Abstract
Objective. IDH1 codon 132 mutation (mostly Arg132His) is frequently found in gliomas and is associated with longer survival. However, it is still unclear whether IDH1 mutation renders the cell more vulnerable to current treatment, radio- and chemotherapy. Materials and Methods. We transduced U87 with wild type IDH1 or IDH1R132H expressing lentivirus and analyzed the radiosensitivity (dose ranging 0 to 10 Gy) under normoxia (20% O2) and moderate hypoxia (1% O2). Results. We observed that IDH1R132H U87 cells grow faster in hypoxia and were more sensitive to radiotherapy (in terms of cell mortality and colony formation assay) compared to nontransduced U87 and IDH1 wt cells. This effect was not observed in normoxia. Conclusion. These data suggest that IDH1R132H mutation increases radiosensitivity in mild hypoxic conditions.
1. Introduction
The IDH1 gene encoding the cytoplasmic NADP+-dependent isocitrate dehydrogenase—and more rarely IDH2, encoding the mitochondrial isoform—are frequently mutated in gliomas, especially low grade gliomas and secondary glioblastomas [1]. IDH1/IDH2 mutation is associated with better clinical outcome, whatever the grade, but it is still not clear whether it is merely a prognostic marker or a predictor of the response to radiotherapy or chemotherapy [2–6]. Recent data IDH1/IDH2 mutation results in a new enzyme function catalyzing the NADPH-dependent reduction of alpha-ketoglutarate to D-2-hydroxyglutarate (D-2HG) [7]. IDH1/IDH2 mutations result in D-2HG accumulation and lowering NADPH levels. On one hand D-2HG inhibits various alpha-ketoglutarate dependant reactions, including histone and DNA demethylation, and is likely to promote—rather than inhibit—HIF1α degradation [8–11]. On the other hand, low NADPH levels might sensitize tumors to oxidative stress, potentiating response to radiotherapy, and may account for the prolonged survival of patients harboring the mutations.
Since the majority of gliomas are poorly responsive to current treatment regimens, the ability to enhance cell radio-chemosensitivity would be of clinical benefit. In this study, we characterized the impact of IDH1 mutation on U87 glioma cell growth and radiosensitivity.
2. Methods and Materials
2.1. Cell Culture and Hypoxia Treatment
The human glioblastoma cell line U87 MG (HTB14) was obtained from the American Type Culture Collection (ATCC, Rockville, MD) and maintained in Dulbecco's modified Eagle's medium (DMEM), supplemented with 10% fetal bovine serum (FBS) and 1% penicillin/streptomycin. Normoxic cells (21% O2) were grown in a humidified-air atmosphere incubator containing 95% air/5% CO2 at 37°C. Hypoxia experiments were performed in a controlled atmosphere chamber (INVIVO2 1000, Ruskinn, Awel, France) set at 1% O2, 94% N2, and 5% CO2 at 37°C.
2.2. Production of Recombinant Expression Lentiviruses
A recombinant pLenti7.3/V5-TOPO expression vector (Invitrogen's ViraPowerTM HiPerformTM Lentiviral Expression Systems; catalog number K5320-00) containing the human IDH1 wild type and IDH1 R132H cDNA was generated. The expression clones and the ViraPower Packaging Mix were cotransfected into the 293FT Cell line to produce lentiviral stocks, which were used to transduce the mammalian U87 cell line. U87-IDH1 wt and U87-IDH1 R132 stable cell lines were acquired using EmGFP selection by flow cytometry. The constructs was verified by DNA sequencing and RT-qPCR analysis.
2.3. Cell Proliferation Assay in Normoxia and in Hypoxia
To evaluate the impact of IDH1 mutation on cell growth in normoxia and in hypoxia by trypan blue dye exclusion method, U87, U87-IDH1 wt, and U87-IDH1 R132H cells (4000/well) plated in 24-well plates (6 plates in total) were incubated at 37°C for six hours in normoxia to adhere; then 3 plates were removed at 37°C in the controlled atmosphere chamber overnight. At 1, 3, and 7 days after exposure to normoxia and hypoxia, the cells were trypsinized, and the number of viable cells per well was determined by counting with trypan blue. The experiment was performed three times in triplicate each.
