Abstract
Importance
Although children's media consumption has been one of the most robust risk factors for childhood obesity, effects of specific parenting influences, such as parental media monitoring, have not been effectively investigated.
Objectives
This study examined the potential influences of maternal and paternal monitoring of child media exposure and children's general activities on children's BMI in middle childhood.
Design
A longitudinal study, taken from a subsample of the Three Generational Study, with assessments at children's ages of 5, 7, and/or 9 years collected from 1998-2012.
Setting
The Three Generational Study, a predominantly Caucasian, Pacific-Northwest U.S. community sample (overall participation rate 90%).
Participants
Analyses included 112 mothers, 103 fathers and their 213 children (55% girls) at ages 5, 7, and/or 9 years. Participation rates ranged from 67% to 72% of all eligible Three Generational Study children across the three assessments.
Main Exposures
Parents reported on their general monitoring of their children (whereabouts and activities), specific monitoring of child media exposure, children's participation in sports and recreational activities, children's media time (hours/week), annual income, and education level. Parental BMI was recorded.
Main Outcome Measure
Predictions to level and change in child BMI z scores were tested.
Results
Linear mixed-effects modeling indicated that more maternal, but not paternal, monitoring of child media exposure predicted lower child BMI z scores at age 7 years (95% CI, −.39 – −.07) and less steeply increasing child BMI z scores from ages 5-9 years (95% CI, −.11 – −.01). These effects held when controlling for more general parental monitoring, and parent BMI, income and education. Results supported that the significant negative effect of maternal media monitoring on children's BMI z scores at age 7 years was marginally accounted for by the effect of child media time. The maternal media monitoring effect on children's BMI z score slopes remained significant once adjusting for children's media time, and sports and recreational activity.
Conclusions
This study suggests that parental behaviors related to children's media consumption may have long-term impacts on children's BMI in middle childhood. The results underscore the importance of targeting parental media monitoring in efforts to prevent childhood obesity.
INTRODUCTION
Children's media consumption has been consistently linked to childhood obesity.1-5 Research on children's media use has focused on identifying factors of direct relevance to weight such as the number of hours children spend watching a television/computer,2,3 the presence of television screens in children's bedrooms,4 or whether eating while watching the television increases caloric intake.5 Although studies have revealed parents’ role in structuring children's physical activities,6,7,8 prior work has not effectively addressed how parents monitor and influence sedentary activities and the links to children's obesity. Better understanding of the role that parents may play in the monitoring of their children's media consumption while also examining more general forms of monitoring is critical to the development of targeted, family-based preventive interventions for obesity. The present study sought to disentangle the potential influences of multiple parenting behaviors and parent and family characteristics on children's body mass indexes (BMI) to identify specific parental behaviors that may protect or put children at risk for unhealthy weight development.
As obesity by middle childhood portends lifelong risk,10 identifying modifiable parental influences such as lack of media monitoring in this period may have implications for both children's and adults’ health. The present study used longitudinal data from middle childhood9 when parents still maintain primary responsibility for children's health behaviors. We first distinguished among parental monitoring behaviors thought to confer specific risk for obesity (media monitoring) versus more general direct monitoring (supervision) and indirect monitoring (communication and time spent with child) that are broadly relevant to developmental risk. We also controlled for potentially confounding family characteristics (parental BMI, income and education). Finally, we explored whether these associations would be attenuated by child behaviors thought to confer specific risk for obesity (child media time, and participation in sports and recreational activities).11
We hypothesized that parental monitoring behaviors (direct, indirect and media monitoring) would be inversely related to intra- and interindividual variation in child BMI beyond prediction from family characteristics (parental BMI, income and education). Given the sedentary behavior associated with media time and potential food advertisement exposure, monitoring of child media exposure was hypothesized to be especially relevant. Lower monitoring of child's whereabouts and activities (direct), and less communication and time spent with child (indirect) were hypothesized to impact child BMI via parental absence and unawareness of children's diets and/or behaviors. Stronger monitoring effects were expected for mothers, who are more often children's primary caregivers, than fathers. Next, we tested whether associations between parents’ monitoring behaviors and children's BMI, especially those related to media monitoring, would be attenuated by child behaviors hypothesized to be inversely (participation in sports and recreational activities) and directly (media time) related to child BMI.
