Abstract
Purpose. To analyse the survival after salvage radiosurgery and to identify prognostic factors. Methods. We retrospectively reviewed 87 consecutive patients, with recurrent high-grade glioma, that underwent stereotactic radiosurgery between 1997 and 2010. We evaluated the survival after initial diagnosis and after reirradiation. The prognostic factors were analysed by bivariate and multivariate Cox regression model. Results. The median age was 48 years old. The primary histology included anaplastic astrocytoma (47%) and glioblastoma (53%). A margin dose of 18 Gy was administered in the majority of cases (74%). The median survival after initial diagnosis was 21 months (39 months for anaplastic astrocytoma and 18.5 months for glioblastoma) and after reirradiation it was 10 months (17 months for anaplastic astrocytoma and 7.5 months for glioblastoma). In the bivariate analyses, the prognostic factors significantly associated with survival after reirradiation were age, tumour and treatment volume at recurrence, recursive partitioning analyses classification, Karnofsky performance score, histology, and margin to the planning target volume. Only the last four showed significant association in the multivariate analyses. Conclusion. stereotactic radiosurgery is a safe and may be an effective treatment option for selected patients diagnosed with recurrent high-grade glioma. The identified prognostic factors could help individualise the treatment.
1. Introduction
Gliomas are primary malignant brain tumours that arise from glial cells. The World Health Organization (WHO) has classified gliomas into four grades of ascending malignancy [1]. According to this classification, grade III and grade IV, also known as anaplastic astrocytoma (AA) and glioblastoma multiforme (GBM), respectively, are the most aggressive and are termed high-grade gliomas (HGG) [1]. The current standard treatment for glioblastoma patients includes maximal surgical resection, followed by temozolomide (TMZ) concomitant with external beam radiation (EBRT), and then subsequently with additional TMZ cycles, following the Stupp protocol [2]. Despite significant improvements in neuroimaging, surgical techniques, radiotherapy, and chemotherapy, the prognosis for these patients is still poor, with a median survival of 14.6 months and an overall survival of 27% after 2 years, dropping then to under 10% after 5 years [2].
Recurrence occurs in more than 90% of the patients [3] and its treatment is not clearly established with a median survival of 3–6 months without treatment [4]. Different options of treatment include: repetition of surgical resection, reirradiation with EBRT, brachytherapy or stereotactic radiosurgery (SRS), chemotherapy, novel therapies, or a combination of the above. Due to the highly invasive nature of HGG and the subsequent difficulty to delineate it, local treatment does not seem to make sense. However, the majority of treatment failures are within the irradiated field; up to 90% of recurrences occurred within 2 cm of the tumour margins [5]. For this reason, local control is one of the main goals of the treatment of recurrent HGG.
Tumour resection is a good option for salvage treatment, but it is associated with many postoperative complications. EBRT exposes the brain to a high risk of radiation-related toxicity and necrosis. Brachytherapy is also associated with serious side effects like infections or risk of haemorrhage. All of this suggests a potential key role for SRS in the management of recurrent HGG; in addition, these tumours are relatively hypoxic with low α/β and a priori good responders to hypofractionated irradiation [4–6].
First conceived by Lars Leksell in 1951, stereotactic radiosurgery (SRS) is an irradiation modality that combines stereotactic technique with highly focused high-energy radiation treatments, making it possible to deliver large doses of radiation to an extremely small target [7].
The experience of reirradiation with radiosurgery for recurrent HGG is limited. At our institution, we have performed single fraction reirradiation (SRS) in selected patients with relatively well defined recurrent tumors as seen on imaging studies, which have an adequate volume.
In this study, we investigated our clinical data to evaluate the efficacy of SRS as a salvage treatment and the potential prolongation of survival time in 87 patients. Additionally we reported the results of overall and post-SRS survival and prognostic factors in patients with recurrent HGG treated with linear accelerator- (LINAC-) based radiosurgery over a 12-year period.
2. Patients and Methods
2.1. Patients
Between 1997 and 2010, 87 consecutive adult patients were treated at Virgen de las Nieves University Hospital (Granada, Spain). All of them underwent SRS LINAC as salvage treatment for recurrent HGG with the following features: (1) pathologically confirmed diagnosis of AA or GBM at the time of initial management; (2) underwent subsequent fractionated radiotherapy treatment with radical intent; (3) developed new or increasing contrast-enhanced lesions at the margin of primary localization in the follow-up magnetic resonance imaging (MRI) after radiotherapy, indicating tumour recurrence or progression; and (4) the size of the lesion was <3 cm.
Data were retrospectively collected by reviewing medical records, last followup in the hospital, and MRI studies and contacting patients and/or families. This way, we obtained information about age, gender, recursive partitioning analyses (RPA) classification [8], Karnofsky performance status (KPS) score, histology as World Health Organization (WHO) grade 3 gliomas AA or GBM, time to relapse, tumour and treatment volume at recurrence, margin to the planning target volume, dose administered, and radiological and neurological responses. Dates of death were obtained from National Death Index (INDEF, Spanish initials).
2.2. Radiosurgery
Outpatient radiosurgery was indicated by a medical staff composed of neurosurgeons, radiologists, radiation oncologists, and physicists involved in treatment planning and target volume determination for all patients.
Treatment was planned on the image fusion of computed tomography (CT) and MRI data, for the contrast-enhancing regions on T1-weighted MRI images, and was delivered using a linear accelerator (LINAC) (Varian 2100) equipped with micro-multileaf collimators (MMC) using 6 MV photons. A BrainLAB stereotactic head frame (BrainLAB A.G., Heimstetten, Germany) was used for every patient. BrainLAB cones were used for the treatment until 2004 when dynamic micro-multileaf collimator was incorporated (Figure 1).
Figure 1.
