Abstract
Background & Aims
Restrained food consumption may alter metabolic function and contribute to eventual weight gain; however, sex differences in these relationships have not been assessed. The objective of this study was to examine the relationship between restrained eating and insulin resistance and the influence of body mass index and sex on this relationship in a large community sample of both men and women. We hypothesized that restrained eating would be related to insulin resistance and this relationship would be influenced by sex and body mass index.
Methods
In this cross-sectional, observational study, we studied 487 individuals from the community (men N=222, women N=265), who ranged from lean (body mass index 18.5–24.9kg/m2, N=173), overweight (body mass index 25–29.9kg/m2, N=159) and obese (body mass index >30kg/m2, N=155) weight categories. We assessed restrained eating using the Dutch Eating Behavior Questionnaire and obtained fasting morning plasma insulin and glucose on all subjects.
Results
In men, but not in women, restrained eating was related to homeostatic model assessment of insulin resistance (HOMA-IR) (p<0.0001). Furthermore, homeostatic model assessment of insulin resistance levels were significantly higher in men who were high-versus low-restrained eaters (p=0.0006).
Conclusions
This study is the first to report sex differences with regard to the relationship between restrained eating and insulin resistance. Our results suggest that high restraint eating is associated with insulin resistance in men but not in women.
Keywords: sex differences, restrained eating, insulin resistance, obesity, dietary restraint
1.1 Introduction1
Obesity affects two-thirds of the United States population (Flegal et al., 2010). Many individuals attempt to control their weight by consciously limiting or restraining food intake. Unfortunately, restrained food consumption may alter metabolic function (Gingras et al., 2000; Keim et al., 2004; Reinhold G. Laessle et al., 1989; Pirke et al., 1990; Schur et al., 2008; Teff et al., 1996) and, in several studies, has been found to lead to eventual weight gain (Klesges et al., 1992; Stice et al., 2005). Some studies attribute this discrepancy to decreased energy expenditure in restrained eaters (Tuschl et al., 1990). Other studies have examined metabolic function in the setting of restrained eating (Gingras et al., 2000; Keim et al., 2004; Reinhold G. Laessle et al., 1989; Pirke et al., 1990; Schur et al., 2008; Teff et al., 1996). Most, but not all, of these studies have found that lean women who are restrained eaters have lower fasting insulin (Pirke et al., 1990), decreased insulin resistance, increased postprandial insulin and glucose, increased insulin sensitivity (Martins et al., 2009), and increased cephalic phase insulin response (Teff et al., 1996) as compared to their non-restrained counterparts. Women who are overweight and obese (OW/OB) restrained eaters are relatively more insulin sensitive as compared to non-restrained OW/OB women (Keim et al., 2004). These studies give valuable insight into metabolic pathophysiology that may contribute to weight gain in some restrained eaters but notably have limitations. A majority of these studies investigate restrained eating in women, rather than including both sexes, have a relatively small sample size, and include subjects who are either lean or OW/OB but do not assess differences across the weight spectrum. Additionally, none of these studies directly compare lean to obese restrained- and unrestrained-eaters in relation to insulin resistance and no study has examined sex differences in these relationships. As differences exist between men and women with respect to insulin resistance (Geer et al., 2009), we contend that men and women differ with regards to the relationship between restrained-eating and insulin resistance and that these metabolic discrepancies may partially account for differential patterns of weight gain in men and women. In this study, we examine the association of restrained eating and insulin resistance and the influence of body mass index (BMI) on this relationship in a large community sample of both men and women. We hypothesized that restrained eating would be related to insulin resistance and this relationship would be influenced by sex and BMI.
1.2 Materials and methods
1.2.1 Subjects: anthropometric and biochemical evaluation
Healthy men and women, between ages 18–50 years, were recruited from the community via local advertisements (see Supplemental methods for subject characteristics). The study was approved by the Yale Human Investigation Committee. All subjects provided signed informed consent. Subjects presented to the laboratory at 8:00am after an overnight fast; blood samples for fasting plasma glucose (FPG) and fasting insulin were obtained; weight and height were measured.
