Abstract
Irritable bowel syndrome (IBS) is a long-lasting, relapsing disorder characterized by abdominal pain/discomfort and altered bowel habits. Intestinal motility impairment and visceral hypersensitivity are the key factors among its multifactorial pathogenesis, both of which require effective treatment. Voltage-gated calcium channels mediate smooth muscle contraction and endocrine secretion and play important roles in neuronal transmission. Antispasmodics are a group of drugs that have been used in the treatment of IBS for decades. Alverine citrate, a spasmolytic, decreases the sensitivity of smooth muscle contractile proteins to calcium, and it is a selective 5-HT1A receptor antagonist. Alverine, in combination with simethicone, has been demonstrated to effectively reduce abdominal pain and discomfort in a large placebo-controlled trial. Mebeverine is a musculotropic agent that potently blocks intestinal peristalsis. Non-placebo-controlled trials have shown positive effects of mebeverine in IBS regarding symptom control; nevertheless, in recent placebo-controlled studies, mebeverine did not exhibit superiority over placebo. Otilonium bromide is poorly absorbed from the GI tract, where it acts locally as an L-type calcium channel blocker, an antimuscarinic and a tachykinin NK2 receptor antagonist. Otilonium has effectively reduced pain and improved defecation alterations in placebo-controlled trials in IBS patients. Pinaverium bromide is also an L-type calcium channel blocker that acts locally in the GI tract. Pinaverium improves motility disorders and consequently reduces stool problems in IBS patients. Phloroglucinol and trimethylphloroglucinol are non-specific antispasmodics that reduced pain in IBS patients in a placebo-controlled trial. Antispasmodics have excellent safety profiles. T-type calcium channel blockers can abolish visceral hypersensitivity in animal models, which makes them potential candidates for the development of novel therapeutic agents in the treatment of IBS.
Keywords: Irritable bowel syndrome, Motility, Treatment, Calcium channel blockers, Spasmolytics
Core tip: Treatment of irritable bowel syndrome (IBS) must target intestinal motility alterations and visceral hypersensitivity. Antispasmodics have been used in the treatment of IBS for decades, and large placebo-controlled trials have recently been conducted on their efficacy. Alverine citrate, in combination with simethicone, effectively reduced abdominal pain and discomfort; while otilonium bromide also improved defecation problems. Pinaverium bromide regulated impaired motility and reduced stool complaints. Phloroglucinol and trimethylphloroglucinol reduced pain in IBS patients. Mebeverine was recently found to be effective only in non-placebo-controlled trials. Antispasmodics are considered safe. T-type calcium channel blockers could represent a future therapeutic option in IBS treatment.
INTRODUCTION
Irritable bowel syndrome (IBS) is a chronic gastrointestinal (GI) disorder affecting a significant proportion of the global population, with a calculated prevalence of approximately 11.2%[1]. IBS has a large impact on health-related quality of life, resulting in reduced work productivity, elevated absenteeism and increased health care use and costs[2,3]. IBS can also seriously impair the patient-doctor relationship[4], because ineffective symptom control can diminish clinicians’ credibility and prompt the patient to seek further opinions[5]. IBS has a long course and high relapse rates, with more than half of IBS patients reporting the same symptom profile after 1 and 7 years and a further 25% having persistent minor IBS symptoms[6]. Regarding the long term persistence of IBS, effective long-term therapies are of great economic importance in both Eastern and Western countries; however, drug trials have revealed an extremely high relapse rate in this disease[7]. Despite intensive research aiming to find new therapeutic pathways, the present possibilities have mostly focused on symptom suppression, and only a few drugs have been found to be more effective than placebo over the long term.
A heterogeneous group of drugs called “antispasmodics” or “spasmolytics” such as direct smooth muscle relaxants (e.g., papaverine, mebeverine, peppermint oil), anticholinergic agents (e.g., butylscopolamine, hyoscine, cimetropium bromide, pirenzepine) and calcium channel blockers (e.g., alverine citrate, otilonium bromide, pinaverium bromide), have been used in therapy for IBS for decades. The aim of these drugs is to reduce defecation symptoms by increasing colonic transit time, improving stool consistency and reducing stool frequency. The pharmacological action of these agents is not always clear, and the mechanisms are often mixed. Nevertheless, meta-analyses performed on studies comparing antispasmodics to placebo or other treatments have uniformly confirmed the positive effects of these drugs, and their side effect profiles have been excellent[8]. Recent adverse reactions, such as severe constipation, ischemic colitis and possible deaths[9], have led to the transient withdrawal of alosetron, a 5-HT3 receptor antagonist, and fatal ventricular arrhythmias caused the retraction of the mixed 5-HT3 antagonist/5-HT4 agonist cisapride in many countries, thus highlighting antispasmodics as attractive and reliable therapeutic options.
The accurate diagnosis of IBS has been a major pitfall in designing clinical trials in the past because a precise definition has been lacking. After the proposal of previous diagnostic criteria by Manning et al[10] and later by Drossmann et al[11], the Rome criteria were developed, emphasizing the importance of a positive diagnosis based on symptoms. Currently, the diagnostic criteria for IBS based on the Rome III system are recurrent abdominal pain or discomfort for at least 3 d per month over the previous 3 mo, associated with two or more of the following: improvement with defecation; and onset associated with a change in frequency of stool; and onset associated with a change in form (appearance) of stool[12]. These criteria must be fulfilled for the previous 3 mo, with symptom onset at least 6 mo prior to diagnosis. Depending on the predominant bowel symptom, IBS can be classified as IBS with constipation (IBS-C, 20%-30% of patients), IBS with diarrhea (IBS-D, 20%-30% of patients) or IBS with “mixed” constipation and diarrhea (IBS-M, up to 45% of patients)[13].
In this review, we aimed to collect and summarize the available data on the efficacy and safety of modern antispasmodics in the treatment of IBS, focusing on placebo-controlled clinical trials using valid patient selection criteria.
PATHOPHYSIOLOGY OF IBS
Profound research over the last few decades has revealed a multifactorial pathogenesis. Preceding enteric infections, altered colonic or small intestinal bacterial flora, increased gut permeability and immune activation may play a role in the development of the disease[14-16]. Signals from the GI tract are processed in the brain, which in turn can influence GI motility, secretion and immune function[17]. This brain-gut axis is essential for the healthy regulation of the GI system, and its structural or functional alteration can lead to the development of disorders such as IBS[18]. Therefore, psychological factors and chronic stress can also be involved in triggering symptoms[19], in association with alterations in the activity of specific brain regions[20,21]. Nevertheless, abnormal intestinal motility and visceral hypersensitivity remain key factors in the pathogenesis of the disease[22]. The origin of visceral hypersensitivity seems to be complex. Intraluminal factors, such as serine-proteases, can increase colonic permeability in IBS-D patients by activating protease-activated receptor-2, resulting in visceral hypersensitivity[23]. Increased colonic permeability in IBS-D patients has been correlated with stool frequency, which also suggests a role in symptom generation[24]. Luminal cysteine-proteases have been shown to increase colonic permeability through the degradation of tight junction proteins, resulting in visceral hypersensitivity in IBS-C patients, possibly through local microinflammation[25]. Colonic mucosal immune activation, which is characterized by mast cell, intraepithelial lymphocyte and lamina propria lymphocyte counts, was found to be significantly higher in IBS-D than in healthy controls[26]. This immune activation was similar to inactive inflammatory bowel disease. Mast cells have been implicated in the development of IBS: the number of degranulating mast cells in colonic mucosa and their spontaneous release of trypsin and histamine were markedly increased in IBS patients compared with controls[27]. Furthermore, mast cells in close proximity to nerve endings have been significantly correlated with the severity and frequency of abdominal pain/discomfort in IBS patients. Enterochromaffin cells can also play important roles in the development of visceral hypersensitivity by producing and releasing serotonin, which activates 5-HT3 receptors located on afferent sensory neurons[28]. Furthermore, the activation of 5-HT4 receptors on sensory afferent neurons triggers the peristaltic reflex, whereas 5-HT4 receptors on colonic smooth muscle mediate relaxation[29,30]. Motility disturbances in IBS patients have been well known for decades. Baseline muscular tone was found to be higher in IBS-D and IBS-M but not in IBS-C compared with healthy individuals[31]. Further abnormalities in colonic motility patterns are characterized by hyperreactivity - namely, a prolonged increase in colonic motor activity after meals, an exaggerated increase in motor activity in response to stressors or cholecystokinin (CCK) and increased motor activity in response to balloon distention[32]. Stress alone can be an important factor in the pathogenesis of motility disturbances, as suggested by long-duration restraint in rats having been shown to induce rapid, dramatic changes in small bowel motility, with gradually increasing differences in colonic motility as measured by electromyography[33]. Colonic motility changes were still present 60 h after such restraint stress, suggesting that these persistent alterations could form the basis of the development of functional disorders. In a study measuring electromyographic activity in the left colon with an intraluminal probe, a large increase in short-spike bursts was induced by stress (via the cold pressor test) in IBS-C patients but not in controls or in chronically constipated patients, and this difference remained significant for 2 h after the stress episode (Figure 1)[34]. Ingestion of a standard meal has provoked the increase of aboral migrating long spike bursts in control subjects, but this propulsive motor effect was largely depressed in IBS-C patients[35]. In a subsequent study, repetitive distention of the distal sigmoid colon below the sensory threshold in IBS patients induced exaggerated colonic motility[36]. Small bowel motility was also impaired, as the repetitive distention inhibited motility of the small intestine in healthy subjects, whereas no such effect was observed in IBS patients[36]. Specific patterns of small bowel motor activity have also been described in IBS patients, such as ileal propulsive waves and clusters of jejunal pressure activity, which have usually been associated with abdominal cramping and pain[37]. Visceral hypersensitivity by itself is not painful, but it can lead to abdominal pain in IBS patients by the effect of an intense stimulus, such as an exaggerated colonic contraction[38]. However, a clear connection between visceral hypersensitivity and motility disturbances could not been established, and these two factors have usually been considered independent, both requiring effective treatment[31].
