Abstract
Objective
To evaluate radiographic progression in patients with ankylosing spondylitis (AS) receiving two different doses of the tumour necrosis factor antagonist golimumab.
Methods
356 patients with AS were randomly assigned to placebo, or golimumab 50 mg or 100 mg every 4 weeks (wks). At wk16, patients with inadequate response early escaped with blinded dose adjustments (placebo→golimumab 50 mg, 50 mg→100 mg). At wk24, patients still receiving placebo crossed over to golimumab 50 mg. Lateral view radiographs of the cervical/lumbar spine were obtained at wk0, wk104 and wk208, and scored (two blinded readers, modified Stoke AS Spine Score (mSASSS)). Observed data were used for wk104 analyses; missing wk208 scores were linearly extrapolated.
Results
Wk104 changes from baseline in mSASSS averaged 1.6±4.6 for placebo crossover, 0.9±2.7 for 50 mg and 0.9±3.9 for 100 mg. By wk208, following golimumab therapy for 3.5–4 years, mean changes in mSASSS were 2.1±5.2 for placebo crossover, 1.3±4.1 for 50 mg and 2.0±5.6 for 100 mg. Less than a third of patients (placebo crossover, 19/66 (28.8%); 50 mg, 29/111 (26.1%); 100 mg, 35/122 (28.7%)) had a definitive change from baseline mSASSS (>2). Less radiographic progression was observed through wk208 in patients without baseline syndesmophytes (0.2 vs 2.8 in patients with ≥1 syndesmophyte; p<0.0001) and with baseline C-reactive protein (CRP) levels ≤1.5 mg/dl (0.9 vs 2.9 with CRP >1.5 mg/dl; p=0.0004).
Conclusions
No difference in mSASSS change was observed between golimumab 50 mg and 100 mg. The radiographic progression rate remained stable at years 2 and 4, suggesting no acceleration of new bone formation over time. Golimumab-treated AS patients with no syndesmophytes and less systemic inflammation at baseline had considerably less radiographic progression.
Keywords: Ankylosing Spondylitis, TNF-alpha, Anti-TNF, Spondyloarthritis
Introduction
Ankylosing spondylitis (AS) is a chronic rheumatic disease of the axial skeleton characterised by spinal inflammation and new bone formation in the form of syndesmophytes and ankylosis. Inflammation in the sacroiliac joints and the spine can be identified by MRI at early and advanced stages of the disease. Both conventional radiographs and MRI are critical for classification and diagnosis of AS. Radiographic spinal changes in AS are quantified by the modified Stoke AS Spine Score (mSASSS). Such changes are largely of osteoproliferative nature and, in comparison with rheumatoid arthritis, they occur rather slowly, in some cases requiring up to 10 years to become visible on plain radiographs.1 Radiographic damage in AS is associated with impaired physical function—independent of patient-reported disease activity.2
Tumour necrosis factor α (TNF) is a key mediator in the pathogenesis of AS, and therapies that inhibit TNF have been shown to reduce the signs and symptoms of this disorder. Separate studies evaluating the effects of the anti-TNF agents adalimumab,3 etanercept4 and infliximab5 on radiographic damage in patients with AS did not demonstrate inhibition of radiographic progression after approximately 2 years of therapy.3–5 However, radiographic progression appeared to have slowed after 4 years of infliximab anti-TNF therapy in a small study6 that included a 12-week, randomised, placebo-controlled phase followed by infliximab treatment in all patients during long-term study extension.
The phase 3, randomised, placebo-controlled, GO-RAISE trial evaluated the safety and efficacy of two doses of golimumab, a human monoclonal anti-TNF antibody, in patients with AS.7 Safety and efficacy results through 2 years have been previously published.8 GO-RAISE also had the aim of assessing the effect of two different doses of golimumab on radiographic progression in patients with AS, including comparisons between immediate and delayed golimumab treatment through 4 years.
