Abstract
Introduction
The literature reflects a resurgence of interest in endoscopic and keyhole endoscope-assisted neurosurgical approaches as alternatives to conventional microsurgical approaches in carefully selected cases. The aim of this study was to assess the technical challenges of neuroendoscopy, and the scope for technological innovations to overcome these barriers.
Materials and Methods
All full members of the Society of British Neurosurgeons (SBNS) were electronically invited to participate in an online survey. The open-ended structured survey asked three questions; firstly, whether the surgeon presently utilises or has experience with endoscopic or endoscope-assisted approaches; secondly, what they consider to be the major technical barriers to adopting such approaches; and thirdly, what technological advances they foresee improving safety and efficacy in the field. Responses were subjected to a qualitative research method of multi-rater emergent themes analysis.
Results
Three clear themes emerged: 1) surgical approach and better integration with image-guidance systems (20%), 2) intra-operative visualisation and improvements in neuroendoscopy (49%), and 3) surgical manipulation and improvements in instruments (74%).
Discussion
The analysis of responses to our open-ended survey revealed that although opinion was varied three major themes could be identified. Emerging technological advances such as augmented reality, high-definition stereo-endoscopy, and robotic joint-wristed instruments may help overcome the technical difficulties associated with neuroendoscopic approaches.
Conclusions
Results of this qualitative survey provide consensus amongst the technology end-user community such that unambiguous goals and priorities may be defined. Systems integrating these advances could improve the safety and efficacy of endoscopic and endoscope-assisted neurosurgical approaches.
Keywords: Endoscopy, Neuroendoscopy, Minimally Invasive Surgical Procedures, Questionnaires
Introduction
Over the last decade, the neurosurgical literature has reflected a resurgence of clinical interest in endoscopic and keyhole endoscope-assisted neurosurgical approaches as alternatives to conventional microsurgical approaches in carefully selected cases1-3. Such approaches promise reduced exposure and manipulation of brain tissue, but can also present substantial technical challenges that may limit their safety and efficacy. Identification and understanding these barriers is a prerequisite to progress in the field. The aim of this study was to assess the technical challenges of neuroendoscopy, and the scope for technological innovations to overcome these barriers.
Materials and Methods
A qualitative study design was adopted to gain a broad understanding of the perceived technical challenges of neuroendoscopy, and the potential for technological solutions. In contrast to quantitative studies, which seek to evaluate a large number of randomly selected participants representing the population of interest using closed surveys, qualitative studies generally sample a small number of participants in more detailed open surveys. Saturation of data collection in qualitative studies is said to occur when no new or relevant information emerges with further participants, which we estimated would require approximately 20 participants based on similar studies in other surgical fields4.
Participants
All 249 full members of the Society of British Neurosurgeons (SBNS) were electronically invited to participate in an online survey on endoscopic and endoscope-assisted neurosurgery. Only one attempt at contact was made with members, and the survey was closed one week following initial distribution as the number of responders had already exceeded our a priori estimate to achieve saturation.
Survey
Participating members were asked to disclose their name, surgical unit and subspecialty interests. The open-ended structured survey asked three questions. Firstly, whether the surgeon presently utilises or has experience with endoscopic or endoscope-assisted approaches. Secondly, what they consider to be the major technical barriers to adopting such approaches. Thirdly, what technological advances they foresee improving safety and efficacy in the field.
Responses were collected, anonymised, and consolidated in a single spreadsheet for qualitative analysis.
Data Analysis
Three authors analysed survey responses (HJM, TPC and AHH). Based on a preliminary screen, responses were first coded for indications of general philosophy on the utilisation of endoscopic and endoscope-assisted approaches, and also for specific barriers to the adoption of such approaches. Subsequently, using iterative analysis, responses were parsed for themes by individual raters (see Figure 1).
Figure 1.
Qualitative analysis methodology.
After agreement was reached on themes, raters returned to the survey responses and binary coded for theme content. Raters initially performed this analysis independently; agreement was reached based on discussion during consensus meetings.
All counts were tallied and expressed as percentages. As each participant may have referenced multiple theme categories, percentage totals did not necessarily tally to 100. Completed surveys were assigned identifying labels based on chronological order of receipt, i.e. ‘Participant 1’, ‘Participant 2’, ‘Participant 3’.
Results
In all, 40 consultant neurosurgeons participated in the survey within a week of initial distribution (response rate 16.1%). Specialty interests of responding neurosurgeons were mostly distributed amongst neuro-oncology (53%), paediatric (43%) or skull base surgery (38%) (see Table 1).
Table 1.
