Abstract
Posteromedial tarsal tunnel syndrome is a disorder affecting the tibial nerve or its branches. Diagnosis is established on the basis of physical examination and can be confirmed by electrophysiological evidence. However, diagnostic imaging is always required to identify the possible site of compression. High-resolution ultrasound (US) is playing an increasingly important role in the study of the nerves thanks to a series of advantages over magnetic resonance imaging, such as lower costs and widespread availability, high spatial resolution, fast examination using axial scans, dynamic and comparative studies, possibility of carrying out a study with the patient in the standing position, US Tinel sign finding, and the contribution of color/power Doppler US. We present the results obtained in a series of 81 patients who underwent US imaging between 2008 and 2013 due to posteromedial tarsal tunnel syndrome.
Keywords: Tarsal tunnel, Tibial nerve, Ultrasound
Riassunto
La sindrome del tunnel tarsale posteriore-mediale è una sofferenza del nervo tibiale o di un suo ramo. La diagnosi è clinica e può essere confermata dall’elettrofisiologia, ma un’indagine con imaging è sempre necessaria per trovare l’elemento di compressione. L’ecografia ad alta risoluzione sta giocando un ruolo sempre più importante per lo studio dei nervi, per i diversi vantaggi rispetto alla risonanza magnetica: costo e disponibilità, risoluzione spaziale, esplorazione rapida mediante tecnica di scansione assiale, dinamica e comparativa, possibilità di uno studio con paziente in piedi, segno di Tinel ecografico, contributo del Doppler.
Introduction
Posteromedial tarsal tunnel syndrome is a disorder affecting the tibial nerve or its branches: the medial plantar nerve, the lateral plantar nerve, the medial calcaneal nerve, the motor branch to the abductor muscle of the fifth toe and/or the inferior calcaneal nerve (Fig. 1). This disorder is less frequent and diagnosis is far more complex than that of carpal tunnel syndrome. The etiology of posteromedial tarsal tunnel syndrome varies and the disease may affect different regions and any of the nerve branches.
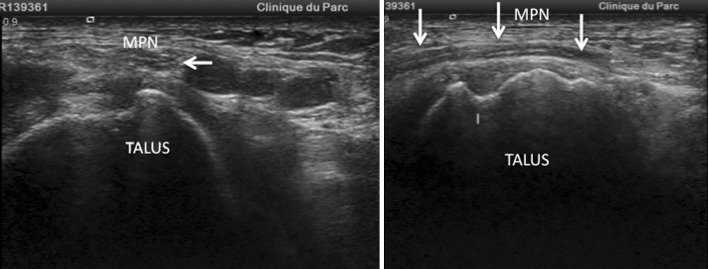
Fig. 1.
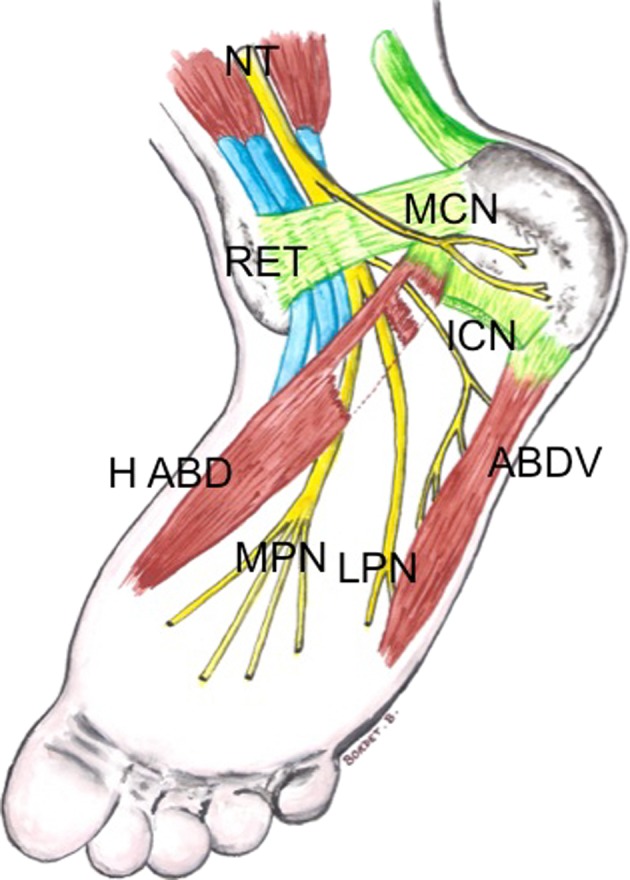
Schematic anatomy of the tarsal tunnel located below the flexor retinaculum (RET) and under the abductor hallucis muscle (H ABD). The tibial nerve (NT) gives rise to a collateral branch, the medial calcaneal nerve (MCN), which is superficial, before it divides into two terminal branches: the medial plantar nerve (MPN) and the lateral plantar nerve (LPN). The inferior calcaneal nerve (ICN) also referred to as the motor branch to the abductor muscle of the fifth toe (ABD V) arises from the lateral plantar nerve at the level of division of the tibial nerve. It travels under the abductor hallucis muscle and under the arch
Diagnosis is established on the basis of physical examination and can be confirmed by electrophysiological evidence. However, diagnostic imaging is always required to identify the site of compression. Magnetic resonance imaging (MRI) is a valid technique for assessing the peripheral nerves, including those in the tarsal tunnel [1, 2], but high-resolution ultrasound (US) is playing an increasingly important role in the study of the nerves thanks to several advantages over MRI:
Lower costs and widespread availability,
Superior spatial resolution compared to MRI (Fig. 2),
Faster examination using axial scans (elevator technique) [3],
Dynamic and comparative studies,
The patients can be studied in the standing position [4],
Positive US Tinel sign can be detected using the probe,
Color/power Doppler US, particularly useful in patients with vascular disorders.
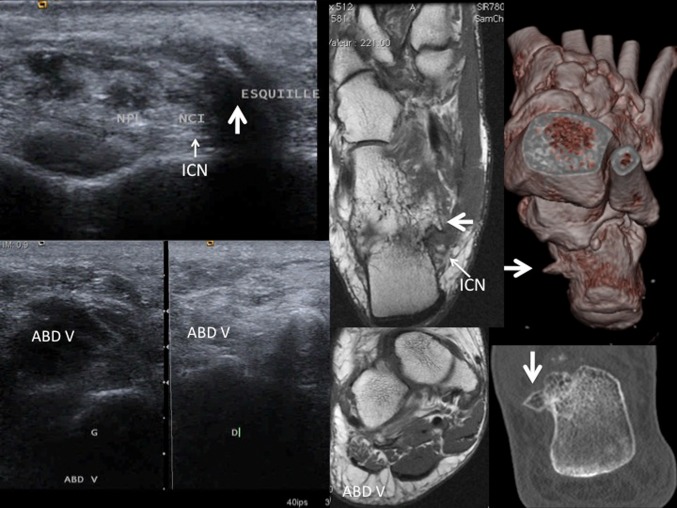
Fig. 2.
