Abstract
Hypertension is a major public health problem due to its high prevalence and cardiovascular complications. Its treatment is aimed at reducing cardiovascular morbidity and mortality, its goal being to maintain blood pressure levels below 140/90 mm Hg. Hypertension control in Brazil is low, and nationwide rates are unknown. The objective of this review was to provide an overview on hypertension control in Brazil from publications in a database. We identified 45 publications. In population-based studies, the highest control rate (57.6%) was reported in a multicenter study in 100 municipalities and the city of São José do Rio Preto, São Paulo state (52.4%), while the lowest rates (around 10%) were identified in microregions of the Rio Grande do Sul state and in the city of Tubarão, Santa Catarina state. In conclusion, the studies assessed showed a wide variation in hypertension control rates. It is worth noting that the comparison between studies was a major limiting factor, because of the different methods used.
Keywords: Hypertension / complications, Review, Hypertension / prevetion & control, Medication Adherence
Introduction
Arterial hypertension is an important public health problem because of its high prevalence and associated cardiovascular complications. Brazilian epidemiological studies have reported arterial hypertension prevalence ranging from 19.2% to 44.4%1. It is generally estimated that more than 30% of Brazilians have arterial hypertension, similarly to the world population2. In 2010, cardiovascular diseases corresponded to 30.6% and 13.4% of the total deaths and hospitalizations of adults aged at least 20 years, respectively3. The treatment of arterial hypertension is aimed at reducing cardiovascular morbidity and mortality, and the blood pressure control goal proposed by the VI Brazilian Guidelines of Arterial Hypertension is systolic and diastolic blood pressure levels lower than 140 mm Hg and 90 mm Hg, respectively. More severe reductions can be aimed depending on the cardiovascular risk profile.
Knowing the control levels for arterial hypertension is highly relevant in planning the therapeutic resources and assessing the extension and effectiveness of the measures adopted. Although arterial hypertension control in Brazil is believed to be low, national rates are unknown. This systematic review of the literature was aimed at providing an overview of arterial hypertension control in Brazil based on publications from a national access-free database, containing full original texts.
Method
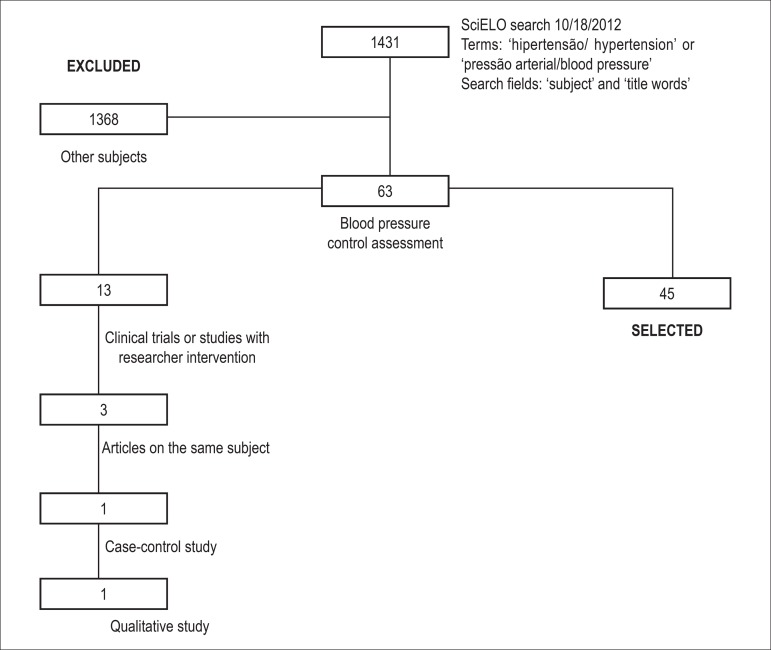
This study is a systematic review of the literature about arterial hypertension control in Brazil. Aiming primarily at elaborating a database of arterial hypertension articles, a bibliographic survey of publications indexed at the Scientific Electronic Library Online (SciELO) was conducted in October 2012. SciELO was chosen because it comprises a selected collection of Brazilian scientific periodicals. The terms "hipertensão/hypertension" and "pressão arterial/blood pressure" were used in the search fields "subject" and "title words", with restriction of neither time period nor idiom, resulting in 1,431 publications.
The present study selected articles with a cross-sectional design and reporting on arterial hypertension control in Brazil. Figure 1 shows the flowchart of the selection of articles. In the case of articles elaborated based on the study of the same cohort, the oldest publication was chosen (n = 3). The articles selected (n = 45) were characterized regarding the year of publication, site of study conduction, subject of the journal, population studied, blood pressure assessment and results of arterial hypertension control. The control rates were presented as percentages of controlled hypertensives described in the articles (n = 37) or based on the subtraction of the percentages of uncontrolled hypertensives from the number 100, described in the article (100 - uncontrolled %, n = 8). The publications were grouped as follows: population-based studies (n = 13); site of study conduction, primary or secondary health care (n = 15); studies with specific populations (n = 12); and studies with interventions (n = 5).
Figure 1.
Flowchart of the selection of articles on arterial hypertension control.
