Abstract
Background
Perforators are a constant anatomical finding in the facial area and any known flap can in theory be based on the first perforator located at the flap rotation axis.
Methods
A case series of single stage reconstruction of moderate sized facial defects using 21 perforator based local flaps in 19 patients from 2008–2013.
Results
A sufficient perforator was located in every case and the flap rotated along its axis (76 %) or advanced (24 %).
Reconstruction was successfully achieved with a high self reported patient satisfaction. Two minor complications occurred early on in the series and corrective procedures were performed in four patients.
Conclusions
The random facial perforator flap seems to be a good and reliable option for the reconstruction of facial subunits, especially the periorbital, nasal and periocular area with a minimal morbidity and a pleasing result in a one stage outpatient setting.
Level of Evidence: Level IV, therapeutic study
Keywords: Local flaps, Perforator, Reconstruction, Face
Introduction
Local flaps, when present, are considered the best reconstructive option for moderate-sized defects in the face [1]. The axial pattern nasolabial and forehead flaps are work horse flaps for coverage of the nasal and perinasal areas due to their rich vascularity, consistent and reliable anatomy enabling a long and flexible flap on a narrow pedicle [2, 3]. The limitations of local flaps are most often due to their limited range of motion and bulkiness at the pedicle site, necessitating a delay and a secondary procedure. The importance of a successful reconstruction of the facial features is apparent due to its exposure, and a simple single-stage method is therefore preferable if available. The purpose of this paper is to share our experience using the workhorse local flaps designed as freestyle perforator-based flaps for the reconstruction of moderate-sized facial skin defects.
Material and methods
Facial tumor removal was performed in 19 patients at Telemark Hospital, Norway, and at Odense University Hospital/Lillebaelt Hospital, Denmark, from 2008 to 2013. The patients, nine women and eight men, ranging from 38 to 86 years (median age, 71 years) were treated for basal cell carcinoma (BCC) (n = 14), squamous cell carcinoma (SCC) (n = 1), morbus Bowen (n = 1), lentigo maligna (n = 1), actinic keratosis (n = 1), and malignant melanoma (n = 1); see Table 1. Sixteen of the flaps were rotated as propeller flaps, 76 %, and five were advanced in a V-Y fascion 24 %. A suitable perforator was identified at the predicted location in every case. The most frequent flap location was nasolabial (NL) in 11 cases, followed by four jowl and NL/jowl, three supratrochlear, one cheek and NL, one zygomatic and one orbicularis oculi musculocutanous flap a modified Trepier; (see Table 1).
Table 1.
Patient data and outcome
| Number | Age | Indication | Location | Type | Rot/deg. | Compl. | Rev. | FU (month) |
|---|---|---|---|---|---|---|---|---|
| 1 | 81 | BCC UL | J | P | 120 | N | N | 63 |
| 2 | 74 | LM C | Z | P | 90 | N | N | 60 |
| 3 | 60 | BCC Ns | NL | P | 150 | Ya | N | 59 |
| 4 | 73 | BCC Ns | NL | P | 150 | N | N | 58 |
| 5 | – | DS Ns | NL | VY | N | N | 58 | |
| 6 | 86 | MB Ns | ST | P | 180 | Yb | N | 57 |
| 7 | 80 | BCC UL | NL/J | VY | N | N | 56 | |
| 8 | 71 | BCC AN | NL | P | 180 | N | N | 52 |
| 9 | 83 | BCC UL | NL/J | VY | N | N | 40 | |
| 10 | 79 | BCC Ns | NL | P | 180 | N | Mi | 37 |
| 11 | 38 | BCC AN/UL | NL | P | 180 | N | Mi | 24 |
| 12 | – | BCC UL+ | NL | VY | N | N | 24 | |
| 13 | 74 | AK Ns | ST | P | 180 | N | N | 15 |
| 14 | 78 | BCC AN | NL | P | 180 | N | Mi | 15 |
| 15 | 68 | BCC FH | ST | P | 150 | N | Mi | 14 |
| 16 | 70 | BCC Ns | NL | P | 180 | N | N | 13 |
| 17 | 83 | SCC C | NL/C | VY | N | N | 8 | |
| 18 | 59 | BCC AN | NL | P | 180 | N | N | 6 |
| 19 | 73 | BCC Ns | NL | P | 180 | N | N | 4 |
| 20 | 54 | MM UL | J | P | 135 | N | N | 3 |
| 21 | 79 | BCC Mc | OO | P | 150 | N | N | 1 |
Compl. complications, Rev. revision, FU follow-up, Rot/deg degree of rotation, BCC basal cell carcinoma, AN ala nasi, NL nasolabial, P propella, Mi minor revision/contouring, UL upper lip, VY VY advancement flap, J jowel, UL + upper lip and adjacent aesthetical unit, MC medial canthus, DS donor site, Ns nose, MB Morbus Bowen, FH forehead, ST supratrochlear, LM lentigo maligna, Z zygomatic, AK actinic keratosis, C cheek, OO orbicularis oculi, SCC squamous cell carcinoma, MM malignant melanoma, N noY yes
aPartial flap loss
bVenous congestion
Operative procedure
The flaps were performed as outpatient procedures in all cases; 18 flaps were performed in local anesthesia, and two patients requested general anesthesia due to anxiety (three flaps). The operation started with tumor resection with wide margins and, where appropriate, conformation of a free margin with frozen section histology. The local flap option was planned based on the most likely location of a useful perforator. In every case, a perforator was located where it was expected to be found by a careful dissection and inspection, and then the skin island was raised and transposed or advanced accordingly. The skin was sutured in two layers with a 5.0 resorbable monofilament suture in the dermis and a monofilament 5.0 nylon in the skin. In the first patients, a penrose drain was placed underneath the flap for drainage, but we found that this was not necessary and was abandoned in the successive flaps. Paper tape and a light dressing were placed on the scar and suture removal planned in 7 days at the local doctors’ office. Patients were followed up in the outpatient clinic at 3 weeks and 3–6 months time, depending on the pathology involved.