Methods
Study design and patients
Patient selection criteria and study design details of the phase 3, multicentre, randomised, placebo-controlled, double-blind, GO-RAISE trial have been previously described.7 Briefly, 356 patients with active AS were randomly assigned (1:1.8:1.8) to receive subcutaneous doses of placebo, golimumab 50 mg or golimumab 100 mg at baseline and every 4 weeks using an adaptive stratified randomisation design with minimisation by biased-coin assignment. Investigational study site and screening C-reactive protein (CRP) level (≤1.5 mg/dl, >1.5 mg/dl) were included as balancing factors in the minimisation algorithm. The protocol was reviewed and approved by the institutional review board or independent ethics committee at each site. All patients provided written informed consent. The study was conducted in the USA, Canada, Europe and Asia.
Patients eligible for enrolment must have had ‘definite’ AS according to the modified New York criteria9 and symptoms of active disease (Bath AS Disease Activity Index (BASDAI)10≥4 and total back pain visual analogue scale score ≥4, each on a scale of 0–10 cm); patients with complete ankylosis were excluded. Stable doses of methotrexate, sulfasalazine and/or hydroxychloroquine were permitted until week 24, after which doses of these medications could be adjusted.
At week 16, patients who had <20% improvement from baseline in total back pain and morning stiffness entered double-blind early escape, such that patients in the placebo group began receiving golimumab 50 mg and those in the golimumab 50-mg group had their dose increased to 100 mg. Patients who were initially assigned to receive golimumab 100 mg did not have any change in treatment regardless of whether they met the early escape criteria. At week 24, all patients who were still receiving placebo crossed over to receive golimumab 50 mg. All patients continued their treatment regimen through week 100 in a double-blinded manner.
The GO-RAISE long-term extension (LTE) started with the week-104 administration of golimumab. The blind was maintained during the LTE until the last patient completed week-104 evaluations and the week-104 database was locked. Patients received golimumab every 4 weeks for approximately 5 years (final injection at week 252) from the initial (week 0) administration of study agent. After the week-104 study unblinding and at the investigator's discretion, patients receiving golimumab 50 mg every 4 weeks could increase their golimumab dose to 100 mg every 4 weeks. Patients receiving golimumab 100 mg every 4 weeks maintained this dose. A protocol amendment also allowed the golimumab dose to be decreased from 100 to 50 mg after unblinding. Through week 256, 12 placebo and 19 50-mg patients increased the golimumab dose from 50 to 100 mg, and four placebo, 12 50-mg and 22 100-mg patients decreased the golimumab dose from 100 to 50-mg (following escalation to 100 mg in the case of placebo and 50 mg patients). Also, beginning at week 104, concomitant disease modifying antirheumatic drug, corticosteroid and non-steroidal anti-inflammatory drug therapy could be adjusted.
Radiographic assessments
Lateral view radiographs of the cervical and lumbar spine were performed at baseline, week 104, and week 208 and scored using the mSASSS scoring method11 as follows: 0=normal; 1=erosion, sclerosis or squaring; 2=syndesmophyte; 3=bridging syndesmophyte (range: 0–72). Scoring was conducted by two, centrally trained, independent readers who were blinded to treatment information and radiograph sequence, and scores were averaged between the two readers for analysis. The annual rate of progression during the trial was calculated as the change in observed (at week 104) or linearly extrapolated (at week 208) mSASSS score from baseline divided by the elapsed time in the trial.
Statistical analysis
Analyses of imaging data collected through week 104 employed observed data; missing data were not imputed. Missing radiographic data at week 208 were replaced via linear extrapolation for 8.7% (26/299) of patients. Only patients with baseline and ≥1 post-baseline score within an analytical window were included in the specific analysis. Radiographic data were summarised through the use of descriptive statistics according to randomised treatment group for all patients included in the radiographic substudy, as well as for patients with or without syndesmophytes at baseline. The presence of syndesmophytes was defined as ≥1 level of spine with a score of ≥2 (syndesmophytes) at baseline for ≥1 reader. Fewer than 20% of patients with baseline syndesmophytes had them evaluated as such by only one reader.
In general, no statistical comparisons were conducted for week 104 or week 208 data, because all patients received golimumab from week 16 or week 24 onward. However, analyses of variance were employed to compare the mSASSS change from baseline between the golimumab 50-mg vs 100-mg groups, patients with baseline CRP ≤1.5 mg/dl vs >1.5 mg/dl, and patients with versus without baseline syndesmophytes. The proportion of patients with a definite change in radiographic progression, defined as mSASSS change >2,12 was also assessed.
