Abstract
BACKGROUND
This study aimed to explore demographic characteristics and clinical presentations of celiac disease (CD) in Northeastern Iran.
METHODS
This was a cross-sectional retrospective study of 193 adults with CD who presented to Mashhad University Gastroenterology Clinic between 2008 and 2013. Patient data that included mode of presentation and the presence of any concomitant illnesses were collected. Intestinal biopsy and serum anti-tissue transglutaminase (anti-tTG) were used for diagnosis. Mucosal lesions were classified according to modified Marsh classification.
RESULTS
Overall, 132 females and 61 males, with a mean age at diagnosis of 32.6 ± 13.2 years were included. The patient’s chief complaints in order of decreasing frequency were dyspepsia (24.6%), diarrhea (20%), anemia (12.8%), and flatulence (7.2%). Bone disease was seen (osteopenia, osteoporosis) in 30% of patients. A positive family history of CD was found in 17.9% of cases. There were 64% who had serum anti-tTG >200 units/ml and 78% had a Marsh classification grade 3 on duodenal biopsy. The histology grade (Marsh) did not show any correlation with anti-tTG serum levels, age, body mass index (BMI) or hemoglobin levels.
CONCLUSION
In Northeastern Iran, CD was seen more commonly in females and with non-diarrheal presentations. Abdominal discomfort, anemia and bone disease were most common primary presentations in this area. Histology grade showed no significant correlation with level of anti-tTG, BMI or hemoglobin levels. We suggest screening for CD in unexplained abdominal discomfort, bone disease and anemia.
Keywords: Celiac Disease, Clinical Presentation, Iran
INTRODUCTION
Celiac disease (CD) is a chronic immune-based enteropathy caused by dietary gluten (protein in wheat, barley, and rye) in genetically predisposed individuals that resolves with the exclusion of gluten from the diet.1-3 Patients with CD may present with a wide range of gastrointestinal symptoms such as diarrhea, steatorrhea, weight loss, bloating, flatulence, and abdominal pain in addition to non-gastrointestinal abnormalities (liver disease, iron deficiency anemia, bone disease, and skin disorders).3,4 However, many patients with CD may have a clinically silent disease without any symptoms.3 A significant proportion of patients are diagnosed through screening at-risk populations such as family members of patients with CD and insulin-dependent diabetics.5
CD is a common entity with a prevalence of approximately 1% worldwide.6 The highest incidence, 1 per 100 to 1 per 300, of CD is observed in Europe.7,8 However, new epidemiological data indicate that CD is commonly found in Middle Eastern countries, particularly Iran.9 The minimum prevalence of gluten sensitivity in a study among an otherwise healthy urban population of Iranian blood donors has been shown to be 1 per166.10 In another study, the prevalence of gluten sensitivity among the general population of the Northern and Southern parts of Iran was 1 per 104.11
There is a higher frequency of CD in patients with type 1 diabetes and irritable bowel syndrome.2,12 Likewise, a higher prevalence has been noted in patients with inflammatory bowel disease and nonalcoholic fatty liver disease.13,14
Since CD is common in Iran, establishing the demographic characteristics and different clinical manifestations of this disease may provide important information with regards to its timely diagnosis and proper management. To the best of our knowledge, few data exist about the epidemiological and clinical features of adult CD in the Northeastern Iranian province of Khorasan Razavi. Therefore, the aim of this study is to investigate the clinical presentation of adult patients diagnosed with CD in this area.
MATERIALS AND METHODS
This was a retrospective cross-sectional study conducted in a large referral university gastroenterology clinic from 2008 to 2013 in Mashhad Iran.
Patients with CD whose disease was confirmed by upper endoscopy and small bowel biopsy that were classified according to the modified Marsh criteria and evidence of positive serology were included in the study. Patients’ data that included the mode of presentation and presence of concomitant illnesses and symptoms were collected by a questionnaire. These data included demographic characteristics, chief complaints (gastrointestinal and non-gastrointestinal), pathology, endoscopy and laboratory results. An osteocore 2 bone densitometer was used in one center with dual energy x-ray absorptiometry (DEXA). Osteoporosis was defined as a T score ≤ -2.5 SD and osteopenia was defined as a T score between -1 and -2.5 SD. Pathology was reported by an expert gastrointestinal pathologist. All anti-tissue transglutaminase (anti-tTG) serology was checked by a Euroimmune kit in one laboratory.
Two educated and trained researchers under the supervision of an expert gastroenterologist completed the questionnaire data.
