Abstract
Objectives
To describe the rate of successful consent using an altered (deferred telephone) consent process in emergency department (ED) patients.
Methods
This study evaluated the consent process employed during a prospective, multicenter, observational study of outcomes in anticoagulated patients with blunt head trauma. The study was approved by the institutional review boards at all participating centers. Patients were not informed of the study during their enrollment at their index ED visit. Patient names, clinical findings, and contact information were collected at the time of initial ED visits. The patients or their legally designated surrogates were contacted by telephone at least 14 days after ED discharge, given all the elements of informed consent, and then were consented for study participation. Study results are presented with simple descriptive statistics.
Results
Five hundred and six patients with a mean age of 75.8 years (SD ±12.2 years) including 274 female subjects (54.2%; 95% CI = 49.7% to 58.6%) were enrolled into the study. Patients or their surrogates were successfully contacted by telephone in 501 out of 506 cases (99.0%, 95% CI = 97.7% to 99.7%). Consent was obtained in 500 out of 501 cases at time of telephone follow-up (99.8%; 95% CI = 98.9% to 100.0%). Surrogates provided consent in 199 cases (39.7%, 95% CI = 35.4% to 44.2%). Median time from ED visit to phone contact was 21 days (IQR 17 to 27 days). The median number of phone attempts for successful contact was 1 (IQR 1 to 2 attempts).
Conclusions
The authors achieved a very high rate of successful telephone follow-up in this predominantly older ED population. Obtaining consent to participate in a research study using a deferred telephone contact process was effective and well-received by both subjects and surrogates. Institutional Review Boards should consider deferred telephone consent for minimal-risk studies requiring telephone follow-up, as opposed to a consent process requiring written documentation at the time of initial ED visit.
INTRODUCTION
The ethical foundations for research include performance of research that has a potential for benefit (principle of beneficence), exposing of patients to minimal risk or appropriate incremental risk (principle of non-maleficence or justice), and protection of patients’ right to autonomy (principle of autonomy).1 The goal of consent is to protect research subject autonomy while allowing for the advancement of science. Because emergency department (ED) patients are enrolled at a time of maximal stress and/or may be unable to consent, obtaining consent for emergency medicine (EM) research is often challenging.
Various acceptable methods of consent exist, including informed consent (consent at the time of study enrollment), surrogate consent (consent by family members), or deferred consent (consent of critical/comatose patients at a later time when they may consent for themselves). In addition, some research may be granted waiver of informed consent (observational, minimal risk research), or exemption from informed consent (deferral of consent for resuscitation research). Regardless of consent methodology, the necessary elements of consent for research include a statement of the nature and purpose of the study, duration of participation, description of procedures to be followed, description of foreseeable risks, disclosure of appropriate alternative treatments, and a statement of confidentiality.
Evidence for the use of verbal consent at the time of telephone follow-up (as opposed to obtaining written informed consent during ED evaluation) is very limited. The objectives of this study were to describe an altered method of informed consent, specifically deferred telephone consent, in an observational, minimal risk, EM research study and to report the rate of successful consent using this process. We hypothesized that telephone consent would be successful in over 90% of eligible patients.
METHODS
Study Design
This was a prospective, multicenter study evaluating the consent process in anticoagulated ED patients with blunt head trauma (planned secondary analysis of a parent study).2 It was approved by the investigational review boards (IRBs) of the participating sites.
Study Setting and Population
This study was performed in a six-site EM network (one academic and five community EDs, including one Level I and one Level II trauma center). Approximately 331,000 patients are evaluated within the network per year. All adult ED patients on warfarin or clopidogrel and sustaining blunt head trauma were eligible. Patients were excluded from this analysis for any of the following reasons: transferred from another hospital, intracranial hemorrhage on ED computed tomography (CT) scan, hospitalized for longer than 14 days from index ED visit, or died in the ED or during hospitalization.
Study Protocol
Eligible patients were identified by on-duty emergency physicians who completed standardized data collection forms (Figure 1). Data collected from the index ED visit included patient demographics and clinical information. Patients were not approached for consent in the ED nor given any information regarding their enrollment into the study. Patients (or their surrogates) were contacted by telephone between 9 am and 6 pm a minimum of 14 days after their index ED visits for a follow-up survey. At the telephone contact, subjects were read the necessary elements for informed consent, including the bill of rights that California law requires be read to all potential medical research subjects,3 and asked whether they agreed to participate and were offered to have all information/consent documents mailed to them (Figure 1). The entire telephone interaction took approximately 5 to 10 minutes.
Figure 1.
