Abstract
Viral infections play an important role in human diseases, and recent outbreaks in the advent of globalization and ease of travel have underscored their prevention as a critical issue in safeguarding public health. Despite the progress made in immunization and drug development, many viruses lack preventive vaccines and efficient antiviral therapies, which are often beset by the generation of viral escape mutants. Thus, identifying novel antiviral drugs is of critical importance and natural products are an excellent source for such discoveries. In this mini-review, we summarize the antiviral effects reported for several natural products and herbal medicines.
Keywords: Antiviral, Drug development, Herbal medicines, Natural products
INTRODUCTION
Viruses are responsible for a number of human pathogeneses including cancer. Several hard-to-cure diseases and complex syndromes including Alzheimer's disease, type 1 diabetes, and hepatocellular carcinoma have been associated with viral infections.[1,2,3] Moreover, due to increased global travel and rapid urbanization, epidemic outbreaks caused by emerging and re-emerging viruses represent a critical threat to public health, particularly when preventive vaccines and antiviral therapies are unavailable. Examples include the recent emergence of dengue virus, influenza virus, measles virus, severe acute respiratory syndrome (SARS) virus, and West Nile virus outbreaks.[4,5,6] To date, however, many viruses remain without effective immunization and only few antiviral drugs are licensed for clinical practice. The situation is further exacerbated by the potential development of drug-resistant mutants, especially when using viral enzyme-specific inhibitors, which significantly hampers drug efficacy.[7,8,9,10] Hence, there is an urgent need to discover novel antivirals that are highly efficacious and cost-effective for the management and control of viral infections when vaccines and standard therapies are lacking.
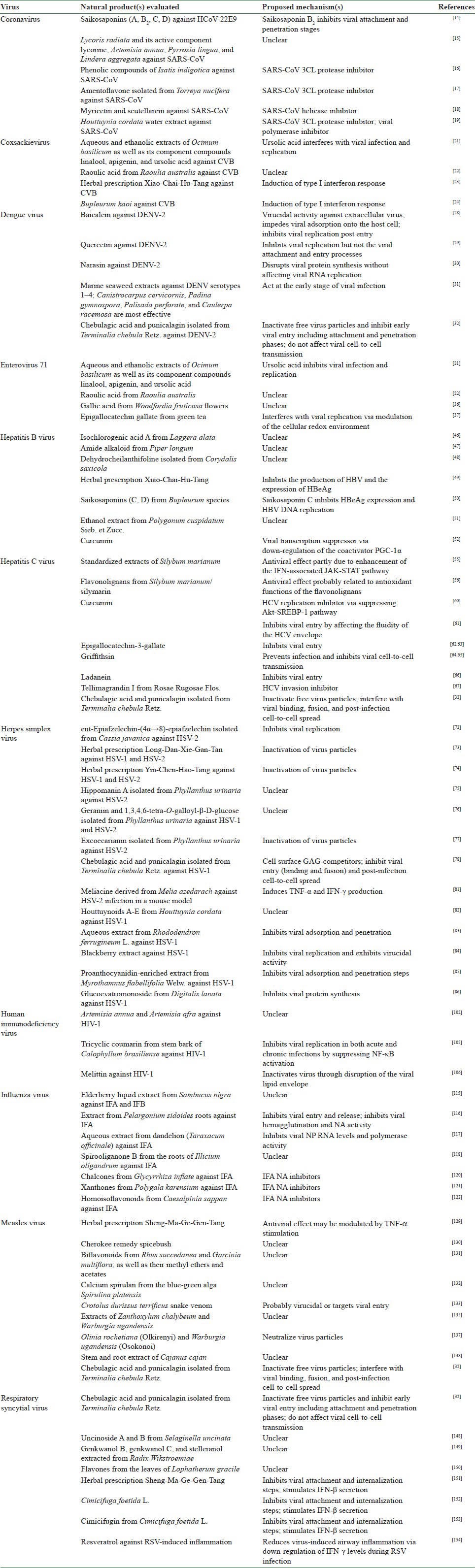
Herbal medicines and purified natural products provide a rich resource for novel antiviral drug development. Identification of the antiviral mechanisms from these natural agents has shed light on where they interact with the viral life cycle, such as viral entry, replication, assembly, and release, as well as on the targeting of virus–host-specific interactions. In this brief report, we summarize the antiviral activities from several natural products and herbal medicines against some notable viral pathogens including coronavirus (CoV), coxsackievirus (CV), dengue virus (DENV), enterovirus 71 (EV71), hepatitis B virus (HBV), hepatitis C virus (HCV), herpes simplex virus, human immunodeficiency virus (HIV), influenza virus, measles virus (MV), and respiratory syncytial virus (RSV) [Table 1].
Table 1.
Antiviral effects from several natural products and herbal medicines against specific viruses.
CORONAVIRUS
CoV is an enveloped, positive-sense single-stranded RNA (ssRNA) virus belonging to the Coronaviridae family. The CoV family consists of several species and causes upper respiratory tract and gastrointestinal infections in mammals and birds. In humans, it mainly causes common cold, but complications including pneumonia and SARS can occur.[11] The known human CoV (HCoV) includes HCoV-229E, -OC43, -NL63, -HKU1, and the more widely known severe acute respiratory syndrome coronavirus (SARS-CoV) which caused a global threat with high mortality in 2003.[12] In 2012, the World Health Organization (WHO) designated a sixth type of HCoV infection identified as the Middle East respiratory syndrome coronavirus (MERS-CoV) which is associated with high fatality.[13]
There are no specific treatments for CoV infection and preventive vaccines are still being explored. Thus, the situation reflects the need to develop effective antivirals for prophylaxis and treatment of CoV infection. We have previously reported that saikosaponins (A, B2, C, and D), which are naturally occurring triterpene glycosides isolated from medicinal plants such as Bupleurum spp. (柴胡 Chái Hú), Heteromorpha spp., and Scrophularia scorodonia (玄參 Xuán Shēn), exert antiviral activity against HCoV-22E9.[14] Upon co-challenge with the virus, these natural compounds effectively prevent the early stage of HCoV-22E9 infection, including viral attachment and penetration. Extracts from Lycoris radiata (石蒜 Shí Suàn), Artemisia annua (黃花蒿 Huáng Huā Hāo), Pyrrosia lingua (石葦 Shí Wěi), and Lindera aggregata (烏藥 Wū Yào) have also been documented to display anti–SARS-CoV effect from a screening analysis using hundreds of Chinese medicinal herbs.[15] Natural inhibitors against the SARS-CoV enzymes, such as the nsP13 helicase and 3CL protease, have been identified as well and include myricetin, scutellarein, and phenolic compounds from Isatis indigotica (板藍根 Bǎn Lán Gēn) and Torreya nucifera (榧 Fěi).[16,17,18] Other anti-CoV natural medicines include the water extract from Houttuynia cordata (魚腥草 Yú Xīng Cǎo), which has been observed to exhibit several antiviral mechanisms against SARS-CoV, such as inhibiting the viral 3CL protease and blocking the viral RNA-dependent RNA polymerase activity.[19]
COXSACKIEVIRUS
CV, including subgroups A (CVA) and B (CVB), is a member of the Picornaviridae family, and the non-enveloped positive-sense ssRNA virus is typically transmitted by fecal–oral route and contact with respiratory secretions. While the symptoms of infection can include mild illnesses such as fever, malaise, rashes, and common cold-like presentation, more severe cases may result in diseases of the central nervous system, including aseptic meningitis, encephalitis, and paralysis.[20] CVA is best known as one of the causative agents of hand, foot, and mouth disease (HFMD) in young children.
Unfortunately, there is no vaccine or specific antiviral therapy available to prevent CV infection or the diseases it causes. Nevertheless, drugs discovered from natural products, herbs, and traditional decoctions have shown some promise for the development of therapeutics against CV infection. The aqueous extract, ethanolic extract, and bioactive compounds including linalool, apigenin, and ursolic acid from the popular culinary/medicinal herb Ocimum basilicum (sweet basil) (羅勒 Luó Lè) have been observed to possess antiviral activity against CVB1.[21] In particular, ursolic acid interferes with CVB1 replication post-infection.[21] Raoulic acid from Raoulia australis has also been reported as a potential antiviral agent against several CVB subtypes, but the mechanism of its effect is unclear.[22] In addition, we have previously reported that both the medicinal prescription Xiao-Chai-Hu-Tang (小柴胡湯 Xiǎo Chái Hú Tang) and its major component herb Bupleurum kaoi (柴胡 Chái Hú) inhibit CVB1 infection via the induction of type I interferon response.[23,24] This finding suggests that type I interferon inducers may be helpful in controlling CVB infection and could be further explored as a treatment strategy.
DENGUE VIRUS
DENV is an enveloped positive-sense ssRNA virus of the Flaviviridae family. As a prominent arbovirus in Southeast Asia, DENV is transmitted by mosquito bites, typically by Aedes aegypti.[25] Four serotypes of the virus exist (DENV1 − 4) and all can cause dengue fever.[26] Clinical manifestations of DENV infection can include inapparent/mild febrile presentation, classical dengue fever (fever, headache, myalgias, joint pains, nausea, vomiting, and skin rash), and life-threatening hemorrhagic diseases, specifically dengue hemorrhagic fever/dengue shock syndrome (DHF/DSS) in severe cases.[27]
Despite being an old disease, current immunization and therapeutic options available for prevention and control of DENV infection are severely limited. Management of dengue-associated diseases consists of preventing the viral infection by mosquito control and relieving symptoms in the infected individuals. Development of prophylactic/therapeutic treatment against DENV infection using natural products may help address some of these current limitations. The flavone baicalein, for example, exerts potent activity against DENV adsorption to the host and post-entry viral replication.[28] In addition, several natural products such as quercetin and narasin, as well as marine seaweed extracts have been observed to possess significant anti-DENV properties.[29,30,31] Recently, we have reported chebulagic acid and punicalagin, two hydrolysable tannins isolated from Terminalia chebula (訶子 Hē Zǐ), as broad-spectrum antiviral agents against several viruses including DENV.[32] Specifically, chebulagic acid and punicalagin can directly inactivate free DENV particles and interfere with the attachment and fusion events during early viral entry. Identification of these natural viral inhibitors could help the development of therapeutics against DENV infection and reduce the risks of DHF/DSS.
