Abstract
Background
In patients with primary hyperaldosteronism, adrenal vein sampling (AVS) has emerged as a gold standard for distinguishing between unilateral and bilateral disease, but multiple criteria have been used and no consensus exists as to the most accurate criterion. The objective of this study was to determine which AVS criteria most accurately identify patients with unilateral surgical disease and are associated with significant clinical improvement after adrenalectomy.
Methods
This is a retrospective analysis of AVS results in 108 patients with primary hyperaldosteronism treated at a single institution. Literature review of AVS criteria was used to distinguish between unilateral and bilateral disease.
Results
Of the 10 AVS criteria identified in the literature, one criterion (ACTH stimulation, positioning: cortisol [adrenal]/cortisol [periphery] [Ca/Cp] > 5.0 and lateralization: aldosterone/cortisol [A/C] [dominant {D}]: A/C [nondominant {ND}] > 4:1) was the most accurate in identifying and correctly predicting lateralization of disease (P value range: < 0.001–0.0369). For this criterion, the true positive rate was 88%. The second most accurate criterion was no ACTH stimulation, positioning Ca/Cp > 1.1 and lateralization: A/C (D): A/C (ND) > 2:1. For this criterion, the overall true positive was 85%. However, we found no significant difference in clinical outcome based on individual criteria fulfillment.
Conclusions
Of the multiple criteria used for AVS evaluation, one criterion has the best accuracy. With the increasing use of AVS, there should be a consensus by which these results are evaluated and surgeons recommend adrenalectomy.
First described by Jerome Conn in 1954, primary hyperaldosteronism is present in 1.4–10% of patients with hypertension and is one of the surgically curable forms of secondary hypertension.1 Testing for serum aldosterone level and plasma renin activity is accurate for screening for primary hyperaldosteronism. Patients with primary hyperaldosteronism may have unilateral or bilateral adrenal hypersecretion of aldosterone. Although cross-sectional imaging may demonstrate unilateral adrenal mass in patients with primary hyperaldosteronism, adrenal venous sampling (AVS) is necessary to distinguish unilateral from bilateral adrenal disease.2 Since its introduction in the 1960s, adrenal vein sampling (AVS) has increased in its use and changes the management approach (medical for bilateral disease and surgical resection for unilateral disease) in up to 50% of patients with primary hyperaldosteronism.3,4
AVS is commonly used in conjunction with computed tomography (CT) imaging to lateralize the lesion. Considering that most aldosteronomas are less than 15 mm in size, adrenal CT may fail or inaccurately identify a nonfunctioning adrenal mass. Several investigators have advocated the use of AVS in selected patients.5,6 In contrast, however, most studies have demonstrated the usefulness of AVS when radiologic findings were indeterminate or when there were bilateral adrenal abnormalities identified.2–4 Young and colleagues highlighted the importance of AVS for proper diagnosis and treatment in a comprehensive, prospective study of 203 patients.4 In 42 of 203 patients (21.7%), they found that without AVS these patients would have been incorrectly excluded for adrenalectomy, and 48 of 203 patients (24.7%) may have had an unnecessary or inappropriate procedure if treatment decisions were based on only CT scan findings. Also, Kempers and colleagues found that reliance on radiographic findings can lead to inappropriate treatment of primary hyperaldosteronism where CT/magnetic resonance imaging (MRI) alone had misdiagnosed 37.8% (359 of 950) of patients.2 We also recently performed an analysis of 114 patients with primary hyperaldosteronism and found 50% of patients would have had inappropriate management without AVS.3
Even though AVS is becoming the gold standard for selecting patients who would benefit from adrenalectomy for their primary hyperaldosteronism, numerous AVS criteria have been used to define unilateral versus bilateral disease, as well as different AVS techniques being used. There is currently no consensus on the best AVS criteria for distinguishing unilateral versus bilateral primary hyperaldosteronism.3 Most criteria have a combination of three components, adrenal vein-to-periphery cortisol ratios to confirm positioning of the catheter in the adrenal veins, aldosterone/cortisol ratios compared between glands to distinguish between the hyper secreting and or suppressed adrenal gland, and/or adrenocorticotropic hormone (ACTH) stimulation to further lateralize the hyperfunctioning gland. The cutoff ratio values used to define lateralization also vary greatly from institution to institution.