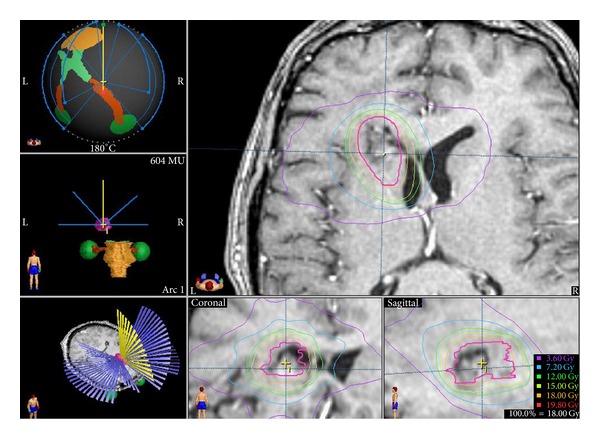
An example of radiosurgery treatment in our department.
The prescribed dose for reirradiation was based on tumour volume, prior radiation dose, time since EBRT, and location of the lesion with proximity to eloquent brain or radiosensitive structures. The GTV (contrast-enhancing lesion in T1-weighted MR images) was expanded by 0–6 mm to generate the planning target volume (PTV). This expansion was related to the year of treatment (without any expansion during the first five years), in the size and location of the recurrence.
2.3. Followup
After SRS, patients were seen for a follow-up visit after 8 weeks and thereafter in 3 months intervals. Each follow-up appointment consisted of a thorough clinical examination, including a neurological assessment and a contrast-enhanced MRI. Local control (LC) was defined as stabilization or decrease of lesion size or enhancement on imaging and lack of consistently increased surrounding T2 signal changes on serial examinations. Local failure was defined as persistent increase in size of the contrast-enhancing lesion (>20% volume increase) or new contiguous areas at the margin of treatment and concomitant T2 signal change. Toxicity was also collected. Differentiating second-time recurrence tumour after SRS from radiation injury based on MRI is difficult. Progressive contrast enhancements over time may represent either a mixture of a viable tumour and radiation-induced necrosis or radiation injury only. Metabolic imaging, MR spectroscopy, and MR perfusion were used as supplements in some uncertain cases.
2.4. Statistical Analyses
The aim of these studies is to examine the overall survival, post-SRS survival, and the identification of prognostic factors with influence on survival after SRS.
Overall survival was calculated from the time of the primary diagnosis to the time of death or last followup. Survival after SRS was calculated from the time of SRS until the death of last followup, using the Kaplan-Meier method.
Bivariate statistical analyses were performed to examine the relationships between the duration of survival after SRS and different variables at the time of the treatment, using Cox regression models. In a first step, those variables which were statistically significant in the bivariate analyses were included in the multivariate model that was finally built using a backward stepwise technique. Diagnosis of the models was performed in order to ensure the goodness of the fit and the fulfilment of implementation conditions. Hazard ratios (HRs) with 95% confidence intervals (CIs) were calculated. Two-sided P values less than 0.05 were considered significant. SPSS version 12 (SPSS, Chicago, IL) was used for statistical analyses, except for multivariate analyses that were performed by “R” version 3.0.2.
3. Results
3.1. Patients
The initial treatment characteristics are shown in Table 1. This initial treatment included: surgery, EBRT within 8–12 weeks after surgery with doses varying 54–66 Gy (mean 60 Gy), and adjuvant chemotherapy in 63 patients. Surgery with complete resection was performed in 43 patients (49.4%). From 1999 up to and including 2004, patients received EBRT alone or in combination with procarbazine, lomustine, and vincristine (PCV). From 2005, patients received the Stupp protocol [9] with temozolomide and EBRT, except for patients without good medical conditions who underwent exclusive EBRT. Thus, 51 patients (58.6%) were treated with the Stupp protocol, 12 patients (13.8%) were treated with EBRT in combination with PCV, and 24 patients (27.6%) were treated with EBRT alone.
Table 1.
Initial treatment features.
| Parameters | Number of patients (%) |
|---|---|
| Number or patients | 87 |
| Primary surgery Complete resection Subtotal resection Biopsy |
43 (49.4) 23 (26.4) 21 (24.2) |
| Adjuvant therapy Stupp protocol PCV + EBRT EBRT without chemotherapy |
51 (58.6) 12 (13.8) 24 (27.6) |
Clinical features in recurrence are summarised in Table 2. Out of 87 patients, 43 were males and 44 females; median age was 49 years old; 41 patients with anaplastic astrocytoma (AA) and 46 with glioblastoma (GBM). The diagnosis was histologically confirmed in all patients. KPS score was higher than 80 in 40 patients. 51 patients (29 with AA and 20 with GBM) had surgery for the first recurrence and radiosurgery for the residual tumour seen on the postoperative MRI after reoperation or for a second recurrence. The median time interval from diagnosis to SRS treatment was 13.8 months (range 5–61 m).
Table 2.
Patient treatment characteristics at recurrence.