METHODS
Participants
Following IRB approval, children (N = 213, 55% girls) and their 103 fathers and 112 mothers were assessed across childhood during the Three Generational Study (3GS)9, which originally examined the intergenerational transmission of risk for psychopathology and substance abuse. Fathers were originally recruited at ages 9-10 years due to elevated neighborhood risk for delinquency (Oregon Youth Study12 [n = 206]) and assessed nearly annually to age 37 years. Eligible 3GS children (up to 2 per partner of the men) participated at the age 5-, 7-, and 9-year assessments (89%, 93%, and 93%, respectively). Children were considered for the present analyses if (1) their heights and weights were measured at least once across the assessments (93%, 97%, and 98% of participating 3GS children, respectively) and (2) they had complete data on other study predictors (86%, 87%, and 82% of those meeting criterion 1). Child participation rates ranged from 67% to 72% of all eligible and 72% to 78% of all participating 3GS children across assessments. Averaged over assessments, independent samples t tests indicated that the included children compared with excluded participating children, had fathers who engaged in more media monitoring (95% CI, .14 – .98), mothers who engaged in less direct monitoring (95% CI, -.05 – -.001) and parents with higher annual incomes (95% CI, 1300 – 12700). No other significant differences existed between the groups for other study predictors or child BMI. 99.5% of children’s mothers and 89% of children’s fathers were the biological parents (others denote stepparents). Information regarding children's living situations is presented in Table 1.
Table 1.
Sample Descriptive Statistics by Assessment
| Assessment: Child age (years) |
||||
|---|---|---|---|---|
| 5 | 7 | 9 | Total | |
| Children (n) | 205 | 184 | 85 | 213 |
| Mothers (n) | 108 | 96 | 58 | 112 |
| Fathers (n) | 99 | 91 | 49 | 103 |
| Child lived with (n) | ||||
| Both biological parents | 111 | 99 | 35 | 245 |
| One biological parent (and possibly his/her partner) | 89 | 81 | 49 | 219 |
| Both biological parents part-time (and possibly their partners) | 5 | 4 | 1 | 10 |
| Children's age, years | 5.35 (.59) | 7.28 (.44) | 9.20 (.31) | 6.79 (1.50) |
| Children's BMI z scores, standardized kg/m2 | .61 (1.13) | .62 (1.19) | .82 (1.17) | .65 (1.16) |
| BMI category (n %): | ||||
| Underweight (< 5 percentile) | 7 (3%) | 6 (3%) | 1 (1%) | 14 (3%) |
| Normal (5th to < 85th percentile) | 122 (60%) | 107 (58%) | 40 (47%) | 269 (57%) |
| Overweight (85th to < 95th percentile) | 43 (21%) | 36 (20%) | 24 (28%) | 103 (22%) |
| Obese (> 95th percentile) | 33 (16%) | 35 (19%) | 20 (24%) | 88 (18%) |
| Parent's average BMI scores, kg/m2 | 27.29 (5.38) | 28.63 (6.00) | 29.29 (5.94) | 28.14 (5.75) |
| Fathers' BMI category (n %): | ||||
| Underweight (< 18.5) | 2 (1%) | 0 (0%) | 0 (0%) | 2 (<1%) |
| Normal (18.5 to < 25) | 37 (18%) | 12 (7%) | 10 (12%) | 59 (12%) |
| Overweight (25 to < 30) | 41 (20%) | 30 (16%) | 17 (20%) | 88 (19%) |
| Obese (>= 30) | 32 (16%) | 26 (14%) | 11 (13%) | 69 (15%) |
| Missing | 93 (45%) | 116 (63%) | 47 (55%) | 256 (54%) |
| Mothers' BMI category (n %): | ||||
| Underweight (< 18.5) | 6 (3%) | 4 (2%) | 0 (0%) | 10 (2%) |
| Normal (18.5 to < 25) | 19 (9%) | 33 (18%) | 12 (14%) | 64 (14%) |
| Overweight (25 to < 30) | 23 (11%) | 17 (9%) | 8 (9%) | 48 (10%) |
| Obese (>= 30) | 24 (12%) | 33 (18%) | 16 (19%) | 73 (15%) |
| Missing | 133 (65%) | 97 (53%) | 49 (58%) | 279 (59%) |
| Mothers' monitoring | ||||
| Direct, 1=Neverto 5=Always | 3.89 (.90) | 3.84 (1.04) | 4.68 (.57) | 4.01 (.96) |
| Indirect, 0 -7 days/week | 5.79 (1.16) | 5.80 (1.08) | 5.67 (1.21) | 5.77 (1.14) |
| Media, 1=Never to 5=Always | 4.28 (.95) | 4.16 (.97) | n/a | 4.22 (.96) |
| Fathers' monitoring | ||||
| Direct, 1=Never to 5=Always | 3.91 (.92) | 3.94 (.88) | 4.70 (.54) | 4.06 (.90) |
| Indirect, 0 - 7 days/week | 4.51 (1.83) | 4.42 (1.79) | 4.36 (1.94) | 4.45 (1.83) |
| Media, 1=Never to 5=Always | 3.82 (1.25) | 3.75 (1.21) | n/a | 3.79 (1.23) |
| Parent's income, per $10,000 | 3.20 (1.83) | 3.35 (1.45) | 3.04 (1.87) | 3.23 (1.70) |
| Parent's education (n %) | ||||