Figure 1.
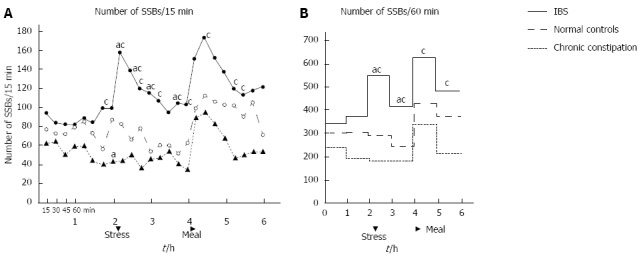
The number of short spike bursts measured by colonic intraluminal electromyography[34]. The values were calculated over the period of 15 (A) and 60 min (B). Each group included 8 patients. The 6-h screening session consisted of three 2-h periods: a control period; a period of stress (during which a cold pressor test was performed for 15 min); and a post-prandial period (patients ingested a 800 kcal meal). SSBs: Short spike bursts. aP < 0.05 vs normal controls; cP < 0.05 vs chronic constipation patients.
VOLTAGE-GATED CALCIUM CHANNELS
Voltage-gated calcium channels are ion channels mediating calcium influx in response to membrane depolarization, and they regulate intracellular processes, such as contraction, secretion, neurotransmission and gene expression, in a variety of cells[39]. Calcium-channels are traditionally classified by their current properties and pharmacology[40]. The L (long-lasting)-type calcium channel is a large-conductance channel that produces long-lasting current at strong depolarizations, and it is generally inhibited by dihydropyridine (DHP) derivatives[41]. L-type currents are most important for muscle and endocrine cells, in which they mediate contraction and secretion[39]. In neurons and cardiac pacemaker cells, L-type currents can also be found to activate at lower voltages. N (neuronal)-type currents are also long-lasting, but they require strongly negative potentials for the complete removal of inactivation and strong depolarizations for activation, and they are not blocked by DHP[41]. In Purkinje cells, three further channels have been identified. P-type currents are blocked by low concentrations of ω-agatoxin, whereas the Q-type is only responsive to high concentrations. Residual currents, which were resistant to all known calcium-blockers at the time of their discovery, were called R (resistant)-type. The last group of voltage-gated calcium channels, the T (transient)-type, is characterized by a small and transient conductance activated upon weak depolarizations[41]. These currents are responsible for modulation of the action potential and for the performance of pacemaker activities.
The medical use of calcium antagonists started in the 1980s with DHP-type antagonists, which block L-type channels, in the treatment of hypertension by exploiting their properties as vasodilators[40]. Because a Ca2+ increase in smooth muscle is required for contraction, calcium antagonists induce relaxation of blood vessels, followed by a consequent reduction in blood pressure. Further, relaxation of the coronary arteries increases coronary flow, acting against angina pectoris. Calcium antagonists have no effect on skeletal muscles; however, they slightly influence cardiac muscle by decreasing pacemaker activity and conduction. Based on the well-known gastrointestinal motility impairments in IBS, calcium antagonists used for cardiovascular conditions appeared to be potential options for relieving symptoms by relaxing the colonic smooth muscles. Therefore, in the late 1980s, nicardipine was proposed for the treatment of irritable bowel syndrome, based on its spasmolytic properties[42]. Nonetheless, cardiovascular side effects have seriously limited the application of such calcium antagonists, thereby inspiring researchers to identify substances that act selectively on the gastrointestinal tract.
MODERN ANTISPASMODICS WITHOUT CARDIOVASCULAR SIDE EFFECTS
Alverine citrate
Experimental studies: Alverine citrate is an antispasmodic drug that inhibits calcium uptake and modulates smooth muscle activity. An experimental study on anesthetized cats showed that alverine acts on vagal sensory endings of the GI tract, where it decreases the responses of mechanoreceptors to mechanical and chemical stimuli[43]. Because chemically induced responses and smooth muscle contraction are both calcium dependent, decreased chemical sensitivity and smooth muscle relaxation can be explained by reduced calcium influx. In addition, a calcium-independent mechanism of action, such as selective 5-HT1A receptor antagonism, might also be present, which has been demonstrated in rats using a 5-HT agonist-induced hypersensitivity model[44]. However, the picture is more complex than first thought - in guinea pig urinary bladder preparations, the frequency of spontaneous contractions in endogenously active smooth muscle was surprisingly increased by low doses of alverine citrate, whereas contraction amplitude was decreased. Higher doses of the drug could suppress both the frequency and amplitude of contractions; nevertheless, the authors speculated that the doses used in clinical practice would not reach this concentration in humans. They concluded that alverine citrate should be considered a true spasmolytic, because it suppresses the duration of spontaneous contractions of the gut, preventing local ischemia and reflectoric pain in the colonic wall evoked by “spasms”. In addition, it has also been noted that alverine can increase calcium influx during action potentials by inhibiting the inactivation of calcium channels, but it reduces the sensitivity of contractile proteins to calcium, consequently suppressing the evoked muscular activity. Stress-induced colonic motility changes are an important factor in the pathogenesis of IBS; therefore, the clinical effects of alverine and the antifoaming agent, simethicone were tested in a rat model of colonic hypersensitivity induced by acute restraint stress[45]. Treatment with simethicone (200 mg/kg po) or alverine citrate (10 mg/kg po) reduced stress-induced increases in colonic permeability and hypersensitivity to distension, but lower doses were ineffective[45]. However, the combination of inactive doses of simethicone (100 mg/kg) with low doses of alverine (7 mg/kg) completely abolished the effects of stress, suggesting a synergistic action.
Clinical trials: Clinical studies on alverine citrate in IBS have been scarce (Table 1). In a randomized, placebo-controlled, double-blind clinical trial conducted in three British centers, after a 2-wk screening period, IBS patients selected according to the modified Rome criteria received 12 wk of treatment with 120 mg alverine citrate three times daily[46]. The patients completed diary cards about abdominal pain or discomfort, bloating, bowel movements, stool consistency, and general well-being; furthermore, the severity and frequency of abdominal pain, bloating, nausea and early satiety were assessed at study visits four times during treatment. Although abdominal pain, bloating and general well-being were all slightly more improved in the alverine-treated group than in the placebo group, when comparing the first diary card to the third, the difference was not statistically significant. This finding might be explained by the placebo effect being exceptionally high, sometimes reaching almost 70%, which would require a study with a much great number of participants to detect a possible positive effect of alverine. Regarding safety, no serious adverse events were reported in the study, and more patients experienced adverse events in the placebo group (48.1%) than in the alverine-treated group (39.6%). Using the well-known spasmolytic properties of alverine, a randomized, placebo-controlled trial showed that pretreatment of patients over 5 d with 60 mg alverine citrate plus 300 mg simethicone three times daily reduced intubation time during colonoscopy by 19%; nonetheless, it did not affect scores for pain, spasm, difficulty or cleanliness[47]. The combination of alverine with simethicone was also tested in a double-blind, placebo-controlled, randomized trial conducted in 17 sites in Hungary and Poland[48]. A total of 412 IBS patients meeting the Rome III criteria received a combination of 60 mg alverine citrate and 300 mg simethicone or placebo three times per day for 4 wk. Combined alverine citrate and simethicone treatment achieved a higher reduction in abdominal pain and discomfort, as measured using visual analog scale (VAS) scores, and significantly more patients responded to therapy than to placebo, regardless of stool pattern. A visible, but not statistically significant, trend was also observed, showing greater improvement in IBS life impact scores with combination therapy than with placebo. No severe drug-related adverse events were noted in the study, and the numbers of adverse events were similar in both groups.
Table 1.