| Parameters | Number of patients | Patients treated by Stupp protocol | Patients diagnosed with AA | Patients diagnosed with GBM |
|---|---|---|---|---|
| Numbers of patients | 87 | 51 | 41 | 46 |
| Gender Male Female |
43 (49.4%) 44 (50.6%) |
27 (52.9%) 24 (47.1%) |
16 (39%) 25 (61%) |
27 (58.7%) 19 (41.3%) |
| Age (years) median (range) |
48.7 (18–78) |
47 (26–71) |
45 (18–78) |
49.5 (26–78) |
| KPS Mean (range) KPS > 80 KPS ≤ 80 |
83 (60–100) 40 (46%) 47 (50%) |
90 (70–100) 28 (54.9%) 23 (45.1%) |
90 (70–100) 22 (53.7%) 19 (46.3%) |
80 (70–100) 18 (39.1%) 28 (60.9%) |
| RPA Mean (range) |
4.1 (3–5) |
4 (3–5) |
4 (3–5) |
4 (3–5) |
| Histology Anaplastic astrocytoma Glioblastoma |
41 (47.1%) 46 (52.9%) |
25 (49%) 26 (51%) |
100% 0 |
0 100% |
| Time to recurrence (months) Mean (range) ≤8 months 9–12 months >12 months |
13.8 (4–61) 29 (33.3%) 30 (34.5%) 28 (32.2%) |
11 (4–61) 14 (27.4%) 19 (27.3%) 18 (35.3%) |
10 (4–61) 12 (29.3%) 15 (36.6%) 14 (34.1%) |
10 (5–28) 17 (36.9%) 15 (32.6%) 13 (30.5%) |
| Tumour volume (cc) Mean (range) <3 cc 4–7 cc >7 cc |
8.7 (1–42.6) 29 (33.3%) 26 (29.9%) 32 (36.8%) |
4 (0.36–34.1) 16 (31.4%) 22 (43.1%) 13 (25.5%) |
5.2 (1–28) 12 (29.3%) 12 (29.3%) 17 (41.4%) |
4 (0.05–34.1) 17 (37%) 14 (30.4%) 15 (32.6%) |
| Location Unifocal Multifocal |
79 (90.8%) 8 (9.2%) |
45 (88.2%) 6 (11.8%) |
39 (95.1%) 2 (4.9%) |
40 (87%) 6 (13%) |
| Dose radiosurgery Mean (range) Dose ≥ 18 Gy |
18.01 Gy (14–20) 76 (87%) |
18 Gy (16–20) 46 (90.2%) |
18 (15–20) 35 (85.4%) |
18 Gy (14–20) 41 (89.1%) |
| PTV margin Mean (range) 0 mm 1–3 mm >3 mm |
1.67 mm (0–6) 43 (49.4%) 22 (25.3%) 22 (25.3%) |
2 mm (0–6) 20 (39.2%) 10 (19.6%) 21 (41.2%) |
2 mm (0–5) 19 (46.3%) 12 (29.3%) 10 (24.4%) |
0 mm (0–6) 24 (52.2%) 10 (21.7%) 12 (26.1%) |
3.2. Radiosurgery and Radiological and Clinical Responses
The median prescribed dose was 18 Gy (range 14–20). The median tumor volume and PTV volume were 4 cc and 6 cc, respectively. The margin of the GTV to create the PTV was 0 mm in the majority of treatments (48.3%) followed by 5 (20.7%). The treatment was administered by cones in 40.2% of cases and by MMC in 59.8%. The majority of patients received only one SRS treatment (89%), while the remainder underwent more than one course of SRS (9.8% two SRSs and 1.2% three SRSs).
The median follow-up after SRS was 10 months (range 1–141 months). The initial radiological response was complete in 7.8%, partial in 24.7%, stabilisation in 32.5%, and progression in 26%. In 9% of the patients the response could not be evaluated, because of death before the MRI. These patients are considered as nonresponders. At the initial evaluation after the SRS, 17.1% of patients were clinically better than before the treatment, 32.9% remained without change, 21.4% were neurologically worse, and 28.6% were not evaluated because of death before the first follow-up visit or incomplete data in the clinical record.
There were no cases of treatment-related adverse events or episodes of acute neurological toxicity. On the follow-up images (10%) there was an increasing oedema with a transient worsening of neurological function for the patients; all of this was considered as adverse radiation effects.
The treatment of local failure post-SRS consisted of surgical resection in three patients, changes in chemotherapy regimen in five patients, and no further treatment for the remainder.
3.3. Survival and Prognostic Factors
At the end of the study 7 patients (8%) were alive with no evidence of disease, 5 patients (5.7%) were alive with disease, and 75 patients (86.2%) were dead. The cause of death was the progression of the tumour in all patients.
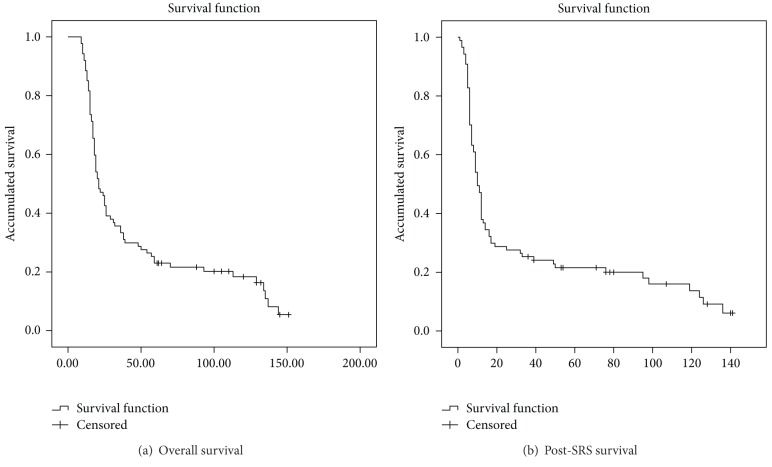
Table 3 shows the information about survival. The median overall survival was 21 months (range 9–151 months), although patients treated by Stupp protocol had higher survival than patients treated by other treatments [10]. Initial treatment (Stupp versus others) was not significantly associated with overall survival (HR = 0.79; 95 % CI = 0.49–1.25). The actuarial global survival rates after 12, 24, and 36 months were 88.5%, 46%, and 35.6%, respectively (Figure 2(a)). The median survival after SRS was 10 months (range 1–141 months), 7.5 months for GBM (range 1–140), and 17 months for AA (4–141). The actuarial survival after SRS rate was 37.9% after 12 months, 28.7% after 24 months, and 25.3% after 36 months (Figure 2(b)).
Table 3.
Survival.
| Stupp protocol | Others Treatments | AA | GBM | |
|---|---|---|---|---|
| OS (median) | 21 months | 19 months | 39 months | 18.5 months |
| Actuarial Sv 12 m 24 m 36 m |
88.5% 46% 35.6% |
88.9% 36.1% 25% |
95.1% 41.5% 30.9% |
82.6% 50% 21.7% |
| Post-SRS Sv | 10 months | 9 months | 17 months | 7.5 months |
| Actuarial post-SRS Sv 12 m 24 m 36 m |
37.9% 28.7% 25.3% |
30.6% 19.4% 16.7% |
70.7% 41.5% 25.7% |
30.4% 13% 10.9% |
OS: overall survival and Sv: survival.