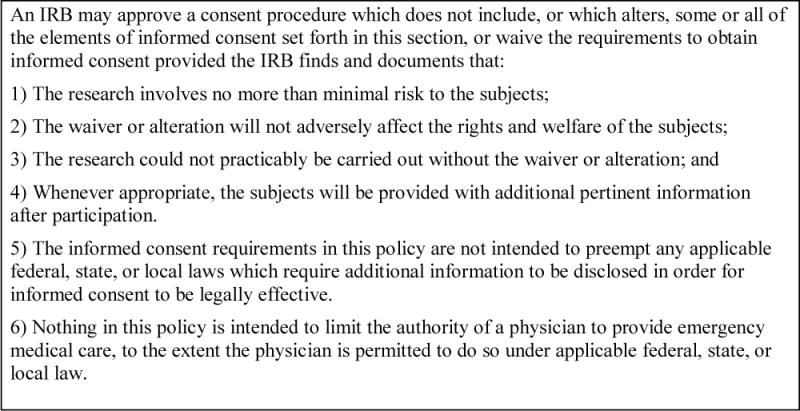
Federal Law 45 CFR 46.116(d)
Each telephone survey was performed either by a physician (DKN) or a research coordinator (ASR). Both investigators followed a standardized IRB-approved telephone script and completed standardized data collection forms. Patients were coded as “lost to follow-up” if investigators were unable to make contact after six telephone attempts, or the available telephone numbers were disconnected.
Outcome Measures
The primary outcome measures were 1) successful telephone contact, and 2) ability to obtain study consent via telephone. Reasons given by patients for refusing to consent were documented as free text.
Data Analysis
Statistical analysis was performed with STATA statistical software (Stata Corp., Version 11.0, College Station, TX). Data are described using simple, descriptive statistics. Continuous variables are described with the mean ± one standard deviation if normally distributed, and median with interquartile range (IQR) if non-normally distributed. 95% confidence intervals (CI) are provided where appropriate.
RESULTS
Five hundred and six subjects were enrolled from April 2009 to May 2010. The mean age was 75.8 years (SD ±12.2 years), and 274 were female (54.2%). An additional 129 subjects were eligible but did not have data collection forms completed by the treating physicians, and thus were not included in the study. Therefore, the ED capture rate (of eligible subjects) was 79.7% (506 out of 635 eligible subjects enrolled).
Follow-up telephone contact was successfully accomplished in 501 of the 506 subjects (99.0%; 95% CI = 97.7% to 99.7%). The median number of calls was one (IQR 1 to 2). The median time to follow-up telephone contact was 21 days (IQR 17 to 27 days).
Consent for study inclusion and conduct of the telephone survey was obtained in 500 of 501 subjects at time of the follow-up call (99.8%; 95% CI = 98.9% to 100.0%). Surrogate consent was obtained in 199 of the 501 subjects (39.7%; 95% CI = 35.4% to 44.2%). The single patient refusing consent stated, “I don’t feel well enough to talk.” No further contact was attempted. Only four patients (0.8%, 95% CI = 0.02% to 1.6%) requested consent documents be mailed.
DISCUSSION
We found the process of deferred telephone consent in a minimal-risk EM research study to be effective and well-accepted by the patients enrolled into the study. The consent rate was extremely high, without evidence of harm to study subject autonomy. No patient objected to being enrolled into an observational study without his or her knowledge or consent.
The IRBs involved in this study declined to waive the requirement for informed consent, as an intervention (telephone follow-up) was performed and the ability to consent patients in the ED was possible. This is consistent with federal law regarding waiver of consent (see Figure 2). In this study, patients were ultimately provided with study and consent information, including the bill of rights (a California human subjects requirement3), at telephone follow-up and for the sole purpose of obtaining consent for study participation. All data for any patients refusing participation were removed from the study. For these reasons, the deferred telephone consent process described in this paper constitutes delayed consent for study participation (inclusion), as opposed to consent limited to the telephone interview portion of the study, or information provided after participation.
Figure 2.
