Abstract
Treatment of chronic hepatitis B (CHB) has markedly improved in the last 15 years due to the availability of direct antivirals which greatly increase therapeutic options. Currently, there are two classes of agents licensed for CHB treatment: standard or pegylated interferon alpha (IFN or Peg-IFN) and five nucleoside/nucleotide analogues (NAs). Long-term treatment with NAs is the treatment option most often used in the majority of CHB patients. Entecavir and tenofovir, the most potent NAs with high barrier to resistance, are recommended as first-line monotherapy by all major treatment guidelines and can lead to long-lasting virological suppression, resulting in histological improvement or reversal of advanced fibrosis and reduction in disease progression and liver-related complications. In this review, we focus on current treatment strategies of chronic hepatitis B and discuss the most recent efficacy and safety data from clinical trials and real life clinical practice. Recent findings of response-guided approaches are also discussed.
Keywords: Chronic hepatitis, Antiviral therapy, Peg-interferon, Nucleos(t)ide analogues, Antiviral resistance
Core tip: Patients with chronic hepatitis B are a heterogeneous population and require different management strategies. In clinical practice, several baseline factors, related to the patient, drug, stage of liver disease, comorbidities, lifestyle factors, coinfections and profile of hepatitis B virus infection, should be taken into consideration in order to individually optimize therapy. Surface antigen of the hepatitis B virus quantification is a potential new biomarker for treatment individualization and response-guided therapy. In the last two decades, the availability of potent oral antivirals changed the natural history of chronic hepatitis B; however, the risk of hepatocellular carcinoma (HCC) has not been abolished and thus regular HCC surveillance in high risk patients is required.
INTRODUCTION
Chronic infection with hepatitis B virus (HBV) is a major health problem worldwide, affecting approximately 350 million people, and is the leading cause of chronic liver disease, cirrhosis and hepatocellular carcinoma (HCC), accounting for over 1 million deaths annually[1].
The goal of chronic hepatitis B (CHB) treatment is to prevent or reduce the development of cirrhosis, end-stage liver disease, HCC and, ultimately, liver-related death. Several studies have shown that the risk of disease progression is reduced by means of sustained suppression of viral replication[2-4]. Furthermore, maintaining viral suppression increases the rate of hepatitis B surface antigen (HBsAg) clearance, which is the ideal end-point of antiviral treatment as it is associated with a definite remission of chronic hepatitis B activity and an improved long-term outcome. However, even if HBsAg loss occurs, HBV cannot be completely eradicated by treatment due to the persistence of the so-called covalently closed circular DNA (cccDNA), the template for viral RNA transcription, in the nucleus of infected hepatocytes[5].
Since the introduction of interferon alpha as an initial antiviral therapy at the end of the 1980s, the treatment of CHB has markedly improved in the last 15 years due to the availability of nucleos(t)ide analogues (NAs), direct antiviral agents which have greatly increased therapeutic options and permitted the achievement of virological response in almost all patients.
In this review, we focus on current treatment strategies of chronic hepatitis B and discuss the most recent long-term NA efficacy and safety data from clinical trials and real life clinical practice.
ANTIVIRAL TREATMENT
Treatment indications
The complex interplay between viral replication and host immune response determines the natural course of chronic HBV infection which can generally be divided into four phases: immune tolerance, immune clearance, low/non replicative and reactivation phases. Liver disease is associated with immunoclearance and reactivation phases; therefore, immunotolerant and inactive carriers do not require treatment, while antiviral therapy should be reserved for HBsAg carriers with active viral replication and biochemical or histological evidence of liver damage. The criteria for identification of candidates for antiviral therapy, according to current guidelines[6-8] are shown in Table 1.
Table 1.
European Association for the Study of the Liver guidelines compared to other international guidelines
| Criteria | EASL 2012[6] | AASLD 2009[7] | APASL 2012[8] |
| HBV DNA treatment threshold | |||
| HBeAg(+) (IU/mL) | 2000 | 20000 | 20000 |
| HBeAg(-) (IU/mL) | 2000 | 2000-20000 | 2000 |
| ALT treatment threshold | > ULN | > 2 × ULN | > 2 × ULN |
| Liver biopsy | Moderate to severe necroinflammation or fibrosis | Not applicable (consider in certain groups) | |
ULN: Upper limits of normal; HBeAg: Hepatitis B e antigen; ALT: Alanine aminotransferase; AASLD: American Association for the Study of Liver Diseases; APASL: Asia Pacific Association for the Study of the Liver; EASL: European Association for the Study of the Liver; HBV: Hepatitis B virus.
In clinical practice, however, the decision-making process is more complex as it involves several factors related to the patient (age, sex, genetics), the drug (efficacy, side effects, resistance barrier), the liver disease (fibrosis, type and extent of inflammation), the liver disease cofactors (alcohol use, diabetes, insulin-resistance, obesity), the co-infections (HDV, HCV, HIV) and the profile of HBV infection (HBeAg-status, HBV DNA levels, genotype, viral heterogeneity) (Figure 1).
Figure 1.
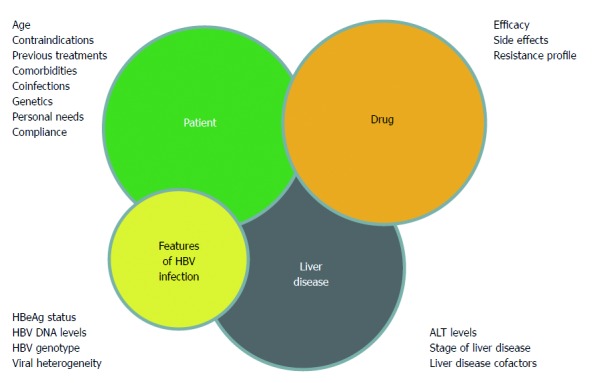
Management of chronic hepatitis B patient: decision making process. ALT: Alanine aminotransferase; HBeAg: Hepatitis B e antigen; ALT: Alanine aminotransferase; HBV: Hepatitis B virus.
