Abstract
Background
Preterm birth is a major health problem that leads to infant morbidity and mortality. The main goal of this study was to find the relationship between social determinants of health and preterm delivery.
Methods
A prospective longitudinal cohort study was carried out on 500 pregnant women in their 24th to 28th gestational weeks in 2012. The pregnant women filled out a self-report questionnaire on the structural determinant, perceived stress, and perceived social support. The participants were followed up until labor and the data about mother and the newborn were collected after labor. The data were analyzed by SPSS 21 and Lisrel 8.8 software programs using pathway analysis.
Results
The final path model fit well (CFI=0.96; RMSEA=0.060). Path analysis showed that among structural factors, income had a direct effect (β=0.06) and the factors of income (β=0.00594), number of children (family size) (β=-0.024), as well as mother's education (β=-0.0084) had the greatest overall effect on gestational age at birth respectively. Also, the results showed that among intermediate factors of social determinants of health, stress in the direct path (β=-0.12) and among the overall effects, the perceived stress (β=-0.12) and perceived social support (β=0.0396) affected the gestational age at birth.
Conclusion
The current study showed that some structural and intermediary determinants such as income and perceived stress had an effect on preterm labor.
Keywords: Intermediary determinants of health, Perceived social support, Perceived stress, Structural determinants of health
Introduction
Preterm birth (PTB) is a global health problem that leads to infant morbidity and mortality (1, 2). Preterm birth (PTB), the birth of an infant prior to 37 completed weeks of gestation, poses an economic burden to family and the state of residence.
The prevalence of preterm delivery in different countries is estimated to be 5 to 13% (3–5). In Iran, the prevalence has been reported between 5.6-34.9% (6). Preterm birth is responsible for 75-90% of all neonatal deaths, prenatal deaths and is a major cause of short and long term neonatal damages (7).
Prematurity has short and long-term complications which include respiratory distress syndrome, dysplasia, anemia, fatigue, kernicterus, intraven-tricular hemorrhage, bleeding into or around the abdominal, bacterial or fungal sepsis, retinopathy, necrotizing enterocolitis, learning and behavioral and cognitive problems (low IQ), mental retardation, blindness, hearing loss, and developmental problems (8–10).
Although technological advances have led to greater survival of preterm infants, morbidity still remains rather high, imposing greater emotional and financial burden on families and the health care system (11).
Studies have identified numerous physiological and psychological risk factors in preterm births including black race, ages below 17 and over 35, low education, poor socio-economic status, poor access to prenatal care, physical abuse, nutritional status, long working hours, psychological characteristics, infection, previous preterm birth, incorrect behaviors (smoking, alcohol and drug abuse), uterine abnormalities, violence and abuse, stress, depression, increased risk of unwanted pregnancies and reduced level of social and financial support, habitat and stressful jobs (1, 10, 12, 13).
All factors are identified as risk factors in societies with low Socioeconomic Status (SES) (14). Despite improvements in standards of life, health care, diagnostic and treatment technologies, causes of two thirds of preterm births are still unknown. Yet, risk factors cannot appropriately predict for whom preterm birth may occur (15).
Since higher preterm rates are observed in poorer societies, it seems that causes should be sought in biological and socio-psychological factors. Today, researchers believe that preterm labor is not merely a disease, but it is a syndrome that may have one or more causes (12). More recent views of scholars emphasize on the role of demographic and health factors.
Various models have been proposed to explain the mechanism of determinants’ effects on healthy pregnancy outcomes. According to Townsend et al.'s model, different birth outcomes are due to the difference in power struggle between social classes. Given this concept, material inequalities such as income differences, people's working conditions, habitats, access to health care facilities and exposure to physical harm, all may affect birth outcomes (16).
These factors may directly or indirectly affect birth outcomes through maternal health behavior and lifestyle. The studies demonstrate that in poor socio-economic conditions, incorrect health behaviors, improper use of prenatal care, poor nutrition, anemia and other maternal diseases, will lead to greater drug abuse and greater obstetric complications such as miscarriage, stillbirth and premature labor. Poor housing, low maternal education and low income are significantly associated with preterm labor (17–20).
Other models emphasize on the direct role of intermediary health determinants in pregnancy outcomes and believe that structural factors are not directly influential, but affect health outcomes through intermediary factors.
In the socio-psychological model, it is stated that social status affects an individual's feelings and this in turn affects her health. It is also believed that different birth outcomes among different socio-economic groups are created by relevant socio-psychological stressors (21). Various investigations on intermediary social determinants indicate that preterm labor is associated with stressful life events, anxiety, depression, stressful jobs and physical abuse (22, 23).