Results
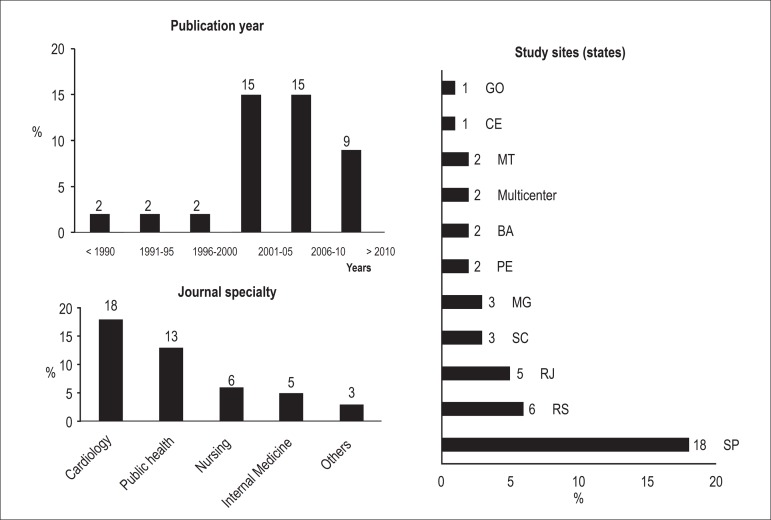
An increase in the number of publications on arterial hypertension control has been observed since 2001 (13.3%, from 1988 to 2000, versus 86.7%, from 2001 to 2012). Regarding the periodicals in which the articles were published, medical journals predominated. Journals of cardiology were the most frequent ones (40.0%), followed by those of public health (28.9%). Journals of nursing contributed with 13.3%, and there was only one publication in a journal of pharmacy. The Brazilian southeastern region corresponded to 57.8% of the sites of study conduction, followed by the southern (20%), northeastern (11.1%) and west-central (6.7%) regions. Two studies were performed in multiple centers in the five geographical regions of the country, and none was conducted exclusively in the northern region. São Paulo state accounted for 40% of the study sites (Figure 2).
Figure 2.
Publication time, journal specialty, and study sites (São Paulo, 2012).
Hypertension control was assessed by use of blood pressure measurement in 32 studies (72.7%). The other studies assessed the registry of blood pressure in medical records (22.7%). One study used blood pressure self-report via telephone call, and another did not inform the blood pressure assessment method. Measurement at the medical office was performed in 32 studies, two of which also carried out ambulatory blood pressure monitoring (ABPM), while another performed home blood pressure monitoring (HBPM) in addition to measurement at medical office. Of the studies measuring blood pressure at the medical office, one third used mercury column devices. Oscillometric devices were used in nine studies, seven of which reported device validation. Eight studies used aneroid devices, manometer calibration being reported in six. Five articles provided no description of blood pressure measurement equipment. Two and three blood pressure measurements per individual predominated in the studies assessed (42.4% and 30.3% of the studies, respectively).
The most common source of recommendation for blood pressure measurement at the medical office was the Brazilian Guidelines of Arterial Hypertension, accounting for 33.3% of the articles, followed by the VI Joint National Committee, 21.2% of the articles. One study informed the World Health Organization as the source of recommendation for blood pressure measurement, another, the American Heart Association, and 13 studies did not mention any. Training of the professional responsible for blood pressure measurement was reported in 57.6% of the studies, while appropriateness of the cuff to arm circumference was mentioned by only 39.4%.
The population-based studies adopted different values of blood pressure control. Only publications from 2001 onward considered values lower than 140 mm Hg and 90 mm Hg for systolic and diastolic blood pressures, respectively. Of those publications, the multicenter study in 100 municipalities and in the city of São José do Rio Preto, São Paulo state, reported the highest control rates (57.6% and 52.4%, respectively). The lowest percentages, around 10%, were identified in microregions of the Rio Grande do Sul state and in the municipality of Tubarão, Santa Catarina state. Most of those articles (n = 7) assessed arterial hypertension control in hypertensives undergoing antihypertensive treatment, reporting rates ranging from 10.1% to 52.4%4-10. Arterial hypertension control of individuals knowing their hypertensive condition (n = 3) ranged from 31.3% to 57.6%11-13. Two articles assessed arterial hypertension control in the total number of hypertensives identified in the sample, reporting rates of 10.4% and 24.2%14,15. Klein et al16 reported the value of arterial hypertension control in the entire population studied (hypertensives and not hypertensives) as of 8.8%, corresponding to 60% of the hypertensives treated (Table 1).
Table 1.
Arterial hypertension control in Brazilian population-based studies (São Paulo, 2012)
| Article | Study site | Population* | Control (%) |
|---|---|---|---|
| dos Santos et al4 | Cáceres, MT | > 10 years | 55.2% men 28.6% women# |
| Piccini e Victora5 | Pelotas, RS | 20-69 years | 32¢ |
| Klein et al16 | Ilha do Governador, RJ | > 20 years | 8.8§ |
| Trindade et al6 | Passo fundo, RS | 18-74 years | 37.5§ |
| Freitas et al7 | Catanduva, SP | ≥ 18 years | 27.6§ |
| Fuchs et al8 | Porto Alegre, RS | ≥ 18 years | 62§ |
| 36¥ | |||
| Gus et al14 | Microregions, RS | ≥ 20 years | 10.4¥ |
| Pereira et al9 | Tubarão, SC | ≥ 18 years | 10.1¥ |
| Rosário et al15 | Nobres, MT | 18-90 years | 24.2¥ |
| Cipullo et al10 | S José Rio Preto, SP | ≥ 18 years | 52.4¥ |
| Mion Jr et al.11 | São Paulo, SP | ≥ 18 years | 35.2¥ |
| Lyra et al.12 | Canaã, PE | ≥ 30 years | 31.3¥ |
| Piccini et al.13 | 100 Brazilian municipalities | 20-59 years | 57.6¥ |
Population representative sample.
hypertension control (systolic and diastolic blood pressure, respectively): < 140 mm Hg and < 90 mm Hg (15-19 years), 150 mm Hg and 90 mm Hg (20-39 years), and 160 mm Hg and 95 mm Hg (≥ 30 years).
hypertension control: < 160 (systolic) and 90 mm Hg (diastolic).
hypertension control: < 160 (systolic) and 95 mm Hg (diastolic).
hypertension control: <140 (systolic) and 90 mm Hg (diastolic).
