Abstract
Objectives
To compare the impact of negotiated vs. mainstreamed follow-up with telephone reinforcement (TR) on maintenance of physical activity (PA) after Fit and Strong! ended.
Methods
A multisite comparative effectiveness trial with repeated measures.
Results
Single group random effects analyses showed significant improvements at 2, 6, 12, and 18 months on PA maintenance, lower-extremity (LE) pain and stiffness, LE function, sit-stand, 6-minute distance walk, and anxiety/depression. Analyses by follow-up condition showed persons in the negotiated with TR group maintained a 21% increase in caloric expenditures over baseline at 18 months, with lesser benefits seen in the negotiated-only, mainstreamed-with-TR, and mainstreamed-only groups. Significant benefits of telephone dose were also seen on LE joint stiffness, pain, and function as well as anxiety and anxiety/depression.
Conclusions
The negotiated follow-up contract that Fit and Strong! uses, bolstered by TR, is associated with enhanced long-term PA maintenance and health outcomes.
Keywords: maintenance, trial, physical activity, arthritis, fit and strong
Osteoarthritis (OA) is the most common chronic condition among older adults and also constitutes a major barrier to their participation in physical activity.1–3 Lower-extremity joint impairment, in particular, that is caused by OA is a known risk factor for disability and institutionalization.4,5 To date, 15 randomized trials of exercise interventions have been conducted among persons with OA. Most trials report positive short-term outcomes at 3 months or less. Only 5 have reported mixed findings on longer-term adherence and related outcomes.5–9 Three of the 5 used telephone reinforcement (TR) for the maintenance phase of their studies; however, these trials did not explicitly examine the effect of this technique on maintenance itself. This paucity of data on maintenance and facilitators of maintenance of exercise behavior among persons with OA indicates an urgent need for additional studies of this issue.
Fit and Strong! is an evidence-based physical activity/behavior-change program that effectively targets this highrisk group.10,11 Fit and Strong! addresses documented strength and aerobic deficits in this population12,13 and is inexpensive and simple to replicate as demonstrated by the fact that it has been adopted by 42 community providers to date. It is a group and facility-based program that meets for 90 minutes 3 times per week for 8 weeks (24 sessions total). The first 60 minutes consist of a multiple-component exercise program that incorporates flexibility/balance, aerobic walking and/or low impact aerobics, and lower-extremity strength training using elastic exercise bands and adjustable ankle cuff weights. The remaining 30 minutes of each session are devoted to group problem solving and education using a curriculum designed to facilitate arthritis symptom management, self-efficacy (SE) for exercise, and commitment to lifestyle change. In Week 6, participants meet with instructors to negotiate an individualized physical activity plan of their choice that can include home-based exercise or an ongoing group/ facility-based program, or some combination of the 2, with the goal of maintaining 20 minutes of flexibility, 20 minutes of aerobic and 20 minutes of resistance training a minimum of 3 times per week. This plan becomes a physical activity maintenance contract that each participant signs at a graduation ceremony on the last day of class.
We previously tested the efficacy of Fit and Strong! in a randomized trial with 215 treatment and control participants.10,11 Relative to controls, treatment participants experienced statistically significant improvements in SE for exercise, exercise participation, and lower-extremity (LE) stiffness at the conclusion of Fit and Strong!, 8 weeks from baseline. These benefits were maintained at 6 months when several other outcomes also were significant, including: increased time-adherence efficacy, reduced LE pain, and a marginally significant increase in SE for arthritis pain management. Despite a substantially smaller sample size at 12 months, significant treatment effects were maintained on SE for exercise and exercise participation, which were accompanied by marginally significant reductions in LE stiffness and pain. No adverse health effects were reported. Effect sizes for SE for exercise and for exercise participation were 0.798 and 0.713, and 0.905 and 0.669, respectively, in the treatment group at 6 and 12 months. The exercise component of Fit and Strong! was originally designed and taught by licensed physical therapists but is now taught by certified exercise instructors. A prior examination of outcomes under both instruction modes showed almost identical participant benefits.14
In 2003, we obtained funding from the National Institutes of Health cross-institute Maintenance of Long Term Behavior Change initiative to compare different methods of bolstering maintenance of physical activity among Fit and Strong! participants after the formal training program ended. Currently, effective methods of facilitating long-term maintenance of physical activity among older adults with OA are not well understood. Social cognitive theory suggests that the development of the individualized, negotiated contract for postintervention maintenance that is currently used by Fit and Strong! is an effective means of achieving this goal.15 The negotiated approach is believed to be effective because it helps program participants identify outcomes of behaviors that are both personally meaningful and achievable.16,17 On the other hand, it is also possible that the ability to refer Fit and Strong! graduates to an ongoing multiple -component group/ facility-based program in the same location (mainstreaming) might minimize barriers to physical activity maintenance. 18–20 This trial tested the comparative effectiveness of these 2 approaches.
Finally, in addition to scant knowledge regarding the effectiveness of the above strategies in bolstering long-term maintenance of physical activity, little is also known about the effectiveness of TR used as a supplement to them.21,22 This study sought to add to knowledge in this area by testing the comparative effectiveness of these 4 different strategies on bolstering maintenance of physical activity among older adults with OA at 6, 12, and 18 months.
METHODS
Design
We used a randomized trial with re peated measures to assess the comparative effects of 2 different ways of bolstering long-term maintenance of physical activity after the 8-week Fit and Strong! program ended. All study participants first enrolled in Fit and Strong! (N=486). At 6 weeks, 419 program completers were randomized to either a negotiated maintenance arm or a mainstreamed arm. Randomization sequences were determined using our own custom software designed to achieve balanced allocation of cases to conditions stratified by arthritis severity. Neither participants nor researchers were blinded to study group. Negotiated participants developed the customary Fit and Strong! individualized maintenance contract that reflected their preferences for an exercise plan post Fit and Strong!. Mainstreamed participants were asked to enroll in a follow-up best-practice group/facility-based multiple-component program offered at the same facility. Half of the participants in both arms were then randomly assigned to receive TR that tapered off over time. Maintenance of physical activity and associated outcomes were assessed at 2, 6, 12, and18 months. Thus, the study used a 2 by 2 factorial design implemented in a multisite randomized trial to assess the time-related effects of negotiated versus mainstreamed follow-up, the main effect of TR versus no TR, and the interaction between follow-up group and receipt of TR on maintenance of physical activity over time.
Setting
The study was conducted at 7 local senior centers in Chicago. Participants were community-dwelling older adults with lower-extremity OA who were recruited by newsletters, local media announcements, and presentations to senior groups. All study methods, measures, and consent procedures were reviewed and approved by the University of Illinois at Chicago Institutional Review Board.
Procedures
Ten trained interviewers scheduled and conducted pre- and posttest measurement. At each measurement time point, participants filled out a self-report survey questionnaire on-site that was accompanied by objective performance measures and body mass index (BMI) taken by the trained interviewers. If participants could not travel to the site for the interview, the survey was mailed or administered over the phone, but no objective or performance measures were obtained.
