Abstract
Peroneal tendon injuries are common also due to the recent increase in sports participants involved in amateur activities. Clinical evaluation generally provides a diagnosis, but diagnostic imaging is often required to confirm a clinical suspicion and make correct management decisions. Ultrasound (US) imaging is the method of choice in the study of peroneal tendon injuries due to the high resolution of the images and the possibility of performing dynamic studies. US is furthermore non-invasive and inexpensive and provides the possibility of performing US-guided steroid infiltration of the tendon sheath or the surrounding tissues. The present paper will address the normal anatomy of the peroneal tendons and related structures, US imaging techniques and the various conditions and injuries which may affect this anatomic region. Also more expensive imaging techniques, such as computed tomography and magnetic resonance imaging, will be mentioned as well as their indications; however, they are required only in rare cases in which diagnosis remains uncertain or for pre-operative assessment.
Keywords: Peroneal tendons, Ankle, Ultrasound
Riassunto
Le lesioni dei tendini peronei sono di frequente riscontro, anche per il recente aumento dell’attività sportiva amatoriale. La valutazione clinica generalmente permette la diagnosi, ma spesso è necessario uno studio di imaging per confermare l’ipotesi clinica e per instaurare una terapia corretta. L’ecografia è indagine di prima istanza per lo studio dei tendini peronei, in virtù dell’alta risoluzione, non invasività, bassi costi, possibilità di realizzare uno studio dinamico, oltre alla possibilità di effettuare, sotto controllo real time, delle infiltrazioni della guaina tendinea o nei tessuti peritendinei. Nel presente articolo vengono esaminati l’anatomia normale dei tendini peronei e delle strutture ad essi connesse, la tecnica di studio ecografica e le varie patologie. Si fa cenno alla realizzazione di altre tecniche di imaging più costose (TC, RM) e alle loro indicazioni, peraltro limitate ai rari casi in cui la diagnosi resti incerta con l’ecografia, alla valutazione pre-operatoria.
Introduction
Injuries to the peroneal tendons are frequently encountered in clinical practice [1, 2]. This can to a certain extent be explained by the recent rise in middle-aged and elderly sports participants involved in amateur activities. Clinical evaluation of these lesions generally suggests the diagnosis, but an imaging study is often performed to confirm clinical suspicion and to obtain more information such as location and extent of the injury, muscle and tendon tropism as well as evaluation of the adjacent anatomical structures as this is essential for establishing a correct therapy.
Ultrasound (US) imaging is the method of choice in the study of peroneal tendon injuries as it is non-invasive and inexpensive, due to the high resolution of the images and the possibility of performing dynamic studies [2–5]. Dynamic US imaging performed during active or passive mobilization of the ankle or by applying pressure with the probe provides more diagnostic information than static imaging techniques [4]. A further advantage of US imaging lies in the possibility of performing US-guided steroid infiltration of the tendon sheath or the surrounding tissues [6].
US imaging is often carried out in addition to plain film X-ray examination, which is widely available and easy to perform. These two imaging techniques are well integrated as plain film X-ray permits an accurate evaluation of the bones, whereas US has difficulty penetrating bone. Other more expensive imaging techniques, such as computed tomography (CT) and magnetic resonance imaging (MRI), are required only in the rare cases in which diagnosis remains uncertain or in pre-operative assessment.
Normal anatomy and biomechanics
The peroneal tendon complex includes the peroneus brevis tendon, peroneus longus tendon, peroneus brevis muscle, peroneus longus muscle, common synovial sheath, superior retinaculum and inferior retinaculum (2). This complex includes also the os peroneum, a small sesamoid bone which is often present in the context of the peroneus longus tendon [7, 8] (Fig. 1).
Fig. 1.
The peroneal tendon complex. a Anatomy diagram; b computed tomography scan (sagittal image reconstruction); c nuclear magnetic resonance (proton density-weighted sagittal scan). 1 Peroneus longus tendon, 2 peroneus brevis tendon, a superior retinaculum, b inferior retinaculum, black arrow os peroneum
The peroneal muscles are located in the lateral compartment of the leg externally to the fibula and are innervated by the superficial peroneal nerve. The peroneus longus muscle is the most superficial and the longest; it originates from the head and upper third of the lateral aspect of the fibula and from the lateral condyle of the tibia, crural fascia and the surrounding intermuscular septa. The muscle bundles run vertically down and continue in the long superficial lamina of the tendon that covers the peroneus brevis muscle. The latter is located deeper than the peroneus longus muscle; it arises from the cortical bone of the distal two-thirds of the fibula and the intermuscular septum. It continues distally in a flat tendon which arises from the anterior portion of the muscle. The myotendinous junction of the peroneus longus muscle is located cranially to the peroneus brevis muscle.
Right above the malleolus, the peroneus longus tendon is located superficially and laterally to the myotendinous junction of the peroneus brevis tendon. Near the peroneal malleolus, the peroneus longus tendon runs posterolaterally to the peroneus brevis tendon (Fig. 2a).
Fig. 2.
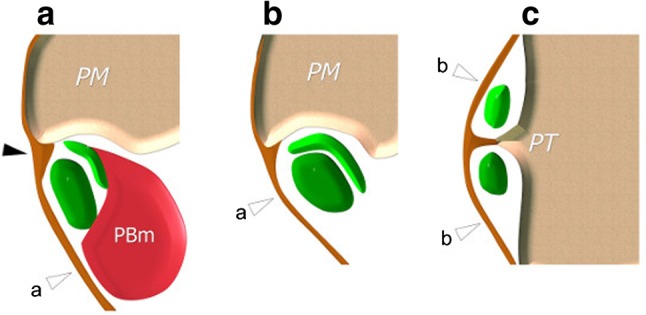
The peroneal tendon complex. Schematic representation perpendicular to the axis of the peroneal tendons, at the a superior malleolus, b malleolus, c inferior malleolus. 1 peroneus longus tendon, 2 peroneus brevis tendon, PBM peroneus brevis muscle, a superior retinaculum, b inferior retinaculum, PM peroneal malleolus, PT peroneal tubercle, black arrowhead fibrocartilage lip, a superior retinaculum, b inferior retinaculum
At the malleolus, the two tendons are reflected on the anterior aspect of the external malleolus where they pass in an osteofibrous groove located anterior to the malleolus and posteriorly to the superior retinaculum [3, 4, 9, 10] (Fig. 2b). The bone morphology of the posterior aspect of the malleolus may vary. In most cases it is more or less concave, and this enables it to limit the instability of the peroneal tendons. However, it may also be flat or in some cases even convex.
