Abstract
Objective:
To conduct a scoping review on the use of technology to deliver mental health services to children and youth in order to identify the breadth of peer-reviewed literature, summarize findings and identify gaps.
Method:
A literature database search identified 126 original studies meeting criteria for review. Descriptive numerical summary and thematic analyses were conducted. Two reviewers independently extracted data.
Results:
Studies were characterized by diverse technologies including videoconferencing, telephone and mobile phone applications and Internet-based applications such as email, web sites and CD-ROMs.
Conclusion:
The use of technologies plays a major role in the delivery of mental health services and supports to children and youth in providing prevention, assessment, diagnosis, counseling and treatment programs. Strategies are growing exponentially on a global basis, thus it is critical to study the impact of these technologies on child and youth mental health service delivery. An in-depth review and synthesis of the quality of findings of studies on effectiveness of the use of technologies in service delivery are also warranted. A full systematic review would provide that opportunity.
Keywords: scoping review, technology, service delivery, children and young people, mental health
Résumé
Objectif:
Mener une étude de portée sur l’utilisation de la technologie pour dispenser des services de santé mentale aux enfants et aux adolescents, afin de déterminer l’ampleur de la littérature révisée par des pairs, de résumer les résultats et d’identifier les lacunes.
Méthode:
Une base de données de recherche de la littérature a recensé 126 études originales satisfaisant aux critères de l’étude. Des analyses thématiques et des résumés numériques descriptifs ont été menés. Deux analystes ont extrait les données indépendamment.
Résultats:
Les études étaient caractérisées par diverses technologies dont la vidéoconférence, le téléphone et les applications de téléphone cellulaire ainsi que les applications sur Internet comme le courriel, les sites Web et les CD-ROM.
Conclusion:
L’utilisation de la technologie joue un rôle majeur dans la prestation de services et de soutien de santé mentale aux enfants et aux adolescents car elle intervient dans la prévention, l’évaluation, le diagnostic, la consultation et les programmes de traitement. Les stratégies connaissent mondialement une croissance exponentielle, il est donc essentiel d’étudier l’impact de ces technologies sur la prestation de services de santé mentale aux enfants et aux adolescents. Une revue approfondie et une synthèse de la qualité des résultats des études sur l’efficacité de l’utilisation des technologies dans la prestation de services sont également justifiées. Une revue systématique complète conviendrait à cet exercice.
Keywords: étude de portée, technologie, prestation de services, enfants et adolescents, santé mentale
Introduction
Canada’s child and youth mental health system is described as fragmented and underfunded with a significant shortage of mental health professionals (Kirby & Keon, 2006). This is problematic as prevalence rates of psychiatric disorder in community samples of children and adolescents range from 15–25 percent (Parker et al., 2003). Rural and northern communities, in particular, suffer from a severe shortage of psychiatric expertise (Parker et al., 2003; Broder, Manson, Boydell, & Teshima, 2004). Geographic and professional isolation make rural communities less attractive to mental health practitioners, and it is challenging to recruit and retain specialists, who tend to concentrate in larger urban locales (Boydell et al., 2006; Volpe, Boydell, & Pignatiello, 2013). Further, numerous barriers make access to mental health care extremely difficult even in urban environments with no shortage of providers. Most barriers are structural, including cost, transportation, or time constraints. More timely access to mental health care can reduce costs and lessen time constraints (Myers et al., 2010). Consequently, delivery of mental health services using new technologies is a growing area of practice and research interest. Videoconferencing and the Internet are used to deliver child and youth mental health services globally via assessment, consultation, and therapy (Lingely-Pottie & McGrath, 2006; Reed, McLaughlin, & Milholland, 2000) and fill service gaps inherent in remote and rural regions (Cruz, Krupinski, Lopez, & Weinstein, 2005; Elford et al., 2000; Meyers, Valentine, & Melzer, 2007; Meyers, Valentine, & Melzer, 2008; Pesamaa et al., 2004, 2007).
Given the burgeoning use of technologies in child and youth mental health delivery, we require an in-depth understanding of how and what technologies are used. A scoping review of the literature was undertaken to identify the breadth of the peer-reviewed literature in this area, describe key findings and identify gaps and further research and practice opportunities. A scoping review aims “to map rapidly the key concepts underpinning a research area and the main sources and types of evidence available” (Arskey & O’Malley, 2005). Scoping studies are particularly relevant to disciplines with emerging evidence, such as e-mental health strategies, where the existence of few randomized controlled trials makes it difficult for researchers to conduct systematic reviews. In these cases, scoping studies are ideal as a range of study designs in both published and grey literature can be included, addressing questions beyond those related to intervention effectiveness, and generating findings that can complement the findings of clinical trials (Levac, Colquoun, & O’Brien, 2010). Unlike a systematic review, the scoping study does not seek to ‘synthesize’ evidence or to aggregate findings from different studies. A scoping study requires some analytic or thematic framework to represent a narrative account of extant literature; however, there is no attempt to describe the ‘weight’ of evidence regarding particular interventions or policies. This is because the scoping study does not seek to assess quality of evidence and as a result does not determine whether particular studies provide robust or generalizable findings (Arksey & O’Malley, 2005).
Methods
Best practice in scoping reviews indicates that they should provide an explicit description of their conceptual framework. Consequently, we draw upon an adapted version of Arksey and O’Malley’s (2005) framework, which involves the following phases:
Development of research questions
The overall research questions are: What is the extent of published evidence on using technology to deliver mental health services to children and youth? What is known from the existing literature about the impact of providing services in this manner? What are the gaps in the knowledge base in this burgeoning field?
Location of relevant publications
The scope of the review focuses on identifying evidence-informed uses of technology for mental health service provision. The technologies covered include videoconferencing, Internet-based interventions, email, telephone and mobile phone applications/interventions. Articles were included if published in the English language and in peer-reviewed journals from the year 2000 to December 31, 2012a. Articles were excluded if they were letters to the editor, dissertations, or focused on technologies used to deliver mental health services to adults, or to deliver mental health information, education and training.
The review was initially broad in scope and range. Keywords were selected to reflect the scope of the work related to videoconferencing, Internet applications and other technologiesb. Searches were conducted with database search engines PsycINFO, EMBASE, and Ovid MEDLINE. The research team developed criteria for review and search terms with a policy stakeholder advisory group and library information specialist.
Screening and selection of publications
The search returned approximately 4387 articles. Article titles and abstracts were first scanned to ascertain article relevance. Two reviewers (KB and MH) independently reviewed a sample of article titles and abstracts (n=200) and then reviewed together to decide upon discrepancies and achieve consensus. Exclusion criteria were applied over three phases wherein articles were read, bibliographies were reviewed and several specialists in the field were consulted with to find additional relevant articles for review. Following this, 126 articles were deemed relevant and full articles were obtained and included in the review (Figure 1).
Figure 1.
Search Results
Charting the data
Articles are organized according to type of technology used. Central themes arising from the literature review are identified using Braun and Clarke’s (2006) guidelines involving a process of thematic content analysis. Articles were read in full, annotated, and entered into table format developed to organize analysis, charting the article reference, participants and methods, objective and results of each of the studies.
Collating and summarising the results
We use a standard data extraction form according to a number of key characteristics, including: the type of technology, author(s) and journal, country, the service/treatment delivered, details about method/design, subjects/participants, key issues or outcomes addressed and gaps in the extant knowledge base (online Appendix I).
Results
Results of our scoping review include a descriptive numerical summary and thematic analysis, based on questions posed during the charting process (Arksey & O’Malley, 2005).
Descriptive numerical summary
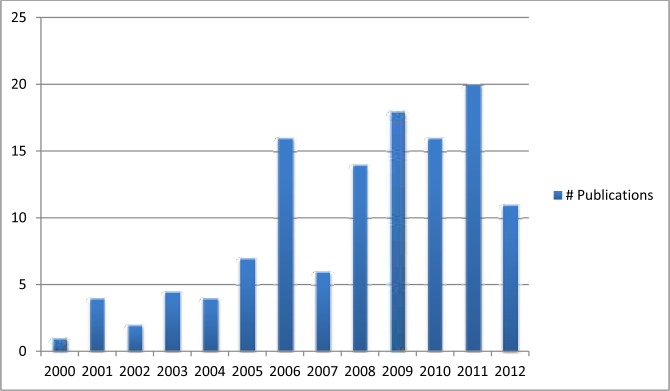
A full listing of 126 publications obtained through our systematic search is provided in Appendix 1. Most papers were published in the last half of our review period and more papers in recent years focus on service delivery via the Internet (Figure 2).
Figure 2.