The purpose of this study was to determine which AVS criteria are most accurate for lateralization and to determine if any criteria were associated with a better clinical outcome from adrenalectomy. We compared the ten criteria identified from the literature in 108 patients with primary hyperaldosteronism, to determine which criterion was most accurate based on biochemical, clinical, and pathologic measures that are associated with unilateral disease and improvement in primary hyperaldosteronism.
METHODS
Patients
Using a computerized medical record database, 108 patients with primary hyperaldosteronism treated between 1991 and 2010 were identified. All 108 patients underwent AVS per the clinical protocol approved by our Institutional Review Board. A retrospective review was performed to review demographics, laboratory, AVS results, and pathology data. Postoperative clinical data, potassium level, aldosterone level, systolic and diastolic blood pressure, and number of anti-hypertensive medications were obtained during clinic follow-up or by telephone interview. All patients had a serum aldosterone and plasma renin level measured for the diagnosis of primary hyperaldosteronism and a confirmatory test with either a sodium chloride loading test, a captopril test, or a posture test.
AVS Technique
All patients in this study underwent AVS, regardless of CT findings. An experienced interventional radiologist performed each AVS. Following bilateral femoral venous catheterization, simultaneous catheterization of the bilateral adrenal veins was performed using either four French Mickaelsson, Simmons 1, or Cobra 2 catheters with or without modifications to sample the right adrenal vein and 4 French Simmon 2 or 3 catheters and rarely a sub three French microcatheter to obtain samples from the left adrenal vein. Peripheral samples were obtained from the right iliac vein. Baseline blood samples were drawn 5 min apart from each adrenal vein and the iliac vein. Next, an intravenous bolus of 0.25 mg of ACTH followed by infusion of ACTH (0.25 mg in 250 ml normal saline) at a rate of 150 cc/hour was administered. Blood samples were collected at 5, 10, and 15 min post-ACTH infusion, and levels for aldosterone and cortisol were measured. Appropriate placement of catheters in the adrenal veins was surmised by contrast venography and subsequently confirmed by appropriately elevated cortisol levels in the adrenal vein samples compared with the peripheral samples.
Sample Interpretation
There were ten criteria for AVS evaluation identified from the literature (Table 1).2,3,6–20 Each of these criteria was used to evaluate the AVS results for each of the 108 patients. There were 3 components to the criteria identified: (1) whether a catheter positioning criteria was specified for AVS, (2) whether ACTH stimulation was used, and (3) the aldosterone-to-cortisol ratio cutoff and or the presence of suppression of 1 gland (nondominant) relative to the other gland or peripheral aldosterone-to-cortisol ratio. Criteria that did not use ACTH stimulation were applied to the prestimulation AVS samples. The criteria were met if AVS results indicated both proper placement in the adrenal veins and lateralization. True positives were defined as those criteria that correctly lateralized the hyperfunctioning gland as was ultimately determined by the operative findings, clinical and laboratory postoperative results.
TABLE 1.
Adrenal vein sampling criteria
| Criteria | Positioning criteria | ACTH stimulation | Lateralization |
|---|---|---|---|
| 1 | NS | No | A/C(D):A/C(ND) > 4:1 and A/C(ND) < A/C (periphery) |
| 2 | NS | No | A/C(D)/A/C (ND) > 1.0 and A/C(ND) < A/C (periphery) |
| 3 | A/C > 1.1 versus periphery | No | A/C(D) > 2:1 |
| 4 | Adrenal/peripheral cortisol > 3:1 | No | A/C (D):A/C (ND) > 3:1 and A/C (ND) < A/C (periphery) |
| 5 | Adrenal/peripheral cortisol > 2:1 | No | A/C (D) and A/C (ND) > 4:1 |
| 6 | Adrenal (D)/peripheral cortisol > 3:1 | No | A/C (D)/A/C (ND) > 2:1 and A/C (ND) < peripheral A/C |
| 7 | NS | Yes | ACTH stimulation: A/C (D): A/C (ND) > 4:1, A/C (ND) < A/C (periphery) |
| 8 | NS | Yes | No positioning criteria, ACTH stimulation: A(D): A(ND) > 10:1 |
| 9 | Adrenal (D)/C (periphery) > 2.0 | Yes | A/C (ND) < A/C (periphery) |
| 10 | Adrenal (D)/C (peripheral) > 5.0 | Yes | ACTH stimulation, positioning, lateralization: A/C (D): A/C (ND) > 4:1 |
D dominant adrenal gland, ND nondominant adrenal gland, A aldosterone, C cortisol, A/C aldosterone-to-cortisol ratio, NS not specified
Clinical Scale Score
Follow-up records were evaluated on the basis of six postoperative findings to determine the presence of clinically significant surgical disease and patient outcome. One point was assigned for each (total score of up to six) of the following criteria: surgical pathology showing adrenocortical adenoma or hyperplasia, postoperative normal blood pressure (< 140 systolic or< 90 diastolic) off anti-hypertensive medications, discontinuation of all anti-hypertensive medications, reduction in number of anti-hypertensive medications, resolution of hypokalemia, and normalization of serum aldosterone level.