Characteristics and primary outcomes of randomized, double-blind, placebo controlled clinical trials in irritable bowel syndrome patients
| Ref. | IBS population | Selection criteria | Treatment | Dose | Duration | Outcome |
| Mitchell et al[46] | All subtypes | Modified Rome | Alverine citrate vs placebo | 120 mg tid | 12 wk | No significant difference compared to placebo |
| Wittmann et al[48] | All subtypes | Rome III | Alverine citrate + | 60 mg tid + | 4 wk | Significantly reduced abdominal pain and discomfort compared to placebo |
| simethicone vs placebo | 300 mg tid | More therapy responders, regardless of stool pattern, compared to placebo | ||||
| Connel et al[52] | All subtypes | Mebeverine vs placebo | 100 mg qid | 12 wk | Superior in controlling IBS symptoms compared to placebo | |
| Kruis et al[58] | All subtypes | Mebeverine vs placebo vs Wheat bran | 400 mg daily | 16 wk | No significant difference compared to placebo | |
| Enck et al[59] | All subtypes | Mebeverine vs placebo vs Dietary fiber | 16 wk | Therapy response rate lower than placebo | ||
| Everitt et al[61] | All subtypes | Rome III | Mebeverine vs | 135 mg tid | 6 wk | No significant difference between drugs |
| methylcellulose vs placebo with/without cognitive behavioral therapy web site (assisted or not) | 3 tbl. bid | Significantly increased enablement at 6 and 12 wk in website group compared to no website group, significantly more participants scored their subjective assessment of global relief as improved at 12 wk in website group compared to no website group. | ||||
| Baldi et al[69] | Abdominal pain predominant | Otilonium bromide vs placebo | 40 mg tid | No significant difference in abdominal pain, bloating and general well-being compared to placebo, but significantly reduced sigmoid motility | ||
| Battaglia et al[70] | All subtypes | Drossman | Otilonium bromide vs placebo | 40 mg tid | 15 wk | Significantly better compared to placebo in reduction of abdominal pain frequency, global score improvement of abdominal pain and discomfort, therapy responder rate, reduced tenderness of the sigmoid colon, higher general well-being and global judgement of investigators; superior in improving severity of diarrhea/constipation, number of evacuations and mucus in stool; more effective in treating diarrhea, but not constipation |
| Clave et al[72] | All subtypes | Rome II | Otilonium bromide vs placebo | 40 mg tid | 15 wk | Reduced abdominal pain frequency and bloating and improved stool frequency and patient global assessment compared to placebo; lower symptom recurrence after treatment |
| Awad et al[85] | All subtypes | Pinaverium bromide vs placebo | 50 mg tid | Significantly reduced post-prandial rectal spike amplitude plus frequency and spontaneous recto-anal inhibitory reflex frequency compared to placebo | ||
| Chassany et al[98] | All subtypes | Rome II | Phloroglucinol + trimethylphloroglucinol vs placebo | 62.2 mg + 80 mg tid | 1 wk | Significantly higher relative decrease of pain intensity and responder rate in the phloroglucinol plus trimethylphloroglucinol group compared to placebo; persisting treatment effect in a higher percent of patients treated with phloroglucinol plus trimethylphloroglucinol |
| Cha et al[99] | IBS-D | Rome III | Phloroglucinol vs placebo | 80 mg tid | 2 wk | Significantly improved subjects' global assessment and decreased stool frequency |
Characteristics and primary outcomes of randomized, double-blind, placebo controlled clinical trials in irritable bowel syndrome (IBS) patients with alverine citrate, mebeverine, otilonium bromide, pinaverium bromide and phloroglucinol. IBS-D: IBS with diarrhea.
Mebeverine
Experimental studies: Mebeverine is a beta-phenyletylamine derivative of reserpine, which has relatively specific effects on smooth muscle cells without atropine-like side effects in humans[49]. It directly blocks voltage-operated sodium channels and inhibits intracellular calcium accumulation[49,50]. It is three times more potent than papaverine in inhibiting the peristaltic reflex of the guinea-pig ileum[51], but further animal studies on its pharmacological effect have been lacking.
Clinical trials: Mebeverine became treatment of interest for IBS in the 1960s. In an early study by Connell[52], iv mebeverine decreased all sigmoid colonic motility, especially in hyperactive subjects, and it had less or no effect in hypoactive subjects. In a subsequent part of the study, mebeverine was superior to placebo at each time point over 12 wk of treatment in IBS patients in terms of symptom improvement and general well-being. Using prolonged ambulant manometry in 12 IBS patients and 6 healthy controls, compared to a placebo period, mebeverine had no significant effects on interdigestive small bowel motor parameters in controls; in contrast, a higher phase 2 motility index was observed in both IBS-D and IBS-C patients, and phase 3 motility was also affected[53]. These alterations in small bowel motile activity by mebeverine suggest possible spasmolytic and prokinetic effects in IBS patients.
Regarding symptom control in IBS, non-placebo-controlled studies have shown positive results. Significant improvement was observed after 6 wk of treatment with both the plain and sustained-release forms of mebeverine, with a minimal number of adverse events[54]. When comparing pinaverium bromide to mebeverine in 91 IBS-D patients, the improvements in global well-being were similar in the two groups, the daily defecation frequencies were markedly decreased, and stool consistencies became well formed in both groups, while no significant side effects were observed[55]. In a clinical trial comparing the effects of ramosteron, a 5-HT3 receptor antagonist, to those of mebeverine in patients with IBS-D, both treatments were equally effective in reducing abdominal pain/discomfort and urgency and improving the stool form score and stool frequency compared to baselines[56].
However, when the effects of mebeverine have been compared to placebo and not compared to another drug or measured by self-control, the results have been controversial. A recent systematic review, including eight randomized trials, revealed that clinical improvement and relief of abdominal pain by mebeverine treatment were not statistically significant compared to placebo[57-59]. No differences were found in the effectiveness of 200 and 135 mg mebeverine doses. Tolerability was excellent, without significant adverse effects. Similarly, no positive effects of mebeverine over placebo were seen in an exploratory study performed in 135 IBS patients fulfilling the Rome III criteria who were recruited from general practice, when mebeverine, methylcellulose and placebo were compared, with or without the combination of a cognitive behavioral therapy-based self-management web site (with or without additional telephone and e-mail support)[60,61]. Disappointingly, the use of the web site also did not improve IBS symptom severity scores or quality of life scores significantly over the “no web site” group; nevertheless, there was a visible trend toward continued improvement in the self-management group (particularly those with telephone support) throughout the study, while the “no web site” group and the medication groups seemed to lose their therapeutic gains from weeks 6 to 12. However, in a study performed in London, personal sessions of cognitive behavioral therapy were beneficial in addition to mebeverine, and the effects persisted for up to six months after therapy, both in terms of symptom relief and improvement in social and work disability[62]. Depression and anxiety predict poor outcomes in mebeverine-treated IBS patients, and in cases of patients with unhelpful coping behaviors (e.g., avoidance), the combination of mebeverine with cognitive-behavioral therapy could be useful[63].
Otilonium bromide
Experimental studies: Otilonium bromide is weakly absorbable from the GI tract due to its quaternal ammonium structure; thus, it is almost completely excreted in the feces[64]. In experimental studies, it accumulated in the walls of the GI tract after oral administration, with minimal systemic absorption[65]. Its effects are rather complex, consisting mainly of L-type calcium-channel blockade, but binding to muscarinic M1, M2, M4 and M5 receptors has also been observed[66]. Antagonism of M3-coupled calcium signals in human colonic crypt cells suggested an anti-secretory action in IBS-D patients[67]. Additionally, by antagonism of tachykinin NK-2 receptors, otilonium not only causes spasmolysis but also reduces peripheral sensory afferent transmission to the central nervous system[64]. These effects suggest that otilonium could be effective in reducing both of the main symptoms of IBS: spasms and abdominal pain.
Clinical trials: In a small study of 15 IBS patients, one week of treatment with otilonium bromide significantly increased the pain threshold of IBS patients to anorectal distension, while thresholds for first sensation and stool remained unchanged[68]. In a multicenter, double-blind, placebo-controlled trial with 72 IBS patients in Italy, treatment with 40 mg otilonium bromide three times daily significantly decreased abdominal pain and bloating, improved well-being and global assessment, while it markedly increased the pain threshold during sigmoid distension. Nevertheless, these results did not differ from those of the placebo group[69]. However, otilonium significantly reduced sigmoid motility during distension, whereas placebo did not, suggesting the need for larger studies, a different setup or more accurate patient selection. Seven years later, the results of a larger trial were published in Italy, including 375 IBS patients selected by the Drossman criteria, when a 2-wk placebo run-in period was included to exclude patients with low compliance or with quickly resolving symptoms[70]. After randomization, the patients received 40 mg otilonium bromide or placebo three times daily for 15 wk, and their symptoms were assessed at weeks 5, 10 and 15. Abdominal pain frequency was reduced in both of the groups, with a statistically significant difference in favor of otilonium after 10 and 15 wk of treatment. The global score improvements in abdominal pain and discomfort were significantly greater in the otilonium group throughout the whole study. Therapy was successful in significantly more patients treated with otilonium than in those treated with placebo. Defecation disturbances improved similarly in both groups. Tenderness of the sigmoid colon, general well-being and global judgements by the investigators all differentially improved in the otilonium-treated group. Extended analysis of the data from this study with different analysis forms 3 years later revealed that otilonium had therapeutic gains over placebo not only in terms of pain intensity, pain frequency and meteorism but also regarding the severity of diarrhea/constipation, the number of evacuations and the presence of mucus in stool[71]. When sorting patients according to stool habits, otilonium was more effective than placebo in treating diarrhea but was only as effective as placebo in managing constipation.
Otilonium bromide in irritable bowel syndrome (OBIS) was a recent international clinical trial in which patients diagnosed according to the Rome II criteria received 40 mg otilonium bromide three times a day or placebo over 15 wk after randomization[72,73]. Otilonium bromide effectively reduced abdominal pain frequency and bloating, while improving stool frequency and patients’ global assessments, compared to placebo. The prominent outcome of this study was the efficacy of otilonium in dramatically reducing abdominal pain frequency from more than half of the days to less than one day per week, compared to the persistent 1-3 episodes in the placebo group. Otilonium had no significant effects on pain severity, stool consistency or mucus in the stool. During the 10-wk follow-up period after finishing treatment, the likelihood of symptom recurrence was significantly higher in the placebo group than in the otilonium group. This finding might be explained by the elongated persistence of otilonium in the colonic wall due to its lipophilic properties. No serious adverse events occurred in the study, and only three adverse events, consisting of dry mouth or nausea, were judged by the investigator to be related to otilonium’s side effects.
