Abstract
Background
Curcumin has shown to affect sperm motility and function in vitro and fertility in vivo. The molecular mechanism(s) by which curcumin affects sperm motility has not been delineated. Since modulation of intracellular pH (pHi) and plasma membrane polarization is involved in sperm motility, the present study was conducted to investigate the effect of curcumin on these sperm (human and murine) parameters.
Methods
The effect of curcumin on sperm forward motility was examined by counting percentages of forward moving sperm. The effect of curcumin on intracellular pH (pHi) was measured by the fluorescent pH indicator 2,7-bicarboxyethyl-5,6-carboxyfluorescein-acetoxymethyl ester (BCECF-AM). The effect of curcumin on plasma membrane polarization was examined using the fluorescence sensitive dye bis (1,3-dibarbituric acid)-trimethine oxanol [DiBAC4(3)].
Results
Curcumin caused a concentration-dependent (p<0.05) decrease in forward motility of both human and mouse sperm. It also caused a concentration-dependent decrease in intracellular pH (pHi) in both human and mouse sperm. Curcumin induced significant (p<0.05) hyperpolarization of the plasma membrane in both human and mouse sperm.
Conclusion
These findings indicate that curcumin inhibits sperm forward motility by intracellular acidification and hyperpolarization of sperm plasma membrane. This is the first study to our knowledge which examined the effect of curcumin on sperm pHi and membrane polarization that affect sperm forward motility. These exciting findings will have application in deciphering the signal transduction pathway involved in sperm motility and function and in development of a novel non-steroidal contraceptive for infertility.
Keywords: Contraception, Curcumin, Polarization, Signal transduction, Sperm forward motility, Sperm
Introduction
Curcumin,1,7-bis(4-hydroxy-3-methoxypheny l)- 1- 6- heptadiene- 3, 5-dione, commonly known as diferuloylmethane, is the yellow pigment component of the curry or turmeric (Curcuma longa) (1). Turmeric extracts have been extensively used for the treatment of several diseases in Ayurvedic medicine in India for several centuries. Curcumin was first extracted from turmeric in its impure form in 1815, but it was not until 1910 when it was crystallized and its structure was elucidated (2). It has antimicrobial, antioxidant, immunomodulatory, anti-inflammatory, anti-Alzheimer and anticancer activity (3–8). It has shown no toxicity in vitro in numerous cell culture systems, and in vivo in animal models and over 13 Phase I human clinical trials. It is generally recognized as safe by the United States Food and Drug Administration (FDA) (2, 4, 5).
Curcumin has been shown to affect several targets in somatic cells for its biological activity (3–8). It inhibits NF-ϰB activity, COX-2, and 5-LOX expression and modulates release of several cytokines (3, 4). It also binds to a number of other proteins including thioredoxin reductase, protein kinases and several receptors (3, 4). However, most of these proteins/factors may not be expressed/ present in terminally non-transcriptional sperm. Also, the sperm has a unique characteristic, the motility, that is not present in other cells. Thus, curcumin may have different molecules/ mechanism(s) for its action that are unique to sperm.
Recently, our laboratory reported, for the first time ever, that the curcumin affects sperm function (motility/capacitation and acrosome reaction/fertilization) in vitro and fertility in vivo. Intravaginal administration of curcumin caused a significant, but reversible reduction in fertility (9). The molecular mechanism(s) by which curcumin inhibits/blocks sperm motility has not been delineated. Since modulation of intracellular pH (pHi) and plasma membrane polarization has been shown to be involved in sperm motility and capacitation/acrosome reaction of several mammalian species (10–21), the present study was conducted to investigate the effect of curcumin on sperm intracellular pH and plasma membrane polarization. It was examined using both human and mouse sperm. It was hypothesized that the curcumin-mediated effect on sperm motility is caused by modulation of pHi and/or membrane polarization. The long-term objective of the study was to understand the molecular mechanism(s) by which curcumin affects sperm motility and function and to develop a novel non-steroidal contraceptive with spermicidal properties.
Methods
Collection of sperm
Human spermatozoa were collected from healthy, fertile men. Semen was liquefied and analyzed for volume, sperm concentration and percent and progressive motility. Only those semen samples that had sperm concentration of >50x106sperm/ml, percent motility of >60%, progressive motility of >+3 (on a scale of 0 to +5), and contamination of immature germ cells and immune cells of <1% were used to collect a pure swim-up sperm population (22). The study was approved by the West Virginia University-Institutional Review Board (IRB) for Human Studies.
Mouse sperm were collected from cauda epididymis and vas deferens of mature BALB/c or CD-1 males. Motile sperm were isolated by the swim-up procedure and washed by centrifugation (500 g, 10 min) with Ham's F-10 medium supplemented with human serum albumin (5 mg/ml) or Modified Sperm Washing Medium™ (Irvine Scientific, Santa Ana, CA, USA). Motile sperm were analyzed for sperm concentration and motility (9). The study was approved by the West Virginia University-Animal Care and Use Committee (ACUC) for animal studies.
