Abstract
Orthotopic liver transplantation (OLT) represents a major treatment for end-stage chronic liver disease, as well as selected cases of hepatocellular carcinoma and acute liver failure. The ever-increasing development of imaging modalities significantly contributed, over the last decades, to the management of recipients both in the pre-operative and post-operative period, thus impacting on graft and patients survival. When properly used, imaging modalities such as ultrasound, multidetector computed tomography, magnetic resonance imaging (MRI) and procedures of direct cholangiography are capable to provide rapid and reliable recognition and treatment of vascular and biliary complications occurring after OLT. Less defined is the role for imaging in assessing primary graft dysfunction (including rejection) or chronic allograft disease after OLT, e.g., hepatitis C virus (HCV) recurrence. This paper: (1) describes specific characteristic of the above imaging modalities and the rationale for their use in clinical practice; (2) illustrates main imaging findings related to post-OLT complications in adult patients; and (3) reviews future perspectives emerging in the surveillance of recipients with HCV recurrence, with special emphasis on MRI.
Keywords: Orthotopic liver transplantation, Ultrasound, Computed tomography, Magnetic resonance imaging, T-tube cholangiography, Endoscopic retrograde cholangiography, Percutaneous transhepatic cholangiography, Orthotopic liver transplantation complications, Human C virus recurrence
Core tip: Complications after orthotopic liver transplantation (OLT) still constitute a significant cause of morbidity and graft loss. Prompt diagnosis is then essential in order to address patients to most proper treatment and assure graft and patient survival, especially in the case of vascular and biliary complications. The review focuses on: (1) the state-of-the-art role for different imaging modalities in assessing post-OLT complications, together with practical recommendations for their use; and (2) future perspective for quantitative imaging modalities in non-invasively assessing primary hepatic complications (for which the role of conventional imaging is still limited), using human C virus recurrence as the most exemplificative scenario.
INTRODUCTION
Orthotopic liver transplantation (OLT) represents a major treatment for end-stage chronic liver disease, as well as selected cases of hepatocellular carcinoma (HCC) and acute liver failure[1,2]. Because of progressive refinements in patient selection, surgical technique, organ preservation and immunosuppressive agents, long-term outcome after the intervention has significantly improved over the last decades, with 5-year graft and patient survival rates of 67% and 74%, respectively[3]. The overwhelming evolution of imaging techniques that has occurred in parallel significantly contributed to reducing morbidity and mortality after OLT[4]. Indeed, last generation imaging techniques have the capability to provide rapid and reliable answers to inquiries coming from surgeons, hepatologists, anesthetists and pathologists forming the OLT-team. In the pre-operative period, imaging is essential in selecting adequate transplant candidates and planning surgery, e.g., by defining biliary and vascular anatomy in living-donors and recipients[5] or evaluating whether patients with HCC fulfill the criteria for transplantation[2]. In the post-operative period, the main role for imaging modalities is monitoring patients and assessing early and late complications, thus significantly influencing post-OLT management and contributing to increase graft and patients survival[3,5].
A variety of diagnostic and interventional imaging modalities are currently available in the field of liver transplantation. Radiologists and referring clinicians should be aware of the specific capabilities of each of them, in order to maximize rapidity and efficacy of the diagnosis, especially in the case of life- and graft-threatening vascular and biliary complications. Less defined is the role of imaging in assessing OLT complications primarily affecting the graft, including rejection or hepatitis C virus (HCV) recurrence. In this paper, we describe and illustrate the state-of-the-art role for imaging techniques in evaluating and managing adult patients in the post-operative period. We also describe future perspectives in the assessment of primary hepatic complications, for which the goal of imaging is to replace biopsy with noninvasive tools. Given the available clinical and radiological evidence, we focus on HCV-infected recipients as the most exemplificative scenario, with special emphasis on magnetic resonance imaging (MRI). Because of the paucity of specific radiological literature, detailed review of other clinical settings, such as that of human B virus (HBV)-patients, is beyond the purpose of this paper.
IMAGING MODALITIES IN ASSESSING POST-OLT PATIENTS
A variety of complications may occur after OLT, as shown in Table 1. Despite defined characteristics and time of presentation, complications frequently show a largely overlapping spectrum of clinical and laboratory findings[5]. In the early post-OLT period, the most difficult differential diagnosis is between rejection, which can be definitively assessed by graft biopsy only, and vascular and/or biliary complications impairing the graft function[6]. On this basis, the aim of state-of-the-art imaging is to detect or exclude complications of vascular and biliary origin, in order to assure prompt treatment and graft survival. Ultrasound (US), multidetector computed tomography (MDCT), MRI and procedures of direct cholangiography are currently the main imaging tools used for this purpose. Figure 1 illustrates the imaging workflow used in our institution to assess post-OLT complications with the above modalities.
Table 1.
Overview of main complications occurring after liver transplantation
| Type of complication | Prevalence in adult OLT patients | Risk factors | Time of onset from OLT |
| Vascular complications | 9% | ||
| Hepatic artery complications | |||
| Hepatic artery thrombosis | 3%-10% | RejectionEnd-to-end anastomosisABO blood group incompatibility Prolonged cold ischemia time of the graftPediatric transplant | Weeks to months |
| Hepatic artery stenosis | 2%-10% | RejectionPoor surgical techniqueClamp injury | Within first 3 mo |
| Pseudoaneurysm | Rare | AngioplastyLiver biopsyFocal infection | Variable |
| Portal vein complications | 1%-13% | ||
| Thrombosis | 1%-2% | Technical problems during surgeryExcessive vessel lengthDiscrepancy between donor and recipient calibersHypercoagulability stateHistory of previous thrombosis | Variable |
| Stenosis | 1% | Variable | |
| IVC and hepatic vins complications | Rare | ||
| Thrombosis and stenosis | < 1% | Size discrepancy between donor and recipient vesselsSuprahepatic caval kinking from liver rotationSurgical techniqueHypercoagulability stateCompression from graft edema or adjacent fluid collectionChronic thrombusNeointimal hyperplasiaRetransplantationPediatric OLTLDLT (hepatic vein stenosis) | Variable |
| Hemorrhage | Up to 3% | Piggyback anastomosis | Early from OLT |
| Biliary complications | 11%-30% | ||
| Bile leak | 4%-5% | T-tube displacement or removal (T-tube leak)Technical failure during surgery (anastomotic leak)HAT (nonanastomotic leak)Ischemic-related injury, immunologically-related injury, cytotoxic injury induced by bile salts (nonanastomotic leak in pts. without HAT) | 1-3 mo |
| Biliary obstruction - anastomotic strictures | Up to 17.6% | Roux-en-Y choledochojejunostomyAnastomotic leakageTechnical factors | Within 1 yr |
| Biliary obstruction - NAS and ITBL | 5%-10% | HAT (NAS)Microangiopathic injury (prolonged warm or cold ischemia times) (ITBL)Immunogenic injury (AB0 incompatibility between donor and recipient, chronic ductopenic rejection, primitive sclerosing cholangitis) (ITBL)cytotoxic injury by bile salts (ITBL) | Within 6 mo (NAS)After 6 mo (ITBL) |
| Stones, casts and sludge | 5.70% | Anastomotic and nonanastomotic biliary stricturesPresence of T-tube or stentHepaticojejunostomyIschemiaInfectionsAlteration in bile composition | Within 1 yr (casts and sludge)After 1 yr (stones) |
| Primary hepatic complications | |||
| Acute cellular rejection | Common | ImmunosuppressionTransplantation for cholestatic diseasePreservation injury | Early from OLT |
| Chronic ductopenic rejection | Up to 17% | Retransplant for chronic rejectionTransplant for cholestatic diseaseCMV infectionLow levels of immunosuppression | 6 wk to 6 mo |
| Other causes of graft dysfunction | - | Variable | Variable |
| Collections, hematoma, abscess | |||
| Biloma | - | Bile leakageHATHAS | Depends on the cause |
| Hematoma, seroma | - | Surgical technique | Depends on the cause |
| Abscess | - | CollectionsBacteremia | Depends on the cause |
| Malignacies | |||
| HCC recurrence | Rare | Selection criteria beyond Milan criteria | Years |
| PTLD | 0.0%-2.9% | EBV infectionCMV donor-recipient mismatchCMV disease | Within 1 yr |
Figure 1.
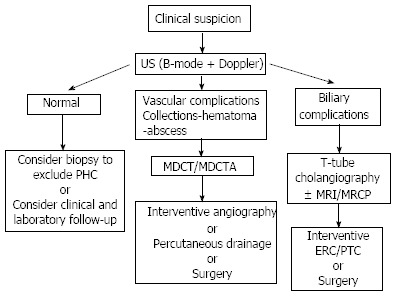
Suggested workflow for the assessment and management of post-transplant complications. US: Ultrasound; MDCT: Multidetector computed tomography; ERC: Endoscopic retrograde cholangiography; PTC: Percutaneous transhepatic cholangiography; MDCTA: Multidetector computed tomography angiography; PHC: Primary hepatic complications.
US
The first-line imaging modality to evaluate post-OLT patients is US, using both grayscale and color Doppler examination. US is accessible and can be performed at patient’s bedside, providing a quick evaluation of the hepatic parenchyma, perihepatic region, biliary tree and vasculature. On the other hand, US lacks panoramicity and is affected, especially in the immediate postoperative period, by fixed patient positioning and limited acoustic windows (related to bowel gas and surgical dressing material). Despite these limitations, US was proven to be accurate and reproducible when performed by skilled operators[7]. Accordingly, US is used to screen complications or follow-up minor findings, usually by performing serial examinations scheduled according to center-specific protocols[8]. In our institution, the baseline examination is performed within few hours of surgery, followed by daily controls until hospital discharge. Close US controls are essential in the surveillance for early graft-threatening complications, as recently emphasized by some investigators[9], who proposed an implantable continuous Doppler monitoring device to screen patients for hepatic artery thrombosis.
B-mode evaluation permits to assess the homogeneity of graft echotexture and bile ducts caliber, as well as the presence of perihepatic and intra-abdominal free fluid or collections. Pulsed and color Doppler examination is used complementarily to investigate vessels patency and flow spectra. Emphasis has been placed on correct optimization of Doppler technique[3], using appropriate angle to provide reliable and reproducible spectra and velocity measurements. Low wall filter, highest gain without background noise, and lowest pulse repetition frequency without aliasing are additional basic requirements to maximize Doppler examination, e.g., in order to detect low flow or avoiding misdiagnosis of hepatofugal flow[3,5,7].
When the interpretation of Doppler studies is inconclusive or challenging, contrast-enhanced US (CEUS) has been advocated as a tool to provide additional, relevant clinical information in assessing arterial and venous stenosis and fistulas, liver infarction and necrosis, liver abscess, hematomas, acute bleeding, and malignancy[10]. Furthermore, CEUS has been reported to be less sensitive than US to hearth-related artifacts, respiration, or lack of patients compliance[11]. Second-generation perfluorocarbon-based contrast agents are currently recommended, since the persistence in the bloodstream exceeds that of first generation, air-based microbubble contrast agents[12,13]. CEUS has been recommended in the case of inconclusive Doppler examination of the graft vasculature to reliably assessing hepatic artery thrombosis or stenosis, as well as evaluating the shape and patency of the caval and portal anastomoses. Alternatively, CEUS may guide targeted Doppler reassessment of arterial branches in order to provide ultimate differentiation between thrombosis and slow flow caused by vasoconstriction or splenic steal[14]. Indeed, microbubbles persisting in the late phase enhance the Doppler signal, which is of help in investigating small vessels missed without contrast. Additional indications to CEUS include: (1) to search for active bleeding; (2) to exclude perfusion defects when parenchymal infarction is suspected; and (3) to monitor the effects of thrombolysis after hepatic artery thrombosis[14]. Moreover, some authors showed the feasibility of US-cholangiograms by injecting sonographic contrast medium into the T-tube[15]. Such an approach has been advocated as a “quick and dirty” evaluation for bile leakage at patient’s bedside, showing good image quality and diagnostic accuracy.
In summary, US/CEUS should be used as the first-line imaging to screen patients for post-OLT complications, especially vascular complications such as hepatic artery thrombosis.
MDCT
In post-OLT patients, MDCT is indicated when clinical and/or US findings are equivocal or suspicious for major complications requiring pre-treatment confirmation. As a general rule, MDCT should be the second-line modality of choice for the assessment of vascular abnormalities and intrahepatic or abdominal complications, both in the early and late post-OLT period[16]. Indeed, Computed Tomography provides a rapid and panoramic representation of the whole abdomen (and possibly the thorax) with high spatial and temporal resolution, thus making possible to incorporate both angiographic (MDCT angiography; MDCTA) and parenchymal studies into a unique examination session[17].
Given the fact that last-generation equipments permit to scan large body volumes in few seconds, the overall duration of MDCT examination is short, which is a further advantage in order to obtain rapid diagnosis and better image quality in critical and less collaborating patients, e.g., by reducing respiratory artifacts. Major drawbacks concerning the use of MDCT are related: (1) to X-ray exposure, which should be avoided in younger patients with the need of repeated examinations; and (2) to contraindications to iv administration of iodinate contrast agents, including renal function impairment and history of adverse reactions.
In summary, MDCT/MDCTA should be used as the preferred second-line modality of choice after US in order to rapidly and panoramically evaluate vascular complications and the effects of vascular complications on the graft.
