation incidence and prevalence at a global level has recently been reported (1990–2010).16 While our findings in sub-Saharan Africa do not provide a direct explanation for increase in atrial fibrillation burden, these results do allow for some speculation in this regard. Even though rheumatic heart disease has been associated with occurrence of atrial fibrillation, the significant decrease in the burden of this condition would suggest that factors other than rheumatic heart disease are responsible for higher atrial fibrillation burden. Ischemic heart disease, hypertension, and cardiomyopathies saw an increased burden in sub-Saharan Africa and these are all conditions associated with higher occurrence of atrial fibrillation. However, there are likely to be multiple factors affecting the rising burden of atrial fibrillation and these could be region-specific. Especially given the etiologic role of atrial fibrillation for stroke, significant additional surveillance is needed and more detailed analysis of the mechanisms of atrial fibrillation is warranted.
Peripheral arterial disease also stood out as one of the CVDs with the largest relative increase in sub-Saharan Africa since 1990. The observation that the prevalence of peripheral arterial disease was higher among adults younger than 55 years old is concerning. It suggests exposure to peripheral arterial disease risk factors – e.g., tobacco smoke exposure, diabetes, hypertension, or hypercholesterolemia – at relatively young ages.17 As peripheral arterial disease may be caused by atrial fibrillation – a condition that also increased in prevalence – atrial fibrillation should be considered as a factor leading to peripheral arterial disease in sub-Saharan Africa.
Though the GBD 2010 estimated for sub-Saharan Africa the world's lowest ischemic heart disease death rates and burden per capita, ischemic heart disease ranked second on the sub-Saharan Africa CVD rank list. The rarity of ischemic heart disease in the region has been documented only in a handful of community surveys and hospital registries.11,18 Lack of data has led to very different conjectures about the impact of urbanization and lifestyle changes on ischemic heart disease in sub-Saharan African populations.1,19 The example of Japan during the 1960's to 1990's should caution us that lifestyle changes and adverse risk factor trends, such as increases in population mean total cholesterol, do not necessarily spur increased ischemic heart disease mortality.20
Heart failure is an important cause of death and disability in sub-Saharan Africa, and unlike in the high-income countries of North America and Europe, it is most often caused by hypertensive heart disease, rheumatic heart disease, or cardiomyopathy and rarely by ischemic heart disease.9,21–24 Heart failure is conspicuously absent among the major CVDs reported on here. Because the GBD cause list is based on ICD classifications, and in the ICD heart failure is not classified as an underlying cause of death and disability, in this analysis most of heart failure burden was assigned to its preventable root CVD causes (e.g., ischemic heart disease, rheumatic heart disease and other valvular heart disease, hypertensive heart disease, and cardiomyopathies). The shortcoming of this emphasis on primary heart failure prevention is that the potential benefits of treating heart failure cases and alleviating prevalent heart failure disability burden are not explicitly estimated, to some degree taking heart failure off the public health agenda for sub-Saharan Africa. It is likely that if heart failure underlying causes were reclassified into heart failure burden, heart failure would rise to be among the major CVDs in sub-Saharan Africa. GBD heart failure burden estimates are needed both for sub-Saharan Africa and globally and will be forthcoming.
Disease burden estimates are important for health system planners in the sub-Saharan Africa region. CVD epidemiology may be changing rapidly in the region, especially in areas where life expectancy is increasing (partly through improved neonatal and communicable disease prevention and treatment) and economic development and urbanization are progressing rapidly. The GBD made estimates for sub-Saharan Africa by “borrowing strength” from cause of death and epidemiology study data within the region and, in a geographically nested fashion, from other world regions. However, the problem of scarce and low-quality CVD epidemiologic data remains an endemic problem for sub-Saharan Africa. Even use of standard measurement instruments developed in other regions may risk erroneous estimates. For example, in the GBD ischemic heart disease analysis, World Health Survey self-reported angina prevalence was unexpectedly high in sub-Saharan Africa nations, perhaps because the Rose angina questionnaire is not equally valid in all populations.8 In 1998, responding to the original GBD (1990) Study, Cooper et al. argued that given lack of good quality vital registration and other surveillance studies, disease burden estimates for sub-Saharan Africa were overly uncertain and that the “complete” appearance of GBD estimates might lead to the misconception that more and better research is not needed.25 We argue with equal force that the best possible epidemiology and burden estimates are needed for decision-making in sub-Saharan Africa now, and that more and better epidemiologic surveillance is desperately needed.