The assessment of hepatic fibrosis with liver biopsy or non-invasive methods is recommended since it can assist the decision to start antiviral therapy. Treatment is mandatory for patients with severe fibrosis or cirrhosis (F3-F4) and patients with compensated or decompensated cirrhosis and detectable HBV DNA should be considered for treatment, independent of ALT levels.
Therapy is indicated for patients with moderate fibrosis (F2), while in those with mild or no fibrosis (F0-F1), the indication for treatment should be assessed individually, taking into account patient age, comorbidities, presence of liver disease cofactors, HDV/HCV/HIV coinfections, family history of HCC or cirrhosis, and extrahepatic manifestations.
Anti-HBV drugs
At present, there are two classes of agents licensed for the treatment of CHB: standard or pegylated interferon alpha (IFN or Peg-IFN) and five nucleoside/nucleotide analogues.
Standard IFN has been largely replaced by Peg-IFN due to the more convenient administration schedule (once weekly versus a thrice weekly subcutaneous injection), the longer half-life without wide fluctuations in serum concentrations, and a more effective viral suppression. There are two pegylated-IFN formulations: Peg-IFN alpha-2a and Peg-IFN alpha-2b which have demonstrated a similar efficacy in clinical trials, but only the former is globally licensed for treatment of CHB, while Peg-IFN alpha-2b has been approved in only a few countries. Peg-IFN is a cytokine with a dual antiviral and immunomodulatory activity and therefore has the potential for an immune-mediated control of HBV infection, thus providing the opportunity to obtain a sustained virological response after treatment discontinuation, and the possibility of inducing HBsAg loss in patients who achieve and maintain undetectable HBV DNA. IFN-based treatment, however, is often complicated by the occurrence of side effects, such as influenza-like symptoms, fatigue, neutropenia, thrombocytopenia and depression, which sometimes require dose modification and cause premature cessation of treatment[9]. Moreover, Peg-IFN is contraindicated in patients with decompensated HBV-related cirrhosis or autoimmune disease, in patients with uncontrolled severe depression or psychosis, in patients receiving immunosuppressive therapy or chemotherapy, and in female patients during pregnancy[6].
NAs are oral direct antiviral agents which specifically inhibit the viral polymerase/reverse transcriptase, an enzyme with a crucial role in the HBV life cycle. As a result, NAs block the production of new virions and progressively reduce serum HBV DNA to undetectable levels, but they have little or no effect on the cccDNA present in the nucleus of the infected hepatocytes. The persistence of the intrahepatic cccDNA determines the reactivation of HBV replication after interrupting NA treatment, thereby justifying the need for a long-term (potentially life-long) therapy for a sustained viral replication control. After lamivudine (LAM), the first nucleoside analogue approved for the treatment of CHB, another two nucleosides, telbivudine (LdT) and entecavir (ETV), and two nucleotide analogues, adefovir (ADV) and tenofovir (TDF), have gradually become available in recent years. NAs are characterized by a different antiviral potency and drug-resistance pattern, while entecavir and tenofovir are the two most potent analogues with a high barrier to resistance development.
The main advantages and disadvantages of Peg-IFN and NAs for treatment of CHB are shown in Table 2.
Table 2.
Main advantages and disadvantages of pegylated interferon alpha and nucleos(t)ides analogues in chronic hepatitis B[6]
| Peg-IFN | Nucleos(t)ides analogues | |
| Advantages | Finite duration (usually 48 wk) | Potent antiviral effect |
| Higher rates of anti-HBe and anti-HBs seroconversion with 12 mo of therapy | Excellent tolerance, good safety | |
| Absence of resistance | Oral administration (once daily) | |
| No contraindication for treatment | ||
| Disadvantages | Moderate antiviral effect | Unknown (perhaps indefinite) duration of treatment |
| Inferior tolerability | Rare HBsAg loss | |
| Risk of adverse events | Risk of viral resistance | |
| Subcutaneous injections | Unknown long-term safety | |
| Contraindications in specific patient subgroups |
Peg-IFN: Pegylated interferon; HBsAg: Hepatitis B surface antigen.
Treatment strategies
There are two different therapeutic strategies for both HBeAg-positive and HBeAg-negative CHB patients: short-term or “curative” treatment and long-term or “suppressive” treatment. The first strategy aims to obtain a sustained suppression of viral replication off-treatment by inducing the immune-controlled status of HBV infection which corresponds to the profile of the inactive carrier, that is, normal ALT levels coupled with HBV DNA < 2000 IU/mL and anti-HBe positivity. This strategy is IFN-based (Peg-IFN administered for 48 wk); a finite treatment with NAs is possible only in HBeAg-positive patients. The second strategy aims to obtain a rapid and long-term maintained viral suppression (HBV DNA < 10-15 UI/mL). This strategy is exclusively based on NAs.
First-line monotherapy
Peg-IFN, entecavir or tenofovir are recommended as first-line monotherapy by all major guidelines in patients with CHB or compensated cirrhosis[6-8]. The most favorable candidates for Peg-IFN are those with low HBV DNA levels, high ALT and HBV, genotype A or B rather than C or D, and those without advanced liver disease.
Entecavir or tenofovir are the only therapeutic options in patients with decompensated liver disease, in those undergoing immunosuppressive treatment or with contraindications, and those unwilling to receive Peg-IFN. As Peg-IFN can achieve a sustained off-therapy response in only a minority of cases and a proportion of patients cannot tolerate or have IFN contraindications or do not wish to be treated with Peg-IFN, long-term treatment with NAs is the most commonly used treatment strategy.
IFN-BASED THERAPY
Published data have demonstrated that in patients with HBeAg-positive CHB, Peg-IFN achieves a more than 30% HBeAg seroconversion rate after one year of treatment[6]. In a registration trial, Peg-IFN alpha-2a provided a sustained immune control which increased post-therapy; in fact, the HBeAg seroconversion rate continued to increase from 27% at the end of treatment to 32% during the six months after discontinuing treatment, and to 42% 1 year post-treatment[10,11]. Moreover, the seroconversion remained stable over time in > 80% of Peg-IFN alpha-2b treated patients, achieving this end-point at the end of therapy[12]. Peg-IFN also determined HBsAg seroconversion in up to 30% of patients with a long-term follow-up[13].