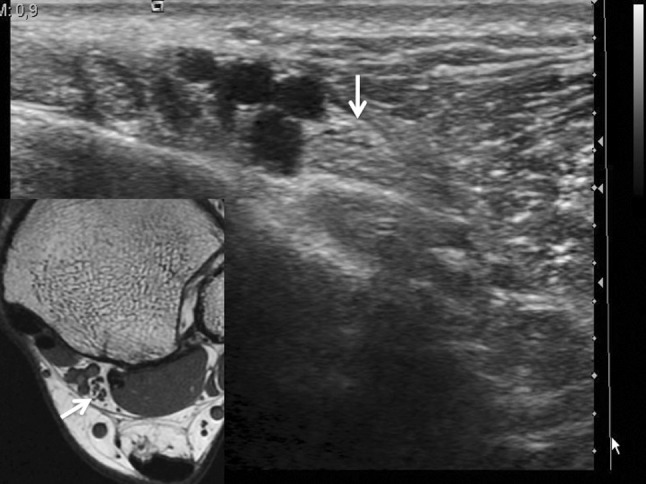
Axial section of the proximal tarsal tunnel showing the tibial nerve (white arrows): correlation between MRI and US imaging
The role of US in this disorder has been pointed out by several authors [2, 4, 5], but to our knowledge, there is only one study of a series of 17 patients reported in the literature, published by Nagaoka in 2005 [6].
The present paper describes the normal US anatomy of the tarsal tunnel as illustrated also in a previous publication [4] and presents the results obtained in a series of 81 patients who underwent US imaging between 2008 and 2013 due to posteromedial tarsal tunnel syndrome.
Physical and complementary examinations
Patients with this disorder present with pain, paresthesia, hypoesthesia, hyperesthesia, muscle cramps or numbness affecting the heel and/or the sole of the foot, and the symptoms may spread to the toes. The location of the symptoms may suggest which nerve branch is affected. Pain in the heel or ankle suggests that the medial calcaneal nerve and the motor branch abductor of the fifth toe are affected. Pain in the medial border of the foot and medial toes suggests that the medial plantar nerve is affected, whereas pain in the lateral border of the foot and the lateral toes suggests that the lateral plantar nerve is affected [7].
These symptoms mainly occur while walking, during exercise, and at night when the patient is at rest. The movements of dorsiflexion and eversion of the foot can also cause the symptoms [8]. The US Tinel sign may be detected using prolonged pressure or tapping with the probe. The symptoms can be reproduced by applying local compression using a tourniquet for the measurement of pressure, thereby increasing the local venous pressure and causing local ischemia [8]. In severe cases, there may be motor involvement, such as loss of power during plantar or toe flexion.
Physical examination may also reveal a possible deformity of the foot such as varus or valgus deformity, which may cause pain while the patient is at rest and during walking due to stretching of the nerve [7].
Tarsal tunnel syndrome is one of the most common causes of heel pain. If US imaging does not reveal a “classic” etiology, typically an inflammatory condition of the plantar fascia, the tarsal tunnel should be explored. The foot may also be affected by a combination of disorders involving the plantar fascia and the motor branch abductor of the fifth toe as this condition is the cause of 15–20 % of cases of heel and/or ankle pain in young patients [9].
Electromyography is always carried out to evaluate the function of the nerves. However, a negative outcome does not exclude possible disorders. Electromyography furthermore allows detection of polyneuritis and radicular neuropathy.
In posteromedial tarsal tunnel syndrome, the diagnostic procedure begins with a traditional X-ray examination for the detection of possible static foot disorders and bone injuries caused by fractures, exostosis or talocalcaneal synostosis. The patient should be referred to MRI and US imaging only after X-ray examination.
Anatomy and US anatomy
The tarsal tunnel is a fibrous osseous tunnel situated posteriorly and inferiorly to the medial malleolus, and it presents a proximal and a distal floor [4, 9]. The proximal retromalleolar floor is limited by the flexor retinaculum and contains the flexor tendons, the posterior tibial tendon, the flexor digitorum longus, the flexor hallucis longus, and the tibial neurovascular bundle (Fig. 3).
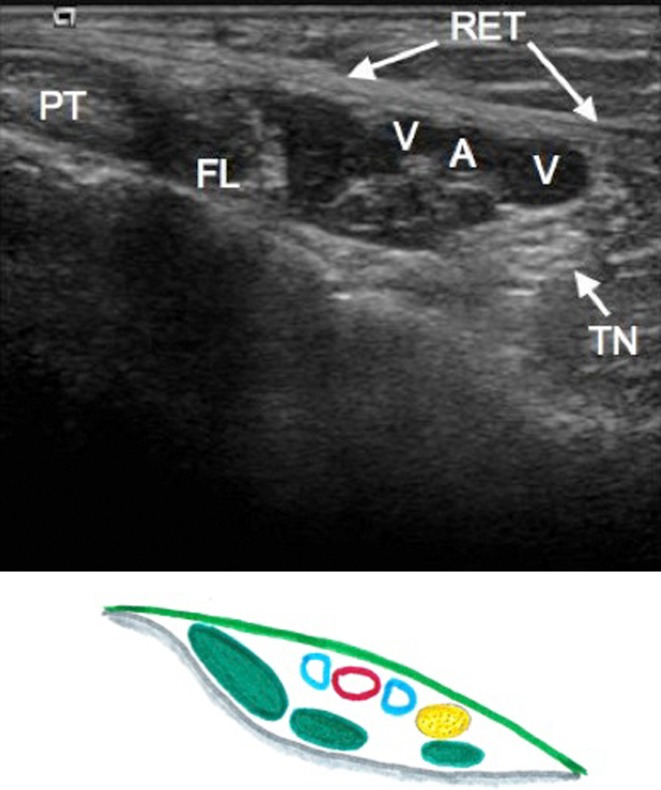
Fig. 3.
US anatomy of the proximal tarsal tunnel, axial scan. PT posterior tibial tendon, FL flexor digitorum longus tendon, TN tibial nerve, RET flexor retinaculum, A posterior tibial artery, V tibial veins
The distal floor is located below the malleolus, at the medial plantar side. It lies between the abductor hallucis muscle and its arch, which are located superficially, and the deep quadratus plantae muscle. The distal portion contains branches of the plantar vessels and tibial plantar nerves.