ENTEROVIRUS 71
EV71 is a member of the Picornaviridae family, possessing a positive-sense ssRNA genome and is non-enveloped. EV71 is ordinarily transmitted by fecal–oral route, but transmission by respiratory droplet is also possible. It is one of the major causes of HFMD in children, is sometimes associated with severe neurological diseases, and can be fatal.[20] The transmission rate in children under 5 years of age is typically high in endemic areas and several outbreaks have occurred over the past few decades.[33,34,35]
Medication and preventive vaccines against EV71 are presently in development and palliative care is used to ameliorate the symptoms. Nevertheless, several natural products and herbal medicines have been shown to possess inhibitory activity against EV71 infection. Extracts and pure constituents of O. basilicum effectively block EV71 infection and replication.[21] In addition, raoulic acid, which has previously been mentioned as an inhibitor to CVB, also suppresses EV71.[22] Gallic acid from Woodfordia fruticosa flowers (蝦子花 Xiā Zǐ Huā) has also been observed to exert anti-EV71 activity.[36] Finally, epigallocatechin gallate from green tea has been identified to interfere with EV71 replication via modulation of the cellular redox environment.[37] Without efficient medical treatment for the prevention and control of infection by EV71, further studies in identifying novel antivirals against the enterovirus are encouraged.
HEPATITIS B VIRUS
HBV is the prototype virus of the Hepadnaviridae family. It is an enveloped virus possessing a relaxed circular, partially double-stranded DNA (dsDNA) genome.[38] HBV causes hepatitis B and the infection is transmitted by exposure to blood or body fluids containing the virus. Although spontaneous recovery is common following acute hepatitis B, medication is recommended for chronic infection because of the risk of developing cirrhosis and hepatocellular carcinoma (HCC). The development of HBV vaccine and nationwide hepatitis B vaccination program in endemic countries such as Taiwan have helped control HBV infection as well as reduce the incidence of childhood HCC.[39]
Despite the existence of preventive vaccines, the present HBV-infected population, including those in areas where vaccination program is unavailable, remains at risk for end-stage liver diseases. Therapeutic treatment against HBV includes nucleotide/nucleoside analogs such as lamivudine, adefovir, tenofovir, telbivudine, and entecavir, as well as the immune modulator pegylated interferon-α (Peg-IFN-α).[40] However, eradication of HBV from the host proves difficult once persistent infection is established, and the situation is further aggravated by risks of selecting drug-resistant viral mutants, treatment failure in non-responders, and potential future viral reactivation. Therefore, anti-HBV drug discovery is still a matter of importance for supporting current therapy and hepatitis B management program to treat some current 300-400 million carriers globally.[41]
Extensive studies have been conducted over the past few decades to identify anti-HBV agents from natural products and herbal medicines, and some have been thoroughly covered elsewhere.[42,43,44,45] As examples, isochlorogenic acid A from Laggera alata, amide alkaloid from Piper longum (假蒟 Jiǎ Jù), and dehydrocheilanthifoline from Corydalis saxicola have been reported for their anti-HBV activities.[46,47,48] We have also previously demonstrated the antiviral effects of the herbal prescription Xiao-Chai-Hu-Tang (小柴胡湯 Xiǎo Chái Hú Tang), the saikosaponins from Bupleurum species (柴胡 Chái Hú), and the ethanol extract from Polygonum cuspidatum sieb. et zucc (虎杖 Hǔ Zhàng) against HBV in vitro.[49,50,51] Another example is curcumin, which has been shown to inhibit HBV gene replication and expression by down-regulating the peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α), the coactivator of HBV transcription.[52] As novel anti-HBV inhibitory agents are being discovered, future studies should also evaluate potential combination treatments with standard nucleotide/nucleoside analogs or IFN-α-based therapies for the management of hepatitis B.
HEPATITIS C VIRUS
HCV is an enveloped flavivirus possessing a positive-sense ssRNA. Transmission of HCV mainly occurs by blood-to-blood contact, such as through intravenous injections, blood transfusion, and various exposures to blood contaminants (tattooing, piercing, razor and toothbrush sharing, etc.). Due to the highly mutable nature of HCV, a preventive vaccine is not yet available. About 70% of infections become persistent, resulting in an estimated 300 million carriers worldwide of which 1-3% may progress to end-stage liver diseases including cirrhosis and HCC.[53] The present standard of care consists of parenteral Peg-IFN-α plus oral ribavirin, and will soon incorporate the new protease inhibitors boceprevir and telaprevir for combination therapy. However, several obstacles remain in the current method of therapeutic treatment against HCV, including limited efficacy for certain viral genotypes, inevitable selection of drug-resistant mutants, serious side-effects, high cost of medication, patient adherence issues, and challenges in the difficult-to-treat populations such as non-responders and liver transplant patients.[54] Thus, continuous development of anti-HCV agents is necessary to meet these shortcomings.
Various natural products have been explored for their antiviral effects against HCV infection. Silybum marianum (also known as “Milk Thistle” or “silymarin”) and its flavonolignans have been demonstrated to exert anti-HCV activity in vitro,[55,56] and several clinical evaluations have shown promising effects in reducing the viral load.[57,58,59] Curcumin has been identified as a potential inhibitor of HCV replication, potentially by suppressing sterol regulatory element binding protein-1 (SREBP-1)-Akt pathway,[60] and more recently its negative effect on HCV entry has been demonstrated.[61] Other natural compounds have been observed to prevent HCV entry as well, and these include epigallocatechin-3-gallate, griffithsin, ladanein, and tellimagrandin I.[62,63,64,65,66,67] Similarly, we have recently identified the hydrolyzable tannins chebulagic acid and punicalagin as potent inhibitors of HCV entry.[32] The two tannins inactivate free virus particles, prevent viral attachment and penetration into the host cell, and disrupt post-infection cell-to-cell transmission of HCV. Since immunization against HCV is at present unavailable, the discovery of novel anti-HCV entry inhibitors could help develop preventive therapies/measures against hepatitis C.
HERPES SIMPLEX VIRUS
Herpes simplex virus type 1 and type 2 (HSV-1 and HSV-2) are enveloped dsDNA viruses belonging to the Herpesviridae family. HSV infection usually causes mucocutaneous lesions that occur in oral/perioral (typically by HSV-1) and genital (commonly by HSV-2) areas, as well as on other body sites. HSV causes lifelong infection by establishing itself in sensory neurons and can be reactivated by various stimuli including sunlight, fever, immunosuppression, menstruation, or stress.[68] Transmission of HSV results from contact with infected lesions and can occur via vertical transmission from infected mother to newborn. Although the disease is usually self-limited and can be treated with antivirals, severe complications can occur, particularly in neonates and immunosuppressed individuals, leading to risk of blindness with keratoconjunctivitis, and the potentially fatal meningitis and encephalitis.[69,70]
No vaccine is available against HSV and there are currently no drugs that can eradicate latent HSV infection. Although primary and recurrent infections can be controlled by nucleoside analogs such as acyclovir, penciclovir, and their prodrugs, the development of drug-resistant virus is becoming a serious problem, especially in immunocompromised patients.[71] Thus, identifying novel anti-HSV agents that act with different mechanisms is crucial for clinical management of HSV. We have previously reported several natural products and herbal medicines that inhibit HSV infection and replication. For instance, ent-epiafzelechin-(4α→8)-epiafzelechin, extracted from Cassia javanica, inhibits HSV-2 replication; the herbal prescriptions Long-Dan-Xie-Gan-Tan (龍膽瀉肝湯 Lóng Dǎn Xiè Gān Tāng) and Yin-Chen-Hao-Tang (茵陳蒿湯 Yīn Chén Hāo Tang) both possess broad efficiency in diminishing HSV-1 and HSV-2 infectivity; hippomanin A, geraniin, 1,3,4,6-tetra-O-galloyl-beta-d-glucose, and excoecarianin isolated from Phyllanthus urinaria (葉下珠 Yè Xià Zhū) can potently impede HSV infection.[72,73,74,75,76,77] In addition, we have also identified the hydrolyzable tannins chebulagic acid and punicalagin as cell surface glycosaminoglycan (GAG) competitors that can inhibit HSV-1 entry and cell-to-cell spread.[78] HSV-1 and also a multitude of viruses employ GAGs as initial attachment receptors during infection of their host cell. Both chebulagic acid and punicalagin are observed to target HSV-1 glycoproteins that interact with GAGs and, in turn, prevent their association with cell surface GAGs as well as subsequent binding receptors.[78] This inhibitory effect is shown (1) against cell-free virus, (2) during the viral attachment and fusion stages, and (3) in the intercellular junction spread of HSV-1, which is mediated by its glycoproteins. Thus, both tannins are demonstrated to be efficient entry inhibitors to HSV-1 and similar effects have been observed on another herpesvirus, the human cytomegalovirus, as well as on several other viruses known to engage GAGs for entry.[32]
Besides the natural products and traditional decoctions mentioned above, a plethora of other natural anti-HSV agents have also been identified.[79,80] Meliacine derived from Melia azedarach is observed to stimulate tumor necrosis factor-alpha (TNF-α) and IFN-g production, and reduce HSV-2 shedding with improvement of virus-induced pathogenesis in a mouse vaginal model of herpetic infection.[81] Houttuynoids A-E are flavonoids isolated from Houttuynia cordata (蕺菜 Jí Cài), which have been found to exhibit potent anti–HSV-1 activity.[82] Similarly, the aqueous extract from Rhododendron ferrugineum L., blackberry extract, and proanthocyanidin-enriched extract from Myrothamnus flabellifolia Welw. have been reported to inhibit HSV-1 infection.[83,84,85] Another example is glucoevatromonoside, a cardenolide from Digitalis lanata, which has been suggested to alter cellular electrochemical gradient and block HSV-1 and HSV-2 propagation in cells.[86] In addition, natural products from the marine environment represent a whole biodiversity in which many algae and sponges have been observed to contain active metabolites with anti-HSV activity.[87,88] The abundance of natural anti-HSV agents discovered should provide novel pharmacological activities against the virus, which could be further explored for potential application in the management of HSV infections.