Figure 2.
Overall and post-SRS survival. Kaplan-Meier survival function.
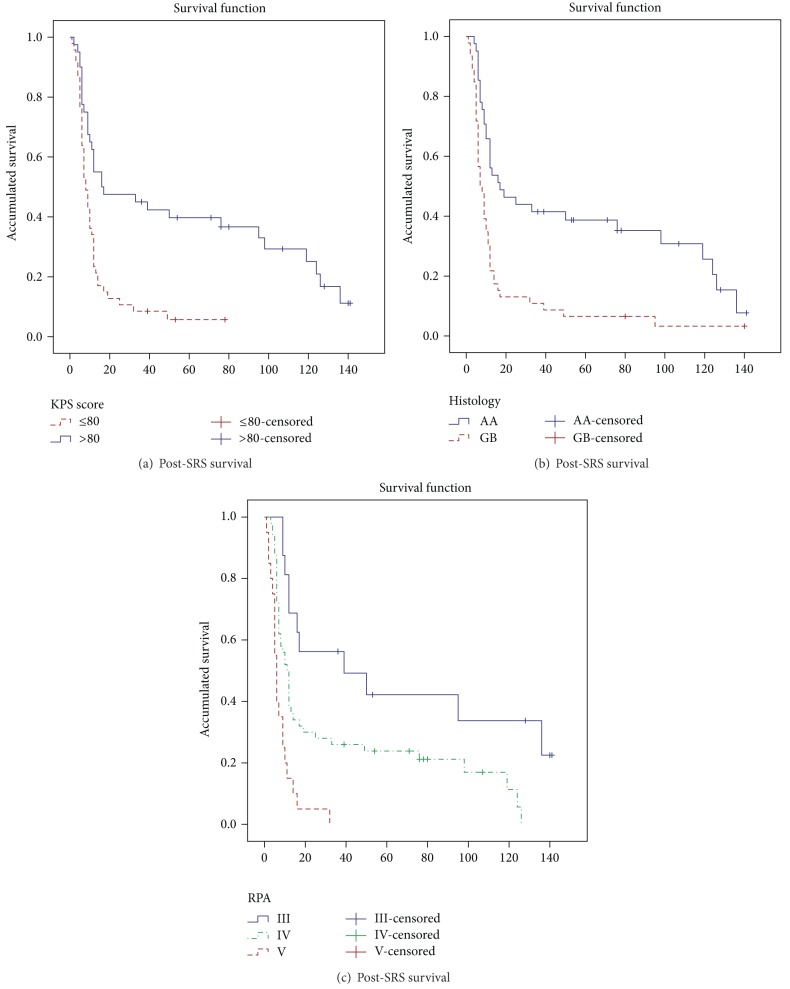
The variables included in the analyses of the prognostic factors of post-SRS survival were age (year old), gender, KPS score, RPA classification, histology (AA or GBM), initial surgery (complete or not), initial treatment (Stupp protocol versus other treatments), time of recurrence (months), focality (unifocal or multifocal), tumour volume (cubic centimeter), treatment volume (cubic centimeter), margin to the PTV (millimeter), and dose (Gy) administered. In the bivariate analyses (Table 4) the following variables were significantly associated with survival post-SRS: age (years old) (HR = 1.04; 95% CI = 1.01–1.05), KPS ≤ 80 versus > 80 (HR = 2.59; 95% CI = 1.55–4.3), RPA IV versus III (HR = 2.39; 95% CI = 1.18–4.82), RPA V versus III (HR = 6.32; 95% CI = 2.82–14.14), GBM versus AA (HR = 2.45; 95% CI = 1.53–3.94), tumour volume (cubic centimetre) (HR = 1.04; 95% CI = 1.01–1.07), treatment volume (cubic centimetre) (HR = 1.03; 95% CI = 1.01–1.06), and margin to the PTV (millimetre) (HR = 0.77; 95% CI = 0.67–0.87). In the multivariate analyses (Table 3) we found that the risk of sudden death was 2.08 times higher in KPS ≤ 80 than KPS > 80 (95% CI = 0.28–0.83) (Figure 3(a)), 3.13 times higher in GBM than AA (95% CI = 1.79–5.48) (Figure 3(b)), 3.46 times higher in RPA IV than RPA III (95% CI = 1.61–7.46), 7.29 times higher in RPA V than RPA III (95% CI = 3.23–16.34) (Figure 3(c)), and 3.19 times higher in PTV margin 0 than PTV ≥ 1 (95 % CI = 1.91–5.31).
Table 4.
Prognostic factors.
| Variables | Bivariate analyses | Multivariate analyses | ||
|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | |
| Age | 1.04 (1.01–1.05) | P < 0.001 | Not significant | |
| KPS (≤80 versus >80) | 2.59 (1.55–4.3) | P < 0.001 | 2.08 (0.28–0.83) | P = 0.008 |
| RPA | ||||
| IV versus III | 2.39 (1.18–4.82) | P = 0.015 | 3.46 (1.61–7.46) | P = 0.001 |
| V versus III | 6.32 (2.82–14.14) | P < 0.001 | 7.29 (3.23–16.34) | P < 0.001 |
| Histology (GBM versus AA) | 2.45 (1.53–3.94) | P < 0.001 | 3.13 (1.79–5.48) | P < 0.001 |
| Tumour volume | 1.04 (1.01–1.07) | P = 0.005 | Not significant | |
| Treatment volume | 1.03 (1.01–1.06) | P = 0.013 | ∗ | |
| Margin to PTV | ||||
| 0 versus ≥1 | 0.77 (0.67–0.87) | P < 0.001 | 3.19 (1.91–5.31) | P < 0.001 |
*This variable was not considered for the multivariate analyses because of the strong correlation (0.97 Spearman' s correlation coefficient) with tumour volume.
