Abstract
Peritonitis is still known as an important complication of continuous ambulatory peritoneal dialysis (CAPD). Multi-drug resistant (MDR) Acinetobacter baumannii is an increasing problem worldwide. Moreover, the increasing reports of carbapenem-resistant A. baumannii strains is common. Although peritoneal dialysis-related peritonitis with MDR A. baumannii is rarely reported, infection with this organism always results in serious peritonitis and increases the possibility of dropout or mortality. Here, we present 7 cases of peritonitis caused by A. baumannii species. Among those 7 cases, 2 involved MDR A. baumannii, and 1 involved a carbapenem-resistant strain. All the MDR bacterial infections failed treatment. We also review the literature about Acinetobacter peritonitis and current treatment protocols.
Key words: Peritonitis, Acinetobacter baumannii, multi-drug resistance, peritonitis treatment
Acinetobacter baumannii, a gram-negative bacterium, has been identified as a significant cause of antibiotic-resistant infections and has emerged as one of the most troublesome pathogens for health care institutions (1). Multidrug resistant (MDR) A. baumannii is a growing problem worldwide, and reports of carbapenem-resistant A. baumannii strains are common. Some A. baumannii strains have been found to be resistant to all known antibiotics (2).
Although MDR A. baumannii is rarely reported in association with peritonitis in peritoneal dialysis (PD) patients, when this organism is present, it results in serious infection and increases the possibility of dropout or mortality (3-5). Here, we present 7 cases of peritonitis caused by A. baumannii. Of those cases, 2 involved MDR A. baumannii, and 1 was caused by a carbapenem-resistant strain. Refractory peritonitis in 3 patients resulted in prolonged hospitalization, the need for catheter removal, and finally PD dropout and a switch to hemodialysis. The other 4 patients were cured and continued PD therapy. Acinetobacter peritonitis and its treatment process are particularly concerning.
Case Descriptions
Over a period of 3 years (2009 - 2011), we diagnosed 7 cases of peritonitis attributed to A. baumannii in patients receiving PD. Susceptibility to various classes of antibiotics was tested using the disk diffusion technique. The procedure for peritoneal effluent culture followed International Society for Peritoneal Dialysis recommendations (6).
Of the 7 episodes, 2 were polymicrobial in nature (Table 1). Of the 7 patients, 3 dropped out from PD and switched to hemodialysis, and 1 of the hemodialysis patients died from a cerebral hemorrhage a year later. The other 4 patients were cured and continued PD therapy (Table 2). In all 3 drop-out cases, the infections were attributed to resistant organisms: in 2 patients the organism was MDR A. baumannii, and in 1 (patient 5), the strain was carbapenem-resistant A. baumannii. Resistance to amikacin was found in only 1 of the 4 patients that were cured (Table 1).
TABLE 1.
Characteristics of Peritoneal Effluent Cultures in Seven Peritoneal Dialysis Patients

TABLE 2.