Among hypertensives in the Family Health Program17-19, the arterial hypertension control rates ranged from 20.0% to 30.7%, and among those being followed up in basic health units, from 30.0% to 53.9%19-21. Arterial hypertension control among hypertensives in secondary health care was assessed in 24.4% of the studies, ten being performed at hypertension outpatient clinics22-31 and one at an internal medicine outpatient clinic32. The lowest control rate was identified in the city of Peruíbe, São Paulo state; however, when blood pressure was assessed by use of home measurement, a significant increase in control was observed (9.9% versus 23.9%)30. The highest control levels in hypertensives of primary health care were obtained in the cities of Porto Alegre (53.9%)21 and São Paulo (45.5%)20 (Table 2).
Table 2.
Arterial hypertension control in Brazilian studies in the primary and secondary health care context (São Paulo, 2012)
| Article | Study site | Population | Control (%) |
|---|---|---|---|
| Pierin et al22 | São Paulo, SP | Outpatient clinic, > 18 years, (n = 205) | 31* |
| Freitas et al23 | São Paulo, SP | Outpatient clinic, > 18 years (n = 1210), | 20.9* |
| Diabetic hypertensives (n = 290) | 23.4* | ||
| Strelec et al24 | São Paulo, SP | Health Care Center, > 18 years (n = 130) | 35* |
| Muxfeldt et al32 | Rio de Janeiro, RJ | Outpatient clinic, adults (n = 1699) | 27* |
| Sanchez et al25 | São Paulo, SP | Outpatient clinic, > 18 years (n = 100) | 35* |
| Coelho et al26 | Ribeirão Preto, SP | Outpatient clinic, 17-86 years (n=245) | 27.8* |
| Mano et al17 | São Paulo, SP | School Health Care Center, > 18 years (n = 113) | 30* |
| FHP, > 18 years (n = 113) | 20* | ||
| Jesus et al27 | São Paulo, SP | Outpatient clinic, > 18 years (n = 511) | |
| 24% women* | |||
| Magnanini et al28 | Rio de Janeiro, RJ | Outpatient clinic, women, resistant hypertension, 24-92 years (n = 382) | 42.4§ |
| Helena et al18 | Blumenau, SC | FHP, adults (n = 595) | 30.7* |
| Pierin et al29 | São Paulo, SP | Outpatient clinic, > 18 years, (251 uncomplicated hypertensives, 260 complicated hypertensives) | |
| uncomplicated hypertension, 29.1%* | |||
| Pierin et al20 | São Paulo, SP | BHCU, adults (n = 440) | 45.5* |
| Ben et al21 | Porto Alegre, RS | BHCU, adults (n = 206) | 53.9* |
| Martins et al19 | Petrópolis, RJ | BHCU, adults, (n = 250) | 39.2* |
| FHP, adults (n = 250) | 29.2* | ||
| Silva et al30 | Peruibe, SP | Outpatient clinic, > 18 years, stage I or II hypertension, (n = 71) | 9.9* |
| 23.9¢ |
BHCU: basic health care unit; FHP: Family Health Program.
Blood pressure control: < 140 mm Hg (systolic) and 90 mm Hg (diastolic). # No information on blood pressure control levels.
Blood pressure control: < 135 mm Hg (systolic) and 80 mm Hg (diastolic) for ambulatory blood pressure monitoring. ¥ Blood pressure control: < 90 mm Hg (diastolic).
Blood pressure control: < 135 (systolic) and 85 mm Hg (diastolic) for home blood pressure monitoring.
Table 3 shows studies with hypertensives in special situations such as diabetics and elderly. It is worth noting that the control of diabetic hypertensives according to the cutoff point of 140/90 mm Hg corresponded to twice that adopting more severe blood pressure reductions recommended for that population23,33,34. Regarding the studies with elderly, three were population-based35,36, and the control rates varied from 27% to 44.6%, reaching 80% when blood pressure was assessed by using ABPM37. Two studies assessed arterial hypertension control of health professional. In the city of Salvador, Bahia state38, the hypertension control rate among nursing professionals undergoing treatment for arterial hypertension was 30.6%, while in a university-affiliated hospital in the city of São Paulo, São Paulo state39, that rate among professionals of several categories (physicians, nurses and administrative) who knew to be hypertensives was 49%. A study40 with hypertensives with the human immunodeficiency virus has reported an arterial hypertension control rate of 14.8%, considering the total number of hypertensives in the cohort. Greater control rates were found among hypertensives from the pharmaceutical (65.7%)41 and social assistance (67.3%)42 settings.
Table 3.
Arterial hypertension control in Brazilian studies with specific groups (São Paulo, 2012)
| Article | Study site | Population | Control (%) |
|---|---|---|---|
| Aquino et al38 | Salvador, BA | Female nurses and nurse's aides, (n=494) | 30.6* |
| Barroso et al33 | Belo Horizonte, MG | Diabetic hypertensives, adults (n=146) | 41.7* |
| 17.1¢ | |||
| Nobre et al31 | 4 Brazilian macroregions | 291 clinics, outpatient clinics, hypertension services, risk stratification of hypertensives, 21-79 years, (n=2810) | low/medium risk, 61.7% |
| high risk, 42.5% | |||
| very high risk, 41.8% | |||
| with renal disease, 32.4% | |||
| Total, 46.5% | |||
| Pinto et al34 | Porto Alegre, RS | Diabetic hypertensives, adults (n=348) | 39* |
| 17¥ | |||
| Firmo et al35 | Bambui, MG | Population ≥ 60 years, on antihypertensive treatment (n=1494) | 38.8* |
| Firmo et al35 | Bambui, MG | Population ≥ 60 years (n=919) | 27* |
| Mion Jr et al39 | São Paulo, SP | University-affiliated hospital professionals, (n=810) | 49* |
| Arruda Jr et al40 | Recife, PE | Individuals with HIV/AIDS, ≥ 18 years (n=958) | 14.8* |
| Santos et al41 | S Caetano do Sul, SP | Hypertensive users of school pharmacy, > 18 years (n=102) | 65.7* |
| Firmo et al36 | Bambui, MG | Population 71-81 years, cohort from 1916 to 1926 (n=313) | 44.6* |
| Population 71-81 years, cohort from 1927 to 1937 (n=484) | 40.1* | ||
| Vitor et al42 | Fortaleza, CE | Hypertensives from a social assistance center (n=49) | 67.3 |
| Bastos-Barbosa et al37 | Ribeirão Preto, SP | ≥ 60 years, followed up at public health care centers, on treatment (n=60) | 80§ |
HIV: human immunodeficiency virus; AIDS: acquired immunodeficiency syndrome.