In spite of all the information in this area, health determinant communication routes are still unknown in incidence of adverse pregnancy outcomes. Thus, this study was conducted to determine the relationship between structural and intermediary health determinants and incidence of preterm birth using path analysis. The aim of this paper was to use a new statistical framework for analysis based on path analysis techniques for showing the relationship between structural and intermediary determinants of health and preterm delivery.
Methods
A prospective longitudinal cohort study was carried out among 500 pregnant women from July 2011 to February 2012. In the first sampling stage, city of Tehran was divided into 4 geographical classes; North, South, East, and West (stratified sampling) and then, one public hospital was chosen from each class and 500 pregnant (24-28 weeks) women from these hospitals were randomly selected. After explaining study objectives, if they met study inclusion criteria, informed consents were obtained from pregnant women and their spouses. Then, initial interviews were conducted and the birth date was determined by the first day of the last menstrual cycle as disclosed by the mother, if unknown, and then first trimester ultrasound was used. Questionnaires were completed during 24-28 weeks of pregnancy to assess structural and intermediate determinants. The subjects were divided based on the determinants (In general, individual's socioeconomic status, perceived stress and perceived social support) and subjects were followed up until labor, near the estimated delivery time. Next the subjects were contacted and asked about the exact date of delivery and the hospital where it occurred. Some information about the delivery was also asked on the phone and then complete information was taken from hospital records and eventually, pregnancy was studied in two groups (preterm labor and term labor). To determine the required sample size, after review of literature and considering the 10% prevalence of preterm birth and accounting for study variables, 3 to 10 subjects were selected for each variable (24). The tools used in the study were questionnaires that included some structural determinants (socio-economic status), and also some intermediary determinants (perceived social support, perceived stress). Questionnaires were completed by a specially trained team of people.
Participants
In this study, women with gestational age between 24-28 weeks, with singleton pregnancy, without history of known medical problems both during and before pregnancy such as cardiovascular diseases, diabetes, kidney disorders, respiratory disorders, autoimmune diseases, and also in a previous pregnancy with problems such as pre-eclampsia, diabetes, premature delivery, intrauterine growth retardation (IUGR), fetal death, premature rupture of fetal membranes (PROM), placental abruption or polyhydramnios were selected. The women with incidence of pre-eclampsia, diabetes, IUGR, fetal death, PROM, placental abruption, and polyhydramnios in the current pregnancy were excluded.
To determine the structural determinants of health status of participants, a questionnaire was designed including income, the education level of pregnant women, the education level of the spouse, residential area, number of people in households, and cost per square meter of their house.
Of 550 subjects, 24 did not meet the inclusion criteria and 11 were not willing to continue. During the follow-up, the address and telephone number of 10 subjects changed and 5 subjects were eliminated due to fetal death and malformations. Therefore, finally data analysis was performed on 500 subjects.
In obstetric questionnaire, mother's age (based on date of birth), marital status, number of pregnancies and deliveries (gravid/para), number of abortions and stillbirths, planned pregnancy (in view of the pregnant women and their husbands), history of problems in previous and current pregnancy were extracted from the obstetrical records of the pregnant women.
To determine the intermediary determinants of health status of participants, 2 questionnaires were used, perceived stress questionnaire and perceived social support.
Perceived stress questionnaire
PSS-14 questionnaire was prepared by Cohen et al. in 2004 and used to assess general perceived stress in the past month. Thoughts and feelings about stressful events, control of overcoming and dealing with psychological pressure and experienced stresses were assessed by this questionnaire. This scale also examined the risk factors in behavioral disorders and indicated stressful relationship processes (25). This questionnaire has frequently been used in various countries; hence, it has been translated into different languages, normalized and used in many countries. In this study, the 14-item version of the questionnaire was used. Scoring was done using the 5 point Likert scale beginning with “Never=0” and ending with “very often=4”. 7 negative items indicated inability to cope with stress, and 7 positive items indicated well-adopted individuals with stressful factors. The lowest score was 0 and the highest 56. Higher scores show greater perceived stress. Cronbach's alpha for this scale in 3 studies was in the range of 0.84 to 0.86 (25).
Bastani (2008) reported Cronbach's alpha of 0.81 for the scale (26). In this study, Cronbach's alpha was 0.92.