Clinical Data for Seven Patients with A. baumannii Peritoneal Dialysis (PD)-Related Peritonitis
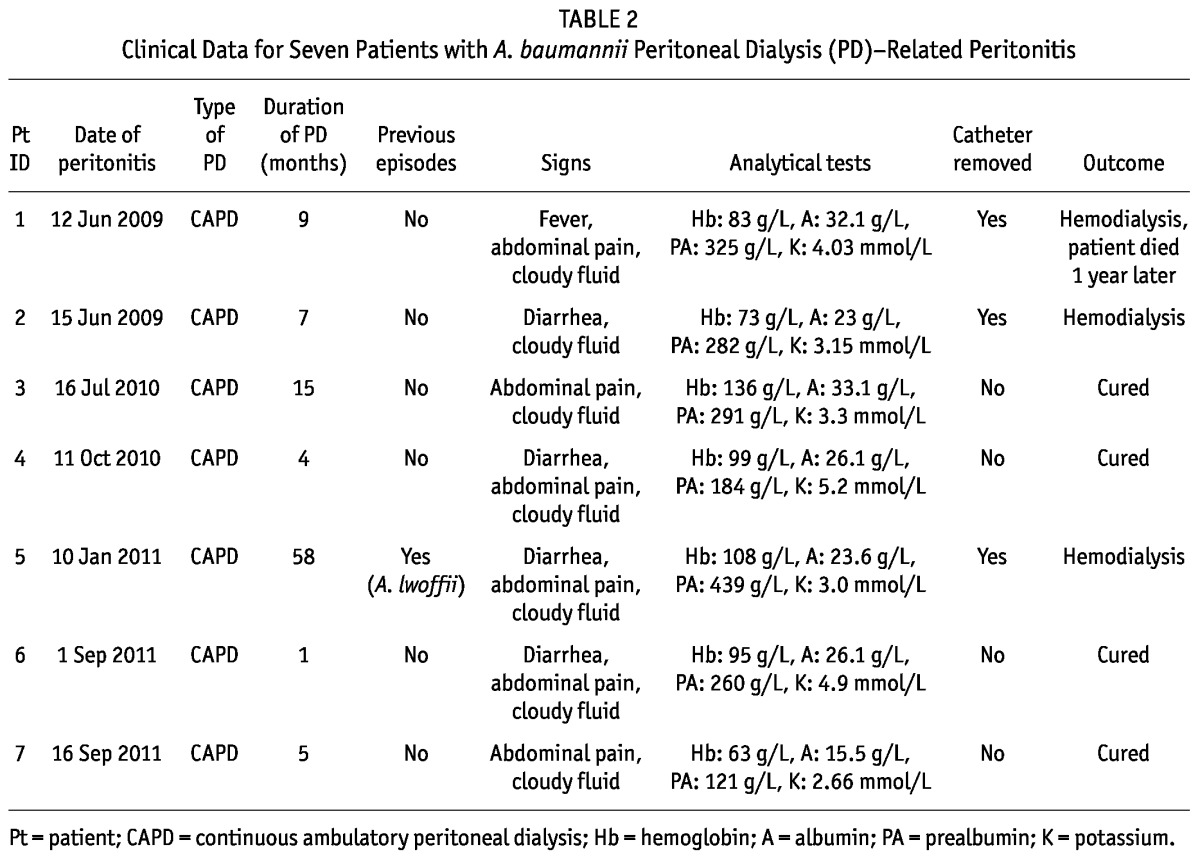
Of the 7 cases, 5 occurred in the patient’s first year of PD (Table 2). Only 1 patient (patient 5) had experienced a previous peritonitis episode: that episode had occurred 20 days earlier, and the diagnosis was peritonitis attributed to A. lwoffii. Antibiotic treatment for 2 weeks was effective, and the white blood cell counts in peritoneal effluent were normal. However, a week later, the patient experienced diarrhea and abdominal pain. Culture of the peritoneal effluent showed A. baumannii that was resistant to many antibiotics, including imipenem (Table 1).
All the cases of A. baumannii infection were community-acquired (Table 2). All patients but 1 (patient 3) were anemic. Serum albumin was below 30 g/L except in 2 patients (patients 1 and 3). All 7 patients had cloudy peritoneal effluent, and abdominal pain was frequent. Diarrhea occurred in 4 cases. Only 1 patient had a fever (Table 2).
During the course of antibiotics in the 4 patients who were cured, white blood cell counts in peritoneal effluent started to decline after 4 days of therapy. However, 1 patient (patient 4) refused to accept continuous therapy and was discharged without any drugs on the 5th day of antibiotic administration. The other 3 cured patients continued treatment for at least 14 days (Table 2).
The patient infected with carbapenem-resistant A. baumannii (patient 5) had previously been infected with A. lwoffii. She also had anemia, hypoproteinemia, and a low body mass index of 16.87. We didn’t think that this patient would be able to survive the recurrent infection, and so her catheter was removed the day the bacterial infection was identified. She was given ciprofloxacin intravenously for 7 days to cure the infection.
Discussion
The outcome of PD-related peritonitis greatly depends on the infecting micro-organism. Gram-positive cocci are still the causative organisms in most cases of peritonitis. Acinetobacter species are seldom involved in PD-related peritonitis, but when they are, delivering effective therapy is difficult (7,8).