Figure 3.
Prognosis factors, Kaplan-Meier survival function.
4. Discussion
Poor prognosis of this HGG with high risk of relapse, mainly within 2 cm of the resection cavity, suggests there is a need to improve local treatment [4]. Hau et al. [11] compared patients who were treated with aggressive salvage therapy including SRS with a group of patients who received no salvage treatment. In that study, the median actuarial survival after recurrence was 8.2 months in the intervention group and 2.2 months in the nonintervention group, indicating that salvage treatment was beneficial.
Several authors have studied the optimal moment to administer SRS: as an initial treatment or as an adjuvant treatment for recurrence [6, 12]. Nowadays, the study with the highest level of evidence is Radiation Therapy Oncology Group 93-05 [12]. Although it was highly criticised, the conclusion was that the addition of SRS at the time of initial treatment did not appreciably enhance survival, quality of life, or neurocognition for GBM. However, Kong et al. [13] showed a survival benefit of SRS as salvage treatment compared with historic control. So far, the main role of SRS takes place at the time of recurrence, for this reason, our department does not recommend SRS as initial treatment.
Managing recurrent HGG is particularly challenging. Surgery is well established as newly diagnoses HGG; however, the reoperation has a low median postoperative survival and high complication rates due to the infiltrative growth pattern of gliomas [14–16]. Skeie et al. [17] reviewed patients treated with SRS, surgery, or both. For recurrent GBM the median survival for SRS was significantly better than surgery. Surgery could be used to decrease the size of a large tumour before SRS. This way, 59% of our patients underwent surgery as salvage treatment after recurrence that allowed the treatment with SRS for the residual tumour. EBRT increases the risk of late cumulative radiation injury, although the recent advances in radiotherapy that reduce the radiation to surrounding brain tissue can turn this treatment into a useful option for tumours with a larger volume [4]. Brachytherapy can have side effects as radiation necrosis, hemorrhage, and infection [4]. Thus, there is a clear advantage of SRS over brachytherapy: the noninvasive approach. There have been many studies suggesting that SRS is effective mainly for HGG [13, 18–20].
Related to adverse side effects due to reirradiation by SRS, early toxicity as headache, nausea, vomiting, and so forth is medically managed, while late complication involves radiation necrosis that typically develops one to three years after radiation. The incidence reported by the literature varies from 0% [21, 22] to 30% [23, 24] and is associated with tumour volume [24]. In our series, none of the patients had radiation necrosis, probably given the short life expectancy. In addition, we believe that SRS provides a highly precise delivery of radiation dose sufficient to induce tumour cell death while sparing surrounding host tissue. For this reason, we think reirradiation by SRS is safe for small tumours.
We analysed our series with 87 patients treated with SRS at the moment of the recurrence. We used a LINAC equipped with micro-multileaf collimators (MMC) using 6 MV photons and a BrainLAB stereotactic head frame. There are different SRS modalities (LINAC, Cyberknife and Gamma knife), and most of the published articles describe the experience with Gamma Knife. However, there is no evidence of which modality is better. The majority of patients received 18 Gy in one fraction, and as other authors pointed, because of the high radiation dose already given in the initial treatment with EBRT, it is difficult to administer a high dose [17]. Skeie et al. [17] did not find any difference in survival when they compared patients who received more than 12 Gy versus ≤12 Gy. In addition, the dose administered was not correlated to survival post-SRS in our study.
The median overall and post-SRS survival in our study is in accordance with the literature (Table 5). The median post-SRS survival varies between 6.5 months [25] and 26 months [13]. These differences may be due to the inhomogeneity among the studies (clinical features of the patients, histological type, modalities of treatment after SRS, and so forth). The study with the largest number of patients is Kong et al.'s study [13] with a post-SRS survival of 26 months for grade III gliomas and 13 months for grade IV gliomas, different data as RPA classifications were not reported.
Table 5.
Studies of SRS as treatment for recurrent high-grade gliomas.
| Study | N | Histological grade | Median dose (Gy) | Median volume (cm3) | Median post-SRS survival (months) | Prognostic factors |
|---|---|---|---|---|---|---|
| Chamberlain et al., 1994 [34] | 15 | IV | 13.4 | 17 | 8 | NR |
| Hall et al., 1995 [35] | 25 | III–IV | 20 | 28 | 6.5 | Age, KPS |
| Shrieve et al., 1995 [27] | 86 | IV | 13 | 10.1 | 12 | Age, volume |
| Larson et al., 1996 [31] | 93 | IV | 16 | 6.5 | 16.4 | Age, grade, KPS, focality, and volume |
| Kondziolka et al., 1997 [36] | 42 | III–IV | 15.5 | 6.5 | 21 | Grade, volume |
| Cho et al., 1999 [23] | 46 | III–IV | 17 | 10 | 11 | Age, grade, KPS, and volume |
| Ulm et al., 2005 [30] | 33 | III–IV | 15 | — | — | Location, RPA |
| Hsieh et al., 2005 [24] | 26 | IV | 12 | 21.6 | 10 | KPS |
| Mahajan et al., 2005 [37] | 41 | IV | — | 4.7 | 11 | None |
| Combs et al., 2005 [21] | 32 | IV | 15 | 10 | 10 | None |
| Kong et al., 2008 [13] | 114 | III–IV | 16 | 10.6 | 26 (III)–13 (IV) | Histology, volume |
| Patel et al., 2009 [18] | 26 | IV | 18 | 10.4 | 8.5 | None |
| Biswas et al., 2009 [38] | 18 | IV | 15 | 8.4 | 5.3 | NR |
| Villavicencio et al., 2009 [25] | 26 | IV | 20 | 7 | 7 | Extent of surgery |
| Pouratian et al., 2009 [22] | 26 | IV | 6 | 21.3 | 9.4 | KPS, PTV margin |
| Torok et al., 2011 [39] | 14 | IV | 24 | 6.97 | 10 | NR |
| Maranzano et al., 2011 [40] | 13 | IV | 17.3 | 5.3 | 11 | Radiation dose |
| Cuneo et al., 2012 [29] | 63 | III/IV | 15 | 4.8 | 11 | Age, KPS, and bevacizumab |
| Park et al., 2012 [41] | 11 | IV | 16 | 13.6 | 17.9 | None |
| Skeie et al., 2012 [17] | 51 | IV | 12.2 | 12.4 | 19 (from initial diagnosis) | None |
| Martínez-Carrillo 2014 | 87 | III/IV | 18.01 | 8.7 | 10 (17 III–7.5 IV) | KPS, RPA, histology, and PTV margin |
NR: not reported.
