Abstract
♦ Background: Patients with end-stage renal failure (ESRF) need integrated health care to maintain a desirable quality of life. Studies suggest that post-discharge nurseled telephone support has a positive effect for patients suffering from chronic diseases. But the post-discharge care is under-developed in mainland China and the effects of post-discharge care on patients with peritoneal dialysis have not been conclusive.
♦ Aim: The purpose of this study is to test the effectiveness of postdischarge nurse-led telephone support on patients with peritoneal dialysis in mainland China.
♦ Methods: A randomized controlled trial was conducted in the medical department of a regional hospital in Guangzhou. 135 patients were recruited, 69 in the study group and 66 in the control group. The control group received routine hospital discharge care. The study group received post-discharge nurse-led telephone support. The quality of life (Kidney Disease Quality of Life Short Form, KDQOL-SF), blood chemistry, complication control, readmission and clinic visit rates were observed at three time intervals: baseline before discharge (T1), 6 (T2) and 12 (T3) weeks after discharge.
♦ Results: Statistically significant effects were found for symptom/problem, work status, staff encouragement, patient satisfaction and energy/fatigue in KDQOL-SF and 84-day (12-week) clinic visit rates between the two groups. The study group had more significant improvement than the control group for sleep, staff encouragement at both T2 and T3, and pain at T2 and patient satisfaction at T3. No significant differences were observed between the two groups for the baseline measures, other dimensions in KDQOL-SF, blood chemistry, complication control, readmission rates at all time intervals and clinic visit rates at the first two time intervals.
♦ Conclusions: Post-discharge nurse-led telephone support for patients undergoing peritoneal dialysis is effective to enhance patients’ well-being in the transition from hospital to home in mainland China.
Key words: Peritoneal dialysis, nursing, telephone support, discharge, China
Chronic kidney disease (CKD), especially end-stage renal failure (ESRF) represents a major public health problem in developed and developing countries (1). Healthcare statistics in mainland China show that ESRF has become one of the major health problems in the adult Chinese population (2). Peritoneal dialysis (PD) is a kind of renal replacement therapy (RRT) which is often presented as an easier and less cumbersome dialysis modality (3). However, long-term PD impacts the patient’s physical, psychological and social well-being, leads to frequent re-hospitalization and may impose a considerable burden on patients and families (4), which induces great demands on integrated health and social care to maintain a desirable quality of life, decrease morbidity during the course of the disease and improve health outcomes of ESRF patients (5).
In recent decades, studies have shown that post-discharge care using a nurse-led case management model produces a positive effect for patients suffering from chronic diseases (6,7). Some studies have shown that post-discharge nurse-led care can bring about positive outcomes for ESRF patients (8,9). However, these studies were mainly done in Canada, UK, USA and Hong Kong (6-12). China is undertaking a nursing development plan (2011 - 2015) that explores the establishment of a long-term care services system that gradually extends to the family and community for the elderly and those suffering from chronic diseases (Ministry of Health, 2011). Quan et al. and Xu et al., at Peking University, have performed nurse- or physician-led care management on PD patients and have found positive intervention to be helpful for improving PD patients’ compliance with dietary restriction of salt and fluid intake and controlling some complications such as seasonal variation of blood pressure, anemia or hyperphosphatemia (13-15). However, it is not certain whether a similar post-discharge nurse-led care model is effective in the context of mainland China.
The aim of this study is to develop an original nurseled telephone support model for peritoneal dialysis patients in mainland China who are discharged from the hospital to home. Furthermore, the effects of the nurseled telephone support program in improving the quality of life and reducing hospital readmission of PD patients were also tested.
Methods
Setting and Subject Recruitment
This study was a randomized controlled trial for PD patients conducted in the renal unit of two local regional hospitals in Guangdong province, China. PD patients were sequentially recruited over 18 months in 2010 - 2012. Patients who were Mandarin-speaking, able to communicate and access a telephone after discharge and agreed to participate were included according to our inclusion criteria. Patients receiving intermittent peritoneal dialysis or hemodialysis and those with planned admissions for special treatment procedures were excluded from the study. Patients with Tenckhoff catheters in situ for less than three months were also excluded because the adaptation period required to adjust to the new treatment regimen may bias quality of life measurements. The other exclusion criteria included: patients with psychosis or dementia, patients who are dying or unable to communicate, and those who have been transferred to another unit during their stay in hospital.
Based on repeated measures analysis of variance, an estimated sample size of 180 (90 in each group) was considered adequate to demonstrate the effects of the experimental intervention. We planned to recruit 90 subjects in each arm to allow for a 20% drop-out rate. The design achieved 78% power with a 5% significance level and 0.3 effect size. The patients were assigned to the study or control group using fifty sets of computer-generated random numbers.
Ethical Approval
This study was approved by the research ethics committees of the study hospitals and the university with which the principal investigator was affiliated and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participating patients needed to give their written consent. The participants were identified by codes, which were not associated with their names. Participants were reassured that their decision to participate or not participate in the study would not affect the care they normally received, the information would be kept confidential and anonymous and they reserved the right to withdraw from the study at any time.
Intervention Protocols and Data Collection
Patients in the control group received routine discharge care, which mainly involved a doctor talking to the patients about special points that needed attention when returning home, a telephone hotline service, a set of free self-help printed materials on maintaining healthy lifestyles and a reminder to attend their outpatient clinic appointment.