The patients’ chief complaints were categorized as gastrointestinal (abdominal pain, diarrhea, constipation, weight loss and flatulence) and non-gastrointestinal (iron deficiency anemia, elevated transaminase levels, skin disease, bone disorders, neurologic symptoms, and thyroid disease).
Statistical analysis
The data was analyzed using the Statistical Package for Social Sciences (SPSS) version 16 (Chicago, IL, USA). Simple statistics were used such as frequency and standard deviation. The chi-square test and Student’s t-test and the Spearman correlation were used for comparisons.
RESULTS
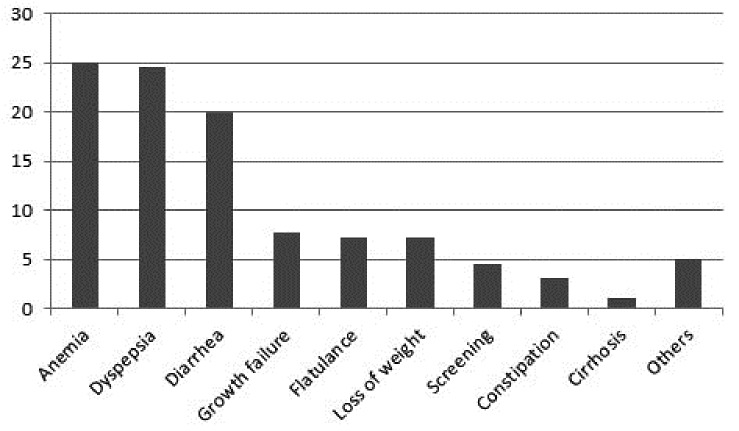
We evaluated a total of 193 patients of which 132 were female (female to male ratio of 2.16:1). The mean age at diagnosis was 32.6 ± 13 years with a significant proportion of patients (32.3%) between 20-30 years of age. The most common chief complaint was dyspepsia (24.6%) followed by diarrhea (20%), anemia (12.8%), short stature (7.7%), flatulence (7.2%), weight loss (7.2%), and constipation (3.1%). Common non-gastrointestinal symptoms consisted of anemia in 60%, and bone disease (osteopenia and/or osteoporosis) in 30%. From 82 patients, a low 25OH D3 was seen in 35 (42%) and an insufficient level was found in 19 (23%) patients. Symptoms of nervous system involvement included neurosis, depression and seizures in 27.7% and skin problems that included allergic dermatitis, dermatitis herpetiformis, alopecia, and koilonychia in 27.7% (Figure 1). Positive serum anti- thyroid peroxidase (anti-TPO) was detected in 29 out of 78 (37%) evaluated patients.
Fig. 1 .
The clinical presentation of celiac patients in Northeastern Iran, 2008-2013 (N= 193).
Concomitant diseases were abortion in 24% (32 from 132 females), dermatitis herpetiformis in 3.1% (6), celiac-induced liver cirrhosis in 1% (2), and cancer in 1% (2) of patients.
A positive family history or CD by active case finding in the family screening was observed in 17.9% of patients.
Mean anti-tTG titers were 100 ± 25 units/ml with serum anti-tTG levels >200 units/ml observed in 118 (60.5%) patients.
In histological evaluation, 2.1% had Marsh 1 lesions, 10.8% presented with Marsh 2 lesions and 78.5% had Marsh 3 lesions. According to the Spearman correlation, there was no significant correlation observed between histology grade according to Marsh criteria and the serum of anti-tTG levels, age, body mass index (BMI) and hemoglobin levels.
DISCUSSION
The results of this study showed that dyspepsia and flatulence were common primary complaints in this group of celiac patients, which is comparable to European countries.15-18 However, present findings contrasted those of previous reports from Iran. For instance, a recent study of 52 patients in Southwestern Iran diarrhea was the most frequent complaint.19 In another study in Tehran, the capital of Iran, a comparative study of 100 Iranian patients with 150 Italian patients was performed. The study showed that diarrhea was the most common complaint in Iranians, while abdominal pain was most common finding in Italian patients.15 Our study showed comparable results with the Italian CD patients.
Celiac patients with non-diarrheal presentations are currently seen more frequently.5 In a large cohort study in the United States, the diarrheal forms of CD in adults has progressively decreased, while the rate of atypical forms and diagnosis by screening is increasing.20-23
In the current study, 60% of patients presented with anemia, which was comparable with a recent study in Tehran, Iran.15 Bone disorders were detected in 30% according to bone densitometry findings. Ehsani-Ardakani et al. have reported a 25% prevalence of bone disorders in CD patients.15 A recent cohort study in Turkey demonstrated a high frequency of metabolic bone diseases and secondary hyperparathyroidism (up to 50%) in untreated cases of CD.22 In our study elevated parathyroid hormone (PTH) was present in 24% of patients who underwent this analysis, whereas vitamin D3 levels was insufficient in 23% and deficient in 42% of patients. Low vitamin D3 levels appeared to have a more important role in bone disorders. Although bone disorder was not a common presenting symptom of our patients, however it was common when we screened the patients.