Measurement of sperm forward motility
The highly purified form of curcumin (cat. #C27727) was obtained from Sigma-Aldrich (St. Louis, MO, USA). Curcumin was dissolved in dimethylsulf-oxide (DMSO) (25-50 mM stock) and then diluted in medium to the desired concentrations. Sperm treated with medium or equivalent volume of DMSO served as the controls. The effect of curcumin on sperm forward motility was examined by incubating 10-100 μl of sperm suspension (100-250x106 motile sperm/ml) with various concentrations of curcumin (50-400 μM, final concentration) up to 1 hr. The percentage of forward moving sperm was recorded every 5-20 min, before and after incubation. Sperm treated with an equivalent volume of medium or DMSO served as the controls. Each treatment in each experiment was tested in duplicate. Each experiment, including various treatment groups, was performed 3-5 times using sperm from 3-5 men or mice on different days to take care of the inter-individual variation among various sperm specimens from different men and mice.
Measurement of sperm intracellular pH
The intracellular pH (pHi) of human and mouse sperm was measured by fluorescent pH-indicator 2,7-bicarb-oxyethy l-5, 6-carboxyfluorescein- acetoxymethylester (BCECF-AM) (Molecular Probes, Eugene, OR, USA) following the manufacturer's protocol as described by Hamamah et al. (23). BCECF is a neutral lipophilic form of bis-carboxyfluorescein which diffuses freely through the plasma membrane. In the cell, it is hydrolyzed by esterases, releasing the BCECF which is retained within the cytoplasm. The fluorescence intensity of BCECF is dependent upon the pH. The motile sperm, isolated by the swim-up procedure, were centrifuged and the pellet was washed and resuspended in 1 ml of phosphate-buffered saline (PBS, pH=7.4). Sperm (8-15x106/ml) were then loaded with 2 μM BCECF (final concentration) and incubated (37°C, 35 min) in dark. Following incubation, sperm were centrifuged, washed (x2) and resuspended in PBS. For the intracellular pH calibration curve, sperm were loaded with BCECF at various extracellular pHs (pHe; 6.8, 7.0, 7.2, 7.4, 7.6 and 7.8) and then treated with 0.1% Triton-X100. Subsequently, the fluorescence intensity was measured as described below, and the calibration curve was constructed by plotting fluorescence intensity versus extracellular pH (24). Using calibration curve, the fluorescence intensity value for each treatment was converted to its respective intracellular pH.
The fluorescence intensity of BCECF is dependent upon the pH with a maximum response at an excitation of λ=535 nm (F1), while at λ=490 nm (F2), the intensity is independent of pH. The pHi was determined graphically using the ratio F1/F2 from a calibration curve obtained after permeabilization of spermatozoa with 0.1% Triton by measuring the maximum fluorescence intensity after adding NaOH and the minimum after adding HCl. The F1/F2 ratio represents a pseudo-linear function of the pH (23).
To examine the effect of curcumin, BCECF-loaded sperm were incubated (37°C, 5-10 min) with various concentrations of curcumin (50-400 μM) and then washed. The treated/control sperm were transferred into wells (200 μL/well) of a black 96-well microplate and the fluorescence intensity was measured (BioTek Synergy2 Multiplatform automated plate reader) using excitation and emission wavelengths of 490 and 535 nm, respectively. Each treatment in each experiment was tested in duplicate. Each experiment, including various treatment groups, was performed 3-5 times using sperm from 3-5 men or mice on different days to take care of the inter-individual variation among various sperm specimens from different men and mice.
All of the appropriate controls were carefully included as described by the manufacturer. Moreover, it was pertinent to examine the effect of cur-cumin per se on fluorescence intensity. Similar experiments carried out with various concentrations (50-400 μM) of curcumin without sperm did not affect the fluorescence intensity, indicating curcumin per se, without sperm, does not affect fluorescence intensity.
Plasma membrane polarization of human and mouse sperm
The changes in sperm plasma membrane polarization were examined using the fluorescence sensitive dye bis (1,3-dibarbituric acid)-trimethine oxanol [DiBAC4(3)] (Molecular Probes, Eugene, OR, USA) following the manufacturer's protocol as described by Rossato et al. (25). The motile sperm in the swim-up fraction were centrifuged, washed (x2) with PBS and incubated (37° C, 1 hr) with 2 μM DiBAC4(3). DiBAC4(3) can enter depolarized cells and then bind to intracellular proteins or membrane and exhibits enhanced fluorescence. Increased depolarization results in additional influx of the anionic dye and an increase in fluorescence. Conversely, hyperpolarization is indicated by a decrease in fluorescence. This dye is excluded from mitochondria because of their overall negative charge. Sperm (8-15x 106/ml) were then centrifuged and washed twice with PBS. The DiBAC4(3)-incubated sperm were aliquoted in different tubes at equal volumes and incubated (5-10 min) with various concentrations of curcumin (100 μM, 200 μM, 300 μM, and 400 μM). Sperm treated with PBS or equivalent volume of DMSO served as the controls. After final washing with PBS, the sperm were transferred into wells (200 μL/well) of a black 96-well microplate and the fluorescence intensity was measured (BioTek Synergy2 Multiplatform automated plate reader) using excitation and emission wavelengths of 485 and 530 nm, respectively. Each treatment in each experiment was tested in duplicate. Each experiment, including various treatment groups, was performed 3-5 times using sperm from 3-5 men or mice on different days to take care of the inter-individual variation among various sperm specimens from different men and mice.