Subspecialty of neurosurgeons participating in survey.
| Subspecialty | Number of participants (%) |
|---|---|
| Neuro-oncology | 21 (53%) |
| Paediatric | 17 (43%) |
| Skull base | 15 (38%) |
| Neurovascular | 12 (30%) |
| Spine and peripheral nerve | 12 (30%) |
| Trauma | 7 (18%) |
| Functional | 4 (10%) |
Of the 40 neurosurgeons that took part in the study, 38 described their own endoscopic practice. The majority performed intraventricular procedures including endoscopic third ventriculostomy (63%) or endonasal transphenoidal procedures (37%) (see Table 2).
Table 2.
Practice of neurosurgeons participating in survey.
| Practice | Number of participants (%) |
|---|---|
| Endoscopic third ventriculostomy and other intraventricular approaches |
24 (63%) |
| Endonasal transphenoidal and extended transphenoidal approaches |
14 (37%) |
| Transcranial endoscope-assisted microsurgery |
8 (21%) |
| Other e.g. endoscopic resection of intraparenchymal brain tumours |
0 (0%) |
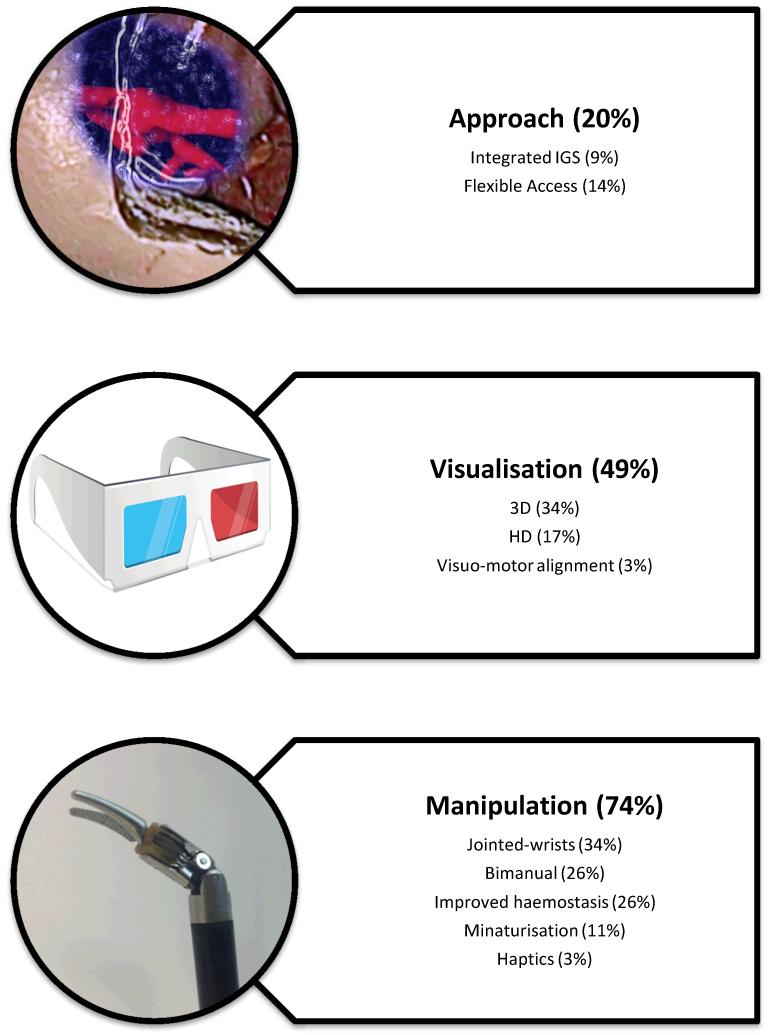
Thirty-five participants provided detailed opinions on the technical challenges of endoscopic and keyhole endoscope-assisted neurosurgical approaches, and the scope for technological innovations to improve safety and efficacy in the field. Three clear themes emerged; 1) surgical approach and better integration with image-guidance systems (20%), 2) intra-operative visualisation and improvements in neuroendoscopy (49%), and 3) surgical manipulation and improvements in instruments (74%). Major themes and subthemes identified in the study are illustrated in Figure 2. Saturation of themes and subthemes were achieved after 5 and 25 participants respectively.
Figure 2.
Themes and subthemes, in order of frequency that they were mentioned. Note that each respondent could mention several sub-themes, so totals do not tally to 100%. IGS = Image Guidance System; 3D = 3-Dimensional; HD = High Definition
Approach
Several neurosurgeons commented on the need for “better image guidance system integration” (Participant 25) into the surgical workflow. Five respondents additionally suggested that such systems could be used to guide “navigatable flexible endoscopes” (Participant 4) during the surgical approach, which would allow critical neurovascular structures to be avoided.