Inclusion/exclusion criteria
Persons were considered ineligible if they were under 60, currently participated in an exercise program, had undergone uncomplicated hip or knee surgery within the previous 6 months or complicated surgery within the past year, had received steroid injections within the previous 3 months, had moderate to severe cognitive impairment, had rheumatoid arthritis, or had diabetes or blood pressure that was not under good control. We used the 10-item Short Portable Mental Status Questionnaire to screen for presence of moderate to severe cognitive impairment. 23 Persons who had more than 3 errors were excluded from participation. Potential enrollees were also examined by the study rheumatologist to determine clinical presence of OA of the hip or knee and to rate degree of functional significance using a modified version of the American College of Rheumatology (ACR) Functional Class.24–26
The interventions
All participants enrolled in the evidence-based 8-week Fit and Strong! program described above that combines flexibility/balance, aerobic walking, and strength training with health education for sustained behavior change.10,11 Eighteen instructors: (6 licensed physical therapists and 12 certified exercise instructors) were trained and implemented the program at 7 senior centers over the 4 years that Fit and Strong! was offered.
In the sixth week of Fit and Strong!, participants were randomized to one of 4 maintenance treatment groups in order to test the differential effectiveness of strategies for supporting long-term behavior change: (a) negotiated maintenance with TR, (b) negotiated maintenance with no TR, (c) mainstreamed to facility-based exercise program with TR, (d) mainstreamed to facility-based exercise program with no TR. Participants in the negotiated arm met with the Fit and Strong! instructor between weeks 6 and 8 to develop individualized, negotiated follow- up plans for physical activity maintenance. These meetings systematically explored participants’ preferences for type, time, and location of follow-up physical activity. Participants were asked if they preferred to exercise in a group, with a buddy, or on their own; using equipment or not; and what time of day and type of exercise they preferred. For example, participants in this group could choose to attend a facility-based class; use facility-or home-based equipment; use walking, cycling, low-impact aerobics, swimming, or some combination thereof for their aerobic activity. However, the plan had to meet the criterion of 20 minutes of flexibility, 20 minutes of aerobic and 20 minutes of strengthening exercise a minimum of 3 times per week. In contrast, participants in the mainstreamed arm were referred to an existing group/facility- based best-practice program offered at the same senior center. The best-practice program provided a balanced program of flexibility, aerobic and strength training exercise and met for one hour 3 times per week on an ongoing basis.27
The protocol for participants in both the negotiated and mainstreamed study arms who received TR specified the receipt of 2 phone calls per month in months 3–6 post-Fit and Strong! and one phone call per month between months 7 and 18. During the month-18 phone call, participants were given a hotline number to call for assistance if needed during the following 6 months. All phone calls asked whether participants were still exercising, what they were doing, and explored barriers and facilitators to exercise. Phone discussions were brief, lasting about 10 to 20 minutes per call. TR was conducted by the master’s-level project manager and 4 graduate students using instruments created by the research team to conduct and document each call. All study staff received training before administering calls. Training focused on background and application of the transtheoretical model and motivational interviewing (MI) principles, described how to monitor physical activity participation, and provided strategies for setting goals, solving problems, and reinforcing progress.28–30
Measures
The following outcomes were assessed at baseline; at the end of the 8-week Fit and Strong! program; and at 6, 12, and 18 months for all participants.
Primary Outcome
Physical activity maintenance
We used the self-report Community Healthy Activities Model Program for older adults (CHAMPS) to assess maintenance of physical activity. The CHAMPS assesses participation in leisure-time, moderate, and vigorous physical activity and nonexercise activities like reading or attending church. It provides frequencies of exercise participation and estimates of weekly caloric expenditure, and is valid, reliable, and sensitive to change.31 The CHAMPS enables researchers to calculate measures of physical activity caloric expenditure and frequency for (a) activities of at least moderate intensity (MET value >= 3.0); and (b) all specified physical activities, including light intensity. These features make it possible to compute 4 variables: caloric expenditure all activity, caloric expenditure for moderate activity, frequency of all activity, and frequency of moderate activity. Reliability analyses in the current sample found a Cronbach alpha of 0.72.
Secondary Outcomes
WOMAC
We used the Western Ontario and McMasters University Osteoarthritis Index (WOMAC) self-report instrument to examine LE pain (5 items), stiffness (2 items), and physical function (17 items), with Cronbach alphas of 0.81, 0.74, and 0.95, respectively, in the current sample.32
Functional lower-extremity muscle strength
We used the timed-stand test in the method described by Guralnik to functionally assess LE muscle strength and endurance.33 Participants rose unassisted from a seated position in a chair without arms and then repeated the procedure 5 times as quickly as possible. Raw scores were transformed into a rate per minute to assess change in those who were unable to perform the test at any point.
Functional exercise capacity
We used the 6-minute distance walk test to measure functional exercise capacity.34 Participants walked for 6 minutes, accompanied by research staff who used a Rolatape to measure distance walked in feet.
Body Mass Index (BMI)
Interviewers measured participants’ height without shoes, rounding to the nearest eighth of an inch, and measured participants’ weight without coat or shoes, rounding to the nearest pound.35 We used the same brand and model of equipment to measure height and weight across all sites.
Depression
We used the self-report GERI-AIMS depression, anxiety, and combined depression/anxiety measure as well as the Center for Epidemiological Study-Depression scale to measure depression and anxiety among participants. 36,37 Reliability analyses indicated alphas of 0.73 for the GERI-AIMS depression, 0.72 for anxiety, and 0.82 for the combined depression/anxiety measure.
Independent Variables
The primary independent variable was group membership, which we coded 1 for negotiated and 0 for mainstreamed. We further coded 1 for receipt of telephone reinforcement and 0 for those not receiving telephone reinforcement. Finally, we included a continuous variable in the model to indicate the total number of telephone calls received during the maintenance follow-up period. Participant demographic variables included age, race, sex, income, and education.
American College of Rheumatology (ACR) Functional Class, as determined by the study rheumatologist was included in the models as a covariate.24 Arthritis functional class is a measure of the impact of arthritis severity on functional ability.