Favourable prognostic factors derived from the most relevant studies published (Table 5) include higher prescription dose, adequate SRS margin, anaplastic astrocytoma, smaller tumour volume, younger age, higher KPS, better RPA, location in noneloquent area, unifocality, and concurrent chemotherapy. However, among the different prognosis factors analysed in the present study, only KPS score, RPA, histology, and margin to the PTV made statistically a significant influence on post-SRS survival in the multivariate analyses. The identification of prognostic factors varies among studies. The difference may be due, in part, to the definition and/or adherence of eligibility criteria, clinical features of the patients, characteristic of the treatment, and so on. Other molecular prognosis factors as O-6-methylguanine-DNA methyltransferase (MGMT) methylation, 1p/19q deletion, or isocitrate dehydrogenase 1/2 (IDH1/2) mutation [26] were not included in these studies, probably because the role of this molecular factors is fairly recent.
Shrieve et al. [27] showed that while under 40 years old patients had a median survival of 49 months; over 40 years old patients had a median survival of 18.2 months (P < 0.001). In our study the age was associated with the post-SRS survival only in the bivariate analyses; thus, for each extra year of life the risk of sudden death was multiplied by 1.04 (95% CI = 1.01–1.05). We did not find this correlation in the multivariate analyses, perhaps because the variability explained by this variable in the bivariate analyses was later explained by the RPA classification in the multivariate model.
The tumour and treatment volumes were identified as prognosis factor for the post-SRS survival in the bivariate analyses but not in the multivariate analyses. Kong et al. [13] and Combs et al. [28] obtained the similar results, although the latter treated patients with fractionated stereotactic radiotherapy instead of SRS.
According to our statistical analyses, higher KPS score was statistically significant correlated with post-SRS survival. In our study the cut-off point was KPS score of 80 (Figure 2(a)), while Cuneo et al. [29] reported the same correlation but with a cut-off point of 70 in the KPS score. Other authors have shown KPS score as prognosis factor for survival with a cut-off point of 90 [22, 24].
RPA classification was a significant predictive value of survival on bivariate and multivariate analyses in this series, reinforcing the predictive value of the RPA classification even with salvage treatments. A survival benefit from SRS for patients with class III through V has also been suggested by Ulm et al. [30] and Skeie et al. [17].
We found that the risk of sudden death was 3.13 times higher in GBM than AA (95% CI = 1.79–5.48) (Figure 2(b)). In HGG group, grade III presents a significant favourable prognosis with respect to grade IV, for overall and postsalvage SRS survival. Larson et al. [31] found that the post-SRS survival was 68 weeks and 38 weeks for grade III and grade IV gliomas, respectively. Kong et al. [13] found similar results with post-SRS survival of 26 months and 13 months for grades III and IV, respectively.
PTV margin was a statistical significant protective factor. Several authors defend the use of an “extended field” to cover the potential microscopic expansion [32, 33]. As mentioned above, this strategy is supported by the acknowledgment that this kind of tumours tend to progress within 2 cm of the contrast-enhancing edge. Koga et al. [32] found a statistically significant difference in the local control between conventional SRS (47%) and extended field (93%). However, the “extended field” depends on the tumour volume, location,and if there are close organs at risk, considering that in reirradiation the treatment volume has a strong correlation with the toxicity.
To obtain better results for this kind of tumours, different strategies are mentioned:
Imaging to improve the target delineation and to evaluate the results after treatment.
New chemotherapy agents and targeted therapies as bevacizumab [29].
Molecular characterisation of these tumours as the determination of the methylation status of MGMT [26].
The main weakness of our study is the retrospective character of the study with a heterogeneous population and nonuniform treatment modalities and selection bias because patients who are candidates for salvage SRS treatment tend to have more favourable prognosis factors than those ineligible patients. However, due to the low incidence of these tumours, a prospective study is difficult and in clinical practice, patients diagnosed with this entity are not homogeneous and neither is the initial treatment which depends on the medical condition of the patients. You can find the same problem related to the homogeneity of the sample in other published articles [3, 4, 13]. In addition, our series has a large number of patients and the results are in accordance with the literature.