The tibial nerve gives rise to a collateral branch, the medial calcaneal nerve, and its two terminal branches, the medial and lateral plantar nerves. The location where the plantar branches of the tibial nerve divide may vary. Sometimes division occurs in the proximal tarsal tunnel, but more often it occurs at the entrance to the inferior distal tarsal tunnel under the abductor hallucis muscle. At US imaging, both plantar nerves are visible in the distal tarsal tunnel under the abductor hallucis muscle. The lateral plantar nerve is situated postero-laterally and the medial plantar nerve is situated antero-medially (Fig. 4).
Fig. 4.
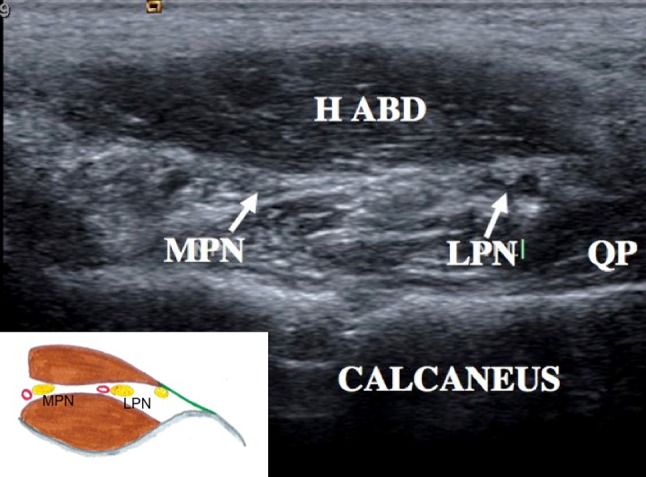
US anatomy of the distal tarsal tunnel, axial scan. LPN lateral plantar nerve, MPN medial plantar nerve, QP quadratus plantae muscle, H ABD abductor hallucis muscle
The medial calcaneal nerve is small. It arises from the tibial nerve, often before its entry into the tarsal tunnel. It may arise also from the proximal portion of the tibial tunnel and it travels superficially to the abductor hallucis muscle. It innervates the posterior portion of the medial aspect of the calcaneus and the posterior third of the fat pad of the foot. It is difficult to visualize it at US imaging, but it may be identified at MRI thanks to the fat signal.
The inferior calcaneal nerve, also referred as the motor branch of the abductor to the fifth toe (called Baxter’s nerve or the first branch of the lateral plantar nerve in Anglo-Saxon medical literature), arises from the lateral plantar nerve or the tibial nerve at the level of division into the terminal plantar branches. The inferior calcaneal nerve travels under the abductor hallucis muscle and crosses its fascia (Fig. 5); it subsequently passes under the calcaneus between the calcaneus and the flexor digitorum brevis near the enthesis of the plantar fascia and joins the abductor of the fifth toe, which it innervates. This nerve can be visualized at US imaging right from the origin and can be traced under the abductor hallucis muscle and below the fascia. Visualization of this nerve is more difficult after it has crossed the plantar bundle because of the attenuation of the echoes due to the plantar fat pad. The inferior calcaneal nerve also innervates the periosteum of the large calcaneal tuberosity.
Fig. 5.
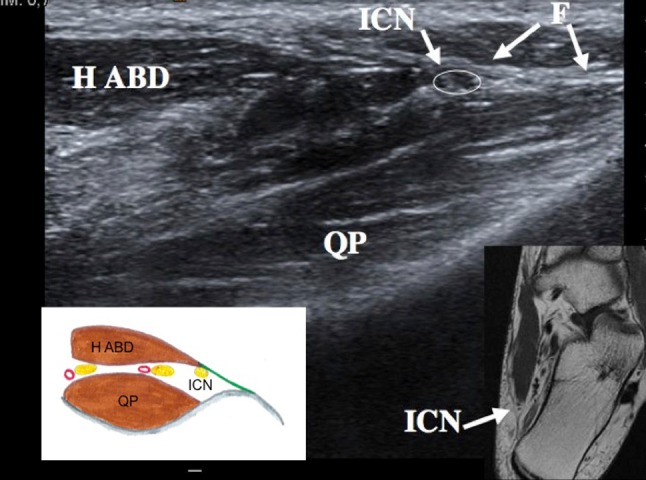
US anatomy of the distal tarsal tunnel, axial scan. ICN inferior calcaneal nerve, also referred to as the nerve of the abductor digiti minimi muscle, H ABD abductor hallucis muscle and fascia (F)
US imaging
To obtain a reliable outcome, US imaging of the tarsal tunnel and the peripheral nerves must be performed by an experienced operator, who is familiar with normal and pathological US findings. Top-of-the-range US equipment including a high frequency probe is required.
Gray-scale and color Doppler US imaging starts with axial scans of the proximal and distal tarsal tunnel on the medial side of the foot arch and with a systematic study of the tibial nerve, the two plantar nerves and the inferior calcaneal nerve. The patient should be in the lateral decubitus position.
US Tinel test should be carried out by tapping over the nerve to elicit symptoms, as a positive US Tinel sign is suggestive of a positive diagnosis of posteromedial tarsal tunnel syndrome, particularly when the symptoms are linked to possible compression elements. In some cases, the US Tinel sign may be the only positive sign in the absence of compression elements or neuropathy. In case of pathological findings, the nerve should be further studied in the longitudinal plane to confirm previous findings.
US examination also includes a systematic study with the patient in the standing position during limb loading [4] using axial scans of the proximal tunnel and the distal tunnel. The following two conditions should be investigated:
Compression caused by bone disorders linked to static foot disorders, including compression by the medial process of the talus in valgus flat foot, which leads to pushing and stretching of the nerves;
Dilation of the plantar veins in the distal tarsal tunnel (vein diameter >5 mm) when the patient is in the standing position. Venous dilation should be suspected in the presence of positive US Tinel sign caused by compression of the veins using the US probe or if the symptoms improve when the patient is wearing Class II support soks.
US can detect muscle atrophy and significant fatty infiltration linked to a neurogenic pathology. In this case, comparison with the muscles of the contralateral foot is essential. If the patient has a disease affecting the nerve to the abductor of the fifth toe, a comparative assessment of the abductor muscles of the fifth toes may show atrophy and hyperechoic appearance of the affected foot and thereby confirm the diagnosis.
Etiology
Tarsal tunnel syndrome occurs for numerous reasons; the frequency of the different etiologies varies in the literature and a compression element is detected between 60 and 80 % [8].
Tarsal tunnel syndrome may be caused by idiopathic conditions or for traumatic reasons (bone diseases, injuries to the ligament, thickening of the flexor retinaculum, hematoma, fibrosis, and iatrogenic damage to the nerves), tendon disorders (tendinopathy and flexor tenosynovitis), supernumerary muscles (accessory soleus muscle, medial fibulocalcaneal muscle, and particularly accessory flexor digitorum muscle [16]) or muscle hypertrophy (abductor hallucis muscle [17] or flexor hallucis muscle of the toes). The syndrome may be caused also by bone disorders (talocrural and subastragalar arthritis and arthropathy with talocalcaneal synovitis and synostosis [10], sustentaculum tali [11], sequelae of fracture, change in static foot posture), expansive lesions (ganglion cysts, particularly epineural ganglions [12], soft tissue tumors including intracanal lipomas and tumors of the nerves), vascular disorders (kinking of the tibial artery, venous aneurysms, and varicose plantar veins particularly in the distal tarsal tunnel, which is commonly reported in the literature) [2, 8, 13, 14].