When we reviewed PD-related peritonitis cases over a period of 3 years, we found that 72.4% were the result of gram-positive cocci; only 7.6% were attributed to Acinetobacter species. Among the Acinetobacter infections, 87.5% were caused by A. baumannii. Other research showed that the most common Acinetobacter species was A. baumannii and that resistance to numerous drugs in this organism has become a public health problem (1,9). Imipenem and meropenem have traditionally been the antimicrobials most effective against A. baumannii (10), but reports of carbapenem-resistant A. baumannii strains are becoming common.
Standardized terminology to describe drug-resistant bacteria was proposed by a group of international experts and published in Clinical Microbiology and Infection (11). Criteria for classifying Acinetobacter species as MDR, extensively drug-resistant (XDR), or pan-drug-resistant (PDR) were described as follows: “MDR was defined as acquired non-susceptibility to at least one agent in three or more antimicrobial categories, XDR was defined as non-susceptibility to at least one agent in all but two or fewer antimicrobial categories... and PDR was defined as non-susceptibility to all agents in all antimicrobial categories” (11, p. 268). According to those criteria, 2 of the 7 cases of peritonitis in our study (patients 2 and 5) were caused by MDR A. baumannii. In 1 of the 2 cases, the bacterium was resistant to carbapenem. Both cases were treated to no effect, and the catheter was ultimately removed.
In our study, 3 A. baumannii peritonitis episodes resulted in PD dropout, and 4 patients were cured. Of the 3 patients who switched to hemodialysis, 1 died of a cerebral hemorrhage (not from infection). All patients who failed to respond to antibiotics were infected with antibiotic-resistant bacilli. We found 1 specimen resistant to carbapenem. The case in which the bacterium was found to be resistant to amikacin suggests that prompted antibiotic resistance in A. baumannii may be a key factor in refractory peritonitis. Solak et al. (5) reported that a patient with A. baumannii peritonitis that was sensitive only to aminoglycosides and tigecycline died of refractory septic shock. Another 2 patients were administered antibiotic therapy and recovered from non-MDR A. baumannii infection (3,4).
Galvao et al. (12) surveyed 23 episodes of Acinetobacter peritonitis, more than half of which occurred in the patient’s first year of PD. In our study, 5 of 7 patients were infected their first year of PD. In all of the patients except patient 5, the Acinetobacter infection was their first episode of peritonitis. In the study by Galvao and colleagues, Acinetobacter accounted for a second peritonitis episode in 6 patients. Interestingly, the incidence of Acinetobacter peritonitis in that study increased significantly in the first 2 - 3 months after a prior episode of peritonitis (12). In our study, 1 episode of Acinetobacter infection occurred at day 20 after a preceding infection.
The clinical features and outcomes of PD-related peritonitis caused by co-infection with Acinetobacter species and other pathogens have rarely been reported. We had 1 patient with co-infection: in patient 7, the peritoneal effluent culture was positive for both A. baumannii and Staphylococcus epidermidis. That patient was cured, which suggests that co-infection with other bacteria may be not a refractory factor in A. baumannii peritonitis. In addition, patient 1 experienced 2 peritonitis episodes during the study, but a sample was not cultured between the two episodes. In that patient, the peritoneal effluent again turned cloudy 20 days into the antibiotic course, and a culture from the removed catheter was positive for Pseudomonas aeruginosa.
Many factors promote peritonitis in PD patients: age (60 years and older), anemia (hemoglobin: <70 g/L), hypoalbuminemia (serum albumin: <30 g/L or, in some research, <35 g/L), hypokalemia (serum potassium: <3.5 mmol/L), diverticulosis, and diabetes, among others (13). In our study, 6 of 7 patients had anemia; the hemoglobin concentration in 1 patient was below 70 g/L. All patients had hypoalbuminemia, and 5 patients had albumin concentrations below 30 g/L. Of our 7 patients, 4 had hypokalemia, and 2 had diabetes. The age of the patients varied from 28 years to 64 years (only 1 patient was more than 60 years of age). Whether the patients had diverticulosis was unknown, because colonoscopies and barium enema examinations were not performed. In a few cases, we presumed that A. baumannii and other frequent bacterial infections were co-equal predisposing factors for peritonitis in PD patients, but hypoalbuminemia was probably more important.