Patients in the study group received a comprehensive discharge planning protocol prior to discharge and a standardized 6-week post-discharge nurse-led telephone support intervention according to previous studies, mainly by Wong, in Hong Kong (8,16). First, the patient’s physical, social, cognitive and emotional needs based on the Omaha System (17) were assessed comprehensively and an individualized education program was conducted by the nurse case manager prior to discharge to strengthen and consolidate past learning experiences, clarify misconceptions and optimize health outcomes according to Wong’s previous reports (8,18). After discharge, nurse case managers began telephonecall contact with patients weekly for six consecutive weeks based on Brooten’s concept and Wong’s research (16,19,20). The first call was conducted within 72 hours after discharge to assess the patient’s status and to give advice as this timeframe is considered the critical period of transition from hospital to home. The content of each telephone call was guided by the protocol and the specific problems identified in the predischarge assessment. The case manager discussed with the patient any problems they encountered, and if necessary made an appropriate referral. The telephone conversations were audiotaped for documentation and reviewed to ensure adequacy and consistency of the interventions.
Data were collected at T1 (on discharge), T2 (6 weeks post-discharge, after completion of the intervention) and T3 (12 weeks post-discharge) which was referenced from Wong’s study of patients with PD (8).
Data Collection for Baseline Demographic and Clinical Characteristics
Demographic and clinical variables including gender, age, marital status, education, occupation, type of housing, home condition, religion, perceived financial status, care-taking support, comorbidity, reason for end-stage renal failure and years on continuous ambulatory peritoneal dialysis were collected from charts and interviews at T1. These measures had been validated in Wong’s study (8). The test-retest reliability was 0.95 and the inter-rater reliability was 0.90.
Data Collection for Quality of Life
The Kidney Disease Quality of Life Short Form (KDQOL-SF, version 1.3, RAND, Santa Monica, CA, USA) specifically for patients receiving dialysis was performed at three different time points to assess the quality of life of patients (21,22). The KDQOL-SF has been reverse-translated into Chinese and was found to be valid for patients in several studies (8,18,23,24). All subscale scores were standardized and transformed so that higher scores represented a desirable quality of life when compared to the lower scores.
Complication Control and Blood Chemical Changes
The observed complication control of participants within 42 days (6 weeks) and 84 days (12 weeks) post-discharge included presence of edema, existence of peritonitis, catheter infections and weight gain. The information provided by the subjects was validated against the documentation in their charts. The ICC inter-rater reliability was 0.93. Blood chemical changes including urea, creatinine, sodium, potassium, phosphate and albumin were investigated to reflect the existence of complications according to some existing reports (25,26).
Health Service Utilization
Patients were asked to report their health service utilization including number of hospitalizations and attended outpatient clinics within 42 days (6 weeks) and 84 days (12 weeks) post-discharge. Days between index discharge and readmission were extracted from the hospital information systems.
Data Analysis
Data were analyzed using SPSS 17.0 for Windows (SPSS Inc., Chicago, IL, USA). Chi-square test and independent t-test were used to compare the background characteristics of the study group and the control group. The independent t-test was used to compare the mean scores of each outcome measure between groups at each time period. General linear model (GLM) measures were used to determine between-groups (study vs control) effects, within-groups (three times) effects and interaction (group × time) effects. All p values were two-tailed. The level of significance was set at 0.05.
Results
Baseline Data
During the data collection period, 186 patients met the eligibility criteria and were assessed by the hospital nurse for recruitment into the study. Twenty-six patients who failed to meet the inclusion criteria were excluded. Of these, 16 were transferred to hemodialysis before discharge. Of the remaining ten, six refused to participate, while four were unable due to their physical condition. The 160 patients who joined the study were randomly assigned to either the study or control group. There were 80 patients in each of the treatment arms. At week 12, 69 of the 80 (86.3%) study patients and 66 of the 80 (82.5%) controls had completed the follow-up questionnaires. A total of 135 patients completed the protocol and were included in the analysis (Figure 1).
Figure 1 —
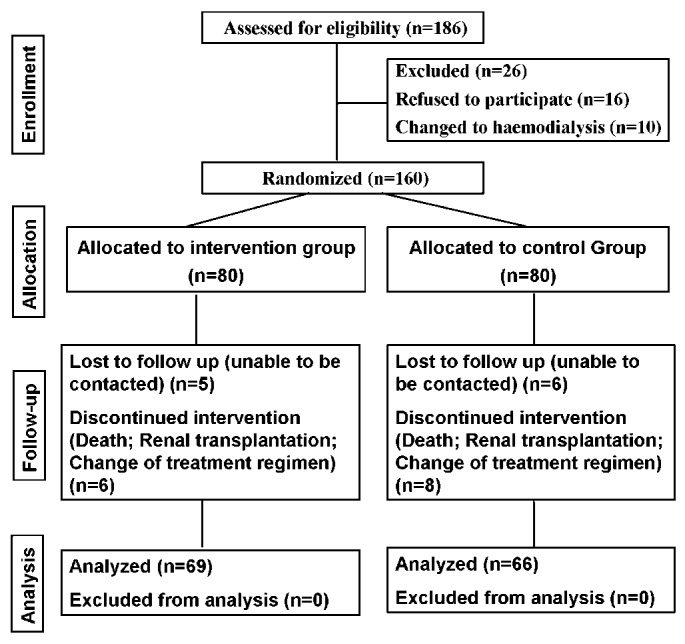
The Consort flowchart for the study.