5. Conclusion
There is no class I evidence establishing a “standard of care” for recurrence. Because local recurrence remains the predominant pattern of failure in patients with HGGs, local salvage treatment with SRS is appropriate and safe and may contribute to a prolonged survival in young patients with AA histology who have a good KPS score and RPA classification, a small volume, and are treated with an adequate margin. In addition, it seems multimodality treatment is better than no salvage therapy, for this reason, we recommend second surgery to reduce the volume of the recurrence and to complete the treatment with SRS if possible.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Louis DN, Ohgaki H, Wiestler OD, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathologica. 2007;114(2):97–109. doi: 10.1007/s00401-007-0243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stupp R, Hegi ME, Mason WP, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. The Lancet Oncology. 2009;10(5):459–466. doi: 10.1016/S1470-2045(09)70025-7. [DOI] [PubMed] [Google Scholar]
- 3.Koga T, Saito N. Efficacy and limitations of stereotactic radiosurgery in the treatment of glioblastoma. Neurologia Medico-Chirurgica. 2012;52(8):548–552. doi: 10.2176/nmc.52.548. [DOI] [PubMed] [Google Scholar]
- 4.Elliott RE, Parker EC, Rush SC, et al. Efficacy of gamma knife radiosurgery for small-volume recurrent malignant gliomas after initial radical resection. World Neurosurgery. 2011;76(1-2):128–140. doi: 10.1016/j.wneu.2010.12.053. [DOI] [PubMed] [Google Scholar]
- 5.Marin LA, Smith CE, Langston MY, Quashie D, Dillehay LE. Response of glioblastoma cell lines to low dose rate irradiation. International Journal of Radiation Oncology Biology Physics. 1991;21(2):397–402. doi: 10.1016/0360-3016(91)90788-6. [DOI] [PubMed] [Google Scholar]
- 6.Elaimy AL, Mackay AR, Lamoreaux WT, et al. Clinical outcomes of gamma knife radiosurgery in the salvage treatment of patients with recurrent high-grade glioma. World Neurosurgery. 2013;80(6):872–878. doi: 10.1016/j.wneu.2013.02.030. [DOI] [PubMed] [Google Scholar]
- 7.Leksell L. Stereotactic radiosurgery. Journal of Neurology Neurosurgery and Psychiatry. 1983;46(9):797–803. doi: 10.1136/jnnp.46.9.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scott CB, Scarantino C, Urtasun R, et al. Validation and predictive power of Radiation Therapy Oncology Group (RTOG) recursive partitioning analyses classes for malignant glioma patients: a report using RTOG 90-06. International Journal of Radiation Oncology Biology Physics. 1998;40(1):51–55. doi: 10.1016/s0360-3016(97)00485-9. [DOI] [PubMed] [Google Scholar]
- 9.Stupp R, Mason WP, Van den Bent MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. The New England Journal of Medicine. 2005;352(10):987–996. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 10.Nava F, Tramacere I, Fittipaldo A, et al. Survival effect of first- and second-line treatments for patients with primary glioblastoma: a cohort study from a prospective registry, 1997–2010. Neuro-Oncology. 2014;16(5):719–727. doi: 10.1093/neuonc/not316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hau P, Baumgart U, Pfeifer K, et al. Salvage therapy in patients with glioblastoma: is there any benefit? Cancer. 2003;98(12):2678–2686. doi: 10.1002/cncr.11845. [DOI] [PubMed] [Google Scholar]
- 12.Souhami L, Seiferheld W, Brachman D, et al. Randomized comparison of stereotactic radiosurgery followed by conventional radiotherapy with carmustine to conventional radiotherapy with carmustine for patients with glioblastoma multiforme: report of Radiation Therapy Oncology Group 93-05 protocol. International Journal of Radiation Oncology Biology Physics. 2004;60(3):853–860. doi: 10.1016/j.ijrobp.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 13.Kong D-S, Lee J-I, Park K, Jong HK, Lim D-H, Nam D-H. Efficacy of stereotactic radiosurgery as a salvage treatment for recurrent malignant gliomas. Cancer. 2008;112(9):2046–2051. doi: 10.1002/cncr.23402. [DOI] [PubMed] [Google Scholar]
- 14.Harsh GR, Levin VA, Gutin PH, Seager M, Silver P, Wilson CB. Reoperation for recurrent glioblastoma and anaplastic astrocytoma. Neurosurgery. 1987;21(5):615–621. doi: 10.1227/00006123-198711000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Mandl ES, Dirven CMF, Buis DR, Postma TJ, Vandertop WP. Repeated surgery for glioblastoma multiforme: only in combination with other salvage therapy. Surgical Neurology. 2008;69(5):506–509. doi: 10.1016/j.surneu.2007.03.043. [DOI] [PubMed] [Google Scholar]
- 16.Dirks P, Bernstein M, Muller PJ, Tucker WS. The value of reoperation for recurrent glioblastoma. Canadian Journal of Surgery. 1993;36(3):271–275. [PubMed] [Google Scholar]
- 17.Skeie BS, Enger PØ, Brøgger J, et al. Gamma knife surgery versus reoperation for recurrent glioblastoma multiforme. World Neurosurgery. 2012;78(6):658–669. doi: 10.1016/j.wneu.2012.03.024. [DOI] [PubMed] [Google Scholar]
- 18.Patel M, Siddiqui F, Jin J-Y, et al. Salvage reirradiation for recurrent glioblastoma with radiosurgery: radiographic response and improved survival. Journal of Neuro-Oncology. 2009;92(2):185–191. doi: 10.1007/s11060-008-9752-9. [DOI] [PubMed] [Google Scholar]
- 19.Binello E, Green S, Germano IM. Radiosurgery for high-grade glioma. Surgical Neurology International. 2012;3(supplement 2):118–126. doi: 10.4103/2152-7806.95423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clavier JB, Voirin J, Kehrli P, Noël G. Systematic review of stereotactic radiotherapy for high-gliomas. Cancer Radiothérapie: Journal de La Société Française de Radiothérapie Oncologique. 2010;14(8):739–754. doi: 10.1016/j.canrad.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 21.Combs SE, Widmer V, Thilmann C, Hof H, Debus J, Schulz-Ertner D. Stereotactic radiosurgery (SRS): treatment option for recurrent glioblastoma multiforme (GBM) Cancer. 2005;104(10):2168–2173. doi: 10.1002/cncr.21429. [DOI] [PubMed] [Google Scholar]