When compared to other spasmolytics in a meta-analysis, otilonium bromide performed outstandingly among 12 different antispasmodics in terms of IBS symptom control[74]. In a double-blind, randomized, active-controlled trial conducted in China of IBS patients selected according to the Rome II criteria, the results confirmed the similar, but not superior, efficacy of otilonium to that of mebeverine in the management of the frequency and intensity of abdominal pain, and abdominal bloating, flatulence and satisfactory stool frequency were all improved similarly by both therapies[75]. The most common side effects of dry mouth and nausea/dizziness - recorded in previous studies as well-might have been caused by peripheral and central muscarinic antagonism, respectively, and could be explained by the known ability of otilonium to bind to muscarinic receptors[66].
Pinaverium bromide
Experimental studies: Pinaverium bromide is also a quaternary ammonium derivate that is poorly absorbed, with pronounced pharmacological effects in the gastrointestinal tract instead of the cardiovascular system[76]. It has a low absorption rate from the GI tract, corroborated by hepato-biliary excretion[64]. It has been shown that its effects are very similar to those of the established L-type calcium-channel blockers (nitrendipine, diltiazem, D600); that is, it reduces the plateau phase of slow waves, thereby inhibiting calcium influx and preventing consequent contractions[77]. Pinaverium has been shown to inhibit the contractile response in dog and rat colonic smooth muscle preparations to acetylcholine, the neurotransmitter of cholinergic intrinsic nerves[77,78]. Similarly, in colonic smooth muscle cells isolated from normal or inflamed human colons, pinaverium bromide inhibits contraction induced by different agonists (CCK 8, carbachol or KCl)[79]. In inflamed colonic cells, pinaverium exerts more pronounced inhibition than the non-GI-selective L-type calcium channel blockers nicardipine and diltiazem. This effect of pinaverium on colonic smooth muscle cells is mediated mainly by the inhibition of calcium influx through L-type calcium channels, thereby inhibiting contractions induced by acetylcholine or KCl in rat preparations[80]. Stress plays an important role in the pathogenesis of IBS; therefore, colonic smooth muscle preparations from cold restraint-stressed rats have also been examined, revealing that the hypermotility observed after stress is mostly related to increased calcium influx into the cells[80]. This observation supports the use of pinaverium in IBS, in which pathological colonic hypermotility must be suppressed. Furthermore, in rats chronically fitted with intraparietal electrodes in the proximal colon, pinaverium bromide has been found to have no effect on colonic long spike bursts in the fasting state, but it inhibits increases in colonic spike burst frequency induced by a meal or by CCK-8[81]. However, it loses its effects in capsaicin-pretreated animals, showing the participation of sensory afferent neurons in the mechanism of action, which might also explain the efficacy of pinaverium bromide in treating the two main features of IBS: motility disorders and gut hypersensitivity.
Clinical trials: Pinaverium bromide has been used for managing functional bowel disorders for decades, with double-blind studies performed as early as 1977[82]. Its effects on colonic smooth muscle have been well established by animal experiments; however, intensive research has only started to characterize its mechanism of modifying GI motility in humans. In an early pilot study performed in 12 IBS patients, colonic motility was detected by surface electromyography over a 2-h fasting period and a 2-h postprandial period following a standard meal, before and after 10 d of treatment with 50 mg pinaverium bromide three times daily[83]. The leading symptoms, such as abdominal pain, bloating and altered bowel habits, started to ameliorate on day 4 of treatment. Abnormal colonic motility patterns (viz., increased frequency and amplitude of contraction, arrhythmia in motoric activity), which were particularly pronounced post-prandially, diminished after 10 d of treatment. In a continuation of this pilot study, the authors studied 22 IBS patients and 7 healthy controls[84]. The healthy controls received no treatment but served as controls for electromyographic measurements. The study protocol was as previously described, except for the length of pinaverium bromide therapy, which was extended to 14 d. The results showed increased fasting and postprandial colonic motility parameters in IBS patients compared to controls, which was effectively reduced by 14 d of pinaverium bromide therapy. Abdominal pain and bloating were also significantly improved by treatment. Stool frequency was normalized by pinaverium bromide therapy in both diarrheic and constipated IBS patients. The effects of pinaverium bromide on intestinal motility were affirmed by a further randomized, double-blind, placebo-controlled trial on IBS patients[85]. Pinaverium bromide was administered in a 50 mg dose (po, tid), and myoelectrical and mechanical activities of the rectum and the internal anal sphincter were recorded before treatment, in the fasting state and at 2 h post-prandially. Post-prandial rectal spike amplitude and frequency, as well as the frequency of the spontaneous recto-anal inhibitory reflex, were significantly decreased after treatment with pinaverium bromide. Pinaverium bromide was also able to change colonic transit and colonic responses to food in IBS patients, as demonstrated by a technique using orally ingested radiopaque markers visible on plain abdominal X-rays[86]. Beneficial effects of pinaverium bromide treatment were also demonstrated by an open trial, in which 61 treated IBS patients experienced significantly reduced abdominal pain, improved stool consistency, reduced defecation straining and urgency, and decreased mucus in stool, with good drug tolerance and few side effects[87]. The clinical efficacy of pinaverium bromide was also evaluated using a statistical technique new to the field-namely, by employing polar vectors on data from a phase IV clinical trial with 1677 Rome III IBS patients receiving pinaverium bromide combined with simethicone[88]. The results showed amelioration of stool frequency and consistency in IBS-C, IBS-D and IBS-M patients; furthermore, the intensity of abdominal pain and bloating was also significantly reduced.
When comparing pinaverium to otilonium bromide in IBS, both treatments were similarly useful in reducing the intensity of pain and in regulating bowel movements, but otilonium was superior to pinaverium in terms of decreasing pain frequency[89]. The side effects were similar in the two groups. The use of pinaverium has generally been considered safe; however, the drug is not licensed for use in pregnant women. In a letter reporting ten involuntary cases of pregnant women taking pinaverium bromide due to dispensing errors, nine individuals delivered healthy babies, while the tenth experienced a spontaneous abortion 1 week after the ingestion of pinaverium[90]. Several women complained of abdominal pain and constipation in parallel with pinaverium use.
Phloroglucinol
Experimental studies: Phloroglucinol is a phenol derivative with non-specific antispasmodic properties, together with its methylated form trimethylphloroglucinol. The mechanism of action is most likely based on the direct inhibition of the voltage-dependent calcium channels of smooth muscle; however, the modulation of prostaglandin or nitric oxide release has also been suggested[91]. Although it has long been used in clinical practice as an antispasmodic for painful urogenital and gastrointestinal conditions, in an early study on anesthetized rats, phloroglucinol was found to be inactive toward the contraction of the duodenum, ileum and colon[92]. Similarly, in anesthetized dogs, phloroglucinol plus trimethyl-phloroglucinol failed to antagonize acetylcholine-induced contraction of the colon[93].
Clinical trials: In parallel with animal studies, phloroglucinol plus trimethyl-phloroglucinol had no clear effects in humans on ascending and sigmoid colon hypermotility evoked by neostigmine[94]. However, in 20 IBS patients, iv phloroglucinol effectively reduced postprandial rectosigmoid motility increases after a test meal, compared to placebo[95]. In another study of IBS patients, phloroglucinol inhibited phasic contractions provoked by intrarectally injected glycerol, but it did not modify colonic tone[96]. In an open-label study of 100 IBS patients selected according to the Rome II criteria, po 50 mg phloroglucinol was administered three times daily for two months[97]. The 68 patients who completed the study reported significant improvement in abdominal pain, frequency of stools per day, urgency, passage of mucus per the rectum, sense of incomplete defecation and bloating. Nevertheless, straining was unchanged. Further, a multicenter, randomized, double-blind, placebo-controlled trial examined the effects of phloroglucinol/trimethylphloroglucinol (62.2 mg P plus 80 mg TMP three times daily) or placebo for 7 d in 307 IBS patients diagnosed using the Rome II criteria[98]. The relative decrease in pain intensity and the responder rate were significantly higher in the P/TMP-treated group, compared to the placebo-treated group. Further, the treatment effect persisted up to the 7th day in a higher percentage of patients treated with P/TMP than in those treated with placebo. The frequency and severity of adverse events did not differ between the two treatment groups, and no adverse events were considered sufficiently serious to stop treatment. Finally, according to a preliminary report, 72 patients with D-IBS, based on the ROME III criteria, were involved in a double-blind, placebo-controlled trial and were treated with placebo or phloroglucinol (80 mg) three times daily for 14 d after a 1-wk run-in period[99]. Significantly more patients reported “moderate or more improvement” in Subjects Global Assessment in the phloroglucinol group than in the placebo group over the 2-wk period of treatment and the 1-wk post-treatment period. Stool frequency decreased significantly in the phloroglucinol group, compared to the placebo group. Individual symptom scores and stool consistency also improved significantly, but they did not differ from those of the placebo group. Regarding its safety, a French epidemiologic study of phloroglucinol in pregnancy did not find evidence of a teratogenic risk in humans[100].