Conclusions
A. baumannii appears to be rapidly developing resistance to multiple antimicrobials, resulting in serious infections and, when treatment is ineffective, high mortality. Our study found 1 specimen of A. baumannii with carbapenem resistance. Perhaps PDR A. baumannii will be the next threat to PD patients. To lower the peritonitis rate, predisposing factors such as malnutrition, anemia, and hypokalemia should be immediately and adequately corrected. Educating patients and caregivers on good hygiene and fluid exchange procedures will also be helpful.
Disclosures
No financial conflict of interest exists.
Acknowledgments
The authors are grateful to Mr. Hao Qian, Mrs. Yan Wang, and Mrs. Pei Zhang for their assistance.
References
- 1. Dijkshoorn L, Nemec A, Seifert H. An increasing threat in hospitals: multidrug-resistant Acinetobacter baumannii. Nat Rev Microbiol 2007; 5:939–51 [DOI] [PubMed] [Google Scholar]
- 2. Peleg AY, Seifert H, Paterson DL. Acinetobacter baumannii: emergence of a successful pathogen. Clin Microbiol Rev 2008; 21:538–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Friedman O, Jassal SV, Bargman JM. Acinetobacter peritoneal dialysis peritonitis: description and relation to the SPICE family of organisms. Perit Dial Int 2008; 28:195–7 [PubMed] [Google Scholar]
- 4. Lee YK, Kim JK, Oh SE, Lee J, Noh JW. Successful antibiotic lock therapy in patients with refractory peritonitis. Clin Nephrol 2009; 72:488–91 [DOI] [PubMed] [Google Scholar]
- 5. Solak Y, Atalay H, Polat I, Yeksan M. CAPD-related peritonitis after renal transplantation. Perit Dial Int 2010; 30:596–9 [DOI] [PubMed] [Google Scholar]
- 6. Li PK, Szeto CC, Piraino B, Bernardini J, Figueiredo AE, Gupta A, et al. on behalf of the International Society for Peritoneal Dialysis. Peritoneal dialysis-related infections recommendations: 2010 update. Perit Dial Int 2010; 30:393–423 [Erratum in: Perit Dial Int 2011; 31:512] [DOI] [PubMed] [Google Scholar]
- 7. Oliveira LG, Luengo J, Caramori JC, Montelli AC, Cunha Mde L, Barretti P. Peritonitis in recent years: clinical findings and predictors of treatment response of 170 episodes at a single Brazilian center. Int Urol Nephrol 2012; 44:1529–37 [DOI] [PubMed] [Google Scholar]
- 8. Ruiz A, Ramos B, Burgos D, Frutos MA, De Novales EL. Acinetobacter calcoaceticus peritonitis in continuous ambulatory peritoneal dialysis (CAPD) patients. Perit Dial Int 1988; 8:285–6 [Google Scholar]
- 9. Doughari HJ, Ndakidemi PA, Human IS, Benade S. The ecology, biology and pathogenesis of Acinetobacter spp.: an overview. Microbes Environ 2011; 26:101–12 [DOI] [PubMed] [Google Scholar]
- 10. Unal S, Garcia-Rodriguez JA. Activity of meropenem and comparators against Pseudomonas aeruginosa and Acinetobacter spp. isolated in the MYSTIC Program, 2002-2004. Diagn Microbiol Infect Dis 2005; 53:265–71 [DOI] [PubMed] [Google Scholar]
- 11. Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 2012; 18:268–81 [DOI] [PubMed] [Google Scholar]
- 12. Galvao C, Swartz R, Rocher L, Reynolds J, Starmann B, Wilson D. Acinetobacter peritonitis during chronic peritoneal dialysis. Am J Kidney Dis 1989; 14:101–4 [DOI] [PubMed] [Google Scholar]
- 13. Yip T, Tse KC, Lam MF, Cheng SW, Lui SL, Tang S, et al. Colonic diverticulosis as a risk factor for peritonitis in Chinese peritoneal dialysis patients. Perit Dial Int 2010; 30:187–91 [DOI] [PubMed] [Google Scholar]