Perceived social support
The MSPSS (27) is a 12-item scale that measures perceived support in 3 domains: family, friends and a significant other. Participants completing the MSPSS were asked to indicate their agreement with items on a 7 point Likert scale, ranging from very strongly disagree to very strongly agree. Total and subscale scores ranged from 0 to 6, with higher scores suggesting greater levels of perceived social support. In Iran, Cronbach's alpha of 0.84 for the scale and 0.90, 0.93 and 0.85, respectively for friends, significant others and family subscale was reported by Sararoudi (28). The intra-class correlation coefficient (ICC) and Cronbach's alpha coefficient for this tool were 0.89 and 0.92 in the present study, respectively.
Ethics approval for this study was provided by Research Council Session in Welfare and Rehabilitation Sciences University dated 17.4.2012.
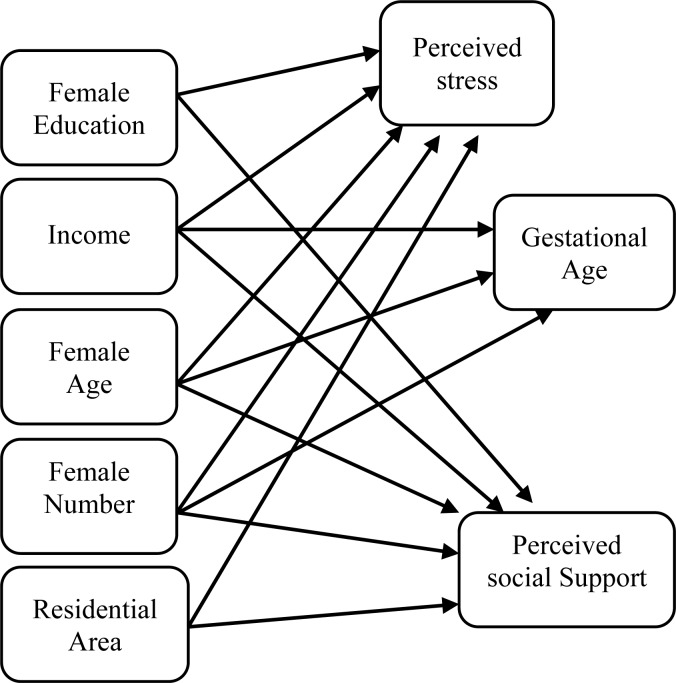
In this study, a conceptual model (Figure 1) was designed to determine the simultaneous relationship between female education, female age, family number, residential area, perceived stress and perceived social support parameters in pregnancy with gestational age.
Figure 1.
Theoretical path model for investigating the effects of structural and intermediary determinants of health on gestational age
In this study, path analysis that is in fact an extension of the regression model was used.
The SPSS 21 and Lisrel 8.8 software were used for data analysis with the application of path analysis.
Results
In the present study, information was collected from 500 mothers and their newborn infants. The incidence of preterm labor was 15.5%. The mean± SD, maximum and minimum values of structural and intermediary determinants of health in the study are shown in (Table 1).
Table 1.
Descriptive statistics for structural and intermediary determinants of health
| Variable | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| Age (years) | 28.46 | 4.98 | 17.00 | 42.00 |
| Education (years) | 11.45 | 3.18 | 0.00 | 20.00 |
| Family number | 1.68 | 1.03 | 1.00 | 8.00 |
| Residential area ( m 2 ) | 70.24 | 29.51 | 12.00 | 300.00 |
| Income (Rials) | 8180000.44 | 3000000.32 | 4000000.00 | 15000000.00 |
| Perceived stress | 21.92 | 8.34 | 0.00 | 46.00 |
| Perceived social support | 60.41 | 13.13 | 0.00 | 84.00 |
Before performing pathway analysis, bivariate analysis was used in order to determine the correlation between the variables (Table 2). As can be seen, gestational age had significant inverse correlation with family number and perceived stress and it had significant correlation with female education. Furthermore, stress had significant inverse relationship with social support of the pregnant mother. Moreover, income had significant inverse correlation with perceived stress.
Table 2.