In patients with HBeAg-negative CHB, Peg-IFN alpha-2a demonstrated a sustained immune control (HBV DNA < 2000 IU/mL) in 31% of patients 1 year post-treatment. Among these, 88% maintained this response up to 5 years follow-up and, remarkably, 28% achieved HBsAg clearance 5 years post-treatment[14].
Peg-IFN treatment remains an attractive therapeutic option since it provides higher rates of off-therapy immune control, including HBsAg clearance, when compared to NAs. However, IFN is effective in only a minority of patients (20%-30%), has a poor tolerability and significant costs. Therefore, the improvement of Peg-IFN efficacy is a major challenge. Several attempts have been made to optimize the cost-effectiveness of IFN-based therapy, including combination therapy, longer treatment duration and identification of pre-treatment and on-treatment predictors of response. De novo combination therapy with NAs did not improve sustained response in either HBeAg-positive or HBeAg-negative patients[10,15-17]. Regarding duration of therapy, the NEPTUNE study conducted in patients with HBeAg-positive CHB reported that dose and duration are important because the highest sustained response was obtained with 180 μg and 48 wk compared to 90 μg and 24 wk[18]. Recently, an Italian multicenter study demonstrated in 128 HBeAg-negative patients (mean age 45 years, 94% genotype D, 13% with cirrhosis) that extended treatment with Peg-IFN alpha-2a to 96 wk was well-tolerated and improved the rates of sustained virological response (29% vs 12%, P = 0.03) in HBeAg-negative genotype D patients when compared to the current standard of care of 48 wk. In addition, 1 year post-treatment, HBsAg clearance (6%) was observed only in the extended therapy group[19]. Among pre-treatment predictors of response, ALT levels, low baseline HBV DNA and virus genotype were significant predictors[6-8]. When combining data from the two largest clinical trials regarding HBeAg-positive CHB patients[9,20], Buster et al [13] found that the best candidates for a sustained response to Peg-IFN were genotype A patients with high levels of ALT (ALT ≥ 2xULN) or low levels of HBV DNA (< 9 log10 copies/mL), and genotypes B and C patients who have both high levels of ALT and low HBV DNA. Genotype D patients have a low chance of sustained response. However, these factors cannot accurately predict response at the individual level; furthermore, ALT and HBV DNA levels are time-dependent and thus their use in clinical practice is difficult.
To obtain additional insight into the individual patient’s probability of achieving response to Peg-IFN, the presence of precore and basal core promoter mutants before treatment has been correlated to the serological and virological response in HBeAg-positive CHB patients. Data from this study demonstrated that the presence of a wild-type virus at baseline was an independent predictor of response to Peg-IFN and can assist in improving patient selection for this treatment option[21].
More recently, the role of IL28B polymorphisms, clearly indicated as a baseline host factor predictor of response in patients with chronic hepatitis C, has also been investigated in CHB patients. Studies in HBeAg-positive patients provided conflicting results[22-24]. The only existing data in HBeAg-negative patients are in 101 subjects treated with either conventional IFN or Peg-IFN alpha 2a for 24 mo and followed for 11 years after treatment. Patients with IL28B rs12979860 genotype CC were shown to have higher EOT (69% vs 45%, P = 0.01) and higher SVR (31% vs 13%, P = 0.02) than non-CC patients. Interestingly enough, CC patients had a higher cumulative probability of clearing HBsAg during an observation period of 16 years (38% vs 12%, P = 0.039)[25]. Further studies are necessary to define the role of IL28B polymorphisms as a baseline factor to improve pre-treatment patient selection.
A promising approach to improve the cost-effectiveness of Peg-IFN therapy is a response-guided treatment based on serum HBsAg kinetics which permits early identification of either responders for whom continuation of treatment to week 48 could be beneficial or non-responders who should discontinue IFN treatment.
Two stopping rules at week 12 have been proposed for HBeAg-positive patients: (1) no HBsAg decline; and (2) HBsAg levels > 20000 IU/mL. The negative predictive value (NPV) for a sustained response ranged from 92% to 100% depending on HBV genotypes; thus, HBV genotype-specific stopping-rules may be considered at week 12. However, at week 24, treatment discontinuation is indicated in all patients with HBsAg > 20000 IU/mL, irrespective of HBV genotype[26,27].
In HBeAg-negative genotype D patients, no HBsAg decline and < 2 log copies/mL HBV DNA decline at week 12 has been proposed as a stopping rule and independently validated with a 100% NPV[28,29]. Overall, therapy with Peg-IFN could be discontinued at week 12 in the 20% of primary non-responders, who are therefore candidates for suppressive therapy with NAs (Figure 2).
Figure 2.
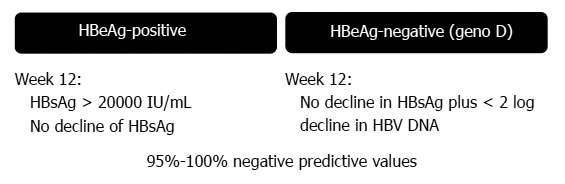
Response-guided therapy using hepatitis B surface antigen levels in pegylated interferon-treated patients: stopping rules[26-29]. HBeAg: Hepatitis B e antigen; HBsAg: Hepatitis B surface antigen.
Recently, it has been demonstrated that, even in HBeAg-negative patients, on-treatment HBsAg kinetics varied according to HBV genotype. In fact, for genotype A, the difference between responders and non-responders was greatest at week 24, while for genotypes B and D, the difference was evident at week 12; there was no significant difference for genotype C over time. Moreover, highly positive predictive values for long-term virological response was obtained by applying end-of-treatment genotype-specific HBsAg level cut-offs[30].