Analyses
We estimated sample sizes using methods outlined by Rochon (1998).38 Based on Rochon’s applications of generalized estimating equations to power computations—a very conservative approach—we concluded that a sample size of 600 would have the power of 0.8 to detect effects of one quarter to one half of a standard deviation in the CHAMPS measures. This baseline sample size was anticipated to accommodate a 33% attrition rate between baseline and 18 months. To account for repeated measures, we examined overall patterns of change over time in study outcomes using a random intercept model, which assumes that data are missing at random (MAR) conditional on covariates. We first conducted a set of analyses controlling for site and found no significant site effects. Therefore, we did not include site as a variable in the analyses. We then analyzed data for the entire sample at baseline, 2, 6, 12, and 18 months to assess the effect of Fit and Strong! on change in study outcomes over time without regard to follow-up maintenance condition. Finally, we examined study outcomes at 6, 12, and 18 months as a function of maintenance treatment, receipt of TR, and their interaction. This analysis treated time nonlinearly by including indicator variables for the 6-, 12- and 18-month measurement time points. We used the 2-month posttest as the new baseline measure because participants were randomly assigned to a follow-up treatment at that time. Prior to analysis a few extreme cases reporting implausible values on the 2 CHAMPS Frequency of Physical Activity measures were rescaled to the 90th percentile of the original distribution for all respondents. We also used the natural logs of caloric expenditure for all physical activity, caloric expenditure for moderate physical activity, and the 6-minute distance walk to address the considerable variability on these measures in this sample. The crucial tests in the model are the interactions of the main effects for the Phone/No Phone by time and the 3-way interaction of Neg/Main × Phone/No Phone × Time.
The random effects model for the data can be written as
Yit=b0 + b1Negotiated + b2Phone + b3Time6 + b4Time12 + b5Time18 + b6Negotiated*Time6 + b7Negotiated *Time12 + b8Negotiated*Time18 + b9Phone*Time6 + b10Phone*Time12 + b11Phone*Time18 +b12Negotiated*Phone+ b 13 Negotiated*Phone*Time 6 + b 14 Negotiated*Phone*Time 12 + b15Negotiated*Phone*Time18+b16ARA+ b17TotalCalls + ui + eit
where b6 – b8 test the negotiated by time interaction, b9 – b11 test the phone by time interaction and b13 – b15 test the 3-way interaction of negotiated by phone by time. Because the actual number of TR calls varied by subject, we also included a variable with the total number of TR calls received. Finally, we included one covariate, arthritis functional class, in order to control for baseline disease severity.
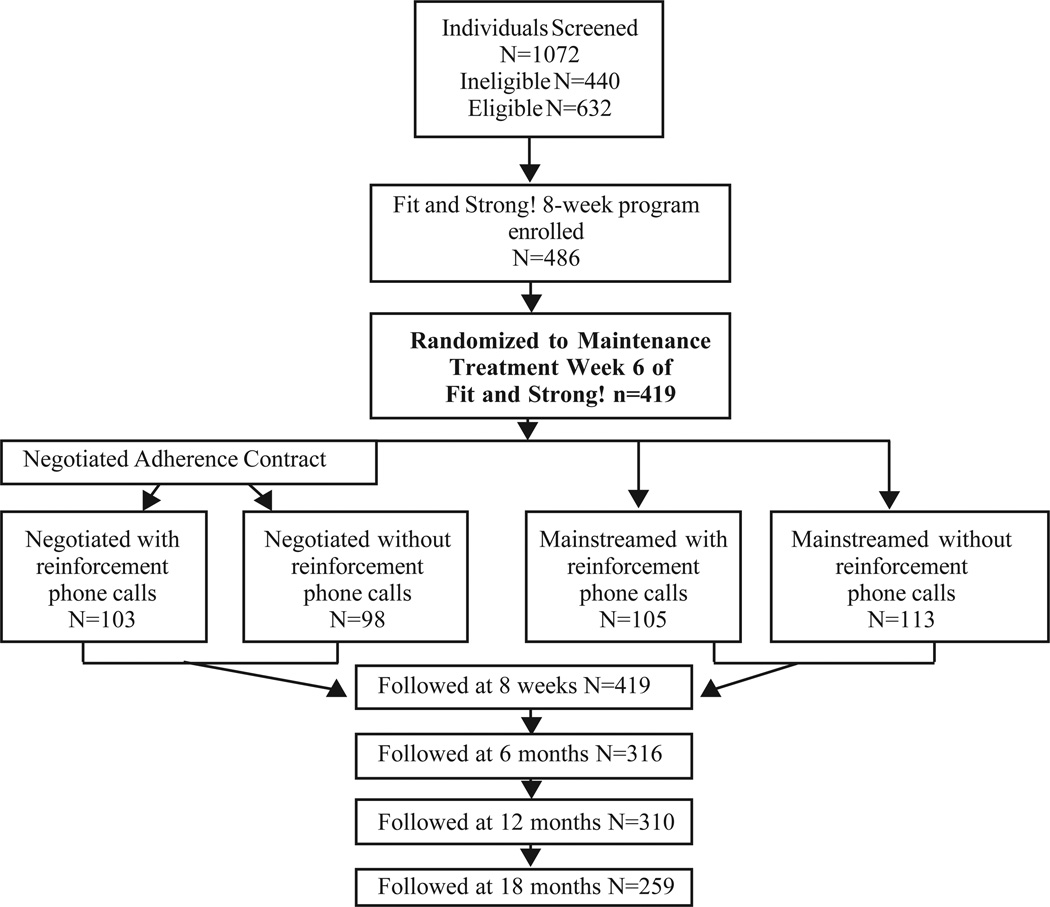
RESULTS
As shown in Figure 1, 1072 persons were screened for eligibility. Of these, 632 were deemed eligible, and 486 (77%) were enrolled in and attended the first class of Fit and Strong! Of the 146 persons who were deemed eligible but did not attend, the most common reasons were inability to contact (28%), change in health status (27%), and other time commitments (14%). Table 1 shows baseline characteristics of the total sample and the characteristics of persons randomly assigned to the maintenance treatment subgroups in Week 6 of Fit and Strong!. Overall, participants had a mean age of 71.1 and the majority were female. A majority of participants (56%) were ethnic minorities, including 49% who were African American and 7% who were Hispanic. A majority had at least a high school education; 34% had annual incomes less than $20,000; and 74% had Class 2 ARA functional class scores, indicating a moderate amount of arthritis functional impairment. Approximately 60% of the total sample also reported presence of hypertension, 23% reported diabetes, and 15% reported presence of other cardiovascular disease. No significant differences were noted by maintenance treatment group on any demographic or disease measures.
Figure 1.
Clinical Flow Diagram
Table 1.