Visualisation
Almost half of responding neurosurgeons described current endoscopic visualisation as a barrier to further adoption of the technique. The most highly cited subtheme was lack of “3D and depth perception” (Participant 21) provided by most presently available neuroendoscopes, which impaired appreciation of complex spatial relationships within the brain. One surgeon qualified their support by suggesting that “3D will help the less experienced the most” (Participant 33), and another cautioned that while improved imaging would be useful, they were “not sure if 3D will be as good as it is hyped to be”.
Several neurosurgeons commented on the “quality of image” (Participant 35) provided by endoscopes, and the need for “better optics” (Participant 4), and “improved pictures…as they tend to degrade over time” (Participant 22). One respondent felt that visuomotor misalignment was another limitation of current neuroendoscopy platforms, stating that “it is awkward…to have to look in one direction and operate in another” (Participant 25).
Manipulation
The majority of survey participants described technical difficulties with available endoscopic instruments as a major limitation of neuroendoscopy. The most highly cited subtheme was lack of dexterity when using rigid instruments down a narrow surgical trajectory, “…the majority of current instruments preclude true microsurgical techniques and rely mostly on traction and pulling” (Participant 28). One surgeon described, for example, how “…stitching or closing dura” (Participant 10) was difficult or impossible to perform through endoscopic approaches. Several neurosurgeons felt that robotic articulated instruments might overcome this barrier, “endoscopic micro-instruments with similar degrees of freedom as a Da Vinci robot” (Participant 2).
Another common subtheme was the “difficulty to free both hands for operating” (Participant 23), thus limiting the bimanual manipulation that characterises microsurgical dissection. Several neurosurgeons expanded on this, explaining that it was “difficult for the assistant to be of any help… so tends to be suction one hand and dissection other hand” (Participant 33). A few respondents suggested that “more user-friendly endoscope holders” (Participant 23) or perhaps a robotic scope holder “that would allow remotely controlled scope movement” (Participant 18), might allow for bimanual manipulation.
Many neurosurgeons were concerned about adequate haemostasis, especially “controlling major arterial bleeding” (Participant 10). Participants felt that current bipolar forceps were inadequate during endoscopic approaches, and that improvements in their design would improve safety. Four neurosurgeons mentioned that “lack of working equipment such as a CUSA that can fit down the scope” also limited the adoption of endoscopic approaches, particularly within the field of neuro-oncology. One surgeon described how endoscopic approaches lacked “haptic quality” (Participant 21) compared to conventional microneurosurgery, and that this might impact surgical performance.
General comments
One respondent emphasised that regardless of tool development, “a fool with a tool is still a fool… the major limitation would be if the surgeon themselves fails to understand this.” (Participant 6). Two neurosurgeons recognised the long learning curve of endoscopic approaches to be a major limitation, and one surgeon commented that “simulation and training” (Participant 21), alongside tool development, would help overcome this.
Discussion
Endoscopy has been applied to the field of neurosurgery since the work of early pioneers such as Walter Dandy approximately a century ago5. In recent years, technological advances such as the development of image-guidance systems, endoscopes with improved image quality, and tube-shaft instruments, have ignited a resurgence of enthusiasm in the field, with specific procedures such as Endoscopic Third Ventriculostomy (ETV) and endoscopic endonasal transphenoidal hypophysectomy now relatively well accepted by the neurosurgical community in carefully selected cases6, 7. The analysis of responses to our open-ended survey revealed that although opinion was varied on the technical challenges of neuroendoscopy, and the scope for technological improvements to overcome these barriers, three major themes could be identified: surgical approach and better integration with image-guidance systems (20%); intra-operative visualisation and improvements in neuroendoscopy (49%); and surgical manipulation and improvements in instruments (74%).
Surgical approach and integration with image-guidance systems
Image guidance systems, are now widely used within neurosurgery and are associated with shorter operated times, reduced blood loss, and less complications than conventional surgery8. In light of the availability and use of image guidance systems it was, at first glance, somewhat counterintuitive that difficulty in surgical access was still identified as a significant limitation of present-day neuroendoscopy. Several neurosurgeons reported the need for better integration of image guidance systems into the surgical workflow. We speculate that the relative paucity of external landmarks and potential for disorientation in endoscopic approaches results in frequent interruptions during surgery to place the image guidance probe and turn away from the operative field to view the image display monitors. In the near future, augmented reality systems may allow for more seamless integration of image guidance systems by overlaying virtual targets onto the surgical scene9-11.