Year of publication
Publications emanate largely from researchers in the US (40%, n=50), Australia (34%, n=41), the UK (10%, n=13), Canada (9%, n=10), and the remaining from the Netherlands (5%, n=6), Sweden (n=2), Finland (n=2) and New Zealand (n=2). When articles were split according to the focus on videoconferencing versus Internet technologies, Australia produced more articles in the Internet arena. Although many different technologies are represented, the majority included the Internet (47%, n=59) and videoconferencing (33%, n=42), followed by telephone (6%, n=8), email (6%, n=7), mobile phone/SMS applications (4%, n=5), and CDROM (4%, n=5).
Studies range from descriptive studies of particular programs to randomized controlled trials (RCTs). Table 1 summarizes this range; most articles report results of questionnaire surveys and pre-post studies followed by RCTs. Relatively few studies were qualitative.
Table 1.
Type of study
| Descriptive study - program | Case study | Qualitative study | Pre-post study | Randomized controlled trial (RCT) | Questionnaire/survey | Excluded (review article, not a specific study) |
|---|---|---|---|---|---|---|
| n=12 | n=17 | n=12 | n=22 | n=25 | n=28 | n=10 |
Thematic analysis
Of 126 articles reviewed, overall satisfaction and a range of positive outcomes (reduced symptomatology and enhanced access to care), preferences of young people, and cost savings are significant motives for using technologies to deliver mental health services. Findings suggest that using various technologiesc contributes to increased access to care, enhanced practitioner capacity, positive patient and family outcomes, and improved quality of life. They are organized in the following thematic categories: (i) overall satisfaction and positive outcomes; (ii) preferences of young people; (iii) technology; (iv) cost; (v) barriers; and, (vi) research gaps.
(i). Overall satisfaction and positive outcomes
Satisfaction data provide preliminary evidence for the effectiveness of telepsychiatry (Myers, Valentine, & Metzer, 2008). The 42 studies reviewed on videoconferencing include many reports of satisfaction levels of practitioners, families and young people. These satisfaction outcomes are based on survey questionnaires and qualitative interviews. A ten-year review of a telepsychiatry service indicates a high level of general satisfaction (Starling & Foley, 2006); satisfaction is rated as being extremely high with rural families (Starling, Rosina, Nunn, & Dossetor, 2003). Parents endorse high satisfaction with their child’s telepsychiatric care (Myers et al., 2008). Responses to a survey questionnaire indicate that the quality and acceptance of telepsychiatry with child welfare families is similar to face-to-face service provision (Keilman, 2005). Referring providers are highly satisfied (Myers et al., 2008) with enhanced provider capacity to deal with complex mental health issues (Greenberg, Boydell, & Volpe, 2006). Rural health care workers, young people and their carers give the technology itself high satisfaction ratings (Koppel, Nunn, & Dossetor, 2001).
An RCT of psychiatric assessments shows that diagnoses and treatment recommendations made by child psychiatrists by telemedicine and in face-to-face interviews are similar 96% of the time (Elford et al., 2000). Another RCT, using cognitive-behavioural therapy (CBT), indicates that psychotherapeutic treatment of depressed children via telemedicine is as effective as face-to-face therapy; parents and children prefer videoconference to face-to-face therapy and comparable decreased symptoms of depression are achieved (Nelson, Barnard, & Cain, 2003). Pesamaa and colleagues (2004) report successful skill implementation via telemedicine and 82% remission from depression post-treatment. In a youth justice setting, 80% of incarcerated youth are successfully prescribed medications, leading to improved mental health status (Myers, Valentine, Morganthaler, & Melzer, 2006). The same study shows youth confidence with psychiatrist recommendations; yet concerns are expressed about privacy issues inherent in telepsychiatry encounters.
Successful outcomes are reported in other studies of videoconferencing, many drawing upon case study methods. Case studies help us understand the particular in all its unique, contextual detail. Rich descriptions made possible by in-depth case study are the key to understanding the inherent complexities of programs (Greenhalgh, Russell, Ashcroft, & Parsons, 2011). Alessi (2003) documents success in properly diagnosing the case of a 15 year old and the positive relationship allowing for this. Miller and colleagues (Miller, Kraus, Fotto Kaak, Sprang, & Burton, 2002) show the effectiveness of telepsychiatry for a young boy in a rural school. Savin and colleagues (Savin, Garry, Zuccaro, & Novins, 2006) describe case studies of American Indians, and report that telepsychiatry enables access to services otherwise unavailable, with high patient and provider satisfaction and costs similar to providing face-to-face consultation. Pakyurek and colleagues (Pakyurek, Yellowlees, & Hilty, 2010) reviewed hundreds of cases and selected five illustrative cases suggesting that in certain cases, consultation processes might be superior to face-to-face as a method of psychiatric assessment. Contributing factors include: the novelty of the consultation, adolescent report of the experience as exciting; some adolescents feel that the interaction is more visual, video-game like, and, consequently, less threatening; capacity to provide direction, along with the extra distance involved (psychological and physical); and perceived authenticity of the interaction. A series of six case studies using WebCam as a therapeutic tool show its applicability in facilitating therapist and client communication (Chlebowski & Fremont, 2011). A case study of a rural Hispanic teen indicates therapeutic success for client and family and results in expansion of videoconferencing practice (Nelson & Bui, 2010). Qualitative research with three high school students indicates preference for mental health service delivery via videoconferencing over all other options (Bischoff, Hollist, Smith, & Flack, 2004).
Videoconferencing articles report positive findings for health care practitioners as well, saving time, costs and improving service quality (Pesamaa et al., 2004). Enhanced capacity of rural practitioners is demonstrated, along with reduced professional isolation (Gelber, 2001; Greenberg, Boydell, & Volpe, 2006; Pignatiello, Boydell, Teshima et al., 2010), and improved distribution of clinical expertise (Pignatiello, Boydell, Teshima, & Volpe, 2010). Mental health clinicians report increased knowledge and skills, and strengthening of relationships with colleagues (Gelber, 2001). Further, practitioners are satisfied with mental health service delivery using videoconferencing technologies (Greenberg, Boydell & Volpe, 2006; Koppel, Nunn, & Dossetor, 2001; Savin et al., 2006). Positive outcomes also include enhanced access to specialty care for practitioners and to mental health services for children, young people and their families. Research indicates that telepsychiatry can increase access to mental health care (Spaulding, Belz, Delurgio, & Williams, 2010) and one study involving rural primary care providers indicates that they perceived telepsychiatry’s ability to treat more patients over time (Hilty, Yellowlees, & Nesbitt, 2006).
The Internet literature identifies the effectiveness of online treatment, specifically CBT therapy, for addressing anxiety issues; young people participate actively, most comply with session schedules and form an effective therapeutic alliance (Spence et al., 2011). Several studies support the success of Internet based programs for a variety of mental health issues including treatment and reduction of symptoms for anxiety and depression (Calear & Christensen, 2010; Christensen, Griffiths, & Korten, 2002; Grover et al., 2011; O’Kearney, Gibson, Christensen, & Griffiths, 2006; O’Kearney, Kang, Christensen, & Griffiths, 2009; Sethi, Campbell, & Ellis, 2010; Stephens-Reicher, Metcalf, Blanchard, Mangan, & Burns, 2011), treatment of posttraumatic stress (Lange, van de Ven, Schrieken, & Emmelkamp, 2001), depression prevention (van Voorhees et al., 2008), assisting families (Jang et al., 2012; van Voorhees et al., 2008; Currie, McGrath, & Day, 2010), promotion of recovery in first episode psychosis (Alvarez-Jimenez et al., 2010), and reduction of symptoms for eating disorders (Grover et al., 2011). MoodGym, an online self-directed CBT program delivered in schools for preventing adolescent anxiety and depression, uses modules to directly address symptoms (Calear, Christensen, Mackinnon, Griffiths, & O’Kearney, 2009; Calear & Christensen, 2010). Three randomized trials comparing MoodGym with routine health class participation and wait list controls indicate that male participants receiving the intervention show reduced depressive symptoms as compared to wait-list controls post-intervention and six-month follow-up. Reduction in depressive symptoms was not observed in females receiving the intervention. Master Your Mood (MYM), an online CBT-based group course for adolescents and young adults with depressive symptoms indicates that, in an RCT, participants show a greater reduction in depressive symptoms compared to wait-list controls three months post-intervention, with reductions sustained at six months (van der Zanden, Kramer, Gerrits, & Cuijpers, 2012). March et al. (March, Spence, & Donovan, 2009) report that at post-treatment assessment, children in an Internet condition show small but significantly greater reductions in anxiety symptoms and increases in functioning than wait-list participants. These improvements are enhanced during the six-month follow-up period, with 75% of the children receiving Internet services free of their primary diagnosis. van Voorhees et al. (2009) RCT of Project CATCH IT, an Internet-based depression prevention program, demonstrate a decrease in depressed mood and in the likelihood of developing clinical depression. Hoek et al. (2011) completed a six-month RCT of an internet based behavior change model, reporting that higher ratings of Internet site ease of use was significantly associated with lower levels of depressed mood, supporting the use of well-designed cost-efficient Internet interventions for adolescents. An RCT of an Internet CBT program for depression showed modest effects in terms of reduced depression in the Internet group compared to treatment as usual (Clarke et al., 2009).