Fit and Strong! Baseline Demographic and Disease Characteristics: By Groupa
| Total N=419 % or mean |
Neg-Tel N=103 % or mean |
Neg-No Tel N=98 % or mean |
Main-Tel N=105 % or mean |
Main-No Tel N=113 % or mean |
|
|---|---|---|---|---|---|
| Age (mean) | 71.1 | 71.31 | 70.88 | 71.27 | 71.06 |
| Range | (59–91) | (60–89) | (60–90) | (59–90) | (60–91) |
| Gender | |||||
| Female | 86.6 | 85.5 | 83.7 | 84.8 | 89.4 |
| Race | |||||
| African American | 49.4 | 43.7 | 54.1 | 53.3 | 46.9 |
| White/Caucasian | 35.8 | 37.9 | 32.7 | 33.3 | 38.9 |
| Hispanic | 7.4 | 7.8 | 10.2 | 6.7 | 5.3 |
| Asian/Pacific Islander | 3.1 | 5.8 | 2.0 | 3.8 | 0.9 |
| Native American | 1.9 | 2.9 | 1.0 | 1.0 | 2.7 |
| Other | 2.4 | 1.9 | 0 | 1.9 | 5.3 |
| Education | |||||
| < High School | 11.9 | 8.8 | 18.9 | 11.8 | 8.11 |
| High School | 21.6 | 24.5 | 12.6 | 23.5 | 23.4 |
| > High School | 66.5 | 66.6 | 68.4 | 64.7 | 68.4 |
| Income | |||||
| <$20,000 | 34.1 | 40.5 | 33.1 | 34.6 | 29.2 |
| ARA Functional Class II | 73.5 | 69.9 | 72.1 | 76.1 | 75.8 |
| Chronic Conditions | |||||
| Hypertension | 60.4 | 55.0 | 61.9 | 73.1 | 52.3 |
| Diabetes | 23.4 | 24.0 | 23.5 | 25.7 | 20.7 |
| Cardiovascular Disease | 15.3 | 14.0 | 17.4 | 17.3 | 12.7 |
No significant difference by group
Posttest Attrition
On average, enrollees attended 19 of 24, or 79.2%, of Fit and Strong! classes. Of the 486 enrollees, 419 (86%) were still attending Fit and Strong! and were randomized to one of the 4 follow-up treatment conditions in week 6 and also completed the 8-week posttest. Of the 419, 316 (75.4%) completed the 6-month posttest, 310 (74%) completed the 12- month posttest, and 259 (62%) completed the 18-month posttest. Overall reasons for loss to follow-up include 91 unable to locate, 29 unable to schedule, and 40 refused. A logistic regression model compared those who remained in the study (responders) to those who left (nonresponders). We regressed a variable indicating continued participation in the study on each of the baseline values of the outcome variables, a dummy variable indicating maintenance treatment condition, and the interaction of the 2. The analyses found no statistically significant differences between responders and nonresponders on demographic characteristics, arthritis severity, or on the baseline values of the outcome measures (not shown). The attrition rate for responders and nonresponders did not differ by maintenance treatment condition (P=0.129). There were no significant effects of attrition either on experimental condition or by experimental condition interactions, eg, negotiated with and without TR, etc.
Total Sample Outcomes Over Time
Table 2 presents pre-posttest findings on outcomes for the entire sample of participants irrespective of follow-up treatment condition.
Table 2.
Fit and Strong! Total Sample Outcomes: Baseline, 2, 6, 12 and 18 Months Findings Over Time
| ARA Class Coefficient Z P-value |
2 mos Coefficient Z P-value |
6 mos Coefficient Z P-value |
12 mos Coefficient Z P-value |
18 mos Coefficient Z P-value |
|
|---|---|---|---|---|---|
| Physical Activity Maintenance | |||||
| Caloric | −0.172 | 0.308 | 0.143 | 0.117 | 0.067 |
| Expenditure | −2.48 | 6.77 | 2.81 | 2.24 | 1.20 |
| (all)a | 0.013 | 0.000 | 0.005 | 0.025 | 0.229 |
| Caloric | −0.124 | 0.338 | 0.138 | 0.103 | 0.027 |
| Expenditure | −1.47 | 5.38 | 1.93 | 1.42 | 0.36 |
| (mod)a | 0.142 | 0.000 | 0.054 | 0.156 | 0.719 |
| Frequency of | −2.412 | 4.107 | 2.254 | 2.840 | 3.085 |
| Physical | −2.97 | 7.41 | 3.69 | 4.57 | 4.70 |
| Activity (all) | 0.001 | 0.001 | 0.001 | 0.001 | 0.000 |
| Frequency of | −0.942 | 3.156 | 1.570 | 1.696 | 1.408 |
| Physical | −2.54 | 12.45 | 5.62 | 5.97 | 4.69 |
| Activity (mod) | 0.006 | 0.000 | 0.000 | 0.000 | 0.000 |
| WOMAC | |||||
| Pain | 0.775 | −0.488 | −0.320 | −0.602 | −0.392 |
| 2.70 | −2.98 | 1.76 | −3.29 | −2.00 | |
| 0.007 | 0.003 | 0.078 | 0.001 | 0.046 | |
| Stiffness | 0.298 | −0.517 | −0.489 | −0.603 | −0.535 |
| 2.35 | −6.40 | −5.48 | −6.66 | −5.51 | |
| 0.019 | 0.000 | 0.000 | 0.000 | 0.000 | |
| Physical | 4.489 | −2.663 | −2.725 | −2.689 | −2.716 |
| Function | 4.49 | −5.08 | −4.66 | −4.59 | −4.35 |
| 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | |
| Objective Measures | |||||
| Timed -stand | −0.955 | 3.334 | 3.112 | 2.766 | 2.582 |
| rate/minute | −1.55 | 9.52 | 7.85 | 6.80 | 6.15 |
| 0.120 | 0.000 | 0.000 | 0.000 | 0.000 | |
| 6-minute | −0.156 | 0.060 | 0.099 | 0.079 | 0.077 |
| distance walka | −4.42 | 2.91 | 4.29 | 3.29 | 3.07 |
| 0.000 | 0.004 | 0.000 | 0.001 | 0.002 | |
| BMI | 0.569 | −0.128 | −0.136 | −0.309 | 0.201 |
| 1.27 | −0.63 | −0.65 | −1.43 | 0.88 | |
| 0.204 | 0.531 | 0.516 | 0.151 | 0.377 | |
| GeriAIMS | 0.118 | −0.239 | −0.142 | −0.170 | −0.081 |
| depression | 0.95 | −3.10 | −1.68 | −1.97 | −0.89 |
| 0.343 | 0.002 | 0.094 | 0.049 | 0.372 | |
| GeriAIMS | 0.167 | −0.384 | −0.319 | −0.329 | −0.368 |
| anxiety | 1.20 | −4.59 | −3.46 | −3.52 | −3.72 |
| 0.232 | 0.000 | 0.001 | 0.000 | 0.000 | |
| GeriAIMS | 0.136 | −0.307 | −0.216 | −0.239 | −0.211 |
| depression/ | 1.16 | −4.61 | −2.94 | −3.21 | −2.68 |
| anxiety | 0.248 | 0.000 | 0.003 | 0.001 | 0.007 |
| CES-D | 0.006 | −1.435 | −0.197 | −0.133 | 0.258 |
| 0.02 | −7.57 | −0.92 | −0.56 | 0.96 | |
| 0.985 | 0.000 | 0.358 | 0.573 | 0.338 |
Note.
Natural log of outcome variable used in analyses
Primary Outcome: Physical Activity Maintenance
Data in Table 2 show that participants as a whole improved significantly at the 8-week conclusion of Fit and Strong! on caloric expenditure for all physical activity at 8 weeks and maintained this improvement at 6 and 12 months. They also improved in caloric expenditure for moderate activity at 8 weeks and maintained a borderline improvement (P=0.054) at 6 months that was not maintained at 12 and 18 months. Participants also improved significantly at all time points on frequency of all physical activity and frequency of moderate physical activity.