2.4. Comparative Cell Viability Assay after Irradiation, in Normoxia and in Hypoxia
To evaluate the effect of IDH1 R132H in the response to radiotherapy, U87 cells, IDH1 wt-U87, and IDH1 R132H-U87 cells were plated (4.103 per well) in 24-well plates. Six hours later at 37°C in normoxia, plates were either kept in normoxia or incubated in the controlled atmosphere chamber 1% O2 overnight. The next day, cells were irradiated with doses ranging from 0 to 10 Gy in order to determine the most discriminating dose. Cells were fixed in paraformaldehyde (PFA) 4%, then stained with Hoechst 33342 (10 μg/mL in PBS, Sigma-Aldrich, France) and photographed in a blinded fashion under fluorescence (4 wells per condition; 4 photographs per well) at 24 h, 48 h, and 120 h, respectively. Cells were counted with ImageJ software (Rasband, WS, ImageJ, US NIH).
2.5. Colony-Formation Assay in Normoxia and in Hypoxia
U87, IDH1 wt-U87, and IDH1 R132H-U87 cells were plated in 6-well containing 0.3% base agar layer. Six hours later, cells were either incubated in the hypoxic or normoxic chamber overnight. The next day, the cells were treated by radiotherapy at the Radiotherapy Department of the Centre de Lutte Contre le Cancer (CLCC) François Baclesse (Caen, France) using an X-ray generator with doses ranging 0–8 Gy (Therac 15-Saturne with a dose rate of 2 Gy/min) and then incubated again for colony formation. One month later, the colonies were fixed in 20% ethanol and stained with 0.05% crystal violet. Colonies that contained more than 50 cells were counted. Survival was calculated as the average number of colonies counted divided by the number of cells plated multiplicated by plating efficiency (PE), where PE is the fraction of colonies counted divided by cells plated without radiation. The clonogenic survival data were generated using JMP software. The experiment was performed five times in triplicate each.
2.6. Statistical Analysis
Results obtained in vitro were expressed as mean ± SEM Image analysis was performed with in-house macros under the ImageJ Software (Rasband, WS, ImageJ, US NIH). All statistical analyses were determined using post hoc tests after significant ANOVA. Values of P < 0.05 were considered statistically significant.
3. Results
3.1. Transduced Cells Express High Quantities of IDH1 wt and IDH1 R132H
The presence of IDH1 R132H transduced gene was confirmed by DNA sequencing. Real time PCR showed a high expression of gene IDH1 wt and IDH1 R132H in transduced U87 cells compared to nontransduced cells (Figure 1).
Figure 1.
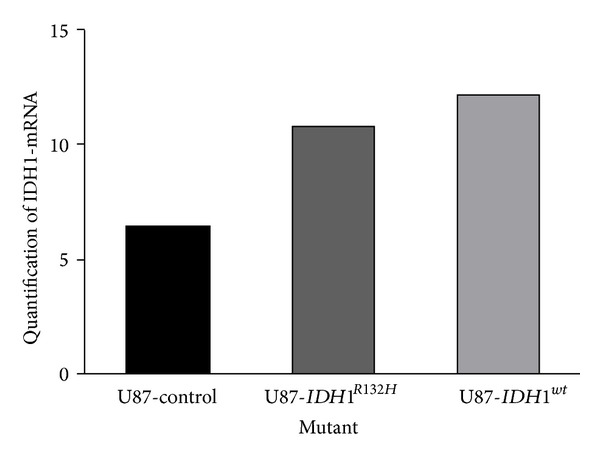
Real time PCR quantified the expression of the IDH1 wt and IDH1 R132H transduced genes.
3.2. IDH1 R132H Expressing U87 Glioma Cells Grow Faster in Hypoxia
We determined whether IDH1 R132H expression directly influences cell growth in normoxia and in hypoxia. The viable cell number per well was determined by counting with trypan blue at 1, 3, and 7 days after incubation in normoxia and in hypoxia. Proliferation rate of U87-IDH1 R132H cells was significantly higher in normoxia than in hypoxia for all the three cell lines. In normoxia, U87, U87-IDH1 wt, and U87-IDH1 R132H cells grew at the same rate, whereas U87-IDH1 R132H grew faster than U87 and U87-IDH1 wt in hypoxia (Figure 2).
Figure 2.
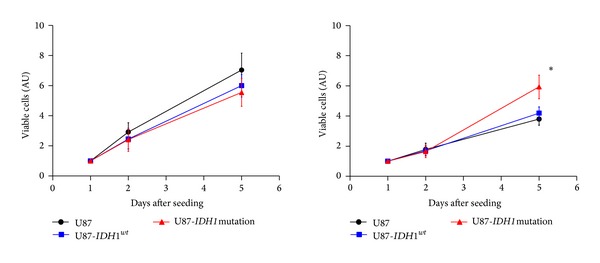
Effect of IDH1 R132H on U87 cell proliferation. U87, IDH1 wt-U87, and IDH1 R132H-U87 cells were incubated in normoxia 20% (left) or hypoxia 1% (right) and cells were counted after 1, 3, and 7 days.