The stabilizing effect of the groove is increased by the presence of a triangular fibrocartilagenous “lip” in the axial plane, adherent to the lateral cortex of the malleolus. The superior retinaculum inserts on this meniscus; it is a robust fibrous band that partially surrounds the peroneal tendons. This forms an osteofibrous tunnel (the superior osteofibrous tunnel) which prevents anterior dislocation of the peroneal tendons during forced joint eversion. A common synovial sheath—formed by a visceral layer adherent to the tendons and a wall layer adherent to the adjacent structures—surrounds the tendons within the tunnel, thereby facilitating their gliding within the sheath.
In the inframalleolar region, the two tendons run along the lateral aspect of the calcaneus with the peroneus longus tendon lying superiorly to the peroneus brevis tendon. The external aspect of the calcaneus has two protuberances: the peroneal tubercle and the retrotrochlear eminence.
The peroneal tubercle is present in 90 % of the population [11] and may vary in morphology and size [12] (Fig. 2c). It is often slightly protruding and sometimes hypertrophied, thereby forming a kind of bone tunnel that surrounds part of one of the peroneal tendons. The peroneal brevis tendon and the peroneal longus tendon lie above and below the peroneal tubercle where they are stabilized by a second retinaculum (inferior retinaculum) which arises from the lateral aspect of the calcaneus and inserts on the apex of the tubercle [9, 10].
A second osteofibrous tunnel (referred to as the inferior osteofibrous tunnel) arises here. Distally to this tunnel the peroneal tendons separate. The peroneal brevis tendon continues straight on to insert on the base of the fifth metatarsal bone. The peroneal longus tendon crosses a bone groove of the inferolateral aspect of the cuboid bone and reaches the sole of the foot to insert on the base of the first and second metatarsal bones and the first cuneiform bone. At the cuboid bone groove, there is often a small sesamoid bone called the os peroneum. The common synovial sheath of the peroneal tendons splits in the inframalleolar region to surround the two diverging tendons. Under physiological conditions, the sheath contains a small amount of synovial fluid which facilitates the gliding of the two tendons in the two osteofibrous tunnels [3, 4].
From a biomechanical point of view, the peroneal longus tendon plantar flexes, abducts and rotates externally to the foot and also stabilizes the arch of the foot emphasizing its concavity. The peroneal brevis tendon helps to abduct and externally rotate the foot.
US imaging technique
Before starting the examination, the US operator should collect the patient’s medical history focusing on possible recent or past injuries, mechanical versus inflammatory ankle pain and possible previous surgery.
The examination is carried out with the patient in the supine position and the hip slightly flexed and in internal rotation, the knee flexed about 30° and the medial aspect of the foot resting on the bed [3, 4]. The distal portion of the peroneal longus tendon at the ball of the foot is studied with the patient in the prone position.
A dynamic study is carried out with the patient in the supine position. It is performed by placing a rigid support under the Achilles tendon and inviting the patient to move the ankle and foot in the various planes. The examination starts with axial imaging of the cranial portion of the muscles extending to the distal portion of the tendons. The axial scans provide a panoramic view and information about the myotendinous junction as well as the relationship with the surrounding anatomical structures (Figs. 3–5). The US probe should be held so that the US beam is always perpendicular to the major axis of the tendon to avoid false hypoechoic patterns due to anisotropy. The peroneal tendons can be studied simultaneously in the supramalleolar region, whereas they have to be studied separately in the inframalleolar region because of their different location. After rotating the probe by 90°, the tendons can be studied using longitudinal scans.
Fig. 4.
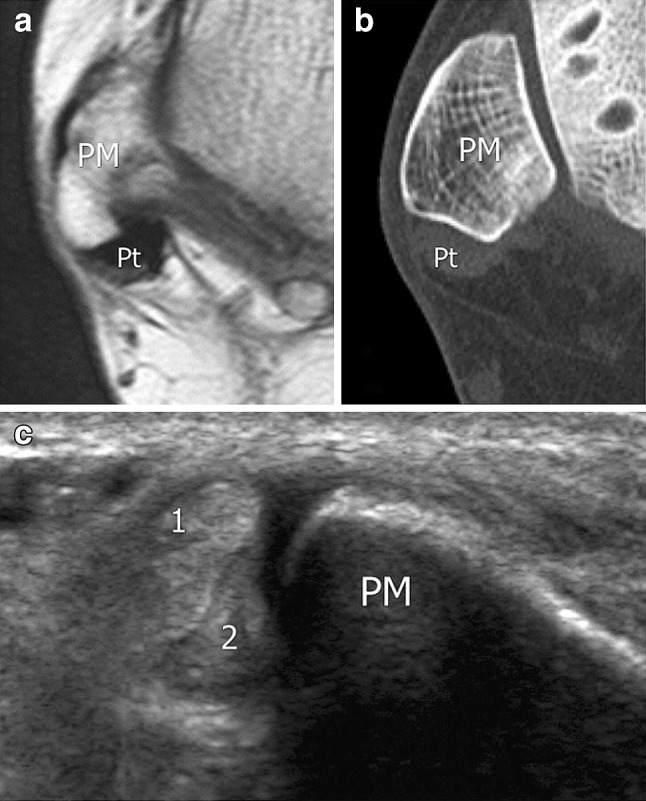
The peroneal tendon complex. Axial scans obtained at the medial malleolus using a nuclear magnetic resonance; b computed tomography; c US imaging. 1 peroneus longus tendon, 2 peroneus brevis tendon, PM peroneal malleolus, Pt peroneal tendons
Fig. 3.
