Abstract
Ischemia–reperfusion (I/R) injury has a complex pathophysiology resulting from a number of contributing factors. Therefore, it is difficult to achieve effective treatment or protection by individually targeting the mediators or mechanisms. Our aim was to analyze the individual and combined effects of N-acetylcysteine (NAC) and the prostaglandin E1 (PGE1) analog alprostadil on hepatic I/R injury in rats. Thirty male Sprague-Dawley rats were randomly divided into five groups (six rats per group) as follows: Control group, I/R group, I/R + NAC group, I/R + alprostadil group, and I/R + NAC + alprostadil group. The rats received injections of NAC (150 mg/kg) and/or alprostadil (0.05 μg/kg) over a period of 30 min prior to ischemia. These rats were then subjected to 60 min of hepatic ischemia followed by a 60-min reperfusion period. Hepatic superoxide dismutase (SOD), catalase, and glutathione levels were significantly decreased as a result of I/R injury, but they were increased in groups treated with NAC. Hepatic malondialdehyde (MDA), myeloperoxidase (MPO), and nitric oxide (NO) activities were significantly increased after I/R injury, but they were decreased in the groups with NAC treatment. Alprostadil decreased NO production, but had no effect on MDA and MPO. Histological results showed that both NAC and alprostadil were effective in improving liver tissue morphology during I/R injury. Although NAC and alprostadil did not have a synergistic effect, our findings suggest that treatment with either NAC or alprostadil has benefits for ameliorating hepatic I/R injury.
Keywords: Alprostadil, Ischemia–reperfusion, N-acetylcysteine, Prostaglandin E1 analog
INTRODUCTION
Hepatic ischemia–reperfusion (I/R) is a key clinical problem associated with numerous adverse events such as hypovolemic shock,[1] disseminated intravascular coagulation,[2] liver transplantation and surgery,[3] cardiac failure and arrest, alcohol toxicity, and several other pathological conditions. The observed pathophysiology of hepatic I/R injury is as follows. The liver is a highly oxygen-utilizing organ. Thus, impairment of blood flow rapidly causes hepatic hypoxia, which may progress to absolute anoxia, particularly in the pericentral regions of the hepatic lobe.
Subsequent reperfusion leads to the activation of Kupffer cells, which are resident macrophages of the liver. These cells contribute to liver pathology by producing reactive oxygen species (ROS) such as superoxides, hydrogen peroxide, and hydroxyl radicals, which have been implicated in cell damage. Oxidative stress can also promote lipid peroxidation, which causes structural and functional derangements and cell death ultimately.[4,5] In addition, pro-inflammatory cytokines, chemokines, and other mediators produced by these cells contribute to post-ischemic tissue injury, systemic inflammatory syndrome, and multiorgan failure. In conjunction with activated complement factors, these inflammatory mediators activate and recruit neutrophils into the post-ischemic liver, which generates excess of reactive oxygen radicals and releases additional proteases and other degradative enzymes.[6,7,8,9]
In addition to an inflammatory response, ROS induces the expression of endothelin-1 and consequent vasoconstriction of sinusoids. This promotes the heterogeneous closure of many microvessels and prolongs ischemia in certain areas of the liver even after reperfusion.[5,10] Therefore, finding appropriate treatments for hepatic I/R injury is of paramount importance.
N-acetylcysteine (NAC) is a small molecule containing a thiol (sulfhydryl-containing) group, which has antioxidant properties and is freely filterable, thus making it readily accessible to the intracellular compartment.[11,12] NAC has been clinically used for more than 30 years, primarily as a mucolytic agent. It has also been used in states of decreased glutathione (GSH) and oxidative stress in HIV infections, cancer, heart diseases, and other diseases. Due to its hepatoprotective activity, intravenous and oral administrations of NAC have been used extensively for the treatment of acetaminophen poisoning. The diverse pharmacological applications of NAC are mainly due to its physiological role as an ROS scavenger.[12,13]
Prostaglandin E1 (PGE1) is a naturally occurring prostaglandin. It was originally introduced as a therapeutic agent because of its potent direct vasodilator actions. Numerous experiments indicate a beneficial effect of PGE1 when intravenously administered to patients with chronic vascular disease due to its possible direct vasodilatory effect causing an increase in local tissue perfusion.[14] Alprostadil is a synthetic form of PGE1 that can function as a PGE1 analog by producing a strong relaxant effect on the smooth muscles of peripheral blood vessels. It functions as a peripheral vasodilator and platelet aggregation inhibitor by interacting with specific G-protein coupled receptors to increase the adenosine levels in plasma. Adenosine is an endogenous byproduct of purine metabolism that causes vasodilation, decreases leukocyte activities, provides for endothelial protection, inhibits platelet aggregation, and ameliorates the rheological properties of blood with a concomitant increase in oxygen delivery to tissues.[15] Although alprostadil has been used for several years in patients with liver transplants,[16] the mechanisms related to its protective effects against hepatic I/R injury remain unknown.
In the present study, the protective effects of NAC and/or alprostadil against hepatic I/R-induced tissue damage in rats were examined by measuring different biochemical parameters. These included the levels of the following parameters: (1) an end product of lipid peroxidation; (2) liver malondialdehyde (MDA); (3) antioxidant enzymes, including catalase (CAT), superoxide dismutase (SOD), and GSH; and (4) indicators of inflammation, including myeloperoxidase (MPO) activity and nitric oxide (NO).
MATERIALS AND METHODS
Animals
Male Sprague-Dawley rats (250-300 g) were obtained from the animal center of the National Science Council, Taiwan, Republic of China. They were fed a standard diet and were given water ad libitum. They were treated according to the regulations in the “Guide for the Care and Use of Laboratory Animals” (National Academy Press, 1996). The use of animals for our experiments was approved by the ethics committee of the National Yang-Ming University, Taipei, Taiwan.