3.3. Effect of Transduced IDH1 R132H on Cell Viability upon Exposure to Doses Ranging 0 to 10 Gy in Normoxia and in Hypoxia
To evaluate the role of IDH1 R132H in the response to radiotherapy, U87, U87-IDH1 wt, and U87-IDH1 R132H were exposed to different doses (range: 0–10 Gy): in normoxia the three cell lines showed the same radiosensitivity profile, whereas in hypoxia, the viability of U87-IDH1 R132H cells was significantly lower after 5 days compared to control cells and IDH1 wt cells (Figure 3) (13% versus 23% and 22% for a dose of 10 Gy, P < 0.001), respectively. This result suggests that IDH1 R132H makes the cells more radiosensitive in hypoxic, but not in normoxic conditions.
Figure 3.
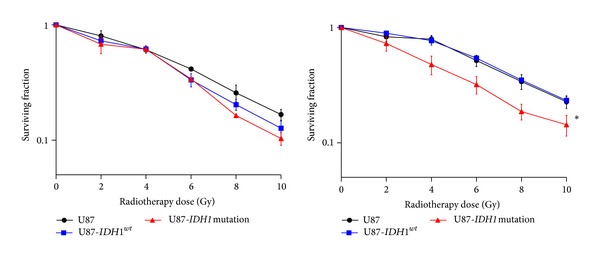
Effect of IDH1 R132H on U87 cell viability after irradiation. Transduced cells were plated and then irradiated with doses ranging from 0 to 10 Gy, in normoxia (20%) (left) and in hypoxia (1%) (right). Cells were counted 5 days later.
3.4. Effect of Transduced IDH1 R132H on Cell Mortality over Time following 8 Gy Irradiation in Normoxia and in Hypoxia
We quantified then cell death at 24 h, 48 h, and 120 h after 8 Gy irradiation. There was no substantial cell death after 24 h. The effect appeared at 48 h in both normoxia and in hypoxia (data not shown) and was maximal after 5 days. Cell death was significantly higher for IDH1 R132H transduced cells in hypoxia but not in normoxia (Figure 4).
Figure 4.
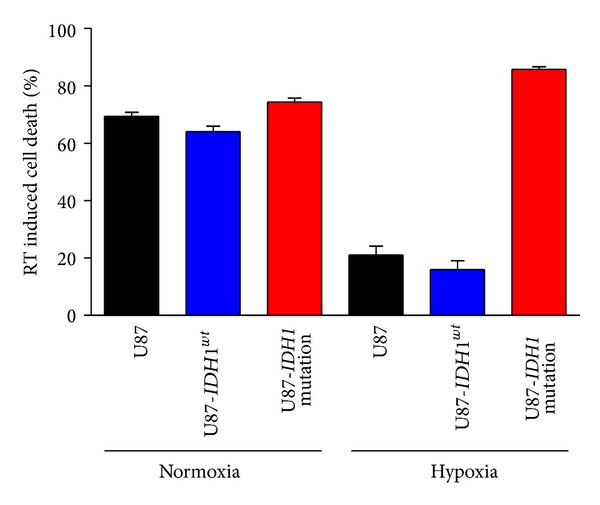
Cell viability after 8 Gy irradiation. Cells were counted before 8 Gy irradiation and 5 days after, in normoxia (20% O2) (left) and in hypoxia (1% O2) (right).
3.5. Radiosensitivity of U87-IDH1 R132H in Hypoxia Is Confirmed by Colony-Formation Assay
A colony-formation assay was used to confirm the effect of IDH1 R132H on the response to radiotherapy. Cells were treated with graded doses of radiation (0, 2, 4, 6, and 8 Gy). Colony-forming efficiency was determined 1 month later and surviving fractions were calculated. In normoxia, U87, U87-IDH1 wt, and U87-IDH1 R132H had the same colony-formation capacity after radiotherapy. In hypoxia, the colony number of U87-IDH1 R132H after radiotherapy was significantly lower than U87 and U87-IDH1 wt (Figure 5). Thus, U87-IDH1 R132H significantly sensitized U87 glioma cells to radiation.
Figure 5.