Intra-operative visualisation and improvements in neuroendoscopy
Endoscopic visualisation was also a major theme identified by respondents. Although endoscopy provides a much wider view angle through narrow surgical corridors compared to microscopy, most available endoscopy systems are impaired by far lower image quality and very few offer stereoscopy. To this end, it is anticipated that the development of high definition (HD) and 3-dimensional (3D) endoscopes will overcome this hurdle. Early studies have already suggested that the use of such endoscopes allows for improved recognition of anatomical landmarks, and better appreciation of complex spatial relationships12-16.
Surgical manipulation and improvements in instruments
Surgical manipulation was the theme most frequently identified by participants as the key to developing safer and more efficacious endoscopic and keyhole endoscope-assisted neurosurgical approaches. Currently available instruments do not allow for dissection in the same way as conventional microsurgical approaches, reducing surgical dexterity to largely co-axial control through narrow corridors, and often limiting neurosurgeons to single-handed manipulation. Most neurosurgical operations, such as tumour resection, are therefore far more difficult to perform through keyhole approaches. Technological advances, such as robotic instruments with articulated wrist-joints, may free neurosurgeons of ergonomic burdens imposed by ‘chopstick’ surgery17.
Limitations of the study
There are several limitations of the present study. Notably, the sample size was small, and the response rate low, reflecting our adoption of a qualitative rather than quantitative study design. A qualitative methodology was selected as the aim of the study was to gain an understanding of the perceived technical limitations of neuroendoscopy, and the possible role for technological advances, rather than measure the frequency of predefined opinions. Although all members of the SBNS were invited to participate in the survey, neurosurgeons almost certainly self-selected if they had a specialist interest in neuroendoscopy, as reflected by the relatively high number of paediatric and skull base neurosurgeons responding (who were far more likely to be routinely involved with intraventricular and endonasal transsphenoidal approaches respectively). The a priori goal of saturation of themes and subthemes was achieved and it is likely that the key findings of the research are externally valid.
Another inherent limitation of the open-ended online survey study design was that it prevented probing of respondents’ answers. However, we do not believe that it would have been feasible to reach as many neurosurgeons had we required them to commit to time-intensive interviews. In any case, several neurosurgeons provided extended answers to the survey prompts, allowing fairly detailed analysis of the major themes and subthemes identified.
Conclusions
We have identified several common themes highlighted by neurosurgeons as important barriers to the adoption of endoscopic and endoscope-assisted neurosurgery. These themes may be summarised as poor integration of current image-guidance systems, lack of 3D visualisation with most presently available neuroendoscopes, and limited scope for dextrous bimanual manipulation with rigid tube-shaft instruments. Emerging technological advances such as augmented reality, high-definition stereo-endoscopy, and robotic joint-wristed instruments, may help overcome the technical difficulties associated with neuroendoscopic approaches18.
Acknowledgements
H. J. Marcus is supported by an Imperial College Wellcome Trust Clinical Fellowship.
Footnotes
Declaration of interest
The authors report no declarations of interest.
References
- 1.Perneczky A, Reisch R. Keyhole approaches in neurosurgery. Volume 1: Concept and surgical technique. 1 ed Springer; 2008. [Google Scholar]
- 2.Reisch R, Stadie A, Kockro RA, Hopf N. The Keyhole Concept in Neurosurgery. World Neurosurg. 2012 Feb 10; doi: 10.1016/j.wneu.2012.02.024. [DOI] [PubMed] [Google Scholar]