MRI
State-of-the-art MRI using 1.5 or 3.0 T magnets is the preferred noninvasive modality to investigate biliary complications. For this purpose, magnetic resonance cholangiography (MRC) technique is required as the core of an MRI examination. MRC enables a panoramic and detailed representation of bile ducts, which appear as markedly hyperintense structures over a low-signal background. This elective representation is based on heavily T2-weighted sequences and requires no iv administration of gadolinium-based contrast agents, which is of help in patients with renal function impairment at risk of developing nephrogenic systemic fibrosis (NSF), i.e., those with a glomerular filtration rate lower than 30 mL/min[18].
Two different techniques are currently available, namely 3D and 2D MRC, based on volumetric fast spin echo (FSE) and 2D single-shot FSE (SS-FSE) sequences, respectively. The 3D technique is acquired during normal patient respiration, and provides numerous thin slices with higher signal-to-noise ratio and spatial resolution as a base for multiplanar reformations ad volumetric reconstructions[19]. The 2D technique is acquired more rapidly, during few and short breath-holds for each thick slab, thus reducing the effect of respiratory artefacts on image quality, even if at price of less defined anatomic detail, unless higher magnetic field strength is used (3.0 T)[20].
Regardless of the technical variant, whose use depends on institutional preferences and expertise, MRC has the advantage to noninvasively depict the biliary system without direct contrast injection, contrary to what occurs in direct cholangiography procedures. As a consequence, bile ducts are represented: (1) in their normal state, rather than artificially dilated by contrast pressure; and (2) below and above obstruction sites[21], thus making visible the whole biliary tract, regardless of impaired contrast passage. Alternatively, MRC can be performed using a T1-weighted sequence after iv administration of hepatobiliary contrast agents (gadobenate dimegluime or gadoxetic acid), that are eliminated at a various amount through the biliary tree[22]. T1-weighted approach is useful to complement conventional T2-weighted MRC in demonstrating bile leakage or in evaluating bileo-digestive anastomosis and bile cast syndrome[23].
One might argue that MRC delays diagnosis when interventional procedures like endoscopic retrograde cholangiography (ERC) or percutaneous transhepatic cholangiography (PTC) are finally needed. However, a positive MRC examination provides a road map of the surgically altered biliary anatomy, which is crucial in planning ERC/PTC or surgery. Additionally, the high negative predictive value inherent to MRC is useful to avoid unnecessary invasive procedures in patients with negative findings[23]. Disadvantages of MRI/MRC consist in reduced availability, costs and prolonged scan time, especially when “all-in-one” examinations are required. Image quality may be significantly affected by respiratory or motion artefacts in more compromised patients, as well as in the presence of ascites, especially when using MRC. Finally, it should be kept in mind that, although sensitive in assessing biliary strictures (accuracy of 92.3%)[24], MRC tends to overestimate them, especially when evaluated on maximum intensity projection (MIP)-reconstructions[25]. Stricture assessment should be performed on 2D images or thin source images when using the 3D technique.
In summary, MRI using MRC is the second-line modality of choice after US for evaluating suspicious biliary complications. In selected cases (e.g., less compliant patients), more rapid “quick and dirty” evaluation of the biliary tree can be performed by MDCT or during interventive ERC and PTC.
Direct cholangiography procedures
After OLT, a T-tube can be left within the reconstructed common bile duct for 1 to 3 mo in order to (1) monitor bile quality and quantity; and (2) perform cholangiography examinations. The use of the T-tube has significantly decreased over the last years. However, if there is a T-tube in place, T-tube cholangiography can be easily performed under fluoroscopic or MDCT guidance to demonstrate biliary leakage in the immediate post-operative period (Figure 2). According to Singh et al[6], T-tube cholangiography should be preferred over MRC because the distension of the bile ducts with contrast medium permits better stricture analysis and functional assessment. However, once the tube is removed, alternative imaging methods must be used.
Figure 2.
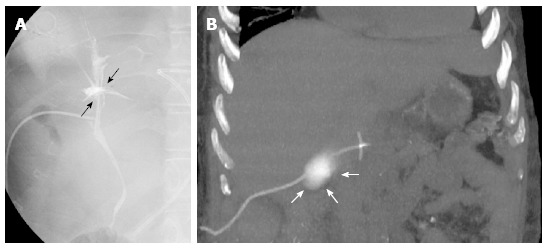
T-tube cholangiography. A: The examination performed few days after liver transplant in a 28-year-old female with primary sclerosing cholangitis shows bile leakage at the anastomotic site (black arrows); B: Fifty-six year-old male recipient. Coronal maximum intensity projection reconstruction from unenhanced multidetector computed tomography scan shows contrast medium extravasation in the right subhepatic space, suggesting T-tube rupture (white arrows).
ERC and PTC provide a panoramic and detail representation of both intra- and extra-hepatic biliary tree. However, these invasive modalities should be avoided for diagnostic purposes in patients with low clinical suspicion, because of the risk of bleeding, infection and other complications[21,26]. ERC and PTC are currently indicated as interventional procedures in the case of biliary obstruction, e.g., by removing stones, performing balloon dilatation or placing stents or biliary drainage[6]. When feasible, preliminary cross-sectional imaging is recommendable in order to provide a road-map for planning interventional procedures.
IMAGING FINDINGS IN THE POST-OPERATIVE PERIOD
The goal of imaging in the post-operative period is to assess early and late OLT complications (Table 1). Preliminary to image analysis, some basic information on surgical technique is needed in order to correctly interpret patients anatomy and imaging findings. Radiologists should be aware of the type of transplantation (e.g., left/right split-liver transplant or living donor liver transplantation), type and number of vascular anastomoses (Figure 3) and type of biliary reconstruction (Figure 4). Regarding the hepatic artery, common sites of anastomosis are the donor junction between hepatic and splenic artery and the recipient branch point of the gastroduodenal and proper hepatic arteries. It is important to know whether alternative surgical techniques have been used in vessel reconstruction, e.g., (1) by interposition of an arterial jump (usually a donor iliac artery) between the donor hepatic artery and the recipient aorta[27]; (2) by insertion of a venous jump (usually, a segment of the donor iliac vein) between the donor portal vein and the recipient mesenteric superior vein[28]; and (3) by directly anastomosing the recipient hepatic artery to the donor portal vein[17]. The knowledge of reconstructed anatomy is essential to correctly identify vascular and biliary structures, and especially anastomoses, because complications often arise from these sites.
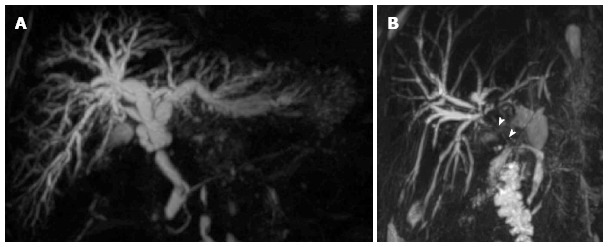
Figure 3.
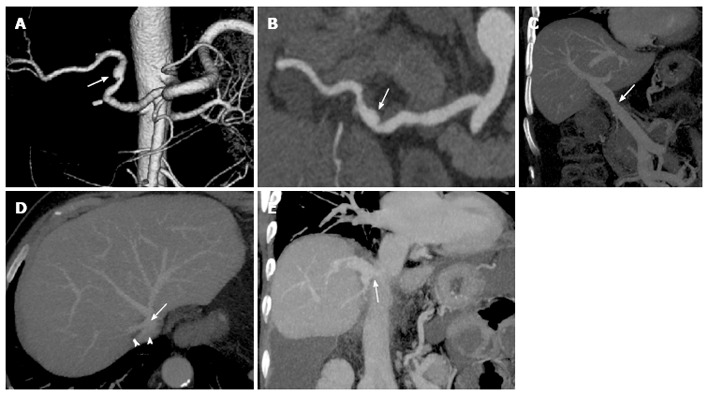
Common vascular anatomy after liver transplant on multidetector computed tomography images. Volume rendering reconstruction (A) and curved-maximum intensity projection (MIP) reconstruction (B) show conventional “fish-mouth” end-to-end anastomosis (arrow) between donor and recipient arterial vessels. Portal vein (C) is usually reconstructed with an end-to-end anastomosis (arrow) between donor and recipient portal veins, as shown in the coronal MIP reconstruction. “Piggyback” reconstruction (D) of the inferior vena cava (IVC), in which an end-to-side anastomosis is performed between the donor IVC (arrow) and the common stump of recipient hepatic veins (arrowheads). The anastomotic site is indicated by the arrow in the coronal MIP reconstruction (E).
Figure 4.
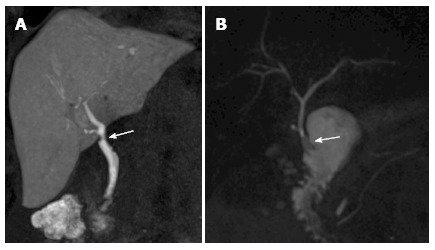
Biliary anatomy after liver transplant on magnetic resonance cholangiography images. A: End-to-end anastomosis (arrow) between the donor common bile duct and the recipient common hepatic duct, as shown in this coronal T1-weighted magnetic resonance cholangiography (MRC) obtained after iv administration of an hepatobiliary contrast agent (gadoxetic acid); B: In the case of technical challenge, re-transplantation or primary sclerosing cholangitis as the cause of the transplant, choledochojejunostomy using a Roux-en-Y anastomosis (arrow) is performed, as shown in this maximum intensity projection reconstruction from a T2-weighted, 3D MRC examination.
Normal findings after OLT
Normal post-OLT imaging findings mirror some “physiologic” effects of the surgical procedure. Not surprisingly, then, it is frequent to observe small amounts of right-sided pleural effusion, ascites or free fluid in the perihepatic region or intersegmental fissure[29]. Additionally, small fluid collections and/or hematomas can be found in the right subhepatic space, as well as along parenchymal resection margin after split liver-OLT and LDLT (Figure 5). Owing to the surgical removal of normal peritoneal reflections, the bared area of the liver is a typical site for fluid an hematoma accumulation[7].
Figure 5.
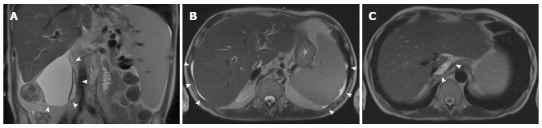
Normal postoperative fluid after liver transplant. Coronal (A) and axial (B, C) T2-weighted single-shot turbo-spin echo magnetic resonance images acquired in a 48 year-old male few days after the intervention show a large fluid collection in the right subhepatic space (arrowheads in A) and a small amount of free fluid in the perihepatic and perisplenic space (arrowheads in B). It is not infrequent to observe a small fluid collection in the retrohepatic space, around the cavo-caval anastomosis (arrowheads in C).
Concerning reconstructed vessels, it is important to emphasize that Doppler US of the normal hepatic artery often shows resistive index (RI) greater than 0.80 in the early postoperative period. Since diastolic velocities increase over few days from OLT, flow spectra rapidly normalize to a rapid systolic upstroke with continuous diastolic flow, an acceleration time less than 80 ms and a resistive index between 0.5 and 0.7[3,30] (Figure 6). Increased RI is associated with older donor age and prolonged ischemia time, although it is not predictive of complications[31]. Postoperative edema has been interpreted as the cause for mild narrowing that can be frequently observed in the early postoperative period along the portal vein course at the porta hepatic[29]. Normal portal flow at Doppler US is continuous, hepatopetal and with mild respiratory variation[3], although it is not unusual to observe high velocity and turbulent flow in the first postoperative days (Figure 6). Of note, normally reconstructed portal vein may show mild narrowing at the anastomotic site, as a consequence of a significant discrepancy in the size of donor and recipient vessels (Figure 3)[29]. Intrahepatic postanastomotic helical-like flow can be observed when the discrepancy in size between donor and recipient portal vein is greater than 50%. In this circumstance, the use of color Doppler is of help in avoiding the misdiagnosis of hepatofugal flow[32]. Sonographic detection of portal venous gas has been described as a transient, additional normal finding in the postoperative period[33].
Figure 6.
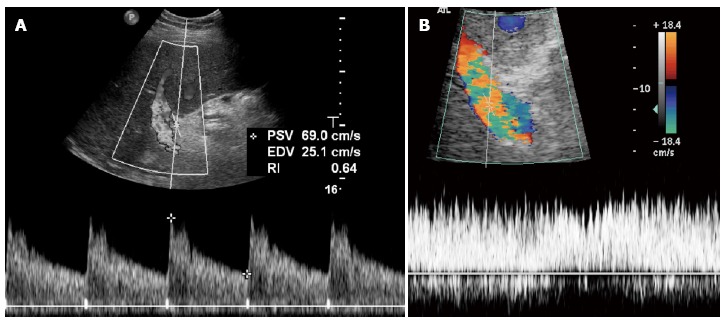
Normal findings doppler ultrasound after the transplant. A: Normal hepatic artery waveform shows a rapid systolic upstroke followed by continuous diastolic flow; B: Portal flow is continuous, hepatopetal and monophasic, with mild respiratory variations that may be masked by increased velocity and flow turbulence, sometimes persisting even in the late post-operative period. PSV: Peak systolic velocity; EDV: End diastolic velocity; RI: Resistance index.