1.2.2 Assessments and Questionnaires
Demographic, physical and mental health assessments were obtained on all subjects. To assess restrained eating we used the Dutch Eating and Behavior Questionnaire (DEBQ) which is a valid measure of eating restraint, emotional eating, and external eating (Vanstrien et al., 1986; Wardle, 1987). In particular, the DEBQ’s Restraint (DEBQ-R) scale has been shown to be an effective tool for examining dietary restraint (R. G. Laessle et al., 1989; van Strien et al., 2007).
1.2.4 Statistical Analyses
Statistical Analysis Software was used to perform demographic statistics, correlations, and general linear model statistical analyses. (see supplemental materials for statistical details).
1.3 Results
1.3.1 Group demographics, behavioral measures, and metabolic parameters
We studied 487 individuals from the community (men N=222, women N=265), who were lean (BMI 18.5–24.9kg/m2, N=173), overweight (BMI 25–29.9kg/m2, N=159) and obese (BMI>30kg/m2, N=155). There were no statistically significant differences between men and women in this sample with regards to age, education, race, BMI, fasting insulin, and HOMA-IR. There was a statistically significant difference between the sexes with regard to FPG and reported restrained eating; men showed significantly higher levels of FPG compared to women, and women reported higher levels of restrained eating compared to men (Supplemental Table 1).
1.3.2 Metabolic parameters as a function of restrained eating, BMI, and gender
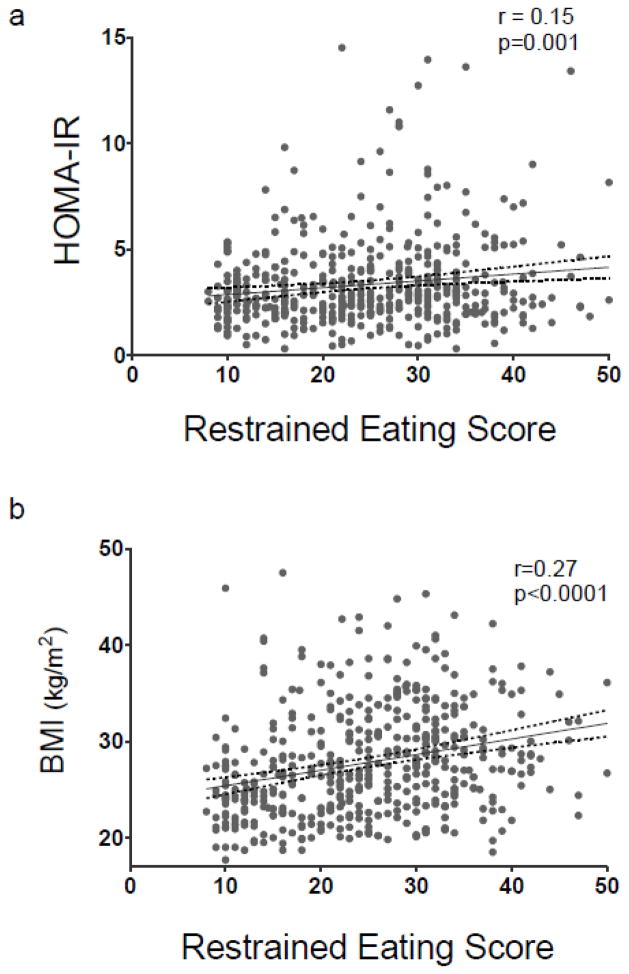
In the whole group, restrained eating was correlated with HOMA-IR (r=0.15, p=0.001) (Figure 1a), insulin (r=0.147, p=0.0012), and BMI (r=0.27, p<0.0001) (Figure 1b), while it was not correlated with glucose (r=0.02, p=0.66). Overall regression models for HOMA-IR indicated a significant effect of restrained eating (t=−2.18, p=0.03), and significant interactions between restrained eating and BMI (t=2.43, p=0.02), restrained eating and sex (t=2.25, p=0.03), BMI and sex (t=2.08, p=0.04), and restrained eating, BMI, and sex (t=−2.54, p=0.01) on HOMA-IR (Supplemental Table 2). On the other hand, overall regression models for fasting insulin indicated that significance level was marginally missed with regard to the effect of restrained eating on insulin (t=−1.96, p=0.051) and the effect of restrained eating and sex (t=1.93, p=0.054) on insulin. There was no significant interaction between sex and BMI (t=1.77, p=0.08) but there was a significant interaction between restrained eating and BMI (t=2.13, p=0.03) and restrained eating, BMI, and sex (t=−2.17, p=0.03).