HUMAN IMMUNODEFICIENCY VIRUS
HIV is a lentivirus of the Retroviridae family. The enveloped virus is characterized by targeting of the immune cells for infection, reverse transcription of its ssRNA genome, and integration into the host chromosomal DNA.[89] Transmission of HIV occurs via exchange of virus-containing blood and body fluids, such as through sexual contact, sharing of contaminated needles/sharp instruments, childbirth, as well as breastfeeding.[90] HIV is the causative agent of acquired immunodeficiency syndrome (AIDS), which is a progressive failure of the immune system due to CD4+ T-lymphocyte depletion that leads to manifestation of life-threatening opportunistic infections and malignancies.[91] To date, AIDS has resulted in more than 25 million deaths and there are currently about 34 million HIV-infected individuals with an estimated 2-3 million newly diagnosed cases annually.[13]
Despite nearly 30 years of research since its discovery, at present there is no effective preventive vaccine or cure for HIV infection. The high antigenic diversity and multiple mechanisms that the virus employs to subvert recognition by the human immune system have made prophylactic/therapeutic management of HIV infection difficult.[92] Nevertheless, the development of the highly active antiretroviral therapy (HAART), which consists of a cocktail of nucleoside analog/non-nucleoside reverse-transcriptase inhibitors, has dramatically decreased the morbidity and mortality associated with HIV/AIDS.[93] However, there is still a pressing need for alternative treatment strategies against HIV infection due to drug resistance problems, treatment-associated toxicity, patient adherence, and restricted accessibility in resource-poor areas.[94,95,96]
An exhaustive list of natural products has been evaluated for anti-retroviral/anti-HIV activity and recently reviewed.[97,98] Moreover, many marine natural products with anti-HIV activities have also been identified in search of novel therapeutics against the AIDS virus.[99,100,101] To briefly mention some examples, the crude extracts of Artemisia annua (黃花蒿 Huáng Huā Hāo) and Artemisia afra have recently been reported as potential anti-HIV medicines.[102] The Calophyllum species is known to contain several coumarins that are observed to exert inhibitory effect against HIV.[103,104] More recently, a tricyclic coumarin derived from the stem bark of Calophyllum brasiliense has been shown to inhibit HIV replication in in vitro models by suppressing nuclear factor-kappa B (NF-κB) activation.[105] Another novel anti-HIV agent is the small peptide melittin, which is the active component of bee venom. The nanoformulated melittin is demonstrated to possess robust efficiency in capturing and inactivating HIV particles by disrupting the viral lipid envelope.[106] Based on the discoveries made so far, the recent progress in identifying natural antivirals against HIV should yield potential novel therapeutics that could play an important role in overcoming the current urgency in anti-HIV/AIDS therapies.
INFLUENZA VIRUS
The influenza A, B, and C viruses (IFA, IFB, and IFC) are enveloped, negative-sense ssRNA viruses classified in the Orthomyxoviridae family. These viruses cause respiratory infection yielding symptoms that include fever, headache, sore throat, sneezing, and muscle and joint pains, and can develop into more severe and potentially fatal conditions such as pneumonia.[107,108] IFA (most epidemic) has a wide host range including birds and humans as well as other mammals, whereas IFB seems to naturally infect humans and IFC (less frequently encountered) can be isolated from humans and swine.[109] Influenza virus infection has produced considerable morbidity in humans. An estimated 250,000-500,000 deaths occur annually due to seasonal epidemics, and in major pandemics, this number has been observed to rise to some 20-40 million deaths, as in the case of the 1918 H1N1 Spanish Flu.[13]
Despite the availability of vaccines based on predicted circulating strains, influenza viruses are known to continuously evolve their hemagglutinin (HA) and neuraminidase (NA) envelope proteins.[110,111] This variation renders any preexisting circulating antibody from earlier exposure or immunization ineffective at neutralizing the virus, hence making the host vulnerable to infection. Furthermore, potential risks of cross-species transmission and host adaptation of influenza viruses between animals and humans resulting in highly pathogenic strains have also raised concerns.[112] Another issue is the widespread development of drug resistance, which has been observed with the first generation of anti-influenza medications, specifically the M2 ion channel blockers amantadine and rimantadine.[113] Resistant strains against the currently approved neuraminidase inhibitors (which prevent the release of mature influenza viruses) including oseltamivir and zanamivir have also already appeared.[114] Due to the drug resistance problems, the rapid evolution of influenza viruses, and the occurrence of several recent outbreaks (e.g., H5N1, H1N1, H7N9),[13] more sophisticated antiviral strategies are urgently needed to prevent and control potential pandemics with emerging influenza strains.
Several natural products have been examined for their effects against influenza. Standardized elderberry (接骨木 Jiē Gǔ Mù; Sambucus nigra) liquid extract exerts in vitro antiviral effects against IFA, IFB, as well as respiratory bacterial pathogens.[115] A licensed commercial extract from Pelargonium sidoides roots inhibits the entry of IFA, impairs viral hemagglutination as well as neuraminidase activity, and improves the symptoms of influenza-infected mice.[116] The aqueous extract from dandelion (蒲公英 Pú Gōng Yīng; Taraxacum officinale) impedes IFA infection and decreases its polymerase activity as well as the nucleoprotein (NP) RNA level.[117] Spirooliganone B from the roots of Illicium oligandrum exhibits potent anti-IFA activities.[118] A multitude of secondary plant metabolites have also been identified as potential influenza NA inhibitors,[119] and more recent ones include chalcones from Glycyrrhiza inflata,[120] xanthones from Polygala karensium,[121] and homoisoflavonoids from Caesalpinia sappan (蘇木Sū Mù).[122] Further exploration of these natural anti-influenza agents for clinical application will help broaden the drug portfolio for prophylactic/therapeutic treatment of potential flu epidemics or pandemics.
MEASLES VIRUS
MV is an enveloped, negative-sense ssRNA virus of the Morbillivirus genus in the Paramyxoviridae family. MV causes measles, an acute infection of the respiratory system characterized by fever, conjunctivitis, coughing, runny nose, nausea, and a generalized macular red rash over the body. Complications can occur leading to pneumonia and encephalitis, which can be potentially fatal.[123] Although highly contagious through contact of respiratory droplets or airborne aerosols, immunization against measles given as a three-part MMR vaccine (measles, mumps, and rubella) has made MV infection relatively uncommon in developed countries. As recovery usually follows uncomplicated MV infection, there are currently no specific antiviral treatments for measles. Despite the existence of a successful vaccine against MV, the virus remains a major killer of children in developing countries.[124,125] Another serious problem is the re-emergence of measles in vaccinated populations and in non-immunized adults, as highlighted by outbreaks in recent years.[6,126,127] These issues emphasize MV's medical importance and the need to develop suitable drug therapies.
Efforts have been made at identifying natural products that inhibit MV and include a number of East and Southeast Asian traditional medicines,[128] the herbal decoction Sheng-Ma-Ge-Gen-Tang (升麻葛根湯 Shēng Má Gé Gēn Tang),[129] the Cherokee remedy spicebush,[130] plant biflavonoids isolated from Rhus succedanea (野漆 Yě Qī) and Garcinia multiflora,[131] calcium spirulan from the blue-green alga Spirulina platensis,[132] Crotalus durissus terrificus snake venom,[133] and several Rwandan and Ugandan medicinal plant extracts,[134,135] among others previously reviewed.[136] In addition, several traditional dietary herb additives of the Maasai, including Olinia rochetiana (Olkirenyi) and Warburgia ugandensis (Osokonoi), have been reported to inhibit MV infection in vitro.[137] Another example is the plant extracts of Cajanus cajan which have been recently suggested to possess anti-MV activity, although the bioactive constituents remain elusive.[138] The two tannins chebulagic acid and punicalagin also show robust effects against MV infection, particularly by inactivating the virus particles, interrupting the binding and fusion phases during viral entry, and preventing post-infection virus spread.[32] Chebulagic acid and punicalagin could, therefore, serve as potential entry inhibitors to MV.