FUTURE PERSPECTIVES: T-TYPE CALCIUM CHANNELS
The low-voltage-activated or T-type Ca2+ channels (T-channels) are a subclass of voltage-gated Ca2+ channels named after their characteristic of being activated by small depolarizations of the plasma membrane[101,102]. They can also generate neuronal spontaneous firing and pacemaker activities, and they generally control excitability[101,102]. In mammals, T-channels are encoded by three pore-forming calcium-channel α1 subunit genes: CaV3.1, CaV3.2 and CaV3.3. The CaV3.2 subtype is expressed in the cell bodies and nerve endings of somatic afferent fibers, where it plays a role in regulating neuronal excitability and modifying pain perception[103,104]. Knockout of the CaV3.2 gene results in decreased mechanical, thermal and chemical sensitivity in mice, compared to their wild-type littermates[105], whereas systemic injections of mibefradil, a T-channel antagonist, induces mechanical and thermal antinociception in rats without affecting their sensorimotor abilities[106]. Interestingly, ethosuximide, an anti-epileptic and relatively selective T-channel blocker, elicits near-complete reversal of mechanical allodynia/hyperalgesia in a rat model of painful peripheral neuropathy induced by the chemotherapeutic agent paclitaxel, whereas opiates and the NMDA receptor antagonist MK-801 are only slightly or not effective in this model[107]. Despite the importance of T-channels in somatic pain perception, their roles in visceral perception and gastrointestinal pathologies have not been well established. Recently, an interesting study demonstrated the possible role of T-channels in the pathophysiology of IBS[108]. IBS was modeled in rats using intracolonic sodium butyrate injections, a method that induces colonic hypersensitivity by reproducing the elevated colonic butyrate concentrations found in a subset of IBS patients resulting from butyrogenic enteric flora[109]. CaV3.2 knockdown treatment prevented butyrate-induced hypersensitivity without modifying colonic sensitivity in control rats, suggesting that CaV3.2 channels do not significantly participate in colonic sensitivity under healthy conditions[108]. Further, the T-channel blocker mibefradil reversed butyrate-mediated colonic hypersensitivity by both intrathecal and topical routes. Similarly, intraperitoneal administration of other T-channel antagonists, ethosuximide and NP078585, produced robust antihyperalgesic effects[108]. T-channels were up-regulated in the dorsal root ganglions (DRGs) of butyrate-treated animals, and neuronal T-type current density was also increased, emphasizing the participation of T-channels in the mechanism of colonic hypersensitivity[108]. Based on these results, the antinociceptive effects of TTA-A2, a state-dependent CaV3 blocker, were tested recently in vitro in cell cultures and in mice DRGs, showing that TTA-A2 potently inhibited recombinant and native T-currents in sensory neurons expressing CaV3.2-like T-type channels, consequently decreasing their excitability[110]. Moreover, in the previously described rat IBS model, systemic administration of TTA-A2 robustly abolished butyrate-induced hypersensitivity and induced a statistically significant dose-dependent antihyperalgesic effect[110]. These results demonstrate that T-channel blockers are promising candidates for further research into novel analgesics that could be potentially useful for treating the characteristic symptoms of IBS, such as visceral pain and discomfort.
CONCLUSION
In conclusion, antispasmodics without cardiovascular actions, such as alverine citrate, mebeverine, otilonium bromide, pinaverium bromide and phloroglucinol, are widely used in therapy for IBS. Their effects are mostly based on their spasmolytic properties via the inhibition of calcium influx into smooth muscle cells. Further, otilonium could have direct inhibitory effects on primary sensory afferents, thus reducing hypersensitivity, which is a common feature in IBS. Otilonium and pinaverium are quaternary ammonium derivatives that are poorly absorbed from the GI tract, therefore mainly acting locally. Clinical trials with antispasmodics in IBS have sometimes been controversial, which can be explained by the marked placebo effect in many cases. Nevertheless, the overall results have generally been positive, showing that antispasmodics are able to regulate GI motility disturbances, defecation alterations and abdominal pain/discomfort, with excellent safety profiles. A new generation of calcium-channel blockers acting on T-type calcium channels could represent a novel therapeutic pathway in the future for the management of IBS.
Footnotes
P- Reviewers: Bonaz BL, Izzo AA S- Editor: Gou SX L- Editor: A E- Editor: Ma S
References
- 1.Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10:712–721.e4. doi: 10.1016/j.cgh.2012.02.029. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal N, Spiegel BM. The effect of irritable bowel syndrome on health-related quality of life and health care expenditures. Gastroenterol Clin North Am. 2011;40:11–19. doi: 10.1016/j.gtc.2010.12.013. [DOI] [PubMed] [Google Scholar]
- 3.Longstreth GF, Wilson A, Knight K, Wong J, Chiou CF, Barghout V, Frech F, Ofman JJ. Irritable bowel syndrome, health care use, and costs: a U.S. managed care perspective. Am J Gastroenterol. 2003;98:600–607. doi: 10.1111/j.1572-0241.2003.07296.x. [DOI] [PubMed] [Google Scholar]
- 4.Quigley EM, Abdel-Hamid H, Barbara G, Bhatia SJ, Boeckxstaens G, De Giorgio R, Delvaux M, Drossman DA, Foxx-Orenstein AE, Guarner F, et al. A global perspective on irritable bowel syndrome: a consensus statement of the World Gastroenterology Organisation Summit Task Force on irritable bowel syndrome. J Clin Gastroenterol. 2012;46:356–366. doi: 10.1097/MCG.0b013e318247157c. [DOI] [PubMed] [Google Scholar]
- 5.Casiday RE, Hungin AP, Cornford CS, de Wit NJ, Blell MT. GPs’ explanatory models for irritable bowel syndrome: a mismatch with patient models? Fam Pract. 2009;26:34–39. doi: 10.1093/fampra/cmn088. [DOI] [PubMed] [Google Scholar]
- 6.Agréus L, Svärdsudd K, Talley NJ, Jones MP, Tibblin G. Natural history of gastroesophageal reflux disease and functional abdominal disorders: a population-based study. Am J Gastroenterol. 2001;96:2905–2914. doi: 10.1111/j.1572-0241.2001.04680.x. [DOI] [PubMed] [Google Scholar]
- 7.Evangelista S. Benefits from long-term treatment in irritable bowel syndrome. Gastroenterol Res Pract. 2012;2012:936960. doi: 10.1155/2012/936960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poynard T, Regimbeau C, Benhamou Y. Meta-analysis of smooth muscle relaxants in the treatment of irritable bowel syndrome. Aliment Pharmacol Ther. 2001;15:355–361. doi: 10.1046/j.1365-2036.2001.00937.x. [DOI] [PubMed] [Google Scholar]
- 9.Lièvre M. Alosetron for irritable bowel syndrome. BMJ. 2002;325:555–556. doi: 10.1136/bmj.325.7364.555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Manning AP, Thompson WG, Heaton KW, Morris AF. Towards positive diagnosis of the irritable bowel. Br Med J. 1978;2:653–654. doi: 10.1136/bmj.2.6138.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drossman DA, Grant Thomson W, Talley NJ, Funch-Jensen P, Janssen J, Whitehead WE. Identification of sub-groups of functional gastrointestinal disorders. Gastroenterol Int. 1990;3:159–172. [Google Scholar]
- 12.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 13.Guilera M, Balboa A, Mearin F. Bowel habit subtypes and temporal patterns in irritable bowel syndrome: systematic review. Am J Gastroenterol. 2005;100:1174–1184. doi: 10.1111/j.1572-0241.2005.40674.x. [DOI] [PubMed] [Google Scholar]
- 14.Spiller RC. Role of infection in irritable bowel syndrome. J Gastroenterol. 2007;42 Suppl 17:41–47. doi: 10.1007/s00535-006-1925-8. [DOI] [PubMed] [Google Scholar]
- 15.McKendrick MW, Read NW. Irritable bowel syndrome--post salmonella infection. J Infect. 1994;29:1–3. doi: 10.1016/s0163-4453(94)94871-2. [DOI] [PubMed] [Google Scholar]