Figure 1.
Scatter plots showing the associations between restrained eating and a) HOMA-IR and b) BMI.
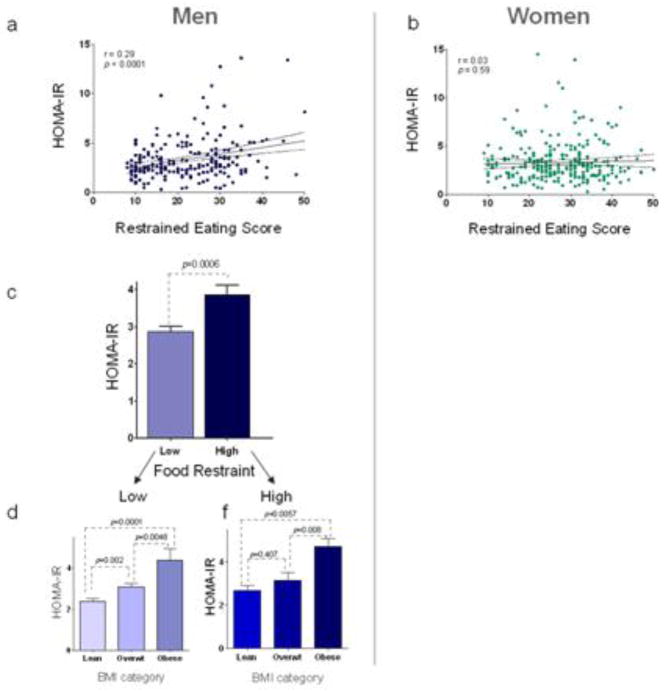
As sex was significantly interacting with restrained eating and BMI for HOMA-IR, follow-up models to explore these associations were conducted separately in men and women. In men, we found a significant relationship of restrained eating with HOMA-IR (t=−2.19, p=0.03), restrained eating with insulin levels (t=−1.99, p=0.05), and significant interactions between restrained eating and BMI (t=2.44, p=0.02) on HOMA-IR and between restrained eating and BMI on insulin (t=2.16, p=0.03). Meanwhile, in women, there were no significant effects of restraint eating on HOMA-IR or insulin and no significant interactions between restrained eating, BMI and HOMA-IR or insulin. (Supplemental Table 2). As HOMA-IR levels and restrained eating scores were correlated in men (r=0.29, p<0.0001) (Figure 2a) but not in women (r=0.03, p=0.59) (Figure 2b), we divided the group into low- and high-restrained eaters (median split) and found that HOMA-IR levels were statistically different in men who were low-versus high-restrained eaters (p=0.0006) (Figure 2c). An assessment of the significant interactions between restraint eating and BMI in men revealed that while in low-restrained eaters, HOMA-IR levels showed a significant graded increase different between each of the BMI categories, men who were high-restrained eaters showed no differences in HOMA-IR levels comparing the lean and overweight men, but a statistically significant difference between lean/overweight as compared to obese high-restrained men (Figure 2d). There were no associations that were significant for restrained eating effects on glucose or its interaction with BMI and sex.
Figure 2. Restrained eating and HOMA-IR levels in men and women.
Restrained eating is associated with insulin resistance in a) men but not in b) women. HOMA-IR levels are different in c) men who are high versus low restrained eaters. The difference in HOMA-IR levels in d) men is related to BMI category.