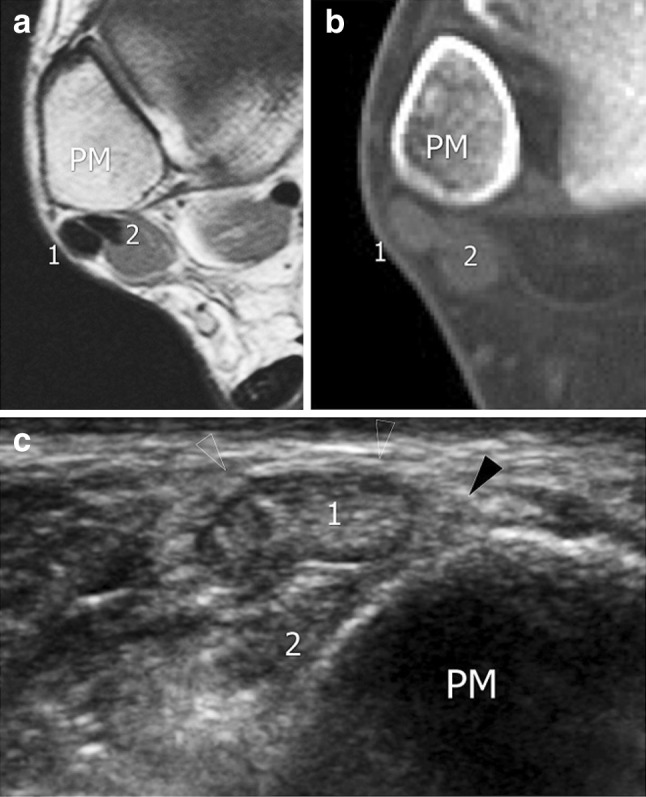
The peroneal tendon complex. Axial scans obtained at the superior malleolus using. a nuclear magnetic resonance; b computed tomography; c US imaging. 1 peroneus longus tendon, 2 peroneus brevis tendon, PM peroneal malleolus
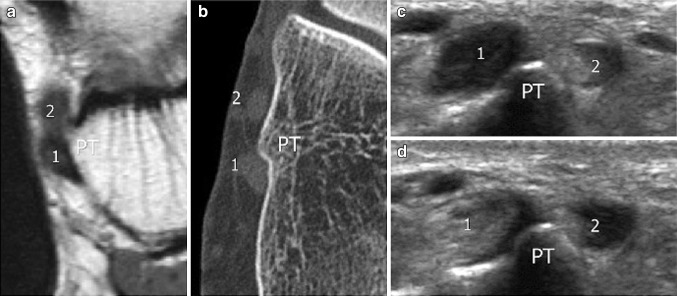
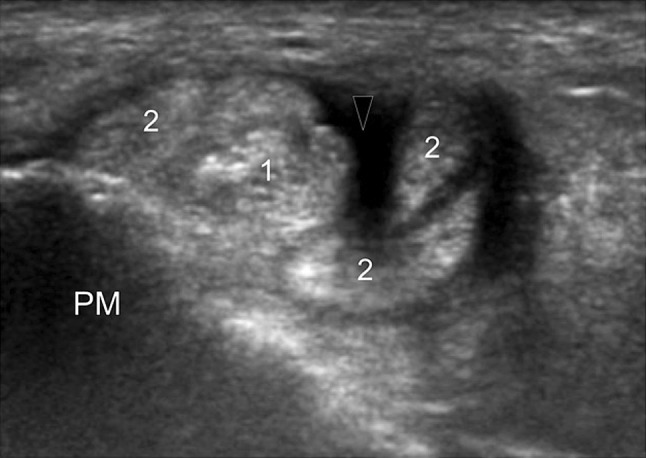
Fig. 5.
The peroneal tendon complex. Axial scans obtained at the medial inframalleolar tunnel using a nuclear magnetic resonance; b computed tomography; c, d US imaging. 1 peroneus longus tendon, 2 peroneus brevis tendon, PT peroneal tubercle. Note that the appearance of the peroneus tendons varies in c and d as a function of the different angles of the probe
Like other tendons, also the peroneal tendons appear on the US scan as hyperechoic structures with regular margins and a characteristic fibrillar appearance on longitudinal scans.
The synovial sheath is rarely visualized under physiological conditions unless a high-resolution probe is used. The superior retinaculum is studied using oblique or axial scans tracing its course, which varies from person to person. The retinaculum appears as a thin hyperechoic band that inserts anteriorly on the lip of the fibrous meniscus which is generally isoechoic or hyperechoic. The inferior retinaculum is thinner and more difficult to evaluate than the superior retinaculum. The peroneal tubercle is more easily visualized on the US scan, but the anatomy may vary. If the patient has an os peroneum, it will appear as an ovoid hyperechoic structure, but shape, size and morphology will vary. It may been a single bone or present with fragment separation (two or more fragments), with posterior acoustic shadowing.
Anatomical variants
Familiarity with the anatomical variants of the peroneal tendon complex is necessary for a correct interpretation of pathological images [13–15]. The US operator must be able to recognize anatomical variants so as not to confuse them with pathological conditions, but also because certain variants may predispose the patient to tendon instability, inflammation or tear.
The peroneus quartus muscle
The peroneus quartus muscle is the most common accessory muscle of the ankle that is present in 22 % of the population [6]. It generally arises from the peroneus brevis muscle, but its distal insertion varies greatly (peroneus longus tendon or peroneus brevis tendon, the base of the fifth metatarsal bone, the lateral aspect of the calcaneus) (Figs. 6, 7). The morphology of the peroneus quartus muscle, which lies posteriorly to the peroneal tendons, may vary. Sometimes it is a voluminous muscle which continues distally as a short tendon, but it may also be a short muscle that continues as a long tendon.
Fig. 6.