In conclusion, the GBD 2010 Study used hierarchical models and meta-regression in an effort to overcome the limitation of sparse data and estimate mortality and burden of disease for sub-Saharan Africa. Our estimates suggest that non-atherosclerotic CVDs are responsible for about half of the CVD burden in the region. Though CVD is responsible for a smaller share of deaths and DALYs compared with other diseases in sub-Saharan Africa, the average age at CVD death is the youngest in the world. Two important policy lessons emerge from the GBD 2010 Study's analysis of CVD in sub-Saharan Africa. First, given the predominance of cerebrovascular disease and hypertensive heart disease burden, hypertension control needs to be a high priority. Second, sparse data led to a high degree of uncertainty about the CVD estimates, leading us to point to the dire need for more support for good quality, population-based epidemiologic research. The recent establishment of a number of high quality local and regional CVD epidemiology studies is an encouraging sign for sub-Saharan Africa CVD epidemiology and burden of disease estimates in the future.
Supplementary Material
Abbreviations and Acronyms
- CVD
cardiovascular disease
- GBD 2010
Global Burden of Disease 2010 Study
- ICD
International Classification of Diseases
- YLD
years lived with disability
- YLL
years of life lost due to disability
Footnotes
Disclaimer: The views expressed in this article do not necessarily represent the views of the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services, or any other government entity.
Statement of Conflict of Interest: All authors have no conflicts of interest to report.
Appendix A. Supplementary data: Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.pcad.2013.09.019.
References
- 1.Mensah GA. Ischaemic heart disease in Africa. Heart. 2008;94(7):836–843. doi: 10.1136/hrt.2007.136523. [DOI] [PubMed] [Google Scholar]
- 2.Bradshaw D, Timaeus IM. Levels and trends of adult mortality. In: Jamison DT, Feachem RG, Makgoba MW, editors. Disease and mortality in Sub-Saharan Africa. 2nd. Washington DC: World Bank; 2006. [PubMed] [Google Scholar]
- 3.Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 4.Murray CJ, Ezzati M, Flaxman AD, et al. GBD 2010: design, definitions, and metrics. Lancet. 2012;380(9859):2063–2066. doi: 10.1016/S0140-6736(12)61899-6. [DOI] [PubMed] [Google Scholar]
- 5.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salomon JA, Vos T, Hogan DR, et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2129–2143. doi: 10.1016/S0140-6736(12)61680-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Forouzanfar MH, Moran AE, Flaxman AD, et al. Assessing the global burden of ischemic heart disease, part 2: analytic methods and estimates of the global epidemiology of ischemic heart disease in 2010. Glob Heart. 2012;7(4):331–342. doi: 10.1016/j.gheart.2012.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Damasceno A, Mayosi BM, Sani M, et al. The causes, treatment, and outcome of acute heart failure in 1006 Africans from 9 countries. Arch Intern Med. 2012;172(18):1386–1394. doi: 10.1001/archinternmed.2012.3310. [DOI] [PubMed] [Google Scholar]