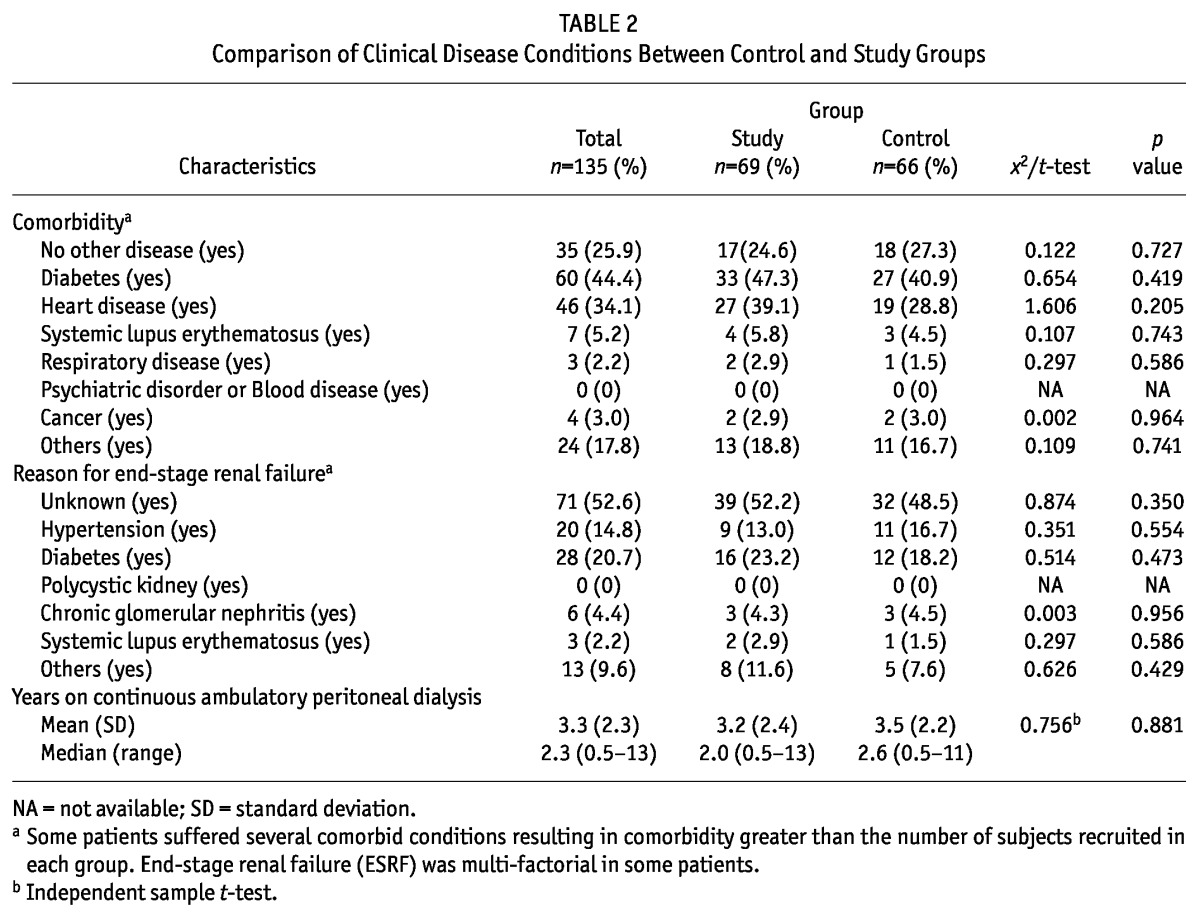
Table 1 and Table 2 display the comparison of baseline demographic data and clinical data between the control and study groups respectively. Among these 135 patients, 79 (58.5%) were male and 56 (41.5%) were female. Their ages ranged from 22 to 76 years, with a mean of 56.3 years (SD = 12.4). Most participants were married (76.3%), 8.9% were single, and others were divorced or widowed. The mean number of years on PD was 2.3, ranging from 0.5 to 13 years. The basic education level was not very high. About half of them (53.3%) were retired. Most of them lived in self-owned flats (91.9%). Chi-square comparison and t-test showed no statistically significant differences between the study and control group in terms of clinical and demographic variables. Successful randomization was therefore confirmed according to the above baseline data.
TABLE 1.
Comparison of Demographic Characteristics Between Groups
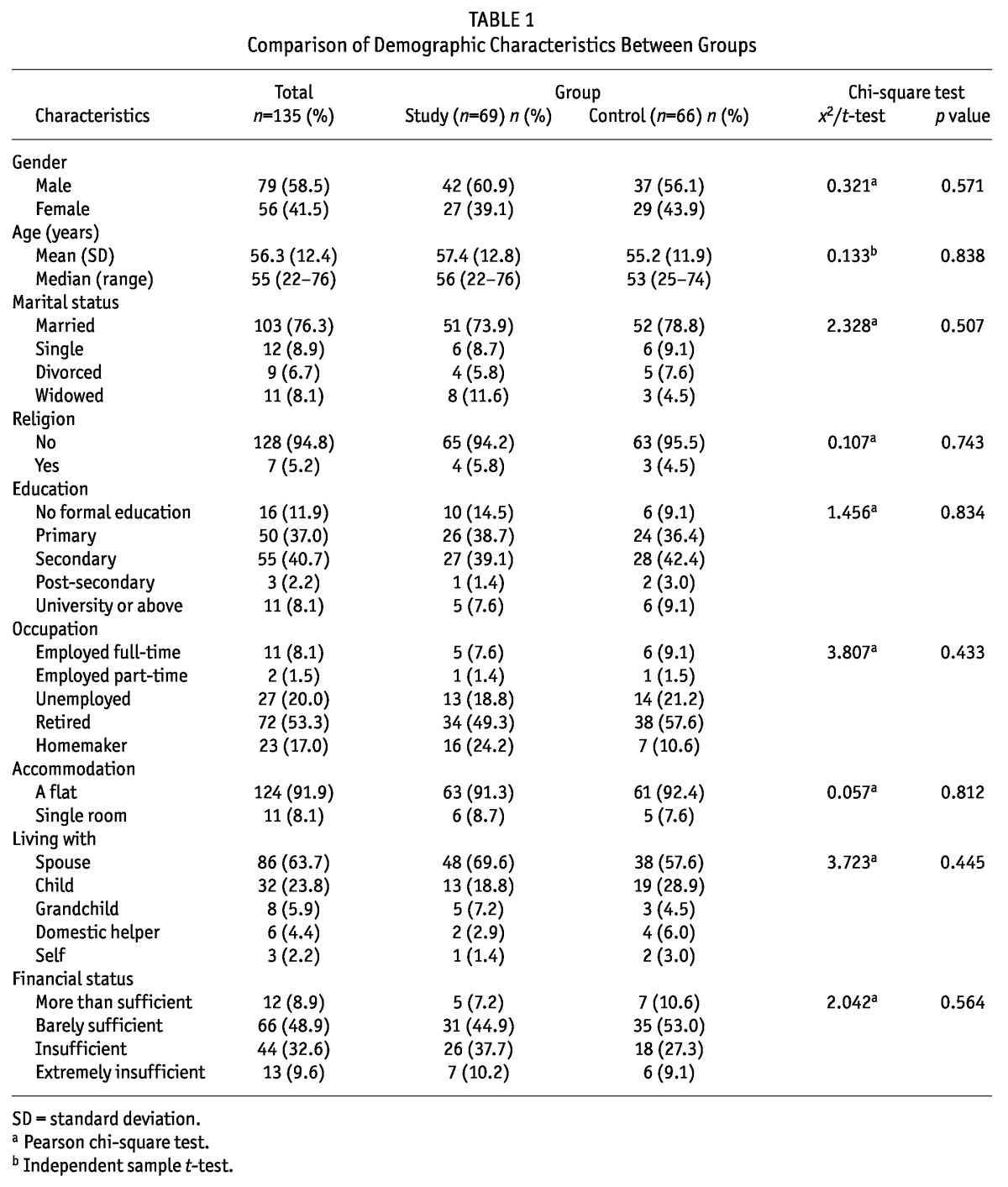
TABLE 2.