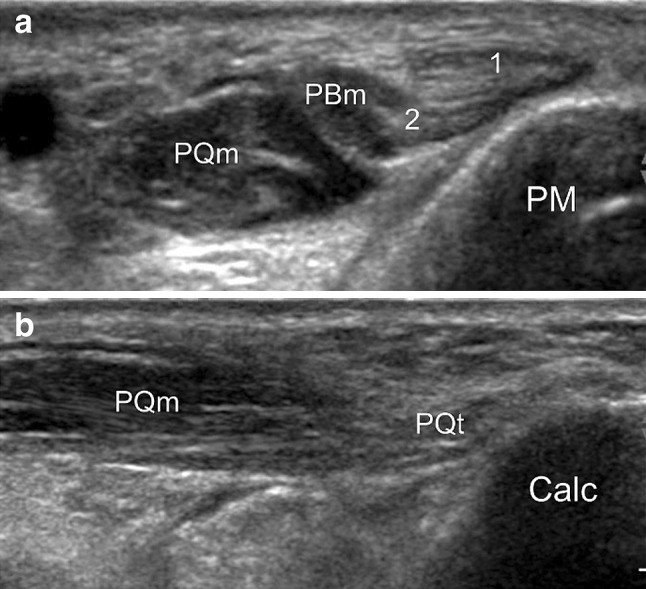
The peroneal tendon complex: the peroneus quartus muscle. US a axial and b longitudinal scans show a peroneus quartus muscle (PQm). The accessory muscle is located posteriorly to the peroneus brevis muscle (PBm). Note in b the short peroneus quartus tendon (PQt) and its insertion on the calcaneus (Calc). 1 peroneus longus tendon, 2 peroneus brevis tendon, PM peroneal malleolus
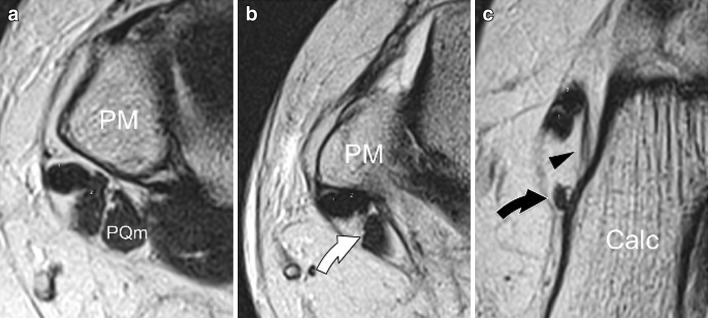
Fig. 7.
The peroneal tendon complex: the peroneus quartus muscle; nuclear magnetic resonance scans obtained in the craniocaudal scan direction show; a peroneus quartus muscle (PQm), b its myotendinous junction (white arrow) and c the distal portion of its tendon (black arrow) which inserts on the lateral aspect of the calcaneus (Calc). 1 peroneus longus tendon, 2 peroneus brevis tendon, PM peroneal malleolus; arrowhead peroneocalcaneal ligament, white arrow myotendinous junction of the peroneus quartus muscle, black arrow peroneus quartus tendon
Most people with a peroneus quartus muscle are asymptomatic. In some there may be signs of tenosynovitis of the peroneal tendons associated with retromalleolar pain and edema. In these cases, inflammatory changes are caused by continuous friction between the tendons in the proximal tunnel. Chronic impingement in addition to inflammatory changes may be responsible for tendon tears [16–18].
The peroneus quartus muscle must be distinguished from the inferior myotendinous junction of the peroneus brevis muscle. Also in this case, the muscle belly of the peroneus brevis muscle tends to enter the proximal peroneal tunnel leading to fissure of the tendon [18]. The distal tendon of the peroneus quartus muscle must also be distinguished from a possible fissure in the peroneus brevis tendon; this tendon can be used for surgical reconstruction of the superior retinaculum of the peroneal tendons [19].
Variants of the calcaneal tubercle
Variations in the shape and size of the peroneal tubercle are frequent, but they rarely cause diseases. The peroneal tubercle is considered hypertrophic when it measures more than 5 mm [14]. In such cases the tubercle can be felt on palpation as a localized swelling at the lateral aspect of the calcaneus, right below the peroneal malleolus. Chronic impingement between a hypertrophic tubercle and the shoes can result in inflammation of the subcutaneous tissue and the soft tissue. The small size of the osteofibrous tunnel associated with hypertrophy of the peroneal tubercle may lead to peroneal tendon impingement resulting in stenosing tenosynovitis [20–22] (Fig. 8).
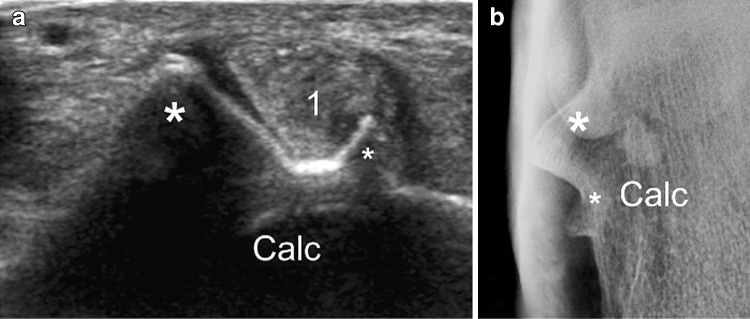
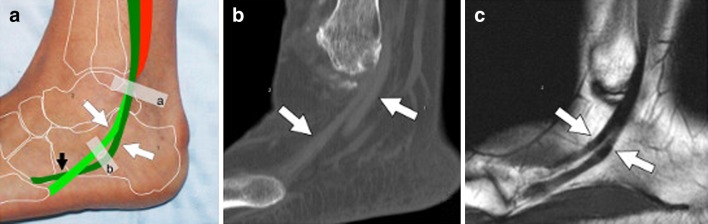
Fig. 8.
The peroneal tendon complex: hypertrophy of the peroneal tubercle. US scan (a) and axial standard X-ray (b) of the calcaneus in a patient with hypertrophy of the peroneal tubercle (PT). The tubercle presents a bifid appearance (asterisks). 1 peroneus longus tendon, Calc calcaneus
Os peroneum
At the cuboid bone groove, the peroneus longus tendon is particularly under stress from a biomechanical point of view as it changes direction and twists the fibers on its own axis. The presence of the small sesamoid bone decreases the local mechanical stress exerted on the tendon.
The os peroneum is present in 20 % of the population and it is bilateral in 60 % of cases [8, 17, 23]. The os peroneum presents different morphologies. It may consist of one bone (of various dimensions and morphology), be bipartite (i.e., divided into two fragments of variable dimensions) which is the most common variant [24], be multipartite (consisting of several fragments of various dimensions) (Fig. 9) or hyperplastic [25].
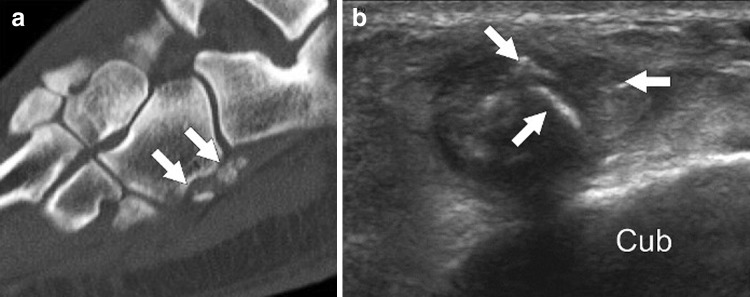
Fig. 9.