- 16.Neal KR, Hebden J, Spiller R. Prevalence of gastrointestinal symptoms six months after bacterial gastroenteritis and risk factors for development of the irritable bowel syndrome: postal survey of patients. BMJ. 1997;314:779–782. doi: 10.1136/bmj.314.7083.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mayer EA, Naliboff BD, Craig AD. Neuroimaging of the brain-gut axis: from basic understanding to treatment of functional GI disorders. Gastroenterology. 2006;131:1925–1942. doi: 10.1053/j.gastro.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 18.Fichna J, Storr MA. Brain-Gut Interactions in IBS. Front Pharmacol. 2012;3:127. doi: 10.3389/fphar.2012.00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whitehead WE. Psychosocial aspects of functional gastrointestinal disorders. Gastroenterol Clin North Am. 1996;25:21–34. doi: 10.1016/s0889-8553(05)70363-0. [DOI] [PubMed] [Google Scholar]
- 20.Drossman DA, Ringel Y, Vogt BA, Leserman J, Lin W, Smith JK, Whitehead W. Alterations of brain activity associated with resolution of emotional distress and pain in a case of severe irritable bowel syndrome. Gastroenterology. 2003;124:754–761. doi: 10.1053/gast.2003.50103. [DOI] [PubMed] [Google Scholar]
- 21.Yuan YZ, Tao RJ, Xu B, Sun J, Chen KM, Miao F, Zhang ZW, Xu JY. Functional brain imaging in irritable bowel syndrome with rectal balloon-distention by using fMRI. World J Gastroenterol. 2003;9:1356–1360. doi: 10.3748/wjg.v9.i6.1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bouin M, Plourde V, Boivin M, Riberdy M, Lupien F, Laganière M, Verrier P, Poitras P. Rectal distention testing in patients with irritable bowel syndrome: sensitivity, specificity, and predictive values of pain sensory thresholds. Gastroenterology. 2002;122:1771–1777. doi: 10.1053/gast.2002.33601. [DOI] [PubMed] [Google Scholar]
- 23.Gecse K, Róka R, Ferrier L, Leveque M, Eutamene H, Cartier C, Ait-Belgnaoui A, Rosztóczy A, Izbéki F, Fioramonti J, et al. Increased faecal serine protease activity in diarrhoeic IBS patients: a colonic lumenal factor impairing colonic permeability and sensitivity. Gut. 2008;57:591–599. doi: 10.1136/gut.2007.140210. [DOI] [PubMed] [Google Scholar]
- 24.Gecse K, Róka R, Séra T, Rosztóczy A, Annaházi A, Izbéki F, Nagy F, Molnár T, Szepes Z, Pávics L, et al. Leaky gut in patients with diarrhea-predominant irritable bowel syndrome and inactive ulcerative colitis. Digestion. 2012;85:40–46. doi: 10.1159/000333083. [DOI] [PubMed] [Google Scholar]
- 25.Annaházi A, Ferrier L, Bézirard V, Lévêque M, Eutamène H, Ait-Belgnaoui A, Coëffier M, Ducrotté P, Róka R, Inczefi O, et al. Luminal cysteine-proteases degrade colonic tight junction structure and are responsible for abdominal pain in constipation-predominant IBS. Am J Gastroenterol. 2013;108:1322–1331. doi: 10.1038/ajg.2013.152. [DOI] [PubMed] [Google Scholar]
- 26.Ahn JY, Lee KH, Choi CH, Kim JW, Lee HW, Kim JW, Kim MK, Kwon GY, Han S, Kim SE, et al. Colonic mucosal immune activity in irritable bowel syndrome: comparison with healthy controls and patients with ulcerative colitis. Dig Dis Sci. 2014;59:1001–1011. doi: 10.1007/s10620-013-2930-4. [DOI] [PubMed] [Google Scholar]
- 27.Barbara G, Stanghellini V, De Giorgio R, Cremon C, Cottrell GS, Santini D, Pasquinelli G, Morselli-Labate AM, Grady EF, Bunnett NW, et al. Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome. Gastroenterology. 2004;126:693–702. doi: 10.1053/j.gastro.2003.11.055. [DOI] [PubMed] [Google Scholar]
- 28.Dunlop SP, Jenkins D, Neal KR, Spiller RC. Relative importance of enterochromaffin cell hyperplasia, anxiety, and depression in postinfectious IBS. Gastroenterology. 2003;125:1651–1659. doi: 10.1053/j.gastro.2003.09.028. [DOI] [PubMed] [Google Scholar]
- 29.Grider JR, Foxx-Orenstein AE, Jin JG. 5-Hydroxytryptamine4 receptor agonists initiate the peristaltic reflex in human, rat, and guinea pig intestine. Gastroenterology. 1998;115:370–380. doi: 10.1016/s0016-5085(98)70203-3. [DOI] [PubMed] [Google Scholar]
- 30.Tam FS, Hillier K, Bunce KT. Characterization of the 5-hydroxytryptamine receptor type involved in inhibition of spontaneous activity of human isolated colonic circular muscle. Br J Pharmacol. 1994;113:143–150. doi: 10.1111/j.1476-5381.1994.tb16186.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kanazawa M, Palsson OS, Thiwan SI, Turner MJ, van Tilburg MA, Gangarosa LM, Chitkara DK, Fukudo S, Drossman DA, Whitehead WE. Contributions of pain sensitivity and colonic motility to IBS symptom severity and predominant bowel habits. Am J Gastroenterol. 2008;103:2550–2561. doi: 10.1111/j.1572-0241.2008.02066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lind CD. Motility disorders in the irritable bowel syndrome. Gastroenterol Clin North Am. 1991;20:279–295. [PubMed] [Google Scholar]
- 33.Wittmann T, Crenner F, Angel F, Hanusz L, Ringwald C, Grenier JF. Long-duration stress. Immediate and late effects on small and large bowel motility in rat. Dig Dis Sci. 1990;35:495–500. doi: 10.1007/BF01536925. [DOI] [PubMed] [Google Scholar]
- 34.Wittmann T, Vaxman F, Crenner F, Angel F, Grenier JF. Colonic electromyographic changes in irritable bowel syndrome (IBS) In: Varró V, de Chatel R, editors. 22 nd Congress of the International Society of Internal Medicine: ed. Monduzzi Editore; 1994. pp. 125–131. [Google Scholar]
- 35.Wittmann T, Vaxman F, Crenner F, Grenier JF. Alterations specifiques de la motricité colique dans la colopathie fonctionelle et constipation chronique. Gastroenterol Clin Biol. 1991;15:135A. [Google Scholar]
- 36.Fukudo S, Kanazawa M, Kano M, Sagami Y, Endo Y, Utsumi A, Nomura T, Hongo M. Exaggerated motility of the descending colon with repetitive distention of the sigmoid colon in patients with irritable bowel syndrome. J Gastroenterol. 2002;37 Suppl 14:145–150. doi: 10.1007/BF03326434. [DOI] [PubMed] [Google Scholar]
- 37.Kellow JE, Phillips SF. Altered small bowel motility in irritable bowel syndrome is correlated with symptoms. Gastroenterology. 1987;92:1885–1893. doi: 10.1016/0016-5085(87)90620-2. [DOI] [PubMed] [Google Scholar]
- 38.Clavé P. Treatment of IBS-D with 5-HT3 receptor antagonists vs spasmolytic agents: similar therapeutical effects from heterogeneous pharmacological targets. Neurogastroenterol Motil. 2011;23:1051–1055. doi: 10.1111/j.1365-2982.2011.01808.x. [DOI] [PubMed] [Google Scholar]
- 39.Catterall WA, Perez-Reyes E, Snutch TP, Striessnig J. International Union of Pharmacology. XLVIII. Nomenclature and structure-function relationships of voltage-gated calcium channels. Pharmacol Rev. 2005;57:411–425. doi: 10.1124/pr.57.4.5. [DOI] [PubMed] [Google Scholar]
- 40.Kochegarov AA. Pharmacological modulators of voltage-gated calcium channels and their therapeutical application. Cell Calcium. 2003;33:145–162. doi: 10.1016/s0143-4160(02)00239-7. [DOI] [PubMed] [Google Scholar]
- 41.Nowycky MC, Fox AP, Tsien RW. Three types of neuronal calcium channel with different calcium agonist sensitivity. Nature. 1985;316:440–443. doi: 10.1038/316440a0. [DOI] [PubMed] [Google Scholar]
- 42.Prior A, Harris SR, Whorwell PJ. Reduction of colonic motility by intravenous nicardipine in irritable bowel syndrome. Gut. 1987;28:1609–1612. doi: 10.1136/gut.28.12.1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abysique A, Lucchini S, Orsoni P, Mei N, Bouvier M. Effects of alverine citrate on cat intestinal mechanoreceptor responses to chemical and mechanical stimuli. Aliment Pharmacol Ther. 1999;13:561–566. doi: 10.1046/j.1365-2036.1999.00497.x. [DOI] [PubMed] [Google Scholar]
- 44.Coelho AM, Jacob L, Fioramonti J, Bueno L. Rectal antinociceptive properties of alverine citrate are linked to antagonism at the 5-HT1A receptor subtype. J Pharm Pharmacol. 2001;53:1419–1426. doi: 10.1211/0022357011777783. [DOI] [PubMed] [Google Scholar]
- 45.Bueno L, Beaufrand C, Theodorou V, Andro-Delestrain MC. Influence of simethicone and alverine on stress-induced alterations of colonic permeability and sensitivity in rats: beneficial effect of their association. J Pharm Pharmacol. 2013;65:567–573. doi: 10.1111/jphp.12021. [DOI] [PubMed] [Google Scholar]
- 46.Mitchell SA, Mee AS, Smith GD, Palmer KR, Chapman RW. Alverine citrate fails to relieve the symptoms of irritable bowel syndrome: results of a double-blind, randomized, placebo-controlled trial. Aliment Pharmacol Ther. 2002;16:1187–1195. doi: 10.1046/j.1365-2036.2002.01277.x. [DOI] [PubMed] [Google Scholar]
- 47.Altintaş E, Uçbilek E, Sezgin O, Sayici Y. Alverine citrate plus simethicone reduces cecal intubation time in colonoscopy - a randomized study. Turk J Gastroenterol. 2008;19:174–179. [PubMed] [Google Scholar]