Results
The GO-RAISE patient population has been described previously. Baseline demographic and disease characteristics were generally similar across randomised treatment groups.7 Of the 356 randomised patients, 299 (84.0%) had pre- and post-treatment data obtained for the GO-RAISE radiographic substudy. Among these patients, baseline mSASSS was numerically higher in placebo patients than in either golimumab group. Although these differences were not statistically significant owing to wide inter-patient variability, the disparity may have contributed to higher rates of progression during the study. Similar proportions of patients across the radiographic substudy treatment groups had ≥1 level of spine with a score of ≥2 (syndesmophytes) at baseline and ≥1 follow-up evaluation (table 1).
Table 1.
Baseline radiographic data
| Placebo | Golimumab 50 mg | Golimumab 100 mg | |
|---|---|---|---|
| Patients randomised, n | 78 | 138 | 140 |
| Patients with evaluable radiographs, n | 66 | 111 | 122 |
| mSASSS | |||
| Mean±SD | 16.1±18.7 | 11.7±16.4 | 13.5±18.9 |
| Median (IQR) | 7.9 (1.0, 28.0) | 3.1 (0.5, 18.0) | 3.5 (0.5, 18.0) |
| p Value vs placebo | 0.27 | 0.49 | |
| Patients with syndesmophytes at baseline and ≥1 follow-up evaluation,* n (%) | 40 (60.6%) | 68 (61.3%) | 71 (58.2%) |
*Defined as ≥1 level of spine with a score ≥2 (syndesmophytes) for ≥1 reader.
mSASSS, modified Stoke Ankylosing Spondylitis Spine Score.
The intra-class correlation coefficients (ICCs) of status scores at baseline, week 104 and week 208 were 0.93, 0.95 and 0.96, respectively, indicating strong agreement between the two readers. The ICCs of the changes from baseline to week 104 (0.36) and week 208 (0.67) indicated moderate agreement between the readers for these measures.
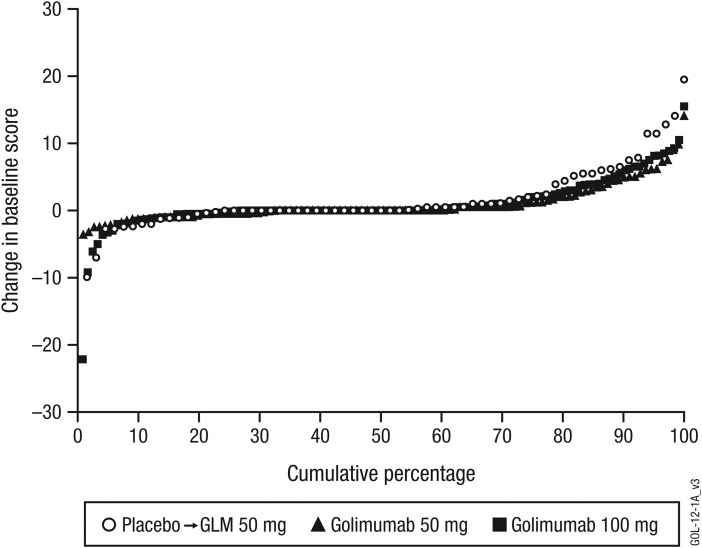
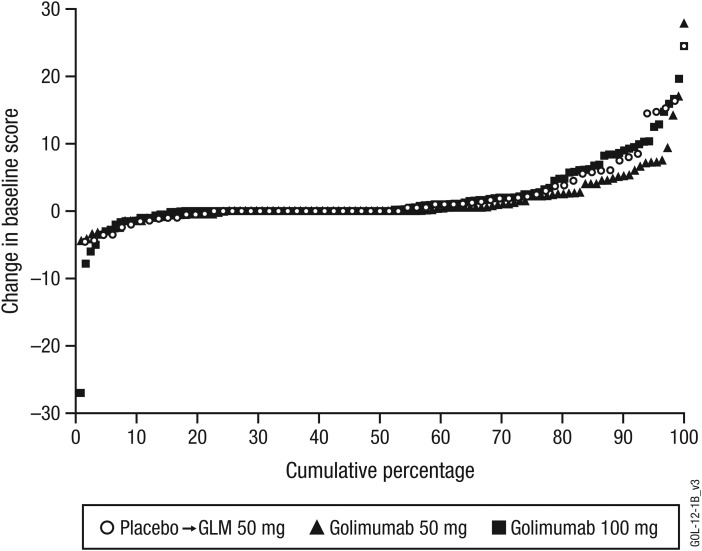
Changes from baseline to week 104 and week 208 in the mSASSS are shown in tables 2 and 3, respectively, and depicted as probability plots in figures 1 and 2, respectively.