Blood pressure control: < 140 mm Hg (systolic) and 90 mm Hg (diastolic). # Blood pressure control: < 160 mm Hg (systolic) and 95 mm Hg (diastolic).
Blood pressure control: < 135 mm Hg (systolic) and 80 mm Hg (diastolic) for ambulatory blood pressure monitoring.
Blood pressure control: < 130 mm Hg (systolic) and 80 mm Hg (diastolic).
Blood pressure control: < 130 mm Hg (systolic) and 85 mm Hg (diastolic).
Five observational studies assessed hypertension control after an intervention (Table 4), and the results showed better blood pressure control after improving the antihypertensive treatment and adopting public health strategies. The samples of two studies43,44 consisted of uncontrolled hypertensives, and thus the initial control was zero. Comparative studies reported better arterial hypertension control with the beginning of treatment or its improvement, including the adoption of the public health strategies recommended by the Brazilian Unified Health Care System45,46. Another study identified a reduction in the control rate after the end of an intervention via telephone with hypertensives followed up at a hypertension outpatient clinic47.
Table 4.
Comparative observational studies on arterial hypertension control before and after interventions (São Paulo, 2012)
| Article | Study site | Population | Intervention | Initial control (%) | Final control (%) |
|---|---|---|---|---|---|
| de Souza e Silva et al43 | Rio de Janeiro, RJ | Users of a university-affiliated hospital, > 20 years (n = 96) | Hypertension outpatient clinic | 0 | 32.9# |
| Sala et al44 | São Paulo, SP | BHCU, ≥ 20 years (n=250) | Aging Health Care Program | 0 | 44.4§ |
| Araujo et al45 | Salvador, BA | FHP, ≥ 20 years (n = 135) | FHP implantation | 28.9 | 57* |
| Gusmão et al47 | São Paulo, SP | Hypertension outpatient clinic, 18-60 years, no target-organ lesion (n = 40) | Three years after ending the program with telephone contact | 78 | 50* |
| Hypertension outpatient clinic, 18-60 years, target-organ lesion or other diseases (n = 37) | 70 | 49* | |||
| Hoepfner et al46 | Joinville, SC | BHCU, adults (n=415) | Improvement in therapy | 12.8 | 36.6¢ |
BHCU: basic health care unit; FHP: Family Health Program.
Blood pressure control: < 90 mm Hg (diastolic).
Blood pressure control: < 160 mm Hg (systolic) and 95 mmHg (diastolic).
Blood pressure control: < 140 mm Hg (systolic) and 90 mmHg (diastolic).
Blood pressure control: < 140 mm Hg (systolic) and 86 mm Hg (diastolic) (or 130/80 mm Hg for diabetes or chronic renal disease).
Discussion
The studies assessed evidenced different arterial hypertension control rates in Brazil. That control results from a complex system involving biological, socioeconomic, cultural and sanitation aspects. The heterogeneity of the Brazilian population demands the expansion of the knowledge on arterial hypertension control and its determinants in different Brazilian regions. Most of the publications on arterial hypertension control were recent, concentrated on the last decade. The older publications corresponded to public health periodicals, indexed in the SciELO database for a longer period, from the end of the 1960s to the beginning of the 1980s. A cardiology journal, first indexed in the mid-1990s, accounted for 40% of the publications on the subject. In addition, in past decades the scientific production gained more incentive for innovation and competition in the elaboration and use of its indicators due to the increase in access to electronic resources and support of national and international research agencies48.
The large majority of studies have adopted systolic and diastolic blood pressure values to control arterial hypertension equal to or lower than 140 mm Hg and 90 mm Hg, respectively. In the studies published before 1999, when data from the III Brazilian Consensus for Arterial Hypertension were published49, the blood pressure levels recommended for control were higher. The arterial hypertension control rates reported by the studies analyzed are very different and difficult to compare. Such differences can be explained by several factors, such as study context (population-based, health care), sampling techniques, methods for blood pressure assessment, and intrinsic characteristics of the population studied.
In population-based studies, adopting systolic and diastolic blood pressure control levels lower than 140 mm Hg and 90 mm Hg, respectively, for hypertensives undergoing treatment, the control rates ranged from 10.1% in the city of Tubarão, Santa Catarina state9, in 2003, to 52.4% in the city of São José do Rio Preto, São Paulo state10, in 2004-2005. The sample from the city of São José do Rio Preto had a higher proportion of elderly (38% versus 20.1%) and a greater percentage of individuals with previous knowledge about their arterial hypertension (74.4% versus 55.6%). The percentage of individuals with an education level lower than seven schooling years was higher in the sample from the city of Tubarão as compared to that from the city of São José do Rio Preto (52.4% versus 44.6%). Although that comparison does not justify the differences found in control rates, it evidences factors known to be associated with arterial hypertension control and that differ in the populations studied.