Similar to videoconferencing, one principle reported advantage of Internet based approaches is the opportunity to increase access in rural locales (Heinicke, Paxton, Mclean, & Wertheim, 2007). There is capacity to provide services for more individuals and respond to the mental health needs of those who may not otherwise receive treatment due to resource limitations (Shandley, Austin, Klein, & Kyrios, 2010; Currie, McGrath, & Day, 2010). For providers, computer screening reduces administration burden, scoring, and report writing (Diamond et al., 2010). The Internet provides availability 24/7 and allows respondents to pause and continue a program, an assessment or treatment plan as they please (Steenhuis, Serra, Minderaa, & Hartman, 2011).
Six studies focusing on email suggest it is a viable alternative to face-to-face and telephone encounters (Cartwright, Gibbon, McDermott, & Bor, 2005; Lyneham & Rapee, 2006). Benefits of using email to deliver services are well documented and include increased time available for contact between young people and clinicians, both frequency of contact and amount of time (Mehta & Chalhoub, 2006). Young people often devote much time composing emails to their clinicians, and receive frequent brief feedback; they feel that their clinician is present, listening, and thinking about them (Yager, 2003b). Much less clinician time is required for reading and responding to messages than is required with telephone use (Yager, 2003a).
Five studies focusing on the use of Compact Disc Read-only Memory (CD-ROM) suggest that adolescents report use of CD-ROM in therapy as acceptable (Cunningham et al., 2009) and are generally satisfied, finding the treatment process beneficial (Brosnan, Sharry, & Fitzpatrick, 2005; Cunningham et al., 2009; Cunningham & Wuthrich, 2008). However these studies are limited due to small sample sizes and restricted range of ages and diagnosis. A multicentre randomised controlled non-inferiority trial of SPARX, a self-help computer programme delivered via CD-ROM for young people with symptoms of depression, was carried out with 187 adolescents aged 12–19. Results show that use of the program resulted in a clinically significant reduction in depression, anxiety, and hopelessness and an improvement in quality of life (Merry et al., 2012). Wuthrich et al.’s (2012) RCT of 43 adolescents supports the effectiveness of a CD-ROM delivered intervention to significantly reduce the total number of anxiety disorders, the severity of the primary disorder and the average severity for all disorders compared with those on the wait list.
Eight studies in our review focus on telephone counselling (largely Kids Help Lines) in mental health service delivery. Several use pre-post measures to compare telephone to online support (Fukkink & Hermanns, 2009; Fukkink, 2011; King, Bambling, Reid, & Thomas, 2006). Counselling via telephone is effective (strong therapeutic alliance formed, less stigmatization, convenient) with families, children and youth. There is decreased distress reported across all studies reviewed. Pre-post and follow up of telephone versus online chat for children with severe emotional problems document improved well being in both treatment approaches (Fukkink & Hermanns, 2009; King et al., 2006). The anonymity telephone counselling provides is perceived as non-threatening support (Fukkink & Hermanns, 2009). Single session telephone support is superior to online counselling, although both achieve significant reduction in distress (King et al., 2006). Telephone-based treatments result in significant diagnosis decreases among children with disruptive or anxiety disorders compared to face-to-face treatment (Lingley-Pottie & McGrath, 2008; McGrath et al., 2011). Telephone support has a statistically significant impact on suicidality and mental state (King, Nurcombe, Bickman, Hides, & Reid, 2003). In one study, a 16-session telephone CBT intervention reduces obsessive-compulsive symptoms in young people (Turner & Heyman, 2009).
Five studies focused on mobile phone applications were reviewed, three of which were randomised control trials with a sample size of over 100 participants (Reid et al., 2011; Whittaker et al., 2012; Kauer et al., 2012). The studies reviewed suggest that it is possible to monitor symptoms and functioning in real time, allowing for personalized early intervention and relapse prevention (Reid et al., 2011; Whittaker et al., 2012) as well as to prompt users to perform specific therapeutic tasks tailored to and contingent on individual needs (Trockel, Manber, Chang, Thurston, & Taylor, 2011). Mobile phone programs are ideally suited to early intervention programs for depression as they are used as an immediate, portable, accessible and non-threatening self-monitoring tool (Kauer et al., 2012), wherein information is transmitted easily. Paediatricians report that mobile programs assist in better understanding of patient functioning and consequently, a high percentage of participants feel that their doctor understands them better (Reid et al., 2012).
(ii). Preferences of young people
The literature suggests young people may be more likely to respond to alternate service delivery strategies such as videoconferencing or Internet-based applications. In the videoconferencing literature, children aged 4–12 are very positive about videoconferencing with 94% liking the system and 29% indicating they prefer a ‘television’ doctor to a ‘real’ doctor (Elford et al., 2001; Elford et al., 2000). They acknowledge a sense of agency, experience helpfulness of the session, and report a positive encounter with the psychiatrist (Boydell, Volpe, & Pignatiello, 2010). High school students appreciate the privacy the technology affords (Bischoff et al., 2004). Qualitative research demonstrates that adolescents and their families feel they are ‘spoken to, rather than at’ (Grealish, Hunter, Glazez, & Potterz, 2005). Adolescents report that telemedicine promotes transfer of power and control by allowing them to feel more comfortable about terminating the consultation or walking out; the process is more structured, and consequently they feel better informed, resulting in a better understanding, sense of shared responsibility and better decision making (Grealish et al, 2005).
Responses to an online administered survey indicate that social networking via Internet is integral to the lives of young adults, with a majority of young people reporting they use such sites (Gowen, Deschaine, Gruttadara, & Markey, 2012). It has been reported as being appealing due to its intuitive structure for young people to engage with each other and with a moderator (Gleeson, Alvarez-Jimenez, & Lederman, 2012). Anonymity is an important aspect of the technology that engages young people (Pretorius, Rowlands, Ringwood, & Schmidt, 2010; Richards, 2009). Youth are generally more open and confident when online, providing more personal details due to perceived distance between client and therapist (Diamond et al., 2010; Read, Farrow, Jaanimagi, & Ouimette, 2009). Burns et al. (Burns, Morey, Lagelee, Mackenzie, & Nicholas, 2007) description of the Reach Out program indicates the site has managed to garner credibility of young people. University students are likely to seek help online first, highlighting the importance of the Internet in reaching out to these individuals (Radhu, Daskalakis, Arpin-Cribbie, Irvine, & Ritvo, 2012). Young people prefer an informal delivery format (Shandley et al., 2010) and indicate that completing therapy and assessments online are easier than paper-and-pencil (Read et al., 2009) and have high levels of readability and ease of understanding (van Voorhees, Ellis, Stuart, Fogel, & Ford, 2005). Younger children and their parents show high levels of compliance in completing Internet-based CBT sessions for anxiety and associated homework tasks (Spence, Holmes, March, & Lipp, 2006). Young people receiving a web-based intervention for bulimia nervosa or atypical bulimia appreciate the flexibility and sense of control over treatment that online treatment affords (Pretorius et al., 2009, 2010). March et al.’s (2009) online sessions to reduce anxiety are rated as interesting and engaging, stimulate motivation and facilitate learning. A comprehensive program of engagement and motivation through online service delivery can be developed, and may enhance participation (Landback et al., 2009). Young people feel empowered by using email and readily engage in use of this medium (Mehta & Chalhoub, 2006). They also respond positively to the multimedia aspects of CD-ROM delivery format (Brosnan et al., 2005; Cunningham et al., 2009).
(iii). The technology
High quality audio is one of the most important factors influencing parent and psychiatrist satisfaction with video-conferencing (Elford et al., 2000). Technical quality issues, referred to as “growing pains,” have essentially disappeared from the literature with refinement of videoconferencing technology and as practitioners become more comfortable and accepting of new technologies (Boydell, Volpe, Kertes, & Greenberg, 2007). The technology itself has moved over time from being a barrier due to technical difficulties to being a facilitator in terms of preferred mode of communication (Boydell et al., 2010).