Thirty rats were randomly divided into five groups (six rats in each group) as follows: Control, I/R, I/R + NAC, I/R + alprostadil, and I/R + NAC + alprostadil groups. Rats in the control group were neither subjected to I/R injury nor any treatment. In the I/R groups with treatments, the rats were subjected to 60 min of hepatic ischemia followed by a 60-min reperfusion period. For the treatment groups, an infusion pump (KDS220; KD Scientific Co., Holliston, MA, USA) was used to infuse 150 mg/kg of NAC and/or 0.05 μg/kg of alprostadil into the femoral vein continuously for 30 min prior to 60 min of hepatic ischemia followed by 60 min of reperfusion.
Animal model and parameters for hepatic I/R injury
The rat model with I/R injury was generated as previously described.[17,18] Briefly, each male Sprague-Dawley rat was anesthetized with urethane (1.25 g/kg, intraperitoneally) and its trachea was cannulated for artificial respiration with a ventilator. A polyethylene (PE-50) catheter was inserted into the femoral artery to monitor blood pressure using a polygraph (TA240S; Gould Co., USA) and for drug administration. The liver was exposed through an upper midline incision and two pieces of fine silk thread were looped along the right and left branches of the portal vein, hepatic artery, and bile duct. This procedure whereby the silk thread was inserted into a snare with a piece of PE-90 tubing provided for the occlusion of the blood supply to the median and left lobes (left branch).
To study I/R injury, ischemia and reperfusion period (each maintained for 60 min) of the median/left lobes with immediate occlusion of the right lobe vasculature was carried out. One hour after completing the reperfusion procedure, the initial ischemic–reperfused median/left lobes were resected and determination of the levels of MPO, MDA, GSH, CAT, SOD, and NO was made. Blood samples for alanine aminotransferase (ALT) and aspartate aminotransferase (AST) measurements were collected immediately after femoral catheterization and completion of the reperfusion procedure.
Biochemical analyses
MPO assay
MPO activity in the liver tissue was determined using a procedure similar to that of Hillegas et al.[19] Harvested liver samples were homogenized in 50 mM potassium phosphate buffer (PB, pH 6.0) and centrifuged at 41,400 × g for 10 min. The pellets were then suspended in 50 mM PB containing 0.5% hexadecyl trimethyl ammonium bromide. After three cycles of freezing and thawing, with sonication between each cycle, the samples were centrifuged at 41,400 × g for 10 min. An aliquot (0.3 ml) was added to 2.3 ml of a reaction mixture containing 50 mM PB, 0.19 mg/ml o-dianisidine, and 20 mM H2O2 solution. Enzyme activity was defined as the amount of MPO that caused a change in the absorbance measured at 460 nm for 3 min. MPO activity was expressed as U/g tissue.
MDA assay
A liver sample (0.5 g) was homogenized in 4.5 ml of thiobarbituric acid (TBA) reagent containing 0.375% TBA, 15% trichloroacetic acid, and 0.25 N HCl. Samples were boiled for 15 min, cooled, and centrifuged. Absorbance of the supernatants was spectrophotometrically measured at 532 nm.[20]
GSH assay
Hepatic GSH levels were determined using a commercial GSH assay kit (Cayman Chemical Co., Ann Arbor, MI, USA). This assay uses a carefully optimized enzymatic recycling method in which glutathione reductase is used to quantify GSH. Liver tissue was first homogenized in 5-10 ml of cold buffer [either 50 mM MES or phosphate, pH 6-7, containing 1 mM ethylenediaminetetraacetic acid (EDTA)] per gram of liver tissue and centrifuged at 10,000 × g for 15 min at 4°C, followed by deproteination with metaphosphoric acid. After adding triethanolamine solution, an assay cocktail [a mixture of MES buffer (11.25 ml), reconstituted cofactor mixture (0.45 ml), reconstituted enzyme mixture (2.1 ml), water (2.3 ml), and reconstituted 5,5′-dithiobis (2-nitrobenzoic acid) (0.45 ml)] was prepared and total GSH in each of the deproteinated samples was determined spectrophotometrically at 405 or 414 nm.
CAT assay
CAT activity was determined using a commercial chemical CAT assay kit (Cayman Chemical Co.). This assay utilizes the peroxidative function of CAT to determine the enzyme activity. Liver tissue was homogenized in 5-10 ml of cold buffer (50 mM potassium phosphate, pH 7.0, containing 1 mM EDTA) per gram of liver tissue and centrifuged at 10,000 × g for 15 min at 4°C. The sample was then mixed sequentially with hydrogen peroxide, potassium hydroxide, Purpald, and potassium periodate, and then read at 540 nm.
SOD assay
Hepatic SOD activity was determined using a commercial SOD assay kit (Cayman Chemical Co.). This assay utilizes a tetrazolium salt to detect superoxide radicals generated by xanthine oxidase and hypoxanthine. Liver tissue was homogenized in 5-10 ml of cold buffer (20 mM HEPES buffer, pH 7.2, containing 1 mM EDTA, 210 mM mannitol, and 70 mM sucrose) per gram of liver tissue and centrifuged at 1500 × g for 5 min at 4°C. The reaction was initiated by adding xanthine oxidase and incubated at room temperature for 20 min, after which the absorbance was read at 450 nm.
NO assay
Hepatic NO activity was determined using a commercial nitrate/nitrite colorimetric assay kit (Cayman Chemical Co.). This assay measures the total nitrate/nitrite concentrations in a simple two-step method. The first step involves the conversion of nitrate to nitrite by nitrate reductase. The second step uses Griess reagent that converts nitrites into deep purple azo compounds which can be measured photometrically to determine the concentration of NO2−.
