Abstract
Objective
We conducted a retrospective investigation of potential clinical, demographic, and neuropsychological risk factors for suicide attempts in patients diagnosed with bipolar disorder.
Method
Participants included 67 adult inpatients and outpatients aged 18–60 years meeting DSM-IV criteria for bipolar disorder (bipolar I and II disorders, bipolar disorder not otherwise specified). We assessed demographic factors, mood symptoms, psychosis, trauma history, trait impulsivity, trait aggression, and reasons for living. The primary outcome measures were the Barratt Impulsiveness Scale-version II, Aggression Questionnaire, and 10 cognitive outcome variables. The cognitive outcome variables assessed cognitive performance across several domains, including processing speed, attention, verbal learning, and executive function. Another aspect of cognitive function, decision making, was assessed using the Iowa Gambling Task. The study was conducted from July 2007–July 2009.
Results
We found that nonattempters reported significantly higher trait impulsivity scores on the Barratt Impulsiveness Scale compared to attempters (t57 = 2.2, P = .03) and that, among attempters, lower trait impulsivity score was associated with higher scores of lethality of prior attempts (r25 = −0.53, P = .01). Analyses revealed no other group differences on demographic, clinical, or neurocognitive variables when comparing attempters versus nonattempters. Regression models failed to identify any significant predictors of past suicide attempt.
Conclusions
The largely negative results of our study are particularly important in highlighting the clinical dilemma faced by many clinicians when trying to predict which patients will make serious suicide attempts and which patients are at a lower risk for acting on suicidal thoughts. A limitation of our work is that we examined stable trait measures of impulsivity among a euthymic sample rather than mood state or the impact of mood state on traits. Overall, we conclude that suicidal behavior is extremely difficult to predict, even when comprehensive clinical and neurocognitive information is available.
Bipolar disorder is a chronic and debilitating mood disorder associated with substantial morbidity and mortality.1,2 Data from the Epidemiologic Catchment Area study3 demonstrated suicide to be more prevalent among patients with bipolar disorder than any other psychiatric group, including patients with major depressive disorder (MDD). Indeed, the odds ratio for suicide attempts is 6.2 for bipolar disorder patients and 3.1 for MDD patients.3 A recent review found that 15%—19% of bipolar disorder patients die by suicide.4 Clearly, suicidality among bipolar disorder patients is a significant public health concern worthy of extensive examination; however, prior studies that have assessed potential clinical and neuropsychological correlates of suicidal behavior5 are limited and have not specifically focused on bipolar disorder cohorts.
Clinical and Demographic Correlates of Suicidal Behavior
Investigations of clinical predictors of suicide attempts have assessed impulsivity-related traits,6 with increased self-reported impulsivity reported among attempters versus nonattempters in some studies,7,8 yet others have failed to find group differences.9,10 Research on suicide has also focused on history of trauma as a potential risk factor. Findings from the Stanley Foundation suggest that almost a quarter of attempters report a history of physical and sexual abuse.11 Others have found that a higher percentage of bipolar disorder patients with a prior attempt report a history of abuse than those patients who have never made an attempt; however, abuse is not an effective predictor of suicide attempt.12 Bipolar subtype may also contribute to suicidal behavior. Recent work found that bipolar I disorder patients were more likely to attempt suicide compared to bipolar II disorder and MDD patients.13 However, this finding is limited by the reliability of bipolar disorder diagnoses, especially the detection of hypomanic/manic episodes among MDD patients.14 Other research has suggested that demographic factors such as sex may be an important predictor of suicide attempt. For example, in one study,11 women were found to be at greater risk for suicide attempts, while another similar study15 failed to show a sex difference. The complexity of suicidality, including individual, clinical, illness-related and stress-related risk factors, may account for the overall lack of consistent outcomes across studies that assess these clinical and demographic variables.4 In the current study, we attempted to resolve inconsistencies in the literature by reexamining relevant clinical and demographic variables in a large sample of comprehensively characterized euthymic bipolar disorder patients.