The Internet supports social networks and existing social connections, both online and offline. One discussion article suggests that it encourages community participation and increases the likelihood of help seeking (Burns et al., 2007). Chat-based services facilitate community and therefore allow therapeutic counseling interventions for an online user community (Richards, 2009). Alongside social networking functions interactive therapy modules can address psychoeducation, relapse prevention, stigma and social anxiety, early warning signs of relapse, depression, and identification and use of personal strengths (Gleeson et al., 2012). Another beneficial feature of social networking sites is the ‘wall’ function that organizes discussion threads into relevant themes where moderators can encourage clients to share successful approaches and personal victories (Gleeson et al., 2012). Online games present clients with engaging scenarios, serving as a catalyst for raising issues and discussing difficulties experienced by adolescents (Burns, Webb, Durkin, & Hickie, 2010). The breadth and flexibility of online applications ensures that technology can be used to deliver mental health services successfully and innovatively with few differences between online and face-to-face delivery (Richards, 2009; Spence et al., 2008, 2011).
(iv). Cost issues
The quality of cost data in the literature is suboptimal and little information is collected in a systematic, controlled, prospective way (Hilty, Yellowlees, Sonik, Derlet, & Hendren, 2009). What literature exists suggests that total travel cost is less per patient using telepsychiatry than costs of travelling for psychiatry services (Elford et al., 2001). Not surprisingly, cost savings to young people and their families are realized for travel time (Spaulding et al., 2010). Sustainability can be challenged by infrastructure costs and low reimbursement by public payers (Myers et al., 2008).
The Internet has the potential to reach a wide audience cost effectively and may help manage health delivery costs; targeting individuals at an early stage using the Internet may prevent symptoms from developing into disorders requiring more costly treatment (Christensen, Reynolds, & Griffiths, 2011). Screening and assessment websites are reported to have ease of administration and low costs (Steenhuis et al., 2009) and can help solve problems associated with administration, interpretation, and data integration (Diamond et al., 2010; Steenhuis et al., 2009). In a study of Internet-based therapy for anxiety, therapists spend an estimated 15 minutes per week reviewing session activities and preparing email responses for each family, translating into a significant cost reduction in terms of therapist time (March et al., 2009). The use of email is also recognized as cost-effective (Trockel et al., 2011). Concerns have also been raised that enhanced awareness due to Internet promotion might lead to an increased demand on an already overburdened health system, however, there is no systematic empirical evidence relevant to this question (Christensen et al., 2011).
(v). Barriers to using technology to deliver mental health services
Few disadvantages are reported in articles focusing on the use of videoconferencing. Technical quality issues previously attributed to the use of videoconferencing are no longer an issue (Boydell et al., 2007). Consultation regarding difficult cases that do not include follow up may lead to frustration and potential burn-out (Diamond & Block, 2010). Barriers to the use of Internet applications include difficulty in engaging young people in their use, perceptions that programs have low adherence, and clinician concerns about value, effectiveness and safety (Christensen et al., 2011). Chat rooms and online environments hold potential dangers, including the possibility of attracting adults who may take advantage of vulnerable adolescents (Webb, Burns, & Collin, 2008). Online treatment or assessment has greater risk for misinterpretation than in-person treatment or assessment (Gerrits, van der Zanden, Visseher, & Conijn, 2007; Steenhuis et al., 2009). Discussion boards without a professional therapist moderator generally lack evidence-based therapeutic content (Gleeson et al., 2012). Technical difficulties in the use of online technology are a potential issue (Pretorius et al., 2010). One review of three semi rural counties in Pennsylvania demonstrates problems with firewalls, out-dated computers, and resistance to incorporating an online screening tool (Steenhuis et al., 2009). Participants in one study feel that the program is impersonal, and report an inability to express feelings to a computer, or lack of motivation to turn to a computer in times of stress/crisis, however indicate at the same time that they like the flexibility and support and actually use it as a stepping stone to further treatment (Pretorius et al., 2010). Christensen et al. (2011) identify few training schemes and highlight lack of developed standards, despite initiatives to address ethical guidelines. They address concerns that Internet therapy may encourage voyeurism and dependency and encourage a “digital divide” due to inequitable access. Additional obstacles in developing online therapy are also acknowledged, primarily lack of evidence of effectiveness of Internet interventions and the inadequate pace at which professional organisations are responding to online therapy.
Disadvantages of using email reported in the literature include concerns about potential breach of confidentiality, boundary violations, clinician failure to recognize the urgency of some email, unwanted disclosure, security issues, slow response, misinterpretation of content, and absence of text-based training (Cartwright et al., 2005; Yager, 2003a, 2003b). Other potential problems include loss of non-verbal and observational data inherent in face-to-face work (Roy & Gillett, 2008). Also, the technology is limited by individual client ownership, usage and phone plans. Email in the workplace can produce increased negative effects on employees, who may have to cope with large numbers of emails and different communication styles (Cartwright et al., 2005). The need for formal staff training in the use of email for service delivery and for procedures and guidelines specifically for child and youth mental health is identified (Cartwright et al., 2005).
Adolescents identify barriers to using CD-ROM, including finding the time to participate and technical problems (Cunningham et al., 2009; Cunningham & Wuthrich, 2008). In Cunningham et al.’s (2009) case series evaluating clinical outcomes, only two of five participants completed all eight set modules within a 12-week time frame. Disadvantages with using CD-ROMs for treatment include extensive time and resources needed to develop such programs, difficulty monitoring program use, potential technical problems, and lack of suitability for some clients (Cunningham et al., 2009; Wuthrich et al., 2012).
(vi). Research gaps
Substantively, and unlike the Internet literature, the video-conferencing articles tend to encompass child and youth mental health generally and few studies focus on a specific diagnostic category. Whilst this generalist focus is important, it behooves us to understand which service delivery methods might be best for which particular disorders when drawing on service delivery via videoconferencing. The literature points to the need for further research in telemental health, particularly for new theoretical and conceptual frameworks to guide development and evaluation of telemental health interventions (Pesamaa et al., 2004). While an accurate diagnosis or treatment recommendation can be made via technology, the literature – with few exceptions (Boydell et al, 2007) – lacks follow-up information on how effectively recommendations are carried out (Lau, Way, & Fremont, 2011). Christensen et al.’s (2011) qualitative review of research literature reports that more research is needed to understand why more young people do not engage with online mental health applications. More research, including qualitative inquiry, is needed to understand the nuances and impact of the service delivered (Boydell et al., 2007; Boydell et al., 2010). The importance of qualitative research is specifically highlighted in helping to design and develop effective Internet-based interventions for young people (Pretorius et al., 2010). Longitudinal studies are desirable to demonstrate whether the use of technology can achieve good long-term mental health outcomes (Boydell et al., 2010). Better-designed controlled trials are also needed to evaluate clinical value (Pesamaa et al., 2004). Two sub-categories included in our scoping review reveal limited studies of social networking and online games.
Discussion
Our discussion corresponds to the key research questions that form the basis of our scoping review: What is the breadth of the literature? What are the key findings? What are the research gaps?
Breadth of literature
This review identified a wide range of technologies used on a global basis to deliver mental health services to children and young people. The literature on the use of Internet technologies has emerged more recently than the videoconferencing literature, which has a longer history in terms of the evidence base. The most widely used technologies are Internet applications and videoconferencing followed by fewer articles on the use of the telephone, email, mobile phone applications and CD-ROM. The studies described are largely based on questionnaires and surveys and pre-post designs (44%). Twenty percent are focused on randomized controlled trials of CBT delivered online or via email and 15% are based on case studies. The remaining papers are descriptive studies of programs and services (11%) and qualitative studies (11%).
Thematic findings
The literature indicates that videoconferencing, the Internet and other technologies have the potential for delivering better mental health information, improved and cost effective mental health services and greater opportunities for the prevention of mental health disorders. Our scoping review demonstrates that information can be delivered consistently, accurately and comprehensively, treatments can be delivered with fidelity, and the Internet can enable storage and prompt retrieval of relevant information. Additionally, young people generally prefer treatments offered via technology.
There is consistent support and high satisfaction on the part of young people, their families and practitioners regarding videoconferencing and Internet service delivery. Nelson et al.’s (2003) RCT shows that all participants (n=14) in the videoconference condition were satisfied with the consultation and indicated that they preferred it to seeing the therapist face-to-face. In a review of telepsychiatry with children, Pakyurek and colleagues (2010) use five case studies of patients seen and argue that there is validity to the argument that in certain cases, consultation processes might be superior to face-to-face as a method of psychiatric assessment. The use of videoconferencing in service delivery shows increased access to care (Savin et al., 2006; Spaulding et al., 2010) as well as enhanced rural practitioner capacity, knowledge, shifting of practice and reduced isolation (Gelber, 2001; Greenberg et al., 2006). Studies support the success of Internet based programs for a variety of mental health issues including treatment and reduction of symptoms for anxiety and depression (Calear & Christensen, 2010; Grover et al., 2011; O’Kearney et al., 2009; Sethi et al., 2010; Stephens-Reicher et al., 2011), treatment of posttraumatic stress (Lange et al., 2001), depression prevention (van Voorhees et al., 2008), assisting carers (Jang et al., 2012; van Voorhees et al., 2008; Currie et al., 2010), and reduction of symptoms for eating disorders (Grover et al., 2011).