Histological analysis
Rats were sacrificed by decapitation and the livers were harvested. Small pieces of liver tissue were placed in a 10% (v/v) formalin solution and processed routinely by embedding them in paraffin. Tissue sections (4-5 μm) were stained with hematoxylin and eosin and examined under a light microscope. Results were interpreted by pathologists.
Statistical analysis
Results are expressed as means ± standard errors of the mean (SEMs). The concentrations of MPO, MDA, GSH, CAT, SOD, NO, ALT, and AST in different experimental groups were compared using the Wilcoxon rank sum test. A P value of < 0.05 indicated statistical significance.
RESULTS
Hepatic I/R induction and effects of NAC and/or alprostadil
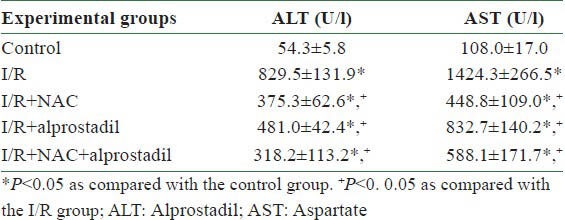
During the experimental procedure, blood pressure was continuously monitored using a polygraph. The blood pressure of all experimental rats remained stable and none of them died during I/R induction. To evaluate the level of liver damage after the reperfusion procedure, blood samples from different groups were collected immediately via the femoral catheters after completing the reperfusion procedure. As shown in Table 1, the ALT and AST levels increased significantly in the I/R group as compared with the control group, while treatment with either NAC or alprostadil ameliorated these increases in ALT and AST. These results indicated that although the liver damage had been attenuated, there was no significant difference between combined treatment (NAC + alprostadil) and each treatment administered separately.
Table 1.
Effects of hepatic I/R injury and pretreatment with NAC and/or alprostadil on alanine aminotransferase and aspartate aminotransferase activities in plasma
The antioxidant activity of NAC and/or alprostadil in the liver
Because antioxidant enzymes are important for maintaining an optimal chemical reducing environment to protect liver from ROS damage, we analyzed the activities of several of these liver enzymes. As shown in Figure 1a, CAT levels were decreased after I/R was induced, and the decrease was significantly lower than that in the control group. Treatment with NAC and NAC + alprostadil improved the CAT activity, while alprostadil alone had no effect on the CAT activity, compared with the I/R group. The level of hepatic SOD in the liver tissue also decreased after I/R induction, which was significantly lower in the control group. Compared with the I/R group, separate treatments with NAC and alprostadil and their combined administration clearly increased the SOD levels. However, there were no synergistic effects of the combined treatment as compared with the results of separate treatments [Figure 1b]. We also measured the levels of GSH, which participates in many metabolic processes that protect cells against the actions of free radicals. As shown in Figure 1c, hepatic GSH levels in the liver tissue decreased after I/R induction, which was significantly lower than in the control group. Compared with the I/R group, GSH levels were significantly increased in the NAC group (226.9 ± 11.0 μM) and in the NAC + alprostadil group (202.1 ± 12.9 μM). The mean liver MDA level, an indicator of lipid peroxidation, was also estimated. The MDA value was significantly higher in the I/R group than in the control group. Compared with the I/R group, the mean MDA level was significantly decreased in the I/R + NAC group. However, there was no significant difference in the MDA levels in either the alprostadil group or the NAC + alprostadil group compared with the I/R group [Figure 1d].
Figure 1.
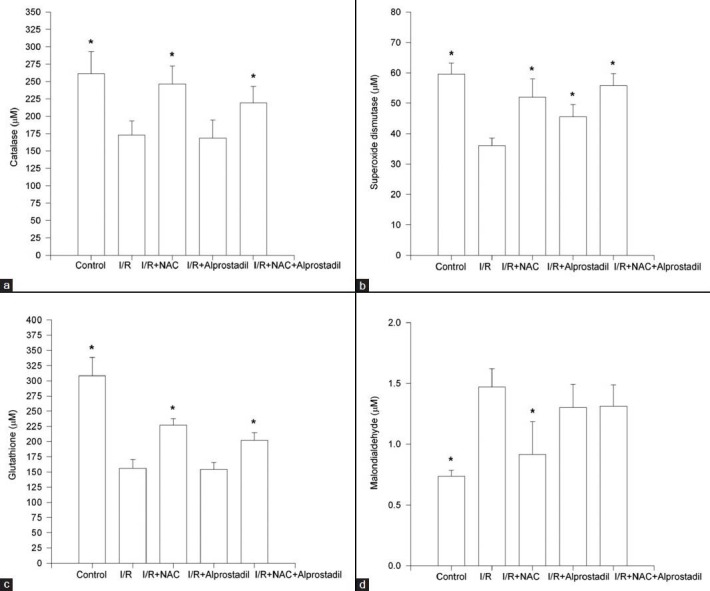
Effects of ischemia–reperfusion (I/R) and pretreatment with NAC and/or alprostadil on (a) catalase, (b) superoxide dismutase, (c) glutathione, and (d) malondialdehyde levels in liver tissues. Procedures are described in Materials and Methods. *P< 0.05 as compared with the I/R group
The anti-inflammatory effect of NAC and/or alprostadil in the liver
Because the inflammatory response after I/R plays a critical role in cell damage, we examined the hepatic MPO levels. This enzyme is reflective of tissue infiltration by neutrophils. As shown in Figure 2a, the mean hepatic MPO level in the I/R group was significantly increased in comparison to the control group. Interestingly, the MPO level in the I/R group that received NAC treatment was lower compared with the I/R group (P < 0.05), whereas there were no significant changes in the MPO levels in the I/R/group treated with either alprostadil or NAC + alprostadil.