Table 2.
Changes from baseline to week 104 in mSASSS (observed data)
| Placebo→golimumab 50 mg* | Golimumab | ||
|---|---|---|---|
| 50 mg* | 100 mg* | ||
| Patients in radiographic substudy, n | 66 | 111 | 122 |
| mSASSS change | |||
| Mean±SD | 1.6±4.6 | 0.9±2.7 | 0.9±3.9 |
| Median (IQR) | 0.0 (0.0, 2.2) | 0.0 (−0.5, 1.2) | 0.0 (−0.2, 2.0) |
| mSASSS change in patients with baseline syndesmophytes,† n | 40 | 68 | 71 |
| Mean±SD | 2.6±5.8 | 1.4±3.3 | 1.3±4.8 |
| Median (IQR) | 1.3 (−1.1, 5.8) | 0.5 (−0.9, 3.2) | 0.4 (−0.5, 3.0) |
| mSASSS change in patients without baseline syndesmophytes,† n | 24 | 42 | 45 |
| Mean±SD | 0.1±0.4 | −0.0±0.7 | 0.3±1.2 |
| Median (IQR) | 0.0 (0.0, 0.0) | 0.0 (−0.4, 0.0) | 0.0 (0.0, 0.0) |
| mSASSS change in all patients with baseline syndesmophytes,† n | All patients 179 | ||
| Mean±SD | 1.6±4.6 | ||
| Median (IQR) | 0.5 (−0.6, 3.9) | ||
| mSASSS change in all patients without baseline syndesmophytes,† n | All patients 111 | ||
| Mean±SD | 0.1±0.9 | ||
| Median (IQR) | 0.0 (0.0, 0.0) | ||
| p Value vs patients with baseline syndesmophytes | 0.0348 | ||
| Annual progression rate at week 104 (change in mSASSS per year), Mean±SD | 0.8±2.2 | 0.4±1.3 | 0.4±1.8 |
*Patients in the placebo group started golimumab 50-mg at either week 16 (early escape) or week 24 (crossover) per protocol. Patients in the 50-mg group could escalate the golimumab dose to 100-mg at week 16 if they qualified for early escape. Patients in the 100-mg group continued to receive 100-mg regardless of early escape status.
†Defined as ≥1 level of spine with a score ≥2 (syndesmophytes) at baseline and a follow-up evaluation for ≥1 reader.
mSASSS, modified Stoke Ankylosing Spondylitis Spine Score.
Table 3.
Changes from baseline to week 208 in mSASSS (employing linear extrapolation for missing data)
| Placebo→golimumab 50 mg* | Golimumab | ||
|---|---|---|---|
| 50 mg* | 100 mg* | ||
| Patients in radiographic substudy, n | 66 | 111 | 122 |
| mSASSS change, by randomised group | |||
| Mean±SD | 2.1±5.2 | 1.3±4.1 | 2.0±5.6 |
| Median (IQR) | 0.0 (0.0, 2.5) | 0.0 (0.0, 2.2) | 0.0 (0.0, 2.7) |
| p Value for 50 vs 100 mg | 0.16 | ||
| mSASSS change, by receipt of 50 mg vs 100 mg, n | 177 | 122 | |
| Mean±SD | – | 1.6±4.5 | 2.0±5.6 |
| Median (IQR) | – | 0.0 (0.0, 2.2) | 0.0 (0.0, 2.7) |
| p Value for 50 vs 100 mg | 0.25 | ||
| mSASSS change in patients with baseline syndesmophytes,† n | 40 | 68 | 71 |
| Mean±SD | 3.6±6.2 | 2.1±5.0 | 2.9±6.5 |
| Median (IQR) | 1.9 (0.0, 5.9) | 0.5 (−0.4, 4.0) | 1.5 (0.0, 6.1) |
| mSASSS change in patients without baseline syndesmophytes,† n | 24 | 42 | 45 |