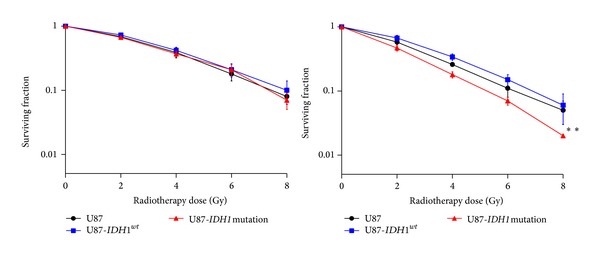
IDH1 R132H-U87 cells have a reduced colony forming cell ability after irradiation in hypoxia. U87, IDH1 wt-U87, and IDH1 R132H-U87 cells were plated 24 h before irradiation (0-2-4-6-8 Gy) in agar and incubated for one month in normoxia (20% O2) and in hypoxia (1% O2). The colonies were fixed in ethanol, stained with 0.05% crystal violet, and counted. Survival rate was estimated by the ratio between the colonies count and the number of cells plated, multiplicated by the plating efficiency.
4. Discussion
We observed here that IDH1 mutated U87 grew faster in moderate hypoxic conditions (1% O2) than in normoxia (21% O2). This contrast with data obtained in normoxia, IDH1 R132H overexpression in established glioma cell lines in vitro, resulted in a marked decrease in proliferation and mice injected with IDH1 R132H-U87 cells had prolonged survival compared to mice injected with IDH1 wt-U87 cells [12].
We found then that IDH1 R132H-U87 were more sensitive to radiotherapy in hypoxic condition. Indeed a high rate of cell proliferation is per se a sensitive factor of the radiation therapy response. But on the other hand, IDH1/IDH2 mutated cells may be more sensitive to oxidative stress. The role of isocitrate dehydrogenase in cellular defense against oxidative stress has been suggested [13]. Indeed, IDH1/IDH2 serves as a major source of cytosolic and mitochondrial NADPH production necessary to regenerate reduced glutathione (GSH) by glutathione reductase and for the activity of NADPH-dependent thioredoxin system, both are important in the protection of cells from oxidative damage [14, 15]. Thus, the decrease of NADPH in IDH1/IDH2 mutated cells might result in an increase of ROS that can damage DNA. Partially in line with our results, U87 cells transduced with IDH1 R132H or IDH2 R172K demonstrated increased sensitivity to radiation but the effect observed in normoxia and hypoxic conditions was not investigated [16].
Despite hypoxia being considered as a factor of radioresistance, we observed here a radiosensitizing effect of IDH1 R132H in glioblastoma cell line in hypoxic but not in normoxic condition. Until recently, IDH1/2 mutations were believed to result in the stabilization of HIF1α [10, 17]. Interestingly Koivunen et al. [11] showed that D-2HG (but not L-2HG) instead of being an inhibitor of EGLN (HIF prolyl 4-hydroxylases) activity acts as a partial agonist of EGLN and promotes the degradation of HIF1α. Because HIF protects cells from irradiation therapy under hypoxic condition, we may hypothesize that IDH mutation, by inducing an inappropriate degradation of HIF, could make the mutated cell more vulnerable to RT.
In conclusion, this study suggests a radiosensitizing effect of IDH1 R132H in glioblastoma cell lines U87 grown under mild hypoxic conditions, which are close to in vivo conditions. We need to confirm this finding on clinical setting: the 1p19q codeletion is a known marker of chemosensitivity. Whether the IDH1/2 mutation is a marker of radiosensitivity should be determined. The ongoing EORTC trial on low grade gliomas, which randomizes radiotherapy versus chemotherapy in low grade gliomas at progression and includes also a prospective observational cohort, will be pivotal to answer this question.