Dermatitis herpetiformis is a relatively common extra-intestinal manifestation of CD,3 however in our study we have found this manifestation in only 3 (1.5%) patients.
According to our observations, 11.3% of the patients were diagnosed at the age of 50 years and older, which agreed with a recent study that reported 9.3% of patients were over 50 years of age at diagnosis.24 The majority of patients (67.7%) were female, a finding comparable to previous studies conducted in the United States, Europe and the Middle East.16,17 Such a higher frequency rate of CD amongst women might be attributed to the higher incidence of autoimmune diseases found in the female population.
Regarding rates of abortion, our findings of a 24% incidence of abortion in female patients with CD was lower than the 46.9% incidence rate in a recently published study.24 We do not know the prevalence of abortion in the general population; in the current study other causes for spontaneous abortion were not evaluated. However reproductive dysfunction should be considered in CD and affected females should be screened accordingly.25,26
We found no direct correlation between serum anti-tTG levels and histological severity according to the Marsh classification. This contrasted findings by Donaldson et al. who showed that IgA anti-tTG levels ≥100 units were observed almost exclusively in adults and children with Marsh grade 3 duodenal histopathology.27
The frequency of CD was significantly higher in patients who have first-degree family members with CD.28,29 This frequency was 17% in our patients compared to 10% in Turkish patients with CD.30 Patients who presented with non-gastrointestinal complaints had more positive family histories of CD than those with gastrointestinal symptoms (p<0.01)(Table 1). Hence patients with a first-degree family member who has an established diagnosis of CD, particularly with non-gastrointestinal symptoms, should be screened for CD.
Table 1. Characteristics in patients with celiac disease (CD) according to major symptoms during 2008-2013 in Northeastern Iran (N=193).
| Chief complaint | p -value | ||
| Characteristics | GI | Non-GI | |
| Sex |
Female: 69 Male: 33 |
Female: 40 Male: 19 |
0.1 |
| Age (y) | 34.1±12.27y | 34.10±12.6 | 0.96 |
| Weight (kg) | 56.71±12.32 | 53.78±12.7 | 0.17 |
| Height (cm) | 160.38±9.82 | 157.46±11.47 | 0.133 |
| BMI | 21.9±4.02 | 21.35±3.89 | 0.45 |
| Mean anti-tTG serum levels (units/ml) | 218.36±75.95 | 221.34±82.03 | 0.8 |
| Hemoglobin (g/dl) | 12.04±2.2 | 10.46±2.05 | 0.001 |
| Positive family history | 9 | 16 | 0.01 |
GI: Gastrointestinal; non-GI: Non-gastrointestinal; BMI: Body mass index; anti-tTG: Anti-tissue transglutaminase antibody
The rate of detection of CD is increasing worldwide and there has been a substantial change in the mode of presentation of patients with CD over recent years. There is decreased the frequency of diarrheal or classic presentation.31 However a significant proportion of patients with CD remain undiagnosed, which highlights the need for improved strategies in the future to better detect patients with non-gastrointestinal symptoms such as anemia, bone disorders, and spontaneous abortion.31
In conclusion, in northeastern Iran, a significant proportion of patients with CD were female and with non-diarrheal presentation. Therefore, the possibility of CD must be entertained when confronted with atypical symptoms such as unexplained anemia, abdominal discomfort, abortion, and bone and thyroid disorders. First-degree relatives of patients with CD, especially when they present with non-gastrointestinal symptoms should be screened properly.
ACKNOWLEDGMENTS
We would like to thank Mr. Jalil Zolfaghari for his tremendous assistance with laboratory collaboration. We express our appreciation to all of our colleagues (Dr. Ahmad Khosravi Khorashad, Dr. Hasan Vossoghinia, Dr. Ali Mokhtarifar, Dr. Ali Bahari, Dr. Hasan Saadatnia, Dr. Hooman Mozaffari, Dr. Mitra Ahadi, Dr. Mohammadreza Farzanefar, and Dr. Mehdi Hayatbakhsh) in Mashhad who referred patients and assisted with data collection. The authors are grateful to the patients for their kind participation.
CONFLICT OF INTEREST
The authors declare no conflict of interest related to this work.