NA-BASED THERAPY
Entecavir and tenofovir are the third-generation NAs recommended as first-line therapy for CHB NA-naïve patients by all international guidelines. In registration trials, both antivirals demonstrated a long-lasting efficacy (viral suppression in more than 95% of patients over 5 years) associated with prevention of developing cirrhosis and, to a greater extent, with fibrosis regression[31-36]. Chang et al[31] first documented the histological reversal of cirrhosis in 4 of 10 cases who met the criteria for efficacy analysis while they were in a 3 to 7 year period of virological response to ETV. More robust evidence of cirrhosis reversion has been offered by Marcellin and colleagues who reported the effect of 5 years of viral suppression on histology in liver fibrosis and cirrhosis in 348 patients who had evaluable histology at baseline and at week 240. Of the 96 (28%) patients with cirrhosis (Ishak score ≥ 5) at baseline, 71 (74%) demonstrated a reduction in fibrosis at year 5 and were no longer cirrhotic[34].
Moreover, registration trials reported a minimal risk of drug resistance (1.2% with ETV and 0% with TDF after 6 years) and a favorable safety profile[31-36]. However, as registration trials are conducted under standardized conditions with strict enrolment criteria in well-selected and compliant patients, long-term efficacy and safety of ETV and TDF are still to be confirmed in real life patients who generally have a more complex clinical profile as they are usually older, with a higher prevalence of cirrhosis and comorbidities treated with several concomitant medications.
Efficacy and safety of entecavir in real life practice
In a retrospective/prospective multicenter Italian study, 418 consecutive NA-naïve patients initiating treatment with ETV 0.5 mg/d were studied. In this cohort, patients were older at baseline (median age 58 years), were predominately infected with HBV genotype D (90%), 49% had cirrhosis, approximately 46% had a body mass index over 25 kg/m2, and 56% had concomitant diseases. Viral suppression was achieved in 99% of patients over 60 mo of therapy, independent of HBeAg status. Only one patient with a partial virological response at week 48 developed resistance at year 3 of treatment, with a cumulative rate of 0.2%. In HBeAg-positive patients, the 5 year cumulative probability of HBeAg seroconversion and HBsAg loss were 55% and 34%, respectively. HCC developed in six non-cirrhotics with a yearly rate of 0.8%. The 204 compensated cirrhotics remained clinically stable, yet 18 developed a HCC, a 5 year cumulative rate of 13% and a yearly rate of 2.6%, making continuous surveillance for liver cancer mandatory[37].
The single center Hong Kong cohort study prospectively included 222 NA-naïve patients (median age 45 years) who demonstrated a 97.4% 5 year cumulative rate of virological response. Only two cases of resistance (corresponding to a 1.2% cumulative resistance rate up to year 5) were reported in this patient cohort[38].
The European network of excellence for Vigilance against Viral Resistance performed a multicenter cohort study with over 10 European referral centers between 2005 and 2010. The study including 243 consecutive NA-naïve patients receiving ETV monotherapy; the cumulative probability of achieving a virological response at week 144 was 90% in HBeAg-positive patients and 99% in HBeAg-negative patients, and the proportion of HBeAg-positive patients with HBeAg loss was 34%[39]. In this cohort, 81% of patients with partial virological response at 48 wk reached a virological response during prolonged ETV monotherapy and no patient developed ETV resistance. When stratifying patients according to their viral load at week 48, 95% of patients with HBV DNA < 1000 IU/mL and 57% of patients with HBV DNA > 1000 IU/mL achieved a virological response without treatment adaptation during the prolonged treatment period beyond week 48. Therefore, the authors concluded that no treatment adaptation is needed in the majority of NA-naïve patients treated with ETV who reach a partial virological response, particularly in those with HBV DNA < 1000 IU/mL at week 48. In addition, data from the Virgil cohort demonstrated that in cirrhotic patients, virological response to ETV is associated with a lower probability of developing a clinical event and disease progression[40].
The safety profile of ETV in real life studies has been largely consistent with those of registration trials as there have been no reports of serious drug-related side effects, discontinuation or renal toxicity[37-41]. One retrospective study identified five cases of lactic acidosis among 16 ETV-treated patients with decompensated liver disease. These patients all had highly impaired liver function, with model for end-stage liver disease scores of 22 or higher[42]. In two subsequent studies enrolling patients with hepatic decompensation, no cases of lactic acidosis were reported[43,44].
Efficacy of tenofovir in real life practice
In the multicenter European cohort study, 374 consecutive NA-naïve patients receiving tenofovir (245 mg/d) were retrospectively and prospectively followed for a median period of 39 mo. At baseline, median age was 55 years, 35% of patients had cirrhosis, and concomitant diseases were present in 47%[45]. Virological response rates increased over time, reaching 97% at year 4, independent of HBeAg status. Virological breakthrough was reported in 2% of patients, with no potential resistance-associated mutations identified to date. In HBeAg-positive patients, cumulative probability of HBeAg seroconversion at 4 years was 37%. Sixteen patients (17%) cleared HBsAg (11 HBeAg-positive patients), six of whom successfully interrupted tenofovir. Most partial virological responders at week 48 achieved undetectable HBV DNA during additional treatment. Serum creatinine and phosphorus median levels remained unchanged over time. The proportion of patients with an eGFR of < 50 mL/min (as calculated by the Modification of Diet in Renal Disease formula) increased from 2% to 3% (year 4). The TDF dose was reduced in 19 patients (5%) because of a decline in the estimated glomerular filtration rate in 17 and low serum phosphate levels in two. Therapy was discontinued in seven patients (2%) who were switched to ETV. Nine additional patients withdrew from TDF and switched to ETV because of non-renal-related side effects. HCC developed in 10 compensated cirrhotics (4 year cumulative probability: 17%, 4.2%/year) and in six non-cirrhotics (4 year cumulative probability: 4%, 1%/year), while no cirrhotics clinically decompensated[45].
Management of antiviral drug resistance
The management of treatment failure has changed significantly in recent years due to the availability of potent antivirals. An appropriate rescue therapy should be initiated with the most effective antiviral drug without cross-resistance to reduce the risk of selecting multiple drug-resistant viral strains (Table 3)[46]. In the past years, the add-on strategy was the therapeutic approach recommended by guidelines in order to prevent the emergence of multi-drug resistant strains and raising the resistance barrier. However, with the availability of more potent drugs, such as entecavir and tenofovir, there is a trend to recommend a switch to a complementary drug with a high barrier to resistance. Both options are considered in the recent EASL guidelines (Table 4)[6]. The switch strategy does not apply to patients who have been exposed to multiple monotherapies; these patients should be treated with add-on strategies in order to minimize the risk of subsequent treatment failure.