All the appropriate controls were carefully included as described by the manufacturer. It was pertinent to examine the effect of curcumin per se on fluorescence intensity. Similar experiments carried out with various concentrations (50-400 μM) of curcumin without sperm did not affect the fluorescence intensity, indicating curcumin per se, without sperm, does not affect fluorescence intensity.
Statistical analysis
The significance of difference among various groups was analyzed using analysis of variance (ANOVA) and Tukey Kramer Multiple Comparison Test. A p ≤ 0.05 was considered statistically significant.
Results
Effect of curcumin on human and mouse sperm forward motility
Curcumin caused a concentration-dependent decrease in human sperm forward motility (Table 1). At 50 μM concentration, there was no apparent (p>0.05) effect on sperm forward motility in 5-10 min (with a slight decrease over time) and in 1 hr it decreased by up to ∼25% (p< 0.001). At 100 μM concentration, there was a significant (p<0.001) decrease in sperm forward motility in 5-10 min which decreased by up to ∼80% in 1 hr. At concentrations ≥200 μM, there was a complete block of sperm forward motility within 5-10 min. DMSO vehicle did not affect (p>0.05) sperm forward motility as compared to medium control.
Table 1.
Effect of curcumin on human sperm forward motility (%)*
| Treatment | 0 min | 5-10 min | 20 min | 40 min | 60 min |
|---|---|---|---|---|---|
| Curcumin | |||||
| 50 μM | 95±5 | 91±6 | 85±5 | 80±7 | 72±8** |
| 100 μM | 95±5 | 40±4** | 26±7** | 20±8** | 18±7** |
| 200 μM | 95±5 | 0±0** | 0±0** | 0±0** | 0±0** |
| 300 μM | 95±5 | 0±0** | 0±0** | 0±0** | 0±0** |
| 400 μM | 95±5 | 0±0** | 0±0** | 0±0** | 0±0** |
| DMSO vehicle | |||||
| 95±5 | 95±5 | 95±5 | 95±5 | 93±6 | |
| Medium control | |||||
| 95±5 | 95±5 | 95±5 | 95±5 | 93±6 | |
Mean±SD
Versus control, significantly different (p<0.001); all others non-significant
Curcumin caused a similar effect on mouse sperm forward motility (Table 2). At 50 μM concentration, there was no apparent (p>0.05) effect on sperm forward motility in 5-10 min (with a slight decrease over time) and in 1 hr, it decreased by up to ∼40% (p<0.001). At 100 μM concentration, there was a significant (p<0.001) decrease in sperm forward motility in 5-10 min, which decreased by up to ∼70% in 1 hr. At concentrations ≥200 μM, there was a complete block of forward motility within 5-10 min. DMSO vehicle did not affect (p>0.05) sperm forward motility as compared to the medium control.
Table 2.
Effect of curcumin on murine sperm forward motility (%)*
| Treatment | 0 min | 5-10 min | 20 min | 40 min | 60 min |
|---|---|---|---|---|---|
| Curcumin | |||||
| 50 μM | 92±8 | 85±7 | 80±6 | 71±4 ** | 61±7 ** |
| 100 μM | 92±8 | 42±9 ** | 35±4 ** | 30±6 ** | 28±6 ** |
| 200 μM | 92±8 | 0±0 ** | 0±0 ** | 0±0 ** | 0±0 ** |
| 300 μM | 92±8 | 0±0 ** | 0±0 ** | 0±0 ** | 0±0 ** |
| 400 μM | 92±8 | 0±0 ** | 0±0 ** | 0±0 ** | 0±0 ** |
| DMSO vehicle | |||||
| 92±8 | 92±8 | 92±8 | 90±7 | 85±8 | |
| Medium control | |||||
| 92±8 | 92±8 | 92±8 | 90±7 | 88±7 | |
Mean±SD
Versus control, significantly different (p<0.001); all others non-significant
Effect of curcumin on human and mouse sperm intracellular pH (pHi)
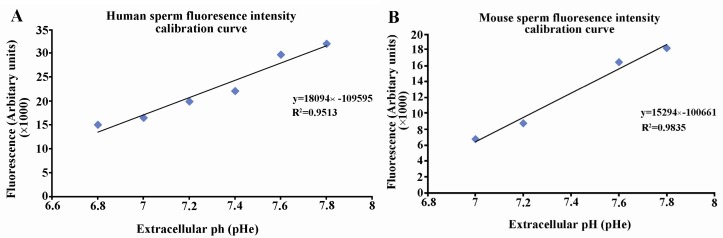
There was a linear relationship between the extracellular pH and the fluorescence intensity both in human (R2=0.9513) and mouse (R2=0.9835) sperm (Figure 1, panel A and B, respectively). With an increase in extracellular pH, there was a corresponding increase in fluorescence intensity. The pH=7.4 was selected in our subsequent experiments to examine the effect of curcumin on intracellular sperm pH (pHi).