The issue of privacy is critical to the uptake and use of technology in the delivery of services. The use of technology raises important questions in relation to regulation and control of record access and authentication of users in situations where it is not easy for each party to verify the identity of the other (Yager, 2003a, 2003b). The issue of the possible inappropriate use of data collected on information, prevention and consumer sites is identified (Christensen et al., 2011).
Research gaps
Several central research gaps are prominent in the literature reviewed, both methodological and substantive. Even with the use of solid designs, sample sizes are frequently small and research participants are often at minimal risk or their disorder is of low severity. Methodologically, more rigorous and high-level analytic qualitative inquiry is required (Boydell et al., 2007; Boydell et al., 2010; Pretorius et al., 2010). Interventions themselves are often very brief and outcomes reported do not focus on the longer term, making longitudinal studies (Boydell et al., 2010) essential. Further, controlled trials (Pesamaa et al., 2004) are needed to further explore and evaluate the value of delivering services via technology. Substantively, in the area of videoconferencing particularly, studies that focus on specific diagnoses rather than on mental health in general are needed. An in-depth review and synthesis of the quality of findings of studies on effectiveness of the use of technologies in service delivery are also warranted. A full systematic review would provide that opportunity.
Limitations
A scoping review is not meant to be exhaustive and does not seek to weigh the quality of the evidence; the goal is to provide a good sense of the literature in a particular area and identify potential research gaps. Because issues of quality appraisal are not addressed, the scoping study has the potential to deal with a greater range of study designs and methodologies than the systematic review. It is likely that additional relevant publications were not included in this review as, due to time and cost considerations, we include only English language publications and exclude books and grey literature although we recognize that they constitute an important source of research information.
Conclusion
The use of technologies such as videoconferencing and the Internet will play a major role in the future delivery of mental health programs aimed at providing prevention, assessment, diagnosis, counseling and treatment programs. As such strategies are growing exponentially on a global basis, it is critical to study the impact of these technologies on child and youth mental health service delivery.
Supplementary Materials
Using Technology to Deliver Mental Health Services to Children and Youth: A Scoping Review
Acknowledgements/Conflicts of Interest
This scoping review was conducted as one component of a policy ready paperd on the use of technology in the delivery of mental health services and support to children and youth, commissioned and funded by the Ontario Centre of Excellence for Child and Youth Mental Health.
Footnotes
The search was completed in January, 2013 results were limited to “2000 to 2012 inclusive.”
Key search terms included: mental disease, mental health care or home mental health care or mental health service, psychiatric nursing or community psychiatric nursing, psychiatric treatment, or psychiatry mental health services or emergency services, psychiatric or social work, community psychiatry, mental disorders, community mental health services, community mental health, community mental health centers, community psychiatry mental health programs, primary mental health prevention, psychiatric clinics, mental health services, psychiatric hospital programs, psychiatry, teleconferencing, telemedicine, computer assisted diagnosis, computer assisted therapy, computer mediated communication, internet, (telepsychiatry or telepsychology or “telemental health”), electronic communication, social media, computer peripheral devices, internet usage, messages, online social networks, online therapy, mobile devices, cellular phones, websites, computers, computer assisted therapy, (“social media” or facebook or twitter or youtube or you-tube), childhood <birth to age 12 yrs> or neonatal <birth to age 1 mo> or infancy <age 2 to 23 mo> or preschool age <age 2 to 5 yrs> or school age <age 6 to 12 yrs> or adolescence <age 13 to 17 yrs> or young adulthood <age 18 to 29 yrs> limit to english language limit to yr= 2000–2012.
Various terms are used throughout the literature to describe videoconferencing and Internet based applications. In this paper, we adhere to the terms used in particular articles when describing them.
Boydell, K. M., Hodgins, M., Pignatiello, A., Teshima, J., Edwards, H., & Willis, D. (2012). Using technology to deliver mental health services to children and youth in Ontario. Ottawa, ON, The Ontario Centre of Excellence for Child and Youth Mental Health. http://www.excellenceforchildandyouth.ca/resource-hub/policy-papers.
References
- Alessi NE. Quantitative documentation of the therapeutic efficacy of adolescent telepsychiatry. Telemedicine Journal and e-Health. 2003;9(3):283–290. doi: 10.1089/153056203322502678. [DOI] [PubMed] [Google Scholar]
- Alvarez-Jimenez M, Gleeson J, Lederma R, Wadley G, Killackey E, McGorry P. Horyzons study: Online recovery for youth onset psychosis. Early Intervention in Psychiatry Conference Proceedings. 2010;4(25) [Google Scholar]
- Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology. 2005;8(1):19–32. [Google Scholar]
- Bischoff RJ, Hollist CS, Smith CW, Flack P. Addressing the mental health needs of the rural underserved: Findings from a multiple case study of a behavioral telehealth project. Contemporary Family Therapy. 2004;26(2):179–198. [Google Scholar]
- Boydell KM, Pong R, Volpe T, Tilleczek K, Wilson E, Lemieux S. Family perspectives on pathways to mental health care for children and youth in rural communities. Journal of Rural Health. 2006;22(2):182–188. doi: 10.1111/j.1748-0361.2006.00029.x. [DOI] [PubMed] [Google Scholar]
- Boydell KM, Volpe T, Kertes A, Greenberg N. A review of the outcomes of the recommendations made during paediatric telepsychiatry consultations. Journal of Telemedicine and Telecare. 2007;13:277–281. doi: 10.1258/135763307781644889. [DOI] [PubMed] [Google Scholar]
- Boydell KM, Volpe T, Pignatiello A. A qualitative a study of young people’s perspectives on receiving psychiatric services via televideo. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2010;19(1):5–11. [PMC free article] [PubMed] [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101. [Google Scholar]
- Broder E, Manson E, Boydell KM, Teshima J. Use of telepsychiatry for child psychiatric issues: First 500 cases. Canadian Psychiatric Association Bulletin. 2004;36(3):11–15. [Google Scholar]
- Brosnan E, Sharry J, Fitzpatrick C. Working Things Out: A therapeutic interactive CD-ROM containing the stories of young people dealing with depression and other mental health problems. Annual Review of CyberTherapy and Telemedicine. 2005;3:117–122. [Google Scholar]
- Burns J, Morey C, Lagelee A, Mackenzie A, Nicholas J. Reach Out! Innovation in service delivery. Medical Journal of Australia. 2007;187(7):31–34. doi: 10.5694/j.1326-5377.2007.tb01333.x. [DOI] [PubMed] [Google Scholar]
- Burns J, Webb M, Durkin LA, Hickie IB. Reach Out Central: A serious game designed to engage young men to improve mental health and wellbeing. Medical Journal of Australia. 2010;192(11):27–30. doi: 10.5694/j.1326-5377.2010.tb03689.x. [DOI] [PubMed] [Google Scholar]
- Calear AL, Christensen H, Mackinnon A, Griffiths KM, O’Kearney R. The YouthMood Project: A cluster randomized controlled trial of an online cognitive behavioural program with adolescents. Journal of Consulting and Clinical Psychology. 2009;77(6):1021–1032. doi: 10.1037/a0017391. [DOI] [PubMed] [Google Scholar]