| 0 Parents > high school education | 94 (46%) | 82 (45%) | 59 (69%) | 235 (49%) |
| 1 Parent > high school education | 84 (41%) | 78 (42%) | 25 (30%) | 187 (40%) |
| 2 Parents > high school education | 27 (13%) | 24 (13%) | 1 (1%) | 52 (11%) |
| Children's sports/recreational activity, 0=Less to 3=More | 1.31 (.67) | 1.33 (.62) | 1.30 (.60) | 1.25 (.61) |
| Children's media time, hours/day | 1.78 (.90) | 1.69 (.73) | n/a | 1.74 (.83) |
Note. Tabled numbers given as mean (standard deviation) unless noted otherwise. Units of measures denote likert scaled scores for parental direct, indirect and media monitoring, and children's sports/recreational activity.
Procedures
Parents and children were assessed when children were ages 5, 7, and 9 years using questionnaires, interviews, and physical measurements. Children participated at 1, 2, or 3 assessments (n = 33, 97, and 83, respectively). For 82% to 94% of the children and 87% to 95% of the parents both parents’ reports were available on all study predictors except for parents’ BMI (measured for both parents for 57% of the children).
Measures
For parental general monitoring, media monitoring, and children's activities, items, response ranges, internal consistencies, percent of total variance explained, and correlations between parents’ scores are provided in eTable 1. Items had to demonstrate adequate associations with their corresponding scales (individual item-to-total correlations of at least .20). Averaged across assessments and scales, item-to-total correlation ranged from .28 – .78. All scales were unidimensional. Maternal and paternal monitoring measures were used at each assessment to form time-variant (intraindividual) variables. Other children and family variables served as controls and were averaged across parents to form time-variant aggregate variables. Cross-time averages of these time-variant measures and of those collected at only 1 or 2 assessments served as time-invariant (interindividual) variables.
Dependent Variable: Children's BMI z scores
Heights and weights were obtained via physical measurements for 92% of the children (n = 195; and 89% [422 of 474] of the time-by-person observations) and by parent reports in the remaining cases. Using the Centers for Disease Control and Prevention growth charts13,14 BMI (kg/m2) scores were converted to standardized BMI-for-age-and-sex z scores (BMIz). Thus, the dependent variable represents deviation from a national average BMI. Two biologically implausible BMIz were excluded from the sample.15,16
Time-Invariant Independent Variables
Three family characteristics variables (parental income and education, measured at all 3 assessments, and parent BMI, measured at 1 or 2 assessments) were averaged and entered into the analyses as time-invariant control predictors. Maternal and paternal monitoring of media exposure and children's media time were only assessed at the age 5- and 7-year assessments; these time-invariant independent variables were computed as averages of these 2 assessments.
Parental Income
Annual household income was the average of the mothers’ and fathers’ reports. One outlier was set to the second highest value of $182,400. Scores were divided by 10,000 so that regression coefficients are interpretable as interindividual differences associated with a $10,000 income difference.
Parental Education
Parents selected their highest level of education completed from 7 categories, ranging from “less than seventh grade” to “graduate degree.” Based on past research17 and for parsimony, parental education was categorized to denote that 0, 1 or 2 parent(s) had greater than 12 years of education at 1 or more assessments. Parental education effects on child BMI were tested for 0 versus 2 parents, and 1 versus 2 parent(s) having had some form of post-secondary education.
Parental BMI
Parents’ BMI was calculated from physical measurements for all fathers and 45% of the mothers (others contributed self-reports). When both parents’ BMI scores were available (n = 121 children, 95 parents), they were averaged; otherwise, the parental BMI variable denoted only paternal (n = 88 children, 19 fathers) or maternal (n = 4 children, 1 mother) BMI.