RESPIRATORY SYNCYTIAL VIRUS
RSV is an enveloped negative-strand ssRNA virus of the Paramyxoviridae family. It is a ubiquitous pathogen and the leading cause of viral lower respiratory tract infection in infants and children.[139] Virtually all children become infected with RSV before the age of 2 years.[140] RSV infection typically results in mild symptoms in healthy adults, but can lead to bronchiolitis or pneumonia in infants and immunocompromised individuals. Moreover, infant RSV infection poses a potential risk for childhood asthma.[141,142] Although RSV causes the most severe disease in young infants, it continues to plague humans throughout the course of a lifetime. Immunity to RSV is generally not sufficient to provide protection and, consequently, humans are prone to repeated reinfections[143,144,145] which can be life-threatening in the elderly or immunocompromised.[146,147]
Currently, immunization against RSV is unavailable, and the few therapies that exist for the treatment of RSV infections such as palivizumab (monoclonal antibody against RSV fusion protein) and ribavirin (nucleoside analogue) are only moderately effective or limited in efficacy. Thus, there is a need to develop novel antivirals for the management of RSV infections. Several plant-derived natural products have been demonstrated to exhibit anti-RSV activity. Uncinoside A and B, the two chromone glycosides isolated from Selaginella uncinata, potently inhibit RSV infection.[148] Three biflavonoids, namely genkwanol B, genkwanol C, and stelleranol, extracted from Radix Wikstroemiae, have been observed to display antiviral activity against RSV.[149] Several flavone 6-C-monoglycosides from the leaves of Lophatherum gracile (淡竹葉 Dàn Zhú Yè) have been shown to reduce RSV infection in cytopathic effect-reduction assay.[150] We have previously also identified several anti-RSV natural medicines, including the herbal prescription Sheng-Ma-Ge-Gen-Tang (升麻葛根湯 Shēng Má Gé Gēn Tang) which is used for treating respiratory diseases, its major component herb Cimicifuga foetida L. (升麻 Shēng Má), as well as the plant-associated bioactive compound cimicifugin.[151,152,153] In addition, the broad-spectrum antiviral activity that we have demonstrated for the hydrolyzable tannins chebulagic acid and punicalagin also includes antiviral effects against RSV infection.[32] Specifically, the two tannins can inactivate RSV particles and also block viral entry-related events, including binding and fusion. Interestingly, both chebulagic acid and punicalagin are, however, ineffective against RSV post-infection spread, but could abrogate the same event in MV, which is another paramyxovirus.[32] Besides targeting the viral infection, some natural products may help improve RSV-induced respiratory tract symptoms, including airway inflammation. Resveratrol is one such example, which has been observed to down-regulate IFN-γ levels and prevent airway inflammation/hyperresponsiveness during RSV infection in mice, suggesting its applicability in reducing RSV-induced airway symptoms.[154]
PROSPECTS AND CONCLUSION
As many viruses remain without preventive vaccines and effective antiviral treatments, eradicating these viral diseases appears difficult. Nonetheless, natural products serve as an excellent source of biodiversity for discovering novel antivirals, revealing new structure–activity relationships, and developing effective protective/therapeutic strategies against viral infections. Many natural products and herbal ingredients are observed to possess robust antiviral activity and their discoveries can further help develop derivatives and therapeutic leads (e.g., glycyrrhetinic acid derivatives as novel anti-HBV agents, acetoxime derivative from the Mediterranean mollusk Hexaplex trunculus as inhibitor against HSV-1, and caffeic acid derivatives as a new type of influenza NA antagonist).[155,156,157] Our discovery of chebulagic acid and punicalagin being capable of inhibiting entry of several viruses due to their GAG-competing properties could help develop broad-spectrum antivirals for prevention and control of these viral pathogens. As many studies in this domain are only preliminary, further exploration in characterizing the bioactive ingredients, defining the underlying mechanisms, as well as assessing the efficacy and potential application in vivo is encouraged in order to help develop effective antiviral treatments. Furthermore, additional studies should also examine the possibility of combination therapies with other natural agents or with standard therapeutics, as a multi-target therapy may help reduce the risk of generating drug-resistant viruses. We believe that natural products will continue to play an important role and contribute to antiviral drug development.
ACKNOWLEDGMENTS
The authors would like to apologize to any investigators whose studies were not included in this review due to space limitation. LTL was supported by a research grant from Taipei Medical University (TMU101-AE1-B12). CCL was supported by funding from the Committee on Chinese Medicine and Pharmacy, Department of Health, Executive Yuan of Taiwan (CCMP 96-RD-026 and CCMP 97-RD-112).
REFERENCES
- 1.Ball MJ, Lukiw WJ, Kammerman EM, Hill JM. Intracerebral propagation of Alzheimer's disease: Strengthening evidence of a herpes simplex virus etiology. Alzheimers Dement. 2013;9:169–75. doi: 10.1016/j.jalz.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hober D, Sane F, Jaidane H, Riedweg K, Goffard A, Desailloud R. Immunology in the clinic review series; focus on type 1 diabetes and viruses: Role of antibodies enhancing the infection with Coxsackievirus-B in the pathogenesis of type 1 diabetes. Clin Exp Immunol. 2012;168:47–51. doi: 10.1111/j.1365-2249.2011.04559.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: A meta-analysis of observational studies. Ann Intern Med. 2013;158:329–37. doi: 10.7326/0003-4819-158-5-201303050-00005. [DOI] [PubMed] [Google Scholar]
- 4.Christou L. The global burden of bacterial and viral zoonotic infections. Clin Microbiol Infect. 2011;17:326–30. doi: 10.1111/j.1469-0691.2010.03441.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cascio A, Bosilkovski M, Rodriguez-Morales AJ, Pappas G. The socio-ecology of zoonotic infections. Clin Microbiol Infect. 2011;17:336–42. doi: 10.1111/j.1469-0691.2010.03451.x. [DOI] [PubMed] [Google Scholar]
- 6.Grais RF, Strebel P, Mala P, Watson J, Nandy R, Gayer M. Measles vaccination in humanitarian emergencies: A review of recent practice. Confl Health. 2011;5:21. doi: 10.1186/1752-1505-5-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sheu TG, Deyde VM, Okomo-Adhiambo M, Garten RJ, Xu X, Bright RA, et al. Surveillance for neuraminidase inhibitor resistance among human influenza A and B viruses circulating worldwide from 2004 to 2008. Antimicrob Agents Chemother. 2008;52:3284–92. doi: 10.1128/AAC.00555-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Geretti AM, Armenia D, Ceccherini-Silberstein F. Emerging patterns and implications of HIV-1 integrase inhibitor resistance. Curr Opin Infect Dis. 2012;25:677–86. doi: 10.1097/QCO.0b013e32835a1de7. [DOI] [PubMed] [Google Scholar]
- 9.Locarnini SA, Yuen L. Molecular genesis of drug-resistant and vaccine-escape HBV mutants. Antivir Ther. 2010;15:451–61. doi: 10.3851/IMP1499. [DOI] [PubMed] [Google Scholar]
- 10.Wyles DL. Antiviral resistance and the future landscape of hepatitis C virus infection therapy. J Infect Dis. 2013;207(Suppl 1):S33–9. doi: 10.1093/infdis/jis761. [DOI] [PubMed] [Google Scholar]
- 11.van der Hoek L. Human coronaviruses: What do they cause? Antivir Ther. 2007;12:651–8. [PubMed] [Google Scholar]
- 12.Geller C, Varbanov M, Duval RE. Human coronaviruses: Insights into environmental resistance and its influence on the development of new antiseptic strategies. Viruses. 2012;4:3044–68. doi: 10.3390/v4113044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. [Last accessed on 2013 Sep 18]. Available from: http://www.who.int .