The only multicenter population-based study that assessed arterial hypertension control in municipalities in the five Brazilian geographical regions13 reported a rate of 57.6%, a figure greater than that of other countries in Latin America (29% to 58%)50 and western Europe (31% to 46%)51. It is worth noting that population-based studies accounted for less than one third of the articles assessed in this review. This evidences the scarcity of such studies, considered fundamental for knowing the conditions that influence the dynamics of hypertension risks and control in populations.
Maintaining the same criteria for arterial hypertension control (< 140/90 mm Hg), the values obtained at hypertension outpatient clinics ranged from 20.9% for non-diabetic hypertensives in the city of São Paulo, São Paulo state, in 200023, to 61.7% for hypertensives at low to medium cardiovascular risk in the five Brazilian geographical regions in 200831. It is worth noting that 9 of 15 studies on arterial hypertension control in primary or secondary health care either had a convenience sample or did not explicit the sample composition. Only three studies have mentioned the constitution of a probabilistic sample and sample calculation.
Regarding the control of diabetic hypertensives, low rates were identified, ranging from 13.4% to 17.1%, considering the cutoff points of 130/80 or 130/85 mm Hg, respectively23,33,34. Those values corresponded to 50% of the control for the cutoff point of 140/90 mm Hg recommended for low to medium cardiovascular risk hypertensives. In the study comparing control rates according to cardiovascular risk stratification and respective blood pressure goals, a 20% to 30% reduction in control was observed for high-risk and very high risk patients, and patients with kidney diseases as compared to low to medium risk patients31. Comorbidities commonly associated with hypertension, such as diabetes mellitus, obesity, and target-organ lesions, are conditions that require more strict control goals, because blood pressure levels over 115/75 mm Hg represent an additional risk for cardiovascular disease52.
Arterial hypertension control is usually unsatisfactory. That might be explained by the insufficient reduction in blood pressure levels due to the ineffective treatment proposed. Another possibility to explain unsatisfactory blood pressure control relates to poor compliance with treatment or lack thereof. Those data of poor hypertension control in addition to other observations resulting from the practice of health care professionals reinforce the hypothesis that not only the diagnosis of arterial hypertension but also its treatment is easy; however, despite the efficacy of the existing therapeutic measures, blood pressure control is not an easy task, considering that it usually requires a life-long treatment. To improve arterial hypertension control, it is important to identify noncompliant patients.
Compliance is a complex behavioral process. The challenge of compliance with treatment requires the involvement of patients and health professionals. To achieve and maintain controlled blood pressure levels, the patient usually requires constant stimulation to change lifestyle and adjust the medication. Hypertensive patients should be observed at regular intervals, aiming at controlling their blood pressure levels, as well as maintaining them controlled in the long run. The major reason of the inadequate arterial hypertension control seems to be noncompliance with the treatment in the long run, regarding both the changes in lifestyle and the observation of the medication prescribed.
Noncompliance with treatment might reach high levels of interruption, considered the greatest degree of lack of compliance and representing a great challenge to health professionals. Several factors interfere with the process of compliance with treatment. Biosocial variables such as age, sex, race, educational level, socioeconomic level, occupation, marital status, religion, lifestyle, cultural aspects and health beliefs should be considered. A cohort study carried out in the city of Porto Alegre showed that interruption of the antihypertensive treatment was associated with smoking habit, a maximum educational level of 5 years, and less than 5 years of disease duration, while an increase in age was associated with a higher probability of follow-up53. However, a study with hypertensives in the city of São Paulo evidenced that higher blood pressure levels during the follow-up were associated with age over 60 years, low educational level, low income, and hypertension duration longer than 5 years22.
Changes in life habits and style, as well as cultural aspects, can also influence compliance with treatment and require determination of the patient and professional team. Knowledge on the disease and its treatment is another factor to be considered. Studies24,25 have shown that hypertensives usually are instructed about their health condition, but are not properly controlled. Discrepancy between getting information about the disease and its treatment and managing to control blood pressure indicates an essential difference between knowledge and compliance. While knowledge is rational, compliance is a complex process, involving emotional factors and concrete practical and logistic barriers. Psychosocial factors, disease chronicity and lack of specific symptoms, as well as long-term complications influence the compliance process. The relationship between health care professionals and hypertensives also deserves attention. The characteristics of the medicamentous treatment, such as side effects, complex therapeutic regimens, and life-long treatment, might influence compliance.
Arterial hypertension control depends on its detection, the structure of health care services and access to them, and compliance with treatment. To achieve blood pressure control, compliance with treatment is essential. In addition to frustrating health care professionals, because it prevents them from achieving their predetermined goals, noncompliance has an inherent negative social impact, because it affects individuals in their productive years.
Most of the population-based studies presented in this review assessed arterial hypertension prevalence and treatment, as well as the knowledge about the disease, in the populations studied4-16. Other studies have assessed relevant subjects, such as biosocial aspects influencing compliance with antihypertensive treatment, knowledge and beliefs about the disease19,22,24-27,29, and health care practices14,17,20,21,34. However, extending the knowledge about arterial hypertension control in Brazil, as well as about its determinant factors, is necessary to improve and assess the health care measures proposed by the Brazilian Unified Health Care System.
Conclusion
The studies assessed showed a wide variation in blood pressure control rates. It is worth noting that the comparison between studies was a limiting factor because of the differences in the methods adopted. However, even considering the most optimistic values, approximately 50% of hypertensives undergoing treatment are exposed to the complications of that disease due to lack of blood pressure control. This is even more alarming for hypertensives with other cardiovascular risks. Nationwide population-based studies, whose assessment criteria are in accordance with current recommendations, are necessary to better plan health care to hypertensives, thus, reducing cardiovascular morbidity and mortality.
Footnotes
Author contributions
Conception and design of the research, Acquisition of data, Analysis and interpretation of the data, Statistical analysis, Writing of the manuscript and Critical revision of the manuscript for intellectual content: Pinho NA, Pierin AMG.