Patient population
From January 2008 to September 2013, 81 patients underwent US examination. All patients presented with clinical evidence of posteromedial tarsal tunnel syndrome; 53 women and 28 men; mean age 50.5 years (range 19–78 years).
In 18 patients, the disease was localized in the proximal tarsal tunnel, in 47 patients in the distal tarsal tunnel, and 16 patients had the disease in both the proximal and the distal tarsal tunnel.
The outcome of electromyography was available in 25 patients, positive in only 13 cases.
Etiology
The aim of US imaging is to identify the cause of posteromedial tarsal tunnel syndrome and confirm clinical diagnosis. In our experience (Table 1), US outcome is rarely normal in these patients, and in the vast majority of cases, a compression element is detected. Some patients present multiple etiologies.
Table 1.
Distribution of disorders in the 81 patients; some had more than one pathology
| Negative outcome of US imaging | N = 5 |
| Neuropathy | N = 7 |
| Varicose plantar veins | N = 21 |
| Aneurism of the tibial veins | N = 2 |
| Thrombophlebitis | N = 2 |
| Kinking of the tibial artery | N = 1 |
| Hypertrophy of the abductor hallucis muscle | N = 1 |
| Accessory soleus muscle | N = 1 |
| Epineural ganglion cyst | N = 6 |
| Arthrogenic/tenosynovial cyst | N = 3 |
| Schwannoma | N = 3 |
| Vascular malformation | N = 1 |
| Lipoma of the distal tarsal tunnel | N = 5 |
| Static foot disorder | N = 17 |
| Fractures and bone disorders | N = 3 |
| Iatrogenic injury | N = 6 |
| Accessory flexor digitorum longus muscle | N = 5 |
US outcome: normal or neuropathy (n = 12)
US did not reveal compression elements or neuropathy in five patients. Of these patients, one had polyneuritis, one patient resulted positive to US Tinel test performed on the lateral plantar nerve, and one patient felt pain at the inferior calcaneal nerve, although US revealed no abnormality.
Neuropathy without compression element was found in seven patients: affecting the tibial nerve in four patients, the lateral plantar nerve in one patient, the medial plantar nerve in one patient, and the inferior calcaneal nerve in one patient. Neuropathy was characterized by hypoechoic thickening of the nerve. Diagnosis can be confirmed by measuring the axial surface of the nerve and compare with that of the proximal and distal portion of the nerve or to that of the contralateral foot (Fig. 6). Unlike the carpal tunnel syndrome, there is no reference value in tarsal tunnel syndrome, which is quite logical because the level of compression varies and the disease can affect different portions of the tibial nerve as well as its collateral branches.
Fig. 6.
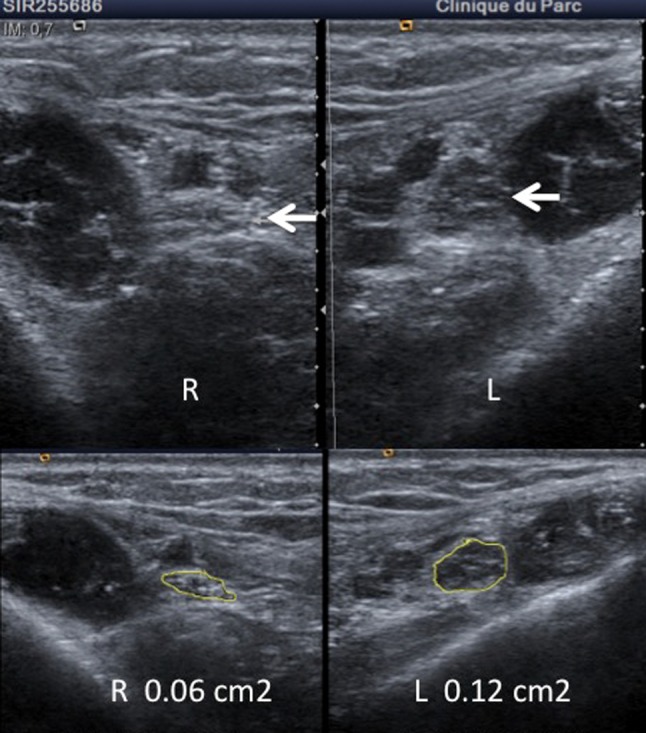
US, axial scans of the proximal tarsal tunnel showing tibial nerve neuropathy of the left foot; the axial surface measures 12 mm2 as compared to the right foot: 6 mm2
Vascular disorders (n = 26)
The most frequently diagnosed disorder in this patient population was varicose plantar veins in the distal tarsal tunnel, detected in 21 patients. Venous dilation increased with the patient in the standing position. The veins are considered as dilated when they measure >5 mm in diameter, are tortuous and with signs of venous stasis (Fig. 7). Echopalpation of the veins may trigger the symptoms. This venous disease has been described in the literature over the years [13, 14] and it seems to be the most common cause of tarsal tunnel syndrome; it was detected in 13 % of patients in a literature review examining 186 cases [8].
Fig. 7.
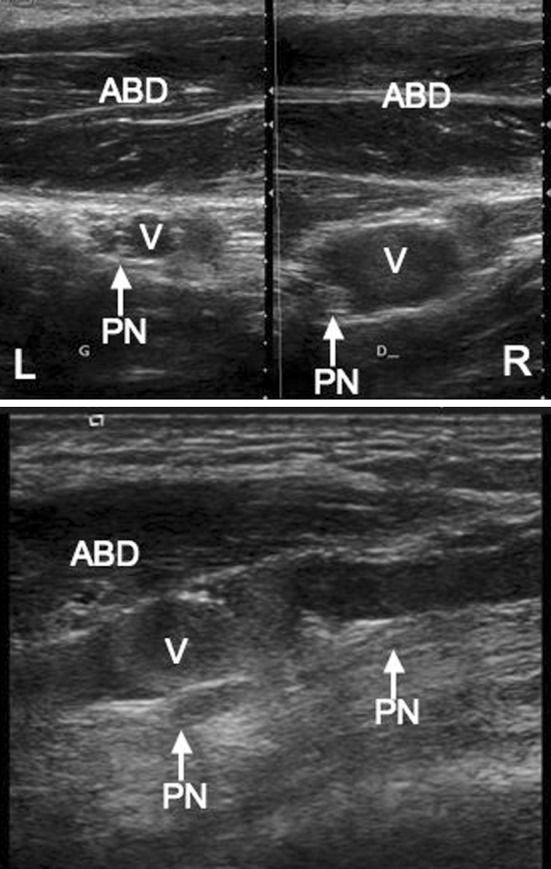
US, axial scan of the distal tarsal tunnel showing a tortuous varicose plantar vein in the right foot (V), and the medial plantar satellite nerve (PN). The left foot is normal
In our series, two patients presented aneurysm of the tibial vein while one patient had kinking of the tibial artery, which trapped the nerve thereby causing the symptoms; this etiology has already been described in the literature [15].