- 14.Cheng PW, Ng LT, Chiang LC, Lin CC. Antiviral effects of saikosaponins on human coronavirus 229E in vitro. Clin Exp Pharmacol Physiol. 2006;33:612–6. doi: 10.1111/j.1440-1681.2006.04415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li SY, Chen C, Zhang HQ, Guo HY, Wang H, Wang L, et al. Identification of natural compounds with antiviral activities against SARS-associated coronavirus. Antivir Res. 2005;67:18–23. doi: 10.1016/j.antiviral.2005.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin CW, Tsai FJ, Tsai CH, Lai CC, Wan L, Ho TY, et al. Anti-SARS coronavirus 3C-like protease effects of Isatis indigotica root and plant-derived phenolic compounds. Antivir Res. 2005;68:36–42. doi: 10.1016/j.antiviral.2005.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ryu YB, Jeong HJ, Kim JH, Kim YM, Park JY, Kim D, et al. Biflavonoids from Torreya nucifera displaying SARS-CoV 3CL (pro) inhibition. Bioorg Med Chem. 2010;18:7940–7. doi: 10.1016/j.bmc.2010.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yu MS, Lee J, Lee JM, Kim Y, Chin YW, Jee JG, et al. Identification of myricetin and scutellarein as novel chemical inhibitors of the SARS coronavirus helicase, nsP13. Bioorg Med Chem Lett. 2012;22:4049–54. doi: 10.1016/j.bmcl.2012.04.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lau KM, Lee KM, Koon CM, Cheung CS, Lau CP, Ho HM, et al. Immunomodulatory and anti-SARS activities of Houttuynia cordata. J Ethnopharmacol. 2008;118:79–85. doi: 10.1016/j.jep.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tapparel C, Siegrist F, Petty TJ, Kaiser L. Picornavirus and enterovirus diversity with associated human diseases. Infect Genet Evol. 2013;14:282–93. doi: 10.1016/j.meegid.2012.10.016. [DOI] [PubMed] [Google Scholar]
- 21.Chiang LC, Ng LT, Cheng PW, Chiang W, Lin CC. Antiviral activities of extracts and selected pure constituents of Ocimum basilicum. Clin Exp Pharmacol Physiol. 2005;32:811–6. doi: 10.1111/j.1440-1681.2005.04270.x. [DOI] [PubMed] [Google Scholar]
- 22.Choi HJ, Lim CH, Song JH, Baek SH, Kwon DH. Antiviral activity of raoulic acid from Raoulia australis against Picornaviruses. Phytomedicine. 2009;16:35–9. doi: 10.1016/j.phymed.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 23.Cheng PW, Ng LT, Lin CC. Xiao chai hu tang inhibits CVB1 virus infection of CCFS-1 cells through the induction of Type I interferon expression. Int Immunopharmacol. 2006;6:1003–12. doi: 10.1016/j.intimp.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 24.Cheng PW, Chiang LC, Yen MH, Lin CC. Bupleurum kaoi inhibits Coxsackie B virus type 1 infection of CCFS-1 cells by induction of type I interferons expression. Food Chem Toxicol. 2007;45:24–31. doi: 10.1016/j.fct.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 25.Black WCt, Bennett KE, Gorrochotegui-Escalante N, Barillas-Mury CV, Fernandez-Salas I, de Lourdes Munoz M, et al. Flavivirus susceptibility in Aedes aegypti. Arch Med Res. 2002;33:379–88. doi: 10.1016/s0188-4409(02)00373-9. [DOI] [PubMed] [Google Scholar]
- 26.Back AT, Lundkvist A. Dengue viruses-an overview. Infect Ecol Epidemiol. 2013;3:19839. doi: 10.3402/iee.v3i0.19839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sam SS, Omar SF, Teoh BT, Abd-Jamil J, AbuBakar S. Review of Dengue hemorrhagic fever fatal cases seen among adults: A retrospective study. PLoS Negl Trop Dis. 2013;7:e2194. doi: 10.1371/journal.pntd.0002194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zandi K, Teoh BT, Sam SS, Wong PF, Mustafa MR, Abubakar S. Novel antiviral activity of baicalein against dengue virus. BMC Complement Altern Med. 2012;12:214. doi: 10.1186/1472-6882-12-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zandi K, Teoh BT, Sam SS, Wong PF, Mustafa MR, Abubakar S. Antiviral activity of four types of bioflavonoid against dengue virus type-2. Virol J. 2011;8:560. doi: 10.1186/1743-422X-8-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Low JS, Wu KX, Chen KC, Ng MM, Chu JJ. Narasin, a novel antiviral compound that blocks dengue virus protein expression. Antivir Ther. 2011;16:1203–18. doi: 10.3851/IMP1884. [DOI] [PubMed] [Google Scholar]
- 31.Koishi AC, Zanello PR, Bianco EM, Bordignon J, Nunes Duarte dos Santos C. Screening of Dengue virus antiviral activity of marine seaweeds by an in situ enzyme-linked immunosorbent assay. PLoS One. 2012;7:e51089. doi: 10.1371/journal.pone.0051089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lin LT, Chen TY, Lin SC, Chung CY, Lin TC, Wang GH, et al. Broad-spectrum antiviral activity of chebulagic acid and punicalagin against viruses that use glycosaminoglycans for entry. BMC Microbiol. 2013;13:187. doi: 10.1186/1471-2180-13-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chang LY, Tsao KC, Hsia SH, Shih SR, Huang CG, Chan WK, et al. Transmission and clinical features of enterovirus 71 infections in household contacts in Taiwan. JAMA. 2004;291:222–7. doi: 10.1001/jama.291.2.222. [DOI] [PubMed] [Google Scholar]
- 34.Wang SM, Ho TS, Lin HC, Lei HY, Wang JR, Liu CC. Reemerging of enterovirus 71 in Taiwan: The age impact on disease severity. Eur J Clin Microbiol Infect Dis. 2012;31:1219–24. doi: 10.1007/s10096-011-1432-6. [DOI] [PubMed] [Google Scholar]
- 35.Huang SW, Kiang D, Smith DJ, Wang JR. Evolution of re-emergent virus and its impact on enterovirus 71 epidemics. Exp Biol Med. 2011;236:899–908. doi: 10.1258/ebm.2010.010233. [DOI] [PubMed] [Google Scholar]
- 36.Choi HJ, Song JH, Park KS, Baek SH. In vitro anti-enterovirus 71 activity of gallic acid from Woodfordia fruticosa flowers. Lett Appl Microbiol. 2010;50:438–40. doi: 10.1111/j.1472-765X.2010.02805.x. [DOI] [PubMed] [Google Scholar]
- 37.Ho HY, Cheng ML, Weng SF, Leu YL, Chiu DT. Antiviral effect of epigallocatechin gallate on enterovirus 71. J Agric Food Chem. 2009;57:6140–7. doi: 10.1021/jf901128u. [DOI] [PubMed] [Google Scholar]
- 38.Liang TJ. Hepatitis B: The virus and disease. Hepatology. 2009;49(5 Suppl):S13–21. doi: 10.1002/hep.22881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ni YH, Chen DS. Hepatitis B vaccination in children: The Taiwan experience. Pathologiebiologie. 2010;58:296–300. doi: 10.1016/j.patbio.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 40.Kwon H, Lok AS. Hepatitis B therapy. Nat Rev Gastroenterol Hepatol. 2011;8:275–84. doi: 10.1038/nrgastro.2011.33. [DOI] [PubMed] [Google Scholar]
- 41.Franco E, Bagnato B, Marino MG, Meleleo C, Serino L, Zaratti L. Hepatitis B: Epidemiology and prevention in developing countries. World J Hepatol. 2012;4:74–80. doi: 10.4254/wjh.v4.i3.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang L, Wang G, Hou W, Li P, Dulin A, Bonkovsky HL. Contemporary clinical research of traditional Chinese medicines for chronic hepatitis B in China: An analytical review. Hepatology. 2010;51:690–8. doi: 10.1002/hep.23384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhan P, Jiang X, Liu X. Naturally occurring and synthetic bioactive molecules as novel non-nucleoside HBV inhibitors. Mini Rev Med Chem. 2010;10:162–71. doi: 10.2174/138955710791185118. [DOI] [PubMed] [Google Scholar]
- 44.Cui X, Wang Y, Kokudo N, Fang D, Tang W. Traditional Chinese medicine and related active compounds against hepatitis B virus infection. Biosci Trends. 2010;4:39–47. [PubMed] [Google Scholar]
- 45.Qiu LP, Chen KP. Anti-HBV agents derived from botanical origin. Fitoterapia. 2013;84:140–57. doi: 10.1016/j.fitote.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 46.Hao BJ, Wu YH, Wang JG, Hu SQ, Keil DJ, Hu HJ, et al. Hepatoprotective and antiviral properties of isochlorogenic acid A from Laggera alata against hepatitis B virus infection. J Ethnopharmacol. 2012;144:190–4. doi: 10.1016/j.jep.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 47.Jiang ZY, Liu WF, Zhang XM, Luo J, Ma YB, Chen JJ. Anti-HBV active constituents from Piper longum. Bioorg Med Chem Lett. 2013;23:2123–7. doi: 10.1016/j.bmcl.2013.01.118. [DOI] [PubMed] [Google Scholar]
- 48.Zeng FL, Xiang YF, Liang ZR, Wang X, Huang DE, Zhu SN, et al. Anti-hepatitis B virus effects of dehydrocheilanthifoline from Corydalis saxicola. Am J Chin Med. 2013;41:119–30. doi: 10.1142/S0192415X13500092. [DOI] [PubMed] [Google Scholar]
- 49.Chang JS, Wang KC, Liu HW, Chen MC, Chiang LC, Lin CC. Sho-saiko-to (Xiao-Chai-Hu-Tang) and crude saikosaponins inhibit hepatitis B virus in a stable HBV-producing cell line. Am J Chin Med. 2007;35:341–51. doi: 10.1142/S0192415X07004862. [DOI] [PubMed] [Google Scholar]