Parental Monitoring of Media Exposure
Parents answered 3 questions regarding their limiting of their child's media exposure.18 Response scales ranged from “1 = never or almost never” to “5 = always or almost always”, in addition to an option for “Never ever watched television/videos or played video games”, which was recoded to 5. At child ages 5 and 7 years respectively, 20% and 7% of children’s mothers and 13% and 5% of children’s fathers restricted their children from playing video games.
Children's Media Time
Parents reported the typical number of hours their child spent (1) watching television/movies and (2) playing video games, during school-year weekdays and weekends.18 A weighted average (5/7*weekday hours + 2/7*weekend hours) was calculated denoting the typical number of hours of media time per day averaged over television/movies and video games. Mothers’ and fathers’ reports were averaged into a composite child media time score.
Time-Varying Predictors (Assessed at Child Ages 5, 7, and 9 Years)
Separate scores for general monitoring and children's activities were created at each of the assessments to assess time-specific associations with child BMIz.
General Parental Monitoring
Parents completed three items describing direct parental monitoring practices (supervision, awareness, and control of child whereabouts and associates). Response scales ranged from “1 = Very often\Everyday” to “5 = Never”. Identical items were used at child ages 5 and 7, but were modified at age 9 years to be more developmentally appropriate.18,19 Five items regarding more indirect forms of parental monitoring (conversation about child's day and time spent with child; response scale: “0 to 7 days/week”) assessed at each age and reported by parents were not significantly associated with direct monitoring practices and, thus, were considered as separate predictors of child BMI.19
Children's Sports and Recreational Activity
Parents reported on their child's participation in sports (2 items)20,21 and family recreational activities (2 items).22 Item response scales were recoded to range from 0 to 3, and mothers’ and fathers’ reports were averaged at each time point creating a composite score (hereafter referred to as activities).
Data Analytic Strategy
Dependence among children's BMIz across middle childhood and siblings’ BMIz were accounted for by fitting three-level linear mixed-effects models. Children's ages were grand-mean centered at the middle assessment (average age 7.3 years), and children's BMIz at age 7.3 years were free to vary within the sample (i.e., random child intercept). Models I and II for mothers and fathers addressed the first set of hypotheses examining the simultaneous influences of (1) direct and indirect general monitoring as both intraindividual and interindividual predictors and (2) media monitoring as an interindividual predictor of children's BMIz while also controlling for interindividual differences in parents’ BMI, income, and education. Model III addressed the second set of hypotheses examining if maternal monitoring effects on children's BMIz were attenuated by children's activities (as an intraindividual and interindividual predictor) and media time (as an interindividual predictor). Averaging mothers’ and fathers’ BMI was necessary to retain sufficient sample size. This results, however, in a loss of information and prevents individual examination of effects, which may vary for children with only 1 versus 2 overweight or obese parent(s). We thus included both a main effect of average parent BMI and an interaction term between parent BMI and a contrast coefficient denoting whether the parental BMI effect on child BMI varied for those children with 2 (coded as 0.5) versus only 1 overweight or obese parent (coded as -0.5). This effect only applies to children with complete data on mothers’ and fathers’ BMI; children with only 1 parent BMI measure (coded as 0) were excluded from the mean comparison and included in the main effect of parent BMI.
RESULTS
Descriptive statistics (Table 1) indicated that children's average BMIz increased from .61 to .82 across middle childhood. Overweight and obesity prevalence across all assessments ranged from 37% to 52% for children. Of the n = 121 children with complete maternal and paternal BMI scores, n = 69, 40 and 12 respectively had 2, 1, or 0 overweight or obese parent(s) at 1 or multiple assessments; of the 92 children with 1 parent report, 55 mothers/fathers were overweight or obese. Mothers’ and fathers’ general direct monitoring showed slight increases over time, whereas all other variables appeared relatively stable. Mothers and fathers reported similar average levels of direct monitoring whereas more indirect and media monitoring were reported by mothers than fathers. Averaged across assessments, children spent 1.74 hours per day, and 30% of children spent more than the American Academy of Pediatrics’ recommendation of a maximum of 2 hours per day, 23 watching television and/or playing video games.