- 48.Wittmann T, Paradowski L, Ducrotté P, Bueno L, Andro Delestrain MC. Clinical trial: the efficacy of alverine citrate/simeticone combination on abdominal pain/discomfort in irritable bowel syndrome--a randomized, double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2010;31:615–624. doi: 10.1111/j.1365-2036.2009.04216.x. [DOI] [PubMed] [Google Scholar]
- 49.Den Hertog A, Van den Akker J. Modification of alpha 1-receptor-operated channels by mebeverine in smooth muscle cells of guinea-pig taenia caeci. Eur J Pharmacol. 1987;138:367–374. doi: 10.1016/0014-2999(87)90475-4. [DOI] [PubMed] [Google Scholar]
- 50.Greenslade FC, Scott CK, Newquist KL, Krider KM, Chasin M. Heterogeneity of biochemical actions among vasodilators. J Pharm Sci. 1982;71:94–100. doi: 10.1002/jps.2600710123. [DOI] [PubMed] [Google Scholar]
- 51.Lindner A, Selzer H, Claassen V, Gans P, Offringa OR, Zwagemakers JM. Pharmacological properties of mebeverine, a smooth-muscle relaxant. Arch Int Pharmacodyn Ther. 1963;145:378–395. [PubMed] [Google Scholar]
- 52.Connell AM. Physiological and clinical assessment of the effect of the musculotropic agent mebeverine on the human colon. Br Med J. 1965;2:848–851. doi: 10.1136/bmj.2.5466.848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Evans PR, Bak YT, Kellow JE. Mebeverine alters small bowel motility in irritable bowel syndrome. Aliment Pharmacol Ther. 1996;10:787–793. doi: 10.1046/j.1365-2036.1996.61203000.x. [DOI] [PubMed] [Google Scholar]
- 54.Van Outryve M, Mayeur S, Meeus MA, Rosillon D, Hendrickx B, Ceuppens M. A double-blind crossover comparison study of the safety and efficacy of mebeverine with mebeverine sustained release in the treatment of irritable bowel syndrome. J Clin Pharm Ther. 1995;20:277–282. doi: 10.1111/j.1365-2710.1995.tb00663.x. [DOI] [PubMed] [Google Scholar]
- 55.Lu CL, Chen CY, Chang FY, Chang SS, Kang LJ, Lu RH, Lee SD. Effect of a calcium channel blocker and antispasmodic in diarrhoea-predominant irritable bowel syndrome. J Gastroenterol Hepatol. 2000;15:925–930. doi: 10.1046/j.1440-1746.2000.02230.x. [DOI] [PubMed] [Google Scholar]
- 56.Lee KJ, Kim NY, Kwon JK, Huh KC, Lee OY, Lee JS, Choi SC, Sohn CI, Myung SJ, Park HJ, et al. Efficacy of ramosetron in the treatment of male patients with irritable bowel syndrome with diarrhea: a multicenter, randomized clinical trial, compared with mebeverine. Neurogastroenterol Motil. 2011;23:1098–1104. doi: 10.1111/j.1365-2982.2011.01771.x. [DOI] [PubMed] [Google Scholar]
- 57.Darvish-Damavandi M, Nikfar S, Abdollahi M. A systematic review of efficacy and tolerability of mebeverine in irritable bowel syndrome. World J Gastroenterol. 2010;16:547–553. doi: 10.3748/wjg.v16.i5.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kruis W, Weinzierl M, Schüssler P, Holl J. Comparison of the therapeutic effect of wheat bran, mebeverine and placebo in patients with the irritable bowel syndrome. Digestion. 1986;34:196–201. doi: 10.1159/000199329. [DOI] [PubMed] [Google Scholar]
- 59.Enck P, Klosterhalfen S, Kruis W. [Determination of placebo effect in irritable bowel syndrome] Dtsch Med Wochenschr. 2005;130:1934–1937. doi: 10.1055/s-2005-872605. [DOI] [PubMed] [Google Scholar]
- 60.Everitt HA, Moss-Morris RE, Sibelli A, Tapp L, Coleman NS, Yardley L, Smith PW, Little PS. Management of irritable bowel syndrome in primary care: feasibility randomised controlled trial of mebeverine, methylcellulose, placebo and a patient self-management cognitive behavioural therapy website. (MIBS trial) BMC Gastroenterol. 2010;10:136. doi: 10.1186/1471-230X-10-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Everitt H, Moss-Morris R, Sibelli A, Tapp L, Coleman N, Yardley L, Smith P, Little P. Management of irritable bowel syndrome in primary care: the results of an exploratory randomised controlled trial of mebeverine, methylcellulose, placebo and a self-management website. BMC Gastroenterol. 2013;13:68. doi: 10.1186/1471-230X-13-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kennedy T, Jones R, Darnley S, Seed P, Wessely S, Chalder T. Cognitive behaviour therapy in addition to antispasmodic treatment for irritable bowel syndrome in primary care: randomised controlled trial. BMJ. 2005;331:435. doi: 10.1136/bmj.38545.505764.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Reme SE, Stahl D, Kennedy T, Jones R, Darnley S, Chalder T. Mediators of change in cognitive behaviour therapy and mebeverine for irritable bowel syndrome. Psychol Med. 2011;41:2669–2679. doi: 10.1017/S0033291711000328. [DOI] [PubMed] [Google Scholar]
- 64.Evangelista S. Quaternary ammonium derivatives as spasmolytics for irritable bowel syndrome. Curr Pharm Des. 2004;10:3561–3568. doi: 10.2174/1381612043382972. [DOI] [PubMed] [Google Scholar]
- 65.Evangelista S, Cochet P, Bromet N, Criscuoli M, Maggi CA. A distribution study with (14)C-otilonium bromide in the rat: evidence for selective tropism for large intestine after oral administration. Drug Metab Dispos. 2000;28:643–647. [PubMed] [Google Scholar]
- 66.Evangelista S, Giachetti A, Chapelain B, Neliat G, Maggi CA. Receptor binding profile of Otilonium bromide. Pharmacol Res. 1998;38:111–117. doi: 10.1006/phrs.1998.0340. [DOI] [PubMed] [Google Scholar]
- 67.Lindqvist S, Hernon J, Sharp P, Johns N, Addison S, Watson M, Tighe R, Greer S, Mackay J, Rhodes M, et al. The colon-selective spasmolytic otilonium bromide inhibits muscarinic M(3) receptor-coupled calcium signals in isolated human colonic crypts. Br J Pharmacol. 2002;137:1134–1142. doi: 10.1038/sj.bjp.0704942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Czimmer J, Süto G, Király A, Mózsik G. Otilonium bromide enhances sensory thresholds of volume and pressure in patients with irritable bowel syndrome. J Physiol Paris. 2001;95:153–156. doi: 10.1016/s0928-4257(01)00020-1. [DOI] [PubMed] [Google Scholar]
- 69.Baldi F, Longanesi A, Blasi A, Monello S, Cestari R, Missale G, Corazziari E, Badiali G, Pescatori M, Anastasio G. Clinical and functional evaluation of the efficacy of otilonium bromide: a multicenter study in Italy. Ital J Gastroenterol. 1991;23:60–63. [PubMed] [Google Scholar]
- 70.Battaglia G, Morselli-Labate AM, Camarri E, Francavilla A, De Marco F, Mastropaolo G, Naccarato R. Otilonium bromide in irritable bowel syndrome: a double-blind, placebo-controlled, 15-week study. Aliment Pharmacol Ther. 1998;12:1003–1010. doi: 10.1046/j.1365-2036.1998.00397.x. [DOI] [PubMed] [Google Scholar]
- 71.Glende M, Morselli-Labate AM, Battaglia G, Evangelista S. Extended analysis of a double-blind, placebo-controlled, 15-week study with otilonium bromide in irritable bowel syndrome. Eur J Gastroenterol Hepatol. 2002;14:1331–1338. doi: 10.1097/00042737-200212000-00008. [DOI] [PubMed] [Google Scholar]
- 72.Clavé P, Acalovschi M, Triantafillidis JK, Uspensky YP, Kalayci C, Shee V, Tack J. Randomised clinical trial: otilonium bromide improves frequency of abdominal pain, severity of distention and time to relapse in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 2011;34:432–442. doi: 10.1111/j.1365-2036.2011.04730.x. [DOI] [PubMed] [Google Scholar]
- 73.Boeckxstaens G, Corazziari ES, Mearin F, Tack J. IBS and the role of otilonium bromide. Int J Colorectal Dis. 2013;28:295–304. doi: 10.1007/s00384-012-1598-0. [DOI] [PubMed] [Google Scholar]
- 74.Ford AC, Talley NJ, Spiegel BM, Foxx-Orenstein AE, Schiller L, Quigley EM, Moayyedi P. Effect of fibre, antispasmodics, and peppermint oil in the treatment of irritable bowel syndrome: systematic review and meta-analysis. BMJ. 2008;337:a2313. doi: 10.1136/bmj.a2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chang FY, Lu CL, Luo JC, Chen TS, Chen MJ, Chang HJ. The evaluation of otilonium bromide treatment in asian patients with irritable bowel syndrome. J Neurogastroenterol Motil. 2011;17:402–410. doi: 10.5056/jnm.2011.17.4.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Christen MMO, Tassignon JP. Pinaverium bromide: A calcium channel blocker acting selectively on the gastrointestinal tract. Drug Dev Res. 1989;18:101–112. [Google Scholar]
- 77.Malysz J, Farraway LA, Christen MO, Huizinga JD. Pinaverium acts as L-type calcium channel blocker on smooth muscle of colon. Can J Physiol Pharmacol. 1997;75:969–975. doi: 10.1139/cjpp-75-8-969. [DOI] [PubMed] [Google Scholar]