- 50.Chiang LC, Ng LT, Liu LT, Shieh DE, Lin CC. Cytotoxicity and anti-hepatitis B virus activities of saikosaponins from Bupleurum species. Planta Med. 2003;69:705–9. doi: 10.1055/s-2003-42797. [DOI] [PubMed] [Google Scholar]
- 51.Chang JS, Liu HW, Wang KC, Chen MC, Chiang LC, Hua YC, et al. Ethanol extract of Polygonum cuspidatum inhibits hepatitis B virus in a stable HBV-producing cell line. Antiviral Res. 2005;66:29–34. doi: 10.1016/j.antiviral.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 52.Rechtman MM, Har-Noy O, Bar-Yishay I, Fishman S, Adamovich Y, Shaul Y, et al. Curcumin inhibits hepatitis B virus via down-regulation of the metabolic coactivator PGC-1alpha. FEBS Lett. 2010;584:2485–90. doi: 10.1016/j.febslet.2010.04.067. [DOI] [PubMed] [Google Scholar]
- 53.El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology. 2012;142:1264–73.e1. doi: 10.1053/j.gastro.2011.12.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Welsch C, Jesudian A, Zeuzem S, Jacobson I. New direct-acting antiviral agents for the treatment of hepatitis C virus infection and perspectives. Gut. 2012;61(Suppl 1):i36–46. doi: 10.1136/gutjnl-2012-302144. [DOI] [PubMed] [Google Scholar]
- 55.Polyak SJ, Morishima C, Shuhart MC, Wang CC, Liu Y, Lee DY. Inhibition of T-cell inflammatory cytokines, hepatocyte NF-kappaB signaling, and HCV infection by standardized Silymarin. Gastroenterology. 2007;132:1925–36. doi: 10.1053/j.gastro.2007.02.038. [DOI] [PubMed] [Google Scholar]
- 56.Polyak SJ, Morishima C, Lohmann V, Pal S, Lee DY, Liu Y, et al. Identification of hepatoprotective flavonolignans from silymarin. Proc Natl Acad Sci U S A. 2010;107:5995–9. doi: 10.1073/pnas.0914009107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ferenci P, Scherzer TM, Kerschner H, Rutter K, Beinhardt S, Hofer H, et al. Silibinin is a potent antiviral agent in patients with chronic hepatitis C not responding to pegylated interferon/ribavirin therapy. Gastroenterology. 2008;135:1561–7. doi: 10.1053/j.gastro.2008.07.072. [DOI] [PubMed] [Google Scholar]
- 58.Neumann UP, Biermer M, Eurich D, Neuhaus P, Berg T. Successful prevention of hepatitis C virus (HCV) liver graft reinfection by silibinin mono-therapy. J Hepatol. 2010;52:951–2. doi: 10.1016/j.jhep.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 59.Marino Z, Crespo G, D’Amato M, Brambilla N, Giacovelli G, Rovati L, et al. Intravenous silibinin monotherapy shows significant antiviral activity in HCV-infected patients in the peri-transplantation period. J Hepatol. 2013;58:415–20. doi: 10.1016/j.jhep.2012.09.034. [DOI] [PubMed] [Google Scholar]
- 60.Kim K, Kim KH, Kim HY, Cho HK, Sakamoto N, Cheong J. Curcumin inhibits hepatitis C virus replication via suppressing the Akt-SREBP-1 pathway. FEBS Lett. 2010;584:707–12. doi: 10.1016/j.febslet.2009.12.019. [DOI] [PubMed] [Google Scholar]
- 61.Anggakusuma, Colpitts CC, Schang LM, Rachmawati H, Frentzen A, Pfaender S, et al. Turmeric curcumin inhibits entry of all hepatitis C virus genotypes into human liver cells. Gut. 2013 doi: 10.1136/gutjnl-2012-304299. [DOI] [PubMed] [Google Scholar]
- 62.Ciesek S, von Hahn T, Colpitts CC, Schang LM, Friesland M, Steinmann J, et al. The green tea polyphenol, epigallocatechin-3-gallate, inhibits hepatitis C virus entry. Hepatology. 2011;54:1947–55. doi: 10.1002/hep.24610. [DOI] [PubMed] [Google Scholar]
- 63.Calland N, Albecka A, Belouzard S, Wychowski C, Duverlie G, Descamps V, et al. (-)-Epigallocatechin-3-gallate is a new inhibitor of hepatitis C virus entry. Hepatology. 2012;55:720–9. doi: 10.1002/hep.24803. [DOI] [PubMed] [Google Scholar]
- 64.Meuleman P, Albecka A, Belouzard S, Vercauteren K, Verhoye L, Wychowski C, et al. Griffithsin has antiviral activity against hepatitis C virus. Antimicrob Agents Chemother. 2011;55:5159–67. doi: 10.1128/AAC.00633-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Takebe Y, Saucedo CJ, Lund G, Uenishi R, Hase S, Tsuchiura T, et al. Antiviral lectins from red and blue-green algae show potent in vitro and in vivo activity against hepatitis C virus. PLoS One. 2013;8:e64449. doi: 10.1371/journal.pone.0064449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Haid S, Novodomska A, Gentzsch J, Grethe C, Geuenich S, Bankwitz D, et al. A plant-derived flavonoid inhibits entry of all HCV genotypes into human hepatocytes. Gastroenterology. 2012;143:213–22.e5. doi: 10.1053/j.gastro.2012.03.036. [DOI] [PubMed] [Google Scholar]
- 67.Tamura S, Yang GM, Yasueda N, Matsuura Y, Komoda Y, Murakami N. Tellimagrandin I, HCV invasion inhibitor from Rosae Rugosae Flos. Bioorg Med Chem Lett. 2010;20:1598–600. doi: 10.1016/j.bmcl.2010.01.084. [DOI] [PubMed] [Google Scholar]
- 68.Fatahzadeh M, Schwartz RA. Human herpes simplex labialis. Clin Exp Dermatol. 2007;32:625–30. doi: 10.1111/j.1365-2230.2007.02473.x. [DOI] [PubMed] [Google Scholar]
- 69.Arduino PG, Porter SR. Herpes Simplex Virus Type 1 infection: Overview on relevant clinico-pathological features. J Oral Pathol Med. 2008;37:107–21. doi: 10.1111/j.1600-0714.2007.00586.x. [DOI] [PubMed] [Google Scholar]
- 70.Chentoufi AA, Benmohamed L. Mucosal herpes immunity and immunopathology to ocular and genital herpes simplex virus infections. Clin Dev Immunol 2012. 2012 doi: 10.1155/2012/149135. 149135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Morfin F, Thouvenot D. Herpes simplex virus resistance to antiviral drugs. J Clin Virol. 2003;26:29–37. doi: 10.1016/s1386-6532(02)00263-9. [DOI] [PubMed] [Google Scholar]
- 72.Cheng HY, Yang CM, Lin TC, Shieh DE, Lin CC. ent-Epiafzelechin- (4alpha-->8)-epiafzelechin extracted from Cassia javanica inhibits herpes simplex virus type 2 replication. J Med Microbiol. 2006;55:201–6. doi: 10.1099/jmm.0.46110-0. [DOI] [PubMed] [Google Scholar]
- 73.Cheng HY, Huang HH, Yang CM, Lin LT, Lin CC. The in vitro anti-herpes simplex virus type-1 and type-2 activity of Long Dan Xie Gan Tan, a prescription of traditional Chinese medicine. Chemotherapy. 2008;54:77–83. doi: 10.1159/000119705. [DOI] [PubMed] [Google Scholar]
- 74.Cheng HY, Lin LT, Huang HH, Yang CM, Lin CC. Yin Chen Hao Tang, a Chinese prescription, inhibits both herpes simplex virus type-1 and type-2 infections in vitro. Antivir Res. 2008;77:14–9. doi: 10.1016/j.antiviral.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 75.Yang CM, Cheng HY, Lin TC, Chiang LC, Lin CC. Hippomanin A from acetone extract of Phyllanthus urinaria inhibited HSV-2 but not HSV-1 infection in vitro. Phytother Res. 2007;21:1182–6. doi: 10.1002/ptr.2232. [DOI] [PubMed] [Google Scholar]
- 76.Yang CM, Cheng HY, Lin TC, Chiang LC, Lin CC. The in vitro activity of geraniin and 1,3,4,6-tetra-O-galloyl-beta-D-glucose isolated from Phyllanthus urinaria against herpes simplex virus type 1 and type 2 infection. J Ethnopharmacol. 2007;110:555–8. doi: 10.1016/j.jep.2006.09.039. [DOI] [PubMed] [Google Scholar]
- 77.Cheng HY, Yang CM, Lin TC, Lin LT, Chiang LC, Lin CC. Excoecarianin, Isolated from Phyllanthus urinaria Linnea, Inhibits Herpes Simplex Virus Type 2 Infection through Inactivation of Viral Particles. Evid Based Complement Alternat Med 2011. 2011 doi: 10.1093/ecam/nep157. 259103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lin LT, Chen TY, Chung CY, Noyce RS, Grindley TB, McCormick C, et al. Hydrolyzable tannins (chebulagic acid and punicalagin) target viral glycoprotein-glycosaminoglycan interactions to inhibit herpes simplex virus 1 entry and cell-to-cell spread. J Virol. 2011;85:4386–98. doi: 10.1128/JVI.01492-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Khan MT, Ather A, Thompson KD, Gambari R. Extracts and molecules from medicinal plants against herpes simplex viruses. Antiviral Res. 2005;67:107–19. doi: 10.1016/j.antiviral.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 80.Superti F, Ammendolia MG, Marchetti M. New advances in anti-HSV chemotherapy. Curr Med Chem. 2008;15:900–11. doi: 10.2174/092986708783955419. [DOI] [PubMed] [Google Scholar]
- 81.Petrera E, Coto CE. Therapeutic effect of meliacine, an antiviral derived from Melia azedarach L., in mice genital herpetic infection. Phytother Res. 2009;23:1771–7. doi: 10.1002/ptr.2850. [DOI] [PubMed] [Google Scholar]
- 82.Chen SD, Gao H, Zhu QC, Wang YQ, Li T, Mu ZQ, et al. Houttuynoids A-E, anti-herpes simplex virus active flavonoids with novel skeletons from Houttuynia cordata. Org Lett. 2012;14:1772–5. doi: 10.1021/ol300017m. [DOI] [PubMed] [Google Scholar]