Figure 2.
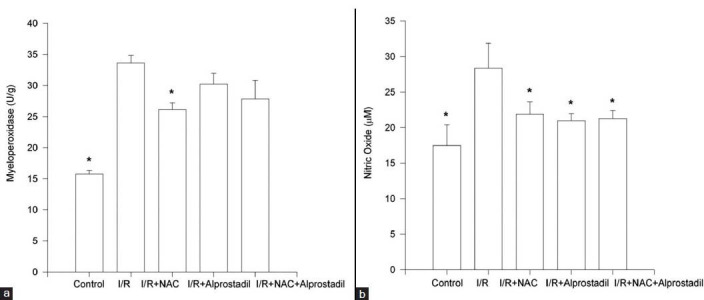
Effects of ischemia–reperfusion (I/R) and pretreatment with NAC and/or alprostadil on (a) myeloperoxidase and (b) nitric oxide levels in liver tissue. Procedures are described in Materials and Methods. *P< 0.05 as compared with the I/R group
We also evaluated the levels of another indicator of inflammation, NO. As shown in Figure 2b, the NO levels in the collected liver tissue increased after I/R, and the increase was significantly higher than that in the control group. Compared with the I/R group, the liver NO levels were significantly lower in the I/R + NAC, I/R + alprostadil, and I/R + NAC + alprostadil groups.
HISTOLOGICAL RESULTS
In order to assess the physiological effects of these treatments in terms of liver protection, we examined liver histology after I/R induction. As shown in Figure 3, in the control group, normal liver parenchyma cells appeared with both hepatocytes and sinusoids around the central vein with a regular morphology. In the I/R group, hepatocytes were prominently swollen with marked vacuolization. Congestion was noted in enlarged sinusoids. The liver parenchyma cells accompanying both hepatocytes and sinusoids around the central vein showed abnormal morphology. In the I/R + NAC group, the I/R + alprostadil group, and the I/R + NAC + alprostadil group, hepatocytes and sinusoids exhibited normal morphology which indicated well-preserved liver parenchyma cells.
Figure 3.
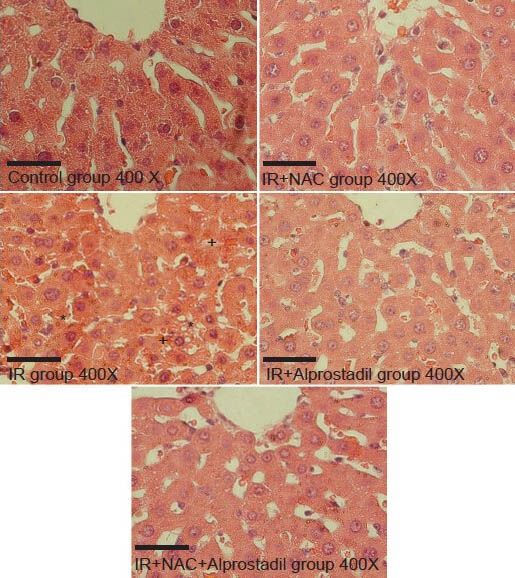
Liver histological analysis. In the control group, normal liver parenchyma cells appear with hepatocytes and sinusoids around the central vein and show regular morphology. In the I/R group, hepatocytes are prominently swollen with marked vacuolization (*). Congestion (+) is noted in enlarged sinusoids. The liver parenchyma cells accompanied by hepatocytes and sinusoids around the central vein show irregular morphology. In the I/R + NAC group, the I/R + alprostadil group, and the I/R + NAC + alprostadil group, hepatocytes and sinusoids are present with normal morphology reflecting well-preserved liver parenchyma cells. The scale bars represent 50 μm. (H and E, ×400)
DISCUSSION
Hepatic I/R injury occurs in many clinical scenarios such as transplantation, trauma, and hepatectomy, and extensive research has been done to improve its clinical results. The aim of some studies was to restore the blood supply to the ischemic liver; however, this could lead to further damage.
This paradox has led to an uncertainty regarding the effectiveness of these treatments. Because I/R injury has a complex pathophysiology that results from a number of contributing factors, it is difficult to achieve effective treatment or protection by targeting only individual mediators or mechanisms. During recent years, the most promising protective strategy against I/R injury to be explored is preconditioning. Preconditioned fasting, ischemia, pharmaceuticals, hyperosmolar solutions, and local somatothermal stimulation (LSTS) have appeared to increase the resistance of cells to ischemia and reperfusion events.[21,22,23,24,25,26]
The goal of this study was to analyze the combined effects of chemicals in preventing liver damage during hepatic I/R injury. For this study, we adopted a rat model that included the simultaneous occlusion of the right lobe vasculature along with reperfusion of the median/left lobes while making sure that the ischemic lobes were well reperfused. This was suggested to be a good model for studying hepatic I/R injury.[17,18,27]
In this model, the time period of I/R is important. If the ischemia period is either too short (<20 min) or too long (>90 min), it would result in either minimal damage or irreversible structural and functional changes, respectively. Sinusoidal perfusion failure is aggravated when the ischemic time period is prolonged to 60 min.[28] Using 60 min of median/left lobar ischemia followed by 60 min of reperfusion as a model, our results showed distinct functional alterations [Table 1]. In addition, this model provided a reproducible system for studying the protective effects of NAC and/or alprostadil on hepatocytes resulting from I/R injury.