One patient had a thrombosed plantar vein associated with pain and very strong signs of neuropathy affecting the plantar nerves. One patient presenting with acute heel pain (Fig. 8) had thrombophlebitis in a satellite vein of the inferior calcaneal nerve in the tarsal tunnel.
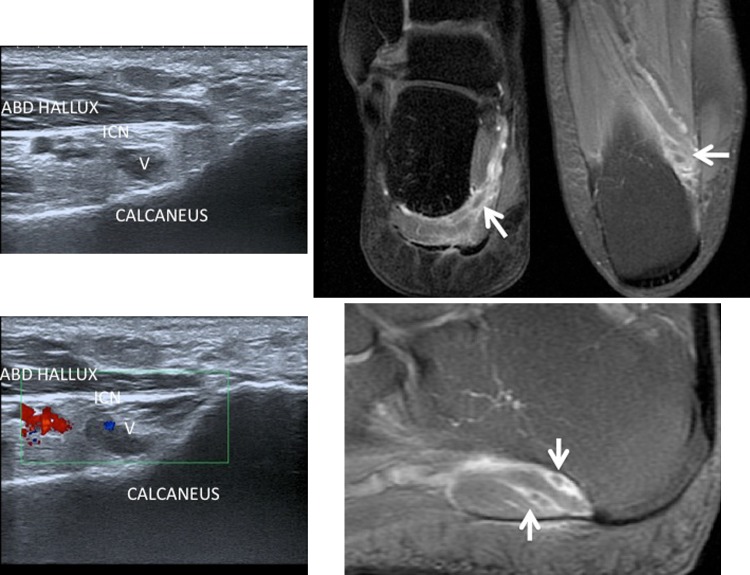
Fig. 8.
Sharp heel pain in a women receiving estrogen–progestin oral contraceptive. US axial scan of the distal tarsal tunnel and MRI in three orthogonal planes show vein thrombosis (V) in a satellite vein of the inferior calcaneal nerve (ICN). By courtesy of Dr. Franck Lapègue
Muscle disorders (n = 7)
According to the literature [16], the accessory flexor muscle of the toes is a common cause of posterior tarsal tunnel syndrome. In our series, this disorder was detected in five patients (Fig. 9). This accessory muscle travels beneath the flexor retinaculum in the tarsal tunnel, satellite of the tibial nerve and the two plantar nerves and ends on the quadratus plantae muscle. Also, this muscle is identifiable at US imaging.
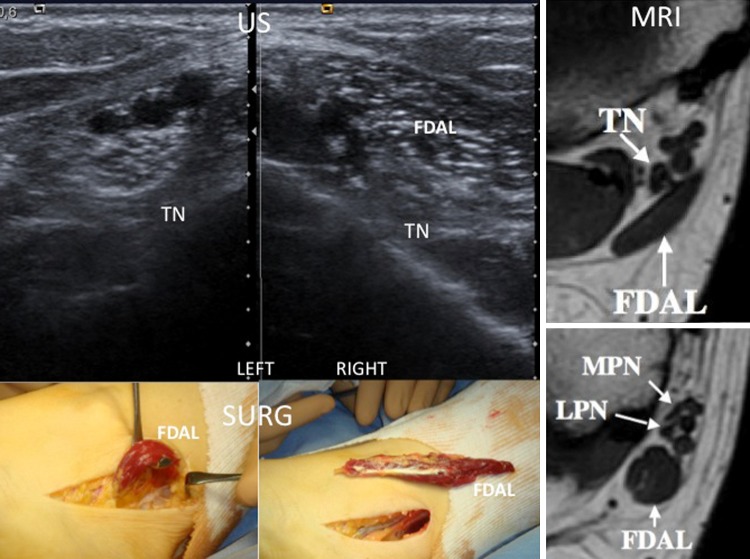
Fig. 9.
Posteromedial tarsal tunnel syndrome of the right foot during limb loading. US imaging and MRI show a flexor digitorum accessorius longus muscle of the toes (FDAL) in the tarsal tunnel, satellite of the tibial nerve (TN), and plantar nerves (LPN, MPN). After surgical removal of the accessory muscle, symptoms disappeared
One patient presented with compression of an accessory soleus muscle (Fig. 10) and one patient presented significant hypertrophy of the abductor hallucis muscle (Fig. 11), which was confirmed by comparison with the contralateral foot. This condition is already reported in the literature [17].
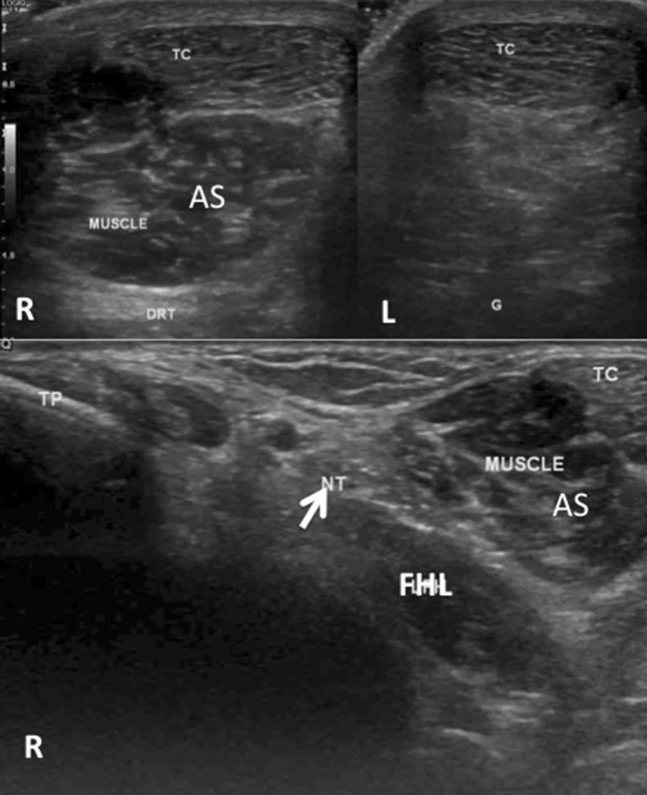
Fig. 10.