Secondary Outcomes
WOMAC LE pain decreased significantly at 2, 12, and 18 months, whereas LE stiffness and physical function improved significantly at all time points. Participants also improved significantly on functional LE muscle strength (timed stand) and functional exercise capacity (6-minute distance walk) at 2, 6, 12, and 18 months; however, no difference was seen between baseline and posttests on BMI. Finally, participants had significantly lower GERI-AIMS depression scores at 2 and 12 months, as well as lower anxiety and combined depression-anxiety scores at 2, 6, 12, and 18 months. Participants also had significantly lower scores on the CES-D at 2 months that were not maintained at 6, 12, and 18 months.
Treatment Outcomes by Maintenance Group
Primary outcome: PA maintenance
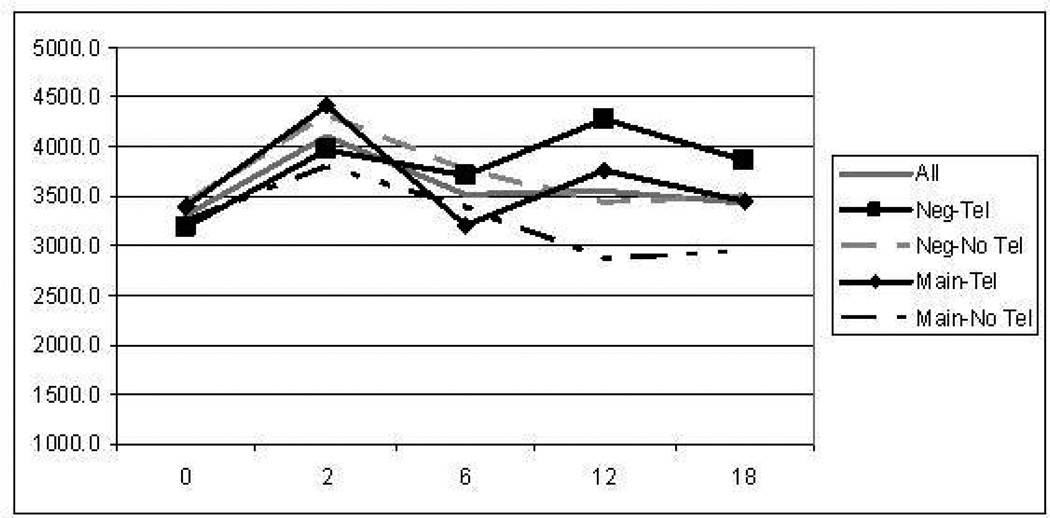
Figure 2 displays the mean values for caloric expenditures for all physical activity by group over time and data in Table 3 show results by group from the random effects modeling. Figure 2 demonstrates that caloric expenditures were maintained at the highest level over time post Fit and Strong! among persons who received negotiated follow-up in conjunction with TR, followed by those in the negotiated-no TR group and the mainstreamed-with-TR group. The lowest performing group with respect to this outcome was the mainstreamed-no-TR group. On average, persons in the negotiated/ TR group increased their caloric expenditure by 788 calories (24.8%) between baseline and the 2-month end of Fit and Strong! At 18 months, on average, persons in this group still maintained a 676 caloric expenditure increase, representing a 21.2% increase over baseline. Data in Table 3 also show a significant positive impact on caloric expenditure for all physical activity at 6 and 12 months for the negotiated-follow-up-with-TR group. A significant decrease was seen on this outcome for those receiving TR at 6 months, but this finding is explained by the interaction of TR with negotiated follow- up. As depicted on Figure 2, participants in the mainstreamed-with-TR arm experienced a substantial decrease on this measure at 6 months. With respect to caloric expenditure for moderate physical activity, one significant positive impact was found at 6 months in the negotiated follow-up arm. However, no other significant effects were found on this outcome for any of the other treatments or time points tested.
Figure 2.
Mean Caloric Expenditure for All Physical Activity by Group Over Time
Table 3.
Outcomes: Random Effects Model: 6-, 12-, and 18-Month Findings by Maintenance Follow-up Conditions
| Neg_6 a Mos Coefficient Z P-value |
Neg_12 Mos Coefficient Z P-value |
Neg_18 Mos Coefficient Z P-value |
Phone_6 b Mos Coefficient Z P-value |
Phone_12 Mos Coefficient Z P-value |
Phone_18 Mos Coefficient Z P-value |
Neg_Ph_ 6 c Coefficient Z P-value |
Neg_Ph_ 12 Coefficient Z P-value |
Neg_Ph_ 18 Coefficient Z P-value |
Total d Calls Coefficient Z P-value |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Physical Activity Maintenance | ||||||||||
| Caloric | −0.135 | −0.097 | 0.093 | −0.352 | −0.099 | 0.112 | 0.483 | 0.335 | −0.054 | −0.007 |
| Expenditure | −1.03 | −0.73 | 0.677 | −2.65 | −0.73 | 0.74 | 2.57 | 1.75 | −0.26 | −0.81 |
| (all)e | 0.152 | 0.233 | 0.2495 | 0.004 | 0.234 | 0.230 | 0.005 | 0.041 | 0.398 | 0.209 |
| Caloric | 0.331 | 0.285 | 0.238 | −0.166 | −0.081 | −0.049 | 0.085 | 0.017 | −0.002 | −0.005 |
| Expenditure | 1.76 | 1.51 | 1.21 | −0.87 | −0.42 | −0.234 | 0.317 | 0.061 | −0.006 | −0.396 |
| (mod)e | 0.040 | 0.066 | 0.114 | 0.193 | 0.337 | 0.408 | 0.376 | 0.476 | 0.498 | 0.346 |
| Frequency | 0.170 | −2.156 | −1.292 | 1.449 | −1.493 | 1.924 | 5.099 | 6.453 | 2.724 | 0.063 |
| of Physical | 0.10 | −1.19 | −0.68 | −0.79 | −0.81 | 0.96 | 1.98 | 2.46 | 0.98 | 0.62 |
| Activity (all) | 0.462 | 0.117 | 0.246 | 0.213 | 0.210 | 0.168 | 0.024 | 0.007 | 0.164 | 0.266 |
| Frequency | 0.598 | −0.436 | 0.109 | −0.060 | −0.447 | 0.824 | 1.269 | 2.251 | 0.575 | 0.015 |
| of Physical | 0.75 | −0.54 | 0.13 | −0.07 | −0.54 | 0.92 | 1.10 | 1.91 | 0.46 | 0.30 |
| Activity (mod) | 0.226 | 0.295 | 0.449 | 0.470 | 0.295 | 0.178 | 0.135 | 0.028 | 0.322 | 0.382 |
| WOMAC | ||||||||||
| WOMAC | −0.428 | −0.223 | −0.618 | 0.191 | −0.084 | −0.519 | −0.401 | 0.002 | 0.390 | −0.078 |
| Pain | −0.86 | −0.44 | −1.161 | 0.37 | −0.16 | −0.90 | −0.55 | 0.00 | 0.49 | −1.97 |
| 0.194 | 0.329 | 0.123 | 0.356 | 0.872 | 0.184 | 0.291 | 0.499 | 0.312 | 0.025 | |