Neuropsychological Correlates of Suicidal Behavior
Neuropsychological studies suggest that suicidality among patients with mood disorders may be associated with executive dysfunction, particularly when highly lethal attempts are made. For example, it has been found that currently depressed individuals with a history of making high lethality suicide attempts perform significantly worse on measures of executive functioning compared to nonpatients, depressed patients with no past history of attempts, and patients with a history of making low lethality suicide attempts.16 A related investigation17 found that a group of nondepressed (Hamilton Depression Rating Scale score > 10) patients diagnosed with psychiatric disorders, including mood disorders (MDD, bipolar disorder), eating disorders, anxiety disorders, or substance abuse, who engaged in violent suicide attempts performed significantly worse on the Iowa Gambling Task, a measure of decision making, when compared to patients who did not have a history of suicide attempt. Cognitive function did not differ between patients who engaged in nonviolent suicide attempts versus patients without a history of suicide attempts. Cognitive function did not differ between patients with violent versus nonviolent suicide attempts.17
Surprisingly few studies have focused on patients with bipolar disorder and, more specifically, examined potential cognitive disturbances that may reflect deficits in executive function among suicide attempters. This shortage of material exists despite a growing literature indicating trait-like impairment in euthymic bipolar disorder patients in this domain.18 One study19 examined a sample of currently mildly depressed, mildly hypomanic, mixed, and euthymic bipolar disorder patients and assessed a variety of cognitive factors and demonstrated deficits in decision making on the Iowa Gambling Task in bipolar I disorder attempters versus nonattempters. Impaired performance on the Iowa Gambling Task was significantly associated with number of suicide attempts.19 In this study,19 interference scores on the Stroop Test were also significantly correlated with an increased number of suicide attempts, suggesting that difficulties with response inhibition are associated with an increased rate of suicide attempts. It was found that a sample of euthymic, manic, depressed, and mixed-episode bipolar disorder patients who have attempted suicide also have more impulsive responses on an immediate response task when compared to bipolar disorder patients who do not have a history of suicide attempt.20 Research examining depressed bipolar I disorder and bipolar II disorder attempters and healthy controls revealed that both groups of bipolar disorder patients exhibit impairments on cognitive tasks assessing working memory, psychomotor speed, and impulsivity compared to healthy controls.21 Other work22 has shown that visual processing impairment on Trail Making Test-Part A and verbal memory deficits on the California Verbal Learning Test are associated with an increased number of suicide attempts among a sample of bipolar I disorder and bipolar II disorder patients in manic, depressed, mixed, and euthymic states. The current work aimed to add to this small set of studies by identifying a homogenous group of euthymic bipolar disorder patients and examining differences between attempters and nonattempters on cognitive tasks as well as cognitive predictors of suicide attempts in this bipolar disorder sample.
In summary, the clinical, demographic, and cognitive predictors of suicidality among bipolar disorder patients remain to be fully elucidated.4 The current study supplements prior work by examining a set of trait and state clinical measures, demographic characteristics, and neurocognitive tasks thought to be relevant to bipolar disorder and suicide. In an effort to identify which patients are at greatest risk for actualized suicide attempts, we first assessed potential differences among attempters and nonattempters, with the secondary aim of developing a multivariate model to predict suicide attempts in bipolar disorder patients.
METHOD
Participants
Participants included 67 adult inpatients and outpatients aged 18–60 years at Zucker Hillside Hospital, a division of the North Shore Long Island Jewish Health System, meeting DSM-IV criteria (Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Patient Edition23) for bipolar I disorder, bipolar II disorder, or bipolar disorder not otherwise specified (NOS). All participants were treated with mood stabilizers, antidepressants, antipsychotics, anticholinergics, anxiolytics, hypnotics, and/or benzodiazepines. Stimulants, dopamine agonists, and tricyclics were disallowed due to effects on cognition. See Table 2 for the pharmacologic profile of each group.
Table 2.
Patient Characteristics
| Variable | Yes | No | P |
|---|---|---|---|
| Columbia Suicide History Form | |||
| Deliberate attempts, % (n/n) | 41.8 (28/67) | 58.2 (39/67) | |
| Aborted attempts, % (n/n) | 39 (10/26) | 14 (5/37) | NS |
| Interrupted attempts, % (n/n) | 19 (5/26) | 3 (1/37) | .03 (χ2 = 4.84) |
| Ambiguous attempts, % (n/n) | 0 (0/26) | 3 (1/37) | NS |
| Lethality rating for deliberate attempts, mean (SD)a | 2.57 (1.89) | NA | |
| Attempter | Nonattempter | P | |
| Alcohol use, % (n/n) | 52 (11/21) | 39 (14/36) | NS |
| Drug use, % (n/n) | 33 (7/21) | 43 (15/35) | NS |
| Medications, % (n/n) | |||
| Lithium | 45 (5/11) | 54 (6/11) | NS |
| Anticonvulsant | 45 (9/20) | 55 (11/20) | NS |
| Antipsychotic | 42 (14/33) | 57 (19/33) | NS |
| Antidepressant | 60 (12/20) | 40 (8/20) | NS |
Lethality is rated as the highest lethality rating among all attempts.