Multipartite os peroneum. Computed tomography (sagittal reconstruction) (a) and US coronal oblique scan (b) in a patient with multipartite os peroneum (arrows). The tubercle presents a bifid appearance (asterisks). Note the characteristic sclerotic, quite sharp margins of the bone fragments which are located close to each other near the base of the fifth metatarsal bone. Cub cuboid
Diagnosis may be difficult, if bipartite or multipartite os peroneum is visualized on plain film X-ray in a patients with local pain. In these cases, differential diagnosis will include cortical avulsion fracture of the base of the fifth metatarsal bone or the cuboid bone, calcification of the soft tissues and fracture of the os peroneum. Diagnosis is facilitated by correlation with clinical findings (previous trauma and local tenderness), a careful analysis of the X-ray features of the os peroneum fragments (margins are regular and sclerotic or irregular and ill defined) and their position relative to the base of the fifth metatarsal bone.
In cases where the os peroneum is unusually large, it may squeeze into the osteofibrous tunnel between the cuboid bone and the calcaneus during the movements of the tendon thereby causing pain. This condition can be assessed at dynamic US imaging.
Tendon tear
Peroneal tendon tear rarely occurs due to a direct blunt trauma. These injuries are commonly the result of excessive tension, such as strain, particularly strain on tendons weakened by degenerative (tendinosis) or inflammatory (tenosynovitis) diseases [2, 26–28]. Generally only one tendon is affected, and contemporary injury to both tendons is rare. US imaging is highly effective in the diagnosis of peroneal tendon tear with a sensitivity and specificity of 100 and 85 %, respectively [2].
Peroneal tendon tear is divided into three categories: partial tear, longitudinal fissure and full-thickness tear.
Partial tear
Partial tear is defined as a tear that affects only a small number of tendon fibers. Partial tendon tear is generally observed in the presence of weakening due to degenerative disorders. However, if a healthy tendon is injured as a result of a direct trauma, US imaging will show the normal structure and volume of the tendon, both cranially and distally to the lesion, which is characterized by discontinuity and partial retraction of the torn tendon fibers. The presence of a serosanguineous fluid collection originating from the tendon sheath will facilitate the diagnosis. Pathological changes may be detected along the long axis of the tendon; they may be more evident during dynamic maneuvers, which will allow the US operator to visualize the damaged tendon fibers.
More frequently, partial tears occur in the presence of pre-existing tendon abnormalities usually secondary to functional overload in connection with sports, such as tennis, football, basketball, running, etc., postural defects or overweight. In these cases, recurrent episodes of local microtrauma lead to microlesions in the tendon fibers, which tend to repair by depositing collagen along the axis of the tendon. The tendon appears thickened and heterogeneously hypoechoic with loss of the characteristic internal fibrillar pattern. Partial tears may in such cases be difficult to differentiate from tendon abnormalities. However, the presence of synovial effusion and the use of dynamic imaging may facilitate identification of partial discontinuity of the tendon.
Longitudinal fissures frequently affect the peroneal tendons (Figs. 10, 12). They are lesions of continuity that extend along the major axis of the tendon and may sometimes involve the entire length of the tendon. In that case, the tendon will be completely split into two hemi-tendons. This lesion is seen mainly in patients with anterior intermittent instability of the peroneal tendons at the external malleolus. In such cases, chronic impingement between the tendons and the bone may lead to progressive thinning of the tendons and eventually to longitudinal fissures [2, 26, 27].
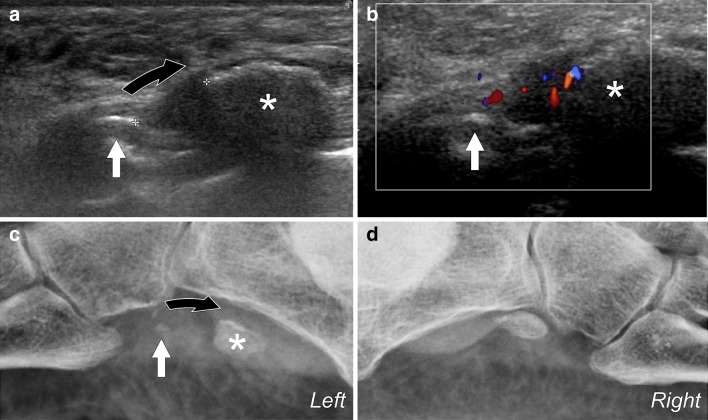
Fig. 10.
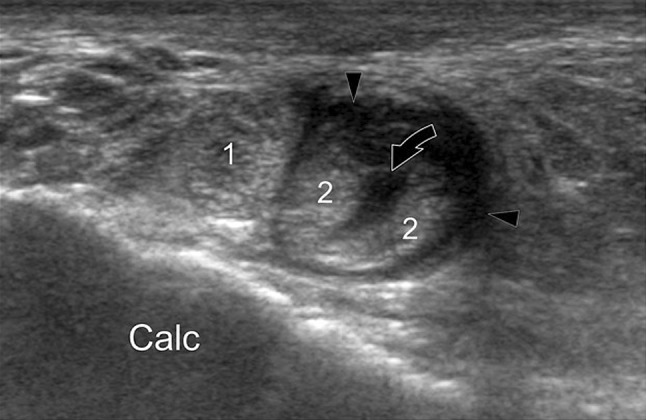
Injury to the peroneal tendons. US coronal oblique scan shows partial-thickness longitudinal fissure of the peroneus brevis tendon (curved arrow) associated with reactive synovial thickening of the tendon sheath (arrowheads). 1 peroneus longus tendon, Calc calcaneus. 1 TPL (peroneus longus tendon); 2 TPB (peroneus brevis tendon), arrowheads associated tenosynovitis, Calc calcaneus
Fig. 12.
