Sir,
We report two cases of ischemic stroke following snake bite. This report sensitizes the practicing physicians that snake bite could be one of the etiological factors of stroke in young patients where other factors have been ruled out.
A 36-year-old male developed epistaxis and hematemesis following a snake bite over the left thumb. He was treated with equine polyvalent anti-snake venom (ASV) at a local hospital. Later he developed generalized seizures and was referred to our hospital. Examination revealed right pupil of 3 mm with normal reaction while left pupil was 5 mm with sluggish reaction. He had left horizontal gaze palsy and brainstem reflexes were absent with asymmetrical motor weakness (right > left) with bilateral extensor planter response. He required mechanical ventilation as the Glasgow coma scale was 7/15. Laboratory parameters revealed a normal coagulation profile and no hematuria. Biochemical profile, electrocardiogram, X-ray chest and 2D-echocardiography were normal. He had no repeat bleeding or seizure. Magnetic resonance imaging (MRI) showed acute infarcts in left cerebellar hemisphere, bilateral occipital lobe and left thalamus suggestive of basilar artery stroke [Figure 1]. He was managed with ASV, tetanus toxoid, antibiotics, anti-edema measures and anti-platelets. Consciousness and weakness improved and was discharged on the 15th day.
Figure 1.
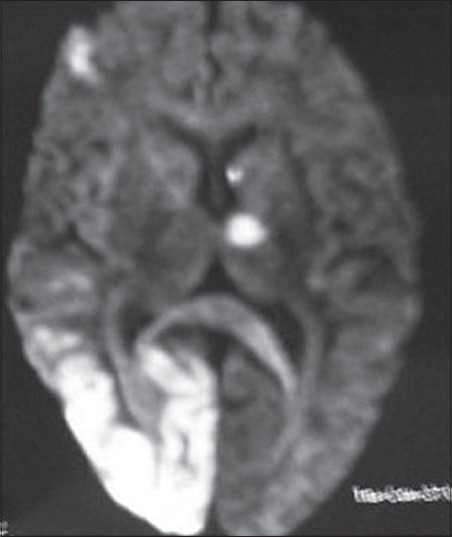
Magnetic resonance imaging of the brain showing acute ischemic infarcts in left cerebellar hemisphere, bilateral occipital lobe and left thalamus
The other case was a 40-year-old male brought to hospital 9 h after snake bite. He was drowsy with two deep fang marks on the foot. The vitals were stable and higher mental function examination revealed Broca's aphasia. Neurological examination was normal. Complete blood count including platelets, bleeding studies and prothrombin time were normal. Fibrinogen degradation products, antinuclear antibody test were within the normal range, as were chest X-ray, electrocardiogram and echocardiogram. MRI [Figure 2] showed infarct in the superior division of left middle cerebral artery. He was treated with ASV in addition to the supportive treatment and was discharged on the 10th day (mRS 1) with some residual dysfunction of naming.
Figure 2.
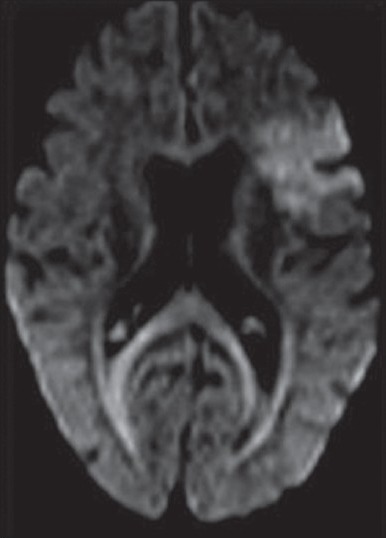
Magnetic resonance imaging of the brain showing acute ischemic infarct in the left superior division of middle cerebral artery territory
Cerebral complications, particularly ischemic infarcts after snake bite are rare. Mosquera et al. in their study have reported 8 patients (2.6%) with cerebro-vascular complications following snake bite (7 hemorrhagic; 1 ischemic).[1] Ischemic stroke is reported in nine out of 500 victims after envenoming in a report from Sri Lanka.[2]
The mechanisms by which cerebral infarction occurs in snake envenomation can be multi-factorial and are as follows:
The venom exhibits anticoagulant and procoagulant effects that can lead to small and even large vessel occlusions due to the microthrombi resulting in cerebral infarction[3]
Haemorrhagins are complement mediated toxic components of snake venom that may result in severe vascular spasm, endothelial damage and increased vascular permeability. All of these may lead to toxic vasculitis and result in thrombosis.[2] A preexisting procoagulant state, due to deficiencies of protein C or S or antithrombin III and antiphospholipid antibodies could account for a tendency towards thrombosis in large vessels
Hypotension can occur due to hypovolaemia from sweating, vomiting, decreased fluid intake and bleeding tendencies leading to low flow state and watershed infarct
Hyperviscosity caused by hypovolemia and hypoperfusion secondary to hypotension and hypercoagulation may also contribute to vessel occlusion[4]
Direct cardiotoxic effects of venom could lead to dysrrhythmias, causing cardiac thromboembolism.
Both these patients were young with no risk factors for stroke. Their clinical and radiological presentation strongly suggested a vascular thrombosis as a cause for their deficit. It could result from toxic vasculitis or toxin induced vascular spasm and endothelial damage. Hypotension as a cause of infarction was not considered because infarction did not involve watershed zones and blood pressure recordings were always normal.
Case 1 had a history of bleeding prior to developing seizure and upper limb weakness but the coagulation profile obtained was normal. However, early treatment with ASV could have resulted in normal coagulation profile. Altered sensorium in the hours after the bite could be related to direct arterial endothelial injuries by venom leading to cerebral edema or toxic encephalopathy.
These two cases illustrate the occurrence of ischemic snake bite, with abnormalities in the coagulation cascade as the likely causative factor. Learning point form these cases is that snake bite should be one of the differential diagnosis for any young patient with stroke. We call to attention, particularly physicians working in rural areas, to look for such less recognized etiologies of stroke in tropical countries so that victims of snakebite with neurological complications can be given more effective and timely treatment.
References
- 1.Mosquera A, Idrovo LA, Tafur A, Del Brutto OH. Stroke following Bothrops spp. snakebite. Neurology. 2003;60:1577–80. doi: 10.1212/01.wnl.0000061614.52580.a1. [DOI] [PubMed] [Google Scholar]
- 2.Thomas L, Tyburn B, Ketterlé J, Biao T, Mehdaoui H, Moravie V, et al. Prognostic significance of clinical grading of patients envenomed by Bothrops lanceolatus in Martinique. Members of the Research Group on Snake Bite in Martinique. Trans R Soc Trop Med Hyg. 1998;92:542–5. doi: 10.1016/s0035-9203(98)90907-5. [DOI] [PubMed] [Google Scholar]
- 3.Panicker JN, Madhusudanan S. Cerebral infarction in a young male following viper envenomation. J Assoc Physicians India. 2000;48:744–5. [PubMed] [Google Scholar]
- 4.Boviatsis EJ, Kouyialis AT, Papatheodorou G, Gavra M, Korfias S, Sakas DE. Multiple hemorrhagic brain infarcts after viper envenomation. Am J Trop Med Hyg. 2003;68:253–7. [PubMed] [Google Scholar]