Figure 1.
Calibration curve of human (panel A) and mouse (panel B) sperm fluorescence intensity at various extracellular pH. BCECF-loaded sperm were treated with 0.1% Triton-X 100 at various extracellular pH (pHe) and the fluorescence intensity was measured. Fluorescence intensity values were then plotted against pHe values to obtain the calibration curve.
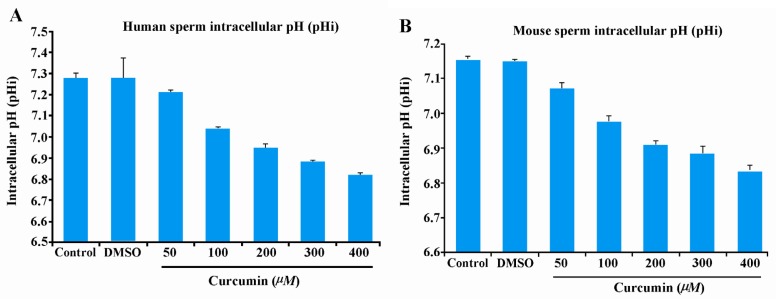
In both human and mouse sperm, curcumin caused a concentration-dependent decrease in intracellular pH (Figure 2), in human (panel A) and mouse (panel B) sperm. In human sperm, control sperm had pHi of 7.3±0.003 which was not significantly different (p>0.05) from DMSO-treated sperm, which had a pHi of 7.3±0.105 (Figure 3, panel A). Treatment with curcumin significantly (p<0.001) decreased intracellular pH in a concentration-dependent manner as compared to control/ DMSO-treated sperm. At 50 μM curcumin concentration, pHi was 7.21±0.010, at 100 μM pHi was 7.04±0.008, at 200 μM pHi was 6.95±0.02, at 300 μM pHi was 6.88±0.0067 and at 400 μM pHi was 6.81±0.014. Comparing the change in pHi within the curcumin-treated groups, the difference was significant (p<0.05) only among 50 μM, 100 μM and 400 μM groups.
Figure 2.
Human (panel A) and mouse (panel B) sperm intracellular pH (pHi) after curcumin treatment. BCEF-loaded sperm were treated with increasing concentrations of curcumin and the fluorescence intensities were measured and converted to intracellular pH using the calibration curve. Intracellular pH (pHi) values (Mean±SE) from 3-5 independent experiments using sperm from 3-5 different men and mice are shown. There was no effect of any concentration of curcumin tested per se on fluorescence intensity without sperm.
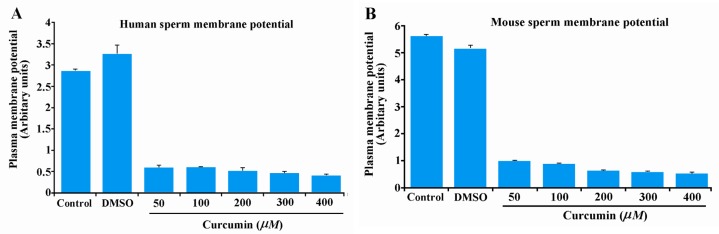
Figure 3.
Effect of curcumin on plasma membrane potential in human (panel A) and mouse (panel B) sperm. Fluorescence intensity values (Mean±SE) from 3-5 independent experiments using sperm from 3-5 different men and mice are shown. Fluorescence intensity values lower than the control indicate hyperpolarization. There was no effect of any concentration of curcumin tested per se on fluorescence intensity without sperm.
Similar results were obtained in mouse sperm (Figure 2, panel B). In mouse sperm, control sperm had pHi of 7.15±0.005 which was not significantly different (p>0.05) from DMSO-treated sperm which had a pHi of 7.15±0.00 (Figure 2, panel B). Treatment with curcumin significantly (p<0.001) decreased intracellular pH in a concentration-dependent manner as compared to control/DMSO-treated sperm. At 50 μM curcumin concentration, pHi was 7.07±0.017, at 100 μM pHi was 6.97±0.017, at 200 μM pHi was 6.91± 0.012, at 300 μM pHi was 6.88±0.02 and at 400 μM pHi was 6.83±0.017. Comparing the changes in pHi within the curcumin-treated groups, the difference was significant (p<0.05) only among 50 μM, 100 μM and 400 μM groups.