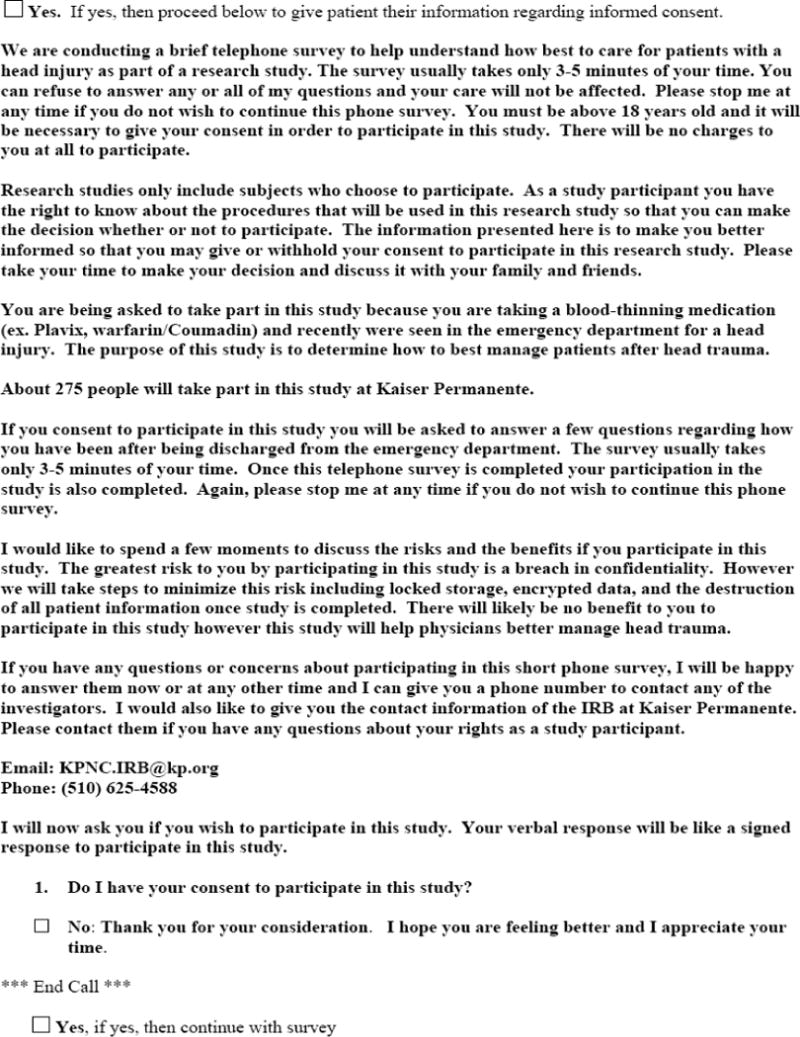
Consent portion of the study telephone script
Obtaining prospective, informed consent in clinical research can be challenging and may bias results. This is particularly true in the ED where consent is often obtained by on-shift staff instead of researchers. Furthermore, patients are consented at a time of maximal stress or are unable to consent themselves, and proxies are often not immediately available.4–8 A survey of physician researchers found that some consider the IRB and strict consent rules as significant barriers to research.9 A second study evaluating patient behavior during the ED consent process found that only 13% of patients spend more than two minutes reading consent documents, and only 49% accepted a copy of the documents. Despite efforts to offer patients study information, many ED patients have minimal desire to receive it and spend little time reading consent documents.10 These observations question the need for extensive, immediate, written consent for minimal-risk or observational EM studies.
Evidence also suggests that the act of obtaining immediate consent influences study results. Several patient groups (minorities, pediatrics, geriatrics, uninsured, severely injured) are less likely to consent for ED research, potentially biasing results.4–7 Only one prior study has evaluated a consent process similar to the current study. Patients enrolled into a medication compliance study were randomized to immediate ED consent versus no ED consent.11 Only one of the 149 subjects undergoing telephone follow-up refused to participate, demonstrating the success and willingness of the subjects to be included in observational research studies without their knowledge. Furthermore, patients unaware of the study (the no ED consent cohort) had lower medication compliance rates, which was due to their lack of awareness regarding the study. The Hawthorne effect suggests that patient behavior may be influenced by the knowledge that they are being observed, therefore altering the reliability of study results.11–13
The ethical foundations for research were set forth in the Belmont Report, and include beneficence, protection of patient autonomy, and justice.1 Although beneficence and justice are primarily protected by the IRB and its decision to approve the study, informed consent is central to maintaining patient autonomy. For several reasons, deferred telephone consent may be preferable to written informed consent in minimal-risk, non-interventional EM research requiring telephone follow-up. Deferred telephone consent simplifies ED enrollment procedures and allows for a complete discussion of study enrollment at a time that is optimal for both patients and investigators. Our results support previous work demonstrating very high enrollment rates using deferred telephone consent, which decreases the risks of systemic bias associated with the consent process. Patients who are enrolled and then consented later are initially unaware that they are being observed, decreasing the potential for the Hawthorne effect to influence results. We believe that deferred consent models (telephone or otherwise) should be considered a viable means of consent in non-interventional studies requiring patient contact at a later date.
Future work should focus on deferred consent protocols in different patient populations and ages, in particular for enrollment of pediatric subjects. Technological advances, such as electronic mail, internet, and/or video-conferencing may also provide other (novel) means for obtaining delayed consent and could be investigated.
LIMITATIONS
Our study population was relatively homogeneous, consisting primarily of insured, older patients with blunt head trauma. Therefore, the high rate of successful telephone consent may not be generalizable to other patient populations. Age, ethnicity, insurance status, and injury severity are associated with variable informed consent rates.4–7 Although we did not collect data on patient ethnicity, the high rate of consent implies no effect of ethnicity.