Results
All 19 patients achieved a satisfactory single-stage reconstruction with 21 perforator-based flaps for the reconstruction of moderate-sized facial defects.. No bleeding or infection occurred. Two minor complications occurred early on in the series. The flaps of patients 3 and 6 suffered from venous stasis with subsequent partial epidermolysis and spontaneous reepithelialization. Neither patient needed additional surgical intervention.
Minor revisions were performed in four cases for improved appearance. The flaps were designed as a propeller in the majority of cases, 76 %, and advancement V-Y in the remaining 24 %. The self-reported patient satisfaction was high. The majority of flaps, 80 % (16/21), were facial artery perforator (FAP) flaps, and in all cases, they survived without a problem. Some initial edema and occasional trap door deformity occur especially in round- or oval-shaped flaps. This however settles in 3–6 months time. Representative cases are depicted in Figs. 1, 2, 3, 4, and 5.
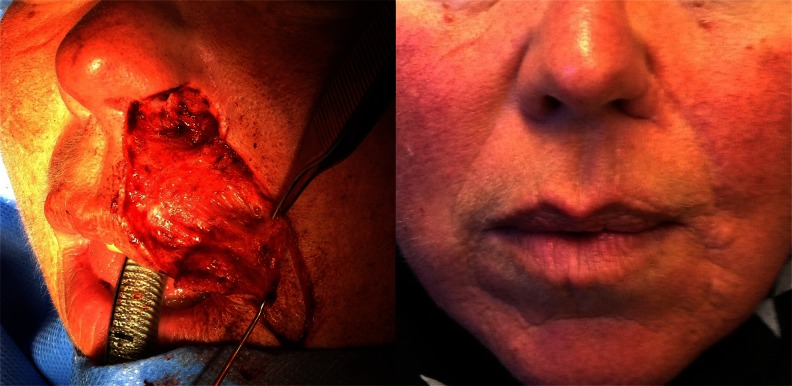
Fig. 1.
Operative technique showing a modeolus FAP flap propeller used for the reconstruction of an upper lip defect with immediate result
Fig. 2.
BCC if the upper lip. The FAP flap used in a V-Y advancement fascion for the reconstruction of a moderate-sized defect of the upper lip with immediate and long-term results in 3 years
Fig. 3.
Glabellar propeller supratrochlear flap, perforator and result 3 weeks post-op
Fig. 4.
Alar reconstruction with a NL propeller flap, immediate result and 6 months after minor revision
Fig. 5.
Combined reconstruction of ala with a propeller NL flap and a V-Y advancement reconstruction of the upper lip and nasal floor; 6 months result after a minor revision
Discussion
We have performed a single-stage reconstruction of moderate-sized defects using 21 perforator-based flaps in 19 patients; see Table 1. In all cases, the intended reconstruction was successfully achieved with a high self-reported patient satisfaction.
The nasolabial flap, and glabellar and forhead flaps are well described as axial pattern flaps on a narrow pedicle or as island flaps [1]. Since then, the knowledge of a perforator-based design evolved from the angiosomal concept introduced by Taylor and Palmer in 1987 [4]. In the year 2000, Dr. Taylor’s team published a study on the facial angiosomes, which is the basis of the flap design which we have used in this series of flaps [5]. The facial artery perforator flap, which we used in 16/ 21 flaps, was first described by Hofer et al. in 2005 including an anatomical dissection to indicate the location of perforators [6]. D‘arpa et al. published a series of nasolabial perforator flaps for alar reconstruction in 2009 [7]. In 2012, Qassemyar et al. published a series of 20 cadaver dissections establishing further the perforosomes of the facial artery perforators [8] already described by Taylor et al. [5]and confirming the results found by Hofer and colleagues [6]. There is no in vitro knowledge of how big a perforosome a perforator can supply. We found that the perforators are consistently located where they have previously been described, and a reliable skin island can be perfused based on any one of those perforators. Flap size varies and has in the more recent cases become bigger and extends well beyond usual random flap design without any surprises in terms of perfusion. Studies with facial transplantation have shown that, due to a rich vascularity and interconnections of perforosomes of the face an extensive area, a whole face, in fact, can survive on a single facial artery anastomosis [9]. With increased understanding of facial perforators and perforosomes, the perforator flaps have become a useful tool for the reconstructive surgeon. We attained a desired anatomical subunit replacement with the chosen flap design and an aesthetically pleasing result with high patient satisfaction in all cases. This seems to indicate that reconstruction of the aesthetic units are best attained by the mobility of the perforator flap and limited only by the donor site, preferably primarily closed within the boundaries of anatomical skin lines.