NAC is known to counteract oxidative stress and replenish GSH levels. This drug has been shown to have antioxidant activity in vitro[29] and in vivo.[30,31] Nagasaki et al.,[32] showed that in a GSH-depleted liver, NAC prevented hepatic injury and improved its integrity after hepatic I/R injury, by acting not only as a substrate for GSH synthesis but also as a direct scavenger of free radicals. However, the evidence that NAC can reduce I/R injury and prevent complications after major surgery is not conclusive.
For example, in a randomized trial, Khan et al., found no significant difference between the control and NAC-treated group in terms of peak serum transaminase levels and the pathological severity of I/R injury.[29,33] The present study demonstrated that NAC administration could improve liver functions and significantly decrease I/R-induced elevations of MPO, MDA, and NO activities while maintaining the levels of GSH, SOD, and CAT. Our histological findings also support the protective role of NAC toward the liver.
We determined the levels of several antioxidant indicators because oxygen-derived free radicals are widely known to be produced in many organs with I/R injury, such as the heart and liver. Recent evidence indicates that reactive oxygen metabolites play a fundamental role in the hepatotoxicity due to various xenobiotics and medications.[34,35,36] Lipid peroxidation is known to play an essential role in damaging the cell membrane through reactive oxygen radicals. I/R injury has been shown to increase MDA levels, which is an important index of lipid peroxidation.[37,38]
In addition, NO is synthesized by a family of enzymes designated as nitric oxide synthases (NOSs). Among these, the inducible isoforms release NO in large amounts during inflammatory or immunologic reactions and are involved in host tissue damage responses. Superoxide anion is known to react with NO to produce peroxynitrite (ONOO−) that can readily modify proteins and other molecules.[39] Thus, apart from being an indicator of inflammation, NO can also interact with free radicals and cause further cell damage. In addition to NO, the enzyme MPO, which is restricted primarily to polymorphonuclear cells, can also serve as an indicator of inflammation and the generation of ROS because an increase in MPO activity reflects tissue neutrophil infiltration. MPO plays a fundamental role in oxidant production by neutrophils. Neutrophils are a potential source of oxygen free radicals[40] and are considered to be the major effector cells involved in tissue damage that occurs in several inflammatory diseases.[41,42] Previous studies have reported that the addition of neutrophils to the perfusate accentuated I/R injury in the isolated perfused kidney. Consistent with this, we observed a significant increase in the MPO activity in the liver tissue after hepatic I/R injury.
Mechanisms that have been proposed to explain I/R renal injury include anoxia followed by the release of oxygen-derived free radicals during reperfusion. It is reasonable to hypothesize that an increase in antioxidant enzyme levels, such as SOD and CAT, and the maintenance of GSH as well as the decrease in MDA and MPO levels due to NAC could ameliorate the liver damage due to I/R injury.
We also examined the protective effects of alprostadil, an analog of PGE1, against liver injury. Prostaglandins are released primarily by activated Kupffer cells during the reperfusion phase.[44] Several animal studies have shown that prostaglandins are effective for treating ischemic liver injury owing to their ability to increase liver perfusion, inhibit platelet aggregation, and also provide direct cytoprotection in a model of isolated perfused cat liver.[45] The protective actions of PGE1 may be related to its ability to reduce both the release of proteases and the generation of oxygen free radicals by activated leukocytes. Because of the synergistic role between platelets and leukocytes and the interaction of these cells with liver sinusoidal endothelial cells (LSECs) during the reperfusion phase,[46] it is conceivable that PGE1's effects on leukocyte adherence may account for its favorable actions.
Greig et al., found that after reperfusion and progression to primary dysfunction, liver function could be restored by treatment with PGE1.[47] However, the use of pharmacological doses of natural prostaglandins in clinical settings is limited because of drug-related side effects.[48] Thus, synthetic prostaglandin analogs have been developed which show milder side effects and longer half-lives.[48] Several of these analogs have actually improved animal survival and prevented parenchymal injury after prolonged periods of warm hepatic inflow occlusion.[49] In the current study, we observed that alprostadil could attenuate the production of NO induced by I/R and increase the amount of SOD. We expected that alprostadil could attenuate the infiltration of neutrophils. However, the value of MPO only increased slightly after the treatment of alprostadil, indicating its liver protection effect might come from pathways other than inhibiting the adhesion of neutrophils.
SOD activity and its amounts are decreased after I/R injury presumably via the inactivation of mature, active SOD within mitochondria.[50] Manson et al., were the first to demonstrate that the administration of SOD could enhance skin flap survival after arterial and venous occlusion.[51,52] Similarly, cardioplegic solutions containing SOD could enhance postoperative cardiac contractile function after hypothermic global ischemia in dogs.[53]
In a study by Yang et al.,[54] NO had direct toxic effects on LSECs during hypoxia reoxygenation. First, NO production and the expression of eNOS and iNOS were increased in LSECs during hypoxia reoxygenation. Second, an NO inhibitor, N-ω-nitro-l-arginine, protected LSECs against apoptosis, while an NO activator, S-nitroso-N-acetylpenicillamine, increased LSEC apoptosis during hypoxia reoxygenation. Our results showing that NAC and alprostadil mediated inhibition of NO production were correlated with better clinical results, indicating a direct toxic role of NO in hepatic I/R injury. However, our results showed that treatment with both NAC and PGE1 was not synergistic. In our study, we have established that alprostadil is a less potent SOD inducer than NAC. Because NAC is a strong antioxidant, the antioxidative effect of alprostadil might not significantly improve the effect of NAC with regard to the reducing activity. Also, it is probable that alprostadil plays a role in downstream of the effect of NAC, such as ROS-induced inflammation signaling; thus, no synergistic effect could be offered by alprostadil in combination of the treatment of NAC.