- 10.Walker R, Whiting D, Unwin N, et al. Stroke incidence in rural and urban Tanzania: a prospective, community-based study. Lancet Neurol. 2010;9(8):786–792. doi: 10.1016/S1474-4422(10)70144-7. [DOI] [PubMed] [Google Scholar]
- 11.Sliwa K, Wilkinson D, Hansen C, et al. Spectrum of heart disease and risk factors in a black urban population in South Africa (the Heart of Soweto Study): a cohort study. Lancet. 2008;371(9616):915–922. doi: 10.1016/S0140-6736(08)60417-1. [DOI] [PubMed] [Google Scholar]
- 12.Ntsekhe M, Damasceno A. Recent advances in the epidemiology, outcome, and prevention of myocardial infarction and stroke in sub-Saharan Africa. Heart. 2013;99(17):1230–1235. doi: 10.1136/heartjnl-2012-303585. [DOI] [PubMed] [Google Scholar]
- 13.Dalal S, Beunza JJ, Volmink J, et al. Non-communicable diseases in sub-Saharan Africa: what we know now. Int J Epidemiol. 2011;40(4):885–901. doi: 10.1093/ije/dyr050. [DOI] [PubMed] [Google Scholar]
- 14.Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol. 2009;8(4):355–369. doi: 10.1016/S1474-4422(09)70025-0. [DOI] [PubMed] [Google Scholar]
- 15.Gersh BJ, Sliwa K, Mayosi BM, Yusuf S. Novel therapeutic concepts: the epidemic of cardiovascular disease in the developing world: global implications. Eur Heart J. 2010;31(6):642–648. doi: 10.1093/eurheartj/ehq030. [DOI] [PubMed] [Google Scholar]
- 16.Chugh S. The global burden of cardiac arrhythmias. Circulation: Under Review. 2013 [Google Scholar]
- 17.Fowkes FG, Rudan D, Rudan I, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013 doi: 10.1016/S0140-6736(13)61249-0. Epub ahead of print. http://dx.doi.org/10.1016/S0140-6736(13)61249-0. [DOI] [PubMed]
- 18.Pobee JO. Study of cardiovascular diseases in developing countries supported by the World Health Organization. Experience in Ghana 1972–1982. Cas Lek Cesk. 1986;125(10):289–292. [PubMed] [Google Scholar]
- 19.Commerford P, Ntsekhe M. Ischaemic heart disease in Africa. How common is it? Will it become more common? Heart. 2008;94(7):824–825. doi: 10.1136/hrt.2008.142778. [DOI] [PubMed] [Google Scholar]
- 20.Iso H. Changes in coronary heart disease risk among Japanese. Circulation. 2008;118(25):2725–2729. doi: 10.1161/CIRCULATIONAHA.107.750117. [DOI] [PubMed] [Google Scholar]
- 21.Khatibzadeh S, Farzadfar F, Oliver J, Ezzati M, Moran A. Worldwide risk factors for heart failure: a systematic review and pooled analysis. Int J Cardiol. 2013;168(2):1186–1194. doi: 10.1016/j.ijcard.2012.11.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sliwa K, Mayosi BM. Recent advances in the epidemiology, pathogenesis and prognosis of acute heart failure and cardiomyopathy in Africa. Heart. 2013;99(18):1317–1322. doi: 10.1136/heartjnl-2013-303592. [DOI] [PubMed] [Google Scholar]
- 23.Ntusi NB, Mayosi BM. Epidemiology of heart failure in sub-Saharan Africa. Expert Rev Cardiovasc Ther. 2009;7(2):169–180. doi: 10.1586/14779072.7.2.169. [DOI] [PubMed] [Google Scholar]
- 24.Bloomfield GS, Barasa FA, Doll JA, Velazquez EJ. Heart failure in sub-saharan Africa. Curr Cardiol Rev. 2013;9(2):157–173. doi: 10.2174/1573403X11309020008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cooper RS, Osotimehin B, Kaufman JS, Forrester T. Disease burden in sub-Saharan Africa: what should we conclude in the absence of data? Lancet. 1998;351(9097):208–210. doi: 10.1016/S0140-6736(97)06512-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