- 78.Baumgartner A, Drack E, Halter F, Scheurer U. Effects of pinaverium bromide and verapamil on the motility of the rat isolated colon. Br J Pharmacol. 1985;86:89–94. doi: 10.1111/j.1476-5381.1985.tb09438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Boyer JC, Magous R, Christen MO, Balmes JL, Bali JP. Contraction of human colonic circular smooth muscle cells is inhibited by the calcium channel blocker pinaverium bromide. Cell Calcium. 2001;29:429–438. doi: 10.1054/ceca.2001.0205. [DOI] [PubMed] [Google Scholar]
- 80.Dai Y, Liu JX, Li JX, Xu YF. Effect of pinaverium bromide on stress-induced colonic smooth muscle contractility disorder in rats. World J Gastroenterol. 2003;9:557–561. doi: 10.3748/wjg.v9.i3.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fioramonti J, Christen MO, Dupre I, Bueno L. Involvement of a CCK-dependent capsaicin-sensitive afferent pathway in the inhibitory effect of pinaverium bromide on the colonic motor response to eating in rats. Fundam Clin Pharmacol. 1997;11:231–236. doi: 10.1111/j.1472-8206.1997.tb00190.x. [DOI] [PubMed] [Google Scholar]
- 82.Levy C, Charbonnier A, Cachin M. [Pinaverium bromide and functional colonic disease (double-blind study] Sem Hop Ther. 1977;53:372–374. [PubMed] [Google Scholar]
- 83.Fehér A, Wittmann T, Kiss J, Rosztóczy A, Varga I, Jánosi J. Therapeutic effect of pinaverium bromide in irritable bowel syndrome (IBS). A pilot study. Zeitschrift für Gastroenterologie. 1993;31:71 A. [Google Scholar]
- 84.Wittmann T, Fehér A, Rosztóczy A, Jánosi J. [Effectiveness of pinaverium bromide therapy on colonic motility disorders in irritable bowel syndrome] Orv Hetil. 1999;140:469–473. [PubMed] [Google Scholar]
- 85.Awad RACV, Dibildox M, Santiago R, Camacho S. Reduction of post-prandial motility by pinaverium bromide a calcium channel blocker acting selectively on the gastrointestinal tract in patients with irritable bowel syndrome. Acta Gastroenterol Latinoam. 1997;27:247–251. [PubMed] [Google Scholar]
- 86.Bouchoucha M, Faye A, Devroede G, Arsac M. Effects of oral pinaverium bromide on colonic response to food in irritable bowel syndrome patients. Biomed Pharmacother. 2000;54:381–387. doi: 10.1016/S0753-3322(01)80005-6. [DOI] [PubMed] [Google Scholar]
- 87.Jayanthi V, Malathi S, Ramathilakam B, Dinakaran N, Balasubramanian V, Mathew S. Role of pinaverium bromide in south Indian patients with irritable bowel syndrome. J Assoc Physicians India. 1998;46:369–371. [PubMed] [Google Scholar]
- 88.López-Alvarenga JC, Sobrino-Cossío S, Remes-Troche JM, Chiu-Ugalde J, Vargas-Romero JA, Schmulson M. Polar vectors as a method for evaluating the effectiveness of irritable bowel syndrome treatments: an analysis with pinaverium bromide 100mg plus simethicone 300mg po bid. Rev Gastroenterol Mex. 2013;78:21–27. doi: 10.1016/j.rgmx.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 89.Defrance P, Casini A. A comparison of the action of otilonium bromide and pinaverium bromide: study conducted under clinical control. Ital J Gastroenterol. 1991;23:64–66. [PubMed] [Google Scholar]
- 90.Einarson A, Bailey B, Koren G. Pregnancy outcome of women exposed to pinaverium due to a dispensing error. Ann Pharmacother. 1999;33:112–113. doi: 10.1345/aph.18175. [DOI] [PubMed] [Google Scholar]
- 91.Bueno L, Fioramonti J, Delvaux M, Frexinos J. Mediators and pharmacology of visceral sensitivity: from basic to clinical investigations. Gastroenterology. 1997;112:1714–1743. doi: 10.1016/s0016-5085(97)70056-8. [DOI] [PubMed] [Google Scholar]
- 92.Subissi A, Brunori P, Bachi M. Effects of spasmolytics on K+-induced contraction of rat intestine in vivo. Eur J Pharmacol. 1983;96:295–301. doi: 10.1016/0014-2999(83)90320-5. [DOI] [PubMed] [Google Scholar]
- 93.Sasaki D, Kido A, Yoshida Y. Effect of antispasmodic drugs on colonic motility. Part I: Laboratory study of the dog. Int J Clin Pharmacol Ther Toxicol. 1984;22:333–337. [PubMed] [Google Scholar]
- 94.Sasaki D, Kido A, Yoshida Y. Effect of antispasmodic drugs on the colonic motility. Part II: Clinical study in man. Int J Clin Pharmacol Ther Toxicol. 1984;22:338–341. [PubMed] [Google Scholar]
- 95.Cargill G, Salin B, Lubin S, Kohler F, Coste T, Rautureau J. [Effect of phloroglucinol on rectosigmoid motility stimulated by a test meal. Study in patients with irritable bowel syndrome] Presse Med. 1992;21:19–23. [PubMed] [Google Scholar]
- 96.Louvel D, Delvaux M, Staumont G, Camman F, Fioramonti J, Bueno L, Frexinos J. Intracolonic injection of glycerol: a model for abdominal pain in irritable bowel syndrome? Gastroenterology. 1996;110:351–361. doi: 10.1053/gast.1996.v110.pm8566580. [DOI] [PubMed] [Google Scholar]
- 97.Jafri W, Yakoob J, Hussain S, Jafri N, Islam M. Phloroglucinol in irritable bowel syndrome. J Pak Med Assoc. 2006;56:5–8. [PubMed] [Google Scholar]
- 98.Chassany O, Bonaz B, Bruley DES Varannes S, Bueno L, Cargill G, Coffin B, Ducrotté P, Grangé V. Acute exacerbation of pain in irritable bowel syndrome: efficacy of phloroglucinol/trimethylphloroglucinol. A randomized, double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2007;25:1115–1123. doi: 10.1111/j.1365-2036.2007.03296.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cha BK, Choi CH, Kim BJ, Oh HC, Kim JW, Do JH, Kim JG, Chang SK. The Effect of Phloroglucinol in Diarrhea-Dominant Irritable Bowel Syndrome: Randomized, Double-Blind, Placebo-Controlled Trial. Gastroenterology. 2011;140:S–611-S-612. [Google Scholar]
- 100.Lacroix I, Hurault-Delarue C, Kessler S, Guitard C, Vidal S, Albouy-Cossard C, Montastruc JL, Damase-Michel C. [First epidemiologic data about phloroglucinol exposure during first trimester of pregnancy] Gynecol Obstet Fertil. 2011;39:694–697. doi: 10.1016/j.gyobfe.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 101.Huguenard JR. Low-threshold calcium currents in central nervous system neurons. Annu Rev Physiol. 1996;58:329–348. doi: 10.1146/annurev.ph.58.030196.001553. [DOI] [PubMed] [Google Scholar]
- 102.Chemin J, Monteil A, Perez-Reyes E, Bourinet E, Nargeot J, Lory P. Specific contribution of human T-type calcium channel isotypes (alpha(1G), alpha(1H) and alpha(1I)) to neuronal excitability. J Physiol. 2002;540:3–14. doi: 10.1113/jphysiol.2001.013269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Todorovic SM, Jevtovic-Todorovic V, Meyenburg A, Mennerick S, Perez-Reyes E, Romano C, Olney JW, Zorumski CF. Redox modulation of T-type calcium channels in rat peripheral nociceptors. Neuron. 2001;31:75–85. doi: 10.1016/s0896-6273(01)00338-5. [DOI] [PubMed] [Google Scholar]
- 104.Zamponi GW, Lewis RJ, Todorovic SM, Arneric SP, Snutch TP. Role of voltage-gated calcium channels in ascending pain pathways. Brain Res Rev. 2009;60:84–89. doi: 10.1016/j.brainresrev.2008.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Choi S, Na HS, Kim J, Lee J, Lee S, Kim D, Park J, Chen CC, Campbell KP, Shin HS. Attenuated pain responses in mice lacking Ca(V)3.2 T-type channels. Genes Brain Behav. 2007;6:425–431. doi: 10.1111/j.1601-183X.2006.00268.x. [DOI] [PubMed] [Google Scholar]
- 106.Todorovic SM, Meyenburg A, Jevtovic-Todorovic V. Mechanical and thermal antinociception in rats following systemic administration of mibefradil, a T-type calcium channel blocker. Brain Res. 2002;951:336–340. doi: 10.1016/s0006-8993(02)03350-4. [DOI] [PubMed] [Google Scholar]
- 107.Flatters SJ, Bennett GJ. Ethosuximide reverses paclitaxel- and vincristine-induced painful peripheral neuropathy. Pain. 2004;109:150–161. doi: 10.1016/j.pain.2004.01.029. [DOI] [PubMed] [Google Scholar]
- 108.Marger F, Gelot A, Alloui A, Matricon J, Ferrer JF, Barrère C, Pizzoccaro A, Muller E, Nargeot J, Snutch TP, et al. T-type calcium channels contribute to colonic hypersensitivity in a rat model of irritable bowel syndrome. Proc Natl Acad Sci USA. 2011;108:11268–11273. doi: 10.1073/pnas.1100869108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bourdu S, Dapoigny M, Chapuy E, Artigue F, Vasson MP, Dechelotte P, Bommelaer G, Eschalier A, Ardid D. Rectal instillation of butyrate provides a novel clinically relevant model of noninflammatory colonic hypersensitivity in rats. Gastroenterology. 2005;128:1996–2008. doi: 10.1053/j.gastro.2005.03.082. [DOI] [PubMed] [Google Scholar]
- 110.Francois A, Kerckhove N, Meleine M, Alloui A, Barrere C, Gelot A, Uebele VN, Renger JJ, Eschalier A, Ardid D, et al. State-dependent properties of a new T-type calcium channel blocker enhance Ca(V)3.2 selectivity and support analgesic effects. Pain. 2013;154:283–293. doi: 10.1016/j.pain.2012.10.023. [DOI] [PubMed] [Google Scholar]