Comparison of Clinical Disease Conditions Between Control and Study Groups
Effects of Intervention on Quality of Life
The effects of post-discharge nurse-led telephone support on quality of life were measured by the KDQOL-SF displayed in Table 3. Our results showed that there were no significant differences between the two groups at the baseline measures. The overall between-group differences were significant in symptom/problem, work status, staff encouragement, patient satisfaction and energy/fatigue, indicating that the study group showed more improvement than the control group. The between-groups effects for pain and general health perception showed a trend towards statistical significance (p = 0.05 and p = 0.07 respectively).
TABLE 3.
Comparison of Kidney Disease Quality of Life (KDQOL) Results
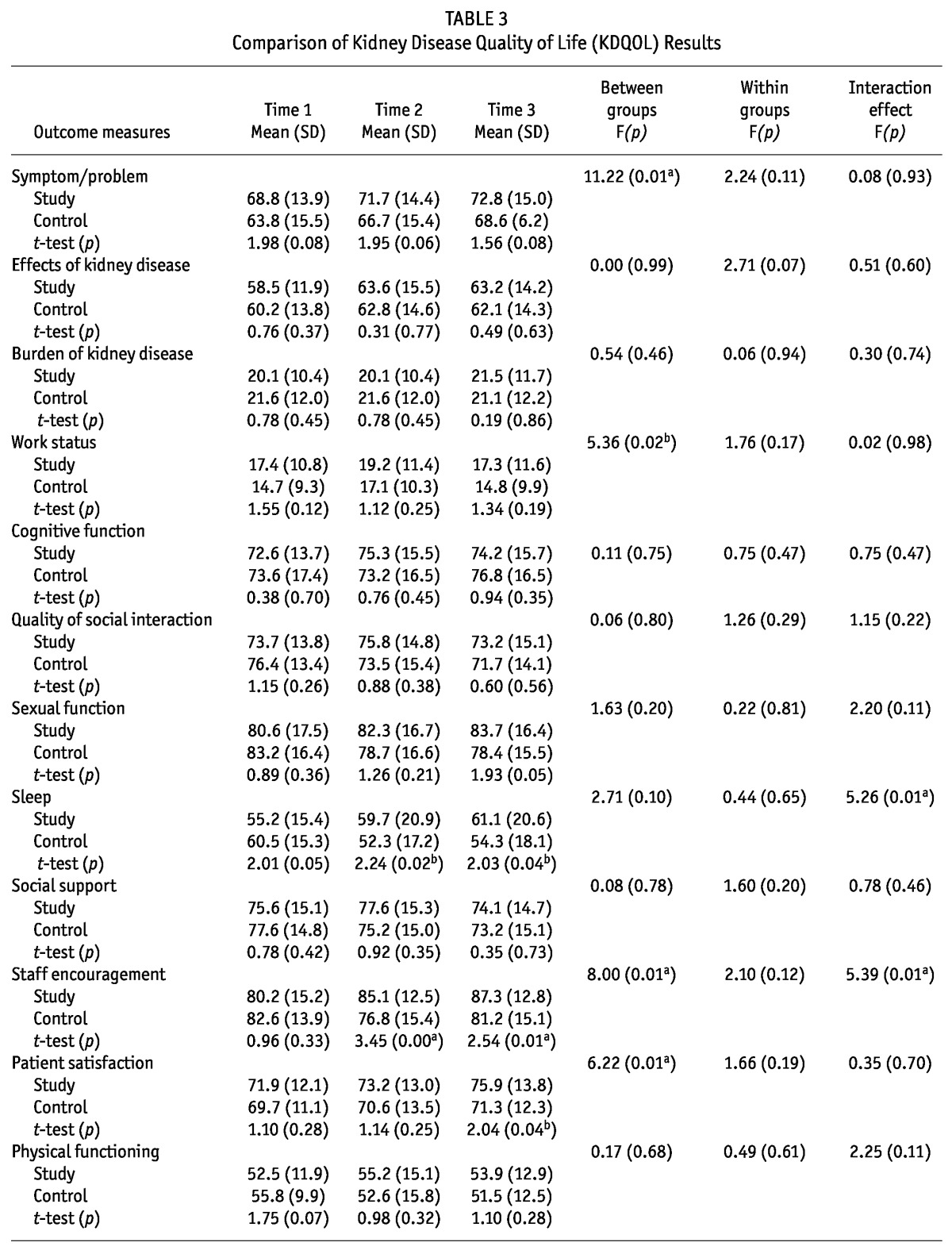
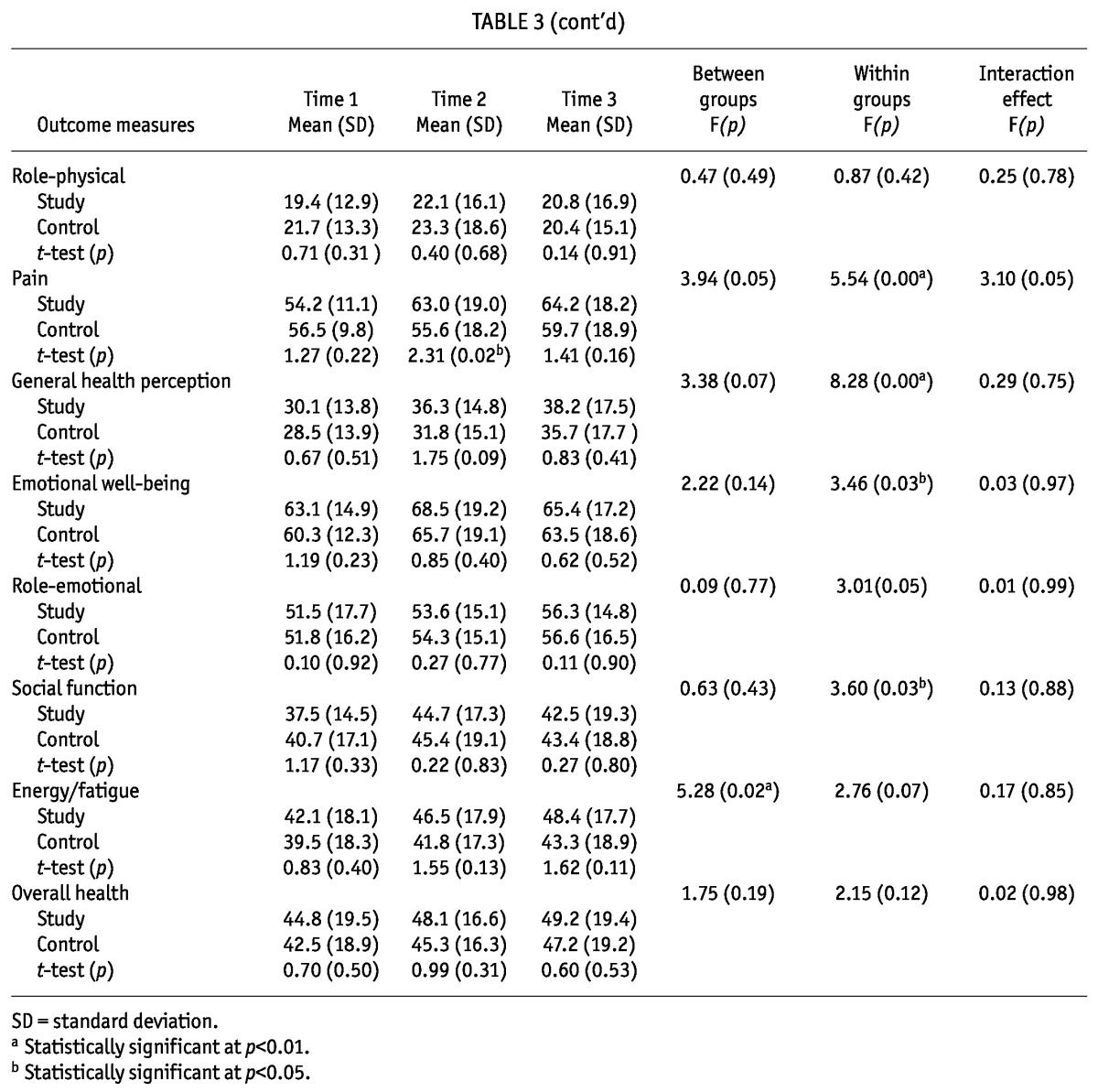
To determine the attribution of time effects for the two groups, repeated measures were conducted separately for the groups at the three time intervals. A few items such as pain, general health perception, emotional well-being and social function showed within-group differences, that is, both groups had improvements over time. For sleep, staff encouragement and pain, the study group had more significant improvements than the control group at T2. At T3, significant differences were noted for sleep, staff encouragement and patient satisfaction with no between-group or within-group significance for these items. For role-emotional and energy/fatigue, the between-groups effect showed a trend towards statistical significance (p = 0.05 and p = 0.07 respectively).
The variables that demonstrated interaction effects (p < 0.05) were quality of sleep and staff encouragement. The statistically significant interaction effect indicated that rates of improvement between the two groups across time were highly different, further implying that one approach worked better at one point than another (27). For pain, a trend towards statistical significance (p = 0.05) between groups and interaction effects were observed.
Effect of Intervention on Blood Chemistry and Complication Control
Blood urea, creatinine, sodium, potassium, phosphate and albumin concentration were used to indicate blood chemistry changes in the two groups. The presence of edema, existence of peritonitis, catheter infections, exit-site condition and weight gain were observed as the complication control of the participants within 42 days (6 weeks) and 84 days (12 weeks) post-discharge. Statistical analysis showed there were no significant differences over time within groups or between groups for blood chemistry and complication control (data not shown), and all the readings were within acceptable range for PD patients.