- 22.Pouratian N, Crowley RW, Sherman JH, Jagannathan J, Sheehan JP. Gamma Knife radiosurgery after radiation therapy as an adjunctive treatment for glioblastoma. Journal of Neuro-Oncology. 2009;94(3):409–418. doi: 10.1007/s11060-009-9873-9. [DOI] [PubMed] [Google Scholar]
- 23.Cho KH, Hall WA, Gerbi BJ, Higgins PD, McGuire WA, Clark HB. Single dose versus fractionated stereotactic radiotherapy for recurrent high-grade gliomas. International Journal of Radiation Oncology Biology Physics. 1999;45(5):1133–1141. doi: 10.1016/s0360-3016(99)00336-3. [DOI] [PubMed] [Google Scholar]
- 24.Hsieh PC, Chandler JP, Bhangoo S, et al. Adjuvant gamma knife stereotactic radiosurgery at the time of tumor progression potentially improves survival for patients with glioblastoma multiforme. Neurosurgery. 2005;57(4):684–692. [PubMed] [Google Scholar]
- 25.Villavicencio AT, Burneikiene S, Romanelli P, et al. Survival following stereotactic radiosurgery for newly diagnosed and recurrent glioblastoma multiforme: a multicenter experience. Neurosurgical Review. 2009;32(4):417–424. doi: 10.1007/s10143-009-0212-6. [DOI] [PubMed] [Google Scholar]
- 26.Masui K, Cloughesy TF, Mischel PS. Review: molecular pathology in adult high-grade gliomas: from molecular diagnostics to target therapies. Neuropathology and Applied Neurobiology. 2012;38(3):271–291. doi: 10.1111/j.1365-2990.2011.01238.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shrieve DC, Alexander E, Wen PY, et al. Comparison of stereotactic radiosurgery and brachytherapy in the treatment of recurrent glioblastoma multiforme. Neurosurgery. 1995;36(2):275–284. doi: 10.1227/00006123-199502000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Combs SE, Edler L, Rausch R, Welzel T, Wick W, Debus J. Generation and validation of a prognostic score to predict outcome after re-irradiation of recurrent glioma. Acta Oncológica. 2013;52(1):147–152. doi: 10.3109/0284186X.2012.692882. [DOI] [PubMed] [Google Scholar]
- 29.Cuneo KC, Vredenburgh JJ, Sampson JH, et al. Safety and efficacy of stereotactic radiosurgery and adjuvant bevacizumab in patients with recurrent malignant gliomas. International Journal of Radiation Oncology Biology Physics. 2012;82(5):2018–2024. doi: 10.1016/j.ijrobp.2010.12.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ulm AJ, Friedman WA, Bradshaw P, Foote KD, Bova FJ. Radiosurgery in the treatment of malignant gliomas: the University of Florida experience. Neurosurgery. 2005;57(3):512–517. doi: 10.1227/01.neu.0000170560.13251.99. [DOI] [PubMed] [Google Scholar]
- 31.Larson DA, Gutin PH, McDermott M, et al. Gamma knife for glioma: selection factors and survival. International Journal of Radiation Oncology Biology Physics. 1996;36(5):1045–1053. doi: 10.1016/s0360-3016(96)00427-0. [DOI] [PubMed] [Google Scholar]
- 32.Koga T, Maruyama K, Tanaka M, et al. Extended field stereotactic radiosurgery for recurrent glioblastoma. Cancer. 2012;118(17):4193–4200. doi: 10.1002/cncr.27372. [DOI] [PubMed] [Google Scholar]
- 33.Sirin S, Oysul K, Surenkok S, et al. Linear accelerator-based stereotactic radiosurgery in recurrent glioblastoma: a single center experience. Vojnosanitetski Pregled. 2011;68(11):961–966. doi: 10.2298/vsp1111961s. [DOI] [PubMed] [Google Scholar]
- 34.Chamberlain MC, Barba D, Kormanik P, Shea WM. Stereotactic radiosurgery for recurrent gliomas. Cancer. 1994;74:1342–1347. doi: 10.1002/1097-0142(19940815)74:4<1342::aid-cncr2820740426>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 35.Hall WA, Djalilian HR, Sperduto PW, et al. Stereotactic radiosurgery for recurrent malignant gliomas. Journal of Clinical Oncology. 1995;13(7):1642–1648. doi: 10.1200/JCO.1995.13.7.1642. [DOI] [PubMed] [Google Scholar]
- 36.Kondziolka D, Flickinger JC, Bissonette DJ, Bozik M, Lunsford LD. Survival benefit of stereotactic radiosurgery for patients with malignant glial neoplasms. Neurosurgery. 1997;41(4):776–785. doi: 10.1097/00006123-199710000-00004. [DOI] [PubMed] [Google Scholar]
- 37.Mahajan A, McCutcheon IE, Suki D, et al. Case-control study of stereotactic radiosurgery for recurrent glioblastoma multiforme. Journal of Neurosurgery. 2005;103(2):210–217. doi: 10.3171/jns.2005.103.2.0210. [DOI] [PubMed] [Google Scholar]
- 38.Biswas T, Okunieff P, Schell MC, et al. Stereotactic radiosurgery for glioblastoma: retrospective analysis. Radiation Oncology. 2009;4, article 11 doi: 10.1186/1748-717X-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Torok JA, Wegner RE, Mintz AH, Heron DE, Burton SA. Re-irradiation with radiosurgery for recurrent glioblastoma multiforme. Technology in Cancer Research and Treatment. 2011;10(3):253–258. doi: 10.7785/tcrt.2012.500200. [DOI] [PubMed] [Google Scholar]
- 40.Maranzano E, Anselmo P, Casale M, et al. Treatment of recurrent glioblastoma with stereotactic radiotherapy: long-term results of a mono-institutional trial. Tumori. 2011;97(1):56–61. doi: 10.1177/030089161109700111. [DOI] [PubMed] [Google Scholar]
- 41.Park K-J, Kano H, Iyer A, et al. Salvage gamma knife stereotactic radiosurgery followed by bevacizumab for recurrent glioblastoma multiforme: a case-control study. Journal of Neuro-Oncology. 2012;107(2):323–333. doi: 10.1007/s11060-011-0744-9. [DOI] [PubMed] [Google Scholar]