Correlations among structural and intermediary determinants of health and preterm delivery
| Age | Education | Family number | Residential area | Income | Perceived stress | Perceived social support | |
|---|---|---|---|---|---|---|---|
| Gestational age | -0.058 | 0.148 ** | -0.252 ** | -0.074 | 0.093 * | -0.153 ** | 0.054 |
| Age | 1 | -0.069 | 0.258 ** | 0.183 ** | 0.102 * | -0.074 | 0.079 |
| Education | -- | 1 | -0.313 ** | 0.093 * | 0.255 ** | -0.041 | 0.189 ** |
| Family number | -- | -- | 1 | 0.197 ** | -0.084 | 0.128 ** | -0.111 * |
| Residential area | -- | -- | -- | 1 | 0.169 ** | -0.013 | 0.006 |
| Income | -- | -- | -- | -- | 1 | -0.110 * | 0.156 ** |
| Perceived stress | -- | -- | -- | -- | -- | 1 | -0.342 ** |
Correlation is significant at the 0.05 level
Correlation is significant at the 0.01 level
The hypothesis related to the effectiveness and causal relationships between structural and intermediary determinants of health and gestational age has been confirmed. Considering that the model's mean square errors (0.060) is less than 0.8, that ratio of chi-square to degree of freedom (2.60) is also less than 3, therefore, the model has high fitness and compatibility, which indicates that the adjusted relationships of variables are based on the theory (Table 3).
Table 3.
Goodness of fit indices for the model
| Model index | χ2 | df | RMSEA | GFI | NFI | CFI | IFI |
|---|---|---|---|---|---|---|---|
| 15.65 | 6 | 0.060 | 0.99 | 0.95 | 0.96 | 0.97 |
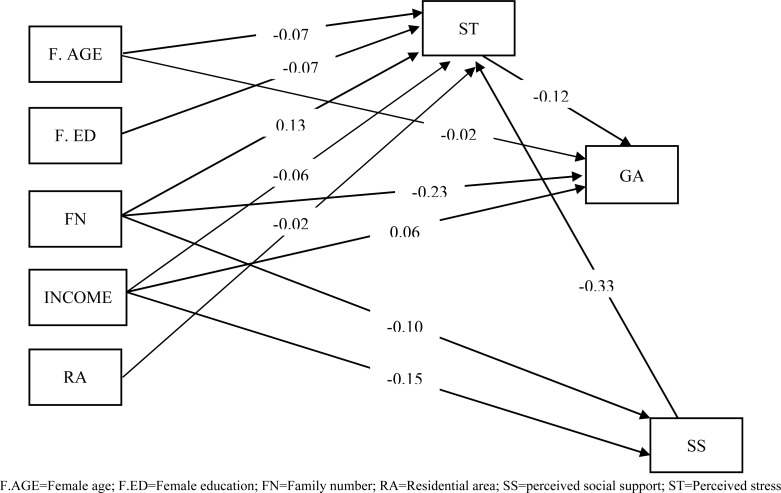
The effect of structural and intermediary determinants of health on gestational age was studied in pathway analysis (Figure 2).
Figure 2.
Full empirical model (Empirical path model for the effects of structural and intermediary determinants of health on gestational age)
In pathway analysis, the effect of variables including female education, female age, family number, residential area, perceived stress and perceived social support on gestational age was studied (Figure 2). As can be seen in the figure, perceived stress (β=-0.12) and family number (β=-0.023) among the direct pathways had the highest effect on gestational age. Social support indirectly through stress (β=0.0396) and income directly (β= 0.06) had an effect on gestational age and in total pathways of perceived stress (β=-0.12) had an effect on gestational age at birth (Table 4).
Table 4.
Path coefficients for structural and intermediary determinants of health on gestational age
| Predictor variables | Effect | Model coefficient | T-value | ||
|---|---|---|---|---|---|
|
| |||||
| Direct | Indirect | Total | |||
| Age | -0.02 | 0.0084 | -0.0116 | -0.0087 | -0.32 |
| Income | 0.06 | 0.00594 | 0.00594 | 0.00058 | 1.35 |
| residential area | - | 0.0024 | 0.0024 | -- | -- |
| Family number | -0.23 | -.01956 | -0.24956 | -0.62 | -4.78 |
| Education | -- | -0.0084 | -0.0084 | -- | -- |
| Perceived social support | -- | 0.0396 | 0.0396 | -- | -- |
| Perceived stress | -0.12 | -- | -0.12 | -0.040 | -2.56 |
Discussion
Path analysis showed that among structural factors, income had a direct effect and the factors of income, number of children (family size), as well as mother's education had the greatest overall effect on gestational age at birth, respectively.
Mothers’ socioeconomic status affects pregnancy outcome, and socioeconomic inequality is one of the indicators of infant health and pregnancy outcome including preterm labor (29). Blumenshine et al. referred to the strong effect of socioeconomic status on preterm labor in their systematic review (22). It is unlikely that low socioeconomic conditions are direct and independent factors for preterm labor, but most probably, unhealthy behaviors, exposure to stress and psychological reactions to stress shorten pregnancy duration (30).