Please cite this paper as:
Ganji A, Esmaielzadeh A, Aafzal Aghayee M, Goshayeshi L, Ghaffarzadegan K. The Clinical Presentation of Celiac Disease: Experiences from Northeastern Iran. Middle East J Dig Dis 2014;6:93-7.
References
- 1.Chomeili B, Aminzadeh M, Hardani AK, Fathizadeh P, Chomeili P, Azaran A. Prevalence of celiac disease in siblings of Iranian patients with celiac disease. Arq Gastroenterol. 2011;48:131–5. doi: 10.1590/s0004-28032011000200009. [DOI] [PubMed] [Google Scholar]
- 2.Honar N, Karamizadeh Z, Saki F. Prevalence of celiac disease in patients with type 1 diabetes mellitus in the south of Iran. Turk J Gastroenterol. 2013;24:122–6. doi: 10.4318/tjg.2013.0541. [DOI] [PubMed] [Google Scholar]
- 3.Rubio-Tapia A, Hill ID, Kelly CP, Calderwood AH, Murray JA. American College of GastroenterologyACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol. 2013;108:656–76. doi: 10.1038/ajg.2013.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rastogi A, Bhadada SK, Bhansali A, Kochhar R, Santosh R. Celiac disease: a missed cause of metabolic bone disease. Indian J Endocrinol Metab. 2012;16:780–5. doi: 10.4103/2230-8210.100674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Green PH. The many faces of celiac disease: clinical presentation of celiac disease in the adult population. Gastroenterology. 2005;128:S74–8. doi: 10.1053/j.gastro.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 6.Reilly NR, Green PH. Epidemiology and clinical presentations of celiac disease. Semin Immunopathol. 2012;34:473–8. doi: 10.1007/s00281-012-0311-2. [DOI] [PubMed] [Google Scholar]
- 7.Rostami Nejad M, Hogg-Kollars S, Ishaq S, Rostami K. Subclinical celiac disease and gluten sensitivity. Gastroenterol Hepatol Bed Bench. 2011;4:102–8. [PMC free article] [PubMed] [Google Scholar]
- 8.Barada K, Abu Daya H, Rostami K, Catassi C. Celiac disease in the developing world. Gastrointest Endosc Clin N Am. 2012;22:773–796. doi: 10.1016/j.giec.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 9.Rostami Nejad M, Rostami K, Emami MH, Zali MR, Malekzadeh R. Epidemiology of celiac disease in Iran: a review. Middle East J Dig Dis. 2011;3:5–12. [PMC free article] [PubMed] [Google Scholar]
- 10.Shahbazkhani B, Malekzadeh R, Sotoudeh M, Moghadam KF, Farhadi M, Ansari R. et al. High prevalence of celiac disease in apparently healthy Iranian blood donors. Eur J Gastroenterol Hepatol. 2003;15:475–8. doi: 10.1097/01.meg.0000059118.41030.96. [DOI] [PubMed] [Google Scholar]
- 11.Akbari MR, Mohammadkhani A, Fakheri H. Screening of the adult population in Iran for coeliac disease: comparison of the tissue-transglutaminase antibody and anti-endomysial antibody tests. Eur J Gastroenterol Hepatol. 2006;18:1181–6. doi: 10.1097/01.meg.0000224477.51428.32. [DOI] [PubMed] [Google Scholar]
- 12.Zobeiri M, Ebrahimi S, Farahvash M, Rezaei M, Abdollahi A. Celiac disease: Serologic prevalence in patients with irritable bowel syndrome. J Res Med Sci. 2012;17:839–42. [PMC free article] [PubMed] [Google Scholar]
- 13.Tavakkoli H, Haghdani S, Adilipour H, Daghaghzadeh H, Minakari M, Adibi P. et al. Serologic celiac disease in patients with inflammatory bowel disease. J Res Med Sci. 2012;17:154–8. [PMC free article] [PubMed] [Google Scholar]
- 14.Rahimi AR, Daryani NE, Ghofrani H, Taher M, Pashaei MR, Abdollahzade S. et al. The prevalence of celiac disease among patients with non-alcoholic fatty liver disease in Iran. Turk J Gastroenterol. 2011;22:300–4. doi: 10.4318/tjg.2011.0216. [DOI] [PubMed] [Google Scholar]