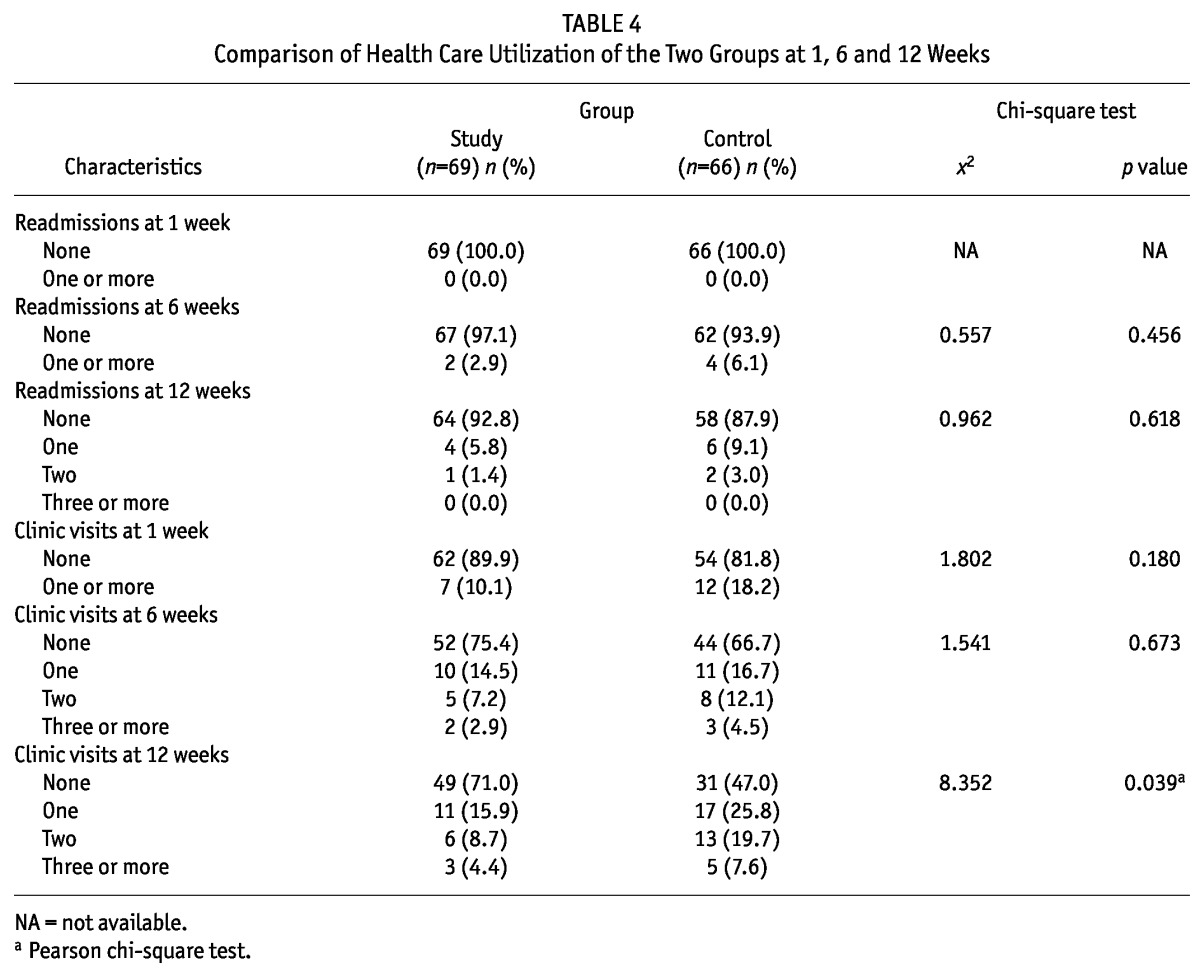
Effect of Intervention on Health-Care Utilization
We compared the baseline data between the readmitted and non-readmitted cases. There was no significant difference detected, so no need was accounted for covariate for subsequent computations. The 7-day (one-week), 42-day (6-week) readmission rates and the 84-day readmission rates showed no significant differences (see Table 4). The intention-to-treat result also showed a lower readmission rate with the study group but the result was not significant. There was a statistically significant difference in the 84-day (12-week) clinic visit rates between the two groups.
TABLE 4.
Comparison of Health Care Utilization of the Two Groups at 1, 6 and 12 Weeks
Discussion
In the present study, we test the effect of nurse-led telephone support on PD patients in mainland China. In agreement with some other studies performed overseas (8,21,28), our results confirmed that post-discharge nurse-led telephone support is helpful for some aspects of quality of life and reducing readministration and clinic visits of PD patients in Guangdong.
We first observed the effects of post-discharge nurseled support on the quality of life of PD patients using the KDQOL-SF scale and the results showed that the scores of quality of life in the study group were higher than those in the control group in about 50% of the general dimensions in the KDQOL-SF. Statistically significant effects were observed in disease-specific dimensions such as symptoms, work status, staff encouragement, patient satisfaction and energy/fatigue between the two groups. Further repeated measures analysis found that both groups have within-group differences for a few items such as pain, general health perception, emotional well-being and social function, indicating that such items improved in both groups over time. These results demonstrated the positive role of nurse-led case management on quality of life of PD patients, which may be a result of encouraging patients and their families to adopt meaningful behavioral change. However, these results are somewhat different from Wong’s existing reports in Hong Kong (8,18). We proposed that the different results may be caused by cultural factors that create additional challenges for mainland Chinese patients’ adherence to treatment. For example, Chinese people are likely to have less adequate knowledge about medication schedules for disease and they prefer to control chronic diseases using Chinese medicine, herbs and diet, in keeping with their cultural beliefs (29) rather than medication. The exact causes of these differences need our further study.