In a review article on the role of structural determinants in preterm labor in Iran, the role of people's socioeconomic status, job and education has been mentioned. Of course, these factors were not studied from determinant perspective, and they were considered as demographic variables. Therefore, the effect of socioeconomic inequality on preterm labor was not accurately assessed (6).
Researchers believe that income inequality can lead to inequalities in health, so that countries with greater income inequality experience lower life expectancy. Different interpretations were mentioned about income inequality and health mechanism. For example, physical, structural, behavioral factors and lifestyle at individual levels are the typical ones (31). Poor people in low-income countries suffer from higher rates of diseases, particularly infectious diseases and malnutrition. Food shortages, unsafe water, poor environmental sanitation, inappropriate shelter, all result in increased exposure to infectious factors that lack of proper medical services in these areas will cause further exposure to such factors (32).
Malnutrition and the resulting infectious diseases both lead to an increase in mother's, infant's and children's mortality. These deaths are all related to poverty. Therefore, improved living conditions and increased national income in poor countries result in improvement and increase in life expectancy. In psychological and social interpretation, the neural and neuroendocrine mechanisms are used for explaining the relationship between income inequality and health. This interpretation explains the effects of socio-economic differences on health by individual's perception of social hierarchy. The difference between rich and poor results in reduced social cohesion or trust. Perceived lower position in the social hierarchy creates negative feelings such as shame and distrust that can lead to poor health through neural and neuroendocrine systems as well as stress-induced inappropriate behaviors such as smoking (31).
Another structural factor that had an indirect and reverse effect on gestational age at birth was mother's education.
Jansen et al. believe that based on measurement of indicator of education level, preterm labor in pregnant women with low socioeconomic status is twice greater than women with high education level. They believe that the educational inequalities that exist in society and cause preterm birth may be due to adverse combination of different characteristics of pregnancy, psychosocial factors, and lifestyle habits which are seen less in educated women (33).
Park et al. (2013) stated that parental education had the greatest effect on the 3 most important outcomes of pregnancy, namely low birth weight, preterm delivery and intrauterine growth retardation (34).
Mother's education affects baby's birth weight by improving the efficiency of health investment. In fact, mother's education is effective on health either directly through increased income that leads to accessing and purchasing material resources such as food with better quality and housing and a better access to health services or indirectly through its role in partner selection. Moreover, it is effective with respect to factors such as decision on the number and timing of pregnancy and growing confidence in the individual as well as increased efficiency in using medical information (35–37).
Therefore, education leads to a better combined input that increases the person's ability and willingness to change preventive health behaviors. The positive effect of this factor on gestational age at birth might be through the effect on mother's health, behaviors during pregnancy such as smoking, using prenatal care or the effect on family characteristics (partner selection, social class) (35).
Path analysis showed that among intermediate factors of social determinants of health, stress in the direct path and among the overall effects, the perceived stress and perceived social support were effective on gestational age at birth.
Researches show that women who experience higher levels of psychosocial stress have higher rates of preterm labor (29). It seems that physiological mechanisms of stress have a role in preterm labor. Endocrine system leads to releasing of adrenocorticotropin, corticotropin-releasing hormone, cortisol, cytokine and prostaglandins in response to mother's physical and psychological stress by activating hypothalamus-pituitary-adrenal axis between mother and fetus.
Furthermore, the immune system causes preterm labor by activating inflammatory process in that physical stress such as infection activates neurochemical factors such as macrophages, endotoxins, cytokines and prostaglandins and as a result it leads to preterm labor (13).
Moreover, recent studies on social supports refer to this important point that close and intimate relationships can have positive and beneficial aspects (38). Studies have shown a significant relationship between social support and health. People with more social support have better health (39, 40). Also, studies indicate that physiological responses to stress are modified through social support, i.e. the individual's reaction rate in the presence of friends is less than when the individual alone is faced with stress (41).
To determine the effect of social support on health, researchers have considered two types of processes. The first process represents the direct effect of social support on health. According to this mechanism, the positive effects of support or lack of support due to social isolation directly affect individuals’ health. The second process acts through what is called the moderating effect. According to this process, social support has no direct effect on health, but it can help modulate acute and chronic stress of people. Several years ago, it became clear that experiencing and dealing with stress factors such as accidents endanger the health of some individuals. To explain this issue, it is assumed that the causal effect of life events on the development of diseases is adjusted by protective factors such as social support. Although vulnerability factors such as lack of support increase individual's readiness to develop the disease after experiencing an accident that induces stress, there is so much evidence for direct effect process and moderator process (42).