- 15.Ehsani-Ardakani MJ, Rostami Nejad M, Villanacci V, Volta U, Manenti S, Caio G. et al. Gastrointestinal and non-gastrointestinal presentation in patients with celiac disease. Arch Iran Med. 2013;16:78–82. [PubMed] [Google Scholar]
- 16.Green PHR, Stavropoulos SN, Panagi SG, Goldstein SL, Mcmahon DJ, Absan H. et al. Characteristics of adult celiac disease in the USA: results of a national survey. Am J Gastroenterol. 2001;96:126–31. doi: 10.1111/j.1572-0241.2001.03462.x. [DOI] [PubMed] [Google Scholar]
- 17.Ciacci C, Cirillo M, Sollazzo R, Savino G, Sabbatini F, Mazzacca G. Gender and clinical presentation in adult celiac disease. Scand J Gastroenterol. 1995;30:1077–81. doi: 10.3109/00365529509101610. [DOI] [PubMed] [Google Scholar]
- 18.Tajuddin T, Razif S, Dhar R, Thorne J, Murray FE. Clinical presentation of adult coeliac disease. Ir Med J. 2011;104:20–2. [PubMed] [Google Scholar]
- 19.Masjedizadeh R, Hajiani E, Hashemi J, Shayesteh A, Moula K, Rajabi T. Celiac disease in South-West of Iran. World J Gastroenterol. 2006;12:4416–9. doi: 10.3748/wjg.v12.i27.4416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rampertab SD, Pooran N, Brar P, Singh P, Green PH. Trends in the presentation of celiac disease. Am J Med. 2006;119:355. doi: 10.1016/j.amjmed.2005.08.044. e9-14. [DOI] [PubMed] [Google Scholar]
- 21.Dore MP, Cuccu M, Pes GM, Mameli L, Manca A, Vidili G. et al. Clinical pattern of celiac disease in a population residing in North Sardinia (Italy) Recenti Prog Med. 2012;103:564–9. doi: 10.1701/1206.13357. [DOI] [PubMed] [Google Scholar]
- 22.Corazza GR, Di Sario A, Cecchetti L, Tarozzi C, Corrao G, Bernardi M. et al. Bone mass and metabolism in patients with celiac disease. Gastroenterology. 1995;109:122–8. doi: 10.1016/0016-5085(95)90276-7. [DOI] [PubMed] [Google Scholar]
- 23.Reilly NR, Fasano A, Green PH. Presentation of celiac disease. Gastrointest Endosc Clin N Am. 2012;22:613–21. doi: 10.1016/j.giec.2012.07.008. [DOI] [PubMed] [Google Scholar]
- 24.Singh P, Shergill S, Makharia GK. Celiac disease in older adults. J Gastrointestin Liver Dis. 2013;22:359–60. [PubMed] [Google Scholar]
- 25.Bykova SV, Sabel’nikova EA, Parfenov AI, Gudkova RB, Krums LM, Chikunova BZ. Reproductive disorders in women with celiac diseaseEffect of the etiotropic therapy. Eksp Klin Gastroenterol. 2011;3:12–8. [PubMed] [Google Scholar]
- 26.Soni S, Badawy SZ. Celiac disease and its effect on human reproduction: a review. J Reprod Med. 2010;55:3–8. [PubMed] [Google Scholar]
- 27.Donaldson MR, Book LS, Leiferman KM, Zone JJ, Neuhausen SL. Strongly positive tissue transglutaminase antibodies are associated with Marsh 3 histopathology in adult and pediatric celiac disease. J Clin Gastroenterol. 2008;42:256–60. doi: 10.1097/MCG.0b013e31802e70b1. [DOI] [PubMed] [Google Scholar]
- 28.Rubio-Tapia A, Van Dyke CT, Lahr BD, Zinsmeister AR, El-Youssef M, Moore SB. et al. Predictors of family risk for celiac disease: a population-based study. Clin Gastroenterol Hepatol. 2008;6:983–7. doi: 10.1016/j.cgh.2008.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murray JA. Celiac disease in patients with an affected member, type 1 diabetes, iron-deficiency, or osteoporosis? Gastroenterology. 2005;128:S52–S6. doi: 10.1053/j.gastro.2005.02.029. [DOI] [PubMed] [Google Scholar]
- 30.Elsurer R, Tatar G, Simsek H, Balaban YH, Aydinli M, Sokmensuer C. Celiac disease in the Turkish population. Dig Dis Sci. 2005;50:136–42. doi: 10.1007/s10620-005-1291-z. [DOI] [PubMed] [Google Scholar]
- 31.Reilly NR, Fasano A, Green PH. Presentation of celiac disease. Gastrointest Endosc Clin N Am. 2012;22:613–21. doi: 10.1016/j.giec.2012.07.008. [DOI] [PubMed] [Google Scholar]