- Calear AL, Christensen H. Review of internet-based prevention and treatment programs for anxiety and depression in children and adolescents. [Review] Medical Journal of Australia. 2010;192(11 Suppl):S12–14. doi: 10.5694/j.1326-5377.2010.tb03686.x. [DOI] [PubMed] [Google Scholar]
- Cartwright M, Gibbon P, McDermott BM, Bor W. The use of email in a child and adolescent mental health service: Are staff ready? Journal of Telemedicine and Telecare. 2005;11(4):199–204. doi: 10.1258/1357633054068865. [DOI] [PubMed] [Google Scholar]
- Chlebowski S, Fremont W. Therapeutic uses of the WebCam in child psychiatry. Academic Psychiatry. 2011;35:263–267. doi: 10.1176/appi.ap.35.4.263. [DOI] [PubMed] [Google Scholar]
- Christensen H, Griffiths KM, Korten A. Web-based cognitive behaviour therapy: Analysis of site usage and changes in depression and anxiety scores. Journal of Medical Internet Research. 2002;4(1):e3. doi: 10.2196/jmir.4.1.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen H, Reynolds J, Griffiths KM. The use of e-health applications for anxiety and depression in young people: Challenges and solutions. Early Intervention in Psychiatry. 2011;5(Suppl 1):58–62. doi: 10.1111/j.1751-7893.2010.00242.x. [DOI] [PubMed] [Google Scholar]
- Clarke G, Kelleher C, Hornbrook M, Debar L, Dickerson J, Gullion C. Randomized effectiveness trial of an Internet, pure self-help, cognitive behavioural intervention for depressive symptoms in young adults. Cognitive Behaviour Therapy. 2009;38(4):222–234. doi: 10.1080/16506070802675353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz M, Krupinski EA, Lopez AM, Weinstein RS. A review of the first five years of the University of Arizona telepsychiatry programme. Journal of Telemedicine and Telecare. 2005;11:234–239. doi: 10.1258/1357633054471821. [DOI] [PubMed] [Google Scholar]
- Cunningham MJ, Wuthrich VM, Rapee RM, Lyneham HJ, Schniering CA, Hudson JL. The Cool Teens CD-ROM for anxiety disorders in adolescents: a pilot case series. European Child and Adolescent Psychiatry. 2009;18(2):125–129. doi: 10.1007/s00787-008-0703-y. [DOI] [PubMed] [Google Scholar]
- Cunningham M, Wuthrich V. Examination of barriers to treatment and user preferences with computer-based therapy using the Cool Teens CD for adolescent anxiety. E-Journal of Applied Psychology. 2008;4(2):12–17. [Google Scholar]
- Currie SL, Mcgrath PJ, Day V. Development and usability of an online CBT program for symptoms of moderate depression, anxiety, and stress in post-secondary students. Computers in Human Behaviour. 2010;26(6):1419–1426. [Google Scholar]
- Diamond JM, Block RM. Telepsychiatry assessments of child or adolescent behaviour disorders: A review of evidence and issues. Telemedicine and e-Health. 2010;16(6):712–716. doi: 10.1089/tmj.2010.0007. [DOI] [PubMed] [Google Scholar]
- Diamond G, Levy S, Bevans K, Fein J, Wintersteen M, Tien A, Creed T. Development, validation, and utility of internet-based, behavioral health screen for adolescents. Pediatrics. 2010;126(1):163–170. doi: 10.1542/peds.2009-3272. [DOI] [PubMed] [Google Scholar]
- Elford DR, White H, St John K, Maddigan B, Ghandi M, Bowering R. A prospective satisfaction study and cost analysis of a pilot child telepsychiatry service in Newfoundland. Journal of Telemedicine and Telecare. 2001;7:73–81. doi: 10.1258/1357633011936192. [DOI] [PubMed] [Google Scholar]
- Elford R, White H, Bowering R, Ghandi A, Maddiggan B, St John K, Battcock A. A randomized, controlled trial of child psychiatric assessments conducted using videoconferencing. Journal of Telemedicine and Telecare. 2000;6:73–82. doi: 10.1258/1357633001935086. [DOI] [PubMed] [Google Scholar]
- Fukkink R. Peer counselling in an online chat service: A content analysis of social support. Cyberpsychology, Behaviour and Social Networking. 2011;14(4):247–251. doi: 10.1089/cyber.2010.0163. [DOI] [PubMed] [Google Scholar]
- Fukkink RG, Hermanns J. Children’s experiences with chat support and telephone support. Journal of Child Psychology and Psychiatry. 2009;50(6):759–766. doi: 10.1111/j.1469-7610.2008.02024.x. [DOI] [PubMed] [Google Scholar]
- Gelber H. The experience in Victoria with telepsychiatry for the child and adolescent mental health service. Journal of Telemedicine and Telecare. 2001;7(Suppl. 2):32–34. doi: 10.1258/1357633011937065. [DOI] [PubMed] [Google Scholar]
- Gerrits R, van der Zanden R, Visscher R, Conijn B. Master your mood online: A preventive chat group intervention for adolescents. Australian e-Journal for the Advancement of Mental Health. 2007;6(3):1–11. [Google Scholar]
- Gleeson J, Alvarez-Jimenez M, Lederman R. Moderated online social therapy for recovery from early psychosis. Psychiatric Services. 2012;63(7):719. doi: 10.1176/appi.ps.20120p719. [DOI] [PubMed] [Google Scholar]
- Gowen K, Deschaine M, Gruttadara D, Markey D. Young adults with mental health conditions and social networking websites: Seeking tools to build community. Psychiatric Rehabilitation Journal. 2012;35(3):245–250. doi: 10.2975/35.3.2012.245.250. [DOI] [PubMed] [Google Scholar]
- Grealish A, Hunter A, Glazez R, Potterz L. Telemedicine in a child and adolescent mental health service: Participants’ acceptance and utilization. Journal of Telemedicine and Telecare. 2005;11(Suppl. 1):53–55. doi: 10.1258/1357633054461921. [DOI] [PubMed] [Google Scholar]
- Greenberg N, Boydell KM, Volpe T. Pediatric telepsychiatry in Ontario: Service provider and caregiver perspectives. Journal of Behavioral Health Services & Research. 2006;33(1):105–111. doi: 10.1007/s11414-005-9001-3. [DOI] [PubMed] [Google Scholar]
- Greenhalgh T, Russell J, Ashcroft R, Parsons W. Why national eHealth programs need dead philosophers: Wittgensteinian reflections on policymakers’ reluctance to learn from history. The Milbank Quarterly. 2011;89(4):533–563. doi: 10.1111/j.1468-0009.2011.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grover M, Naumann U, Mohammaddar L, Glennon D, Ringwood S, Eisler I, Schmidt U. A randomized controlled trial of an Internet-based cognitive-behavioural skills package for carers of people with anorexia nervosa. Psychological Medicine. 2011;41(12):2581–2591. doi: 10.1017/S0033291711000766. [DOI] [PubMed] [Google Scholar]
- Heinicke BE, Paxton SJ, Mclean SA, Wertheim EH. Internet-delivered targeted group intervention for body dissatisfaction and disordered eating in adolescent girls: A randomized controlled trial. Journal of Abnormal Child Psychology. 2007;35(3):379–391. doi: 10.1007/s10802-006-9097-9. [DOI] [PubMed] [Google Scholar]
- Hilty DM, Yellowlees PM, Nesbitt TS. Evolution of telepsychiatry to rural sites: Changes over time in types of referral and in primary care providers’ knowledge, skills and satisfaction. General Hospital Psychiatry. 2006;28:367–373. doi: 10.1016/j.genhosppsych.2006.05.009. [DOI] [PubMed] [Google Scholar]
- Hilty DM, Yellowlees PM, Sonik P, Derlet M, Hendren RL. Rural child and adolescent telepsychiatry: Successes and struggles. Pediatric Annals. 2009;38(4):228–232. [PubMed] [Google Scholar]
- Hoek W, Marko M, Fogel J, Schuurmans J, Gladstone T, Bradford N, Van Voorhees BW. A randomized controlled trial of a primary care Internet-based depression prevention intervention for adolescents: 6-month outcomes and predictors of improvement. Translational Research. 2011;158(6):315–325. doi: 10.1016/j.trsl.2011.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang J, Dixon DR, Tarbox J, Granpeesheh D, Kornack J, De Nocker Y. Randomized trial of an eLearning program for training family members of children with autism in the principles and procedures of applied behaviour analysis. Research in Autism Spectrum Disorders. 2012;6(2):852–856. [Google Scholar]
- Kauer S, Reid S, Crooke A, Khor A, Hearps S, Jorm A, Patton G. Self-monitoring using mobile phones in the early stages of adolescent depression: Randomized controlled trial. Journal of Medical Internet Research. 2012;14(3):67–87. doi: 10.2196/jmir.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keilman P. Telepsychiatry with child welfare families referred to a family service agency. Telemedicine and e-Health. 2005;11(1):98–101. doi: 10.1089/tmj.2005.11.98. [DOI] [PubMed] [Google Scholar]