Table 3.
Cross-resistance data for the most frequent resistant hepatitis B virus variants[43]
| HBV variant | LVD | LdT | ETV | ADV | TDF |
| Wild-type | S | S | S | S | S |
| M204I/V | R | R | I | S | S |
| L180M + M204V | R | R | I | S | S |
| A181T/V | R | R | S | R | I |
| N236T | S | S | S | R | I |
| A181T/V + N236T | R | R | S | R | R |
| L180M + M204V/I ± I179T ± T184G ± S202I/G ± M250I/V | R | R | R | S | S |
HBV: Hepatitis B virus; LVD: Lamivudine; LdT: Telbivudine; ETV: Entecavir; ADV: Adefovir; TDF: Tenofovir; S: Sensitive; I: Intermediate/reduced susceptibility; R: Resistant.
Table 4.
European Association for the Study of the Liver 2012 Guidelines recommendations in resistant patients[6]
| Resistance | Action |
| LAM resistance | Switch to TDF (add ADV if TDF not available) |
| ADV resistance | If patient was NA naive before ADV: switch to ETV or TDF; |
| ETV may be preferred in such patients with high viremia | |
| If patient had prior LAM resistance: switch to TDF and add a nucleoside analogue | |
| LdT resistance | Switch to or add TDF (add ADV if TDF not available) |
| ETV resistance | Switch to or add TDF (add ADV if TDF not available) |
| TDF resistance | TDF resistance not detected to date: add a nucleoside analogue |
| Switch to ETV if patient had no prior LAM resistance or add ETV in patients with LAM resistance |
LAM: Lamivudine; ADV: Adefovir dipivoxil; TDF: Tenofovir; LdT: Telbivudine; ETV: Entecavir.
NA treatment discontinuation
In HBeAg-positive patients with documented HBeAg seroconversion, NA-treatment can be discontinued after 6-12 mo consolidation therapy[6-8], although the optimal duration of consolidation treatment is not clearly defined. However, the long-term durability of HBeAg seroconversion induced by NAs is controversial and high relapse rates have been reported, suggesting that long-term continuation of NA-treatment, irrespective of the occurrence of HBeAg seroconversion, appears to be necessary[47].
Overall, the ideal end-point for stopping NA-treatment is HBsAg loss; however, the likelihood of HBsAg clearance is very low in clinical practice[6-8]. Studies are underway to determine if it is possible to successfully combine the potent effects of NAs with Peg-IFN to increase the HBsAg clearance rates and allow more patients to stop therapy. Recent reports propose quantification of serum HBsAg levels together with serum HBV DNA levels for predicting the outcome after treatment discontinuation in individual patients and thus whether therapy can be safely stopped. Petersen and colleagues showed that stopping long-term NA-therapy in HBeAg-negative CHB patients without advanced liver disease might be an option for patients with HBsAg titers < 500 IU/mL since these selected patients developed a high rate of HBsAg loss off-therapy.
CONCLUSION
Chronic hepatitis B remains a serious clinical problem because of its worldwide distribution and potential adverse sequelae. Over the last decades, treatment of CHB has greatly advanced due to the availability of safe and effective drugs and new standards of care and guidelines have been developed. Both Peg-IFN and two NAs, entecavir and tenofovir, can currently be prescribed as first-line monotherapy for CHB.
Peg-IFN treatment is the only short-term treatment strategy which provides significant off-treatment sustained responses, including loss of HBsAg. However, as Peg-IFN is effective in 20%-30% of patients, it should be considered only for patients with an elevated possibility of response based on pre-treatment and on-treatment factors. In particular, quantitative serum HBV-DNA and HBsAg levels may be suitable to identify patients early who are unlikely to benefit from Peg-IFN early during the treatment course, thereby avoiding unnecessary therapy. Nevertheless, despite this individualized and response-guided approach, increasing the cost-effectiveness of Peg-IFN therapy remains a clinical challenge. Combining Peg-IFN with NAs appears to be the most appealing approach to increase the efficacy of antiviral therapy and new trials on a combination of Peg-IFN with ETV or TDF are required.
Currently, NAs represent the treatment option most often used in the majority of CHB patients. TDF and ETV suppress HBV replication in most treatment-naïve field practice patients with CHB but fail to prevent HCC development, independent of liver disease severity. NA long-term administration raises several concerns: the patient’s commitment to lifelong treatment, adherence, long-term safety, drug resistance in the long-term and costs. Different strategies combining Peg-IFN with ETV or TDF might achieve an antiviral synergy and provide new opportunities to increase HBsAg clearance rates and shorten treatment duration.
Finally, development of new antiviral agents targeting other steps in the HBV replication cycle (viral entry, capsid assembly, viral RNA transcription and epigenetic control of cccDNA) and new immune therapies restoring immune response to HBV remain a major research challenge to improve the efficacy of current antiviral therapy and to achieve HBsAg loss and HBV eradication.
ACKNOWLEDGMENTS
The authors are grateful to Ms. Paulene Butts for her assistance in the preparation of the manuscript.