- 3.Prevedello DM, Doglietto F, Jane JA, Jr., Jagannathan J, Han J, Laws ER., Jr. History of endoscopic skull base surgery: its evolution and current reality. J Neurosurg. 2007 Jul;107(1):206–213. doi: 10.3171/JNS-07/07/0206. [DOI] [PubMed] [Google Scholar]
- 4.Pernar LI, Ashley SW, Smink DS, Zinner MJ, Peyre SE. Master surgeons’ operative teaching philosophies: a qualitative analysis of parallels to learning theory. J Surg Educ. 2012 Jul-Aug;69(4):493–498. doi: 10.1016/j.jsurg.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Hsu W, Li KW, Bookland M, Jallo GI. Keyhole to the brain: Walter Dandy and neuroendoscopy. J Neurosurg Pediatr. 2009 May;3(5):439–442. doi: 10.3171/2009.1.PEDS08342. [DOI] [PubMed] [Google Scholar]
- 6.Rasul FT, Marcus HJ, Toma AK, Thorne L, Watkins LD. Is endoscopic third ventriculostomy superior to shunts in patients with non-communicating hydrocephalus? A systematic review and meta-analysis of the evidence. Acta Neurochir (Wien) 2013 May;155(5):883–889. doi: 10.1007/s00701-013-1657-5. [DOI] [PubMed] [Google Scholar]
- 7.Goudakos JK, Markou KD, Georgalas C. Endoscopic versus microscopic trans-sphenoidal pituitary surgery: a systematic review and meta-analysis. Clin Otolaryngol. 2011 Jun;36(3):212–220. doi: 10.1111/j.1749-4486.2011.02331.x. [DOI] [PubMed] [Google Scholar]
- 8.Paleologos TS, Wadley JP, Kitchen ND, Thomas DG. Clinical utility and cost-effectiveness of interactive image-guided craniotomy: clinical comparison between conventional and image-guided meningioma surgery. Neurosurgery. 2000 Jul;47(1):40–47. doi: 10.1097/00006123-200007000-00010. discussion 47-48. [DOI] [PubMed] [Google Scholar]
- 9.Kawamata T, Iseki H, Shibasaki T, Hori T. Endoscopic augmented reality navigation system for endonasal transsphenoidal surgery to treat pituitary tumors: technical note. Neurosurgery. 2002 Jun;50(6):1393–1397. doi: 10.1097/00006123-200206000-00038. [DOI] [PubMed] [Google Scholar]
- 10.Caversaccio M, Garcia Giraldez J, Thoranaghatte R, et al. Augmented reality endoscopic system (ARES): preliminary results. Rhinology. 2008 Jun;46(2):156–158. [PubMed] [Google Scholar]
- 11.Thoranaghatte RU, Giraldez JG, Zheng G. Landmark based augmented reality endoscope system for sinus and skull-base surgeries. Conf Proc IEEE Eng Med Biol Soc. 2008;2008:74–77. doi: 10.1109/IEMBS.2008.4649094. [DOI] [PubMed] [Google Scholar]
- 12.Conrad J, Philipps M, Oertel J. High-definition imaging in endoscopic transsphenoidal pituitary surgery. Am J Rhinol Allergy. 2011 Jan-Feb;25(1):e13–17. doi: 10.2500/ajra.2010.25.3542. [DOI] [PubMed] [Google Scholar]
- 13.Fraser JF, Allen B, Anand VK, Schwartz TH. Three-dimensional neurostereoendoscopy: subjective and objective comparison to 2D. Minim Invasive Neurosurg. 2009 Feb;52(1):25–31. doi: 10.1055/s-0028-1104567. [DOI] [PubMed] [Google Scholar]
- 14.Schroeder HW, Nehlsen M. Value of high-definition imaging in neuroendoscopy. Neurosurg Rev. 2009 Jul;32(3):303–308. doi: 10.1007/s10143-009-0200-x. discussion 308. [DOI] [PubMed] [Google Scholar]
- 15.Roth J, Fraser JF, Singh A, Bernardo A, Anand VK, Schwartz TH. Surgical approaches to the orbital apex: comparison of endoscopic endonasal and transcranial approaches using a novel 3D endoscope. Orbit. 2011 Jan;30(1):43–48. doi: 10.3109/01676830.2010.543004. [DOI] [PubMed] [Google Scholar]
- 16.Roth J, Singh A, Nyquist G, et al. Three-dimensional and 2-dimensional endoscopic exposure of midline cranial base targets using expanded endonasal and transcranial approaches. Neurosurgery. 2009 Dec;65(6):1116–1128. doi: 10.1227/01.NEU.0000360340.85186.7A. discussion 1128-1130. [DOI] [PubMed] [Google Scholar]
- 17.Marcus H, Nandi D, Darzi A, Yang GZ. Surgical Robotics Through a Keyhole: From Today’s Translational Barriers to Tomorrow’s “Disappearing” Robots. IEEE Trans Biomed Eng. 2013 Mar;60(3):674–681. doi: 10.1109/TBME.2013.2243731. [DOI] [PubMed] [Google Scholar]
- 18.Marcus HJ, Seneci CA, Payne CJ, Nandi D, Darzi A, Yang GZ. Robotics in Keyhole Transcranial Endoscope-assisted Microsurgery: A Critical Review of Existing Systems and Proposed Specifications for New Robotic Platforms. Neurosurgery. 2013 Aug 5; doi: 10.1227/NEU.0000000000000123. [DOI] [PubMed] [Google Scholar]