Concerning bile ducts, mild anastomotic narrowing is a frequent cholangiographic and MRC finding that should be interpreted as normal, unless biliary dilatation upstream and symptoms of biliary origin are present (Figure 4)[34]. In most cases, anastomotic narrowing is the effect of surrounding edema, resolving during the first week after OLT[35]. In our experience, anastomotic narrowing is a common finding, especially in the case of donor-to-recipient common bile duct disproportion, in which the recipient common bile duct is larger than the donor hepatic duct[34].
Transplantation implies the interruption of normal lymphatic drainage, causing lymphedema. In the immediate postoperative period, lymphedema manifests with small reactive lymph nodes in the porta hepatis and portocaval space[29] and, more importantly, as periportal edema[36]. Periportal edema is better appreciated on CT and MRI images, presenting as a periportal collar of fluid-attenuating or high signal intensity on T2- or diffusion-weighted images, respectively (Figure 7), and should not be interpreted as a sign of acute rejection[36].
Figure 7.
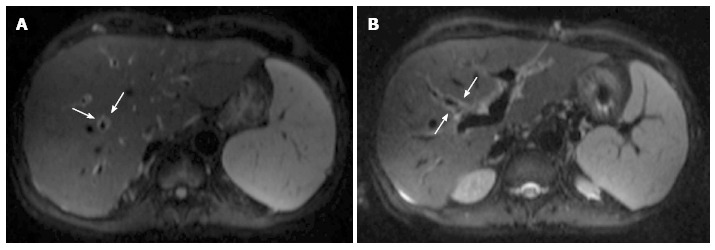
Periportal edema on magnetic resonance diffusion-weighted imaging. Axial b = 500 s/mm2 diffusion-weighted images acquired on a 54-year-old male patient show a thin rim of hyperintense signal surrounding intrahepatic portal branches (arrows in A and B).
The correlation with the clinical and biochemical status of patients is of primary importance in order to avoid misinterpretation of normal post-OLT findings. However, major criterion in the differential diagnosis with complications is the transient nature, since the above findings tend to resolve in a few weeks after the intervention[6].
Vascular complications
Hepatic artery thrombosis: The most common and challenging vascular complication after OLT is represented by hepatic artery thrombosis (HAT). Because of the surgical sacrifice of collateral branches originating from the arterial network surrounding the extrahepatic biliary tree, the hepatic artery remains the sole blood supply to the bile ducts[37]. As a consequence, HAT has a devastating effect on the biliary epithelium, inducing biliary ischemia and necrosis rapidly if untreated. Clinically, HAT is a potential cause of fulminant hepatic necrosis with graft dysfunction. However, most patients present with an insidious subacute scenario of mild alteration of liver function tests, which evolves into a combination of bile leaks with intrahepatic bilomas formation, anastomotic bile duct stricture, perihepatic fluid collections, bile peritonitis and sepsis. Recurrent bacteremia is frequent, being associated with bilomas superinfection, intrahepatic abscesses and nonanastomotic strictures[3,5]. Prompt recognition of HAT is essential, since surgical thrombectomy or thrombolysis are frequently ineffective once patients become symptomatic, thus leading to the need of retransplantation[38].
Doppler US is the first-line modality to evaluate HAT, showing 92% diagnostic accuracy[39]. Diagnosis is made when no Doppler signal is found along the hepatic artery distribution. Of note, a normal hepatic flow detected at the porta hepatis does not exclude HAT at a different location[40]. It is then essential to evaluate carefully the anastomotic site, when possible, and extend Doppler study to right and left branches of the hepatic artery. False-positive results at Doppler US have been related to low cardiac output, arterial spasm or severe parenchymal edema, whereas false-negative results may be the consequence of flow signal from collateral arteries that have been formed in the periportal space during subacute or chronic HAT evolution[3,5]. Collateralization should be taken into account when Doppler US shows extra-or intrahepatic “parvus-tardus” flow waveforms similar to that of significant arterial stenosis, with slowed systolic acceleration time (> 0.08 s) and RI less than 0.5[41,42]. In our experience, collaterals often show dampening of the systolic peak with normal RI. In doubtful cases, CEUS was proven to improve flow recognition[43,44], obviating arteriography in 62.9% of inconclusive Doppler US results. Hom et al[43] showed 100% sensitivity and specificity using a second-generation perfluorocarbon contrast agent[13].
In the case of suspicious or inclusive Doppler US, MDCTA or magnetic resonance angiography (MRA) are required to confirm HAT[3]. Thrombus appears as a filling defect within the hepatic artery or hepatic artery amputation, associated with intrahepatic infarction areas, bilomas or abscesses and signs of biliary obstruction in the case of biliary strictures (Figure 8). In our experience, MDCTA outperforms MRA both in terms of image quality, scan duration and feasibility in more compromised patients, in accordance with previous results[31]. Digital subtraction angiography is usually reserved to interventional procedures when indicated by clinical conditions and cross-sectional imaging findings.
Figure 8.
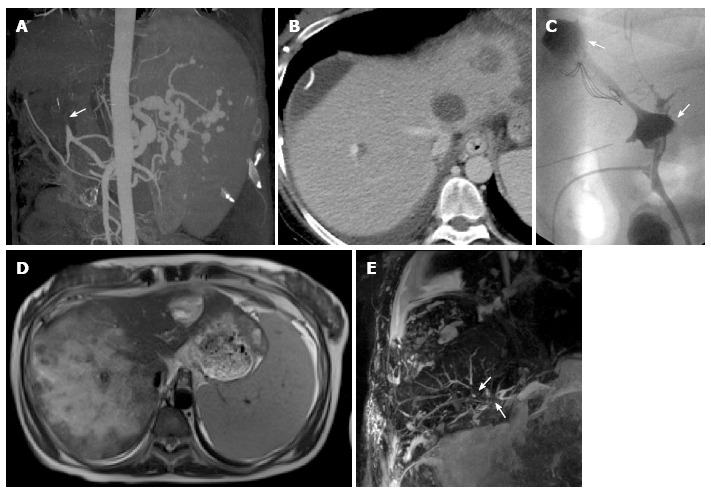
Sequels of hepatic artery thrombosis in a 28-year-old female patient transplanted for primary sclerosing cholangitis. Coronal maximum intensity projection reconstruction (A) from multidetector computed tomography (MDCT) arterial angiographic phase shows abrupt interruption of the hepatic artery at the anastomotic site (arrow). The venous phase from the same MDCT examination (B) shows subhepatic and intrahepatic hypoattenuating fluid collections that were shown to be bilomas at T-tube cholangiography (arrows in C). Magnetic resonance imaging shows rapid evolution to massive liver infarction on axial T2-weighted single-shot turbo-spin-echo imaging (D), with multiple intra- and extrahepatic biliary strictures on magnetic resonance cholangiography (arrows in E). Patient required urgent re-transplantation.
Other hepatic artery complications: Hepatic artery stenosis (HAS) is the second, most frequent complication involving the hepatic artery after OLT. Clinical presentation varies from mild elevation of liver function tests to severe graft dysfunction[45], depending on the degree of the stenosis. Indeed, worsening stenosis may cause HAT and/or liver ischemia, which in turn may result in multiple biliary strictures, sepsis, and graft loss. The major purpose for imaging is to detect HAS early, in order to plan proper treatment, i.e., surgical reconstruction or balloon angioplasty depending on the timing from OLT and the location and length of the stenosis[5,46,47]. Prompt intervention leads to prolonged patients and graft survival (about 65% and 56% at 4 years, respectively)[45]. Doppler US is the modality of choice for screening patients postoperatively. Flow alterations in the presence of HAS include an increase in peak systolic velocity at the site of stenosis (> 200 cm/s), poststenotic turbulent flow and parvus-tardus waveform at intrahepatic samples (acceleration time > 0.08 s and RI < 0.5)[41]. Park et al[48] found that the combination of the parvus-tardus waveform and a peak intrahepatic arterial systolic velocity ≤ 48 cm/s provides an increase in specificity and positive predictive value in the assessment of HAS. MDCTA or MRA with image reformation and three-dimensional reconstruction are used to assess the site, extent and severity of the focal narrowing of the vessel (Figure 9). It has been reported that MRA tend to overestimate the stenosis, with the risk of inducing a relatively high false-positive rate[49].
Figure 9.
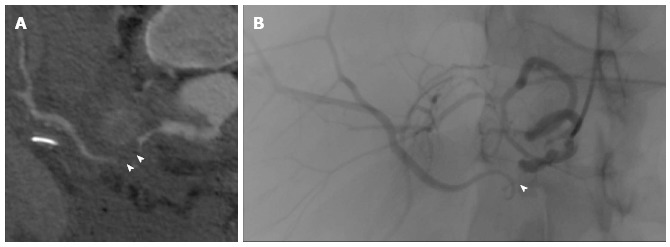
Hepatic artery stenosis. Stenosis is visible (arrowheads) on curved thick-multiplanar reformation from multidetector computed tomography angiography (A) and digital subtraction angiography (B) performed to place a stent.
Further complications involving the hepatic artery include pseudoaneurysm and arterioportal fistula. Pseudoaneurysm is a rare event, occurring either at the anastomosis, typically after angioplasty, or within the liver as an effect of biopsy, biliary intervention or focal infection[7,50]. Although found incidentally in most cases, pseudoaneurysm should be treated promptly with surgery or endovascular approach, since rupture may cause intraperitoneal bleeding, acute shock and hemobilia or gastrointestinal hemorrhage via fistula formation[28]. On imaging, pseudoaneurysm appears as a cystic structure abutting the vessel course, showing turbulent, bidirectional or even slow monophasic flow on Doppler US[28,31]. Every anechoic collection near the hepatic artery should be carefully evaluated with Doppler US to rule out pseudoaneurysm (Figure 10)[6,31]. Lesion confirmation is obtained by MDCTA or MRA, which depict contrast distribution within the lesion similar to that of arterial vessels. Arterioportal fistula is a common sequel of liver biopsies performed during the first week after OLT. However, arterioportal fistula resolves spontaneously in 90% of cases after a week[3]. Fistulas are easily detected on MDCTA, appearing as early enhancement of a portal branch during the arterial phase. The supplied parenchyma often shows a wedge-shaped transient hepatic attenuation difference (THAD)[6].
Figure 10.
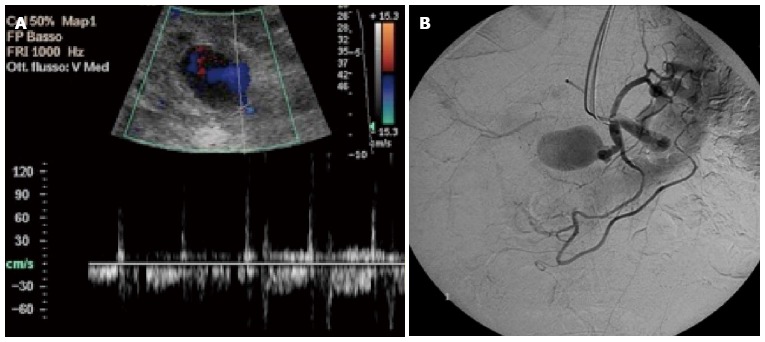
Pseudoaneurysm of the hepatic artery following angioplasty in a 63-year-old male transplanted patient. A: Color Doppler examination shows a cystic formation near the hepatic artery, with a complex flow waveform related to partial thrombosis: high velocity peaks (blood inflow) are followed by diastolic reversal flow (outflow); B: Pseudoaneurysm has been confirmed by digital subtraction angiography by showing contrast filling.
Portal vein thrombosis and stenosis: Portal vein thrombosis (PVT) has been associated to risk factors shown in Table 1, but can occur also in the case of elevated downstream flow resistance (e.g., because of inferior vena cava stricture) or low portal inflow (usually because of a steal through persistent portosystemic collaterals and/or the splenic vein). Clinical manifestations of PVT range from absence of symptoms to variceal hemorrhage, ascites, and graft dysfunction. Symptomatic cases require thrombolysis or surgery (thrombectomy or interposition of a venous graft)[5]. PVT is commonly detected because of absent flow in the main extrahepatic trunk at color Doppler US, with or without definite delineation of an intraluminal echogenic thrombus on B-mode[7]. Partial PVT is less common and with less clinical significance than complete PVT, and is generally found incidentally during patients follow-up. The association between lack of portal trunk detection, hypertrophic hepatic artery and multiple, thin venous vessel at the porta hepatis suggest the evolution of PVT to cavernomatosis[51].
As PVT, portal vein stenosis (PVS) can be clinically silent or manifesting with signs of portal hypertension and graft dysfunction. Stenosis is assessed as hemodynamically significant when a prestenotic/postenotic pressure gradient larger than 5 mmHg is found on portography. Significant stenosis should be treated with balloon angioplasty, stenting or even surgery (including retransplantation in severe cases)[50]. On Doppler US, the diagnosis of PVS requires high clinical suspicion, because of the frequency of caliber discrepancy between donor and recipient veins mimicking a stenosis. Most sensitive criteria for PVS are a peak anastomotic velocity > 125 cm/s or an anastomotic-to-preanastomotic velocity ratio equal or larger than 3:1[52]. Persistance of helical flow, postanastomotic portal vein dilatation and signs of portal hypertension are additional signs of PVS.
MDCTA and MRA confidently confirm the diagnosis of PVT or PVS (Figure 11)[53]. In selected cases, transhepatic or transjugular portography may be required, e.g., to measure pressure gradients[54].