Posteromedial tarsal tunnel syndrome of the right foot during limb loading. Voluminous accessory soleus muscle (AS) in contact with the tibial nerve (arrow) in the proximal tarsal tunnel of the right foot. There is no accessory muscle in the left foot
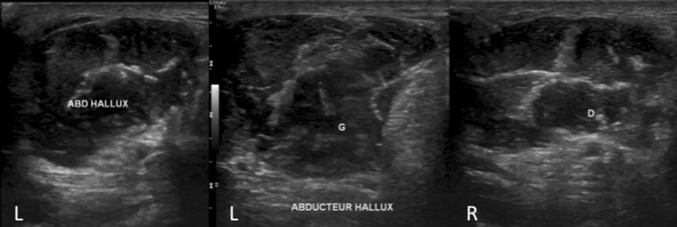
Fig. 11.
Posteromedial tarsal tunnel syndrome of the left foot. Comparative coronal imaging of the distal tarsal tunnel shows significant hypertrophy of the abductor hallucis muscle of the left foot causing plantar nerve entrapment
Cysts (n = 9)
The most common cystic disease is epineural ganglion cyst, which was detected in 6 of the 81 patients. These cysts may affect the tibial and plantar nerves (Figs. 12, 13) and also arise in the posterior subtalar compartment, but the origin is not always clear. In one patient, an epineural ganglion cyst was identified arising from the distal portion of the lateral plantar nerve causing substantial neurogenic damage to the intrinsic muscles. MRI showed an edema in addition to severe muscle atrophy due to denervation. MRI evidenced more accurately than US imaging the epineural ganglion cyst arising from the Lisfranc joint.
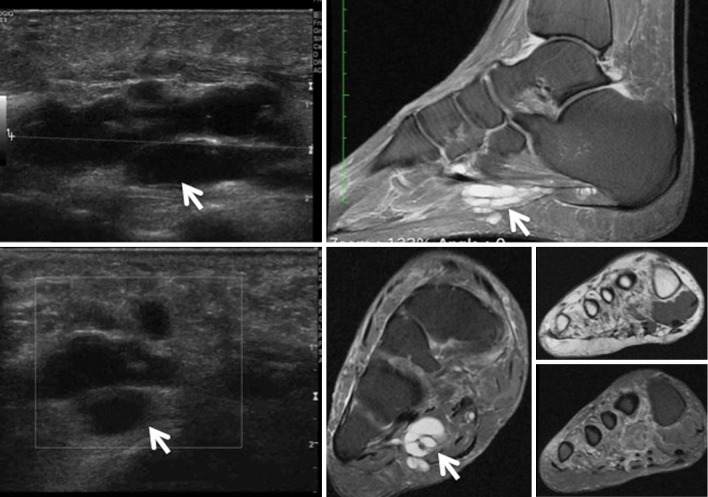
Fig. 12.
Lateral plantar pain. US and MRI show a large epineural ganglion cyst adjacent to the plantar nerve, edema and atrophy due to denervation of the intrinsic muscles innervated by the lateral plantar nerve: lumbrical, interosseous, abductor hallucis, flexor muscles, and the opponent of the fifth toe
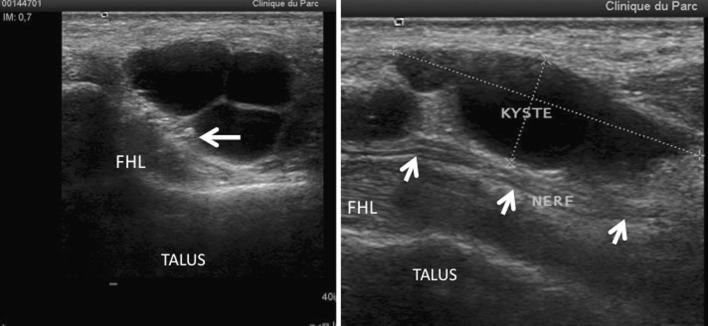
Fig. 13.
US shows a large epineural ganglion cyst adjacent to the tibial nerve (arrows)
One patient had a cyst of the tenosynovial sheath of the flexor muscles and two patients had arthrosynovial cysts of the posterior subtalar recess.
Tumors (n = 9)
Neurogenic tumor was the cause of symptoms in three patients. In two patients, the tumor affected the tibial nerve and in one patient, the inferior calcaneal nerve. One patient had angiomatous capillary–venous malformation developed in the tarsal tunnel.
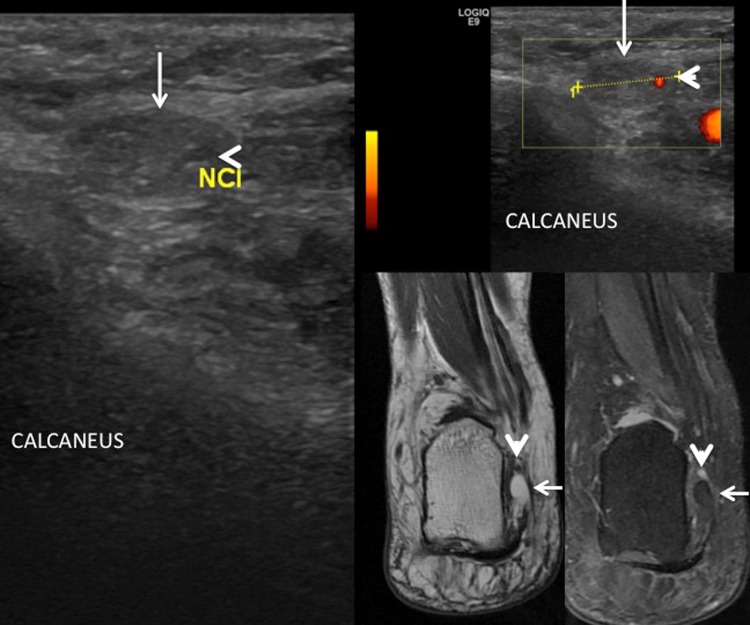
Five patients had lipoma in the distal tarsal tunnel with consequent compression of the inferior calcaneal nerve (Fig. 14); the etiology of this lesion is described in the literature [18]. These patients presented with ankle pain, pain in the posterior portion of the foot and sometimes a palpable, painful swelling. US imaging showed a hypo- or hyperechoic nodular lesion, and the lipomatous nature of the lesion was therefore difficult to diagnose at US. In these five patients, diagnosis was confirmed by MRI.
Fig. 14.