| Mean±SD | −0.1±0.5 | 0.1±0.9 | 0.4±1.6 |
| Median (IQR) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) |
| mSASSS change in all patients with baseline syndesmophytes,† n | All patients 179 | ||
| Mean±SD | 2.8±5.9 | ||
| Median (IQR) | 1.1 (0.0, 5.2) | ||
| mSASSS change in all patients without baseline syndesmophytes,† n | All patients 111 | ||
| Mean±SD | 0.2±1.2 | ||
| Median (IQR) | 0.0 (0.0, 0.0) | ||
| p Value vs patients with baseline syndesmophytes | <0.0001 | ||
| mSASSS change >2, n (%) | |||
| Proportions of patients by randomised treatment group | 19 (28.8%) | 29 (26.1%) | 35 (28.7%) |
| Proportion of all patients | All patients 83/299 (27.8%) | ||
| Annual progression rate at week 208 (change in mSASSS per year), Mean±SD | 0.5±1.3 | 0.4±1.7 | 0.5±1.4 |
*Patients in the placebo group started golimumab 50 mg at either week 16 (early escape) or week 24 (crossover) per protocol. Patients in the 50-mg group could escalate the golimumab dose to 100 mg at week 16 if they qualified for early escape. Patients in the 100-mg group continued to receive 100 mg regardless of early escape status.
†Defined as ≥1 level of spine with a score ≥2 (syndesmophytes) at baseline and a follow-up evaluation for ≥1 reader.
mSASSS, modified Stoke Ankylosing Spondylitis Spine Score.
Figure 1.
Probability plot of change from baseline to week 104 in modified Stoke Ankylosing Spondylitis Spine Score (observed data). GLM, golimumab.
Figure 2.
Probability plot of change from baseline to week 208 in modified Stoke Ankylosing Spondylitis Spine Score (linearly extrapolated data). GLM, golimumab.
Using observed data only, mean±SD changes in mSASSS from baseline to week 104 were 1.6±4.6 in the placebo→golimumab 50-mg group, 0.9±2.7 in the golimumab 50-mg group and 0.9±3.9 in the golimumab 100-mg group (table 2). Utilising linear extrapolation to replace approximately 9% (28/299 data points) of missing data, mean±SD changes from baseline to week 208 were 2.1±5.2 in the placebo→golimumab 50-mg group, 1.3±4.1 in the golimumab 50-mg group and 2.0±5.6 in the golimumab 100-mg group. No difference was observed between golimumab 50 mg and 100 mg in mSASSS change from baseline to week 208 when assessed by randomised treatment group (p = 0.16) or by golimumab dose (p = 0.25; table 3).
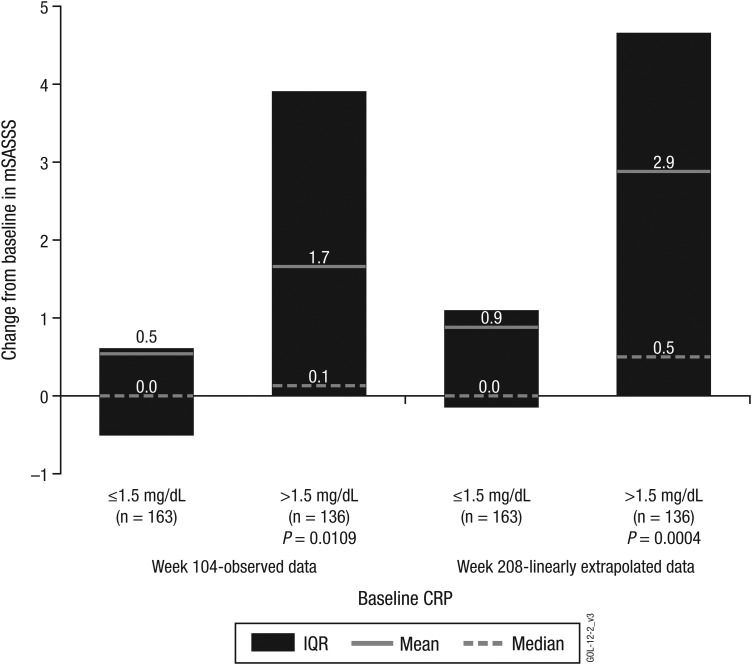
Less radiographic progression from baseline was observed among all golimumab-treated patients with baseline CRP ≤1.5 mg/dl at both week 104 (mean±SD mSASSS change of 0.5±2.7) and week 208 (0.9±3.2) when compared with patients who had baseline CRP levels >1.5 mg/dl (1.7±4.6, p=0.0109; and 2.9±6.3, p=0.0004; figure 3).