Parents’ General and Media Monitoring
The first set of hypotheses relating parental monitoring behaviors to children's BMIz while controlling for family characteristics were partially supported for mothers only (Table 2, Models I and II respectively). Maternal media monitoring predicted level and change in children's BMIz; maternal and paternal general forms of monitoring did not. Children whose mothers engaged in less media monitoring had higher BMIz at age 7 years and more steeply increasing BMIz from ages 5-9 years. The years in which parents engaged in more direct and indirect monitoring, however, were not predictive of concurrent decreases in children's BMIz across middle childhood. Parent BMI predicted children's BMIz at age 7 years but not changes in child BMIz from 5-9 years. The parental BMI effect at age 7 years was amplified for children with 2 versus 1 overweight or obese parent(s). Children from homes where only 1 versus 2 parents had more than 12 years of education had higher BMI z scores at age 7 years, but no significant differences emerged in predicting child BMIz slopes. Finally, effects for neither versus both parent(s) with more than 12 years of education and parental income did not significantly predict either outcome. The maternal and paternal monitoring models respectively explained 3% and 2% of children's variability in BMIz across time and 24% and 19% of the variability between children's BMIz 24.
Table 2.
Multilevel Models: Parameter Estimates
| Model |
|||
|---|---|---|---|
| Model 1: Maternal Monitoring | Model 2: Paternal Monitoring | Model 3: Maternal Monitoring Controlling for Child Behavior | |
| Fixed effects (sample range for predictor variables) | |||
| Child BMIz at age 7 years (intercept) | .21 (.38) | .22 (.43) | .23 (.38) |
| Change in child BMIz from 5-9 years (slope) | .03 (.12) | .07 (.13) | .03 (.12) |
| Time-variant intraindividual effects: | |||
| Mothers'/fathers' direct monitoring (1 - 5) | −.07 (.12) | .004 (.15) | −.08 (12) |
| Mothers'/fathers' indirect monitoring, days/week (0 - 7) | −.003(.13) | −.02 (.07) | .001 (.13) |
| Children's sports/recreational activities (0 - 2.9) | -- | -- | −.17 (.20)M |
| Residual variance | .55 (.22)*** | .56 (.25)*** | .54 (.22)*** |
| Time-invariant interindividual effects: | |||
| Prediction of child BMIz at age 7 years (intercept): | |||
| Mothers'/fathers' direct monitoring (1 - 5) | .15 (.25) | −.06 (.26) | .17 (.25) |
| Mothers'/fathers' indirect monitoring, days/week (0 - 7) | .10 (.22) | .003 (.13) | .11 (.22) |
| Mothers'/fathers' media monitoring (1 - 5) | −.23 (.16)** | −.05 (.13) | -.15 (.16)M |
| Parents' BMI, kg/m2 (17.3 - 45.9) | .04 (.03)* | .04 (.03)* | .03 (.03)* |
| 2 vs. 1 overweight or obese parent(s) | .02 (.01)* | .017 (.018)M | .019 (.016)* |
| Parents' income, per $10,000 (.3 - 18.2) | .05 (.10) | .03 (.11) | .07 (.09) |
| 0 vs. 2 parents with >12 years education | .27 (.43) | .35 (.51) | .25 (.42) |
| 1 vs. 2 parent(s) with >12 years education | .51 (.43)* | .50 (.48)* | .49 (.42)* |
| Children's sports/recreational activities (0 - 2.8) | -- | -- | .07 (.35) |
| Children's media time, hours/day (.2 - 5.1) | -- | -- | .24 (.18)** |
| Prediction of change in child BMIz from 5-9 years (slope): | |||
| Mothers'/fathers' direct monitoring (1 - 5) | −.01 (.08) | −.06 (.08) | -.01 (.08) |
| Mothers'/fathers' indirect monitoring, days/week (0 - 7) | −.01 (.06) | .02 (.05) | -.01 (.06) |
| Mothers'/fathers' media monitoring (1 - 5) | −.06 (.05)* | −.03 (.06) | -.058 (.057)* |
| Parents' BMI, kg/m2 (17.3 - 45.9) | −.001 (.01) | −.002 (.01) | -.001 (.01) |
| 2 vs. 1 overweight or obese parent(s) | .001 (.004) | .002 (.004) | .001 (.004) |
| Parents' income, per $10,000 (.3 - 18.2) | .02 (.03) | .01 (.03) | .02 (.03) |
| 0 vs. 2 parents with >12 years education | −.06 (.15) | −.09 (.16) | -.06 (.14) |
| 1 vs. 2 parent(s) with >12 years education | .01 (.13) | −.02 (.13) | .01 (.13) |
| Children's sports/recreational activities (0 - 2.8) | -- | -- | .03 (.11) |
| Children's media time, hours/day (.2 - 5.1) | -- | -- | -.001 (.06) |
| Random effect | |||
| Child BMIz age 7 years (intercept) | .60 (.14)*** | .67 (.23)*** | .57 (.13)*** |
Note. Tabled numbers given as parameter estimates (error measurement [i.e., standard error times the critical value]). Units of measures denote likert scaled scores for parental direct, indirect and media monitoring, and children's sports/recreational activity.
p < .001.
p < .01.
p < .05.
p < .10.