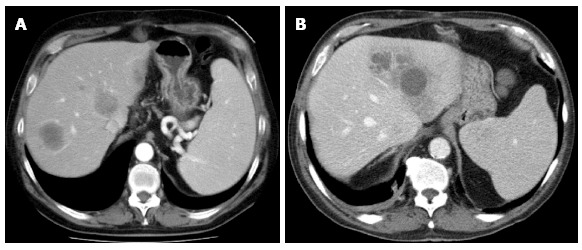
Figure 11.
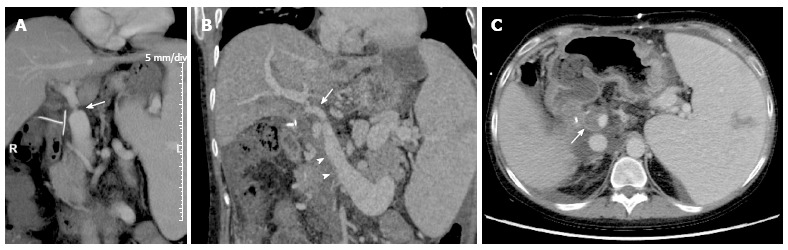
Portal vein complications on multidetector computed tomography images of the same patient of Figure 8. A: Coronal maximum intensity projection (MIP) reconstruction shows a significant portal stenosis at the site of end-to-end anastomosis (arrow). Signs of portal hypertension such as splenomegaly and venous collaterals coexist; B: As shown in the coronal MIP reconstruction, thrombosis occurred after a few days, appearing as a filling defect extending from the superior mesenteric vein (arrowheads) to the portal trunk and portal bifurcation (arrow); C: Axial multidetector computed tomography image shows the partial filling defect in the portal lumen (arrow). R: Right.
Inferior vena cava and hepatic veins complications: Complications of the inferior vena cava (IVC) and hepatic veins include stenosis and thrombosis, that usually occur at the site of surgical anastomosis[55]. Clinical manifestations vary from lower extremity edema to Budd-Chiari syndrome, depending on the degree of impairment of the venous drainage. When the “piggyback” anastomosis is present, a small but clinically significant risk of hemorrhage from cavocaval dehiscence has been reported[56]. Stenosis may be treated with balloon-expandable stents or angioplasty, whereas thrombosis often requires surgery or re-OLT[57,58]. Treatment planning may necessitate hemodynamic pressure measurements above and below the obstruction site.
Direct recognition of a focal narrowing of IVC and/or hepatic veins may be difficult on grayscale US. On Doppler US, the presence of a stenosis is suggested by identifying turbulent flow with color aliasing and increased flow velocity. However, caval stenosis can be reliably assessed when a preanastomotic/postanastomotic velocity gradient of at least 3:1 is found[6]. The detection of monophasic waveform is a sensitive sign for hepatic vein stenosis[5], especially if combined with a pulsatility index less than 0.45[52,59]. However, this sign lacks specificity. Reversal of hepatic venous flow is expected in the case of severe stenosis[3]. However, the detection of biphasic or triphasic hepatic vein waveforms is of help in excluding stenosis[60]. Thrombosis can be detected as echogenic material within the vessel lumen on B-mode and absence of flow on Doppler US[7].
MDCT and MRI with sagittal and coronal reformation provide a panoramic representation of IVC and hepatic veins, and are essential in defining the site and the extent of stenosis and thrombosis (Figure 12), together with secondary findings including hepatic vein distention, hepatomegaly, ascites, and signs of Budd-Chiari syndrome (liver mosaic pattern perfusion) and portal hypertension[17,29].
Figure 12.
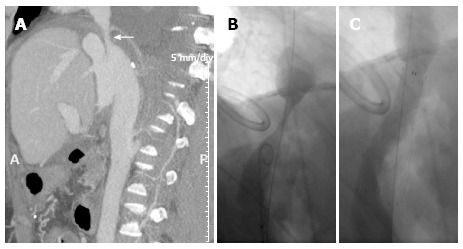
Caval stenosis in a 54-year-old patient. Sagittal maximum intensity projection reconstruction from multidetector computed tomography (A) shows a supranastomotic stenosis of the inferior vena cava (arrow) that is confirmed in the angiogram before (B) and after (C) stenting. A: Anterior; P: Posterior.
Biliary complications
Biliary complications still represent the “Achilles’ heel” of liver transplant, being the second cause of graft dysfunction after rejection[12]. The incidence of biliary complications is higher in LDLT recipients (14%-32%), especially under the form of biliary leakage from the resection margin of the graft[5,26]. Clinical manifestations are often insidious, being similar to that of rejection, HAT and infection, and include mild abdominal symptoms, signs of cholangitis and peritonitis and elevated serum bilirubin and liver enzymes[7,60]. Biliary complications require prompt recognition because they can lead to graft and/or patient loss unless properly treated. Complication following choledochocholedochal anastomosis are usually managed with ERC or PTC, e.g., by performing balloon dilatation, stenting, drainage, or casts/stones clearance. On the contrary, complications following Roux-en-Y choledochojejunostomy often require a surgical approach[6].
Bile leakage: Leakage is the most common early biliary complication[61], arising either from the T-tube insertion site (typically after T-tube removal or dislocation) or biliary anastomosis (as a consequence of technical problems during surgery)[26]. Less commonly, leakage occurs diffusely from necrotic bile ducts (nonanastomotic leak) in patients with HAT (up to 89% of cases) or various disorders (Table 1)[26]. Cut surface represent the most common site of bile leak in LTDT donors and recipients[26]. Small bile leaks tend to resolve spontaneously and can be monitored over time. On the contrary, larger leaks translate into biloma formation, with increased risk of superinfection and sepsis because of post-OLT immunosuppression. Treatment should be targeted both to large bilomas (percuteaneosus aspiration and drainage) and persistent leaks (transhepatic biliary drainage, stenting, surgical repair or biliary reconstruction)[62,63]. When HAT is the primary cause of bile leakage, retransplantation is often required.
US, MDCT and MRI detection of free peritoneal fluid and/or fluid collections (bilomas) on intra-/extrahepatic site or along the cut surface in LDTD patients should raise the suspicion of bile-leakage in the appropriate clinical context (Figure 8). Bilomas are easily detected on US as anechoic collections in the perihepatic and subhepatic space. However, bilomas or intraperitoneal bile are indirect signs of leak, and are virtually indistinguishable from fluid collections and ascites. On the other hand, direct demonstration of the leak can be difficult even when using T2-weighted MRC[26]. This is why final diagnosis is often obtained by direct cholangiography procedures only[61]. Recently, emphasis has been placed on the use of T1-weighted MRC using hepatospecific contrast agents[22]. After iv administration, hepatospecific contrast agents are excreted to a various amount into the biliary tree, thus having the potential to show the site of the leak and passage of contrast medium within bilomas or perihepatic free fluid. Nonetheless, the degree of biliary enhancement can be significantly delayed and/or impaired in patients with decreased liver function. In our institution, we reserve hepatospecific contrast agents to patients with total bilirubin equal or less than 5 mg/dL. Because of low sensitivity (50%) and relatively low specificity (79%), hepatobiliary scintigraphy has not gained routine use in diagnosing bile leak[61].
Biliary obstruction: Main sources of obstruction after OLT include strictures and biliary casts, sludge and stones. Strictures are anastomotic or nonanastomotic in nature. Nonanastomotic strictures involve intrahepatic and/or extrahepatic bile ducts at multiple sites, occurring as a consequence of necrosis with fibrotic reaction after HAT (properly said nonastomotic strictures; NAS), or various causes of bile duct injury in patients without HAT (Ischemic-type biliary lesions; ITBL) (Table 1)[26]. Regardless of etiology, US is useful (1) to detect biliary dilatation as an indirect sign of strictures; or (2) to identify concomitant causes, e.g., HAT. However, MRC is the best noninvasive tool to evaluate the number, site and extent of strictures, both in early and late post-operative period (Figure 13). Strictures appear as a tight, smoothly marginated focal zone of decreased signal intensity along bile ducts[25,26]. Biliary dilatation upstream is common, although often delayed and less pronounced than expected based on the degree of the stricture, possibly in relation with graft-related factors reducing bile ducts compliance[64]. NAS and ITBL typically involve the hepatic confluence, showing thin or absent luminal signal, often extended to the proximal hepatic duct[26]. Of note, it is not infrequent to observe mild biliary dilatation without strictures in OLT recipients. Nonobstructive dilatation has been attributed to an increase in basal contraction of sphincter of Oddi after surgical denervation, and is asymptomatic in most patients[26].
Figure 13.
Biliary strictures on coronal maximum intensity projection reconstructions from volumetric magnetic resonance cholangiography. A: Anastomotic stricture at the middle third of the extrahepatic bile duct in a 53-year-old female patient, with biliary dilation upstream; B: Anastomotic stricture extended to the proximal hepatic duct (arrowheads) in a 62 year-old patient with patent hepatic artery.
Biliary casts and sludge usually complicate anastomotic or nonanastomotic strictures, occurring both at intrahepatic or extrahepatic bile ducts as the consequence of bile stasis[26]. Superimposition of additional strictures because of progressive fibrotic changes may result in a dissemination of strictures associated with interposed dilated tracts with casts (biliary cast syndrome)[3]. On MRC, biliary casts, sludge or stones appear as anintense filling defects surrounded by a thin film of hyperintense bile. Stones can be differentiated from casts and sludge because they tend to show more round, regular and smooth margins[6,26].
Primary hepatic complications
An important group of post-OLT disorders might be classified as “primary hepatic complications” (PHC). PHC manifest with graft dysfunction and can be caused by the following factors: immunological (acute and chronic rejection, chronic hepatitis, de novo or recurrent autoimmune disease), viral (recurrent HBV and/or HCV hepatitis, de novo cytomegalovirus, HBV, HCV, HBV and other viruses-related hepatitis), toxic (usually drugs-related) and ischemic (late effects of ischemic and reperfusion injury, manifesting within few days from OLT)[65,66]. Among them, major sources of graft loss are represented by: (1) chronic ductopenic rejection, that typically affects the graft between 6 wk to 6 mo after transplantation and occurs in up to 17% of patients[3]; and (2) recurrent disease, exemplified at best by HCV recurrence. PHC can be a co-manifestation of vascular or biliary complications, e.g., multiple biliary strictures in recurrent sclerosing cholangitis.
Imaging findings lack sensitivity and specificity in assessing PHC and the effects of therapies[3,5,6]. For example, previous attempts to correlate loss of phasicity of the hepatic vein at Doppler US with acute cellular rejection showed conflicting results[5,67]. Therefore, imaging findings overlap with those occurring in normal grafts[5]. Recently, Sandrasegaran et al[68] showed that MRI quantitative evaluation of the graft with DWI has the potential to assess the presence vs absence of PHC, but further investigations are needed to consolidate these promising results. Histological examination of biopsy specimens is mandatory for diagnosing and monitoring primary parenchymal complications[69]. Regarding PHC, the main role for imaging is to exclude those vascular and biliary complications mimicking rejection and other parenchymal disorders. We’ll discussed below future perspectives in imaging chronic parenchymal disorders, using HCV recurrence as the most exemplificative scenario.
Hepatic and extrahepatic collections, hematoma and abscess
After OLT, seromas and hematomas are a frequent finding near areas of vascular anastomosis (hepatic hilum, IVC) or the perihepatic/subhepatic space[6]. Sonographic appearance is nonspecific, because the fluid content can be equally uniformly anechoic, loculated or inhomogeneously echogenic due to fibrin septa or separation of blood components[7,12]. Bilomas have similar location and appearance on US. MDCT can be useful: (1) in assessing the hematic content, since acute hematoma is hyperattenuating compared to simple fluid collections, whereas older hematomas can show hematocrit level[3]; and (2) in excluding active bleeding. Best characterization is provided by MRI, which shows typical signal intensity patterns for fluid or hemorrhagic content[29]. However, MDCT and MRI are rarely needed, since most collections are self-limiting and without clinical significance, unless they enlarge or become superinfected.
Abscesses can occur as the result of: (1) bacteremia; (2) superinfection of a seroma, hematoma or biloma; and (3) superinfection of liver infarcted area, usually in patients with HAT or HAS and biliary necrosis (Figure 8). Features of abscess can be typical on MDCT and MRI, with focal hypovascular lesions surrounded by a rim of contrast enhancement (Figure 14) and sometimes intralesional gas. On the other hand, imaging findings can be nonspecific, making percutaneous drainage indispensable for diagnosis and treatment[3].
Figure 14.
Multiple liver abscesses arising from infected bilomas in a 48-year-old recipient with hepatic artery stenosis.
In the case of seromas, bilomas, hematomas and abscesses, the main role for imaging is to establish the site and the amount of the collection in order to plan or guide interventional diagnostic or therapeutic procedures[12].