In summary, preconditioning with NAC and/or alprostadil treatments had a beneficial effect in protecting the rat liver against I/R injury. These protective effects provided by NAC or alprostadil are easily applied and may provide new avenues for the prevention of ischemic liver disease or problems that arise in liver transplantation.
REFERENCES
- 1.de la Monte SM, Arcidi JM, Moore GW, Hutchins GM. Midzonal necrosis as a pattern of hepatocellular injury after shock. Gastroenterology. 1984;86:627–31. [PubMed] [Google Scholar]
- 2.Yoshikawa T, Murakami M, Yoshida N, Seto O, Kondo M. Effects of superoxide dismutase and catalase on disseminated intravascular coagulation in rats. Thromb Haemost. 1983;50:869–72. [PubMed] [Google Scholar]
- 3.Arthur MJ. Reactive oxygen intermediates and liver injury. J Hepatol. 1988;6:125–31. doi: 10.1016/s0168-8278(88)80472-0. [DOI] [PubMed] [Google Scholar]
- 4.McCord JM. Oxygen-derived free radicals in postischemic tissue injury. N Engl J Med. 1985;312:159–63. doi: 10.1056/NEJM198501173120305. [DOI] [PubMed] [Google Scholar]
- 5.Vollmar B, Glasz J, Leiderer R, Post S, Menger MD. Hepatic microcirculatory perfusion failure is a determinant of liver dysfunction in warm ischemia-reperfusion. Am J Pathol. 1994;145:1421–31. [PMC free article] [PubMed] [Google Scholar]
- 6.Jaeschke H, Farhood A, Bautista AP, Spolarics Z, Spitzer JJ. Complement activates kupffer cells and neutrophils during reperfusion after hepatic ischemia. Am J Physiol. 1993;264:G801–9. doi: 10.1152/ajpgi.1993.264.4.G801. [DOI] [PubMed] [Google Scholar]
- 7.Jaeschke H, Farhood A, Smith CW. Neutrophils contribute to ischemia/reperfusion injury in rat liver In Vivo. FASEB J. 1990;4:3355–9. [PubMed] [Google Scholar]
- 8.Jaeschke H, Farhood A, Bautista AP, Spolarics Z, Spitzer JJ, Smith CW. Functional inactivation of neutrophils with a mac-1 (cd11b/cd18) monoclonal antibody protects against ischemia-reperfusion injury in rat liver. Hepatology. 1993;17:915–23. [PubMed] [Google Scholar]
- 9.Mavier P, Preaux AM, Guigui B, Lescs MC, Zafrani ES, Dhumeaux D. In vitro toxicity of polymorphonuclear neutrophils to rat hepatocytes: Evidence for a proteinase-mediated mechanism. Hepatology. 1988;8:254–8. doi: 10.1002/hep.1840080211. [DOI] [PubMed] [Google Scholar]
- 10.Aruoma OI, Halliwell B, Hoey BM, Butler J. The antioxidant action of n-acetylcysteine: Its reaction with hydrogen peroxide, hydroxyl radical, superoxide, and hypochlorous acid. Free Radic Biol Med. 1989;6:593–7. doi: 10.1016/0891-5849(89)90066-x. [DOI] [PubMed] [Google Scholar]
- 11.De Vries N, De Flora S. N-acetyl-l-cysteine. J Cell Biochem Suppl. 1993;17F:270–7. doi: 10.1002/jcb.240531040. [DOI] [PubMed] [Google Scholar]
- 12.Holdiness MR. Clinical pharmacokinetics of n-acetylcysteine. Clin Pharmacokinet. 1991;20:123–34. doi: 10.2165/00003088-199120020-00004. [DOI] [PubMed] [Google Scholar]
- 13.Cuzzocrea S, Mazzon E, Costantino G, Serraino I, De Sarro A, Caputi AP. Effects of n-acetylcysteine in a rat model of ischemia and reperfusion injury. Cardiovasc Res. 2000;47:537–48. doi: 10.1016/s0008-6363(00)00018-3. [DOI] [PubMed] [Google Scholar]
- 14.Acciavatti A, Laghi Pasini F, Capecchi PL, Messa GL, Lazzerini PE, De Giorgi L, et al. Effects of alprostadil on blood rheology and nucleoside metabolism in patients affected with lower limb chronic ischaemia. Clin Hemorheol Microcirc. 2001;24:49–57. [PubMed] [Google Scholar]
- 15.Koshitani T, Kodama T, Sato H, Takaaki J, Imamura Y, Kato K, et al. A synthetic prostaglandin e1 analog, alprostadil alfadex, relaxes sphincter of oddi in humans. Dig Dis Sci. 2002;47:152–6. doi: 10.1023/a:1013288109127. [DOI] [PubMed] [Google Scholar]
- 16.Kornberg A, Schotte U, Kupper B, Hommann M, Scheele J. Impact of selective prostaglandin e1 treatment on graft perfusion and function after liver transplantation. Hepatogastroenterology. 2004;51:526–31. [PubMed] [Google Scholar]
- 17.Canada AT, Stein K, Martel D, Watkins WD. Biochemical appraisal of models for hepatic ischemia-reperfusion injury. Circ Shock. 1992;36:163–8. [PubMed] [Google Scholar]
- 18.Chiu JH, Ho CT, Wei YH, Lui WY, Hong CY. In vitro and in vivo protective effect of honokiol on rat liver from peroxidative injury. Life Sci. 1997;61:1961–71. doi: 10.1016/s0024-3205(97)00836-9. [DOI] [PubMed] [Google Scholar]