1.4 Discussion
The relationship between restrained eating and effects on metabolic milieu has been investigated in several small studies, generally conducted in women (Keim et al., 2004; Martins et al., 2009; Pirke et al., 1990; Teff et al., 1996); thus possible sex differences have largely been ignored. Given that there are known sex differences with regard to insulin resistance (Geer et al., 2009) as well as restrained eating (Alexander et al., 1995), we investigated whether sex differences exist between the association of restrained eating and insulin resistance. We found in men, but not in women, restrained eating is related to HOMA-IR, a measure of insulin resistance. This study is the first to report sex differences with regard to the relationship between restrained eating and insulin resistance. Additionally, no study has examined how BMI, sex, and restrained eating may relate to insulin resistance; our study shows that these variables interact and significantly relate to insulin resistance.
We found no interaction between restrained eating, insulin resistance, and BMI in women. Previous studies have reported that women who are restrained eaters are more insulin sensitive relative to those who are non-restrained (Keim et al., 2004; Martins et al., 2009). Our results may differ as we included a comparatively large sample of young women (N=267) from the community, screening out for psychiatric disorders including eating disorders. On the other hand, we found that in men insulin resistance was associated with restrained eating.
It has been reported that men may have higher insulin resistance than women possibly due to more visceral and hepatic adipose tissue in the setting of lower estrogen levels, which may be protective, as well as lower adiponectin levels (Geer et al., 2009). In the literature, two small studies examine insulin and glucose levels as they relate to restrained eating in lean and overweight men (Martins et al., 2009; Schur et al., 2008). In one study, lean men characterized as restrained eaters were found to have lower fasting insulin and lower postparandial insulin and glucose as compared to non-restrained lean men (Martins et al., 2009). In another study, in men who were lean or overweight, no relation was found with restrained eating insulin and glucose (Schur et al., 2008). Notably both of these studies included a small number of men (N=12 and N=10 respectively) and did not include any obese men (Martins et al., 2009; Schur et al., 2008). Our study includes a larger sample of men (N=222) who were lean, overweight, and obese and found that restrained eating is related to HOMA-IR levels. Restrained eaters who are obese had higher HOMA-IR levels than both the lean and overweight groups, thus this type of eating behavior may be associated with insulin resistance. In men who are high-restrained eaters, there were no differences between HOMA-IR levels in lean and overweight men but a statistically significant difference between lean/overweight as compared to obese high-restrained men. These differences suggest that restrained eating may affect men who are obese, highly-restrained eaters differently than men who are lean or overweight, highly-restrained eaters. Based on these findings, one may speculate that highly restrained food intake may confer some benefit in lean or overweight men with respect to metabolic function, but may contribute to insulin resistance or perhaps exacerbate metabolic dysfunction in obese men. Furthermore, some compensatory eating behaviors may be contributing to alterations in glucose metabolism/insulin function and higher insulin resistance may be affecting eating behavior in these individuals. Finally, restrained eating score was significantly higher in women as compared to men; this is consistent with previous findings (Kiefer et al., 2005).
There are several limitations of this study. First, its cross-sectional nature precludes determination of causality. Future longitudinal studies would be beneficial in assessing whether restrained eating contributes to the development of insulin resistance or whether insulin resistance affects restrained eating behaviors. Second, we do not report on actual food intake by recall or food frequency questionnaire. Lastly, it should be noted that our community sample was young (mean age 29.9 yrs), therefore, many of the complications associated with insulin resistance have not yet developed, thus our data may not be applicable to an older population with comorbid conditions.