- King R, Bambling M, Reid W, Thomas I. Telephone and online counselling for young people: A naturalistic comparison of session outcome, session impact and therapeutic alliance. Counselling and Psychotherapy Research. 2006;6(3):175–181. [Google Scholar]
- King R, Nurcombe B, Bickman L, Hides L, Reid W. Telephone counselling for adolescent suicide prevention: Changes in suicidality and mental state from beginning to end of a counseling session. Suicide & Life-Threatening Behavior. 2003;33(4):400–411. doi: 10.1521/suli.33.4.400.25235. [DOI] [PubMed] [Google Scholar]
- Kirby MJL, Keon WJ. Out of the Shadows at Last: Transforming Mental Health, Mental Illness and Addiction Services in Canada. Highlights and Recommendations: Children and Youth. Ottawa, ON: Standing Senate Committee on Social Affairs Science and Technology; 2006. pp. 135–155. Retrieved from http://www.parl.gc.ca/39/1/parlbus/commbus/senate/com-e/soci-e/rep-e/rep02may06part2-e.htm#_Toc133223085. [Google Scholar]
- Kopel H, Nunn K, Dossetor D. Evaluating satisfaction with a child and adolescent psychological telemedicine outreach service. Journal of Telemedicine and Telecare. 2001;7(Suppl. 2):35–40. doi: 10.1258/1357633011937074. [DOI] [PubMed] [Google Scholar]
- Landback J, Prochaska M, Ellis J, Dmochowska K, Kuwabara SA, Gladstone T, Van Voorhees BW. From prototype to product: Development of a primary care/internet based depression prevention intervention for adolescents (CATCH-IT) Community Mental Health Journal. 2009;45(5):349–354. doi: 10.1007/s10597-009-9226-3. [DOI] [PubMed] [Google Scholar]
- Lange A, van de Ven JP, Schrieken B, Emmelkamp PM. Interapy: Treatment of posttraumatic stress through the Internet: A controlled trial. Journal of Behavior Therapy and Experimental Psychiatry. 2001;32(2):73–90. doi: 10.1016/s0005-7916(01)00023-4. [DOI] [PubMed] [Google Scholar]
- Lau ME, Way BB, Fremont WP. Assessment of SUNY Upstate Medical University’s Child Telepsychiatry Consultation Program. International Journal of Psychiatry in Medicine. 2011;42(1):93–104. doi: 10.2190/PM.42.1.g. [DOI] [PubMed] [Google Scholar]
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: Advancing the methodology. Implementation Science. 2010;5(69) doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lingely-Pottie P, McGrath PJ. A therapeutic alliance can exist without face-to-face contact. Journal of Telemedicine and Telecare. 2006;12:396–399. doi: 10.1258/135763306779378690. [DOI] [PubMed] [Google Scholar]
- Lingley-Pottie P, McGrath PJ. Telehealth: A child and family-friendly approach to mental health-care reform. Journal of Telemedicine and Telecare. 2008;14:225–226. doi: 10.1258/jtt.2008.008001. [DOI] [PubMed] [Google Scholar]
- Lyneham HJ, Rapee RM. Evaluation of therapist-supported parent-implemented CBT for anxiety disorders in rural children. Behaviour Research and Therapy. 2006;44(9):1287–1300. doi: 10.1016/j.brat.2005.09.009. [DOI] [PubMed] [Google Scholar]
- March S, Spence SH, Donovan CL. The efficacy of an Internet-based cognitive-behavioral therapy intervention for child anxiety disorders. Journal of Pediatric Psychology. 2009;34(5):474–487. doi: 10.1093/jpepsy/jsn099. [DOI] [PubMed] [Google Scholar]
- McGrath PJ, Lingley-Pottie P, Thurston C, Maclean C, Cunningham C, Waschbusch DA, Chaplin W. Telephone-based mental health interventions for child disruptive behavior or anxiety disorders: Randomized trial and overall analysis. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50(11):1162–1172. doi: 10.1016/j.jaac.2011.07.013. [DOI] [PubMed] [Google Scholar]
- Mehta S, Chalhoub N. An E-mail for your thoughts. Child and Adolescent Mental Health. 2006;11(3):168–170. doi: 10.1111/j.1475-3588.2006.00405.x. [DOI] [PubMed] [Google Scholar]
- Merry SN, Stasiak K, Shepherd M, Frampton C, Fleming T, Lucassen MFG. The effectiveness of SPARX, a computerised self help intervention for adolescents seeking help for depression: Randomised controlled non-inferiority trial. British Medical Journal. 2012;344(e2598) doi: 10.1136/bmj.e2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller TW, Kraus R, Fotto Kaak O, Sprang R, Burton D. Telemedicine: A child psychiatry case report. Telemedicine Journal and e-Health. 2002;6(1):139. doi: 10.1089/15305620252933482. [DOI] [PubMed] [Google Scholar]
- Myers KM, Valentine J, Morganthaler R, Melzer S. Telepsychiatry with incarcerated youth. Journal of Adolescent Health. 2006;38:643–648. doi: 10.1016/j.jadohealth.2005.07.015. [DOI] [PubMed] [Google Scholar]
- Myers KM, Valentine JM, Melzer SM. Feasibility, acceptability, and sustainability of telepsychiatry for children and adolescents. Psychiatric Services. 2007;58(11):1493–1497. doi: 10.1176/ps.2007.58.11.1493. [DOI] [PubMed] [Google Scholar]
- Myers KM, Valentine JM, Melzer SM. Child and adolescent telepsychiatry: Utilization and satisfaction. Telemedicine and e-Health. 2008;14(2):131–137. doi: 10.1089/tmj.2007.0035. [DOI] [PubMed] [Google Scholar]
- Myers KM, Vander Stoep A, Mccarty CA, Klein JB, Palmer NB, Geyer JR, Melzer SM. Child and adolescent telepsychiatry: Variations in utilization, referral patterns and practice trends. Journal of Telemedicine and Telecare. 2010;16:128–133. doi: 10.1258/jtt.2009.090712. [DOI] [PubMed] [Google Scholar]
- Nelson EL, Barnard M, Cain S. Treating childhood depression over videoconferencing. Telemedicine Journal and e-Health. 2003;9(1):49–55. doi: 10.1089/153056203763317648. [DOI] [PubMed] [Google Scholar]
- Nelson EL, Bui T. Rural Telepsychology services for children and adolescents. Journal of Clinical Psychology: In Session. 2010;66(5):490–501. doi: 10.1002/jclp.20682. [DOI] [PubMed] [Google Scholar]
- O’Kearney R, Gibson M, Christensen H, Griffiths K. Effects of a cognitive-behavioural internet program on depression, vulnerability to depression and stigma in adolescent males: A school-based controlled trial. Cognitive Behaviour Therapy. 2006;35(1):43–54. doi: 10.1080/16506070500303456. [DOI] [PubMed] [Google Scholar]
- O’Kearney R, Kang K, Christensen H, Griffiths K. A controlled trial of a school-based Internet program for reducing depressive symptoms in adolescent girls. Depression and Anxiety. 2009;26(1):65–72. doi: 10.1002/da.20507. [DOI] [PubMed] [Google Scholar]
- Pakyurek M, Yellowlees P, Hilty D. The child and adolescent telepsychiatry consultation: Can it be a more effective clinical process for certain patients than conventional practice? Telemedicine and e-Health. 2010;16(3):289–292. doi: 10.1089/tmj.2009.0130. [DOI] [PubMed] [Google Scholar]
- Parker Z, Steele M, Junek W, Morin L, Davidson S, Fleisher W, Yates T. Child Psychiatry in Canada: Physician Resources Position Statement of the Canadian Academy of Child Psychiatry. Ottawa, ON: Canadian Psychiatric Association; 2003. [Google Scholar]
- Pesamaa L, Ebeling H, Kuusamaki ML, Winblad I, Isohanni M, Moilanen I. Videoconferencing in child and adolescent psychiatry in Finland – an inadequately exploited resource. Journal of Telemedicine and Telecare. 2007;13:125–129. doi: 10.1258/135763307780677631. [DOI] [PubMed] [Google Scholar]
- Pesamaa L, Ebeling H, Kuusamaki ML, Winblad I, Isohanni M, Moilanen I. Videoconferencing in child and adolescent telepsychiatry: A systematic review of the literature. Journal of Telemedicine and Telecare. 2004;10:187–192. doi: 10.1258/1357633041424458. [DOI] [PubMed] [Google Scholar]
- Pignatiello T, Boydell KM, Teshima J, Volpe T. Supporting primary care through pediatric telepsychiatry. Canadian Journal of Community Mental Health. 2010;27(2):139–151. [Google Scholar]
- Pretorius N, Arcelus J, Beecham J, Dawson H, Doherty F, Eisler I, Schmidt U. Cognitive-behavioural therapy for adolescents with bulimic symptomatology: The acceptability and effectiveness of internet-based delivery. Behaviour Research and Therapy. 2009;47(9):729–736. doi: 10.1016/j.brat.2009.05.006. [DOI] [PubMed] [Google Scholar]
- Pretorius N, Rowlands L, Ringwood S, Schmidt U. Young people’s perceptions of and reasons for accessing a web-based cognitive behavioural intervention for bulimia nervosa. European Eating Disorders Review. 2010;18(3):197–206. doi: 10.1002/erv.985. [DOI] [PubMed] [Google Scholar]