- 19.Hillegass LM, Griswold DE, Brickson B, Albrightson-Winslow C. Assessment of myeloperoxidase activity in whole rat kidney. J Pharmacol Methods. 1990;24:285–95. doi: 10.1016/0160-5402(90)90013-b. [DOI] [PubMed] [Google Scholar]
- 20.Buege JA, Aust SD. Microsomal lipid peroxidation. Methods Enzymol. 1978;52:302–10. doi: 10.1016/s0076-6879(78)52032-6. [DOI] [PubMed] [Google Scholar]
- 21.Chiu JH, Tsou MT, Tung HH, Tai CH, Tsai SK, Chih CL, et al. Preconditioned somatothermal stimulation on median nerve territory increases myocardial heat shock protein 70 and protects rat hearts against ischemia-reperfusion injury. J Thorac Cardiovasc Surg. 2003;125:678–85. doi: 10.1067/mtc.2003.29. [DOI] [PubMed] [Google Scholar]
- 22.Liu Z, Xu Z, Shen W, Li Y, Zhang J, Ye X. Effect of pharmacologic preconditioning with tetrandrine on subsequent ischemia/reperfusion injury in rat liver. World J Surg. 2004;28:620–4. doi: 10.1007/s00268-004-7172-3. [DOI] [PubMed] [Google Scholar]
- 23.Oreopoulos GD, Wu H, Szaszi K, Fan J, Marshall JC, Khadaroo RG, et al. Hypertonic preconditioning prevents hepatocellular injury following ischemia/reperfusion in mice: A role for interleukin 10. Hepatology. 2004;40:211–20. doi: 10.1002/hep.20281. [DOI] [PubMed] [Google Scholar]
- 24.Takahashi Y, Tamaki T, Tanaka M, Konoeda Y, Kawamura A, Katori M, et al. Efficacy of heat-shock proteins induced by severe fasting to protect rat livers preserved for 72 hours from cold ischemia/reperfusion injury. Transplant Proc. 1998;30:3700–2. doi: 10.1016/s0041-1345(98)01201-9. [DOI] [PubMed] [Google Scholar]
- 25.Vajdova K, Heinrich S, Tian Y, Graf R, Clavien PA. Ischemic preconditioning and intermittent clamping improve murine hepatic microcirculation and kupffer cell function after ischemic injury. Liver Transpl. 2004;10:520–8. doi: 10.1002/lt.20126. [DOI] [PubMed] [Google Scholar]
- 26.Pan PJ, Chan RC, Yang AH, Chou CL, Cheng YF, Chiu JH. Protective effects of preconditioned local somatothermal stimulation on neuromuscular plasticity against ischemia--reperfusion injury in rats. J Orthop Res. 2008;26:1670–4. doi: 10.1002/jor.20693. [DOI] [PubMed] [Google Scholar]
- 27.Lin YH, Chiu JH, Tung HH, Tsou MT, Lui WY, Wu CW. Preconditioning somatothermal stimulation on right seventh intercostal nerve territory increases hepatic heat shock protein 70 and protects the liver from ischemia-reperfusion injury in rats. J Surg Res. 2001;99:328–34. doi: 10.1006/jsre.2001.6177. [DOI] [PubMed] [Google Scholar]
- 28.Koo A, Komatsu H, Tao G, Inoue M, Guth PH, Kaplowitz N. Contribution of no-reflow phenomenon to hepatic injury after ischemia-reperfusion: Evidence for a role for superoxide anion. Hepatology. 1992;15:507–14. doi: 10.1002/hep.1840150325. [DOI] [PubMed] [Google Scholar]
- 29.Moldeus P, Cotgreave IA, Berggren M. Lung protection by a thiol-containing antioxidant: N-acetylcysteine. Respiration. 1986;50(Suppl 1):31–42. doi: 10.1159/000195086. [DOI] [PubMed] [Google Scholar]
- 30.Look MP, Rockstroh JK, Rao GS, Barton S, Lemoch H, Kaiser R, et al. Sodium selenite and n-acetylcysteine in antiretroviral-naive hiv-1-infected patients: A randomized, controlled pilot study. Eur J Clin Invest. 1998;28:389–97. doi: 10.1046/j.1365-2362.1998.00301.x. [DOI] [PubMed] [Google Scholar]
- 31.Staal FJ, Ela SW, Roederer M, Anderson MT, Herzenberg LA. Glutathione deficiency and human immunodeficiency virus infection. Lancet. 1992;339:909–12. doi: 10.1016/0140-6736(92)90939-z. [DOI] [PubMed] [Google Scholar]
- 32.Nagasaki H, Nakano H, Boudjema K, Jaeck D, Alexandre E, Baek Y, et al. Efficacy of preconditioning with n-acetylcysteine against reperfusion injury after prolonged cold ischaemia in rats liver in which glutathione had been reduced by buthionine sulphoximine. Eur J Surg. 1998;164:139–46. doi: 10.1080/110241598750004805. [DOI] [PubMed] [Google Scholar]
- 33.Knight KR, MacPhadyen K, Lepore DA, Kuwata N, Eadie PA, O’Brien BM. Enhancement of ischaemic rabbit skin flap survival with the antioxidant and free-radical scavenger n-acetylcysteine. Clin Sci (Lond) 1991;81:31–6. doi: 10.1042/cs0810031. [DOI] [PubMed] [Google Scholar]
- 34.Akhgari M, Abdollahi M, Kebryaeezadeh A, Hosseini R, Sabzevari O. Biochemical evidence for free radical-induced lipid peroxidation as a mechanism for subchronic toxicity of malathion in blood and liver of rats. Hum Exp Toxicol. 2003;22:205–11. doi: 10.1191/0960327103ht346oa. [DOI] [PubMed] [Google Scholar]