1.4.1 Conclusions
Current findings suggest that insulin resistance may be linked to behavioral aspects of eating, such as food restraint. It is important to note that there were no differences in HOMA-IR levels across restrained groups in any BMI category; this suggests less of a direct effect of restraint category on insulin sensitivity. Food restraint may become salient in the context of stress and emotional eating, e.g. restrained eaters (men and women) increase food intake when under stressful conditions (Greeno et al., 1994; Oliver et al., 1999), while self-reported emotional eating is lower in normal weight individuals than in overweight or obese individuals (Geliebter et al., 2003). Thus, further studies may benefit from exploring stress, emotional factors, and food restraint effects on insulin resistance, i.e. assessing stress with the Perceived Stress Scale and examining how this may relate to insulin resistance and eating behavior. Our data underscore the need for research which investigates the relationship between eating behavior and metabolic state as well as how potential sex differences may affect treatment approaches.
Supplementary Material
Highlights.
In men, but not in women, restrained eating was related to HOMA-IR
HOMA-IR levels were higher in men who were high-vs. low-restrained eaters
Sex differences may exist between restrained eating and insulin resistance
Acknowledgments
Grant Funding: This work publication was made possible by UL1-DE019586, PL1-DA024859, K12 DK094714, and by CTSA grant number UL1 RR024139 from the National Center for Research Resources (NCRR) and the National Center for Advancing Translational Science (NCATS), components of the National Institutes of Health (NIH), and NIH roadmap for Medical Research.
Footnotes
Non-standard abbreviations: BMI, body mass index; DEBQ, Dutch Eating Behavior Questionnaire; FPG, fasting plasma glucose; HOMA-IR, Homeostatic Model Assessment of insulin resistance; OW, Overweight; OB, Obese; SAS, Statistical Analysis Software
Conflict of interest: The authors declare that they have no conflicts of interest associated with this manuscript.
Author contributions: R.S. was responsible for the funding and study design; R.S. and E.G. were responsible for the data collection; P.G., R.S., and A.M.J. conducted data analysis; R.S. and A.M.J contributed to the interpretation of the data; A.M.J. and R.S. wrote the manuscript. The authors thank Robert Sherwin in his guidance interpreting the data.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ania M. Jastreboff, Email: Ania.Jastreboff@yale.edu.
Edward C. Gaiser, Email: Edward.Gaiser@yale.edu.
Peihua Gu, Email: Peihua.Gu@yale.edu.
Rajita Sinha, Email: Rajita.Sinha@yale.edu.
References
- Alexander JM, Tepper BJ. Use of Reduced-Calorie/Reduced-Fat Foods by Young Adults: Influence of Gender and Restraint. Appetite. 1995;25(3):217–230. doi: 10.1006/appe.1995.0057. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. 2009.2014 [pii] [DOI] [PubMed] [Google Scholar]
- Geer EB, Shen W. Gender differences in insulin resistance, body composition, and energy balance. Gender Medicine. 2009;6(Part10):60–75. doi: 10.1016/j.genm.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geliebter A, Aversa A. Emotional eating in overweight, normal weight, and underweight individuals. Eating Behaviors. 2003;3(4):341–347. doi: 10.1016/s1471-0153(02)00100-9. [DOI] [PubMed] [Google Scholar]
- Gingras JR, Harber V, Field CJ, McCargar LJ. Metabolic assessment of female chronic dieters with either normal or low resting energy expenditures. The American Journal of Clinical Nutrition. 2000;71(6):1413–1420. doi: 10.1093/ajcn/71.6.1413. [DOI] [PubMed] [Google Scholar]