Statistical Methods
Once the AVS results were evaluated using the 10 identified criteria, the true positive rate was determined in those patients who underwent adrenalectomy and only in those in whom the postoperative serum aldosterone level and or postoperative blood pressure was normal off medications. McNemar and chi-square analysis were then used for comparison of criteria to determine statistical significance. All calculations were completed using StatView statistical software (SAS, Inc., Cary, NC).
RESULTS
Of 108 patients, 91 underwent adrenalectomy for unilateral disease, while 17 underwent medical management for bilateral disease based on AVS sampling results. The demographic and clinical characteristics of the study cohort are summarized in Table 2. While undergoing AVS, all patients had successful adrenal vein catheterization confirmed by elevated adrenal vein cortisol compared with peripheral vein cortisol and bilateral venography.
TABLE 2.
Demographic and clinical characteristics of study cohort
| Type | Distribution |
|---|---|
| Gender | |
| Male | 63 |
| Female | 45 |
| Age (years) | |
| Mean | 50 |
| Median | 51 |
| Range | 23–73 |
| History of hypertension (years) | |
| Mean | 13.1 |
| Median | 11 |
| Range | 0–40 |
| Number of anti-hypertensive medications | |
| Mean | 2.7 |
| Median | 3 |
| Range | 0–6 |
Each AVS dataset for the 108 patients was evaluated by the 10 separate criteria. A patient met criteria if AVS values were within guidelines for both positioning (for both adrenal veins) and lateralization. All 10 criteria were applied to all 108 patient AVS study results. True positive results were determined for each criterion if the determined lateralization was confirmed by the pathology and follow-up data to be consistent with unilateral disease. The results of the different criteria are summarized in Tables 3 and 4. Criterion 10, ACTH stimulation, positioning: cortisol (adrenal)/cortisol (periphery) (Ca/Cp) > 5.0 and lateralization: aldosterone/cortisol (A/C) (dominant [D]): A/C (nondominant [ND]) > 4:1, was the most accurate. Criterion 10 had the highest true positive rate compared with the other criteria (P value < 0.001–.04), excluding criterion 3 (P value = 0.54). Of ten cases not fulfilling criterion 10, four patients failed to meet positioning criteria and six failed to meet lateralization criteria. Criterion 3, no ACTH stimulation, positioning Ca/Cp > 1.1 and lateralization: A/C (D): A/C (ND) > 2:1 was the second most accurate criterion. Criterion 3 had a significantly higher positive rate than the other criteria (P value < 0.001–0.01), excluding criterion 7 (P value = 0.14), 9 (P value = 0.13) and 10 (P value = 0.54). We also performed a subset analysis of only those patients (N = 76) in our cohort who had adrenalectomy and who had normal postoperative serum aldosterone levels and or normal postoperative blood pressure readings off medications (Table 4). We found criterion ten had the highest positive rate.
TABLE 3.