Figure 3.
Change in modified Stoke Ankylosing Spondylitis Spine Score (mSASSS) at week 104 (observed data) and week 208 (linearly extrapolated data) by baseline C-reactive protein (CRP) level.
Less radiographic progression from baseline was also observed in golimumab-treated patients with no baseline syndesmophytes (mean mSASSS changes ranging from −0.0 to 0.3 at week 104 and from −0.1 to 0.4 at week 208) when compared with patients who did have syndesmophytes at baseline (mean mSASSS changes ranging from 1.3 to 2.6 at week 104 and from 2.1 to 3.6 at week 208). Also at both week 104 and week 208, all patients without syndesmophytes at baseline, regardless of treatment group (n=111), exhibited significantly less radiographic progression (mean mSASSS changes of 0.1 and 0.2, respectively) when compared with all patients who had syndesmophytes at baseline (n=179; mean mSASSS changes of 1.6 (p=0.0348) and 2.8 (p<0.0001), respectively) (tables 2 and 3).
When assessed either by randomised treatment group or for all golimumab-treated patients combined, approximately 26–29% of patients had a definite change of >2 units in mSASSS from baseline to week 208 (table 3). The mean rates of radiographic progression at week 104 (0.4 mSASSS units/year for both 50 mg and 100 mg) were similar to those at week 208 (0.4 for 50 mg, 0.5 for 100 mg) (tables 2 and 3).
Discussion
This study is the first clinical trial to provide a substantial amount of radiographic data through 4 years of anti-TNF biological therapy in patients with AS, the findings of which show that the radiographic progression observed in these patients who had been treated with 50 mg or 100 mg of the human monoclonal anti-TNF antibody golimumab subcutaneously every 4 weeks remained stable at years 2 and 4, suggesting no acceleration of new bone formation over time. Study findings also indicated no apparent difference between the two golimumab dosages.
As previously reported, clinical results of the GO-RAISE trial of golimumab in patients with AS showed significant improvements at week 24 in the signs and symptoms of AS as measured by the Assessment of SpondyloArthritis International Society improvement criteria and the BASDAI.7 In the current radiographic analysis through 2 years and 4 years of the GO-RAISE trial, one is cautioned avoid making comparisons between the golimumab and placebo groups at weeks 104 and 208 because, for ethical reasons and consistent with the design of earlier studies, the placebo-controlled period was restricted to the first 6 months of the study.
As expected, the findings from our study with golimumab are in concordance with published radiographic data for adalimumab, etanercept and infliximab.3–6 As with these anti-TNF agents, treatment with golimumab does not appear to inhibit radiographic progression in the spines of patients with AS. The proportion of patients demonstrating mSASSS change >2 through 2 years in GO-RAISE was also consistent with published data pertaining to 2-year radiographic findings of patients with AS, some of whom participated in infliximab or etanercept anti-TNF trials.12 The mSASSS rate of radiographic progression through the initial 2 years of anti-TNF therapy in previous AS trials has been approximately 1 mSASSS unit.3–6 At both weeks 104 and 208, the mean annual rate of radiographic progression among golimumab-treated patients was 0.4–0.5 units; however, any comparison of absolute scores between studies is hazardous and should be interpreted with caution. It should be noted that direct statistical testing comparing progression rates at the two time points is not appropriate due to different analytical rules that were applied for week 104 (observed) and week 208 (linearly extrapolated) data.