| WOMAC | −0.166 | −0.031 | 0.111 | −0.183 | 0.224 | 0.000 | −0.139 | −0.403 | −0.166 | −0.041 |
| Stiffness | −0.68 | −0.13 | 0.42 | −0.73 | 0.89 | −0.001 | −0.393 | −1.124 | −0.429 | −2.411 |
| 0.249 | 0.450 | 0.337 | 0.234 | 0.376 | 0.500 | 0.347 | 0.131 | 0.334 | 0.008 | |
| WOMAC | −2.404 | 0.186 | −0.785 | −0.922 | 0.796 | −1.191 | 0.658 | −1.903 | −0.725 | −0.356 |
| Physical | −1.58 | 0.12 | −0.49 | −0.57 | 0.50 | −0.675 | 0.293 | −0.845 | −0.299 | −2.397 |
| 0.057 | 0.452 | 0.313 | 0.283 | 0.621 | 0.250 | 0.385 | 0.199 | 0.383 | 0.009 | |
| Objective Measures | ||||||||||
| Time | 0.342 | 0.345 | 0.005 | 0.101 | −1.185 | 1.563 | −1.372 | 0.733 | −1.603 | 0.141 |
| Stand | 0.31 | 0.30 | 0.00 | 0.09 | −1.03 | 1.283 | −0.870 | 0.452 | −0.954 | 1.534 |
| rate/minute | 0.377 | 0.382 | 0.499 | 0.464 | 0.152 | 0.100 | 0.193 | 0.326 | 0.170 | 0.063 |
| 6-minute | −0.011 | 0.012 | −0.054 | −0.091 | −0.101 | −0.258 | 0.091 | 0.026 | 0.261 | 0.004 |
| walke | −0.15 | 0.17 | −0.74 | −1.24 | −1.35 | −3.16 | 0.90 | 0.25 | 2.36 | 1.00 |
| 0.440 | 0.434 | 0.2295 | 0.108 | 0.089 | 0.001 | 0.185 | 0.401 | 0.009 | 0.159 | |
| BMI | −0.002 | −0.043 | −0.351 | 0.027 | −0.130 | 2.097 | 0.450 | 0.441 | −1.865 | −0.064 |
| observed | 0.00 | −0.06 | −0.44 | 0.03 | −0.16 | 2.380 | 0.404 | 0.391 | −1.556 | −0.784 |
| 0.499 | 0.478 | 0.329 | 0.487 | 0.437 | 0.009 | 0.343 | 0.348 | 0.060 | 0.217 | |
| Depression/ Anxiety | ||||||||||
| GeriAIMS | 0.060 | 0.020 | 0.193 | 0.095 | 0.386 | −0.033 | −0.103 | −0.287 | 0.138 | −0.205 |
| depression | 0.24 | 0.12 | 0.731 | 0.37 | 1.50 | −0.12 | −0.29 | −0.79 | 0.36 | −1.56 |
| 0.811 | 0.905 | 0.465 | 0.709 | 0.134 | 0.905 | 0.775 | 0.432 | 0.733 | 0.119 | |
| GeriAIMS | 0.061 | 0.144 | −0.143 | 0.137 | 0.053 | −0.381 | −0.333 | −0.502 | 0.045 | −0.036 |
| anxiety | 0.24 | 0.56 | −0.53 | 0.53 | 0.20 | −1.113 | −0.907 | −1.341 | 0.112 | −1.925 |
| 0.811 | 0.577 | 0.595 | 0.596 | 0.842 | 0.266 | 0.364 | 0.180 | 0.910 | 0.027 | |
| GeriAIMS | 0.041 | 0.061 | 0.013 | 0.066 | 0.179 | −0.204 | −0.175 | −0.344 | 0.115 | −0.030 |
| depression/ | 0.19 | 0.29 | 0.06 | 0.31 | 0.82 | −0.860 | −0.575 | −1.107 | 0.350 | −1.831 |
| anxiety | 0.847 | 0.776 | 0.952 | 0.761 | 0.414 | 0.390 | 0.565 | 0.268 | 0.726 | 0.034 |
| CES-D | 0.612 | −1.104 | 0.426 | −1.099 | 0.610 | 0.352 | −1.590 | −0.848 | −0.833 | −0.013 |
| 1.01 | −1.66 | 0.57 | −1.78 | 0.90 | 0.429 | −1.832 | −0.886 | −0.751 | −0.335 | |
| 0.314 | 0.049 | 0.569 | 0.038 | 0.370 | 0.668 | 0.034 | 0.376 | 0.453 | 0.738 |
Note.
Negotiated (1) vs Mainstreamed (0) follow-up
Phone (1) vs No Phone (0)
Interaction of Negotiated and Phone
Volume of calls
Natural log of outcome variable used in analyses
With respect to frequency of all physical activities, significant positive effects were again seen for the negotiated-follow- up –with-TR-group at 6 and 12 months. No other differences were seen for any other treatment conditions at any other time points for this variable. Finally, significant positive differences were seen for the fourth and final outcome—frequency of moderate physical activity—again for the negotiated-follow-up-with-TR group at 12 months, with no other effects for any other treatments at any time points.
Secondary Outcomes
WOMAC
There were no significant differences on any of the WOMAC subscales by maintenance treatment or TR over time. However, significant improvements were seen on the Pain, Stiffness, and Physical Function subscales with increased “dose” or receipt of TR.
Functional lower extremity strength (timed-stand)
There were no significant differences by maintenance treatment, receipt of TR, their interaction, or dose of TR on the timed-stand test at any time points.
Functional exercise capacity (6-minute distance walk)
A significant improvement on this measure was seen for the negotiated-follow-up-with-TR group at 18 months despite a significant decline at 18 months on this measure among persons receiving TR vs no TR. This finding is explained by a decrease in scores on the measure among the mainstreamed-with-TR group at 18 months compared to all other groups. There was no significant difference on this outcome by telephone dose.
Body Mass Index (BMI)
We saw no significant difference on this outcome as a function of maintenance condition at any time point. We saw a significant increase in BMI at 18 months among persons receiving TR vs those who did not. The interaction of follow-up group by telephone condition was not significant at any time points, and no relationship was seen between this outcome and telephone dose.