In the present study, we also observed the interaction effects of post-discharge nurse-led telephone support on dimensions in the KDQOL-SF. The results showed that the interaction effects were observed in quality of sleep and staff encouragement. Sleep disturbances could create anxiety and mood disturbance, and long-term insomnia is related to psychiatric disorders such as anxiety, depressive symptoms, pain frequency and lower health-related quality of life (30,31). During our post-discharge nurseled telephone intervention, we give the patient early detection and intervention for sleep disturbance and post-hoc analysis showed that for sleep, staff encouragement and pain, the study group had more significant improvement than the control group at 6 weeks post-discharge and a similar trend for sleep was observed at 12 weeks. These results demonstrated the importance of sleep quality in quality of life in patients.
Besides the parameters shown in the KDQOL-SF, we observed the effects of post-discharge nurse-led telephone support on other dimensions such as biological changes and complication controls that would be related to quality of life. The results did not show significant changes in blood chemistry and complication control in the study group. These results are in line with Wong’s study on continuous ambulatory peritoneal dialysis patients in Hong Kong (8,18) and in contradiction with some other studies (13-15,32,33). As blood chemistry and complication control are related factors that could influence the clinical outcomes, many of them such as low levels of albumin and hemoglobin in the blood are associated with low quality of life (34,35). We speculated that, in the present study, the above inconsistent results were possibly related to different observed aspects of symptoms, small sample size, and short follow-up period and we did not make further adherence analysis.
To confirm the effects of nurse-led telephone support on improving the quality of life for PD patients, we made a comparison of health care utilization, including readmission rates and clinic visit rates after patient discharge, between the two groups at three different time intervals. The results showed that except for 84-day (12-week) clinic visit rates, no significant differences were detected in readmission rates and clinic visit rates between the two groups. This may be attributed to the baseline clinical disease conditions between the study and control group, which showed no significant differences at the beginning.
There are a number of limitations to our present study. First, this study took place in two local hospitals in Guangzhou, China. With a small sample size, relatively short duration of follow-up and different background from other places, the effects of intervention cannot be generalized to the whole population of patients in mainland China. Second, the intervention of this study was performed mostly according to the existing literature from other countries and Hong Kong. More vigorous tests of construct validity have not been conducted in mainland China. For example, before enrollment in this study, patients and their family members were invited by the training nurse managers to discuss some realistic action plans in the recovery process and get some related messages, including exercise regimen, medication, fluid and diet adherence behaviors, technical procedures for home peritoneal dialysis and avoidance of infection. The run-in period to exclude the effect of prior treatment should be controlled more rigorously. Third, outcome measures used in this study relied on self-reporting by the clients and we did not have a mechanism to validate if the self-reporting truly reflected actual practice. Meanwhile, a double-blind design would have the possibility of contamination of the placebo group during telephone conversations. Fourth, we did not collect non-adherence level and clinical data that provides inference to the level of renal disease risk and adherence, other than the health assessment data which have already been reported in the paper.
Conclusion
In conclusion, the present study evaluated the effectiveness of a post-discharge nurse-led telephone support model on improving quality of life for PD patients in mainland China. This study adds to the literature about the value of nurse-led telephone support and provides a structured protocol for use and further testing in mainland China. It will be helpful for China to develop accessible health care services, which refers to obtaining the right services at the right time to promote improved health outcomes. Further studies will be performed on patients’ compliance with the medication and the relationship to the clinic conditions and quality of life in PD patients and other chronic patients.
Disclosures
The authors have no financial conflicts of interest to declare.
Acknowledgments
The work was partly supported by Outstanding young talents training project of Guangdong Province (Grant No. LYM11035) and the Guangdong Natural Science Foundation, China (Grant No. S2011040005590). We would like to thank the following renal nurses for collecting data: Hongchun Chen in the department of nephrology at the General Hospital of Guangzhou Military Command of PLA, Yan Li and Meini Fang, in the department of organ transplantation, Nanfang Hospital, Southern Medical University. We are grateful to all patients who contributed to the study.
References
- 1. Sharif A, Baboolal K. Update on dialysis economics in the UK. Perit Dial Int 2011; 31(Suppl 2):S58–62 [DOI] [PubMed] [Google Scholar]
- 2. Li PK, Chow KM, Szeto CC. Is there a survival advantage in Asian peritoneal dialysis patients? Int J Artif Organs 2003; 26(5):363–72 [DOI] [PubMed] [Google Scholar]
- 3. Sinnakirouchenan R, Holley JL. Peritoneal dialysis versus hemodialysis: risks, benefits, and access issues. Adv Chronic Kidney Dis 2011; 18(6):428–32 [DOI] [PubMed] [Google Scholar]