Accuracy of adrenal vein sampling criteria in all patients
| Criteria | Percent of patient who fulfilled criteria | Criteria 10 χ2 P value* |
Criteria 3 χ2 P value* |
|---|---|---|---|
| 1 | 58 | 0.0002 | 0.0014 |
| 2 | 75 | 0.0013 | 0.0087 |
| 3 | 85 | 0.5367 | |
| 4 | 29 | < 0.0001 | < 0.0001 |
| 5 | 53 | < 0.0001 | 0.0002 |
| 6 | 36 | < 0.0001 | < 0.0001 |
| 7 | 73 | 0.0369 | 0.1386 |
| 8 | 60 | 0.0004 | 0.0030 |
| 9 | 78 | 0.0337 | 0.1299 |
| 10 | 88 | – | 0.5367 |
Comparison of the two most accurate criteria (criteria 3 and 10) is listed
TABLE 4.
Accuracy of adrenal vein sampling criteria in patients who had adrenalectomy
| Criteria | Percent of all patient who had adrenalectomy and fulfilled criteria | Percent of patient who fulfilled criteriaa |
|---|---|---|
| 1 | 58 | 37 |
| 2 | 64 | 38 |
| 3 | 85 | 49 |
| 4 | 29 | 16 |
| 5 | 54 | 32 |
| 6 | 36 | 16 |
| 7 | 73 | 45 |
| 8 | 60 | 36 |
| 9 | 78 | 50 |
| 10 | 88 | 54 |
Percent of patients who fulfilled the AVS criteria and had normal serum aldosterone and or normal blood pressure off medications
Of the 17 patients who did not have an adrenalectomy, 6 patients met 1 or more of the lateralization criteria. Also, one patient met all ten criteria, one patient met criteria 1, 2, 3, 9, and 10, two patients met criteria 3 only, and two patients met criteria 9 only. All 17 patients who did not undergo adrenalectomy had imaging with CT. CT findings consisted of two patients with bilateral normal adrenal glands, nine patients with bilateral adrenal masses, and six patients with evidence of unilateral adrenal mass (2 right, 4 left). Unfortunately, no follow-up data is available for the 17 patients who did not undergo adrenalectomy to determine the true negative or false negative rates.
Postoperative records for 91 patients who had an adrenalectomy were reviewed to document clinically significant surgical disease. Clinical significance was evaluated using the Clinical Scale Score. Of the 91 patients, 89 had sufficient clinical information and the results are summarized in Fig. 1. All patients had a cortical adenoma or hyperplasia on pathology and had an improvement in 1 or more clinical endpoint evaluated. There was, however, no significant difference in clinical outcome based on individual criteria fulfillment.
FIG. 1.
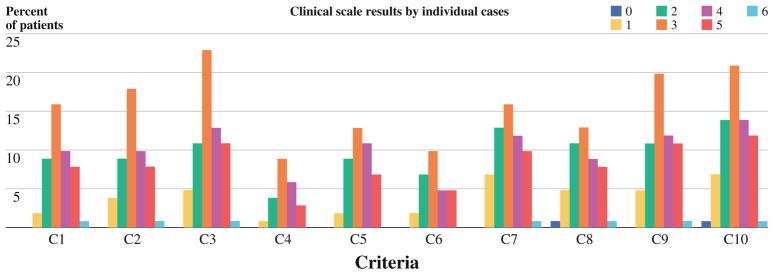
Clinical outcome of patients undergoing adrenalectomy. A total of six points (1 per each variable) were assigned for the following indicators of unilateral disease and improvement after adrenalectomy: surgical pathology showing adrenocortical adenoma or hyperplasia, postoperative normal blood pressure (< 140 systolic or < 90 diastolic) off anti-hypertensive medication, discontinuation of all anti-hypertensive medications, reduction in number of anti-hypertensive medications, resolution of hypokalemia, and normalization of serum aldosterone level. Y axis is the percent of patients with each total score. X axis is the tencriteria compared
DISCUSSION
The management of primary hyperaldosteronism has dramatically changed in the last two decades with the recognition that AVS is critical for appropriately selecting patients who have unilateral disease and who would benefit from adrenalectomy. However, the specific technique and criteria for determining lateralization based on AVS results remains controversial. In our study, we found that one of 10 criteria compared had the highest accuracy (criterion 10: ACTH stimulation, positioning: cortisol [adrenal]/cortisol [periphery] [Ca/Cp] > 5.0 and lateralization: aldosterone/cortisol [A/C] [dominant {D}]: A/C [nondominant {ND}] > 4:1). Criterion 10 was significantly better compared with the other criteria (P value < 0.001–0.04), excluding criterion 3 (P value = 0.54). We, however, found that none of the AVS criteria evaluated were associated with a significantly different outcome from adrenalectomy for primary hyperaldosteronism, when comparing clinical and or laboratory endpoints of disease resolution, or when considering only those patients with normal postoperative serum aldosterone and or normal blood pressure off medications.