Parents’ General and Media Monitoring Controlling for Children's Behaviors
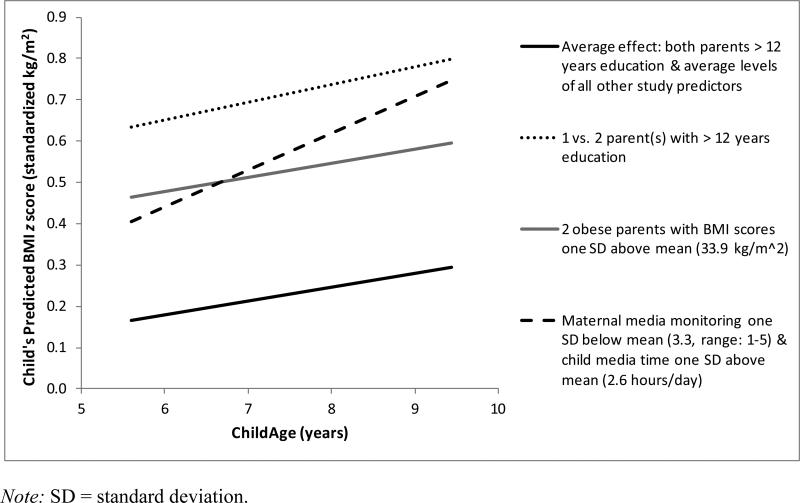
Finally, we considered whether children's activities and media time might attenuate the associations between parental BMI and education, and maternal media monitoring and child BMIz (Table 2, Model III). Intraindividual increases in children's activities across middle childhood were marginally associated with concurrent decreases in children's BMIz; however, interindividual variability in children's activities did not relate to lower BMIz at age 7 years or less steeply increasing BMIz from ages 5 to 9 years. Next, results supported that the negative effect of maternal media monitoring on BMIz at age 7 years was marginally accounted for by the effect of child media time, whereas the effect of maternal media monitoring on children's BMIz slopes remained significant once adjusting for children's media time and activities. The significance of all family characteristics effects remained unchanged from the prior maternal monitoring model, Model I. The addition of children's activities and media time yielded improvement in model fit over Model I (TRd[5] = 11.43, p = .043,) 25 explaining 4% of children's variability in BMIz across time and 27% of the variability between children's BMIz 24. Figure 1 depicts children's predicted BMIz given their age and the predictor variables identified in Model III.
Figure 1.
Children's predicted BMI z scores across middle childhood at illustrative levels of maternal monitoring, family characteristics and children's behaviors (Table 2, Model III).
DISCUSSION
This study highlights the importance of parenting behavior in children's weight development across middle childhood. Less maternal monitoring of media exposure predicted higher BMI at age 7 years and increasing deviance from child BMI norms from ages 5 to 9 years. Several competing explanations for these effects were ruled out. First, whereas lower parent education, higher parent BMI and having 2 versus 1 overweight or obese parent(s) were risk factors for child obesity, they did not account for effects of maternal media monitoring on child BMI z scores. Second, maternal media monitoring, but not direct or indirect general monitoring, was associated with child BMI. Thus, low maternal media monitoring does not appear to reflect more general parental disengagement or lack of awareness regarding children's behaviors and whereabouts. The association between lower maternal media monitoring and higher child BMI was primarily explained by a tendency for these children to spend more hours per week watching television and playing videogames. This supports the validity of our interpretation that child media time has direct effects on BMI, is under substantial control by parents, and therefore is a prime target for family intervention.
The link between children's media time and obesity is not new.1-5 To our knowledge, however, the link has not been established in longitudinal studies that sufficiently control for the competing influences of parents’ BMI, income, education, and other forms of parenting (i.e., general monitoring/supervision). The American Academy of Pediatrics recommends that child media time should be limited to 2 hours per day,23 but children spend more time in front of a screen than is recommended.26 The results of interventions aimed at decreasing television time have not been adequate,27,28 perhaps because of their low intensity.29 Yet, strengthening parental practices regarding limiting child media usage is an important focus in family-based interventions.
Findings also indicated that child BMI was marginally responsive to changes in children's participation in sports and recreational activities over time, such that deviations from age and sex norms were greater in years of decreased activity. Future research should explore these associations using more comprehensive measures of physical activity and explore dietary options and child eating patterns.