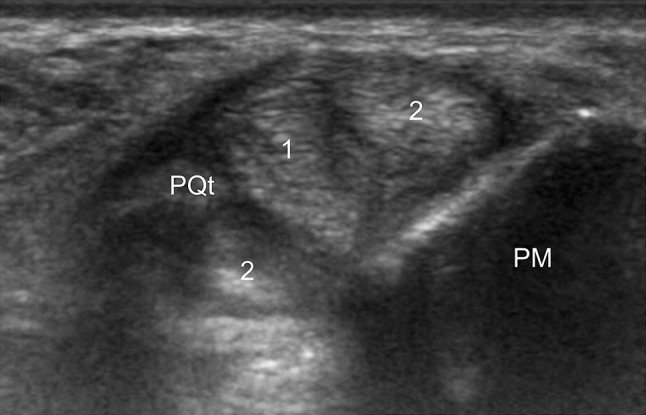
Injury to the peroneal tendons. US axial oblique scan demonstrating full-thickness longitudinal fissure of the peroneus brevis tendon (2). The peroneus longus tendon lies between the two hemi-tendons of the peroneus brevis tendon. Note the presence of an accessory peroneus quartus tendon (PQT). PM peroneal malleolus
The peroneus brevis tendon is most frequently affected in case of instability as it is compressed against the cortical bone by the peroneus longus tendon [16, 29, 30]. This explains why peroneus brevis tendon fissures mainly occur near the apex of the malleolus and why the deep tendon fibers near the cortical bone are involved first, and the superficial fibers only later. In some cases there are multiple longitudinal fissures (Fig. 11). These lesions are visible on US [3] and must be differentiated from the presence of a peroneus quartus tendon [31]. US investigation should include static and dynamic US imaging (flexion, extension, eversion) using short-axis and long-axis scans. It is also useful to exert different pressures using the probe to reveal the possible distance between the damaged tendon fibers.
Fig. 11.
Injury to the peroneal tendons. US axial oblique scan demonstrating multiple full-thickness longitudinal fissures of the peroneus brevis tendon associated with signs of reactive synovial hypertrophy (arrowhead). 1 peroneus longus tendon, PM peroneal malleolus. 1 TPL (peroneus longus tendon), 2 TPB (peroneus brevis tendon); arrowhead tenosynovitis, PM peroneal malleolus
Partial-thickness longitudinal tears can be visualized on US as hypoechoic fissures of the tendon and are generally eccentric (Fig. 10). Short-axis appearance of horseshoe-shaped curving at the superior malleolus suggests tendon fissure in the initial stage and seems to be due to an initial thinning of the tendon with degenerative changes of the central tendon fibers.
A full-thickness longitudinal lesion appears on US as a hypoechoic cleft extending throughout the thickness of the tendon. The lesion most commonly affects the peroneus brevis tendon with the formation of two hemi-tendons which are frequently different in size. US axial scans of the adjacent tissues will show the tendon split at the superior malleolus. The two hemi-tendons are traced up to the medial malleolus where they join in a thickened, hypoechoic and irregular tendon. At the malleolus, the peroneus longus tendon lies between the two hemi-tendons, thereby separating them. In the presence of associated tenosynovitis, US will show thickening of the synovial tendon sheath which may appear hypervascularized on color Doppler and possibly also synovial effusion.
The most common differential diagnosis includes the presence of a peroneus quartus tendon. In that case the tendon presents a regular structure and sharp contours. US permits tracing it from its origin at the accessory muscle to the insertion on the lateral aspect of the calcaneus or the inferior retinaculum. In some cases the presence of an accessory tendon may lead to peroneus brevis tendon fissure (Fig. 12).
Full-thickness tear
Full-thickness tear generally affects only one tendon, but sometimes both tendons are torn. Peroneus brevis tendon injuries do not present characteristics which are different from those of other tendon lesions [32]. However, the presence of an os peroneum may in some cases permit diagnosis of full-thickness tear on the basis of plain film X-ray examination only. The os peroneum is easily visualized on an internal oblique view of the foot near the groove of the cuboid bone at the base of the fifth metatarsal bone [33]. The tear may occur caudally (type 1), at the sesamoid bone (type 2) or distally (type 3) [3].
In type 1 tears, the os peroneum remains in place and appears normal. These injuries are therefore not revealed on plain film X-ray.
Diagnosis of type 2 tears is based on possible fragmentation of the sesamoid bone [23, 33]. If the os peroneum is fractured, the movement of the peroneus longus tendon will progressively retract the proximal fragments leading to diastasis between the fragments.
Peroneus longus tendon tears type 3 are suspected if there is posterior dislocation of the small sesamoid bone, measured as the distance that separates it from the base of the fifth metatarsal bone. Under physiological conditions, the os peroneum is situated about 8–10 mm from the base of the fifth metatarsal bone. US examination permits distinction of the anatomic variants of the os peroneum (hyperplasia, bipartite or multipartite).
Lesion proximal to the os peroneum (type 1)
In type 1 tears, the proximal tendon stump is retracted and surrounded by serosanguineous fluid leaking from the tendon sheath. The os peroneum will be in place, and the distal tendon stump will appear partially lax.
Plain film X-ray examination will be of little help as there is no significant dislocation of the os peroneum. US imaging will show the location of the lesion and the swollen proximal tendon stump, which is hypoechoic and irregular, surrounded by serosanguineous fluid and later by inflammatory tissue which is well demonstrated on color Doppler US.
A dynamic study will confirm the diagnosis and reveal the presence of undamaged tendon fibers, if any. Measurement of the distance between the tendon stumps may facilitate surgical planning.
Lesion at the os peroneum (type 2)
In this case the os peroneum will appear fractured and present two or more bone fragments characterized by irregular margins and surrounded by serosanguineous fluid in various stages of organization (related to the time elapsed between the injury and the examination) (Fig. 13). The bone fragments, which may be of different sizes and morphology, are rarely dislocated immediately after the injury, because some tiny ligaments tie the os peroneum to the adjacent structures. Only on the following days, due to the traction exerted by the peroneus longus tendon there is a progressive dislocation of one or more posterior fragments. A dislocation of more than 6 mm strongly suggests the presence of fracture [26, 34].