Effect of curcumin on human and mouse sperm plasma membrane polarization
The effect of various concentrations of curcumin on plasma membrane polarization was evaluated using both human and mouse sperm. In human sperm, treatment with DMSO did not significantly (p>0.05) affect fluorescence intensity as compared to control sperm (control: 2861±43.016; DMSO: 3252± 215.860) (Figure 3, panel A). Treatment with curcumin caused significant (p<0.001) hyperpolarization of sperm plasma membrane as compared to control/DMSO-treated sperm (Figure 3, panel A). At 50 μM curcumin, fluorescence intensity were 601±51.052, at 100 μM, 597±20.664, at 200 μM, 522±72.421, at 300 μM, 458±47.576 and at 400 μM 414±29.464. Comparing the changes in fluorescence intensities within the curcumin-treated groups, the differences were not-significant.
Similar results were obtained in mouse sperm (Figure 3, panel B). In mouse sperm, treatment with DMSO did not significantly affect fluorescence intensity as compared to control (control: 5592.085±2.186; DMSO: 5130.905±130.770) (Figure 3, panel B). Treatment with curcumin caused significant (p<0.001) hyperpolarization of sperm plasma membrane as compared to control/DMSO-treated sperm (Figure 3, panel B). At 50 μM curcumin, fluorescence intensity was 997.502±22.229, at 100 μM was 877.356±41.328, at 200 μM was 624.331±42.116, at 300 μM was 578.929±43.245 and at 400 μM was 522.431±57.900. Comparing the changes in fluorescence intensity within the curcumin-treated groups, the difference was significant (p<0.05) only between 50 μM and 400 μM groups.
Discussion
The data indicated that curcumin affects sperm forward motility starting at 100 μM concentration, with a complete block at ≥200 μM concentration within 5-10 min in both human and murine sperm. These findings correlate well with the earlier published data (9). In general, forward motility corresponded well with overall motility and progressive motility, as a decrease in forward motility corresponded with decrease in overall and progressive motility. Also, there was a loss of sperm viability when there was a decrease in forward motility. The totally immotile sperm were completely non-viable as tested by eosin-nigrosin staining (data not shown).
The present study was conducted to examine the mechanism by which curcumin affects sperm forward motility. The findings indicated that curcumin acidified sperm intracellularly and hyperpolarized cell membrane of both human and mouse sperm. There was a concentration-dependent decrease in pHi from 7.3 to 6.81 at highest concentration (400 μM) of curcumin tested. These findings correlate well with the effect of curcumin on human and murine sperm forward motility. Starting at 100 μM concentration, there was a significant effect within 5-10 min, with a total block at ≥200 μM concentration. All the human and murine sperm samples tested demonstrated a similar phenotype. DMSO vehicle did not affect the pHi.
The pHi plays an important role in modulating mammalian sperm motility (12, 17, 20). These cumulative findings indicate that the acidic pHi inhibits sperm motility, which is in agreement with our findings. The pHi of 6.6-6.8 has been reported in one study for uncapacitated murine sperm (13). In this study, the pHi of control murine sperm was slightly higher, ∼7.15. This may be due to different methodologies/media and/or the strain of mice used and/or various degrees of capacitation of sperm preparations. The pHi of 7.25 was observed for control human sperm in this study. This is in agreement with a previous published study (24). The sodium-proton membrane exchange mechanism can modulate pHi and affect motility (26). The pHi changes are also involved in sperm motility as the sperm cell passes through the epididymis (27, 28). Also, the pH of the epididymal cauda fluid is acidic in almost all species (29) and acts directly on the pHi to decrease the sperm motility (28). Our extensive data search in PubMed and Google Scholar did not yield any publication which has examined the effect of curcumin on intracellular pH in sperm or any other cell types.
Curcumin caused hyperpolarization of sperm plasma membrane in both human and mouse sperm. The degree of decrease in intracellular florescence intensity is indicative of the degree of hyperpolarization. Hyperpolarization is a change which makes cell's membrane potential more negative. It is the opposite of depolarization. The change in sperm membrane potential has been shown to be involved in sperm motility and function (18, 19, 21, 24, 25, 28, 30–33). For mouse sperm, intracellular alkalinization produces a hyperpolarization of sperm membrane potential which may be important for both hyperactivated motility and acrosome reaction. In this study, curcumin induced hyperpolarization and intracellular acidification which correlate with a reduction/block of sperm motility. There was more drastic effect on hyperpolarization than on change in pHi. At 50 μM concentration, which did not significantly decrease the pHi, it showed a significant effect on membrane polarization in both human and mouse sperm. It is possible that curcumin may affect pHi and membrane potential by interacting with different molecules and signal transduction cascades. Besides sperm, hyperpolarization has also been connected to intracellular pHi changes in several other cell systems (34).
Although there is no publication which has examined the effect on sperm, curcumin has been reported to affect membrane potential in other cell systems. Curcumin affects plasma membrane permeability of rat thymocytes (35). Curcumin inhibits sarco/endoplasmic reticulum Ca++ATPase (Ser CA) pump that has a major role in maintaining lower levels of intracellular [Ca++] by importing extracellular protons in rabbit skeleton muscle (36). A study by Cao et al. (37) examined the effect of curcumin on changes in mitochondrial membrane potential in human hepatomaG2 (HepG2) cells. Their study showed that HepG2 cells incubated with curcumin induced oxidative damage to mitochondrial DNA through mitochondrial membrane hyperpolarization.