Footnotes
P- Reviewers: Gong ZJ, Faintuch J S- Editor: Gou SX L- Editor: Roemmele A E- Editor: Wang CH
References
- 1.Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat. 2004;11:97–107. doi: 10.1046/j.1365-2893.2003.00487.x. [DOI] [PubMed] [Google Scholar]
- 2.Mommeja-Marin H, Mondou E, Blum MR, Rousseau F. Serum HBV DNA as a marker of efficacy during therapy for chronic HBV infection: analysis and review of the literature. Hepatology. 2003;37:1309–1319. doi: 10.1053/jhep.2003.50208. [DOI] [PubMed] [Google Scholar]
- 3.Chen CF, Lee WC, Yang HI, Chang HC, Jen CL, Iloeje UH, Su J, Hsiao CK, Wang LY, You SL, et al. Changes in serum levels of HBV DNA and alanine aminotransferase determine risk for hepatocellular carcinoma. Gastroenterology. 2011;141:1240–1248, 1248.e1-2. doi: 10.1053/j.gastro.2011.06.036. [DOI] [PubMed] [Google Scholar]
- 4.Chen CJ, Yang HI. Natural history of chronic hepatitis B REVEALed. J Gastroenterol Hepatol. 2011;26:628–638. doi: 10.1111/j.1440-1746.2011.06695.x. [DOI] [PubMed] [Google Scholar]
- 5.Raimondo G, Allain JP, Brunetto MR, Buendia MA, Chen DS, Colombo M, Craxì A, Donato F, Ferrari C, Gaeta GB, et al. Statements from the Taormina expert meeting on occult hepatitis B virus infection. J Hepatol. 2008;49:652–657. doi: 10.1016/j.jhep.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 6.European Association for the Study of the Liver. EASL clinical practice guidelines: Management of chronic hepatitis B virus infection. J Hepatol. 2012;57:167–185. doi: 10.1016/j.jhep.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 7.Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50:661–662. doi: 10.1002/hep.23190. [DOI] [PubMed] [Google Scholar]
- 8.Liaw YF, Leung N, Kao JH, Piratvisuth T, Gane E, Han KH, Guan R, Lau GK, Locarnini S. Asian-Pacific consensus statement on the management of chronic hepatitis B: a 2008 update. Hepatol Int. 2008;2:263–283. doi: 10.1007/s12072-008-9080-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Zonneveld M, Flink HJ, Verhey E, Senturk H, Zeuzem S, Akarca US, Cakaloglu Y, Simon C, So TM, Gerken G, de Man RA, Hansen BE, Schalm SW, Janssen HL. The safety of pegylated interferon alpha-2b in the treatment of chronic hepatitis B: predictive factors for dose reduction and treatment discontinuation. Aliment Pharmacol Ther. 2005;21:1163–1171. doi: 10.1111/j.1365-2036.2005.02453.x. [DOI] [PubMed] [Google Scholar]
- 10.Lau GK, Piratvisuth T, Luo KX, Marcellin P, Thongsawat S, Cooksley G, Gane E, Fried MW, Chow WC, Paik SW, et al. Peginterferon Alfa-2a, lamivudine, and the combination for HBeAg-positive chronic hepatitis B. N Engl J Med. 2005;352:2682–2695. doi: 10.1056/NEJMoa043470. [DOI] [PubMed] [Google Scholar]
- 11.Lau GKK, Piratvisuth T, Luo HX, Marcellin P, Thongsawat S, Cooksley G, Gane E, Fried MW, Popescu M, Wu J. Durability of response and occurrence of late response to peginterferon alpha-2a (40KD) [Pegasys] one year post-treatment in patients with HBeAg-positive chronic hepatitis B. J Hepatol. 2006;44 Suppl 2:S23–S24. [Google Scholar]
- 12.Buster EH, Flink HJ, Cakaloglu Y, Simon K, Trojan J, Tabak F, So TM, Feinman SV, Mach T, Akarca US, Schutten M, Tielemans W, van Vuuren AJ, Hansen BE, Janssen HL. Sustained HBeAg and HBsAg loss after long-term follow-up of HBeAg-positive patients treated with peginterferon alpha-2b. Gastroenterology. 2008;135:459–467. doi: 10.1053/j.gastro.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 13.Buster EH, Hansen BE, Lau GK, Piratvisuth T, Zeuzem S, Steyerberg EW, Janssen HL. Factors that predict response of patients with hepatitis B e antigen-positive chronic hepatitis B to peginterferon-alfa. Gastroenterology. 2009;137:2002–2009. doi: 10.1053/j.gastro.2009.08.061. [DOI] [PubMed] [Google Scholar]
- 14.Piratvisuth T, Marcellin P, Brunetto M, Bonino F, Farci P, Yurdaydin C, Gurel S, Popescu M. Sustained Immune Control 1 Year Post-Treatment With Peginterferon Alfa-2a [40KD] (Pegasys) is Durable up to 5 Years Post-Treatment and is Associated With a High Rate of HBsAg Clearance in HBeAg-Negative Chronic Hepatitis B. Hepatol Int. 2010;4:Abs210. [Google Scholar]
- 15.Marcellin P, Lau GK, Bonino F, Farci P, Hadziyannis S, Jin R, Lu ZM, Piratvisuth T, Germanidis G, Yurdaydin C, et al. Peginterferon alfa-2a alone, lamivudine alone, and the two in combination in patients with HBeAg-negative chronic hepatitis B. N Engl J Med. 2004;351:1206–1217. doi: 10.1056/NEJMoa040431. [DOI] [PubMed] [Google Scholar]
- 16.Piccolo P, Lenci I, Demelia L, Bandiera F, Piras MR, Antonucci G, Nosotti L, Mari T, De Santis A, Ponti ML, et al. A randomized controlled trial of pegylated interferon-alpha2a plus adefovir dipivoxil for hepatitis B e antigen-negative chronic hepatitis B. Antivir Ther. 2009;14:1165–1174. doi: 10.3851/IMP1466. [DOI] [PubMed] [Google Scholar]
- 17.Rijckborst V, ter Borg MJ, Cakaloglu Y, Ferenci P, Tabak F, Akdogan M, Simon K, Raptopoulou-Gigi M, Ormeci N, Zondervan PE, et al. A randomized trial of peginterferon alpha-2a with or without ribavirin for HBeAg-negative chronic hepatitis B. Am J Gastroenterol. 2010;105:1762–1769. doi: 10.1038/ajg.2010.186. [DOI] [PubMed] [Google Scholar]