Criterion 10 incorporates three components to determine lateralization. First, positioning confirmation was required with a high Ca/Cp ratio. Ceral and colleagues supported the use of this same ratio with findings that acceptable clinical determination can be made with Ca/Cp greater or equal to five.17 Secondly, ACTH stimulation was used once when successful canalization was determined. While not required for successful interpretation of results, ACTH stimulation does improve the number of patients who can have their tumor lateralized with AVS.3 Finally, a moderate A/C ratio of 4:1 for dominant-to-nondominant adrenal gland comparison was used. The combined effect of correct positioning, ACTH stimulation and a moderate A/C ratio allow for a large number of patients to meet lateralization criteria as evidenced by the high true positive rate. The ten cases that did not meet criterion 10 were: 4 cases that did not meet the positioning criterion and six that did not meet the criterion for lateralization. Because these four patients were medically managed for bilateral disease, no conclusion regarding the presence of surgical disease can be drawn. In contrast, criterion 3 incorporates two components of AVS. Positioning confirmation is based on a lower Ca/Cp ratio, thus increasing the number of patients who would meet the criterion. ACTH stimulation is not used, and the A/C cutoff ratio is lower. Rossi and colleagues advocated for use of the same criteria in 104 patients that helped to substantiate the use of AVS in primary hyperaldosteronism evaluation.16
Regarding the patients who did not undergo adrenalectomy, it is impossible to determine the presence of clinically significant surgical disease or long-term outcome. Of the six patients who met one or more of the analyzed criteria, four had imaging indicating either absent or bilateral disease. The two patients with CT imaging suggestive of the disease had an MRI that was indeterminate. No speculation as to the true presence of surgical disease can be determined from this study since no surgery was ever preformed. Only a prospective randomized study in which patients in this situation were either observed or underwent adrenalectomy could provide meaningful data in regard to the AVS results accurately showing bilateral disease regardless of the criteria fulfilled.
We believe our study has several strengths to allow for a comparison of the different criteria used for AVS lateralization. These include a relatively large study cohort, complete AVS records and a standardized approach for measurement, and comprehensive AVS values encompassing all the values used in the ten criteria compared. Moreover, we were able to include patients who did not have adrenalectomy to more accurately determine the criteria accuracies for distinguishing between unilateral and bilateral disease. An experienced interventional radiologist performed all of the AVS, and there was successful adrenal vein cannulation in all cases using two methods for confirmation. Lastly, both non-ACTH and ACTH values were available to allow for a comprehensive comparison among the ten criteria.
There are several limitations in our study as it was retrospective, such as selection bias due to our institution being a referral center and that our cohort may not be reflective of the majority of patients with primary hyperaldosteronism. Also, there is no consensus criterion on when adrenalectomy has been successful in patients with unilateral disease (normal potassium, normal serum aldosterone, normal blood pressure, no need for anti-hypertensive, reduction in the number of anti-hypertensive medications needed to control the blood pressure, reduced hypertension, and/or presence of cortical adenoma/hyperplasia).2,3,6–20 To account for this, we used the Clinical Scale Score as a way to attempt to validate the presence of clinically significant surgical disease and to determine postoperative clinical improvement. All but two patients had records for analysis, all of which had clinical evidence of disease, as well as evidence of clinical improvement. We also performed a subset analysis of only those cases in which the patients had normal postoperative serum aldosterone levels and or normal postoperative blood pressure off medication and found criterion ten followed by criteria 9 and three had the highest true positive rate. Another limitation of any retrospective study analyzing the accuracy of AVS results for correctly determining the presence of unilateral versus bilateral disease is that those patients found to have bilateral disease are medically managed so no gold standard can be used to truly determine if this diagnosis was correct.2,11,21 For this reason, the accuracies found for the criteria we compared may be an overestimation.