There were some study limitations. The sample was not racially/ethnically representative of the U.S. population and was relatively small, thus not permitting child gender comparisons. Other limitations include subjective measures of children's activities and media time and parental behavior and our inability to rule out potential social desirability biases. Incomplete data precluded the ability to test intraindividual effects of media monitoring on child BMI, and independent maternal and paternal BMI effects on child BMI. Further, although the study employed a longitudinal design it was not possible to distinguish the temporal ordering of predictors and outcomes, and the design does not allow for causal inferences. Additionally, we did not consider the potentially bidirectional relationship between child activities and parental monitoring, and child BMI, nor how parental monitoring may differ for overweight, less active children versus more active children who become overweight. Finally, models explained relatively little variation in children's BMI across middle childhood and approximately a quarter of the variation between children's BMI at age 7 years. Thus, future research must identify additional explanatory variables.
CONCLUSION
The present study examined the influences that parents’ behaviors may have on children's weight across middle childhood. Results suggest that interventions aimed at parental supervision and control of child media exposure may promote healthy child weight development during middle childhood.
Supplementary Material
ACKNOWLEDGEMENTS
Funding Sources: The project described was supported by awards from National Institutes of Health (NIH), U.S. PHS to Dr. Capaldi: Award Number R01 DA 015485 (Adjustment Problems and Substance Use in Three Generations) from the National Institute of Drug Abuse (NIDA); 1R01AA018669 (Understanding Alcohol Use over Time in Early Mid-Adulthood for At-Risk Men) from the National Institute on Alcohol Abuse and Alcoholism (NIAAA); and HD 46364 (Risk for Dysfunctional Relationships in Young Adults) from the National Institute of Child Health and Development (NICHD). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, NIAAA, NIDA, or NICHD. Paulina Nowicka was supported by the Sweden-America Foundation, the Swedish Society for Medical Research and the VINNMER Marie Curie International Qualification. All specified funding organizations (NIH, NIAAA, NIDA, NICHD, the Sweden-America Foundation, the Swedish Society for Medical Research, and the VINNMER Marie Curie International Qualification) had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr. Tiberio had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study conceptualization: Nowicka, Kerr, Tiberio, Capaldi, Pears, and Kim. Analysis plan and model refinements: Tiberio and Kerr. Interpretation of data: Tiberio, Kerr, and Nowicka. Drafting of the manuscript: Nowicka, Tiberio, and Kerr. Critical revision of the manuscript for important intellectual content: Capaldi, Pears, Kim, Nowicka, Kerr, and Tiberio. Study supervision: Capaldi.
Conflict of Interest: The authors have no conflicts of interest to disclose.
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
REFERENCES
- 1.Robinson TN. Reducing children's television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282(16):1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 2.Crespo CJ, Smit E, Troiano RP, et al. Television watching, energy intake, and obesity in US Children: results from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 2001;155(3):360–365. doi: 10.1001/archpedi.155.3.360. [DOI] [PubMed] [Google Scholar]
- 3.Proctor MH, Moore LL, Gao D, et al. Television viewing and change in body fat from preschool to early adolescence: the Framingham Children's Study. Int J Obes Relat Metab Disord. 1999;27(7):827–833. doi: 10.1038/sj.ijo.0802294. [DOI] [PubMed] [Google Scholar]
- 4.Dennison BA, Erb TA, Jenkins PL. Television viewing and television in bedroom associated with overweight risk among low-income preschool children. Pediatrics. 2002;109(6):1028–1035. doi: 10.1542/peds.109.6.1028. [DOI] [PubMed] [Google Scholar]
- 5.Wiecha JL, Peterson KE, Ludwig DS, et al. When children eat what they watch: impact of television viewing on dietary intake in youth. Arch Pediatr Adolesc Med. 2006;160(4):436–442. doi: 10.1001/archpedi.160.4.436. [DOI] [PubMed] [Google Scholar]
- 6.Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. 2000;32:963–75. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Kerr J, Rosenberg D, Sallis JF, Saelens BE, Frank LD, Conway TL. Active commuting to school: associations with environment and parental concerns. Med Sci Sports Exerc. 2006;38:787–94. doi: 10.1249/01.mss.0000210208.63565.73. [DOI] [PubMed] [Google Scholar]