V-Y flaps are well published in the literature; however, we found in this small series, that a better understanding of their perforator origin has made them a safer choice and better reconstructive option. The supratrochlear flap is well known and has been used as an axial flap at least since the description of Sushruta Samhita, most often referred to as a forehead flap. The interconnection of the angular and supratrochlear artery indicates that a forehead flap could be based on either of the arteries increasing the freedom of rotation [10]. Forehead flaps often suffer from a venous congestion due to a compression, as was the case in our first propeller version which was probably due to a tight-fitting design causing tension on the distal part of the flap. The modeolus is the safest and most consistent perforator location [6, 8], and this has been the base of some of our biggest flaps and most satisfactory reconstructions of FAP flaps. The alar reconstruction in one stage has been published [7], since we started using it, and more recently, the supratrochlear flap was described by the same team [11]. This leaves only the zygomatic and modified Trepier periorbital flap remaining to be published.
Conclusion
We found that perforators are a constant anatomical finding in the facial area, and any known flap can, in theory, be based on the first perforator located at the flap rotation axis.
The random facial perforator flap seems to be a good and reliable option for the reconstruction of facial subunits, especially the periorbital, nasal, and periocular areas with a minimal morbidity and a pleasing result in a one-stage outpatient setting.
Acknowledgments
Conflict of interest
The authors declare no conflict of interest.
Patient consent
Patients provided written consent for the use of their images.
Ethical Standards
This study has been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All patients gave their informed consent prior to their inclusion in this study.
References
- 1.Jackson IT (2010) Local flaps of the head and neck. Quality Medical Pub; 2 edition
- 2.Thornton JF, Weathers WM. Nasolabial flap for nasal tip reconstruction. Plast Reconstr Surg. 2008;122(3):775–781. doi: 10.1097/PRS.0b013e318182370b. [DOI] [PubMed] [Google Scholar]
- 3.Jackson IT. Midline forehead flaps in nasal reconstruction. Eur J Plast Surg. 2004;27(3):105–113. [Google Scholar]
- 4.Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg. 1987;40(2):113–141. doi: 10.1016/0007-1226(87)90185-8. [DOI] [PubMed] [Google Scholar]
- 5.Houseman ND, Taylor GI, Pan WR. The angiosomes of the head and neck: anatomic study and clinical applications. Plast Reconstr Surg. 2000;105(7):2287–2313. doi: 10.1097/00006534-200006000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Hofer SO, Posch NA, Smit X. The facial artery perforator flap for reconstruction of perioral defects. Plast Reconstr Surg. 2005;115(4):996–1003. doi: 10.1097/01.PRS.0000154208.67390.5C. [DOI] [PubMed] [Google Scholar]
- 7.D'Arpa S, Cordova A, Pirrello R, Moschella F. Free style facial artery perforator flap for one stage reconstruction of the nasal ala. J Plast Reconstr Aesthet Surg. 2009;62(1):36–42. doi: 10.1016/j.bjps.2008.06.057. [DOI] [PubMed] [Google Scholar]
- 8.Qassemyar Q, Havet E, Sinna R. Vascular basis of the facial artery perforator flap: analysis of 101 perforator territories. Plast Reconstr Surg. 2012;129(2):421–493. doi: 10.1097/PRS.0b013e31822b6771. [DOI] [PubMed] [Google Scholar]
- 9.Pomahac B, Bueno EM, Sisk GC, Pribaz JJ. Current principles of facial allotransplantation: the Brigham and Women's Hospital Experience. Plast Reconstr Surg. 2013;131(5):1069–1076. doi: 10.1097/PRS.0b013e3182865cd3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kelly CP, Yavuzer R, Keskin M, Bradford M, Govila L, Jackson IT. Functional anastomotic relationship between the supratrochlear and facial arteries: an anatomical study. Plast Reconstr Surg. 2008;121(2):458–465. doi: 10.1097/01.prs.0000297651.52729.ec. [DOI] [PubMed] [Google Scholar]
- 11.Cordova A, D'Arpa S, Moschella F. A new one-stage method for nose reconstruction: the supratrochlear artery perforator propeller flap. Plast Reconstr Surg. 2012;129(3):571e–573e. doi: 10.1097/PRS.0b013e3182419bc4. [DOI] [PubMed] [Google Scholar]