This is the first study to evaluate different doses of an anti-TNF agent in patients with established AS. The findings indicate no observable differences in mSASSS change between the 50 mg and 100 mg doses. This is in line with the GO-RAISE clinical findings through 2 years that demonstrated no difference in clinical efficacy between the two doses.8 At the same time, these findings do not support the hypothesis that blocking TNF may have stimulatory effects on new bone formation over time.13
Anti-TNF therapy has been shown to reduce both serum levels of inflammatory biomarkers14 and spinal inflammation evaluated by MRI.15 Additionally, decreased serum levels of interleukin-6 have demonstrated an association with later improvements in spinal inflammation.14 However, the relationship between spinal inflammation and radiographic damage is unclear,1 16 and the lack of inhibition of radiographic progression following anti-TNF therapy suggests that bone formation in AS is at least partly dissociated from inflammation.
Interestingly, mSASSS scores at both week 104 and week 208 indicated significantly less radiographic progression from baseline in patients with no baseline syndesmophytes when compared with patients who did have syndesmophytes at baseline. These data confirm earlier findings indicating that the presence of syndesmophytes at baseline predicts a greater rate of spinal radiographic progression.12 16
Despite the current findings, there remains a potential role for anti-TNF therapy to prevent structural changes when given at much earlier time points in the course of axial spondyloarthritis corresponding to an inhibition of development of structural changes in AS. This hypothesis, however, needs to be tested. As suggested by MRI findings related to the phenomenon of fatty degeneration,17 the lack of effect on new bone formation in patients with more advanced AS may be because inflammatory lesions have already reached a more mature stage. Similarly, significantly less radiographic progression was observed in patients with baseline serum levels CRP≤1.5 mg/dl, that is, those with less systemic inflammation, than in patients with more extensive baseline inflammation (CRP>1.5 mg/dl). To determine whether baseline syndesmophytes and elevated CRP interact to have a combined effect on radiographic progression, and if so, whether an anti-TNF agent disrupts the synergistic interaction, further investigation is required.
The current analyses of radiographic data in the GO-RAISE trial are limited by the lack of placebo control past the initial 24 weeks of the 208-week study period for radiographic progression. That 8.7% of patients were missing radiographic data through 4 years of therapy also limits interpretation of these data.
In summary, results of this first report on the effects of long-term golimumab therapy on radiographic progression in AS suggest that neither dose of this TNF-antagonist inhibits structural progression in afflicted patients. Further, the findings suggest no acceleration of new bone formation over time in patients treated with golimumab for 4 years. Longer-term follow-up studies will be necessary to further evaluate the effects of this treatment on radiographic progression in patients with AS.
Acknowledgments
The authors thank the patients, the investigators and the study personnel who made this trial possible. The authors also thank Michelle Perate, MS and Mary Whitman, PhD of Janssen Services, LLC, a Johnson & Johnson pharmaceutical company, who helped prepare the manuscript.
Footnotes
Funding: This study was supported by Janssen Research & Development, LLC and Merck-Schering-Plough Research Institute, Inc.
Competing interests: XB has received honoraria for talks, advisory boards and grants for studies from Abbott, Amgen, Janssen Research & Development, MSD (Schering-Plough), Novartis, Pfizer (Wyeth) and UCB. JB has received honoraria for talks, advisory boards and grants for studies from Janssen Research & Development, Celltrion, Amgen, Abbott, Roche, BMS, Novartis, Pfizer (Wyeth), MSD (Schering-Plough), Sanofi-Aventis and UCB. AD has received payments for educational lectures, teleconferences and serving on advisory boards for Janssen, a company that may have a commercial interest in the results of this research. This potential conflict of interest has been reviewed and managed by Oregon Health & Science University. K-GAH has received honoraria for educational lectures from Abbott, BMS, Janssen Research & Development, MSD (Schering-Plough), Novartis, Pfizer (Wyeth), Roche and UCB. RI has received consulting fees from Merck, Schering-Plough, Abbott, Amgen and Sanofi-Aventis. DvdH has received consulting fees and/or research grants from Abbott, Amgen, BMS, Janssen, Chugai, Merck, Novartis, Pfizer, Roche, Sanofi-Aventis, Schering-Plough, UCB and Wyeth. AB, BH, YZ and SX are employees of Janssen Research & Development, LLC, a Johnson & Johnson pharmaceutical company, and own stock and/or stock options in Johnson & Johnson.