- 8.Carver A, Timperio A, Hesketh K, Crawford D. Are children and adolescents less active if parents restrict their physical activity and active transport due to perceived risk? Soc Sci Med. Jun. 2010;70(11):1799–805. doi: 10.1016/j.socscimed.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 9.Capaldi DM, Pears KC, Kerr DCR. The Oregon Youth Study Three-Generational Study: theory, design, and findings. Bulletin of the International Society for the Study of Behavioural Development (ISSBD) 2012;2(62):29–33. [Google Scholar]
- 10.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869–973. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 11.Barlow SE. Expert Committee. Expert Committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120:S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 12.Capaldi DM, Patterson GR. Psychometric Properties of Fourteen Latent Constructs from the Oregon Youth Study. Springer-Verlag; New York: 1989. [Google Scholar]
- 13.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States: methods and development. National Center for Health Statistics. Advance Data from Vital and Health Statistics. 2000;314:1–27. [PubMed] [Google Scholar]
- 14.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. National Center for Health Statistics. Vital Health Stat. 2002;11(246):1–190. [PubMed] [Google Scholar]
- 15.Dibley MJ, Goldsby JB, Staehling NW, Trowbridge FL. Development of normalized curves for the international growth reference: historical and technical considerations. Am J Clin Nutr. 1987;46(5):736–748. doi: 10.1093/ajcn/46.5.736. [DOI] [PubMed] [Google Scholar]
- 16.Dibley MJ, Staehling NW, Nieburg P, Trowbridge FL. Interpretation of Z-score anthropometric indicators derived from the international growth reference. Am J Clin Nutr. 1987;46:749–762. doi: 10.1093/ajcn/46.5.749. [DOI] [PubMed] [Google Scholar]
- 17.Moraeus L, Lissner L, Yngve A, et al. Multi-level influences on childhood obesity in Sweden: societal factors, parental determinants and child's lifestyle. Int J Obesity. 2012:1–8. doi: 10.1038/ijo.2012.79. [DOI] [PubMed] [Google Scholar]
- 18.Capaldi DM, Pears KC, Wilson J, Bruckner L. Parent Interview. Unpublished instrument. Oregon Social Learning Center; Eugene: 1998. [Google Scholar]
- 19.Capaldi DM, Wilson J. Monitor and Parent-Child Relationship. Oregon Social Learning Center; Eugene: 1998. Unpublished instrument. [Google Scholar]
- 20.Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 profile. University of Vermont, Department of Psychology; Burlington, VT: 1991. [Google Scholar]
- 21.Achenbach TM. Manual for the Child Behavior Checklist/2-3 and 1992 Profile. University of Vermont, Department of Psychology; Burlington, VT: 1992. [Google Scholar]
- 22.Patterson GR. Family Activities Checklist. Unpublished instrument. Oregon Social Learning Center; Eugene: 1982. [Google Scholar]
- 23.American Academy of Pediatrics Committee on Public Education, Children, Adolescents, and Television. Pediatrics. 2001;107(2):423–426. doi: 10.1542/peds.107.2.423. [DOI] [PubMed] [Google Scholar]
- 24.Bryk AS, Raundenbush SW. Applications in the study of individual change. In: Bryk AS, Raudenbush SW, editors. Hierarchical Linear Models. Sage; Newbury Park, CA: 1992. pp. 130–154. [Google Scholar]
- 25.Satorra A, Bentler P. Scaling corrections for statistics in covariance structure analysis. University of California: Department of Statistics; Los Angeles: [April 4, 2012]. http://escholarship.org/uc/item/8dv7p2hr. Published October 25, 2011. [Google Scholar]
- 26.Fakhouri TH, Huges JP, Brody DJ, Kit BK, Ogden CL. Physical activity and screen-time viewing among elementary school-aged children in the United States from 2009-2010. JAMA Pediatr. 2013;167(3):223–229. doi: 10.1001/2013.jamapediatrics.122. [DOI] [PubMed] [Google Scholar]
- 27.Schmidt ME, Haines J, O'Brien A, et al. Systematic review of effective strategies for reducing screen time among young children. Obesity. 2012;20(7):1338–1354. doi: 10.1038/oby.2011.348. [DOI] [PubMed] [Google Scholar]
- 28.Steeves JA, Thompson DL, Bassett DR, Fitzhugh EC, Raynor HA. A review of different behavior modification strategies designed to reduce sedentary screen behaviors in children. J Obes. 2012 doi: 10.1155/2012/379215. Article ID 379215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Birken CS, Maguire J, Mekky M, et al. Office-based randomized controlled trial to reduce screen time in preschool children. Pediatrics. 2012;130(6):1110–1115. doi: 10.1542/peds.2011-3088. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.