- 18.Liaw YF, Jia JD, Chan HL, Han KH, Tanwandee T, Chuang WL, Tan DM, Chen XY, Gane E, Piratvisuth T, et al. Shorter durations and lower doses of peginterferon alfa-2a are associated with inferior hepatitis B e antigen seroconversion rates in hepatitis B virus genotypes B or C. Hepatology. 2011;54:1591–1599. doi: 10.1002/hep.24555. [DOI] [PubMed] [Google Scholar]
- 19.Lampertico P, Viganò M, Di Costanzo GG, Sagnelli E, Fasano M, Di Marco V, Boninsegna S, Farci P, Fargion S, Giuberti T, et al. Randomised study comparing 48 and 96 weeks peginterferon α-2a therapy in genotype D HBeAg-negative chronic hepatitis B. Gut. 2013;62:290–298. doi: 10.1136/gutjnl-2011-301430. [DOI] [PubMed] [Google Scholar]
- 20.Janssen HL, van Zonneveld M, Senturk H, Zeuzem S, Akarca US, Cakaloglu Y, Simon C, So TM, Gerken G, de Man RA, Niesters HG, Zondervan P, Hansen B, Schalm SW. Pegylated interferon alfa-2b alone or in combination with lamivudine for HBeAg-positive chronic hepatitis B: a randomised trial. Lancet. 2005;365:123–129. doi: 10.1016/S0140-6736(05)17701-0. [DOI] [PubMed] [Google Scholar]
- 21.Sonneveld MJ, Rijckborst V, Zeuzem S, Heathcote EJ, Simon K, Senturk H, Pas SD, Hansen BE, Janssen HL. Presence of precore and core promoter mutants limits the probability of response to peginterferon in hepatitis B e antigen-positive chronic hepatitis B. Hepatology. 2012;56:67–75. doi: 10.1002/hep.25636. [DOI] [PubMed] [Google Scholar]
- 22.Tseng TC, Yu ML, Liu CJ, Lin CL, Huang YW, Hsu CS, Liu CH, Kuo SF, Pan CJ, Yang SS, et al. Effect of host and viral factors on hepatitis B e antigen-positive chronic hepatitis B patients receiving pegylated interferon-α-2a therapy. Antivir Ther. 2011;16:629–637. doi: 10.3851/IMP1841. [DOI] [PubMed] [Google Scholar]
- 23.Sonneveld MJ, Wong VW, Woltman AM, Wong GL, Cakaloglu Y, Zeuzem S, Buster EH, Uitterlinden AG, Hansen BE, Chan HL, et al. Polymorphisms near IL28B and serologic response to peginterferon in HBeAg-positive patients with chronic hepatitis B. Gastroenterology. 2012;142:513–520.e1. doi: 10.1053/j.gastro.2011.11.025. [DOI] [PubMed] [Google Scholar]
- 24.Wu X, Xin Z, Zhu X, Pan L, Li Z, Li H, Liu Y. Evaluation of susceptibility locus for response to interferon-α based therapy in chronic hepatitis B patients in Chinese. Antiviral Res. 2012;93:297–300. doi: 10.1016/j.antiviral.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 25.Lampertico P, Viganò M, Cheroni C, Facchetti F, Invernizzi F, Valveri V, Soffredini R, Abrignani S, De Francesco R, Colombo M. IL28B polymorphisms predict interferon-related hepatitis B surface antigen seroclearance in genotype D hepatitis B e antigen-negative patients with chronic hepatitis B. Hepatology. 2013;57:890–896. doi: 10.1002/hep.25749. [DOI] [PubMed] [Google Scholar]
- 26.Sonneveld MJ, Hansen BE, Piratvisuth T, Jia JD, Zeuzem S, Gane E, Liaw YF, Xie Q, Heathcote EJ, Chan HL, et al. Response-guided peginterferon therapy in hepatitis B e antigen-positive chronic hepatitis B using serum hepatitis B surface antigen levels. Hepatology. 2013;58:872–880. doi: 10.1002/hep.26436. [DOI] [PubMed] [Google Scholar]
- 27.Piratvisuth T, Marcellin P, Popescu M, Kapprell HP, Rothe V, Lu ZM. Hepatitis B surface antigen: association with sustained response to peginterferon alfa-2a in hepatitis B e antigen-positive patients. Hepatol Int. 2011:Epub ahead of print. doi: 10.1007/s12072-011-9280-0. [DOI] [PubMed] [Google Scholar]
- 28.Rijckborst V, Hansen BE, Cakaloglu Y, Ferenci P, Tabak F, Akdogan M, Simon K, Akarca US, Flisiak R, Verhey E, Van Vuuren AJ, Boucher CA, ter Borg MJ, Janssen HL. Early on-treatment prediction of response to peginterferon alfa-2a for HBeAg-negative chronic hepatitis B using HBsAg and HBV DNA levels. Hepatology. 2010;52:454–461. doi: 10.1002/hep.23722. [DOI] [PubMed] [Google Scholar]
- 29.Rijckborst V, Hansen BE, Ferenci P, Brunetto MR, Tabak F, Cakaloglu Y, Lanza AG, Messina V, Iannacone C, Massetto B, et al. Validation of a stopping rule at week 12 using HBsAg and HBV DNA for HBeAg-negative patients treated with peginterferon alfa-2a. J Hepatol. 2012;56:1006–1011. doi: 10.1016/j.jhep.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 30.Brunetto MR, Marcellin P, Cherubini B, Yurdaydin C, Farci P, Hadziyannis SJ, Rothe V, Regep L, Bonino F. Response to peginterferon alfa-2a (40KD) in HBeAg-negative CHB: on-treatment kinetics of HBsAg serum levels vary by HBV genotype. J Hepatol. 2013;59:1153–1159. doi: 10.1016/j.jhep.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 31.Chang TT, Lai CL, Kew Yoon S, Lee SS, Coelho HS, Carrilho FJ, Poordad F, Halota W, Horsmans Y, Tsai N, et al. Entecavir treatment for up to 5 years in patients with hepatitis B e antigen-positive chronic hepatitis B. Hepatology. 2010;51:422–430. doi: 10.1002/hep.23327. [DOI] [PubMed] [Google Scholar]