Some scientists have investigated the role of biological mechanisms especially inflammatory processes for the effect of social support on stress reduction (43). The second potential mechanism considered is the effects of social support on health behaviors. Social support relationships facilitate health-promoting behaviors such as not smoking, not drinking too much alcohol, healthy diet and physical activity. Biological processes such-as changes in function of cardiovascular, neurohormonal and immune systems mediate the relationship between these behaviors and health. For example, many studies have shown that there is a relationship between the optimal level of social support and lower blood pressure in everyday life (44).
During pregnancy, social support for mother's health and welfare are essential. Providing supportive, emotional and informational resources can relieve physical and psychological changes related to pregnancy. Also, support encourages mothers to have healthy behaviors and to make changes in their lifestyle in order to improve their physical health (45). Studies indicate that components of social support including effective emotional support and positive interaction have an inverse relationship with inadequate prenatal care (46).
A number of prospective studies have examined the effect of social support during pregnancy on birth weight and pregnancy duration. Initial studies concluded that support could reduce difficulties during pregnancy in women who experience higher levels of stress, but this finding was not true about women who had lower levels of stress. This finding was based on the effect of model of coping with stress in social support. However, recent findings suggest a direct relationship between social support and pregnancy outcomes (45). Social support as a mediator of stress and its effects have been studied in high-risk pregnancies. It has been revealed that it has a negative relationship with stress and a positive correlation with adjustment. So, when a woman is exposed to a high-risk pregnancy and tries to adjust with her stressors, social support is considered an important variable (47).
Conclusion
The current study showed that structural and intermediary determinants had an effect on preterm labor. This study suggested that future investigations concerning not only the research on the medical factors but also investigations on the effects of the social factors on health are appropriate fields for more scrutiny.
Acknowledgement
This research is derived from the PhD thesis in specialized research on social determinants of health approved by Research Council Session in Welfare and Rehabilitation Sciences University dated 17.4.2012. We appreciate the cooperation of the honorable research deputy of university and the head of research center for social determinants of health, and all participants in this study.
To cite this article: Dolatian M, Mirabzadeh A, Setareh Forouzan A, Sajjadi H, Alavimajd H, Mahmoodi Z. Relationship between Structural and Intermediary Determinants of Health and Preterm Delivery. J Reprod Infertil. 2014;15(2):78-86.
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371(9606):75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang YP, Liu XH, Gao SH, Wang JM, Gu YS, Zhang JY, et al. Risk factors for preterm birth in five Maternal and Child Health hospitals in Beijing. PLoS One. 2012;7(12):e52780. doi: 10.1371/journal.pone.0052780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Souza NL, Pinheiro-Fernandes AC, Clara-Costa Ido C, Cruz-Enders B, de Carvalho JB, da Silva Mde L. Domestic maternal experience with preterm newborn children. Rev Salud Publica (Bogota) 2010;12(3):356–67. doi: 10.1590/s0124-00642010000300002. [DOI] [PubMed] [Google Scholar]
- 4.Subramaniam A, Abramovici A, Andrews WW, Tita AT. Antimicrobials for preterm birth prevention: an overview. Infect Dis Obstet Gynecol. 2012;2012:157–159. doi: 10.1155/2012/157159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Namavar Jahromi B, Salarian L, Shiravani Z. Maternal risk factors and neonatal outcome of the admitted patients for preterm spontaneous uterine contractions. Iran Red Crescent Med J. 2011;13(12):877–83. [PMC free article] [PubMed] [Google Scholar]