- 35.Kumar O, Sugendran K, Vijayaraghavan R. Oxidative stress associated hepatic and renal toxicity induced by ricin in mice. Toxicon. 2003;41:333–8. doi: 10.1016/s0041-0101(02)00313-6. [DOI] [PubMed] [Google Scholar]
- 36.Tafazoli S, Spehar DD, O’Brien PJ. Oxidative stress mediated idiosyncratic drug toxicity. Drug Metab Rev. 2005;37:311–25. doi: 10.1081/dmr-55227. [DOI] [PubMed] [Google Scholar]
- 37.Cuzzocrea S, Reiter RJ. Pharmacological action of melatonin in shock, inflammation and ischemia/reperfusion injury. Eur J Pharmacol. 2001;426:1–10. doi: 10.1016/s0014-2999(01)01175-x. [DOI] [PubMed] [Google Scholar]
- 38.Reiter RJ, Acuna-Castroviejo D, Tan DX, Burkhardt S. Free radical-mediated molecular damage. Mechanisms for the protective actions of melatonin in the central nervous system. Ann N Y Acad Sci. 2001;939:200–15. [PubMed] [Google Scholar]
- 39.Ischiropoulos H, Beckman JS. Oxidative stress and nitration in neurodegeneration: Cause, effect, or association? J Clin Invest. 2003;111:163–9. doi: 10.1172/JCI17638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weiss SJ, Ward PA. Immune complex induced generation of oxygen metabolites by human neutrophils. J Immunol. 1982;129:309–13. [PubMed] [Google Scholar]
- 41.Heinzelmann M, Mercer-Jones MA, Passmore JC. Neutrophils and renal failure. Am J Kidney Dis. 1999;34:384–99. doi: 10.1016/s0272-6386(99)70375-6. [DOI] [PubMed] [Google Scholar]
- 42.Zimmerman BJ, Grisham MB, Granger DN. Role of oxidants in ischemia/reperfusion-induced granulocyte infiltration. Am J Physiol. 1990;258:G185–90. doi: 10.1152/ajpgi.1990.258.2.G185. [DOI] [PubMed] [Google Scholar]
- 43.Bonventre JV, Weinberg JM. Recent advances in the pathophysiology of ischemic acute renal failure. J Am Soc Nephrol. 2003;14:2199–210. doi: 10.1097/01.asn.0000079785.13922.f6. [DOI] [PubMed] [Google Scholar]
- 44.Decker K. Biologically active products of stimulated liver macrophages (kupffer cells) Eur J Biochem. 1990;192:245–61. doi: 10.1111/j.1432-1033.1990.tb19222.x. [DOI] [PubMed] [Google Scholar]
- 45.Araki H, Lefer AM. Cytoprotective actions of prostacyclin during hypoxia in the isolated perfused cat liver. Am J Physiol. 1980;238:H176–81. doi: 10.1152/ajpheart.1980.238.2.H176. [DOI] [PubMed] [Google Scholar]
- 46.Sindram D, Porte RJ, Hoffman MR, Bentley RC, Clavien PA. Synergism between platelets and leukocytes in inducing endothelial cell apoptosis in the cold ischemic rat liver: A kupffer cell-mediated injury. FASEB J. 2001;15:1230–2. doi: 10.1096/fj.00-0554fje. [DOI] [PubMed] [Google Scholar]
- 47.Greig PD, Woolf GM, Abecassis M, Forster J, Strasberg SM, Taylor BR, et al. Prostaglandin e1 for primary nonfunction following liver transplantation. Transplant Proc. 1989;21:3360–1. [PubMed] [Google Scholar]
- 48.Totsuka E, Todo S, Zhu Y, Ishizaki N, Kawashima Y, Jin MB, et al. : Attenuation of ischemic liver injury by prostaglandin e1 analogue, misoprostol, and prostaglandin i2 analogue, op-41483. J Am Coll Surg. 1998;187:276–86. doi: 10.1016/s1072-7515(98)00179-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Suzuki S, Nakamura S, Koizumi T, Sakaguchi S, Baba S, Muro H, et al. The beneficial effect of a prostaglandin i2 analog on ischemic rat liver. Transplantation. 1991;52:979–83. doi: 10.1097/00007890-199112000-00008. [DOI] [PubMed] [Google Scholar]
- 50.Russell WJ, Jackson RM. Mnsod protein content changes in hypoxic/hypoperfused lung tissue. Am J Respir Cell Mol Biol. 1993;9:610–6. doi: 10.1165/ajrcmb/9.6.610. [DOI] [PubMed] [Google Scholar]
- 51.Manson PN, Anthenelli RM, Im MJ, Bulkley GB, Hoopes JE. The role of oxygen-free radicals in ischemic tissue injury in island skin flaps. Ann Surg. 1983;198:87–90. doi: 10.1097/00000658-198307000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Manson PN, Narayan KK, Im MJ, Bulkley GB, Hoopes JE. Improved survival in free skin flap transfers in rats. Surgery. 1986;99:211–5. [PubMed] [Google Scholar]
- 53.Stewart JR, Blackwell WH, Crute SL, Loughlin V, Greenfield LJ, Hess ML. Inhibition of surgically induced ischemia/reperfusion injury by oxygen free radical scavengers. J Thorac Cardiovasc Surg. 1983;86:262–72. [PubMed] [Google Scholar]
- 54.Yang H, Majno P, Morel P, Toso C, Triponez F, Oberholzer J, et al. Prostaglandin e (1) protects human liver sinusoidal endothelial cell from apoptosis induced by hypoxia reoxygenation. Microvasc Res. 2002;64:94–103. doi: 10.1006/mvre.2002.2404. [DOI] [PubMed] [Google Scholar]