We were unable to confirm the legal status of family surrogates contacted during telephone follow-up calls (similar to use of surrogate consent in the ED). Therefore, it is conceivable that a surrogate caregiver could misrepresent his or her actual legal ability to provide informed consent. We believe the likelihood of this occurring is rare, and that the actual risk to the patient, should such misrepresentation occur, is small.
Finally, a randomized controlled comparing consent in the ED versus consent at home would better address this issue. Unfortunately, the design of the parent study did not allow such a trial.2
CONCLUSIONS
We achieved a very high rate of successful telephone follow-up in this predominantly older ED population. Obtaining study consent using a deferred, telephone contact process is effective and well-received by both subjects and surrogates. IRBs should strongly consider deferred telephone consent for minimal-risk studies requiring telephone follow-up, as opposed to a consent process requiring written documentation at the time of initial ED visit.
Acknowledgments
Funding: This work was supported by the Garfield Memorial Fund (Kaiser Permanente). Dr. Nishijima was supported through a Mentored Clinical Research Training Program Award (K30 and KL2), grant UL1 RR024146 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research.
Footnotes
Presented in part at the Annual Meeting of the Society for Academic Emergency Medicine, Phoenix, AZ, June 2010
References
- 1.The National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research, Report of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. Elkridge, MD: 1979. April 18, 1979. [Google Scholar]
- 2.Nishijima DK, Offerman SR, Ballard DW, et al. Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. Ann Emerg Med. 2012;59:460–8. doi: 10.1016/j.annemergmed.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.State of California. Experimental Research Subject’s Bill of Rights. Available at: http://ag.ca.gov/research/pdfs/bill_of_rights.pdf. Accessed Feb 1, 2013.
- 4.Holmes JF, Holubkov R, Kuppermann N. Guardian availability in children evaluated in the emergency department for blunt head trauma. Acad Emerg Med. 2009;16:15–20. doi: 10.1111/j.1553-2712.2008.00293.x. [DOI] [PubMed] [Google Scholar]
- 5.Dutton RP, Stansbury LG, Hemlock B, Hess JR, Scalea TM. Impediments to obtaining informed consent for clinical research in trauma patients. J Trauma. 2008;64:1106–12. doi: 10.1097/TA.0b013e318165c15c. [DOI] [PubMed] [Google Scholar]
- 6.Glickman SW, Anstrom KJ, Lin L, et al. Challenges in enrollment of minority, pediatric, and geriatric patients in emergency and acute care clinical research. Ann Emerg Med. 2008;51:775–80. doi: 10.1016/j.annemergmed.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Mitchell AM, Kline JA. Systematic bias introduced by the informed consent process in a diagnostic research study. Acad Emerg Med. 2008;15:225–30. doi: 10.1111/j.1553-2712.2008.00066.x. [DOI] [PubMed] [Google Scholar]
- 8.Monico E, Larkin GL, Degutis L. Informed consent for research: current practices in academic emergency medicine. Acad Emerg Med. 2008;15:573–6. doi: 10.1111/j.1553-2712.2008.00098.x. [DOI] [PubMed] [Google Scholar]
- 9.Whitney SN, Alcser K, Schneider C, McCullough LB, McGuire AL, Volk RJ. Principal investigator views of the IRB system. Int J Med Sci. 2008;5:68–72. doi: 10.7150/ijms.5.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baren J, Campbell CF, Schears RM, Shofer FS, Datner EM, Hollander JE. Observed behaviors of subjects during informed consent for an emergency department study. Ann Emerg Med. 2010;55:9–14. doi: 10.1016/j.annemergmed.2009.09.023. [DOI] [PubMed] [Google Scholar]
- 11.Campbell SG, McCarvill EM, Magee KD, Cajee I, Crawford M. The consent and prescription compliance (COPRECO) study: does obtaining consent in the emergency department affect study results in a telephone follow-up study of medication compliance? Acad Emerg Med. 2008;15:932–8. doi: 10.1111/j.1553-2712.2008.00234.x. [DOI] [PubMed] [Google Scholar]
- 12.Murray M, Swan AV, Kiryluk S, Clarke GC. The Hawthorne effect in the measurement of adolescent smoking. J Epidemiol Comm Health. 1988;42(3):304–6. doi: 10.1136/jech.42.3.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kohli E, Ptak J, Smith R, Taylor E, Talbot EA, Kirkland KB. Variability in the Hawthorne effect with regard to hand hygiene performance in high- and low- performing inpatient care units. Infect Control Hosp Epidemiol. 2009;30:222–5. doi: 10.1086/595692. [DOI] [PubMed] [Google Scholar]