- 6.Dolatian M, Mirabzadeh A, Forouzan AS, Sajjadi H, Alavi Majd H, Moafi F. Preterm delivery and psycho-social determinants of health based on World Health Organization model in Iran: a narrative review. Glob J Health Sci. 2012;5(1):52–64. doi: 10.5539/gjhs.v5n1p52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burkman RT. Clinical obstetrics: the fetus and mother. JAMA. 2007;298(2):229–30. [Google Scholar]
- 8.Berghella V. Preterm birth: prevention and management. Singapor: Wiley-Blackwell; 2010. p. 8. [Google Scholar]
- 9.Pillitteri A. Maternal and child health nursing: Care of the childbearing and childrearing family. Lippin-cott Williams & Wilkins; 2010. p. 1139. [Google Scholar]
- 10.Cunningham FG, Williams JW, Leveno KJ, Bloom S, Hauth JC. Williams obstetrics. 23rd ed. New York: McGraw-Hill Medical; 2010. p. 804. [Google Scholar]
- 11.Melnyk BM, Crean HF, Feinstein NF, Fairbanks E. Maternal anxiety and depression after a premature infant's discharge from the neonatal intensive care unit: explanatory effects of the creating opportunities for parent empowerment program. Nurs Res. 2008;57(6):383–94. doi: 10.1097/NNR.0b013e3181906f59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Edwin Chandraharan SA. Recent advances in management of preterm labor. J Obstet Gynecol India. 2005;55(2):118–24. [Google Scholar]
- 13.Strange LB, Parker KP, Moore ML, Strickland OL, Bliwise DL. Disturbed sleep and preterm birth: a potential relationship? Clin Exp Obstet Gynecol. 2009;36(3):166–8. [PubMed] [Google Scholar]
- 14.Kramer MS, Seguin L, Lydon J, Goulet L. Socio-economic disparities in pregnancy outcome: why do the poor fare so poorly? Paediatr Perinat Epi-demiol. 2000;14(3):194–210. doi: 10.1046/j.1365-3016.2000.00266.x. [DOI] [PubMed] [Google Scholar]
- 15.Okun ML, Schetter CD, Glynn LM. Poor sleep quality is associated with preterm birth. Sleep. 2011;34(11):1493–8. doi: 10.5665/sleep.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meng G, Thompson ME, Hall GB. Pathways of neighbourhood-level socio-economic determinants of adverse birth outcomes. Int J Health Geogr. 2013;12:32. doi: 10.1186/1476-072X-12-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Minkler M, Fuller-Thomson E, Guralnik JM. Gradient of disability across the socioeconomic spectrum in the United States. N Engl J Med. 2006;355(7):695–703. doi: 10.1056/NEJMsa044316. [DOI] [PubMed] [Google Scholar]
- 18.Taylor-Robinson D, Agarwal U, Diggle PJ, Platt MJ, Yoxall B, Alfirevic Z. Quantifying the impact of deprivation on preterm births: a retrospective cohort study. PLoS One. 2011;6(8):e23163. doi: 10.1371/journal.pone.0023163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li X, Sundquist J, Kane K, Jin Q, Sundquist K. Parental occupation and preterm births: a nationwide epidemiological study in Sweden. Paediatr Perinat Epidemiol. 2010;24(6):555–63. doi: 10.1111/j.1365-3016.2010.01149.x. [DOI] [PubMed] [Google Scholar]
- 20.Vettore MV, Gama SG, Lamarca Gde A, Schilithz AO, Leal Mdo C. Housing conditions as a social determinant of low birthweight and preterm low birthweight. Rev Saude Publica. 2010;44(6):1021–31. doi: 10.1590/s0034-89102010005000045. [DOI] [PubMed] [Google Scholar]
- 21.Elstad JI. The psychosocial perspective on social inequalities in health. Sociol Health Illn. 1998;20(5):598–618. [Google Scholar]
- 22.Blumenshine P, Egerter S, Barclay CJ, Cubbin C, Braveman PA. Socioeconomic disparities in adverse birth outcomes: a systematic review. Am J Prev Med. 2010;39(3):263–72. doi: 10.1016/j.amepre.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 23.Kramer MS, Goulet L, Lydon J, Seguin L, Mc Namara H, Dassa C, et al. Socio-economic disparities in preterm birth: causal pathways and mechanisms. Paediatr Perinat Epidemiol. 2001;15(Suppl 2):104–23. doi: 10.1046/j.1365-3016.2001.00012.x. [DOI] [PubMed] [Google Scholar]
- 24.Munro BH. Statistical methods for health care research. Philadelphia: Lippincott Williams & Wilkins; 2005. p. 377. [Google Scholar]
- 25.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96. [PubMed] [Google Scholar]
- 26.Bastani F, Rahmatnejad L, Jahdi F, Haghani H. Breastfeeding self efficacy and perceived stress in primiparous mothers. Iran J Nurs. 2008;21(54):9–24. [Google Scholar]