Several molecules/mechanisms are involved in regulation of sperm intracellular pH and membrane polarization. Sodium-hydrogen exchange has been suggested as a mediator of pH regulation in various mammalian sperm (27, 38, 39). At least two sodium-hydrogen exchangers (NHE1 and NHE5) have been shown to be expressed in spermatozoa. The catalytic subunit of protein kinase A (PKA) is involved in activation of motility evoked by HCO3 - anion (40). Capacitation-associated hyperpolarization involves a decrease in intracellular [Na+] regulated by PKA through activation of the cystic fibrosis transmembrane conductance regulator (CFTR) (41). Alkalinization activates the intracellular pH-sensitive I(KSper), inducing the membrane potential to approach negative potentials where Ca2+ entry via I(CatSper) is maximized (33, 42). The exact molecular mechanism(s) and signal transduction pathway involved in modulation of sperm intracellular pH and membrane potential by curcumin need further investigation. There are several mechanisms that can affect sperm motility/function leading to infertility (43, 44). This preliminary data indicates that curcumin may inhibit tyrosine phosphorylation of a subset of sperm surface proteins and Ca2+ channels (unpublished data). Tyrosine phosphorylation has been shown to be involved in sperm motility, capacitation/acrosome reaction and function (16).
Conclusion
The findings indicate that curcumin causes intracellular acidification and membrane hyperpolarization which may be involved in inhibiting sperm forward motility. This is the first study to our knowledge that examined the effect of curcumin on sperm pHi and membrane potential. These exciting findings will have application in deciphering the molecular mechanism(s) involved in curcumin action and in delineating the signal transduction pathway relevant to sperm motility and function. Also, this data may have clinical application in development of a novel non-steroid contraceptive with spermicidal properties.
Acknowledgement
We sincerely thank Bidur Paudel, Morgan Lough, Clara Beth Novotny, and Vanessa Cuppett for performing several of these experiments and their help in data analysis and excellent typing assistance. We also thank Don Zeh and Melanie Clemmer, Ph.D., at the Andrology Laboratory at the Center for Reproductive Medicine at West Virginia University for help in consenting men for providing semen specimens used in this study. This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
To cite this article: Naz RK. The Effect of Curcumin on Intracellular pH (pHi), Membrane Hyperpolarization and Sperm Motility. J Reprod Infertil. 2014;15(2):62-70.
Conflict of Interest
The author reports no conflict of interest.
References
- 1.Tayyem RF, Heath DD, Al-Delaimy WK, Rock CL. Curcumin content of turmeric and curry powders. Nutr Cancer. 2006;55(2):126–31. doi: 10.1207/s15327914nc5502_2. [DOI] [PubMed] [Google Scholar]
- 2.Singh S. From exotic spice to modern drug? Cell. 2007;130(5):765–8. doi: 10.1016/j.cell.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 3.Sharma RA, Gescher AJ, Steward WP. Curcumin: the story so far. Eur J Cancer. 2005;41(13):1955–68. doi: 10.1016/j.ejca.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 4.Aggarwal BB, Sundaram C, Malani N, Ichikawa H. Curcumin: The Indian solid gold. Adv Exp Med Biol. 2007;595:1–75. doi: 10.1007/978-0-387-46401-5_1. [DOI] [PubMed] [Google Scholar]
- 5.Corson TW, Crews CM. Molecular understanding and modern application of traditional medicines: Triumphs and trials. Cell. 2007;130(5):769–74. doi: 10.1016/j.cell.2007.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta SC, Patchva S, Koh W, Aggarwal BB. Discovery of curcumin, a component of the golden spice, and its miraculous biological activities. Clin Exp Pharmacol Physiol. 2013;39:283–99. doi: 10.1111/j.1440-1681.2011.05648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yallapu MM, Ebeling MC, Jaggi M, Chauhan SC. Plasma proteins interaction with curcumin nanoparticles: implications in cancer therapeutics. Curr Drug Metab. 2013;14(4):504–15. doi: 10.2174/1389200211314040012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yallapu MM, Jaggi M, Chauhan SC. Curcumin nano-medicine: a road to cancer therapeutics. Curr Pharm Des. 2013;19(11):1994–2010. doi: 10.2174/138161213805289219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Naz RK. Can curcumin provide an ideal contraceptive? Mol Reprod Dev. 2011;78(2):116–23. doi: 10.1002/mrd.21276. [DOI] [PubMed] [Google Scholar]