Study Association
This study is not associated with any post-graduation program.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
There were no external funding sources for this study.
References
- 1.Passos VMA, Assis TD, Barreto SM. Hipertensão arterial no Brasil: estimativa de prevalência a partir de estudos de base populacional Epidemiologia e Serviços de Saúde. Epidemiologia e Serviços de Saúde. 2006;15(1):35–45. [Google Scholar]
- 2.Sociedade Brasileira de Cardiologia. Sociedade Brasileira de Hipertensão. Sociedade Brasileira de Nefrologia VI Diretrizes brasileiras de hipertensão. Arq Bras Cardiol. 2010;95(1) supl. 1:1–51. [PubMed] [Google Scholar]
- 3.Brasil. Ministério da Saude Datasus: informações de saude. [Citado em 2012 nov 14]. Disponivel em: http://www.datasus.gov.br/tabnet/tabnet.htm.
- 4.dos Santos MA, Koike SK, Caporossi EM. Hipertensão arterial e medidas de controle referidas na população urbana de Cáceres/MT. Rev Inst Med Trop São Paulo. 1988;30(3):208–211. doi: 10.1590/s0036-46651988000300015. [DOI] [PubMed] [Google Scholar]
- 5.Piccini RX, Victora CG. Hipertensão arterial sistêmica em área urbana no sul do Brasil: prevalência e fatores de risco. Rev Saúde Pública. 1994;28(4):261–267. doi: 10.1590/s0034-89101994000400004. [DOI] [PubMed] [Google Scholar]
- 6.Trindade IS, Heineck G, Machado JR, Ayzemberg H, Formighieri M, Crestani M, et al. Prevalência da hipertensão arterial sistêmica na população urbana de Passo Fundo (RS) Arq Bras Cardiol. 1998;71(2):127–130. doi: 10.1590/s0066-782x1998000800006. [DOI] [PubMed] [Google Scholar]
- 7.Freitas OC, Resende de Carvalho F, Marques Neves J, Veludo PK, Silva Parreira R, Marafiotti Gonçalves R, et al. Prevalence of hypertension in the urban population of Catanduva, in the State of São Paulo, Brazil. Arq Bras Cardiol. 2001;77(1):19–21. doi: 10.1590/s0066-782x2001000700002. [DOI] [PubMed] [Google Scholar]
- 8.Fuchs SC, Petter JG, Accordi MC, Zen VL, Pizzol AD, Jr, Moreira LB, et al. Establishing the prevalence of hypertension: influence of sampling criteria. Arq Bras Cardiol. 2001;76(6):445–452. doi: 10.1590/s0066-782x2001000600002. [DOI] [PubMed] [Google Scholar]
- 9.Pereira MR, Coutinho MS, Freitas PF, D'Orsi E, Bernardi A, Hass R. Prevalência, conhecimento, tratamento e controle de hipertensão arterial sistêmica na população adulta urbana de Tubarão, Santa Catarina, Brasil, em 2003. Cad Saúde Pública. 2007;23(10):2363–2374. doi: 10.1590/s0102-311x2007001000011. [DOI] [PubMed] [Google Scholar]
- 10.Cipullo JP, Martin JF, Ciorlia LA, Godoy MR, Cação JC, Loureiro AA, et al. Prevalência e fatores de risco para hipertensão em uma população urbana brasileira. Arq Bras Cardiol. 2010;94(4):519–526. doi: 10.1590/s0066-782x2010005000014. [DOI] [PubMed] [Google Scholar]
- 11.Mion D, Jr, Pierin AM, Bensenor IM, Marin JC, Costa KR, Henrique LF, et al. Hipertensão arterial na cidade de São Paulo: prevalência referida por contato telefônico. Arq Bras Cardiol. 2010;95(1):99–106. doi: 10.1590/s0066-782x2010005000051. [DOI] [PubMed] [Google Scholar]
- 12.Lyra R, Silva Rdos S, Montenegro RM, Junior, Matos MV, Cézar NJ, Fernandes VO, et al. High prevalence of arterial hypertension in a Brazilian Northeast population of low education and income level, and its association with obesity and metabolic syndrome. Rev Assoc Med Bras. 2012;58(2):209–214. [PubMed] [Google Scholar]
- 13.Piccini RX, Facchini LA, Tomasi E, Siqueira FV, Silveira DSd, Thumé E, et al. Promoção, prevenção e cuidado da hipertensão arterial no Brasil. Rev. Saúde Pública. 2012;46(3):543–550. doi: 10.1590/s0034-89102012005000027. [DOI] [PubMed] [Google Scholar]
- 14.Gus I, Harzheim E, Zaslavsky C, Medina C, Gus M. Prevalência, reconhecimento e controle da hipertensão arterial sistêmica no estado do Rio Grande do Sul. Arq Bras Cardiol. 2004;83(5):424–428. doi: 10.1590/s0066-782x2004001700009. [DOI] [PubMed] [Google Scholar]
- 15.Rosário TM, Scala LC, França GV, Pereira MR, Jardim PC. Prevalência, controle e tratamento da hipertensão arterial sistêmica em Nobres - MT. Arq Bras Cardiol. 2009;93(6):672–678. doi: 10.1590/s0066-782x2009001200018. [DOI] [PubMed] [Google Scholar]
- 16.Klein CH, Silva NA, Nogueira AR, Bloch KV, Campos LH. Hipertensão arterial na Ilha do Governador, Brasil: II. Prevalência. Cad Saúde Pública. 1995;11(2):187–201. doi: 10.1590/s0102-311x1995000200003. [DOI] [PubMed] [Google Scholar]
- 17.Mano GM, Pierin AM. Avaliação de pacientes hipertensos acompanhados pelo Programa Saúde da Família em um Centro de Saúde Escola. Acta Paul enferm. 2005;18(3):269–275. [Google Scholar]