Malignancy: HCC and de novo tumors
OLT is a curative option for HCC. However, the likelihood of HCC recurrence vary according to selection criteria for OLT: rates of recurrence at 4 years are 10% for patients with HCC within the Milan criteria, and up to 60% for patients with HCC outside Milan criteria[70]. When stringent selection criteria are applied, the recurrence rate is not affected by potential tumor underestimation at initial imaging examinations[71], and the survival rate approximates that of transplanted patients without HCC[5]. The risk for recurrence depends on tumor size, number of lesions, differentiation and the presence of vascular invasion. Most studies report a median time for recurrence of 12.3-19.2 mo from OLT[72]. Nowadays, there is no consensus on how to perform imaging surveillance in patients undergoing OLT for known HCC or in patients with incidental HCC found in the explanted liver. Recent guidelines provided by the American Association for the Study of Liver Disease and the American Society of Transplantation suggest to perform abdominal and chest MDCT every 6 mo for 3 years after OLT. In the case of recurrent allograft cirrhosis in patients without previous HCC, abdominal imaging every 6 to 12 mo is recommended[69], though de novo HCC seems to be extremely rare in this subset of patients[72]. A few imaging studies investigated whether recurrent HCC shows specific image patterns compared to native HCC. Based on locations, rates of recurrence were reported to be 1%-23% in the allograft only, 38.5%-53% in extrahepatic sites, and 31%-38.5% in both allograft and extrahepatic sites[72]. These results have been recently confirmed by Lee et al[72], who showed that the most prominent volume of recurrent tumor burden occurs near the transplanted liver (ICV, hepatorenal space and the surgical scar along anterior abdominal wall), suggesting that surgical manipulation occurring during the OLT may lead to intraoperative spilling of tumor cells capable to survive years before growing into detectable nodules. These results are of interest both in making radiologists aware of studying specific locations where recurrence is commoner (Figure 15), and in suggesting that the most frequent way of HCC recurrence is intra abdominal seeding rather than hematogenous or lymphatic spread. Concerning metastatic disease, it most frequently involves the lungs, lymph nodes, adrenal glands and bone[3].
Figure 15.

Recurrence of hepatocarcinoma in a 65-year-old human B virus infected male transplanted patient. On the subtracted arterial phase magnetic resonance imaging (A) two mildly hypervascular lesions are visible in the extrahepatic region, between the stomach and left diaphragm (arrows). Lesions, that were histologically confirmed to be hepatocellular carcinoma, show absence of contrast wash-out on the venous phase (arrows in B) and hepatocellular contrast uptake in the hepatospecific phase (arrows in C). A regenerative nodule with intense contrast uptake is visible in the hepatospecific phase only (arrowhead in C).
Because of co-existing risk factors (including smoking, EBV infection and inflammatory bowel disease in patients with primitive sclerosing cholangitis) and the immunosuppressive therapy, transplanted patients are at higher risk to develop de novo malignancies, with a cumulative incidence increasing with time from OLT (up to 20% at 10 years)[69]. Most frequent tumors arising in the post-OLT period are skin cancers and post-transplant lymphoproliferative disease (PTLD). Although globally uncommon (incidence of 0.9%-2.9%), PTLD is a serious complication[69], typically occurring within the first year from OLT. As detailed elsewhere[73], PTLD is a term encompassing a spectrum of hematologic conditions ranging from abnormal polyclonal lymphoid hyperplasia to overt monoclonal lymphoma. The majority of PTLDs consist in B-lymphocyte proliferations activated by EBV infection; such a proliferation lacks self-limitation due to immunosuppression. PTLD can manifest: (1) with a nodal and/or extranodal form involving almost all organs; and (2) as localized or disseminated disease. In liver recipients, PTLD is more frequently extranodal in nature, with intra-abdominal and extrahepatic disease as the most frequent manifestation. Extrahepatic PTLD presents as an ill-defined soft tissue mass, typically involving the hepatic hilum and determining encasement or narrowing of the hepatic artery, portal vein and common bile duct. The lesion usually is hypoechoic on US, hypoattenuating on CT and with T1 hypointensity and mildly T2 hypointensity on MRI[73]. Contrast enhancement may be heterogeneous or occur at the periphery of the lesion[74]. Liver involvement presents with well defined, hypovascular focal lesions or, less frequently, with an infiltrative pattern showing similar US, MDCT and MRI features than the extrahepatic masses. When small or large bowel are involved, wall thickening, eccentric mass, luminal ulceration and perivisceral fat stranding are common findings[73]. Imaging plays a pivotal role in the early diagnosis of the lesions, assessment of the disease extent, guiding biopsy and monitoring the treatment response[73]. MDCT is the preferred modality due to ready availability and panoramicity. CT-positron emission tomography (CT-PET) also has an important role, being used in evaluating the response to therapy, especially when there is need to differentiate residual tumor from fibrosis or necrosis[75].
FUTURE PERSPECTIVES IN OLT IMAGING: MRI IN HCV-INFECTED PATIENTS
Clinical background
HCV recurrence after OLT is a challenging scenario. In the western world, HCV is the most common indication for OLT when considering both HCV-related cirrhosis and HCV-related HCC[76]. Of note, the overall graft and patient survival rates are 23% lower in HCV-infected OLT recipients compared to non-HCV infected ones[77]. This is linked to the invariable recurrence of infection occurring within the first year from transplantation, as detectable with histology and HCV RNA levels[68]. Recurrent disease translates into chronic liver disease, with chronic active hepatitis occurring in up to 63% of patients within 3 years from the diagnosis of re-infection. Final evolution is represented by graft cirrhosis, that occurs in a median time of 8-10 years, although up to 30% of patients (so called “rapid progressors”) develop recurrent cirrhosis more rapidly (3-5 years)[68]. Of note: (1) cirrhosis evolves faster in HCV-infected patients who received OLT compared to not-transplanted ones; and (2) retransplantation in HCV-infected patients shows worse prognosis than in the non-HCV group[78].
On this basis, re-infected OLT recipients are addressed to antiviral therapy with the goal of sustained viral clearance, thus preventing liver-related complications and allograft loss. There is no consensus about the timing of antiviral therapy, i.e., whether to start antiviral drugs before or after histological criteria for treatment are fulfilled[79]. However, serial liver biopsies remain the standard of reference in monitoring the effects of infection and/or therapy by grading necroinflammation and staging fibrosis associated with chronic liver disease[78]. Currently, antiviral therapy is indicated as soon as early fibrosis is detected (e.g., ≥ 2 over a scale of 4) or in the presence of moderate-to-severe necroinflammatory activity[68,78,80]. In this setting, special emphasis has been attributed to the serial assessment of fibrosis, since sustained virological eradication is associated with fibrosis stabilization or regression[81].
Current imaging of liver fibrosis in OLT patients
Liver biopsy shows major drawbacks, including morbidity, sampling errors and inter- and intra-observer variability in histopathologic interpretation. Over the last years, different serum marker panels, indices composed of routine laboratory tests or imaging techniques have been intensively investigated as instruments to quantify fibrosis noninvasively. The ideal noninvasive tool should be readily available, reproducible and reliable in assessing the whole spectrum of fibrosis manifestations. Of note, conventional imaging has an established role in evaluating the cirrhotic liver, with US, MDCT and MRI showing typical and well-known features both in native and transplanted liver[82], including alterations of parenchymal homogeneity and surface, splenomegaly, increase of portal diameter and so on. On the contrary, there is no current indication to assess fibrosis with conventional imaging modalities, because of nonspecific findings. In the setting of transplanted patients with HCV recurrence, imaging is thus demanded to provide additional quantitative information compared to conventional studies, with the goal of replacing biopsy in terms of: (1) early recognition of recipients with progression to advanced fibrosis and/or cirrhosis; (2) early recognition of mild fibrosis; and (3) monitoring the effects of therapy[83].
Transient elastography (TE), a sonography-based technique providing measures of liver elasticity in response to mechanical excitation, is the best studied imaging modality in this setting[84-89]. TE (namely, FibroScan®) gained popularity in European countries because of proven capability to noninvasively predict liver fibrosis in a variety of clinical conditions, including recurrence of HCV in transplanted patients[90]. In a recent metanalysis by Adebajo et al[91], TE showed pooled sensitivity and specificity of 83% in detecting significant stage of fibrosis (defined as stage ≥ 2). Current data suggest that, in HCV re-infected transplant recipients, state-of-the-art TE is a useful complement to biopsy in order to exclude cirrhosis in patients (1) not candidates for treatment, thus avoiding unnecessary biopsies; or (2) who have histological evidence of advanced fibrosis. The absence of biological effects makes TE repeatable and safe[83]. On the other hand, TE shows a limited role as an alternative to biopsy for early stages of fibrosis[78]. Although TE is user-friendly and reproducible, quantitative cut-off values (1) can be co-influenced by hepatitis-associated necroinflammatory activity or extrahepatic cholestasis; and (2) do not represent absolute reference values, because of equipment-related variability[83,85]. Furthermore, TE results may be affected by limited operators experience, presence of ascites and narrow intercostal window[82].
Nowadays, alternative elastographic techniques are under evaluation, including (1) acoustic radiation force impulse (ARFI) approach, which uses short-duration, high intensity acoustic pulses to mechanically generate shear waves propagating through the liver; or (2) shear wave elastography (SWE), that allows a 2D quantitative elasticity map of the liver in a single US sequence by using an ultrafast imaging approach. In a recent study by Crespo et al[85], the estimation of shear waves velocity with ARFI was shown: (1) to provide higher technical successful rate than TE; and (2) to provide a diagnosis of significant fibrosis (F ≥ 2 according to the Scheuer classification) as accurate as TE both in transplanted patients [areas under the curve (AUC) at receiving operating characteristics analysis of 0.867 and 0.902, respectively] and non-transplanted patients (AUCs of 0.897 and 0.890, respectively). A few data exist on SWE of liver-tranpslanted patients. According to Yoon et al[92], this technique has the potential to realiably detect rejection or recurrent hepatitis early after OLT (4 wk), both in HCV- and non HCV-patients.
In summary, sonography-based techniques evaluating liver elasticity represent promising tools in the setting of post-OLT recurrence of HCV, but technical refinements and larger validation studies are still needed before replacing biopsy as the standard of reference.
MRI of liver fibrosis in OLT patients
One might suppose that MRI has no potential role in the serial assessment of liver fibrosis, being expensive, not readily available, time-consuming and contraindicated in patients with metallic devices in the body. A major, additional concern is related to the risk of systemic nephrogenic fibrosis (SNF) in patients with severe renal impairment (GFR less than 30 mL/min) when iv administration of gadolinium chelates is indicated[18]. Nonetheless, the advantage underlying MRI is the capability of “all-in-one” examinations[93] in which both conventional imaging and quantitative techniques for fibrosis assessment can be acquired within a unique imaging session. MRI also provides panoramic representation of the liver, which in theory translates into the possibility of performing (1) multiple quantitative measurements at different liver sites; or (2) measurements over large regions of parenchyma, thus reducing the risk of error sampling inherent to the inhomogeneity of fibrosis distribution. As detailed elsewhere[82], different MRI techniques have been investigated in order to assess fibrosis in HCV patients, including DWI, magnetic resonance elastography (MRE), dynamic contrast enhanced (DCE) perfusion imaging and MRS. Nonetheless, there is still a paucity of studies using quantitative MRI techniques in the subset of recurrent HCV transplanted patients.
DWI expresses brownian motion of water molecules within tissues under the form of the apparent diffusion coefficient (ADC). ADC is a quantitative index which is expected to reduce because of the deposition of collagen fibers, glycosaminoglycans and proteoglycans occurring in fibrosis and cirrhosis[82]. Several studies confirmed that the ADC is significantly lower in cirrhotic livers compared to non-cirrhotic livers[94-97]. However, conflicting results have been reported, in non-transplanted subjects, concerning the capability of detecting intermediate stages of fibrosis with DWI[82,96,98-100]. According to one recent study[94], although liver ADC shows a trend to progressive decrease as fibrosis stage increases, ADC values are not useful for differentiating low-stage from high-stage fibrosis in patients with chronic liver disease of different aetiologies. Furthermore, experiences on animal models[101] or humans[102] found that, when correcting DWI estimates for additional phenomena occurring in vivo, e.g., tissue microperfusion, difference in ADC between normal and fibrotic livers become not significant, even in the “extreme” case of cirrhosis. To our knowledge, only one study[68] tested DWI in assessing hepatic parenchymal disorders after OLT. Results on forty-one patients were in line with known limitations of DWI, since analysis showed no significant correlation between ADC and histological evidence of viral hepatitis, fibrosis or necroinflammation, as well as fat deposition and acute and chronic rejection. Nevertheless, ADC was found to be significantly lowered in patients with histological abnormalities compared to those with negative biopsy results, suggesting that DWI might be useful at least to exclude the presence of primary parenchymal complications. Of note, an ADC cut-off of 0.98 × 10-3 mm2/s was found as acceptably sensitive (78%) in assessing the presence of necroinflammatory score ≥ 3 and fibrosis stage ≥ 2 in a subset of 27 HCV patients, even if at price of low specificity (58%). Disappointing results of DWI are probably related to the current lack of technical standard across different centers and studies, as witnessed by the absence of absolute reference values for normal and pathologic ADCs. One might expected better results by applying the same MRI sequence, b-values (factors influencing the strength of diffusion-weightening) and other acquisition parameters, whose optimization should help in minimizing intra- and inter-scanner variability affecting DWI in its present form. DWI is attractive tool, since it can be performed in the context of routine MRI examinations with minimal increase in the scan time. Promising results on animal models[103] and humans[104] have been obtained by the application of diffusion tensor imaging (DTI), a technical variant of DWI in which water molecules motion is assessed over multiple, numerous spatial directions. However, liver DTI is still technically challenging for abdominal applications. Preliminary experiences should be consolidated by larger studies.