Abbreviations: NA = not applicable, NS = nonsignificant.
Exclusion criteria were substance abuse/dependence within 1 month of study participation, unstable or severe medical illness, and history of significant neurologic injury, mental retardation, or dementia. Patients had not received electroconvulsive therapy within 12 months of study participation.24
The North Shore Long Island Jewish Health System Institutional Review Board reviewed and approved all study procedures. All participants provided written informed consent prior to their participation. Data were collected from July 2007 to July 2009.
Assessments
Suicide attempts were determined using the Columbia Suicide History Form.25 For primary analyses, we used a stringent definition of suicide attempters who reported at least 1 deliberate attempt. Deliberate attempts do not include ambiguous (self-injurious acts without intent to die), aborted (steps toward a suicidal act that are terminated before the act occurs), or interrupted attempts (self-injurious acts interrupted by outside circumstances). For secondary analyses, we classified individuals based on having made any kind of the above-described attempts. We also assessed current suicidal ideation with the Beck Scale for Suicidal Ideation.26
Clinical
The following symptom and mood ratings were administered to participants: 17-item Hamilton Depression Rating Scale (HDRS-17)27 and Clinician-Administered Rating Scale for Mania (CARS-M).28 Self-report measures included the Childhood Trauma Questionnaire,29 Barratt Impulsiveness Scale-version II (BIS-II),30 Aggression Questionnaire,31 and Reasons for Living Inventory.32
Neuropsychological cognitive testing
Neuropsychological tasks administered were previously associated with suicidality and/or bipolar disorder.33,34 We assessed the following cognitive domains: (1) attention (Wechsler Adult Intelligence Scale-Revised [WAIS-R]: Digit Span), (2) processing speed (WAIS-R Digit Symbol, Trail Making Test-Parts A and B, Letter Fluency, and Category Fluency), (3) verbal learning and memory (Hopkins Verbal Learning Test), and (4) executive function (Wisconsin Card Sorting Test, Stroop Color Word Test). Premorbid intellectual functioning (IQ) was assessed using the Wide Range Achievement Test reading subscale.
Decision making
A computerized version of the Iowa Gambling Task35 was administered. The Iowa Gambling Task is a decision-making task thought to reflect emotional decision making. The goal of the Iowa Gambling Task is for participants to make choices that maximize monetary gain and minimize monetary loss. Participants choose a card from 1 of 4 decks; 2 decks (A, B) are disadvantageous (monetary loss), while 2 decks are advantageous (C, D) (monetary gain). The task consists of 100 trials.
Statistical Analyses
We examined clinical, demographic, and cognitive differences between attempters and nonattempters. We also tested for significant predictors of prior suicide attempts. Data were analyzed using SPSS 11.0 (IBM, Chicago, Illinois).
Clinical and demographic
First, we assessed group differences in clinical characteristics using a series of t tests. Measures included the following: mood disorder type (bipolar I disorder, bipolar II disorder, bipolar disorder NOS), history of psychosis (yes, no), trauma history (yes, no), trait impulsivity (BIS-II total score), aggression (Aggression Questionnaire total score), reasons for living (Reasons for Living Inventory total score), and current depressive (HDRS-17) and manic symptoms (CARS-M). Demographic variables included age, sex, and race (white, nonwhite). We submitted the same variables as predictors to a binary logistic regression analysis. Premorbid IQ was included in order to control for individual differences in cognitive function.
We conducted follow-up analyses examining the association (Pearson correlation) between impulsivity (attention, motor, nonplanning, overall impulsiveness) and highest level of lethality from all prior attempts.6–8
Neuropsychological cognitive testing
In order to afford the advantage of statistically powering the study for fewer dependent measures, we entered neuropsychological tests into a principal components analysis. The principal components analysis was a factor analytic model using varimax rotation. Four factors were identified with eigenvalues greater than 1.0 and together explained 65% of the variance. Each of the 4 factors accounted for 28.5%, 14.5%, 12.2%, and 10.4% of the variance, respectively. The 4 factors were (1) processing speed (WAIS-R Digit Symbol, Trail Making Test-Parts A and B, Letter Fluency, and Category fluency), (2) executive function (Wisconsin Card Sorting Test, Stroop Color Word Test), (3) attention (WAIS-R Digit Span), and (4) verbal learning and memory (Hopkins Verbal Learning Test). Factor structure and loadings of the neuropsychological factors derived from the principal components analysis are reported as supplemental information (eTable 1 at PSYCHIATRIST.COM).