- Radhu N, Daskalakis ZJ, Arpin-Cribbie CA, Irvine J, Ritvo P. Evaluating a web-based cognitive-behavioral therapy for maladaptive perfectionism in university students. Journal of American College Health. 2012;60(5):357–366. doi: 10.1080/07448481.2011.630703. [DOI] [PubMed] [Google Scholar]
- Read JP, Farrow SM, Jaanimagi U, Ouimette P. Assessing trauma and traumatic stress via the Internet: Measurement equivalence and participant reactions. Traumatology. 2009;15(1):94–102. [Google Scholar]
- Reed GM, McLaughlin CJ, Milholland K. Ten interdisciplinary principles for professional practice in telehealth: Implications for psychology. Professional Psychology: Research and Practice. 2000;31:170–178. [Google Scholar]
- Reid S, Kauer S, Hearps S, Crooke A, Khor A, Sanci L, Patton G. A mobile phone application for the assessment and management of youth mental health problems in primary care: A randomised controlled trial. BMC Family Practice. 2011;12:131–144. doi: 10.1186/1471-2296-12-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid S, Kauer S, Khor A, Hearps S, Sanci L, Kennedy A, Patton G. Using a mobile phone application in youth mental health: An evaluation study. Australian Family Physician. 2012;41(9):711–714. [PubMed] [Google Scholar]
- Richards D. Features and benefits of online counselling: Trinity College online mental health community. British Journal of Guidance & Counselling. 2009;37(3):231–242. [Google Scholar]
- Roy H, Gillett T. E-mail: A new technique for forming a therapeutic alliance with high-risk young people failing to engage with mental health services? A case study. Clinical Child Psychology and Psychiatry. 2008;13(1):95–103. doi: 10.1177/1359104507086344. [DOI] [PubMed] [Google Scholar]
- Savin D, Garry MT, Zuccaro P, Novins D. Telepsychiatry for treating rural American Indian youth. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(4):484–488. doi: 10.1097/01.chi.0000198594.68820.59. [DOI] [PubMed] [Google Scholar]
- Sethi S, Campbell AJ, Ellis LA. The use of computerized self-help packages to treat adolescent depression and anxiety. Journal of Technology in Human Services. 2010;28(3):144–160. [Google Scholar]
- Shandley K, Austin D, Klein B, Kyrios M. An evaluation of ‘Reach Out Central’: An online gaming program for supporting the mental health of young people. Health Education Research. 2010;25(4):563–574. doi: 10.1093/her/cyq002. [DOI] [PubMed] [Google Scholar]
- Spaulding R, Belz N, Delurgio S, Williams AR. Cost savings of telemedicine utilization for child psychiatry in a rural Kansas community. Telemedicine and e-Health. 2010;16(8):867–871. doi: 10.1089/tmj.2010.0054. [DOI] [PubMed] [Google Scholar]
- Spence SH, Donovan CL, March S, Gamble A, Anderson R, Prosser S, Kenardy J. Online CBT in the treatment of child and adolescent anxiety disorders: Issues in the development of BRAVE-ONLINE and two case illustrations. Behavioural and Cognitive Psychotherapy. 2008;36(4):411–430. [Google Scholar]
- Spence SH, Donovan CL, March S, Gamble A, Anderson RE, Prosser S, Kenardy J. A randomized controlled trial of online versus clinic-based CBT for adolescent anxiety. Journal of Consulting and Clinical Psychology. 2011;79(5):629–642. doi: 10.1037/a0024512. [DOI] [PubMed] [Google Scholar]
- Spence SH, Holmes JM, March S, Lipp OV. The feasibility and outcome of clinic plus Internet delivery of cognitive-behavior therapy for childhood anxiety. Journal of Consultation and Clinical Psychology. 2006;74(3):614–621. doi: 10.1037/0022-006X.74.3.614. [DOI] [PubMed] [Google Scholar]
- Starling J, Rosina R, Nunn K, Dossetor D. Child and adolescent telepsychiatry in New South Wales: Moving beyond clinical consultation. Australasian Psychiatry. 2003;11S:S117–S121. [Google Scholar]
- Starling J, Foley S. From pilot to permanent service: Ten years of paediatric telepsychiatry. Journal of Telemedicine and Telecare. 2006;12(Suppl. 3):80–82. [Google Scholar]
- Steenhuis MP, Serra M, Minderaa RB, Hartman CA. An Internet version of the diagnostic interview schedule for children (disc-iv): Correspondence of the ADHD section with the paper-and-pencil version. Psychological Assessment. 2009;21(2):231–234. doi: 10.1037/a0015925. [DOI] [PubMed] [Google Scholar]
- Stephens-Reicher J, Metcalf A, Blanchard M, Mangan C, Burns J. Reaching the hard-to-reach: How information communication technologies can reach young people at greater risk of mental health difficulties. Australasian Psychiatry. 2011;19(Suppl 1):S58–61. doi: 10.3109/10398562.2011.583077. [DOI] [PubMed] [Google Scholar]
- Trockel M, Manber R, Chang V, Thurston A, Taylor CB. An e-mail delivered CBT for sleep-health program for college students: Effects on sleep quality and depression symptoms. Journal of Clinical Sleep Medicine. 2011;7(3):276–281. doi: 10.5664/JCSM.1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner C, Heyman I. A pilot study of telephone cognitive-behavioural therapy for obsessive-compulsive disorder in young People. Behavioural and Cognitive Psychotherapy. 2009;37:469–474. doi: 10.1017/S1352465809990178. [DOI] [PubMed] [Google Scholar]
- van der Zanden R, Kramer J, Gerrits R, Cuijpers P. Effectiveness of an online group course for depression in adolescents and young adults: A randomized trial. Journal of Medical Internet Research. 2012;14(3):e86. doi: 10.2196/jmir.2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Voorhees BW, Ellis J, Stuart S, Fogel J, Ford D. Pilot study of a primary care internet-based depression prevention intervention for late adolescents. Canadian Child and Adolescent Psychiatry Review. 2005;14(2):40–43. [PMC free article] [PubMed] [Google Scholar]
- van Voorhees BW, Fogel J, Reinecke MA, Gladstone T, Stuart S, Gollan J, Bell C. Randomized clinical trial of an Internet-based depression prevention program for adolescents (Project CATCH-IT) in primary care: 12-week outcomes. Journal of Developmental and Behavioral Pediatrics. 2009;30(1):23–37. doi: 10.1097/DBP.0b013e3181966c2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Voorhees BW, Vanderplough-Booth K, Fogel J, Gladstone T, Bell C, Stuart S, Reinecke MA. Integrative internet-based depression prevention for adolescents: A randomized clinical trial in primary care for vulnerability and protective factors. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2008;17(4):184–196. [PMC free article] [PubMed] [Google Scholar]
- Volpe T, Boydell KM, Pignatiello A. Attracting child psychiatrists to a televideo consultation service: The TeleLink experience. International Journal of Telemedicine and Applications. 2013. p. 8. Article ID 146858. http://dx.doi.org/10.1155/2013/146858. [DOI] [PMC free article] [PubMed]
- Webb M, Burns J, Collin P. Providing online support for young people with mental health difficulties: Challenges and opportunities explored. Early Intervention in Psychiatry. 2008;2(2):108–113. doi: 10.1111/j.1751-7893.2008.00066.x. [DOI] [PubMed] [Google Scholar]
- Whittaker R, Merry S, Stasiak K, Mcdowell H, Doherty I, Shepherd M, Rodgers A. MEMO-A mobile phone depression prevent/intervention for adolescents: Development process post program findings on acceptability from a randomized controlled trial. Journal of Medical Internet Research. 2012;14(1):169–179. doi: 10.2196/jmir.1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wuthrich V, Rapee R, Cunningham M, Lyneham H, Hudson J, Schniering CA. A randomized controlled trial of the Cool Teens CD-ROM computerized program for adolescent anxiety. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51(3):261–270. doi: 10.1016/j.jaac.2011.12.002. [DOI] [PubMed] [Google Scholar]
- Yager J. E-mail therapy for anorexia nervosa: Prospects and limitations. European Eating Disorders Review. 2003a;11(3):198–209. [Google Scholar]
- Yager J. Monitoring patients with eating disorders by using e-mail as an adjunct to clinical activities. Psychiatric Services. 2003b;54(12):1586–1588. doi: 10.1176/appi.ps.54.12.1586. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Using Technology to Deliver Mental Health Services to Children and Youth: A Scoping Review