In summary, we believe there should be a consensus by which AVS results are evaluated and surgeons recommend adrenalectomy. Our study findings suggest that 1 criterion has the best overall accuracy (positioning: cortisol [adrenal]/cortisol [periphery] [Ca/Cp] > 5.0 and lateralization: aldosterone/cortisol [A/C] [dominant {D}]: A/C [non-dominant {ND}] > 4:1) and should be used in the evaluation of patients with primary hyperaldosteronism undergoing AVS for surgical evaluation.
References
- 1.Conn JW, Cohen EL, Rovner DR. Landmark article Oct 19, 1964: suppression of plasma renin activity in primary aldosteronism. In: Conn JW, Cohen EL, Rovner DR, editors. Distinguishing primary from secondary aldosteronism in hypertensive disease. JAMA. 1985;253:558–66. doi: 10.1001/jama.253.4.558. [DOI] [PubMed] [Google Scholar]
- 2.Kempers MJ, Lenders JW, van Outheusden L, van der Wilt GJ, Schultze Kool LJ, Hermus AR, et al. Systematic review: diagnostic procedures to differentiate unilateral from bilateral adrenal abnormality in primary aldosteronism. Ann Intern Med. 2009;151:329–37. doi: 10.7326/0003-4819-151-5-200909010-00007. [DOI] [PubMed] [Google Scholar]
- 3.Mathur A, Kemp CD, Dutta U, Baid S, Ayala A, Chang RE, et al. Consequences of adrenal venous sampling in primary hypdraldosteronism and predictors of unilateral adrenal disease. J Am Coll Surg. 2010;211:384–90. doi: 10.1016/j.jamcollsurg.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Young WF, Stanson AW, Thompson GB, Grant CS, Farley DR, van Heerden JA. Role for adrenal venous sampling in primary aldosteronism. Surgery. 2004;136:1227–35. doi: 10.1016/j.surg.2004.06.051. [DOI] [PubMed] [Google Scholar]
- 5.Zarnegar R, Bloom AI, Lee J, Kerlan RK, Jr, Wilson MW, Laberge JM, et al. Is adrenal venous sampling necessary in all patients with hyperaldosteronism before adrenalectomy? J Vasc Interv Radiol. 2008;19:66–71. doi: 10.1016/j.jvir.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 6.Tan YY, Ogilvie JB, Triponez F, Caron NR, Kebebew EK, Clark OH, et al. Selective use of adrenal venous sampling in the lateralization of aldosterone-producing adenomas. World J Surg. 2006;30:879–85. doi: 10.1007/s00268-005-0622-8. discussion 86–7. [DOI] [PubMed] [Google Scholar]
- 7.Auchus RJ, Wians FH, Jr, Anderson ME, Dolmatch BL, Trimmer CK, Josephs SC, et al. What we still do not know about adrenal vein sampling for primary aldosteronism. Horm Metab Res. 2010;42:411–5. doi: 10.1055/s-0030-1252060. [DOI] [PubMed] [Google Scholar]
- 8.Mulatero P, Bertello C, Sukor N, Gordon R, Rossato D, Daunt N, et al. Impact of different diagnostic criteria during adrenal vein sampling on reproducibility of subtype diagnosis in patients with primary aldosteronism. Hypertension. 2010;55:667–73. doi: 10.1161/HYPERTENSIONAHA.109.146613. [DOI] [PubMed] [Google Scholar]
- 9.Miotto D, De Toni R, Pitter G, Seccia TM, Motta R, Vincenzi M, et al. Impact of accessory hepatic veins on adrenal vein sampling for identification of surgically curable primary aldosteronism. Hypertension. 2009;54:885–9. doi: 10.1161/HYPERTENSIONAHA.109.134759. [DOI] [PubMed] [Google Scholar]
- 10.Seccia TM, Miotto D, De Toni R, Pitter G, Mantero F, Pessina AC, et al. Adrenocorticotropic hormone stimulation during adrenal vein sampling for identifying surgically curable subtypes of primary aldosteronism: comparison of 3 different protocols. Hypertension. 2009;53:761–6. doi: 10.1161/HYPERTENSIONAHA.108.128553. [DOI] [PubMed] [Google Scholar]