- 32.Shouval D, Lai CL, Chang TT, Gadano A, Wu SS, Halota W, Sievert W, Tsai N, Zhang H, Iloeje U. Three years of entecavir (ETV) re-treatment of HBeAg(-) ETV patients who previously discontinued ETV treatment: results from study ETV-901. Hepatology. 2008;48 Suppl 1:722A. [Google Scholar]
- 33.Marcellin P, Heathcote EJ, Buti M, Gane E, de Man RA, Krastev Z, Germanidis G, Lee SS, Flisiak R, Kaita K, et al. Tenofovir disoproxil fumarate versus adefovir dipivoxil for chronic hepatitis B. N Engl J Med. 2008;359:2442–2455. doi: 10.1056/NEJMoa0802878. [DOI] [PubMed] [Google Scholar]
- 34.Marcellin P, Gane E, Buti M, Afdhal N, Sievert W, Jacobson IM, Washington MK, Germanidis G, Flaherty JF, Schall RA, et al. Regression of cirrhosis during treatment with tenofovir disoproxil fumarate for chronic hepatitis B: a 5-year open-label follow-up study. Lancet. 2013;381:468–475. doi: 10.1016/S0140-6736(12)61425-1. [DOI] [PubMed] [Google Scholar]
- 35.Tenney DJ, Rose RE, Baldick CJ, Pokornowski KA, Eggers BJ, Fang J, Wichroski MJ, Xu D, Yang J, Wilber RB, et al. Long-term monitoring shows hepatitis B virus resistance to entecavir in nucleoside-naïve patients is rare through 5 years of therapy. Hepatology. 2009;49:1503–1514. doi: 10.1002/hep.22841. [DOI] [PubMed] [Google Scholar]
- 36.Kitrinos KM, Corsa A, Liu Y, Flaherty J, Snow-Lampart A, Marcellin P, Borroto-Esoda K, Miller MD. No detectable resistance to tenofovir disoproxil fumarate after 6 years of therapy in patients with chronic hepatitis B. Hepatology. 2014;59:434–442. doi: 10.1002/hep.26686. [DOI] [PubMed] [Google Scholar]
- 37.Lampertico P, Soffredini R, Vigano` M, Minola E, Cologni G, Rizzi M, Zaltron S, Vavassori A, Castelli F, Angeli E, et al. 5-year entecavir treatment in NUC-naive, field-practice patients with chronic hepatitis B showed excellent viral suppression and safety profile but no prevention of HCC in cirrhotics. J Hepatol. 2013;58 Suppl 1:S306–S307. [Google Scholar]
- 38.Seto WK, Lam YF, Fung J, Wong DKH, Lai CL, Yuen MF. Serum hepatitis B surface antigen levels during five years entecavir therapy in Asian chronic hepatitis B patients. J Hepatol. 2013;58 Suppl 1:S314. [Google Scholar]
- 39.Zoutendijk R, Reijnders JG, Brown A, Zoulim F, Mutimer D, Deterding K, Petersen J, Hofmann WP, Buti M, Santantonio T, et al. Entecavir treatment for chronic hepatitis B: adaptation is not needed for the majority of naïve patients with a partial virological response. Hepatology. 2011;54:443–451. doi: 10.1002/hep.24406. [DOI] [PubMed] [Google Scholar]
- 40.Zoutendijk R, Reijnders JG, Zoulim F, Brown A, Mutimer DJ, Deterding K, Hofmann WP, Petersen J, Fasano M, Buti M, et al. Virological response to entecavir is associated with a better clinical outcome in chronic hepatitis B patients with cirrhosis. Gut. 2013;62:760–765. doi: 10.1136/gutjnl-2012-302024. [DOI] [PubMed] [Google Scholar]
- 41.Buti M, Morillas RM, Prieto M, Diago M, Pérez J, Solà R, Bonet L, Palau A, Testillano M, García-Samaniego J, et al. Efficacy and safety of entecavir in clinical practice in treatment-naive Caucasian chronic hepatitis B patients. Eur J Gastroenterol Hepatol. 2012;24:535–542. doi: 10.1097/MEG.0b013e3283511287. [DOI] [PubMed] [Google Scholar]
- 42.Lange CM, Bojunga J, Hofmann WP, Wunder K, Mihm U, Zeuzem S, Sarrazin C. Severe lactic acidosis during treatment of chronic hepatitis B with entecavir in patients with impaired liver function. Hepatology. 2009;50:2001–2006. doi: 10.1002/hep.23346. [DOI] [PubMed] [Google Scholar]
- 43.Shim JH, Lee HC, Kim KM, Lim YS, Chung YH, Lee YS, Suh DJ. Efficacy of entecavir in treatment-naïve patients with hepatitis B virus-related decompensated cirrhosis. J Hepatol. 2010;52:176–182. doi: 10.1016/j.jhep.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 44.Liaw YF, Sheen IS, Lee CM, Akarca US, Papatheodoridis GV, Suet-Hing Wong F, Chang TT, Horban A, Wang C, Kwan P, Buti M, Prieto M, Berg T, Kitrinos K, Peschell K, Mondou E, Frederick D, Rousseau F, Schiff ER. Tenofovir disoproxil fumarate (TDF), emtricitabine/TDF, and entecavir in patients with decompensated chronic hepatitis B liver disease. Hepatology. 2011;53:62–72. doi: 10.1002/hep.23952. [DOI] [PubMed] [Google Scholar]
- 45.Lampertico P, Soffredini R, Yurdaydin C, Idilman R, Papatheodoridis GV, Margariti E, Buti M, Esteban R, Zaltron S, Vavassori A, et al. Four years of tenofovir monotherapy for NUC naive field practice European patients suppresses HBV replication in most patients with a favorable renal safety profile but does not prevent HCC in patients with or without cirrhosis. Hepatology. 2013;58 Issue 1:653A. [Google Scholar]
- 46.Zoulim F, Locarnini S. Management of treatment failure in chronic hepatitis B. J Hepatol. 2012;56 Suppl 1:S112–S122. doi: 10.1016/S0168-8278(12)60012-9. [DOI] [PubMed] [Google Scholar]
- 47.Reijnders JG, Perquin MJ, Zhang N, Hansen BE, Janssen HL. Nucleos(t)ide analogues only induce temporary hepatitis B e antigen seroconversion in most patients with chronic hepatitis B. Gastroenterology. 2010;139:491–498. doi: 10.1053/j.gastro.2010.03.059. [DOI] [PubMed] [Google Scholar]