- 27.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Personal Assess. 1988;52(1):30–41. [Google Scholar]
- 28.Sararoudi RB, Sanei H, Baghbanian A. The relationship between type D personality and perceived social support in myocardial infarction patients. J Res Med Sci. 2011;16(5):627–33. [PMC free article] [PubMed] [Google Scholar]
- 29.Berghella V, Roman A, Daskalakis C, Ness A, Baxter JK. Gestational age at cervical length measurement and incidence of preterm birth. Obstet Gynecol. 2007;110(2 Pt 1):311–7. doi: 10.1097/01.AOG.0000270112.05025.1d. [DOI] [PubMed] [Google Scholar]
- 30.Kramer MS, Victora CG, Semba R, Bloem M. Nutrition and health in developing countries. Totowa: Humana press Inc; 2001. p. 57. [Google Scholar]
- 31.Chun HM. The effect of parental occupation on low birth weight [dissertation]; Hong Kong: University of Hong Kong; 2004. p. 58. [Google Scholar]
- 32.Doyal L. Gender and the 10/90 gap in health research. Bull World Health Organ. 2004;82(3):162. [PMC free article] [PubMed] [Google Scholar]
- 33.Jansen PW, Tiemeier H, Jaddoe VW, Hofman A, Steegers EA, Verhulst FC, et al. Explaining educational inequalities in preterm birth: the generation r study. Arch Dis Child Fetal Neonatal Ed. 2009;94(1):F28–34. doi: 10.1136/adc.2007.136945. [DOI] [PubMed] [Google Scholar]
- 34.Park MJ, Son M, Kim YJ, Paek D. Social inequality in birth outcomes in Korea, 1995-2008. J Korean Med Sci. 2013;28(1):25–35. doi: 10.3346/jkms.2013.28.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chevalier A, O'Sullivan V. Mother's education and birth weight [discussion papers] Germany: Royal Holloway University of London & London School of Economics and IZA; 2007. p. 43. [Google Scholar]
- 36.Solar O, Irwin A. A conceptual framework for action on the social determinants of health. Production. Geneva: World Health Organization; 2010. Apr, p. 31. [Google Scholar]
- 37.Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (part 1) J Epidemiol Community Health. 2006;60(1):7–12. doi: 10.1136/jech.2004.023531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marmot MG, Wilkinson RG. Social determinants of health. USA: Oxford University Press; 2006. p. 160. [Google Scholar]
- 39.Berkman LF. The role of social relations in health promotion. Psychosom Med. 1995;57(3):245–54. doi: 10.1097/00006842-199505000-00006. [DOI] [PubMed] [Google Scholar]
- 40.Bovier PA, Chamot E, Perneger TV. Perceived stress, internal resources, and social support as determinants of mental health among young adults. Qual Life Res. 2004;13(1):161–70. doi: 10.1023/B:QURE.0000015288.43768.e4. [DOI] [PubMed] [Google Scholar]
- 41.Glynn LM, Christenfeld N, Gerin W. Gender, social support, and cardiovascular responses to stress. Psychosom Med. 1999;61(2):234–42. doi: 10.1097/00006842-199903000-00016. [DOI] [PubMed] [Google Scholar]
- 42.Seeman TE. Social ties and health: the benefits of social integration. Ann Epidemiol. 1996;6(5):442–51. doi: 10.1016/s1047-2797(96)00095-6. [DOI] [PubMed] [Google Scholar]
- 43.Reblin M, Uchino BN. Social and emotional support and its implication for health. Curr Opin Psychiatry. 2008;21(2):201–5. doi: 10.1097/YCO.0b013e3282f3ad89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Croezen S, Picavet HS, Haveman-Nies A, Verschuren WM, de Groot LC, van't Veer P. Do positive or negative experiences of social support relate to current and future health? Results from the Do-etinchem Cohort Study. BMC Public Health. 2012;12:65. doi: 10.1186/1471-2458-12-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Feldman PJ, Dunkel-Schetter C, Sandman CA, Wadhwa PD. Maternal social support predicts birth weight and fetal growth in human pregnancy. Psychosom Med. 2000;62(5):715–25. doi: 10.1097/00006842-200009000-00016. [DOI] [PubMed] [Google Scholar]
- 46.Leal Mdo C, Pereira AP, Lamarca Gde A, Vettore MV. The relationship between social capital, social support and the adequate use of prenatal care. Cad Saude Publica. 2011;27(Suppl 2):S237–53. doi: 10.1590/s0102-311x2011001400011. [DOI] [PubMed] [Google Scholar]
- 47.Black KD. Stress, symptoms, self-monitoring confidence, well-being, and social support in the progression of preeclampsia/gestational hypertension. J Obstet Gynecol Neonatal Nurs. 2007;36(5):419–29. doi: 10.1111/j.1552-6909.2007.00173.x. [DOI] [PubMed] [Google Scholar]