- 11.Kline GA, Harvey A, Jones C, Hill MH, So B, Scott-Douglas N, et al. Adrenal vein sampling may not be a gold-standard diagnostic test in primary aldosteronism: final diagnosis depends upon which interpretation rule is used. Variable interpretation of adrenal vein sampling. Int Urol Nephrol. 2008;40:1035–43. doi: 10.1007/s11255-008-9441-9. [DOI] [PubMed] [Google Scholar]
- 12.Rossi GP, Pitter G, Bernante P, Motta R, Feltrin G, Miotto D. Adrenal vein sampling for primary aldosteronism: the assessment of selectivity and lateralization of aldosterone excess baseline and after adrenocorticotropic hormone (ACTH) stimulation. J Hypertens. 2008;26:989–97. doi: 10.1097/HJH.0b013e3282f9e66a. [DOI] [PubMed] [Google Scholar]
- 13.Tamura Y, Adachi J, Chiba Y, Mori S, Takeda K, Kasuya Y, et al. Primary aldosteronism due to unilateral adrenal microadenoma in an elderly patient: efficacy of selective adrenal venous sampling. Intern Med. 2008;47:37–42. doi: 10.2169/internalmedicine.47.0333. [DOI] [PubMed] [Google Scholar]
- 14.Auchus RJ, Chandler DW, Singeetham S, Chokshi N, Nwariaku FE, Dolmatch BL, et al. Measurement of 18-hydroxycorticosterone during adrenal vein sampling for primary aldosteronism. J Clin Endocrinol Metab. 2007;92:2648–51. doi: 10.1210/jc.2006-2631. [DOI] [PubMed] [Google Scholar]
- 15.Baba Y, Hokotate H, Nakajo M. Comparison of adrenal vein sampling value between aldosterone producing adrenal adenoma and non-functioning adrenal adenoma: evaluation using receiver operating characteristic analysis. Acta Radiol. 2005;46:750–5. doi: 10.1080/02841850500215568. [DOI] [PubMed] [Google Scholar]
- 16.Rossi GP, Sacchetto A, Chiesura-Corona M, De Toni R, Gallina M, Feltrin GP, et al. Identification of the etiology of primary aldosteronism with adrenal vein sampling in patients with equivocal computed tomography and magnetic resonance findings: results in 104 consecutive cases. J Clin Endocrinol Metab. 2001;86:1083–90. doi: 10.1210/jcem.86.3.7287. [DOI] [PubMed] [Google Scholar]
- 17.Ceral J, Solar M, Krajina A, Ballon M, Suba P, Cap J. Adrenal venous sampling in primary aldosteronism: a low dilution of adrenal venous blood is crucial for a correct interpretation of the results. Eur J Endocrinol. 2010;162:101–7. doi: 10.1530/EJE-09-0217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mulatero P, Stowasser M, Loh KC, Fardella CE, Gordon RD, Mosso L, et al. Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continents. J Clin Endocrinol Metab. 2004;89:1045–50. doi: 10.1210/jc.2003-031337. [DOI] [PubMed] [Google Scholar]
- 19.Phillips JL, Walther MM, Pezzullo JC, Rayford W, Choyke PL, Berman AA, et al. Predictive value of preoperative tests in discriminating bilateral adrenal hyperplasia from an aldosterone-producing adrenal adenoma. J Clin Endocrinol Metab. 2000;85:4526–33. doi: 10.1210/jcem.85.12.7086. [DOI] [PubMed] [Google Scholar]
- 20.Magill SB, Raff H, Shaker JL, Brickner RC, Knechtges TE, Kehoe ME, et al. Comparison of adrenal vein sampling and computed tomography in the differentiation of primary aldosteronism. J Clin Endocrinol Metab. 2001;86:1066–71. doi: 10.1210/jcem.86.3.7282. [DOI] [PubMed] [Google Scholar]
- 21.Minami I, Yoshimoto T, Hirono Y, Izumiyama H, Doi M, Hirata Y. Diagnostic accuracy of adrenal venous sampling in comparison with other parameters in primary aldosteronism. Endocr J. 2008;55:839–46. doi: 10.1507/endocrj.k07e-164. [DOI] [PubMed] [Google Scholar]