MRE uses a driver system placed near patients’ right chest wall, which generates acoustic shear waves passing through the liver during the acquisition of an MRI phase-contrast sequence[105]. A dedicated software then elaborates waves propagation patterns, providing quantitative stiffness values throughout the entire liver with high technical successful rate[106], good reproducibility[107], and no influence of co-existing steatosis[105]. In non-transplanted patients, MRE showed promising results by assessing a significant correlation between liver stiffness and fibrosis increase, with better results than aspartate aminotransferase-to-platelet ratio[107]. Differently from TE, MRE has been shown to reliably differentiate between intermediate stages of fibrosis, i.e., METAVIR scores F0-F1 versus F2-F3, F2-F3 vs F4, and F0-F1 vs F4[106-108]. Using a shear stiffness cut-off value of 2.93 kPa, Yin et al[109] found sensitivity and specificity for detecting all grades of liver fibrosis of 98% and 99%, respectively. As far as we know, a few papers investigated the role for MRE in transplanted patients. In a recent preliminary study by Lee et al[110], the authors compared the accuracy of MRE and several biomarkers (aminotransferase-to-platelet ratio, aspartate aminotransferase-to-alanine aminotransferase ratio, and FIBROSpect II) in diagnosing the presence of fibrosis (METAVIR stage ≥ 1) in 32 OLT recipients with HCV recurrence. Using a ≥ 3.81 kPa cut-off, MRE performed better than biomarkers, showing accuracy of 81.3%. By combining MRE with FIBROSpect II, the overall accuracy increased to 92.9%, thus avoiding unnecessary biopsies in 22 patients, only 2 of which had fibrosis stage ≥ 1. Notably, MRE was used as the guidance to perform liver biopsy in this study, with the rationale of offering direct correlation between MRE estimates and tissue sampling. Perumpail et al[111] showed high success rate of MRI-guided biopsy in liver recipients, thus emphasizing the capability of providing tissue sampling from regions of highest liver stiffness as a method to potentially minimize sampling errors in assessing liver fibrosis. Despite promising results, some drawbacks currently affects MRE[110]. First, there is a need to determine whether confounding factors have the potential to increase allograft stiffness in addition to fibrosis, including edema or changes in regional blood flow. Second, MRE equipment still needs standardization among different institutions, as witnessed by the lack of definite reference values for different stages of fibrosis.
CONCLUSION
Imaging has a pivotal role in assessing vascular and biliary complications after OLT. Doppler US, MDCTA and MRC are the most useful imaging tools in order to provide rapid and reliable diagnoses, as well as a road-map to minimize the morbidity associated with interventional or surgical procedures. Technique optimization, knowledge of post-surgical anatomy and knowledge of clinical characteristics of main complications are essential in order to interpret images and address patients to proper management. Less defined is the role for imaging in those complications primarily arising from liver parenchyma, including rejection and other forms of graft dysfunction requiring biopsy for final diagnosis. Recurrence of HCV is a challenging clinical scenario emphasizing the need to go beyond conventional imaging with functional, noninvasive modalities of graft assessment like TE, DWI and MRE. Intensive research and technical development are still needed to achieve the ideal goal of imaging patients with “all-in-one” examinations capable to answer different inquires efficiently.
ACKNOWLEDGMENTS
The authors thank Dr. Paolo Divis for having performed final editing of images.
Footnotes
P- Reviewers: Christoph FD, Nakajima H, Neuberger J, Tam PKH S- Editor: Ma YJ L- Editor: A E- Editor: Wu HL
References
- 1.Varma V, Mehta N, Kumaran V, Nundy S. Indications and contraindications for liver transplantation. Int J Hepatol. 2011;2011:121862. doi: 10.4061/2011/121862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tanwar S, Khan SA, Grover VP, Gwilt C, Smith B, Brown A. Liver transplantation for hepatocellular carcinoma. World J Gastroenterol. 2009;15:5511–5516. doi: 10.3748/wjg.15.5511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Itri JN, Heller MT, Tublin ME. Hepatic transplantation: postoperative complications. Abdom Imaging. 2013;38:1300–1333. doi: 10.1007/s00261-013-0002-z. [DOI] [PubMed] [Google Scholar]
- 4.Boraschi P, Donati F. Complications of orthotopic liver transplantation: imaging findings. Abdom Imaging. 2004;29:189–202. doi: 10.1007/s00261-003-0109-8. [DOI] [PubMed] [Google Scholar]
- 5.García-Criado A, Gilabert R, Bargalló X, Brú C. Radiology in liver transplantation. Semin Ultrasound CT MR. 2002;23:114–129. doi: 10.1016/s0887-2171(02)90032-6. [DOI] [PubMed] [Google Scholar]
- 6.Singh AK, Nachiappan AC, Verma HA, Uppot RN, Blake MA, Saini S, Boland GW. Postoperative imaging in liver transplantation: what radiologists should know. Radiographics. 2010;30:339–351. doi: 10.1148/rg.302095124. [DOI] [PubMed] [Google Scholar]
- 7.Crossin JD, Muradali D, Wilson SR. US of liver transplants: normal and abnormal. Radiographics. 2003;23:1093–1114. doi: 10.1148/rg.235035031. [DOI] [PubMed] [Google Scholar]
- 8.Sanyal R, Lall CG, Lamba R, Verma S, Shah SN, Tirkes T, Berry WA, Sandrasegaran K. Orthotopic liver transplantation: reversible Doppler US findings in the immediate postoperative period. Radiographics. 2012;32:199–211. doi: 10.1148/rg.321115006. [DOI] [PubMed] [Google Scholar]
- 9.de Jong KP, Bekker J, van Laarhoven S, Ploem S, van Rheenen PF, Albers MJ, van der Hilst CS, Groen H. Implantable continuous Doppler monitoring device for detection of hepatic artery thrombosis after liver transplantation. Transplantation. 2012;94:958–964. doi: 10.1097/TP.0b013e318269e6ad. [DOI] [PubMed] [Google Scholar]
- 10.Rennert J, Dornia C, Georgieva M, Roehrl S, Fellner C, Schleder S, Stroszczynski C, Jung EM. Identification of early complications following liver transplantation using contrast enhanced ultrasound (CEUS). First results. J Gastrointestin Liver Dis. 2012;21:407–412. [PubMed] [Google Scholar]
- 11.Rossi S, Rosa L, Ravetta V, Cascina A, Quaretti P, Azzaretti A, Scagnelli P, Tinelli C, Dionigi P, Calliada F. Contrast-enhanced versus conventional and color Doppler sonography for the detection of thrombosis of the portal and hepatic venous systems. AJR Am J Roentgenol. 2006;186:763–773. doi: 10.2214/AJR.04.1218. [DOI] [PubMed] [Google Scholar]
- 12.Caiado AH, Blasbalg R, Marcelino AS, da Cunha Pinho M, Chammas MC, da Costa Leite C, Cerri GG, de Oliveira AC, Bacchella T, Machado MC. Complications of liver transplantation: multimodality imaging approach. Radiographics. 2007;27:1401–1417. doi: 10.1148/rg.275065129. [DOI] [PubMed] [Google Scholar]
- 13.Berry JD, Sidhu PS. Microbubble contrast-enhanced ultrasound in liver transplantation. Eur Radiol. 2004;14 Suppl 8:96–103. [PubMed] [Google Scholar]
- 14.Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsøe CP, Piscaglia F, Wilson SR, Barr RG, Chammas MC, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver--update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultraschall Med. 2013;34:11–29. doi: 10.1055/s-0032-1325499. [DOI] [PubMed] [Google Scholar]
- 15.Chopra SS, Eisele R, Stelter L, Seehofer D, Grieser C, Warnick P, Denecke T. Contrast enhanced ultrasound cholangiography via T-tube following liver transplantation. Ann Transplant. 2012;17:108–112. doi: 10.12659/aot.883700. [DOI] [PubMed] [Google Scholar]
- 16.Bismpa K, Zlika S, Fouzas I, Imvrios G, Papanikolaou V, Petridis A. Imaging of complications of liver transplantation: multidetector computed tomography findings. Transplant Proc. 2012;44:2751–2753. doi: 10.1016/j.transproceed.2012.09.015. [DOI] [PubMed] [Google Scholar]
- 17.Quiroga S, Sebastià MC, Margarit C, Castells L, Boyé R, Alvarez-Castells A. Complications of orthotopic liver transplantation: spectrum of findings with helical CT. Radiographics. 2001;21:1085–1102. doi: 10.1148/radiographics.21.5.g01se061085. [DOI] [PubMed] [Google Scholar]
- 18.Chow DS, Bahrami S, Raman SS, Rotchel S, Sayre JW, Busuttil RW, Lu DS. Risk of nephrogenic systemic fibrosis in liver transplantation patients. AJR Am J Roentgenol. 2011;197:658–662. doi: 10.2214/AJR.10.5976. [DOI] [PubMed] [Google Scholar]
- 19.Hyodo T, Kumano S, Kushihata F, Okada M, Hirata M, Tsuda T, Takada Y, Mochizuki T, Murakami T. CT and MR cholangiography: advantages and pitfalls in perioperative evaluation of biliary tree. Br J Radiol. 2012;85:887–896. doi: 10.1259/bjr/21209407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim SY, Byun JH, Lee SS, Park SH, Jang YJ, Lee MG. Biliary tract depiction in living potential liver donors: intraindividual comparison of MR cholangiography at 3.0 and 1.5 T. Radiology. 2010;254:469–478. doi: 10.1148/radiol.09090003. [DOI] [PubMed] [Google Scholar]
- 21.Fulcher AS, Turner MA. Orthotopic liver transplantation: evaluation with MR cholangiography. Radiology. 1999;211:715–722. doi: 10.1148/radiology.211.3.r99jn17715. [DOI] [PubMed] [Google Scholar]
- 22.Salvolini L, Urbinati C, Valeri G, Ferrara C, Giovagnoni A. Contrast-enhanced MR cholangiography (MRCP) with GD-EOB-DTPA in evaluating biliary complications after surgery. Radiol Med. 2012;117:354–368. doi: 10.1007/s11547-011-0731-4. [DOI] [PubMed] [Google Scholar]
- 23.Boraschi P, Donati F. Biliary-enteric anastomoses: spectrum of findings on Gd-EOB-DTPA-enhanced MR cholangiography. Abdom Imaging. 2013;38:1351–1359. doi: 10.1007/s00261-013-0007-7. [DOI] [PubMed] [Google Scholar]
- 24.Cereser L, Girometti R, Como G, Molinari C, Toniutto P, Bitetto D, Zuiani C, Bazzocchi M. Impact of magnetic resonance cholangiography in managing liver-transplanted patients: preliminary results of a clinical decision-making study. Radiol Med. 2011;116:1250–1266. doi: 10.1007/s11547-011-0707-4. [DOI] [PubMed] [Google Scholar]
- 25.Laghi A, Pavone P, Catalano C, Rossi M, Panebianco V, Alfani D, Passariello R. MR cholangiography of late biliary complications after liver transplantation. AJR Am J Roentgenol. 1999;172:1541–1546. doi: 10.2214/ajr.172.6.10350286. [DOI] [PubMed] [Google Scholar]
- 26.Girometti R, Cereser L, Como G, Zuiani C, Bazzocchi M. Biliary complications after orthotopic liver transplantation: MRCP findings. Abdom Imaging. 2008;33:542–554. doi: 10.1007/s00261-007-9316-z. [DOI] [PubMed] [Google Scholar]
- 27.Ishigami K, Zhang Y, Rayhill S, Katz D, Stolpen A. Does variant hepatic artery anatomy in a liver transplant recipient increase the risk of hepatic artery complications after transplantation? AJR Am J Roentgenol. 2004;183:1577–1584. doi: 10.2214/ajr.183.6.01831577. [DOI] [PubMed] [Google Scholar]
- 28.Nghiem HV. Imaging of hepatic transplantation. Radiol Clin North Am. 1998;36:429–443. doi: 10.1016/s0033-8389(05)70033-6. [DOI] [PubMed] [Google Scholar]
- 29.Ito K, Siegelman ES, Stolpen AH, Mitchell DG. MR imaging of complications after liver transplantation. AJR Am J Roentgenol. 2000;175:1145–1149. doi: 10.2214/ajr.175.4.1751145. [DOI] [PubMed] [Google Scholar]