- 4. Brown EA. Can quality of life be improved for the increasing numbers of older patients with end-stage kidney disease? Expert Rev Pharmacoecon Outcomes Res 2010; 10(6):661–6 [DOI] [PubMed] [Google Scholar]
- 5. Dimkovic N, Aggarwal V, Khan S, Chu M, Bargman J, Oreopoulos DG. Assisted peritoneal dialysis: what is it and who does it involve? Adv Perit Dial 2009; 25:165–70 [PubMed] [Google Scholar]
- 6. Naylor MD. A decade of nurse led telephone support research with vulnerable elders. J Cardiovasc Nurs 2000; 14(3):1–14; quiz 88-9: [DOI] [PubMed] [Google Scholar]
- 7. Shu CC, Hsu NC, Lin YF, Wang JY, Lin JW, Ko WJ. Integrated post-discharge nurse led telephone support in a hospitalist system to improve discharge outcome: an experimental study. BMC Med 2011; 9(1):96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chow SK, Wong FK. Health-related quality of life in patients undergoing peritoneal dialysis: effects of a nurse-led case management programme. J Adv Nurs 2010; 66(8):1780–92 [DOI] [PubMed] [Google Scholar]
- 9. Car J, Sheikh A. Telephone consultations. BMJ 2003; 326(7396):966–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Trachtenberg M, Ryvicker M. Research on transitional care: from hospital to home. Home Healthc Nurse 2011; 29(10):645–51 [DOI] [PubMed] [Google Scholar]
- 11. Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The care span: The importance of nurse led telephone support in achieving health reform. Health Aff (Millwood) 2011; 30(4):746–54 [DOI] [PubMed] [Google Scholar]
- 12. McDonagh JE, Kelly DA. The challenges and opportunities for nurse led telephone support research. Pediatr Transplant 2010; 14(6):688–700 [DOI] [PubMed] [Google Scholar]
- 13. Quan L, Dong J, Li Y, Zuo L. The effectiveness of intensive nursing care on seasonal variation of blood pressure in patients on peritoneal dialysis. J Adv Nurs 2012; 68(6):1267–75 [DOI] [PubMed] [Google Scholar]
- 14. Xu Y, Dong J, Zuo L. Is frequency of patient-physician clinic contact important in peritoneal dialysis patients? Perit Dial Int 2009; 29(Suppl 2):S83–9 [PubMed] [Google Scholar]
- 15. Quan L, Xu Y, Luo SP, Wang L, LeBlanc D, Wang T. Negotiated care improves fluid status in diabetic peritoneal dialysis patients. Perit Dial Int 2006. Jan-Feb; 26(1):95–100 [PubMed] [Google Scholar]
- 16. Brooten D, Youngblut J. Nurse dose as a concept. Imagethe J Nursing Scholarship 2006; 38(1):94–9 [DOI] [PubMed] [Google Scholar]
- 17. Martin K. The Omaha System: A Key to Practice, Documentation and Information Management, 2nd ed. St. Louis: Elsevier; 2005. [Google Scholar]
- 18. Wong FK, Chow SK, Chan TM. Evaluation of a nurse-led disease management programme for chronic kidney disease: a randomized controlled trial. Int J Nurs Stud 2010; 47(3):268–78 [DOI] [PubMed] [Google Scholar]
- 19. Brooten D, Youngblut JM, Deatrick J, Naylor M, York R. Patient problems, advanced practice nurse (APN) interventions, time and contacts among five patient groups. J Nursing Scholarship 2003; 3(1):73–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wong FKY, Chow S, Chang K, Lee A, Liu J. Effects of nurse follow-up on emergency room revisits: a randomized controlled trial. Soc Sci Med 2004; 59(11):2207–18 [DOI] [PubMed] [Google Scholar]
- 21. Hays R, Kallich J, Mapes D, Coons S, Carter W. Development of the kidney disease quality of life (KDQOLTM) instrument. Quality of Life Research 1994; 3(5):329–38 [DOI] [PubMed] [Google Scholar]
- 22. Hays R, Kallich JD, Mapes DL, Coons SJ, Amin N, Carter WB. Kidney Disease Quality of Life Short Form (KDQOL-SFTM): A Manual for Use and Scoring. Santa Monica, CA: RAND; 1997. [Google Scholar]
- 23. Monica CA, Li CM. Development of the Hong Kong Chinese Version of the Kidney Disease Quality of Life Short Form (KDQOL-SF) Instrument. Unpublished master’s thesis. The Hong Kong Polytechnic University, Hong Kong: 1998. [Google Scholar]
- 24. Ma ZD, Zheng ZH, Zhang DH, Hao YT, Ye RG, Lou TQ, et al. Multi-center investigation of quality of life in hemodialysis and peritoneal dialysis patients. Chin J Nephrol 2004; 20(6):400–5 [Google Scholar]
- 25. Vlaminck H, Maes B, Jacobs A, Reyntjens S, Evers G. The dialysis diet and fluid non-adherence questionnaire: validity testing of a self-report instrument for clinical practice. J Clin Nurs 2001; 10(5):707–14 [DOI] [PubMed] [Google Scholar]
- 26. Wong FKY, Chung L. Establishing a model for nurse-led clinic: structure, process and outcome. J Adv Nurs 2006; 53(3):358–69 [DOI] [PubMed] [Google Scholar]
- 27. Portney L, Watkins M. Foundations of Clinical Research: Applications to Practice, 3rd ed. Upper Saddle River, NJ: Pearson; 2008. [Google Scholar]
- 28. Naylor M, Keating SA. Transitional care. Am J Nurs 2008; 108(9 Suppl):58–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zhao Y, Lee WM, Wong FKY. China (People’s Republic of). In D’Avanzo CE, Geissler EM, eds. Cultural Health Assessment. St Louis, MO: Mosby; 2008: 158–64 [Google Scholar]
- 30. Driscoll H, Serody L, Patrick S, Maurer J, Bensasi S, Houck P, et al. Sleeping well, aging well: a descriptive and cross-sectional study of sleep in “successful agers” 75 and older. Am J Geriatric Psych 2008; 16(1):74–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Edwards RR. Duration of sleep contributes to next-day pain report in the general population. Pain 2008; 137(1):202–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lee JK, Grace KA, Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA 2006; 296(21):2563–71 [DOI] [PubMed] [Google Scholar]
- 33. Pladevall M, Keoki WL, Potts LA, Divine G, Xi H, Lafata J. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care 2004; 27(12):2800–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Baiardi F, Degli E, Cocci R, Fabbri A, Sturani A, Valpiani G, et al. Effects of clinical and individual variables on quality of life in chronic renal failure patients. J Nephr 2002; 15(1):61–7 [PubMed] [Google Scholar]
- 35. Bakewell A, Higgins R, Edmunds M. Quality of life in peritoneal patients: decline over time and association with clinical outcomes. Kidney Int 2002; 61(1):239–49 [DOI] [PubMed] [Google Scholar]