- 83.Gescher K, Kuhn J, Hafezi W, Louis A, Derksen A, Deters A, et al. Inhibition of viral adsorption and penetration by an aqueous extract from Rhododendron ferrugineum L. as antiviral principle against herpes simplex virus type-1. Fitoterapia. 2011;82:408–13. doi: 10.1016/j.fitote.2010.11.022. [DOI] [PubMed] [Google Scholar]
- 84.Danaher RJ, Wang C, Dai J, Mumper RJ, Miller CS. Antiviral effects of blackberry extract against herpes simplex virus type 1. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:e31–5. doi: 10.1016/j.tripleo.2011.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gescher K, Kuhn J, Lorentzen E, Hafezi W, Derksen A, Deters A, et al. Proanthocyanidin-enriched extract from Myrothamnus flabellifolia Welw. exerts antiviral activity against herpes simplex virus type 1 by inhibition of viral adsorption and penetration. J Ethnopharmacol. 2011;134:468–74. doi: 10.1016/j.jep.2010.12.038. [DOI] [PubMed] [Google Scholar]
- 86.Bertol JW, Rigotto C, de Padua RM, Kreis W, Barardi CR, Braga FC, et al. Antiherpes activity of glucoevatromonoside, a cardenolide isolated from a Brazilian cultivar of Digitalis lanata. Antiviral Res. 2011;92:73–80. doi: 10.1016/j.antiviral.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 87.Vo TS, Ngo DH, Ta QV, Kim SK. Marine organisms as a therapeutic source against herpes simplex virus infection. Eur J Pharm Sci. 2011;44:11–20. doi: 10.1016/j.ejps.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 88.Sagar S, Kaur M, Minneman KP. Antiviral lead compounds from marine sponges. Mar Drugs. 2010;8:2619–38. doi: 10.3390/md8102619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sierra S, Kupfer B, Kaiser R. Basics of the virology of HIV-1 and its replication. J Clin Virol. 2005;34:233–44. doi: 10.1016/j.jcv.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 90.Shaw GM, Hunter E. HIV transmission. Cold Spring Harb Perspect Med. 2012;2:11. doi: 10.1101/cshperspect.a006965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Moss JA. HIV/AIDS Review. Radiol Technol. 2013;84:247–67. [PubMed] [Google Scholar]
- 92.Burton DR, Desrosiers RC, Doms RW, Koff WC, Kwong PD, Moore JP, et al. HIV vaccine design and the neutralizing antibody problem. Nat Immunol. 2004;5:233–6. doi: 10.1038/ni0304-233. [DOI] [PubMed] [Google Scholar]
- 93.Ghosh RK, Ghosh SM, Chawla S. Recent advances in antiretroviral drugs. Expert Opin Pharmacother. 2011;12:31–46. doi: 10.1517/14656566.2010.509345. [DOI] [PubMed] [Google Scholar]
- 94.Evans A, Lee R, Mammen-Tobin A, Piyadigamage A, Shann S, Waugh M. HIV revisited: The global impact of the HIV/AIDS epidemic. Skinmed. 2004;3:149–56. doi: 10.1111/j.1540-9740.2004.02304.x. [DOI] [PubMed] [Google Scholar]
- 95.Piot P, Quinn TC. Response to the AIDS pandemic: A global health model. N Engl J Med. 2013;368:2210–8. doi: 10.1056/NEJMra1201533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Margolis AM, Heverling H, Pham PA, Stolbach A. A review of the toxicity of HIV medications. J Med Toxicol. doi: 10.1007/s13181-013-0325-8. [In press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Singh IP, Bodiwala HS. Recent advances in anti-HIV natural products. Nat Prod Rep. 2010;27:1781–800. doi: 10.1039/c0np00025f. [DOI] [PubMed] [Google Scholar]
- 98.Cos P, Maes L, Vlietinck A, Pieters L. Plant-derived leading compounds for chemotherapy of human immunodeficiency virus (HIV) infection-an update (1998-2007) Planta Med. 2008;74:1323–37. doi: 10.1055/s-2008-1081314. [DOI] [PubMed] [Google Scholar]
- 99.Zhou X, Liu J, Yang B, Lin X, Yang XW, Liu Y. Marine natural products with anti-HIV activities in the last decade. Curr Med Chem. 2013;20:953–73. [PubMed] [Google Scholar]
- 100.Kim SK, Karadeniz F. Anti-HIV activity of extracts and compounds from marine algae. Adv Food Nutr Res. 2011;64:255–65. doi: 10.1016/B978-0-12-387669-0.00020-X. [DOI] [PubMed] [Google Scholar]
- 101.Vo TS, Kim SK. Potential anti-HIV agents from marine resources: An overview. Mar Drugs. 2010;8:2871–92. doi: 10.3390/md8122871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lubbe A, Seibert I, Klimkait T, van der Kooy F. Ethnopharmacology in overdrive: The remarkable anti-HIV activity of Artemisia annua. J Ethnopharmacol. 2012;141:854–9. doi: 10.1016/j.jep.2012.03.024. [DOI] [PubMed] [Google Scholar]
- 103.Huerta-Reyes M, Basualdo Mdel C, Abe F, Jimenez-Estrada M, Soler C, Reyes-Chilpa R. HIV-1 inhibitory compounds from Calophyllum brasiliense leaves. Biol Pharm Bull. 2004;27:1471–5. doi: 10.1248/bpb.27.1471. [DOI] [PubMed] [Google Scholar]
- 104.Cesar GZ, Alfonso MG, Marius MM, Elizabeth EM, Angel CB, Maira HR, et al. Inhibition of HIV-1 reverse transcriptase, toxicological and chemical profile of Calophyllum brasiliense extracts from Chiapas, Mexico. Fitoterapia. 2011;82:1027–34. doi: 10.1016/j.fitote.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 105.Kudo E, Taura M, Matsuda K, Shimamoto M, Kariya R, Goto H, et al. Inhibition of HIV-1 replication by a tricyclic coumarin GUT-70 in acutely and chronically infected cells. Bioorg Med Chem Lett. 2013;23:606–9. doi: 10.1016/j.bmcl.2012.12.034. [DOI] [PubMed] [Google Scholar]
- 106.Hood JL, Jallouk AP, Campbell N, Ratner L, Wickline SA. Cytolytic nanoparticles attenuate HIV-1 infectivity. Antivir Ther. 2013;18:95–103. doi: 10.3851/IMP2346. [DOI] [PubMed] [Google Scholar]
- 107.Eccles R. Understanding the symptoms of the common cold and influenza. Lancet Infect Dis. 2005;5:718–25. doi: 10.1016/S1473-3099(05)70270-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Rello J, Pop-Vicas A. Clinical review: Primary influenza viral pneumonia. Crit Care. 2009;13:235. doi: 10.1186/cc8183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Pleschka S. Overview of influenza viruses. Curr Top Microbiol Immunol. 2013;370:1–20. doi: 10.1007/82_2012_272. [DOI] [PubMed] [Google Scholar]
- 110.Yamada S, Suzuki Y, Suzuki T, Le MQ, Nidom CA, Sakai-Tagawa Y, et al. Haemagglutinin mutations responsible for the binding of H5N1 influenza A viruses to human-type receptors. Nature. 2006;444:378–82. doi: 10.1038/nature05264. [DOI] [PubMed] [Google Scholar]
- 111.van der Vries E, Collins PJ, Vachieri SG, Xiong X, Liu J, Walker PA, et al. H1N1 2009 pandemic influenza virus: Resistance of the I223R neuraminidase mutant explained by kinetic and structural analysis. PLoS Pathog. 2012;8:e1002914. doi: 10.1371/journal.ppat.1002914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Mak PW, Jayawardena S, Poon LL. The evolving threat of influenza viruses of animal origin and the challenges in developing appropriate diagnostics. Clin Chem. 2012;58:1527–33. doi: 10.1373/clinchem.2012.182626. [DOI] [PubMed] [Google Scholar]
- 113.Fiore AE, Fry A, Shay D, Gubareva L, Bresee JS, Uyeki TM. Antiviral agents for the treatment and chemoprophylaxis of influenza --- recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2011;60:1–24. [PubMed] [Google Scholar]
- 114.Samson M, Pizzorno A, Abed Y, Boivin G. Influenza virus resistance to neuraminidase inhibitors. Antiviral Res. 2013;98:174–85. doi: 10.1016/j.antiviral.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 115.Krawitz C, Mraheil MA, Stein M, Imirzalioglu C, Domann E, Pleschka S, et al. Inhibitory activity of a standardized elderberry liquid extract against clinically-relevant human respiratory bacterial pathogens and influenza A and B viruses. BMC Complement Altern Med. 2011;11:16. doi: 10.1186/1472-6882-11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Theisen LL, Muller CP. EPs (R) 7630 (Umckaloabo (R)), an extract from Pelargonium sidoides roots, exerts anti-influenza virus activity in vitro and in vivo. Antiviral Res. 2012;94:147–56. doi: 10.1016/j.antiviral.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 117.He W, Han H, Wang W, Gao B. Anti-influenza virus effect of aqueous extracts from dandelion. Virol J. 2011;8:538. doi: 10.1186/1743-422X-8-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ma SG, Gao RM, Li YH, Jiang JD, Gong NB, Li L, et al. Antiviral Spirooliganones A and B with Unprecedented Skeletons from the Roots of Illicium oligandrum. Org Lett. 2013;15:4450–3. doi: 10.1021/ol401992s. [DOI] [PubMed] [Google Scholar]
- 119.Grienke U, Schmidtke M, von Grafenstein S, Kirchmair J, Liedl KR, Rollinger JM. Influenza neuraminidase: A druggable target for natural products. Nat Prod Rep. 2012;29:11–36. doi: 10.1039/c1np00053e. [DOI] [PubMed] [Google Scholar]
- 120.Dao TT, Nguyen PH, Lee HS, Kim E, Park J, Lim SI, et al. Chalcones as novel influenza A (H1N1) neuraminidase inhibitors from Glycyrrhiza inflata. Bioorg Med Chem Lett. 2011;21:294–8. doi: 10.1016/j.bmcl.2010.11.016. [DOI] [PubMed] [Google Scholar]