Ethics approval: The protocol was reviewed and approved by the institutional review board or independent ethics committee at each site. All patients provided written informed consent. The study was conducted in the United States, Canada, Europe and Asia.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Schett G, Coates LC, Ash ZR, et al. Structural damage in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis: traditional views, novel insights gained from TNF blockade, and concepts for the future. Arthritis Res Ther 2011;13(Suppl 1):S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Landewé R, Dougados M, Mielants H, et al. Physical function in ankylosing spondylitis is independently determined by both disease activity and radiographic damage of the spine. Ann Rheum Dis 2009;68:863–7 [DOI] [PubMed] [Google Scholar]
- 3.van der Heijde D, Salonen D, Weissman BN, et al. ; for the Canadian (M03-606) study group and the ATLAS study group. Assessment of radiographic progression in the spines of patients with ankylosing spondylitis treated with adalimumab for up to 2 years. Arthritis Res Ther 2009;11:R127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van der Heijde D, Landewé R, Einstein S, et al. Radiographic progression of ankylosing spondylitis after up to two years of treatment with etanercept. Arthritis Rheum 2008;58:1324–31 [DOI] [PubMed] [Google Scholar]
- 5.van der Heijde D, Landewé R, Baraliakos X, et al. ; the Ankylosing Spondylitis Study for the Evaluation of Recombinant Infliximab Therapy Study Group. Radiographic findings following two years of infliximab therapy in patients with ankylosing spondylitis. Arthritis Rheum 2008;58:3063–70 [DOI] [PubMed] [Google Scholar]
- 6.Baraliakos X, Listing J, Brandt J, et al. Radiographic progression in patients with ankylosing spondylitis after 4 yrs of treatment with the anti-TNF-α antibody infliximab. Rheumatology (Oxford) 2007;46:1450–3 [DOI] [PubMed] [Google Scholar]
- 7.Inman RD, Davis JC, Jr, van der Heijde D, et al. Efficacy and safety of golimumab in patients with ankylosing spondylitis: results of a randomized, double-blind, placebo-controlled, phase III trial. Arthritis Rheum 2008;58:3402–12 [DOI] [PubMed] [Google Scholar]
- 8.Braun J, Deodhar A, Inman RD, et al. Golimumab administered subcutaneously every 4 weeks in ankylosing spondylitis: 104-week results of the GO-RAISE study. Ann Rheum Dis 2012;71:661–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis: a proposal for modification of the New York criteria. Arthritis Rheum 1984;27:361–8 [DOI] [PubMed] [Google Scholar]
- 10.Garrett S, Jenkinson T, Kennedy LG, et al. A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol 1994;21:2286–91 [PubMed] [Google Scholar]
- 11.Creemers MCW, Franssen MJAM, van't Hof MA, et al. Assessment of outcome in ankylosing spondylitis: an extended radiographic scoring system. Ann Rheum Dis 2005;64:127–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baraliakos X, Listing J, Rudwaleit M, et al. Progression of radiographic damage in patients with ankylosing spondylitis: defining the central role of syndesmophytes. Ann Rheum Dis 2007;66:910–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lories R. The balance of tissue repair and remodeling in chronic arthritis. Nat Rev Rheumatol 2011;7:700–7 [DOI] [PubMed] [Google Scholar]
- 14.Visvanathan S, Wagner C, Marini JC, et al. Inflammatory biomarkers, disease activity and spinal disease measures in patients with ankylosing spondylitis after treatment with infliximab. Ann Rheum Dis 2008;67:511–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sieper J, Baraliakos X, Listing J, et al. Persistent reduction of spinal inflammation as assessed by magnetic resonance imaging in patients with ankylosing spondylitis after 2 yrs of treatment with the anti-tumour necrosis factor agent infliximab. Rheumatology (Oxford) 2005;44:1525–30 [DOI] [PubMed] [Google Scholar]
- 16.Haroon N, Maksymowych WP, Rahman P, et al. Radiographic severity of ankylosing spondylitis is associated with polymorphism of the large multifunctional peptidase 2 gene in the Spondyloarthritis Research Consortium of Canada Cohort. Arthritis Rheum 2012;64:1119–26 [DOI] [PubMed] [Google Scholar]
- 17.Maksymowych WP, Morency N, Conner-Spady B, et al. Suppression of inflammation and effects on new bone formation in ankylosing spondylitis: evidence for a window of opportunity in disease modification. Ann Rheum Dis. 2013;72:23–8 [DOI] [PubMed] [Google Scholar]