- 30.García-Criado A, Gilabert R, Salmerón JM, Nicolau C, Vilana R, Bianchi L, Buñesch L, García-Valdecasas JC, Rimola A, Brú C. Significance of and contributing factors for a high resistive index on Doppler sonography of the hepatic artery immediately after surgery: prognostic implications for liver transplant recipients. AJR Am J Roentgenol. 2003;181:831–838. doi: 10.2214/ajr.181.3.1810831. [DOI] [PubMed] [Google Scholar]
- 31.Bhargava P, Vaidya S, Dick AA, Dighe M. Imaging of orthotopic liver transplantation: review. AJR Am J Roentgenol. 2011;196:WS15–WS25 Quiz WS15-WS25. doi: 10.2214/AJR.09.7221. [DOI] [PubMed] [Google Scholar]
- 32.Rosenthal SJ, Harrison LA, Baxter KG, Wetzel LH, Cox GG, Batnitzky S. Doppler US of helical flow in the portal vein. Radiographics. 1995;15:1103–1111. doi: 10.1148/radiographics.15.5.7501853. [DOI] [PubMed] [Google Scholar]
- 33.Chezmar JL, Nelson RC, Bernardino ME. Portal venous gas after hepatic transplantation: sonographic detection and clinical significance. AJR Am J Roentgenol. 1989;153:1203–1205. doi: 10.2214/ajr.153.6.1203. [DOI] [PubMed] [Google Scholar]
- 34.Campbell WL, Foster RG, Miller WJ, Lecky JW, Zajko AB, Lee KY. Changes in extrahepatic bile duct caliber in liver transplant recipients without evidence of biliary obstruction. AJR Am J Roentgenol. 1992;158:997–1000. doi: 10.2214/ajr.158.5.1566706. [DOI] [PubMed] [Google Scholar]
- 35.Valls C, Alba E, Cruz M, Figueras J, Andía E, Sanchez A, Lladó L, Serrano T. Biliary complications after liver transplantation: diagnosis with MR cholangiopancreatography. AJR Am J Roentgenol. 2005;184:812–820. doi: 10.2214/ajr.184.3.01840812. [DOI] [PubMed] [Google Scholar]
- 36.Lang P, Schnarkowski P, Grampp S, van Dijke C, Gindele A, Steffen R, Neuhaus P, Felix R. Liver transplantation: significance of the periportal collar on MRI. J Comput Assist Tomogr. 1995;19:580–585. [PubMed] [Google Scholar]
- 37.Orons PD, Sheng R, Zajko AB. Hepatic artery stenosis in liver transplant recipients: prevalence and cholangiographic appearance of associated biliary complications. AJR Am J Roentgenol. 1995;165:1145–1149. doi: 10.2214/ajr.165.5.7572493. [DOI] [PubMed] [Google Scholar]
- 38.Akun E, Yaprak O, Killi R, Balci NC, Tokat Y, Yuzer Y. Vascular complications in hepatic transplantation: single-center experience in 14 years. Transplant Proc. 2012;44:1368–1372. doi: 10.1016/j.transproceed.2012.02.027. [DOI] [PubMed] [Google Scholar]
- 39.Flint EW, Sumkin JH, Zajko AB, Bowen A. Duplex sonography of hepatic artery thrombosis after liver transplantation. AJR Am J Roentgenol. 1988;151:481–483. doi: 10.2214/ajr.151.3.481. [DOI] [PubMed] [Google Scholar]
- 40.Dravid VS, Shapiro MJ, Needleman L, Bonn J, Sullivan KL, Moritz MJ, Gardiner GA. Arterial abnormalities following orthotopic liver transplantation: arteriographic findings and correlation with Doppler sonographic findings. AJR Am J Roentgenol. 1994;163:585–589. doi: 10.2214/ajr.163.3.8079850. [DOI] [PubMed] [Google Scholar]
- 41.Dodd GD, Memel DS, Zajko AB, Baron RL, Santaguida LA. Hepatic artery stenosis and thrombosis in transplant recipients: Doppler diagnosis with resistive index and systolic acceleration time. Radiology. 1994;192:657–661. doi: 10.1148/radiology.192.3.8058930. [DOI] [PubMed] [Google Scholar]
- 42.Vit A, De Candia A, Como G, Del Frate C, Marzio A, Bazzocchi M. Doppler evaluation of arterial complications of adult orthotopic liver transplantation. J Clin Ultrasound. 2003;31:339–345. doi: 10.1002/jcu.10190. [DOI] [PubMed] [Google Scholar]
- 43.Hom BK, Shrestha R, Palmer SL, Katz MD, Selby RR, Asatryan Z, Wells JK, Grant EG. Prospective evaluation of vascular complications after liver transplantation: comparison of conventional and microbubble contrast-enhanced US. Radiology. 2006;241:267–274. doi: 10.1148/radiol.2411050597. [DOI] [PubMed] [Google Scholar]
- 44.Clevert DA, Stickel M, Minaifar N, Löhe F, Graeb C, Jauch KW, Reiser M. Contrast-enhanced ultrasound in liver transplant: first results and potential for complications in the postoperative period. Clin Hemorheol Microcirc. 2009;43:83–94. doi: 10.3233/CH-2009-1223. [DOI] [PubMed] [Google Scholar]
- 45.Abbasoglu O, Levy MF, Vodapally MS, Goldstein RM, Husberg BS, Gonwa TA, Klintmalm GB. Hepatic artery stenosis after liver transplantation--incidence, presentation, treatment, and long term outcome. Transplantation. 1997;63:250–255. doi: 10.1097/00007890-199701270-00013. [DOI] [PubMed] [Google Scholar]
- 46.Rostambeigi N, Hunter D, Duval S, Chinnakotla S, Golzarian J. Stent placement versus angioplasty for hepatic artery stenosis after liver transplant: a meta-analysis of case series. Eur Radiol. 2013;23:1323–1334. doi: 10.1007/s00330-012-2730-9. [DOI] [PubMed] [Google Scholar]
- 47.Hamby BA, Ramirez DE, Loss GE, Bazan HA, Smith TA, Bluth E, Sternbergh WC. Endovascular treatment of hepatic artery stenosis after liver transplantation. J Vasc Surg. 2013;57:1067–1072. doi: 10.1016/j.jvs.2012.10.086. [DOI] [PubMed] [Google Scholar]
- 48.Park YS, Kim KW, Lee SJ, Lee J, Jung DH, Song GW, Ha TY, Moon DB, Kim KH, Ahn CS, et al. Hepatic arterial stenosis assessed with doppler US after liver transplantation: frequent false-positive diagnoses with tardus parvus waveform and value of adding optimal peak systolic velocity cutoff. Radiology. 2011;260:884–891. doi: 10.1148/radiol.11102257. [DOI] [PubMed] [Google Scholar]
- 49.Glockner JF, Forauer AR, Solomon H, Varma CR, Perman WH. Three-dimensional gadolinium-enhanced MR angiography of vascular complications after liver transplantation. AJR Am J Roentgenol. 2000;174:1447–1453. doi: 10.2214/ajr.174.5.1741447. [DOI] [PubMed] [Google Scholar]
- 50.Glockner JF, Forauer AR. Vascular or ischemic complications after liver transplantation. AJR Am J Roentgenol. 1999;173:1055–1059. doi: 10.2214/ajr.173.4.10511177. [DOI] [PubMed] [Google Scholar]
- 51.Wozney P, Zajko AB, Bron KM, Point S, Starzl TE. Vascular complications after liver transplantation: a 5-year experience. AJR Am J Roentgenol. 1986;147:657–663. doi: 10.2214/ajr.147.4.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chong WK, Beland JC, Weeks SM. Sonographic evaluation of venous obstruction in liver transplants. AJR Am J Roentgenol. 2007;188:W515–W521. doi: 10.2214/AJR.06.1262. [DOI] [PubMed] [Google Scholar]
- 53.Stafford-Johnson DB, Hamilton BH, Dong Q, Cho KJ, Turcotte JG, Fontana RJ, Prince MR. Vascular complications of liver transplantation: evaluation with gadolinium-enhanced MR angiography. Radiology. 1998;207:153–160. doi: 10.1148/radiology.207.1.9530311. [DOI] [PubMed] [Google Scholar]
- 54.Pieters PC, Miller WJ, DeMeo JH. Evaluation of the portal venous system: complementary roles of invasive and noninvasive imaging strategies. Radiographics. 1997;17:879–895. doi: 10.1148/radiographics.17.4.9225389. [DOI] [PubMed] [Google Scholar]
- 55.Pfammatter T, Williams DM, Lane KL, Campbell DA, Cho KJ. Suprahepatic caval anastomotic stenosis complicating orthotopic liver transplantation: treatment with percutaneous transluminal angioplasty, Wallstent placement, or both. AJR Am J Roentgenol. 1997;168:477–480. doi: 10.2214/ajr.168.2.9016230. [DOI] [PubMed] [Google Scholar]
- 56.Navarro F, Le Moine MC, Fabre JM, Belghiti J, Cherqui D, Adam R, Pruvot FR, Letoublon C, Domergue J. Specific vascular complications of orthotopic liver transplantation with preservation of the retrohepatic vena cava: review of 1361 cases. Transplantation. 1999;68:646–650. doi: 10.1097/00007890-199909150-00009. [DOI] [PubMed] [Google Scholar]
- 57.Lee JM, Ko GY, Sung KB, Gwon DI, Yoon HK, Lee SG. Long-term efficacy of stent placement for treating inferior vena cava stenosis following liver transplantation. Liver Transpl. 2010;16:513–519. doi: 10.1002/lt.22021. [DOI] [PubMed] [Google Scholar]
- 58.Liu XL, Li FQ, Li X, Li B, Yan LN, Wei YG. Treatment of hepatic venous outflow stenosis after living donor liver transplantation by insertion of an expandable metallic stent. Hepatobiliary Pancreat Dis Int. 2009;8:424–427. [PubMed] [Google Scholar]
- 59.Ko EY, Kim TK, Kim PN, Kim AY, Ha HK, Lee MG. Hepatic vein stenosis after living donor liver transplantation: evaluation with Doppler US. Radiology. 2003;229:806–810. doi: 10.1148/radiol.2293020700. [DOI] [PubMed] [Google Scholar]
- 60.Sheng R, Sammon JK, Zajko AB, Campbell WL. Bile leak after hepatic transplantation: cholangiographic features, prevalence, and clinical outcome. Radiology. 1994;192:413–416. doi: 10.1148/radiology.192.2.8029406. [DOI] [PubMed] [Google Scholar]
- 61.Verdonk RC, Buis CI, Porte RJ, Haagsma EB. Biliary complications after liver transplantation: a review. Scand J Gastroenterol Suppl. 2006;(243):89–101. doi: 10.1080/00365520600664375. [DOI] [PubMed] [Google Scholar]
- 62.Keogan MT, McDermott VG, Price SK, Low VH, Baillie J. The role of imaging in the diagnosis and management of biliary complications after liver transplantation. AJR Am J Roentgenol. 1999;173:215–219. doi: 10.2214/ajr.173.1.10397129. [DOI] [PubMed] [Google Scholar]
- 63.Ward EM, Wiesner RH, Hughes RW, Krom RA. Persistent bile leak after liver transplantation: biloma drainage and endoscopic retrograde cholangiopancreatographic sphincterotomy. Radiology. 1991;179:719–720. doi: 10.1148/radiology.179.3.2027980. [DOI] [PubMed] [Google Scholar]
- 64.Girometti R, Molinari C, Del Pin M, Toniutto P, Bitetto D, Como G, Zuiani C, Bazzocchi M. Degree of bile-duct dilatation in liver-transplanted patients with biliary stricture: a magnetic resonance cholangiography-based study. Radiol Med. 2012;117:1097–1111. doi: 10.1007/s11547-012-0805-1. [DOI] [PubMed] [Google Scholar]
- 65.Desai M, Neuberger J. Chronic liver allograft dysfunction. Transplant Proc. 2009;41:773–776. doi: 10.1016/j.transproceed.2009.01.038. [DOI] [PubMed] [Google Scholar]
- 66.Neuberger J. Chronic allograft dysfunction: diagnosis and management. Is it always progressive? Liver Transpl. 2005;(11 Suppl 2):S63–S68. doi: 10.1002/lt.20603. [DOI] [PubMed] [Google Scholar]
- 67.Coulden RA, Britton PD, Farman P, Noble-Jamieson G, Wight DG. Preliminary report: hepatic vein Doppler in the early diagnosis of acute liver transplant rejection. Lancet. 1990;336:273–275. doi: 10.1016/0140-6736(90)91804-j. [DOI] [PubMed] [Google Scholar]
- 68.Sandrasegaran K, Ramaswamy R, Ghosh S, Tahir B, Akisik FM, Saxena R, Kwo P. Diffusion-weighted MRI of the transplanted liver. Clin Radiol. 2011;66:820–825. doi: 10.1016/j.crad.2010.12.020. [DOI] [PubMed] [Google Scholar]
- 69.Lucey MR, Terrault N, Ojo L, Hay JE, Neuberger J, Blumberg E, Teperman LW. Long-term management of the successful adult liver transplant: 2012 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Liver Transpl. 2013;19:3–26. doi: 10.1002/lt.23566. [DOI] [PubMed] [Google Scholar]
- 70.Roberts JP. Tumor surveillance-what can and should be done? Screening for recurrence of hepatocellular carcinoma after liver transplantation. Liver Transpl. 2005;(11 Suppl 2):S45–S46. doi: 10.1002/lt.20605. [DOI] [PubMed] [Google Scholar]
- 71.Llovet JM, Bruix J, Fuster J, Castells A, Garcia-Valdecasas JC, Grande L, Franca A, Brú C, Navasa M, Ayuso MC, et al. Liver transplantation for small hepatocellular carcinoma: the tumor-node-metastasis classification does not have prognostic power. Hepatology. 1998;27:1572–1577. doi: 10.1002/hep.510270616. [DOI] [PubMed] [Google Scholar]
- 72.Lee CH, Brubaker LM, Gerber DA, Ku YM, Kim YH, Shin SS, Semelka RC. MRI findings of recurrent hepatocellular carcinoma after liver transplantation: preliminary results. J Magn Reson Imaging. 2011;33:1399–1405. doi: 10.1002/jmri.22326. [DOI] [PubMed] [Google Scholar]