Patient with heel pain, a painful swelling, and positive US Tinel sign on the lower calcaneal nerve. Axial US scan of the distal tarsal tunnel shows a hypoechoic lesion near the inferior calcaneal nerve (arrowheads). MRI, T1-weighted scans, and T1-weighted scans with fat suppression after gadolinium injection show the lipomatous nature of the lesion
Static foot disorders and bone diseases (n = 20)
Valgus flat foot is the leading cause of posteromedial tarsal tunnel syndrome. According to the literature [8], the etiology is very common and in our series this abnormality was revealed in 16 patients (Fig. 15). Sensitivity of US imaging increases when the examination is performed with the patient in the standing position. In this way, the medial process of the talus comes into contact with the distal portion of the tibial nerve and the plantar nerves, which are compressed. Physical examination and radiography during limb loading confirmed the diagnosis.
Fig. 15.
Posteromedial tarsal tunnel syndrome. US imaging performed with the patient in the standing position; axial scans show compression of the medial plantar nerve (MPN) exerted by the medial process of the talus
Tarsal tunnel syndrome was caused by fracture of the calcaneus (Fig. 16) in two patients and by exostosis on the sustentaculum tali in one patient. In these three patients, computed tomography (CT) was performed to confirm the bone disease.
Fig. 16.
Heel pain resulting from calcaneal fractures. US imaging shows the bones (arrow) in contact with the inferior calcaneal nerve (ICN) in the distal tarsal tunnel. The image reveals atrophy and fatty infiltration of the abductor muscle of the fifth toe (ABD V). CT shows a bone fragment on the medial surface of the heel. MRI reveals contact between the bone fragment and fibrosis entrapping the nerve thereby confirming atrophy and fatty infiltration of the abductor muscle of the fifth toe
One patient had talocalcaneal synostosis, a disease which is well described in the literature [10]. Diagnosis was established at US imaging [6], which showed a prominent bone structure and absence of the posterior subtalar joint space.
Iatrogenic disorders (n = 6)
Four patients had surgical injury to the tibial nerve or its branches: in one patient after surgical treatment of the posterior junction, in three patients after treatment of posterior subtalar arthrodesis. US imaging showed the nerve lesion and its location (Fig. 17).
Fig. 17.
Plantar numbness after surgery on the posterior junction. US shows interruption of the tibial nerve (arrows)
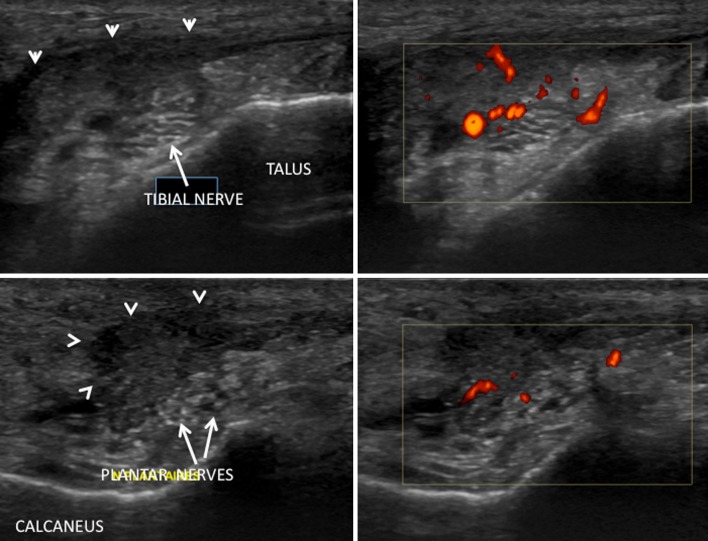
Two patients presented with pain in the area of the tibial nerve: in one patient linked to compression by a hematoma (after removal of a lipoma of the posteromedial border of the foot) and in one patient linked to extensive post-surgical fibrosis after surgical treatment of posteromedial tarsal tunnel syndrome (Fig. 18).
Fig. 18.
Recurrent posteromedial tarsal tunnel syndrome after decompression. US axial scan and power Doppler US of the proximal and distal tarsal tunnel show a large mass of vascularized scar tissue at power Doppler US (arrowheads) in contact with the tibial nerve and the plantar nerves
Particular cases (n = 5)
Four patients presented with a combination of heel pain, inferior calcaneal nerve pain, and enthesopathy of the plantar fascia.
One patient presented with clinical signs and symptoms of posteromedial tarsal tunnel syndrome, but the pain was caused by a schwannoma of the tibial nerve located in the distal third of the leg. The lesion was detected at US imaging and confirmed at MRI (Fig. 19).
Fig. 19.
Posteromedial tarsal tunnel syndrome. At US imaging, the tarsal tunnel appears normal, but a schwannoma (arrows) is detected on the tibial nerve in the distal third of the leg. Diagnosis was confirmed by MRI
MRI
In 27 patients, MRI was performed in addition to US imaging. MRI was performed in patients whose US outcome was normal, in case of diagnostic discordance between the clinician and the US operator, if US imaging did not provide a clear diagnosis and particularly in patients with suspected expansive lesions. In 17 of these patients, MRI confirmed US outcome.
In two patients, MRI provided additional information on neurogenic myopathy, which was not identified at US imaging: one patient had edema as the only sign of denervation of the quadratus plantae muscle; one patient had an epineural ganglion cyst arising in the lateral plantar nerve with muscular atrophy of the intrinsic plantar muscles innervated by the lateral plantar nerve.
MRI delivers better quality images of the soft tissues than US imaging, and MRI was therefore useful in the characterization of the fatty nature of the lipomas located in the distal tarsal tunnel.
MRI outcome was normal in nine patients. In five of these patients, US imaging revealed no pathology, but in four patients US imaging revealed pathologies, which were not visible on MRI: in one patient, US revealed medial compression of the talus bone linked to valgus flat foot, in one patient tibial vein aneurysm, in one patient the presence of varicose plantar veins and in one patient isolated neuropathy of the tibial nerve identified through comparison with the contralateral foot.
Surgical treatment
To date, 23 of the 81 patients have undergone surgery and there has been no case of discrepancy between US imaging and surgical findings, which confirmed nerve compression evidenced at US imaging.
Patients with posteromedial tarsal tunnel syndrome are referred to surgical treatment only in severe cases, particularly if the patient presents with debilitating symptoms, if electromyography shows significant changes or a compression element is detected at US imaging. In other cases, medical treatment may be appropriate, including orthotic devices and/or podiatric treatment if the patient has static foot disorders, support soks in case of varicose veins or infiltration of cortisone derivatives.
Limitations of US imaging
Like all other diagnostic imaging methods, US imaging presents some limitations. The method is operator dependent and requires a relationship of mutual trust between the patient’s general physician and the US operator. The images transmitted to the clinician should be understandable and sufficiently explained. Transmission of commented video files may also improve the quality of information provided to the clinician and improve comprehension.