Fig. 13.
a Longitudinal US scan obtained at the os peroneum in a patient with type 2 tendon tear. The proximal bone fragment (big asterisk) is larger than the distal fragment (white arrow) and is proximally dislocated (curved arrow) due to the traction exerted by the peroneus longus tendon. The dislocation can be evaluated at US imaging (calipers). The distal fragment, which is smaller, seems not to be dislocated. b Color Doppler shows significant hyperemia present in the fracture. c Plain film X-ray confirms US findings showing dislocation of the bone fragments. d Plain film X-ray of the contralateral normal ankle. Note the correct position of the os peroneum at the calcaneal cuboid joint
In the presence of a bipartite or multipartite os peroneum, the differential diagnosis may be difficult at plain film X-ray examination. It should be based on the margins of the fragments, whether they are rounded or irregular, and on the presence or absence of a sclerotic margin. US imaging will confirm the diagnosis by showing the bone fragments separated by a heterogeneously hypoechoic area representing hematoma in the process of organization and inflammatory tissue. Color Doppler US will show local hypervascularity. US-guided compression of the fractured os peroneum is painful.
Lesion distal to the os peroneum (type 3)
When the injury to the peroneus longus tendon affects the distal portion of the os peroneum, the morphology of the sesamoid bone appears normal, although it is proximally dislocated. Generally, retraction of the os peroneum is limited to the distal osteofibrous tunnel near the inferior retinaculum. The os peroneum is rarely dislocated more proximally due to the concomitant injury to the inferior retinaculum. In that case the sesamoid bone is visible on the X-ray posteriorly to the talus and may mimic an os trigonum [34, 35]. Plain film X-ray examination can establish the location of the tendon rupture [26, 33, 36], and comparative X-ray examination is generally very useful. If the patient has an os peroneum in both feet (as it is the case in 30 % of the population) it can be visualized in its usual position in the contralateral foot. US imaging can confirm injury to the tendon distally to the os peroneum and the dislocation of the sesamoid bone at the inferior retinaculum. The tendon stump situated distally to the bone can be measured, thereby providing information required in possible surgical planning. The tendon stump will be surrounded by inhomogeneous serosanguineous effusion in various stages of organization and inflammatory reparative tissue. The tendon visualized caudally to the lesion will appear lax. Dynamic US imaging will confirm the diagnosis and permit assessment of the tendon stump and dislocation of the os peroneum.
US imaging plays an essential role in the follow-up of injuries to the peroneal tendon complex whether the patient undergoes conservative management or surgical treatment.
Acknowledgments
Conflict of interest
Lucio Molini and Stefano Bianchi declare that they have no conflict of interest related to this paper.
Human and animal studies
The study described in this article does not include any procedures involving humans or animals.
References
- 1.Philbin TM, Landis GS, Smith B. Peroneal tendon injuries. J Am Acad Orthop Surg. 2009;17:306–317. doi: 10.5435/00124635-200905000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Grant TH, Kelikian AS, Jereb SE, McCarthy RJ. Ultrasound diagnosis of peroneal tendon tears. A surgical correlation. J Bone Joint Surg Am. 2005;87:1788–1794. doi: 10.2106/JBJS.D.02450. [DOI] [PubMed] [Google Scholar]
- 3.Bianchi S, Delmi M, Molini L. Ultrasound of peroneal tendons. Semin Musculoskelet Radiol. 2010;14(3):292–306. doi: 10.1055/s-0030-1254519. [DOI] [PubMed] [Google Scholar]
- 4.Bianchi S, Martinoli C, Gaignot C, De Gautard R, Meyer JM. Ultrasound of the ankle: anatomy of the tendons, bursae, and ligaments. Semin Musculoskelet Radiol. 2005;9:243–259. doi: 10.1055/s-2005-921943. [DOI] [PubMed] [Google Scholar]
- 5.Neustadter J, Raikin SM, Nazarian LN. Dynamic sonographic evaluation of peroneal tendon subluxation. AJR Am J Roentgenol. 2004;183:985–988. doi: 10.2214/ajr.183.4.1830985. [DOI] [PubMed] [Google Scholar]
- 6.Muir JJ, Curtiss HM, Hollman J, Smith J, Finnoff JT. The accuracy of ultrasound-guided and palpation-guided peroneal tendon sheath injections. Am J Phys Med Rehabil. 2011;90(7):564–571. doi: 10.1097/PHM.0b013e31821f6e63. [DOI] [PubMed] [Google Scholar]
- 7.Oyedele O, Maseko C, Mkasi N, Mashanyana M. High incidence of the os peroneum in a cadaver sample in Johannesburg, South Africa: possible clinical implications? Clin Anat. 2006;19(7):605–610. doi: 10.1002/ca.20224. [DOI] [PubMed] [Google Scholar]
- 8.Sobel M, Pavlov H, Geppert MJ, Thompson FM, DiCarlo BF, Davis WH. Painful os peroneum syndrome: a spectrum of conditions responsible for lateral foot pain. Foot Ankle Int. 1994;15:112–124. doi: 10.1177/107110079401500306. [DOI] [PubMed] [Google Scholar]
- 9.Numkarunarunrote N, Malik A, Aguiar RO, Trudell DJ, Resnick D. Retinacula of the foot and ankle: MRI with anatomic correlation in cadavers. AJR Am J Roentgenol. 2007;188(4):W348–W354. doi: 10.2214/AJR.05.1066. [DOI] [PubMed] [Google Scholar]
- 10.Demondion X, Canella C, Moraux A, Cohen M, Bry R, Cotten A. Retinacular disorders of the ankle and foot. Semin Musculoskelet Radiol. 2010;14(3):281–291. doi: 10.1055/s-0030-1254518. [DOI] [PubMed] [Google Scholar]
- 11.Hyer CF, Dawson JM, Philbin TM, Berlet GC, Lee TH. The peroneal tubercle: description, classification, and relevance to peroneus longus tendon pathology. Foot Ankle Int. 2005;26:947–950. doi: 10.1177/107110070502601109. [DOI] [PubMed] [Google Scholar]