- Greeno CG, Wing RR. Stress-induced eating. Psychol Bull. 1994;115(3):444–464. doi: 10.1037/0033-2909.115.3.444. [DOI] [PubMed] [Google Scholar]
- Keim NL, Horn WF. Restrained Eating Behavior and the Metabolic Response to Dietary Energy Restriction in Women[ast][ast] Obesity. 2004;12(1):141–149. doi: 10.1038/oby.2004.19. [DOI] [PubMed] [Google Scholar]
- Kiefer I, Rathmanner T, Kunze M. Eating and dieting differences in men and women. The Journal of Men’s Health & Gender. 2005;2(2):194–201. http://dx.doi.org/10.1016/j.jmhg.2005.04.010. [Google Scholar]
- Klesges RC, Isbell TR, Klesges LM. Relationship between dietary restraint, energy intake, physical activity, and body weight: a prospective analysis. J Abnorm Psychol. 1992;101(4):668–674. doi: 10.1037//0021-843x.101.4.668. [DOI] [PubMed] [Google Scholar]
- Laessle RG, Tuschl RJ, Kotthaus BC, Pirke KM. Behavioral and biological correlates of dietary restraint in normal life. Appetite. 1989;12(2):83–94. doi: 10.1016/0195-6663(89)90098-6. [DOI] [PubMed] [Google Scholar]
- Laessle RG, Tuschl RJ, Kotthaus BC, Pirke KM. A comparison of the validity of three scales for the assessment of dietary restraint. [Comparative Study] J Abnorm Psychol. 1989;98(4):504–507. doi: 10.1037//0021-843x.98.4.504. [DOI] [PubMed] [Google Scholar]
- Martins C, Morgan LM, Robertson MD. Effects of restrained eating behaviour on insulin sensitivity in normal-weight individuals. Physiol Behav. 2009;96(4–5):703–708. doi: 10.1016/j.physbeh.2009.01.006. S0031-9384(09)00018-3 [pii] [DOI] [PubMed] [Google Scholar]
- Oliver G, Wardle J. Perceived Effects of Stress on Food Choice. Physiology & Behavior. 1999;66(3):511–515. doi: 10.1016/s0031-9384(98)00322-9. [DOI] [PubMed] [Google Scholar]
- Pirke KM, Tuschl RJ, Spyra B, Laessle RG, Schweiger U, Broocks A, Zitzelsberger G. Endocrine findings in restrained eaters. Physiol Behav. 1990;47(5):903–906. doi: 10.1016/0031-9384(90)90017-x. 0031-9384(90)90017-X [pii] [DOI] [PubMed] [Google Scholar]
- Schur EA, Cummings DE, Callahan HS, Foster-Schubert KE. Association of cognitive restraint with ghrelin, leptin, and insulin levels in subjects who are not weight-reduced. Physiology & Behavior. 2008;93(4–5):706–712. doi: 10.1016/j.physbeh.2007.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Presnell K, Shaw H, Rohde P. Psychological and behavioral risk factors for obesity onset in adolescent girls: a prospective study. J Consult Clin Psychol. 2005;73(2):195–202. doi: 10.1037/0022-006X.73.2.195. 2005-02854-001 [pii] [DOI] [PubMed] [Google Scholar]
- Teff KL, Engelman K. Palatability and dietary restraint: Effect on cephalic phase insulin release in women. Physiology & Behavior. 1996;60(2):567–573. doi: 10.1016/s0031-9384(96)80033-3. [DOI] [PubMed] [Google Scholar]
- Tuschl RJ, Platte P, Laessle RG, Stichler W, Pirke KM. Energy expenditure and everyday eating behavior in healthy young women. The American Journal of Clinical Nutrition. 1990;52(1):81–86. doi: 10.1093/ajcn/52.1.81. [DOI] [PubMed] [Google Scholar]
- van Strien T, Herman CP, Engels RCME, Larsen JK, van Leeuwe JFJ. Construct validation of the Restraint Scale in normal-weight and overweight females. Appetite. 2007;49(1):109–121. doi: 10.1016/j.appet.2007.01.003. [DOI] [PubMed] [Google Scholar]
- Vanstrien T, Frijters JER, Bergers GPA, Defares PB. The Dutch Eating Behavior Questionnaire (Debq) for Assessment of Restrained, Emotional, and External Eating Behavior. International Journal of Eating Disorders. 1986;5(2):295–315. [Google Scholar]
- Wardle J. Eating style: a validation study of the Dutch Eating Behaviour Questionnaire in normal subjects and women with eating disorders. [Research Support, Non-U.S. Gov’t] J Psychosom Res. 1987;31(2):161–169. doi: 10.1016/0022-3999(87)90072-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.