- 18.Helena ET, Nemes MI, Eluf-Neto J. Avaliação da assistência a pessoas com hipertensão arterial em Unidades de Estratégia Saúde da Família. Saúde Soc. 2010;19(3):614–626. [Google Scholar]
- 19.Martins TL, Atallah AN, Silva EM. Blood pressure control in hypertensive patients within Family Health Program versus at Primary Healthcare Units: analytical cross-sectional study . Sao Paulo Med J. 2012;130(3):145–150. doi: 10.1590/S1516-31802012000300003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pierin AM, Marroni SN, Taveira LA, Benseñor IJ. Controle da hipertensão arterial e fatores associados na atenção primária em Unidades Básicas de Saúde localizadas na Região Oeste da cidade de São Paulo. Cien Saude Colet. 2011;16(1):1389–1400. doi: 10.1590/s1413-81232011000700074. [DOI] [PubMed] [Google Scholar]
- 21.Ben AJ, Neumann CR, Mengue SS. Teste de Morisky-Green e Brief Medication Questionnaire para avaliar adesão a medicamentos. Rev Saude Publica. 2012;46(2):279–289. doi: 10.1590/s0034-89102012005000013. [DOI] [PubMed] [Google Scholar]
- 22.Pierin AM, Mion D, Jr, Fukushima JT, Pinto AR, Kaminaga MM. O perfil de um grupo de pessoas hipertensas de acordo com conhecimento e gravidade da doença. Rev Esc Enferm USP. 2001;35(1):11–18. [Google Scholar]
- 23.Freitas JB, Tavares A, Kohlmann O, Jr, Zanella MT, Ribeiro AB. Cross-sectional study on blood pressure control in the Department of Nephrology of the Escola Paulista de Medicina - UNIFESP. Arq Bras Cardiol. 2002;79(2):123–128. doi: 10.1590/s0066-782x2002001100003. [DOI] [PubMed] [Google Scholar]
- 24.Strelec MA, Pierin AM, Mion D., Jr The influence of patient's consciousness regarding high blood pressure and patient's attitude in face of disease controlling medicine intake. Arq Bras Cardiol. 2003;81(4):349–354. doi: 10.1590/s0066-782x2003001200002. [DOI] [PubMed] [Google Scholar]
- 25.Sanchez CG, Pierin AM, Mion D., Jr Comparação dos perfis dos pacientes hipertensos atendidos em Pronto-Socorro e em tratamento ambulatorial. Rev Esc Enferm USP. 2004;38(1):90–98. doi: 10.1590/s0080-62342004000100011. [DOI] [PubMed] [Google Scholar]
- 26.Coelho EB, Moysés M, Neto, Palhares R, Cardoso MC, Geleilete TJ, Nobre F. Relação entre a assiduidade às consultas ambulatoriais e o controle da pressão arterial em pacientes hipertensos. Arq Bras Cardiol. 2005;85(3):157–161. doi: 10.1590/s0066-782x2005001600002. [DOI] [PubMed] [Google Scholar]
- 27.Jesus ES, Augusto MA, Gusmão J, Mion D, Júnior, Ortega K, Pierin AM. Profile of hypertensive patients: biosocial characteristics, knowledge, and treatment compliance . Acta paul enferm. 2008;21(1):59–65. [Google Scholar]
- 28.Magnanini MM, Nogueira Ada R, Carvalho MS, Bloch KV. Monitorização ambulatorial da pressão arterial e risco cardiovascular em mulheres com hipertensão resistente. Arq Bras Cardiol. 2009;92(6):448–453. 467–472, 484–489. [Google Scholar]
- 29.Pierin AM, Jesus Edos S, Augusto MA, Gusmão J, Ortega K, Mion D., Jr Variáveis biopsicossociais e atitudes frente ao tratamento influenciam a hipertensão complicada. Arq Bras Cardiol. 2010;95(5):648–654. doi: 10.1590/s0066-782x2010005000132. [DOI] [PubMed] [Google Scholar]
- 30.Silva GC, Pierin AM. A monitorização residencial da pressão arterial e o controle de um grupo de hipertensos. Rev Esc Enferm USP. 2012;46(4):922–928. doi: 10.1590/s0080-62342012000400020. [DOI] [PubMed] [Google Scholar]
- 31.Nobre F, Ribeiro AB, Mion D., Jr Controle da pressão arterial em pacientes sob tratamento anti-hipertensivo no Brasil: Controlar Brasil. Arq Bras Cardiol. 2010;94(5):663–670. doi: 10.1590/s0066-782x2010005000035. [DOI] [PubMed] [Google Scholar]
- 32.Muxfeldt ES, Nogueira Ada R, Salles GF, Bloch KV. Demographic and clinical characteristics of hypertensive patients in the internal medicine outpatient clinic of a university hospital in Rio de Janeiro. Sao Paulo Med J. 2004;122(3):87–93. doi: 10.1590/S1516-31802004000300003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barroso WK, Jardim PC, Jardim TS, Souza CU, Magalhães AL, Ibrahim FM, et al. Hypertensive diabetic patients: guidelines for conduct and their difficulties. Arq Bras Cardiol. 2003;81(2):143–147. 137–142. doi: 10.1590/s0066-782x2003001000003. [DOI] [PubMed] [Google Scholar]
- 34.Pinto LC, Ricardo ED, Leitão CB, Kramer CK, Zanatta CM, Gross JL, et al. Controle inadequado da pressão arterial em pacientes com diabete melito tipo 2. Arq Bras Cardiol. 2010;94(5):651–655. doi: 10.1590/s0066-782x2010005000034. [DOI] [PubMed] [Google Scholar]