We used t tests to examine group differences in neuropsychological functioning. We assessed predictors of suicide attempt using a binary logistic regression with our 4 cognitive factors, premorbid IQ, age, and sex as predictor variables.
Decision making
We determined the proportion of cards chosen from disadvantageous decks (A, B) for 5 sets of 20 trials (Tl-20, T21-40, T41-60, T61-80, and T81-100) and total monetary losses/gains.36 The Iowa Gambling Task expectancy-valence model was enlisted using Matlab v. 7.3.0.298.37,38 This model yields 3 scores: recency (effects of memory for the most recent outcome on task performance), attention to losses/gains (persistence in choosing from disadvantageous or advantageous decks), and consistency (reliability of decision making).38 t Tests and Pearson correlations were used to assess outcomes.
RESULTS
Participants
The mean ± SD age of the final sample (N = 67) was 42.2 ± 11.5 years (range, 19.5–61.5), and 44.8% (n/N = 30/67) were female. The percentage of subjects who were white was 64.2% (n/N = 43/67), and 35.8% (n/N = 24/67) were nonwhite (Asian or Pacific Islander, black, Hispanic, other) (Table 1).
Table 1.
Clinical and Demographic Characteristics of Attempters Versus Nonattempters
| Variable | Attempter (n = 28) |
Nonattempter (n = 39) |
P |
|---|---|---|---|
| Demographic | |||
| Age, mean (SD), γ | 43.7 (10.7) | 41.1 (12.0) | NS |
| Female sex, % (n/n) | 50 (14/28) | 41 (16/39) | NS |
| White, % (n/n) | 68 (19/28) | 62 (24/39) | NS |
| Mood type | |||
| Bipolar I disorder, % (n/n) | 75 (21/28) | 77 (30/39) | NS |
| Bipolar II disorder, % (n/n) | 14 (4/28) | 18 (7/39) | NS |
| Bipolar disorder NOS, % (n/n) | 11 (3/28) | 5 (2/39) | NS |
| Psychosis, % (n/n) | 64 (18/28) | 63 (24/38) | NS |
| Trauma history, % (n/n) | 74 (20/27) | 72 (28/39) | NS |
| BIS-II total score, mean (SD) | 62.96 (8.84) | 69.88 (15.16) | < .05 |
| Aggression Questionnaire score, mean (SD) | 68.8 (23.5) | 72.6 (23.4) | NS |
| RFL total score, mean (SD) | 204.66 (47.72) | 211.48 (50.73) | NS |
| HDRS-17 score, mean (SD) | 8.60 (7.51) | 10.76 (6.92) | NS |
| CARS-M score, mean (SD) | 4.29 (3.58) | 5.24 (6.20) | NS |
Abbreviations: BIS-II = Barratt Impulsiveness Scale-version II, CARS-M = Clinician-Administered Rating Scale for Mania, HDRS-17 = 17-item Hamilton Depression Rating Scale, NOS = not otherwise specified, NS = nonsignificant, RFL = Reasons for Living Inventory.
When using the stringent, deliberate definition of attempt, we found that 41.8% (n/N = 28/67; mean ± SD age, 43.7 ± 12.0) of our sample had made at least 1 prior suicide attempt (“attempters”), while the remaining 58.2% (n/N = 39/67) had never attempted suicide (“nonattempters”). Data from a subset of our attempter sample (n = 25) indicate that a mean (SD) of approximately 14 (12) years elapsed between the time of the study and the past suicide attempt. Lethality was defined according to the medical consequences and damage related to the suicidal act and ranges from 0 (no attempt) to 8 (death), with increasing scores indicating increasing medical consequences and damage.
For secondary analyses, using our broad definition of suicide attempt, which incorporated ambiguous (n = 1), aborted (n = 15), and interrupted (n = 6) attempts (Table 2), we found that 50.7% (n/N = 34/67; mean ± SD age, 42.5 ± 11.0 years) of our sample were attempters, while the remaining 49.2% (n/N = 33/67) were nonattempters.