- 12.Ruiz JR, Christman RA, Hillstrom HJ. 1993 William J. Stickel Silver Award. Anatomic considerations of the peroneal tubercle. J Am Podiatr Med Assoc. 1993;83:563–575. doi: 10.7547/87507315-83-10-563. [DOI] [PubMed] [Google Scholar]
- 13.Sookur PA, Naraghi AM, Bleakney RR, Jalan R, Chan O, White LM. Accessory muscles: anatomy, symptoms, and radiologic evaluation. Radiographics. 2008;28:481–499. doi: 10.1148/rg.282075064. [DOI] [PubMed] [Google Scholar]
- 14.Saupe N, Mengiardi B, Pfirrmann CW, Vienne P, Seifert B, Zanetti M. Anatomic variants associated with peroneal tendon disorders: MR imaging findings in volunteers with asymptomatic ankles. Radiology. 2007;242:509–517. doi: 10.1148/radiol.2422051993. [DOI] [PubMed] [Google Scholar]
- 15.Wang XT, Rosenberg ZS, Mechlin MB, Schweitzer ME. Normal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging features. Radiographics. 2005;25:587–602. doi: 10.1148/rg.253045123. [DOI] [PubMed] [Google Scholar]
- 16.Sobel M, Geppert MJ, Olson EJ, Bohne WH, Arnoczky SP. The dynamic of peroneus tendon splits: a proposed mechanism, technique of diagnosis, and classification of injury. Foot Ankle. 1992;13:413–422. doi: 10.1177/107110079201300710. [DOI] [PubMed] [Google Scholar]
- 17.Sammarco GJ. Peroneal tendon injuries. Orthop Clin N Am. 1994;25:135–145. [PubMed] [Google Scholar]
- 18.Unlu MC, Bilgili M, Akgun I, Kaynak G, Ogut T, Uzun I. Abnormal proximal musculotendinous junction of the peroneus brevis muscle as a cause of peroneus brevis tendon tears: a cadaveric study. J Foot Ankle Surg. 2010;49(6):537–540. doi: 10.1053/j.jfas.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 19.Mick CA, Lynch F. Reconstruction of the peroneal retinaculum using the peroneus quartus. A case report. J Bone Joint Surg Am. 1987;69:296–297. doi: 10.2106/00004623-198769020-00023. [DOI] [PubMed] [Google Scholar]
- 20.Vuillemin V, Guerini H, Bard H, Morvan G. Stenosing tenosynovitis. J Ultrasound. 2012;15(1):20–28. doi: 10.1016/j.jus.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boya H, Pinar H. Stenosing tenosynovitis of the peroneus brevis tendon associated with hypertrophy of the peroneal tubercle. J Foot Ankle Surg. 2010;49(2):188–190. doi: 10.1053/j.jfas.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 22.Bruce WD, Christofersen MR, Phillips DL. Stenosing tenosynovitis and impingement of the peroneal tendons associated with hypertrophy of the peroneal tubercle. Foot Ankle Int. 1999;20:464–467. doi: 10.1177/107110079902000713. [DOI] [PubMed] [Google Scholar]
- 23.Peacock KC, Resnick EJ, Thoeder JJ. Fracture of the os peroneum with rupture of the peroneus longus tendon. A case report and review of the literature. Clin Orthop. 1986;202:223–226. [PubMed] [Google Scholar]
- 24.Bessette BJ, Hodge JC. Diagnosis of the acute os peroneum fracture. Singapore Med J. 1998;39:326–327. [PubMed] [Google Scholar]
- 25.Bianchi S, Martinoli C. Ultrasound of the musculoskeletal system. Berlin; New York: Springer; 2007. [Google Scholar]
- 26.Smania L, Craig JG, von Holsbeeck M. Ultrasonographic findings in peroneus longus tendon rupture. J Ultrasound Med. 2007;26:243–246. doi: 10.7863/jum.2007.26.2.243. [DOI] [PubMed] [Google Scholar]
- 27.Dombek MF, Lamm BM, Saltrick K, Mendicino RW, Catanzariti AR. Peroneal tendon tears: a retrospective review. J Foot Ankle Surg. 2003;42:250–258. doi: 10.1016/S1067-2516(03)00314-4. [DOI] [PubMed] [Google Scholar]
- 28.Rademaker J, Rosenberg ZS, Delfaut EM, Cheung YY, Schweitzer ME. Tear of the peroneus longus tendon: MR imaging features in nine patients. Radiology. 2000;214:700–704. doi: 10.1148/radiology.214.3.r00mr35700. [DOI] [PubMed] [Google Scholar]
- 29.Diaz GC, van Holsbeeck M, Jacobson JA. Longitudinal split of the peroneus longus and peroneus brevis tendons with disruption of the superior peroneal retinaculum. J Ultrasound Med. 1998;17:525–529. doi: 10.7863/jum.1998.17.8.525. [DOI] [PubMed] [Google Scholar]
- 30.Krause JO, Brodsky JW. Peroneus brevis tendon tears: pathophysiology, surgical reconstruction, and clinical results. Foot Ankle Int. 1998;19:271–279. doi: 10.1177/107110079801900502. [DOI] [PubMed] [Google Scholar]
- 31.Sayeed Y, Finnoff JT, Pawlina W, Smith J. Atypical anomalous peroneal (fibularis) tendon: potential pitfall in musculoskeletal sonography. J Ultrasound Med. 2011;30(5):710–713. doi: 10.7863/jum.2011.30.5.710. [DOI] [PubMed] [Google Scholar]
- 32.Dombek MF, Orsini R, Mendicino RW, Saltrick K. Peroneus brevis tendon tears. Clin Podiatr Med Surg. 2001;18(3):409–427. [PubMed] [Google Scholar]
- 33.Bianchi S, Abdelwahab IF, Tegaldo G. Fracture and posterior dislocation of the os peroneum associated with rupture of the peroneus longus tendon. Can Assoc Radiol J. 1991;42:340–344. [PubMed] [Google Scholar]
- 34.Brigido MK, Fessell DP, Jacobson JA, Widman DS, Craig JG, Jamadar DA, et al. Radiography and US of os peroneum fractures and associated peroneal tendon injuries: initial experience. Radiology. 2005;237:235–241. doi: 10.1148/radiol.2371041067. [DOI] [PubMed] [Google Scholar]
- 35.Tehranzadeh J, Stoll DA, Gabriele OM. Case report 271. Posterior migration of the os peroneum of the left foot, indicating a tear of the peroneal tendon. Skeletal Radiol. 1984;12(1):44–47. doi: 10.1007/BF00373176. [DOI] [PubMed] [Google Scholar]
- 36.Peterson JJ, Bancroft LW. Os peroneal fracture with associated peroneus longus tendinopathy. AJR Am J Roentgenol. 2001;177(1):257–258. doi: 10.2214/ajr.177.1.1770257a. [DOI] [PubMed] [Google Scholar]