- 35.Firmo JO, Uchôa E, Lima-Costa MF. Projeto Bambuí: fatores associados ao conhecimento da condição de hipertenso entre idosos. Cad Saúde Pública. 2004;20(2):512–521. doi: 10.1590/s0102-311x2004000200019. [DOI] [PubMed] [Google Scholar]
- 36.Firmo JO, Peixoto SV, Loyola AI, Filho, Uchôa E, Lima-Costa MF. Prevalence estimates for hypertension in Latin America and the Caribbean: are they useful for surveillance? Cad Saúde Pública. 2011;27(3):s427–s434. doi: 10.1590/s0102-311x2011001500013. [DOI] [PubMed] [Google Scholar]
- 37.Bastos-Barbosa RG, Ferriolli E, Moriguti JC, Nogueira CB, Nobre F, Ueta J, et al. Adesão ao tratamento e controle da pressão arterial em idosos com hipertensão. Arq Bras Cardiol. 2012;99(1):636–641. doi: 10.1590/s0066-782x2012005000054. [DOI] [PubMed] [Google Scholar]
- 38.Aquino EM, Magalhães LB, Araújo MJ, Almeida MC, Leto JP. Hypertension in a female nursing staff-pattern of occurrence, diagnosis, and treatment. Arq Bras Cardiol. 2001;76(3):197–208. doi: 10.1590/s0066-782x2001000300003. [DOI] [PubMed] [Google Scholar]
- 39.Mion D, Jr, Pierin AM, Bambirra AP, Assunção JH, Monteiro JM, Chinen RY, et al. Hypertension in employees of a University General Hospital. Rev Hosp Clin Fac Med Sao Paulo. 2004;59(6):329–336. doi: 10.1590/S0041-87812004000600004. [DOI] [PubMed] [Google Scholar]
- 40.Arruda ER, Junior, Lacerda HR, Moura LC, Albuquerque Mde F, Miranda Dde B, Filho, Diniz GT. Risk factors related to hypertension among patients in a cohort living with HIV/AIDS. Braz J Infect Dis. 2010;14(3):281–287. doi: 10.1590/s1413-86702010000300014. [DOI] [PubMed] [Google Scholar]
- 41.Santos BR, Teixeira J, Gonçalves D, Gatti RM, Yavo B, Aragão CC. Blood pressure levels and adherence to treatment of hypertensive patients, users of a school pharmacy. Braz J Pharm Sci. 2010;46(3):421–430. [Google Scholar]
- 42.Vitor AF, Monteiro FP, Morais HC, Vasconcelos JD, Lopes MV, Araujo TL. Perfil das condições de seguimento terapêutico em portadores de hipertensão arterial. Esc Anna Nery. 2011;15(2):251–260. [Google Scholar]
- 43.de Souza e Silva NA, Aguiar GR, Nogueira Ada R, Duarte MM, Alves RH. Importância clínica dos custos diretos hospitalares em pacientes com hipertensão arterial em tratamento num hospital universitário, Rio de Janeiro, Brasil. Rev Saúde Pública. 1986;20(4):293–302. [PubMed] [Google Scholar]
- 44.Sala A, Nemes A, Filho, Eluf-Neto J. Avaliação da efetividade do controle da hipertensão arterial em unidade básica de saúde. Rev Saúde Pública. 1996;30(2):161–167. doi: 10.1590/s0034-89101996000200008. [DOI] [PubMed] [Google Scholar]
- 45.Araujo JC, Guimarães AC. Controle da hipertensão arterial em uma unidade de saúde da família. Rev Saúde Pública. 2007;41(3):368–374. doi: 10.1590/s0034-89102007000300007. [DOI] [PubMed] [Google Scholar]
- 46.Hoepfner C, Franco SC. Inércia clínica e controle da hipertensão arterial nas unidades de atenção primária à saúde. Arq Bras Cardiol. 2010;95(2):223–228. doi: 10.1590/s0066-782x2010005000095. [DOI] [PubMed] [Google Scholar]
- 47.Gusmão JL, Mion D, Jr, Pierin AM. Health-related quality of life and blood pressure control in hypertensive patients with and without complications. Clinics (Sao Paulo) 2009;64:619–628. doi: 10.1590/S1807-59322009000700003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fundação de Amparo à Pesquisa de São Paulo (FAPESP) Indicadores de ciência, tecnologia e inovação em São Paulo. São Paulo: 2010. [Google Scholar]
- 49.Kohlmann O, Jr, Guimarães AC, Carvalho MH, Chaves HC, Jr, Machado CA, Praxedes JN, et al. III Consenso Brasileiro de hipertensão arterial. Arq Bras Endocrinol Metab. 1999;43(4):257–286. [Google Scholar]
- 50.Ordúñez P, Silva LC, Rodríguez MP, Robles S. Prevalence estimates for hypertension in Latin America and the Caribbean: are they useful for surveillance? Rev Panam Salud Publica. 2001;10(4):226–231. doi: 10.1590/s1020-49892001001000002. [DOI] [PubMed] [Google Scholar]
- 51.Wang YR, Alexander GC, Stafford RS. Outpatient hypertension treatment, treatment intensification, and control in Western Europe and the United States. Arch Intern Med. 2007;167(2):141–147. doi: 10.1001/archinte.167.2.141. [DOI] [PubMed] [Google Scholar]
- 52.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute. National High Blood Pressure Education Program Coordinating Committee Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 53.Busnello RG, Melchior R, Faccin C, Vettori D, Petter J, Moreira LB, et al. Characteristics associated with the dropout of hypertensive patients followed up in outpatient referral clinic. Arq Bras Cardiol. 2001;76(5):349–354. doi: 10.1590/s0066-782x2001000500001. [DOI] [PubMed] [Google Scholar]