Clinical and Demographic Characteristics
Patients were stable at the time of assessment (HDRS-17 mean ± SD score = 9.8 ±7.3 [range, 0–28]; CARS-M mean ± SD score = 5.0 ± 5.2 [range, 0–29]) (Table 1). Attempters did not differ significantly from nonattempters on depression (t65 = 1.21, P = .23) or mania (t64 = 0.73, P = .47). There were no group differences in Aggression Questionnaire scores (t51 = 0.58, P = .56), Reasons for Living Inventory scores (t62 = 0.54, P = .59), bipolar disorder subtype (χ22 =0.82, P = .66), history of psychosis (χ21 = 0.01, P = .93), or Childhood Trauma Questionnaire scores (χ21 = 0.04, P = .83).
On the BIS-II, attempters reported lower trait impulsivity compared to nonattempters (t57 = 2.2, P = .03). Within the attempter group, we found a significant negative correlation between lethality and motor impulsiveness (r26 = −0.40, P = .04) as well as overall impulsiveness (motor, nonplanning, and attention) (r25 = −0.53, P = .01).
There were no significant differences between attempters and nonattempters on demographic variables: age (t65 = − 0.93, P = .35), sex (χ21 = 0.53, P = .47), and race (χ22 = 0.28, P = .56).
Our regression model did not yield significant clinical and demographic predictors of suicide attempts among bipolar disorder patients (Table 3). In secondary analyses, we used a broader definition of suicide attempt that included individuals who engaged in less deliberate suicidal acts. A notable difference in our findings was that WRAT scores were a significant predictor of attempter group (P = .04, OR = .90). However, groups did not differ when directly compared using t tests (t64 = 0.34, P = .74: attempters, mean ± SD score = 98.9 ± 12.2; nonattempters, mean ± SD score = 99.8 ± 8.9). Also, when broadly defined, impulsivity did not differ significantly between attempters (BIS-II total mean ± SD score = 64.5 ± 10.1) and nonattempters (BIS-II total mean ± SD score = 69.3 ± 15.5) (F = 2.0, P > .16). All other subscales, including motor, attention, and nonplanning subscales, were nonsignificant (all P values > .16).
Table 3.
Logistic Regression Analyses of Clinical and Demographic Predictors of Suicide Attempt
| Predictor | Odds Ratio |
95% CI | β | SE | Pa | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Age | 0.98 | 0.90 | 1.06 | −0.02 | 0.04 | .58 |
| Sex | 0.48 | 0.42 | 10.41 | 0.74 | 0.82 | .36 |
| Race | 0.95 | 0.13 | 6.65 | −0.06 | 1.00 | .96 |
| Mood type | 3.11 | 0.79 | 12.20 | 1.14 | 0.70 | .10 |
| Psychosis | 0.04 | 0.00 | 1.52 | −3.21 | 1.85 | .08 |
| Trauma history | 0.28 | 0.04 | 2.11 | −1.28 | 1.03 | .22 |
| BIS-II total score | 0.99 | 0.93 | 1.06 | −0.01 | 0.03 | .83 |
| Aggression Questionnaire | 0.99 | 0.95 | 1.03 | −0.01 | 0.02 | .64 |
| RFL total score | 0.98 | 0.96 | 1.00 | −0.02 | 0.01 | .10 |
| HDRS-17 | 0.90 | 0.79 | 1.03 | −0.10 | 0.07 | .12 |
| CARS-M | 1.02 | 0.86 | 1.20 | 0.02 | 0.09 | .85 |
| WRAT-III | 0.93 | 0.84 | 1.03 | −0.07 | 0.05 | .16 |
All P values are nonsignificant.
Abbreviations: BIS-II = Barratt Impulsiveness Scale-version II, CARS-M = Clinician-Administered Rating Scale for Mania, HDRS-17 = 17-item Hamilton Depression Rating Scale, RFL = Reasons for Living Inventory, SE = standard error, WRAT-III = Wide Range Achievement Test reading subscale.