- 10.Garbers DL, Watkins HD, Hansbrough JR, Smith A, Misono KS. The amino acid sequence and chemical synthesis of speract and speract analogues. J Biol Chem. 1981;257(6):2734–7. [PubMed] [Google Scholar]
- 11.Babcock DF, Rufo GA, Jr, Lardy HA. Potassium-dependent increases in cytosolic pH stimulate metabolism and motility of mammalian sperm. Proc Natl Acad Sci USA. 1983;80(5):1327–31. doi: 10.1073/pnas.80.5.1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Babcock DF, Pfeiffer DR. Independent elevation of cytosolic [Ca2+] and pH of mammalian sperm by voltage-dependent and pH-sensitive mechanisms. J Biol Chem. 1987;262(31):15041–7. [PubMed] [Google Scholar]
- 13.Zeng Y, Oberdorf JA, Florman HM. pH regulation in mouse sperm: identification of Na(+)-, Cl(-)-, and HCO3(-)-dependent and arylaminobenzoate-dependent regulatory mechanisms and characterization of their roles in sperm capacitation. Dev Biol. 1996;173(2):510–20. doi: 10.1006/dbio.1996.0044. [DOI] [PubMed] [Google Scholar]
- 14.Hamamah S, Gatti JL. Role of the ionic environment and internal pH on sperm activity. Hum Reprod. 1998 Dec;13(Suppl 4):20–30. doi: 10.1093/humrep/13.suppl_4.20. [DOI] [PubMed] [Google Scholar]
- 15.Darszon A, Iabarca P, Nishigaki T, Espinosa F. Ion channels in sperm physiology. Physiol Rev. 1999;79(2):481–510. doi: 10.1152/physrev.1999.79.2.481. [DOI] [PubMed] [Google Scholar]
- 16.Naz RK, Rajesh PB. Role of tyrosine phosphorylation in sperm capacitation/acrosome reaction. Reprod Biol Endocrinol. 2004;2:75. doi: 10.1186/1477-7827-2-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gagnon C, de Lamirande E, Jonge CD, Barratt C, editors. Cambridge: Cambridge University Press; 2006. Controls of sperm motility; p. 108. The Sperm Cell. [Google Scholar]
- 18.Zeng XH, Yang C, Kim ST, Lingle CJ, Xia XM. Deletion of the Slo3 gene abolishes alkalization-activated K+ current in mouse spermatozoa. Proc Natl Acad Sci USA. 2011;108(14):5879–84. doi: 10.1073/pnas.1100240108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De La Vega-Beltran JL, Sanchez-Cardenas C, Krapf D, Hernandez-Gonzalez EO, Wertheimer E, Trevino CL, et al. Mouse sperm membrane potential hyperpolarization is necessary and sufficient to prepare sperm for the acrosome reaction. J Biol Chem. 2012;287(53):44384–93. doi: 10.1074/jbc.M112.393488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lishko PV, Kirichok Y, Ren D, Navarro B, Chung JJ, Clapham DE. The control of male fertility by spermatozoan ion channels. Ann Rev Physiol. 2012;74:453–75. doi: 10.1146/annurev-physiol-020911-153258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chavez JC, de la Vega-Beltran JL, Escoffier J, Visconti PE, Trevino CL, Darszon A, et al. Ion perme-abilities in mouse sperm reveal an external trigger for Slo3-dependent hyperpolarization. PLoS One. 2013;8(4):60578. doi: 10.1371/journal.pone.0060578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Samuel AS, Naz RK. Isolation of human single chain variable fragment antibodies against specific sperm antigens for immunocontraceptive development. Hum Reprod. 2008;23(6):1324–37. doi: 10.1093/humrep/den088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamamah S, Magnoux E, Royere D, Barthelemy C, Dacheux JL, Gatti JL. Internal pH of human spermatozoa: effect of ions, human follicular fluid and progesterone. Mol Hum Reprod. 1996;2(4):219–24. doi: 10.1093/molehr/2.4.219. [DOI] [PubMed] [Google Scholar]
- 24.Jain R, Jain A, Kumar R, Verma V, Mikhuri JP, Sharma VL, et al. Functional attenuation of human sperm by novel, non-surfactant spermicides: precise targeting of membrane physiology without affecting structure. Hum Reprod. 2010;25(5):1165–76. doi: 10.1093/humrep/deq036. [DOI] [PubMed] [Google Scholar]
- 25.Rossato M, Di Virgilio F, Rizzuto R, Galeazzi C, Foresta C. Intracellular calcium store depletion and acrosome reaction in human spermatozoa: role of calcium and plasma membrane potential. Mol Hum Reprod. 2001;7(2):119–28. doi: 10.1093/molehr/7.2.119. [DOI] [PubMed] [Google Scholar]
- 26.Wong PYD, Lee WM, Tsang AYF. The effects of extracellular sodium on acid release and motility initiation in rat caudal epididymal spermatozoa in vitro. Exp Cell Res. 1981;131(1):97–104. doi: 10.1016/0014-4827(81)90410-9. [DOI] [PubMed] [Google Scholar]
- 27.Carr DW, Acott TS. Intracellular pH regulates bovine sperm motility and protein phosphorylation. Biol Reprod. 1989;41(5):907–20. doi: 10.1095/biolreprod41.5.907. [DOI] [PubMed] [Google Scholar]