- 73.Borhani AA, Hosseinzadeh K, Almusa O, Furlan A, Nalesnik M. Imaging of posttransplantation lymphoproliferative disorder after solid organ transplantation. Radiographics. 2009;29:981–1000; discussion 1000-1002. doi: 10.1148/rg.294095020. [DOI] [PubMed] [Google Scholar]
- 74.Beaty SD, Silva AC, Depetris G. AJR teaching file: incidental hepatic mass. AJR Am J Roentgenol. 2008;190:S62–S64. doi: 10.2214/AJR.07.7075. [DOI] [PubMed] [Google Scholar]
- 75.Von Schulthess GK, Hany TF. Imaging and PET-PET/CT imaging. J Radiol. 2008;89:438–447; quiz 448. [PubMed] [Google Scholar]
- 76.Kim WR, Terrault NA, Pedersen RA, Therneau TM, Edwards E, Hindman AA, Brosgart CL. Trends in waiting list registration for liver transplantation for viral hepatitis in the United States. Gastroenterology. 2009;137:1680–1686. doi: 10.1053/j.gastro.2009.07.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Forman LM, Lewis JD, Berlin JA, Feldman HI, Lucey MR. The association between hepatitis C infection and survival after orthotopic liver transplantation. Gastroenterology. 2002;122:889–896. doi: 10.1053/gast.2002.32418. [DOI] [PubMed] [Google Scholar]
- 78.Terrault N. Liver transplantation in the setting of chronic HCV. Best Pract Res Clin Gastroenterol. 2012;26:531–548. doi: 10.1016/j.bpg.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 79.Berenguer M, Prieto M, Palau A, Carrasco D, Rayón JM, Calvo F, Berenguer J. Recurrent hepatitis C genotype 1b following liver transplantation: treatment with combination interferon-ribavirin therapy. Eur J Gastroenterol Hepatol. 2004;16:1207–1212. doi: 10.1097/00042737-200411000-00020. [DOI] [PubMed] [Google Scholar]
- 80.Wiesner RH, Sorrell M, Villamil F. Report of the first International Liver Transplantation Society expert panel consensus conference on liver transplantation and hepatitis C. Liver Transpl. 2003;9:S1–S9. doi: 10.1053/jlts.2003.50268. [DOI] [PubMed] [Google Scholar]
- 81.Veldt BJ, Poterucha JJ, Watt KD, Wiesner RH, Hay JE, Kremers WK, Rosen CB, Heimbach JK, Charlton MR. Impact of pegylated interferon and ribavirin treatment on graft survival in liver transplant patients with recurrent hepatitis C infection. Am J Transplant. 2008;8:2426–2433. doi: 10.1111/j.1600-6143.2008.02362.x. [DOI] [PubMed] [Google Scholar]
- 82.Bonekamp S, Kamel I, Solga S, Clark J. Can imaging modalities diagnose and stage hepatic fibrosis and cirrhosis accurately? J Hepatol. 2009;50:17–35. doi: 10.1016/j.jhep.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 83.Bellido-Muñoz F, Giráldez-Gallego A, Roca-Oporto C, García-Cayuela T, Pascasio-Acevedo JM, Sousa-Martín JM. Monitoring the natural evolution and response to treatment of post liver transplant recurrent hepatitis C using transient elastography: preliminary results. Transplant Proc. 2012;44:2082–2086. doi: 10.1016/j.transproceed.2012.07.090. [DOI] [PubMed] [Google Scholar]
- 84.Carrión JA, Navasa M, Bosch J, Bruguera M, Gilabert R, Forns X. Transient elastography for diagnosis of advanced fibrosis and portal hypertension in patients with hepatitis C recurrence after liver transplantation. Liver Transpl. 2006;12:1791–1798. doi: 10.1002/lt.20857. [DOI] [PubMed] [Google Scholar]
- 85.Crespo G, Fernández-Varo G, Mariño Z, Casals G, Miquel R, Martínez SM, Gilabert R, Forns X, Jiménez W, Navasa M. ARFI, FibroScan, ELF, and their combinations in the assessment of liver fibrosis: a prospective study. J Hepatol. 2012;57:281–287. doi: 10.1016/j.jhep.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 86.Harada N, Soejima Y, Taketomi A, Yoshizumi T, Ikegami T, Yamashita Y, Itoh S, Kuroda Y, Maehara Y. Assessment of graft fibrosis by transient elastography in patients with recurrent hepatitis C after living donor liver transplantation. Transplantation. 2008;85:69–74. doi: 10.1097/01.tp.0000297248.18483.16. [DOI] [PubMed] [Google Scholar]
- 87.Beckebaum S, Iacob S, Klein CG, Dechêne A, Varghese J, Baba HA, Sotiropoulos GC, Paul A, Gerken G, Cicinnati VR. Assessment of allograft fibrosis by transient elastography and noninvasive biomarker scoring systems in liver transplant patients. Transplantation. 2010;89:983–993. doi: 10.1097/TP.0b013e3181cc66ca. [DOI] [PubMed] [Google Scholar]
- 88.Kamphues C, Lotz K, Röcken C, Berg T, Eurich D, Pratschke J, Neuhaus P, Neumann UP. Chances and limitations of non-invasive tests in the assessment of liver fibrosis in liver transplant patients. Clin Transplant. 2010;24:652–659. doi: 10.1111/j.1399-0012.2009.01152.x. [DOI] [PubMed] [Google Scholar]
- 89.Corradi F, Piscaglia F, Flori S, D’Errico-Grigioni A, Vasuri F, Tamé MR, Andreone P, Boni P, Gianstefani A, Bolondi L. Assessment of liver fibrosis in transplant recipients with recurrent HCV infection: usefulness of transient elastography. Dig Liver Dis. 2009;41:217–225. doi: 10.1016/j.dld.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 90.Rigamonti C, Fraquelli M, Bastiampillai AJ, Caccamo L, Reggiani P, Rossi G, Colombo M, Donato MF. Transient elastography identifies liver recipients with nonviral graft disease after transplantation: a guide for liver biopsy. Liver Transpl. 2012;18:566–576. doi: 10.1002/lt.23391. [DOI] [PubMed] [Google Scholar]
- 91.Adebajo CO, Talwalkar JA, Poterucha JJ, Kim WR, Charlton MR. Ultrasound-based transient elastography for the detection of hepatic fibrosis in patients with recurrent hepatitis C virus after liver transplantation: a systematic review and meta-analysis. Liver Transpl. 2012;18:323–331. doi: 10.1002/lt.22460. [DOI] [PubMed] [Google Scholar]
- 92.Yoon JH, Lee JY, Woo HS, Yu MH, Lee ES, Joo I, Lee KB, Yi NJ, Lee YJ, Han JK, et al. Shear wave elastography in the evaluation of rejection or recurrent hepatitis after liver transplantation. Eur Radiol. 2013;23:1729–1737. doi: 10.1007/s00330-012-2748-z. [DOI] [PubMed] [Google Scholar]
- 93.Boraschi P, Donati F, Gigoni R, Salemi S, Urbani L, Filipponi F, Falaschi F, Bartolozzi C. Complications after liver transplantation: evaluation with magnetic resonance imaging, magnetic resonance cholangiography, and 3-dimensional contrast-enhanced magnetic resonance angiography in a single session. Can Assoc Radiol J. 2008;59:259–263. [PubMed] [Google Scholar]
- 94.Sandrasegaran K, Akisik FM, Lin C, Tahir B, Rajan J, Saxena R, Aisen AM. Value of diffusion-weighted MRI for assessing liver fibrosis and cirrhosis. AJR Am J Roentgenol. 2009;193:1556–1560. doi: 10.2214/AJR.09.2436. [DOI] [PubMed] [Google Scholar]
- 95.Moteki T, Horikoshi H. Evaluation of hepatic lesions and hepatic parenchyma using diffusion-weighted echo-planar MR with three values of gradient b-factor. J Magn Reson Imaging. 2006;24:637–645. doi: 10.1002/jmri.20682. [DOI] [PubMed] [Google Scholar]
- 96.Koinuma M, Ohashi I, Hanafusa K, Shibuya H. Apparent diffusion coefficient measurements with diffusion-weighted magnetic resonance imaging for evaluation of hepatic fibrosis. J Magn Reson Imaging. 2005;22:80–85. doi: 10.1002/jmri.20344. [DOI] [PubMed] [Google Scholar]
- 97.Girometti R, Furlan A, Bazzocchi M, Soldano F, Isola M, Toniutto P, Bitetto D, Zuiani C. Diffusion-weighted MRI in evaluating liver fibrosis: a feasibility study in cirrhotic patients. Radiol Med. 2007;112:394–408. doi: 10.1007/s11547-007-0149-1. [DOI] [PubMed] [Google Scholar]
- 98.Lewin M, Poujol-Robert A, Boëlle PY, Wendum D, Lasnier E, Viallon M, Guéchot J, Hoeffel C, Arrivé L, Tubiana JM, et al. Diffusion-weighted magnetic resonance imaging for the assessment of fibrosis in chronic hepatitis C. Hepatology. 2007;46:658–665. doi: 10.1002/hep.21747. [DOI] [PubMed] [Google Scholar]
- 99.Boulanger Y, Amara M, Lepanto L, Beaudoin G, Nguyen BN, Allaire G, Poliquin M, Nicolet V. Diffusion-weighted MR imaging of the liver of hepatitis C patients. NMR Biomed. 2003;16:132–136. doi: 10.1002/nbm.818. [DOI] [PubMed] [Google Scholar]
- 100.Aubé C, Racineux PX, Lebigot J, Oberti F, Croquet V, Argaud C, Calès P, Caron C. [Diagnosis and quantification of hepatic fibrosis with diffusion weighted MR imaging: preliminary results] J Radiol. 2004;85:301–306. doi: 10.1016/s0221-0363(04)97582-8. [DOI] [PubMed] [Google Scholar]
- 101.Annet L, Peeters F, Abarca-Quinones J, Leclercq I, Moulin P, Van Beers BE. Assessment of diffusion-weighted MR imaging in liver fibrosis. J Magn Reson Imaging. 2007;25:122–128. doi: 10.1002/jmri.20771. [DOI] [PubMed] [Google Scholar]
- 102.Girometti R, Furlan A, Esposito G, Bazzocchi M, Como G, Soldano F, Isola M, Toniutto P, Zuiani C. Relevance of b-values in evaluating liver fibrosis: a study in healthy and cirrhotic subjects using two single-shot spin-echo echo-planar diffusion-weighted sequences. J Magn Reson Imaging. 2008;28:411–419. doi: 10.1002/jmri.21461. [DOI] [PubMed] [Google Scholar]
- 103.Cheung JS, Fan SJ, Gao DS, Chow AM, Man K, Wu EX. Diffusion tensor imaging of liver fibrosis in an experimental model. J Magn Reson Imaging. 2010;32:1141–1148. doi: 10.1002/jmri.22367. [DOI] [PubMed] [Google Scholar]
- 104.Taouli B, Chouli M, Martin AJ, Qayyum A, Coakley FV, Vilgrain V. Chronic hepatitis: role of diffusion-weighted imaging and diffusion tensor imaging for the diagnosis of liver fibrosis and inflammation. J Magn Reson Imaging. 2008;28:89–95. doi: 10.1002/jmri.21227. [DOI] [PubMed] [Google Scholar]
- 105.Venkatesh SK, Yin M, Ehman RL. Magnetic resonance elastography of liver: technique, analysis, and clinical applications. J Magn Reson Imaging. 2013;37:544–555. doi: 10.1002/jmri.23731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Huwart L, Sempoux C, Vicaut E, Salameh N, Annet L, Danse E, Peeters F, ter Beek LC, Rahier J, Sinkus R, et al. Magnetic resonance elastography for the noninvasive staging of liver fibrosis. Gastroenterology. 2008;135:32–40. doi: 10.1053/j.gastro.2008.03.076. [DOI] [PubMed] [Google Scholar]
- 107.Huwart L, Sempoux C, Salameh N, Jamart J, Annet L, Sinkus R, Peeters F, ter Beek LC, Horsmans Y, Van Beers BE. Liver fibrosis: noninvasive assessment with MR elastography versus aspartate aminotransferase-to-platelet ratio index. Radiology. 2007;245:458–466. doi: 10.1148/radiol.2452061673. [DOI] [PubMed] [Google Scholar]
- 108.Rouvière O, Yin M, Dresner MA, Rossman PJ, Burgart LJ, Fidler JL, Ehman RL. MR elastography of the liver: preliminary results. Radiology. 2006;240:440–448. doi: 10.1148/radiol.2402050606. [DOI] [PubMed] [Google Scholar]
- 109.Yin M, Talwalkar JA, Glaser KJ, Manduca A, Grimm RC, Rossman PJ, Fidler JL, Ehman RL. Assessment of hepatic fibrosis with magnetic resonance elastography. Clin Gastroenterol Hepatol. 2007;5:1207–1213.e2. doi: 10.1016/j.cgh.2007.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lee VS, Miller FH, Omary RA, Wang Y, Ganger DR, Wang E, Rao S, Levitsky J. Magnetic resonance elastography and biomarkers to assess fibrosis from recurrent hepatitis C in liver transplant recipients. Transplantation. 2011;92:581–586. doi: 10.1097/TP.0b013e31822805fa. [DOI] [PubMed] [Google Scholar]
- 111.Perumpail RB, Levitsky J, Wang Y, Lee VS, Karp J, Jin N, Yang GY, Bolster BD, Shah S, Zuehlsdorff S, et al. MRI-guided biopsy to correlate tissue specimens with MR elastography stiffness readings in liver transplants. Acad Radiol. 2012;19:1121–1126. doi: 10.1016/j.acra.2012.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]