- 121.Dao TT, Dang TT, Nguyen PH, Kim E, Thuong PT, Oh WK. Xanthones from Polygala karensium inhibit neuraminidases from influenza A viruses. Bioorg Med Chem Lett. 2012;22:3688–92. doi: 10.1016/j.bmcl.2012.04.028. [DOI] [PubMed] [Google Scholar]
- 122.Jeong HJ, Kim YM, Kim JH, Kim JY, Park JY, Park SJ, et al. Homoisoflavonoids from Caesalpinia sappan displaying viral neuraminidases inhibition. Biol Pharm Bull. 2012;35:786–90. doi: 10.1248/bpb.35.786. [DOI] [PubMed] [Google Scholar]
- 123.Sabella C. Measles: Not just a childhood rash. Cleve Clin J Med. 2010;77:207–13. doi: 10.3949/ccjm.77a.09123. [DOI] [PubMed] [Google Scholar]
- 124.Clements CJ, Cutts FT. The epidemiology of measles: Thirty years of vaccination. Curr Top Microbiol Immunol. 1995;191:13–33. doi: 10.1007/978-3-642-78621-1_2. [DOI] [PubMed] [Google Scholar]
- 125.Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349:1269–76. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- 126.Mossong J, Muller CP. Modelling measles re-emergence as a result of waning of immunity in vaccinated populations. Vaccine. 2003;21:4597–603. doi: 10.1016/s0264-410x(03)00449-3. [DOI] [PubMed] [Google Scholar]
- 127.Zandotti C, Jeantet D, Lambert F, Waku-Kouomou D, Wild F, Freymuth F, et al. Re-emergence of measles among young adults in Marseilles, France. Eur J Epidemiol. 2004;19:891–3. doi: 10.1023/b:ejep.0000040453.13914.48. [DOI] [PubMed] [Google Scholar]
- 128.Kurokawa M, Ochiai H, Nagasaka K, Neki M, Xu H, Kadota S, et al. Antiviral traditional medicines against herpes simplex virus (HSV-1), poliovirus, and measles virus in vitro and their therapeutic efficacies for HSV-1 infection in mice. Antiviral Res. 1993;22:175–88. doi: 10.1016/0166-3542(93)90094-y. [DOI] [PubMed] [Google Scholar]
- 129.Huang SP, Shieh GJ, Lee L, Teng HJ, Kao ST, Lin JG. Inhibition effect of shengma-gegen-tang on measles virus in Vero cells and human peripheral blood mononuclear cells. Am J Chin Med. 1997;25:89–96. doi: 10.1142/S0192415X97000123. [DOI] [PubMed] [Google Scholar]
- 130.McWhorter JH. Spicebush. A Cherokee remedy for the measles. N C Med J. 1996;57:306. [PubMed] [Google Scholar]
- 131.Lin YM, Flavin MT, Schure R, Chen FC, Sidwell R, Barnard DL, et al. Antiviral activities of biflavonoids. Planta Med. 1999;65:120–5. doi: 10.1055/s-1999-13971. [DOI] [PubMed] [Google Scholar]
- 132.Hayashi T, Hayashi K, Maeda M, Kojima I. Calcium spirulan, an inhibitor of enveloped virus replication, from a blue-green alga Spirulina platensis. J Nat Prod. 1996;59:83–7. doi: 10.1021/np960017o. [DOI] [PubMed] [Google Scholar]
- 133.Petricevich VL, Mendonca RZ. Inhibitory potential of Crotalus durissus terrificus venom on measles virus growth. Toxicon. 2003;42:143–53. doi: 10.1016/s0041-0101(03)00124-7. [DOI] [PubMed] [Google Scholar]
- 134.Cos P, Hermans N, De Bruyne T, Apers S, Sindambiwe JB, Vanden Berghe D, et al. Further evaluation of Rwandan medicinal plant extracts for their antimicrobial and antiviral activities. J Ethnopharmacol. 2002;79:155–63. doi: 10.1016/s0378-8741(01)00362-2. [DOI] [PubMed] [Google Scholar]
- 135.Olila D, Olwa O, Opuda-Asibo J. Screening extracts of Zanthoxylum chalybeum and Warburgia ugandensis for activity against measles virus (Swartz and Edmonston strains) in vitro. Afr Health Sci. 2002;2:2–10. [PMC free article] [PubMed] [Google Scholar]
- 136.Barnard DL. Inhibitors of measles virus. Antivir Chem Chemother. 2004;15:111–9. doi: 10.1177/095632020401500301. [DOI] [PubMed] [Google Scholar]
- 137.Parker ME, Chabot S, Ward BJ, Johns T. Traditional dietary additives of the Maasai are antiviral against the measles virus. J Ethnopharmacol. 2007;114:146–52. doi: 10.1016/j.jep.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 138.Nwodo UU, Ngene AA, Iroegbu CU, Onyedikachi OA, Chigor VN, Okoh AI. In vivo evaluation of the antiviral activity of Cajanus cajan on measles virus. Arch Virol. 2011;156:1551–7. doi: 10.1007/s00705-011-1032-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Hall CB. Prospects for a respiratory syncytial virus vaccine. Science. 1994;265:1393–4. doi: 10.1126/science.7915433. [DOI] [PubMed] [Google Scholar]
- 140.Ruuskanen O, Ogra PL. Respiratory syncytial virus. Curr Probl Pediatr. 1993;23:50–79. doi: 10.1016/0045-9380(93)90003-U. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Braciale TJ. Respiratory syncytial virus and T cells: Interplay between the virus and the host adaptive immune system. Proc Am Thorac Soc. 2005;2:141–6. doi: 10.1513/pats.200503-022AW. [DOI] [PubMed] [Google Scholar]
- 142.Sigurs N, Gustafsson PM, Bjarnason R, Lundberg F, Schmidt S, Sigurbergsson F, et al. Severe respiratory syncytial virus bronchiolitis in infancy and asthma and allergy at age 13. Am J Respir Crit Care Med. 2005;171:137–41. doi: 10.1164/rccm.200406-730OC. [DOI] [PubMed] [Google Scholar]
- 143.Glezen WP, Taber LH, Frank AL, Kasel JA. Risk of primary infection and reinfection with respiratory syncytial virus. Am J Dis Child. 1986;140:543–6. doi: 10.1001/archpedi.1986.02140200053026. [DOI] [PubMed] [Google Scholar]
- 144.Hall CB, Walsh EE, Long CE, Schnabel KC. Immunity to and frequency of reinfection with respiratory syncytial virus. J Infect Dis. 1991;163:693–8. doi: 10.1093/infdis/163.4.693. [DOI] [PubMed] [Google Scholar]
- 145.Henderson FW, Collier AM, Clyde WA, Jr, Denny FW. Respiratory- syncytial-virus infections, reinfections and immunity. A prospective, longitudinal study in young children. N Engl J Med. 1979;300:530–4. doi: 10.1056/NEJM197903083001004. [DOI] [PubMed] [Google Scholar]
- 146.Falsey AR, Walsh EE. Respiratory syncytial virus infection in adults. Clin Microbiol Rev. 2000;13:371–84. doi: 10.1128/cmr.13.3.371-384.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Hall CB, Long CE, Schnabel KC. Respiratory syncytial virus infections in previously healthy working adults. Clin Infect Dis. 2001;33:792–6. doi: 10.1086/322657. [DOI] [PubMed] [Google Scholar]
- 148.Ma LY, Ma SC, Wei F, Lin RC, But PP, Lee SH, et al. Uncinoside A and B, two new antiviral chromone glycosides from Selaginella uncinata. Chem Pharm Bull (Tokyo) 2003;51:1264–7. doi: 10.1248/cpb.51.1264. [DOI] [PubMed] [Google Scholar]
- 149.Huang W, Zhang X, Wang Y, Ye W, Ooi VE, Chung HY, et al. Antiviral biflavonoids from Radix Wikstroemiae (Liaogewanggen) Chin Med. 2010;5:23. doi: 10.1186/1749-8546-5-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Wang Y, Chen M, Zhang J, Zhang XL, Huang XJ, Wu X, et al. Flavone C-glycosides from the leaves of Lophatherum gracile and their in vitro antiviral activity. Planta Med. 2012;78:46–51. doi: 10.1055/s-0031-1280128. [DOI] [PubMed] [Google Scholar]
- 151.Wang KC, Chang JS, Chiang LC, Lin CC. Sheng-Ma-Ge-Gen-Tang (Shoma-kakkon-to) inhibited cytopathic effect of human respiratory syncytial virus in cell lines of human respiratory tract. J Ethnopharmacol. 2011;135:538–44. doi: 10.1016/j.jep.2011.03.058. [DOI] [PubMed] [Google Scholar]
- 152.Wang KC, Chang JS, Chiang LC, Lin CC. Cimicifuga foetida L. inhibited human respiratory syncytial virus in HEp-2 and A549 cell lines. Am J Chin Med. 2012;40:151–62. doi: 10.1142/S0192415X12500127. [DOI] [PubMed] [Google Scholar]
- 153.Wang KC, Chang JS, Lin LT, Chiang LC, Lin CC. Antiviral effect of cimicifugin from Cimicifuga foetida against human respiratory syncytial virus. Am J Chin Med. 2012;40:1033–45. doi: 10.1142/S0192415X12500760. [DOI] [PubMed] [Google Scholar]
- 154.Zang N, Xie X, Deng Y, Wu S, Wang L, Peng C, et al. Resveratrol-mediated gamma interferon reduction prevents airway inflammation and airway hyperresponsiveness in respiratory syncytial virus-infected immunocompromised mice. J Virol. 2011;85:13061–8. doi: 10.1128/JVI.05869-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Wang LJ, Geng CA, Ma YB, Huang XY, Luo J, Chen H, et al. Synthesis, biological evaluation and structure-activity relationships of glycyrrhetinic acid derivatives as novel anti-hepatitis B virus agents. Bioorg Med Chem Lett. 2012;22:3473–9. doi: 10.1016/j.bmcl.2012.03.081. [DOI] [PubMed] [Google Scholar]
- 156.Hsu MJ, Hung SL. Antiherpetic potential of 6-bromoindirubin-3’- acetoxime (BIO-acetoxime) in human oral epithelial cells. Arch Virol. 2013;158:1287–96. doi: 10.1007/s00705-013-1629-3. [DOI] [PubMed] [Google Scholar]
- 157.Xie Y, Huang B, Yu K, Shi F, Liu T, Xu W. Caffeic acid derivatives: A new type of influenza neuraminidase inhibitors. Bioorg Med Chem Lett. 2013;23:3556–60. doi: 10.1016/j.bmcl.2013.04.033. [DOI] [PubMed] [Google Scholar]