- 28.Gatti JL, Billard R, Christen R. Ionic regulation of the plasma membrane potential of rainbow trout (Salmo gairdneri) sperm: role in the inititation of motility. J Cell Physiol. 1990;143(3):546–54. doi: 10.1002/jcp.1041430320. [DOI] [PubMed] [Google Scholar]
- 29.Setchell BP, Maddocks S, Brooks DE, Knobil E, Neill JD, editors. Vol. 1. New York: Raven Press; 1994. Anatomy, vasculature, innervation, and fluids of the male reproductive tract; p. 1063. The Physiology of Reproduction. [Google Scholar]
- 30.Brewis IA, Morton IE, Mohammad SN, Browes CE, Moore HD. Measurement of intracellular calcium concentration and plasma membrane potential in human spermatozoa using flow cytometry. J Androl. 2000;21(2):238–49. [PubMed] [Google Scholar]
- 31.Patrat C, Serres C, Jouannet P. Induction of a sodium influx by progesterone in human spermatozoa. Biol Reprod. 2000;62(5):1380–6. doi: 10.1095/biolreprod62.5.1380. [DOI] [PubMed] [Google Scholar]
- 32.Patrat C, Serres C, Jouannet P. Progestrone induces hyperpolarization after a transient depolarization phase in human spermatozoa. Biol Reprod. 2002;66(6):1775–80. doi: 10.1095/biolreprod66.6.1775. [DOI] [PubMed] [Google Scholar]
- 33.Navarro B, Kirichok Y, Clapham DE. KSper, a pH sensitive K+ current that controls sperm membrane potential. Proc Natl Acad Sci USA. 2007;104(18):7688–92. doi: 10.1073/pnas.0702018104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gresik M, Kolarova N, Farkas V. Hyperpolarization and intracellular acidification in Trichoderma viride as a response to illumination. J Gen Microbiol. 1991;137(11):2605–9. doi: 10.1099/00221287-137-11-2605. [DOI] [PubMed] [Google Scholar]
- 35.Jaruga E, Salvioli S, Dobrucki J, Chrul S, Bandorowicz-Pikula J, Sikora E, et al. Apoptosis-like, reversible changes in plasma membrane asymmetry and permeability, and transient modifications in mitochondrial membrane potential induced by curcumin in rat thymocytes. FEBS Lett. 1998;433(3):287–93. doi: 10.1016/s0014-5793(98)00919-3. [DOI] [PubMed] [Google Scholar]
- 36.Bilmen JG, Khan S, Javed MH, Michelangeli F. Inhibition of the SERCA Ca2+ pumps by curcumin. Curcumin putatively stabilizes the interaction between the nucleotide-binding and phosphorylation domains in the absence of ATP. Eur J Biochem. 2001;268(23):6318–27. doi: 10.1046/j.0014-2956.2001.02589.x. [DOI] [PubMed] [Google Scholar]
- 37.Cao J, Liu Y, Jia J, Zhou HM, Kong Y, Yang G, et al. Curcumin induces apoptosis through mitochondrial hyperpolarization and mtDNA damage in human hepatoma G2 cells. Free Radic Biol Med. 2007;43(6):968–75. doi: 10.1016/j.freeradbiomed.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 38.Schackmann RW, Chock PB. Alteration of intracellular [Ca2+] in sea urchin sperm by the egg peptide speract. Evidence that increased intracellular Ca2+ is coupled to Na+ entry and increased intracellular pH. J Biol Chem. 1986;261(19):8719–28. [PubMed] [Google Scholar]
- 39.Garcia MA, Meizel S. Regulation of intracellular pH in capacitated human spermatozoa by a Na+/ H+ exchanger. Mol Reprod Dev. 1999;52(2):189–95. doi: 10.1002/(SICI)1098-2795(199902)52:2<189::AID-MRD10>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 40.Morgan DJ, Weisenhaus M, Shum S, Su T, Zheng R, Zhang C, et al. Tissue specific PKA inhibition using a chemical genetic approach and its application to studies on sperm capacitation. Proc Natl Acad Sci USA. 2008;105(52):20740–5. doi: 10.1073/pnas.0810971105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Escoffier J, Krapf D, Navarrete F, Darszon A, Visconti PE. Flow cytometry analysis reveals a decrease in intracellular sodium during sperm capacitation. J Cell Sci. 2012;125(Pt 2):473–85. doi: 10.1242/jcs.093344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McPartlin LA, Visconti PE, Bedford-Guaus SJ. Guaninenucleotide exchange factors (RAPGEF3/RAPGEF4) induce sperm membrane depolarization and acrosomal exocytosis in capacitated stallion sperm. Biol Reprod. 2011;85(1):179–88. doi: 10.1095/biolreprod.110.085555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ohl DA, Naz RK. Infertility due to antisperm antibodies. Urology. 1995;46(4):591–602. doi: 10.1016/S0090-4295(99)80282-9. [DOI] [PubMed] [Google Scholar]
- 44.Sikka SC. Role of oxidative stress and antioxidants in andrology and assisted reproductive technology. J Androl. 2004;25(1):5–18. doi: 10.1002/j.1939-4640.2004.tb02751.x. [DOI] [PubMed] [Google Scholar]