Unlike MRI, US imaging cannot detect muscle edema caused by denervation. Diagnosis of atrophy and fatty infiltration of the muscles is more difficult on US than MRI and requires comparison with the contralateral foot. In case of soft tissue mass, US is not sufficiently accurate and must be supported by MRI using intravenous injection of gadolinium. US imaging provides information on the morphology, but not on the severity of the neuropathy and the impact on the nerve, and it cannot evaluate the function of the nerve. On rare occasions, the usefulness of US imaging may furthermore be reduced, e.g., in patients with limited echogenicity or in very obese patients.
Conclusions
US imaging generally permits a reliable study of the posteromedial tarsal tunnel, and in the present study, US revealed compression elements in 84 % of cases. In the absence of compression elements, US imaging can detect neuropathy and/or US Tinel sign, which may confirm clinical diagnosis. The US technique has numerous well-known advantages: high spatial resolution, faster examination using axial scans (“elevator technique”), and the possibility to study patients during limb loading, which is very useful in the diagnosis of varicose plantar veins and in the investigation of pain due to nerve injury associated with static foot disorders. These two disorders frequently occurred in the present patient population (21 and 17 cases, respectively). Other common causes were cysts including epineural ganglion cysts (six patients) and the presence of an accessory flexor digitorum longus muscle of the toes (five patients). The present series highlights the importance of a systematic evaluation of the distal tarsal tunnel, which is the site of the disease in more than 50 % of cases.
In US and MRI evaluation of heel pain, the tarsal tunnel must be studied systematically, particularly if no other cause has been detected, including plantar fascia disorders, which may be associated with the neuropathy.
Acknowledgments
Conflict of interest
Olivier Fantino declares that he has no conflict of interest related to this study.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients.
Animal studies
The study described in this article did not include any procedures involving animals.
References
- 1.Erickson SJ, Quinn SF, Kneeland JB, Smith JW, Johnson JE, Carrera GF, et al. MR imaging of the tarsal tunnel and related spaces: normal and abnormal findings with anatomic correlation. AJR Am J Roentgenol. 1990;155:323–328. doi: 10.2214/ajr.155.2.2115260. [DOI] [PubMed] [Google Scholar]
- 2.Kerr R, Frey C. MR imaging in tarsal tunnel syndrome. J Comput Assist Tomogr. 1991;15(2):280–286. doi: 10.1097/00004728-199103000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Martinoli C, Bianchi S, Gandolfo N, Valle M, Simonetti S, Derchi LE. US of nerve entrapments in osteofibrous tunnel of the upper and lower limbs. Radiographics. 2000;20(6):1818. doi: 10.1148/radiographics.20.6.g00no001818. [DOI] [PubMed] [Google Scholar]
- 4.Fantino O, Coillard JY, Borne J, Bordet B. Ultrasound of the tarsal tunnel: normal and pathological imaging features. J Radiol. 2011;92(12):1072–1080. doi: 10.1016/j.jradio.2011.03.026. [DOI] [PubMed] [Google Scholar]
- 5.Demondion X, Boutry N, Bry R, Khalil C, Jaspart M, Cotten A. Tibial nerve entrapment syndromes at the ankle and foot level: imaging assessment. Rev Rhum. 2007;74:409–414. doi: 10.1016/j.rhum.2007.02.002. [DOI] [Google Scholar]
- 6.Nagaoka M, Matsuzaki H. Ultrasonography in tarsal tunnel syndrome. J Ultrasound Med. 2005;24(8):1035–1040. doi: 10.7863/jum.2005.24.8.1035. [DOI] [PubMed] [Google Scholar]
- 7.Bouysset M, Coury F, Labarre-Vila A, Damiano J, Gerbay B, Tebib J. Considérations sur le syndrome du canal tarsien postéromédial et les formes apparentées (lésions du nerf tibial et de ses branches) Méd Chir Pied. 2012;28:69–72. doi: 10.1007/s10243-012-0334-3. [DOI] [Google Scholar]
- 8.Lau JT, Daniels TR. Tarsal tunnel syndrome: a review of the literature. Foot Ankle Int. 1999;20:201–209. doi: 10.1177/107110079902000312. [DOI] [PubMed] [Google Scholar]
- 9.Demondion X (2011) Anatomie normale des nerfs du pied, les sièges du conflit. In: Le pied, GETROA-GEL OPUS XXXVIII. Sauramps Médical, Montpellier p 243–52
- 10.Lee MF, Chan PT, Chau LF, Yu KS. Tarsal tunnel syndrome caused by talocalcaneal coalition. Clin Imaging. 2002;26:140–143. doi: 10.1016/S0899-7071(01)00355-2. [DOI] [PubMed] [Google Scholar]
- 11.Garchar DJ, Lewis JE, DiDomenico LA. Hypertrophic sustentaculum tali causing a tarsal tunnel syndrome: a case report. J Foot Ankle Surg. 2001;40:110–112. doi: 10.1016/S1067-2516(01)80053-3. [DOI] [PubMed] [Google Scholar]
- 12.Fujita I, Matsumoto K, Minami T, Kizaki T, Akisue T, Yamamoto T. Tarsal tunnel syndrome caused by epineural ganglion of the posterior tibial nerve: report of 2 cases and review of the literature. J Foot Ankle Surg. 2004;43(3):185–190. doi: 10.1053/j.jfas.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 13.Pasku DS, Karampekios SK, Kontakis GM, Katonis PG. Varicosities as an etiology of tarsal tunnel syndrome and the significance of tinel’s sign: report of two cases in young men and a review of the literature. J Am Podiatr Med Assoc. 2009;99(2):144–147. doi: 10.7547/0980144. [DOI] [PubMed] [Google Scholar]
- 14.Gould N, Alvarez R. Bilateral tarsal tunnel syndrome caused by varicosities. Foot Ankle. 1983;3:290–292. doi: 10.1177/107110078300300510. [DOI] [PubMed] [Google Scholar]
- 15.Kim E, Childers MK. Tarsal tunnel syndrome associated with a pulsating artery: effectiveness of high-resolution ultrasound in diagnosing tarsal tunnel syndrome. J Am Podiatr Med Assoc. 2010;100(3):209–212. doi: 10.7547/1000209. [DOI] [PubMed] [Google Scholar]
- 16.Wittmayer BC, Freed L. Diagnosis and surgical management of flexor digitorum accessorius longus-induced tarsal tunnel syndrome. J Foot Ankle Surg. 2007;46:484–487. doi: 10.1053/j.jfas.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 17.Ghosh SK, Raheja S, Tuli A. Potential sites of compression of tibial nerve branches in foot: a cadaveric and imaging study. Clin Anat. 2013;26(6):768–779. doi: 10.1002/ca.22203. [DOI] [PubMed] [Google Scholar]
- 18.Chen WS. Lipoma responsible for tarsal tunnel syndrome. Apropos of 2 cases. Rev Chir Orthop Reparatrice Appar Mot. 1992;78(4):251–254. [PubMed] [Google Scholar]