Depression
There were no significant differences on the GERI-AIMS depression, anxiety, or combined depression/anxiety measures by follow-up treatment, receipt of TR, or the interaction of the 2 conditions at any time point. However, significant decreases in anxiety and depression/ anxiety were seen with increasing number of telephone calls. With respect to CES-D scores, significant decreases were seen at 12 months in the negotiated-follow-up group. Significant decreases in CES-D scores were also seen for participants in the negotiated-follow-up-with-TR group at 6 months relative to those in the mainstreamed-with-TR condition. There were also significant decreases at 6 months among participants who received TR relative to those who did not, but this latter difference is attributable to the interaction between negotiated group and TR. Interestingly, no relationship was seen on the CES-D between depression and telephone dose.
Adverse health outcomes
No adverse health outcomes were reported by participants.
DISCUSSION
This study examined outcomes to Fit and Strong! over 18 months and found strong effects for the total study sample on maintenance of physical activity and secondary outcomes at 2 months (end of formal program) that were maintained at 6, 12, and 18 months. Specific improvements maintained at 18 months included increased involvement in physical activity, decreased LE pain and stiffness and increased LE function, improved observed LE strength (timed-stands), and observed aerobic capacity (6-minute distance walk), as well as decreased anxiety and depression.
When outcomes were examined by follow-up condition, a clear pattern was seen on the primary study outcome of physical activity maintenance for the interaction between negotiated follow-up and TR. Persons in the negotiated-follow-up condition who also received TR maintained the greatest improvement in caloric expenditure for all physical activity at 18 months (Figure 2) and also showed benefits on this outcome at 6 and 12 months in the random effects analysis. The same interaction effect was seen at 6 and 12 months for frequency of all physical activities and frequency of moderate physical activities at 12 months. These findings strongly support the importance of bolstering the customary negotiated follow-up that Fit and Strong! incorporates with TR.
Two additional effects of negotiated follow-up with TR were seen on the 6-minute distance walk at 18 months and the CESD at 6 months. The next most frequently observed relationship was seen between telephone dose and secondary outcomes. Significant benefits with increased telephone dose were seen on the LE pain, stiffness, and physical function scales of the WOMAC and on the anxiety and depression/anxiety GERI-AIMS scales. Finally, 2 effects of negotiated-follow-up alone were seen on caloric expenditure for moderate physical activity at 6 months and the CES-D at 12 months whereas no benefits were seen for the mainstreamed-only condition. Importantly, when benefits were seen, they tended to be associated with TR in combination with the negotiated-follow-up condition. In the negotiated condition—the customary Fit and Strong! practice—the instructor sits with each participant in weeks 6 and 7 of the program and reviews his or her preferences for and access to different types of physical activity opportunities. On the basis of the informed discussion, the participant develops an individualized maintenance plan, signs it, and takes it home as a contract that will be honored or modified as needed once the formal program ends. It appears from these findings that this negotiated strategy for follow-up maintenance of physical activity, when combined with tapered TR, was more effective than referral without TR to a best-practice multiple-component physical activity program at the same site where Fit and Strong! was offered.
It is important to note that a dose-response relationship between volume of reinforcement calls was seen on 5 secondary outcomes, including LE pain, stiffness, and physical function and the GERIAIMS anxiety and combined depression and anxiety measures. The 3 WOMAC measures assess components of LE joint function that are considered to show the most proximal effects of Fit and Strong! If TR helps participants to maintain and/or refine their negotiated plan, it is reasonable to see an impact of dose on these outcomes and also reasonable that the dose would decrease anxiety and depression that is arthritis specific.
Three other studies have examined the effects of physical activity interventions on participants with knee OA over 18 or 24 months.5,6,9 All 3 tested a facility-based initial treatment in conjunction with TR provided during transition and maintenance phases. All 3 found beneficial effects of the exercise programs on participant outcomes but did not isolate and test the impact of the TR that was offered on maintenance and related outcomes. Thus, this study is unique in directly assessing the impact of TR as an intentional reinforcement adjunct to 2 different types of long-term maintenance strategies.
Finally, it is also important to note that the findings reported here have limitations. We experienced attrition from posttest measurement, particularly at month 18. However, attrition analyses failed to find any systematic impact of membership in each of the 4 study groups on attrition.
We conclude that this study provides strong evidence that the negotiated follow- up incorporated in the current version of Fit and Strong! when coupled with TR is effective in maintaining initial 2-month physical activity gains out to 18 months. Our findings also show the presence of a dose-response between the volume of TR calls received and maintenance of improvement in LE pain, stiffness, and function and arthritis-specific anxiety and depression. Future analyses will examine in greater detail the relationships between barriers and facilitators to exercise maintenance in this sample as well as instances of and circumstances surrounding relapse and reactivation. Finally, an important issue for further study is the comparative effectiveness of other reinforcement mechanisms. Although TR was effective in this study, it is not inexpensive to provide, which may impede its widespread translation and dissemination into community- based settings. Other forms of reinforcement, like participant and instructor videos, will also be important to test if we are to maximize the successful translation of evidence-based programs in the future.
Acknowledgments
This study was funded by the National Institute on Aging (R01 AG23424). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health. We gratefully acknowledge the many participants who took part in the study. We also acknowledge the involvement and significant contribution of the following organizations and individuals: Chicago Department of Senior Services, Greater Chicago Chapter of the Arthritis Foundation, and the UIC Survey Research Lab. The authors gratefully acknowledge the use of software developed by Michael Berbaum, PhD, that was used to stratify and randomly assign study participants.
Contributor Information
Susan L. Hughes, Center for Research on Health and Aging, Institute for Health Research and Policy, University of Illinois Chicago, Chicago, IL..
Rachel B. Seymour, Center for Research on Health and Aging, Institute for Health Research and Policy, University of Illinois Chicago, Chicago, IL..
Richard T. Campbell, Biostatistics, School of Public Health, Institute for Health Research and Policy, Chicago, IL..
Pankaja Desai, Center for Research on Health and Aging, Institute for Health Research and Policy, University of Illinois Chicago, Chicago, IL..
Gail Huber, Assistant Professor, Department of Physical Therapy and Human Movement Sciences, Northwestern University, Chicago, IL..