Acknowledgments
This work was supported by Grants from the Institut National du Cancer (INCA; PL 046), the Association pour la Recherche sur le Cancer, the Centre National de la Recherche Scientifique (CNRS), the University of Caen-Basse Normandie, the Conseil Régional de Basse-Normandie. The authors wish to thank the Radiotherapy Department of the CLCC François Baclesse (Caen, France), especially A. Batalla and P. Chevallier for giving them an access to the irradiator.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Parsons DW, Jones S, Zhang X, et al. An integrated genomic analysis of human glioblastoma multiforme. Science. 2008;321(5897):1807–1812. doi: 10.1126/science.1164382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sanson M, Marie Y, Paris S, et al. Isocitrate dehydrogenase 1 codon 132 mutation is an important prognostic biomarker in gliomas. Journal of Clinical Oncology. 2009;27(25):4150–4154. doi: 10.1200/JCO.2009.21.9832. [DOI] [PubMed] [Google Scholar]
- 3.Van Den Bent MJ, Dubbink HJ, Marie Y, et al. IDH1 and IDH2 mutations are prognostic but not predictive for outcome in anaplastic oligodendroglial tumors: a report of the European Organization for Research and Treatment of Cancer Brain Tumor Group. Clinical Cancer Research. 2010;16(5):1597–1604. doi: 10.1158/1078-0432.CCR-09-2902. [DOI] [PubMed] [Google Scholar]
- 4.Houillier C, Wang X, Kaloshi G, et al. IDH1 or IDH2 mutations predict longer survival and response to temozolomide in low-grade gliomas. Neurology. 2010;75(17):1560–1566. doi: 10.1212/WNL.0b013e3181f96282. [DOI] [PubMed] [Google Scholar]
- 5.van den Bent MJ, Brandes AA, Taphoorn MJB, et al. Adjuvant PCV chemotherapy in newly diagnosed anaplastic oligodendroglioma-long term follow-up of EORTC Brain Tumor Group study 26951. Journal of Clinical Oncology. 2013;31(3):344–350. doi: 10.1200/JCO.2012.43.2229. [DOI] [PubMed] [Google Scholar]
- 6.Cairncross JG, Wang M, Jenkins RB, et al. Benefit from procarbazine, lomustine, and vincristine in oligodendroglial tumors is associated with mutation of IDH. Journal of Clinical Oncology. 2014;32(8):783–790. doi: 10.1200/JCO.2013.49.3726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dang L, White DW, Gross S, et al. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature. 2009;462(7274):739–744. doi: 10.1038/nature08617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lu C, Ward PS, Kapoor GS, et al. IDH mutation impairs histone demethylation and results in a block to cell differentiation. Nature. 2012;483(7390):474–478. doi: 10.1038/nature10860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turcan S, Rohle D, Goenka A, et al. IDH1 mutation is sufficient to establish the glioma hypermethylator phenotype. Nature. 2012;483(7390):479–483. doi: 10.1038/nature10866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu W, Yang H, Liu Y, et al. Oncometabolite 2-hydroxyglutarate is a competitive inhibitor of α-ketoglutarate-dependent dioxygenases. Cancer Cell. 2011;19(1):17–30. doi: 10.1016/j.ccr.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koivunen P, Lee S, Duncan CG, et al. Transformation by the (R)-enantiomer of 2-hydroxyglutarate linked to EGLN activation. Nature. 2012;483(7390):484–488. doi: 10.1038/nature10898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bralten LBC, Kloosterhof NK, Balvers R, et al. IDH1 R132H decreases proliferation of glioma cell lines in vitro and in vivo. Annals of Neurology. 2011;69(3):455–463. doi: 10.1002/ana.22390. [DOI] [PubMed] [Google Scholar]
- 13.Jin HL, Sung YK, In SK, Park J-W. Regulation of ionizing radiation-induced apoptosis by mitochondrial NADP+-dependent isocitrate dehydrogenase. Journal of Biological Chemistry. 2007;282(18):13385–13394. doi: 10.1074/jbc.M700303200. [DOI] [PubMed] [Google Scholar]
- 14.Shi J, Zuo H, Ni L, et al. An IDH1 mutation inhibits growth of glioma cells via GSH depletion and ROS generation. doi: 10.1007/s10072-013-1607-2. Neurological Sciences. In press. [DOI] [PubMed] [Google Scholar]
- 15.Mohrenz IV, Antonietti P, Pusch S, et al. Isocitrate dehydrogenase 1 mutant R132H sensitizes glioma cells to BCNU-induced oxidative stress and cell death. Apoptosis. 2013;18:1416–1425. doi: 10.1007/s10495-013-0877-8. [DOI] [PubMed] [Google Scholar]
- 16.Li S, Chou AP, Chen W, et al. Overexpression of isocitrate dehydrogenase mutant proteins renders glioma cells more sensitive to radiation. Neuro-Oncology. 2013;15:57–68. doi: 10.1093/neuonc/nos261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhao S, Lin Y, Xu W, et al. Glioma-derived mutations in IDH1 dominantly inhibit IDH1 catalytic activity and induce HIF-1α . Science. 2009;324(5924):261–265. doi: 10.1126/science.1170944. [DOI] [PMC free article] [PubMed] [Google Scholar]