H. Justina Chang, Fishbein Fellow, JAMA, Chicago, IL..
REFERENCES
- 1.Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation — United States, 2003—2005. Morb Mortal Wkly Rep. 2006 Oct 13;55(40):1089.2–1092.2. [PubMed] [Google Scholar]
- 2.Bolen J, Murphy L, Greenlund K, et al. Arthritis as a potential barrier to physical activity among adults with heart disease — United States, 2005 and 2007. Morb Mortal Wkly Rep. 2009b Feb 27;58(07):165–169. [PubMed] [Google Scholar]
- 3.Bolen J, Hootman J, Helmick CG, et al. Arthritis as a potential barrier to physical activity among adults with diabetes — United States, 2005 and 2007. Morb Mortal Wkly Rep. 2008 May 9;57(18):486–489. [PubMed] [Google Scholar]
- 4.Dunlop D, Hughes SL, Edelman P, et al. Impact of joint impairment on disability and disability-specific domains at four years. J Clin Epidemiol. 1998;51:1253–1261. doi: 10.1016/s0895-4356(98)00128-0. [DOI] [PubMed] [Google Scholar]
- 5.Messier SP, Loeser RF, Miller GD, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the arthritis, diet, and activity promotion trial. Arthritis Rheum. 2004;50:1501–1510. doi: 10.1002/art.20256. [DOI] [PubMed] [Google Scholar]
- 6.Ettinger WH, Jr, Burns R, Messier SP, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST) JAMA. 1997;277:25–31. [PubMed] [Google Scholar]
- 7.Sullivan T, Allegrante JP, Peterson MG, et al. One-year follow-up of patients with osteoarthritis of the knee who participated in a program of supervised fitness walking and supportive patient education. Arth Care Res. 1998;11(4):228–233. doi: 10.1002/art.1790110403. [DOI] [PubMed] [Google Scholar]
- 8.Deyle GD, Henderson NE, Matekel RL, et al. Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee a randomized, controlled trial. Ann Intern Med. 2000;132(2):173–181. doi: 10.7326/0003-4819-132-3-200002010-00002. [DOI] [PubMed] [Google Scholar]
- 9.Thomas KS, Muir KR, Doherty M, et al. Home based exercise programme for knee pain and knee osteoarthritis: randomised controlled trial. BMJ Primary Care. 2002;325(7367):752–756. doi: 10.1136/bmj.325.7367.752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hughes SL, Seymour RB, Campbell RT, et al. Impact of the Fit and Strong! intervention on older adults with osteoarthritis. Gerontologist. 2004;44:217–228. doi: 10.1093/geront/44.2.217. [DOI] [PubMed] [Google Scholar]
- 11.Hughes SL, Seymour RB, Campbell RT, et al. Long-term impact of Fit and Strong! on Older Adults with osteoarthritis. Gerontologist. 2006;46:801–814. doi: 10.1093/geront/46.6.801. [DOI] [PubMed] [Google Scholar]
- 12.Minor MA, Hewett JE, Weber RR, et al. Efficacy of physical conditioning exercise in patients with rheumatoid arthritis and osteoarthritis. Arthritis Rheum. 1989;32:1396–1405. doi: 10.1002/anr.1780321108. [DOI] [PubMed] [Google Scholar]
- 13.Semble EL, Loeser RF, Wise CM. Therapeutic exercise for rheumatoid arthritis and osteoarthritis. Semin Arthritis Rheum. 1990;20:32–40. doi: 10.1016/0049-0172(90)90092-t. [DOI] [PubMed] [Google Scholar]
- 14.Seymour RB, Hughes SL, Campbell R, et al. Comparison of two methods of conducting the Fit and Strong! Program. Arthritis Rheum. 2009;61(7):876–884. doi: 10.1002/art.24517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bandura A. Self-Efficacy: The Exercise of Control. New York: WH: Freeman and Company; 1997. [Google Scholar]
- 16.Stewart AL, Verboncoeur CJ, McLellan BY, et al. Physical activity outcomes of CHAMPS II: a physical activity promotion program for older adults. J Gerontol A Biol Sci Med Sci. 2001;56A:M465–M470. doi: 10.1093/gerona/56.8.m465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jensen GM, Lorish CD. Promoting patient cooperation with exercise programs, linking research, theory, and practice. Arth Care Res. 1994;7:181–189. doi: 10.1002/art.1790070405. [DOI] [PubMed] [Google Scholar]
- 18.Duncan TE, McAuley E. Social support and efficacy cognitions in exercise adherence, a latent growth curve analysis. J Behav Med. 1993;16:199–218. doi: 10.1007/BF00844893. [DOI] [PubMed] [Google Scholar]
- 19.Rhodes RE, Martin AD, Taunton JE, et al. Factors associated with exercise adherence among older adults: an individual perspective. Sports Med. 1999;28:397–411. doi: 10.2165/00007256-199928060-00003. [DOI] [PubMed] [Google Scholar]
- 20.Chao D, Foy CG, Farmer D. Exercise adherence and older adults: challenges and strategies. Control Clin Trials. 2000;21:S211–S217. doi: 10.1016/s0197-2456(00)00081-7. [DOI] [PubMed] [Google Scholar]
- 21.van der Bij AK, Laurant MGH, Wensing M. Effectiveness of physical activity interventions for older adults a review. Am J Prev Med. 2002;22(2):120–133. doi: 10.1016/s0749-3797(01)00413-5. [DOI] [PubMed] [Google Scholar]
- 22.Rubak S, Sandbaek A, Laritzen T, et al. Motivational interviewing: a systematic review and meta-analysis. Brit J Gen Pract. 2005;55(513):305–312. [PMC free article] [PubMed] [Google Scholar]
- 23.Kahn RL, Goldfarb AI, Pollack M, Peck A. Brief objective measures for the determination of mental status in the aged. Am J Psychiatry. 1960;117:120–124. doi: 10.1176/ajp.117.4.326. [DOI] [PubMed] [Google Scholar]
- 24.American Rheumatism Association. Dictionary of the Rheumatic Diseases. Vol. 1. New York: Contact Association International; 1982. [Google Scholar]
- 25.Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis. Arthritis Rheum. 1986;29:1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 26.Altman R, Alarcon G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34:505–514. doi: 10.1002/art.1780340502. [DOI] [PubMed] [Google Scholar]
- 27.Hughes SL, Seymour RB, Campbell RT, et al. Best practice physical activity programs for older adults: findings from the National Impact Study. Am J Public Health. 2009;99:362–368. doi: 10.2105/AJPH.2007.131466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prochaska J, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 29.Miller WR. Motivational interviewing with problem drinkers. Behavioral Psychotherapy. 1983;11:147–172. [Google Scholar]
- 30.Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. New York: Guilford Press; 1991. [Google Scholar]
- 31.Stewart AL, Mills KM, King AC, et al. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc. 2001;33:1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 32.Bellamy N. Pain assessment in osteoarthritis, experience with the WOMAC osteoarthritis index. Semin Arthritis Rheum. 1989;18:14–17. doi: 10.1016/0049-0172(89)90010-3. [DOI] [PubMed] [Google Scholar]
- 33.Guralnik JM, Ferrucci L, Simonsick EM, et al. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk, a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132:919–923. [PMC free article] [PubMed] [Google Scholar]
- 35.Washburn RA, Smith KW, Jette AM, Janney CA. The physical activity scale for the elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 36.Hughes SL, Edelman P, Chang RW, et al. The GERI-AIMS, Reliability and validity of the Arthritis Impact Measurement Scales adapted for elderly respondents. Arthritis Rheum. 1991;34:856–865. doi: 10.1002/art.1780340711. [DOI] [PubMed] [Google Scholar]
- 37.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 38.Rochon J. Application of GEE procedures for sample size calculations in repeated measures experiments. Statistics in Medicine. 1998;17(14):1643–1658. doi: 10.1002/(sici)1097-0258(19980730)17:14<1643::aid-sim869>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]