Neuropsychological Characteristics
Cognitive testing
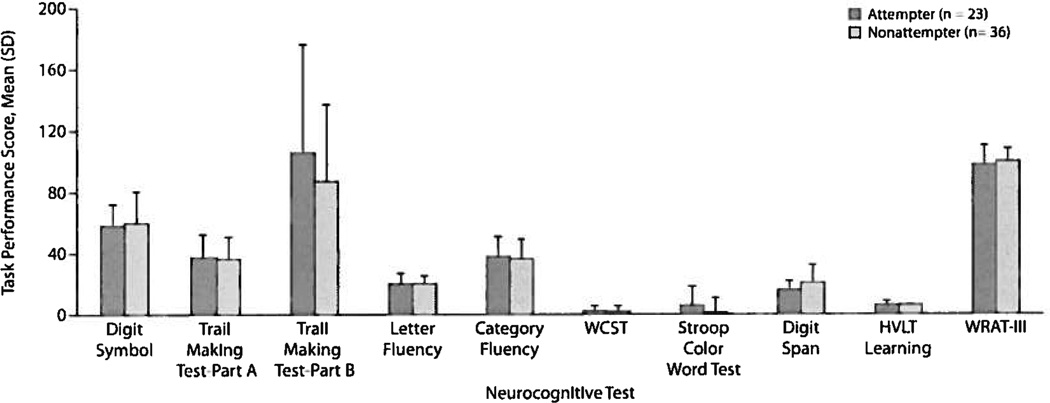
There were no significant differences between attempters and nonattempters on processing speed, attention, verbal learning, or executive function (all t57 values > −1.04; all P values > .30) (Figure 1). We did not find evidence of premorbid IQ differences between attempters and nonattempters (t64 = 0.74, P = .46). Our regression revealed no significant cognitive predictors of suicide attempts (Table 4).
Figure 1. Neurocognitive Performance for Attempters Versus Nonattempters.
Abbreviations: HVLT = Hopkins Verbal Learning Test, WCST = Wisconsin Card Sorting Test, WRAT-III = Wide Range Achievement Test reading subscale.
Table 4.
Logistic Regression Analyses of Cognitive Predictors of Suicide Attempt
| Predictor | Odds Ratio |
95% CI | β | SE | Pa | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Processing speed | 1.01 | 0.55 | 1.85 | 0.01 | 0.31 | .97 |
| Executive function | 1.19 | 0.66 | 2.14 | 0.17 | 0.30 | .56 |
| Attention | 1.47 | 0.78 | 2.78 | 0.39 | 0.32 | .23 |
| Verbal learning | 0.76 | 0.39 | 1.48 | −0.27 | 0.34 | .42 |
| WRAT-III | 0.97 | 0.91 | 1.03 | −0.03 | 0.03 | .33 |
| Age | 1.02 | 0.97 | 1.08 | 0.02 | 0.03 | .36 |
| Sex | 0.96 | 0.29 | 3.12 | −0.05 | 0.60 | .94 |
All P values are nonsignificant.
Abbreviations: SE = standard error, WRAT-III = Wide Range Achievement Test reading subscale.
Decision making
Attempters and nonattempters did not differ on total monetary losses/gains or net scores (t42 < 1.93, all P values > .06) (Table 5). We did not find significant group differences using expectancy-valence model (t42 > −0.69, all P values > .49). Highest level of lethality was not significantly correlated with any of the Iowa Gambling Task outcome measures (net scores, recency, attention to losses/gains, and reliability) (all r22 values < 0.31; all P values > .16). As some of these data were skewed, we repeated these analyses using nonparametric tests and found that this did not change the results. These results are inconsistent with the few existing findings of deficits on the Iowa Gambling Task among bipolar disorder patients with past suicide attempts.17,19
Table 5.
Decision Making Among Attempters Versus Nonattempters
| Iowa Gambling Task | Attempter, Mean (SD) |
Nonattempter, Mean (SD) |
P |
|---|---|---|---|
| Total amount won, $ | 84.94 (8.59) | 81.59 (5.70) | NS |
| Total amount lost, $ | −99.23 (16.43) | −90.24 (14.48) | NS |
| Total no. of cards chosen from | |||
| Deck A | 21.27 (8.04) | 21.18 (4.24) | NS |
| Deck B | 32.36 (13.58) | 28.09 (8.67) | NS |
| Deck C | 21.36 (7.35) | 21.00 (6.08) | NS |
| Deck D | 25.00 (9.58) | 29.73 (12.90) | NS |
| Net scores | |||
| T1–T20 | −3.00 (6.23) | −0.18 (4.78) | NS |
| T21–T40 | −0.18 (4.97) | 0.18 (4.32) | NS |
| T41–T60 | −1.73 (7.54) | 1.36 (7.21) | NS |
| T61–T80 | −0.95 (8.19) | 0.73 (8.13) | NS |
| T81–T100 | −1.23 (6.80) | 0.14 (7.00) | NS |
| Total net score (sum of net scores) | −7.09 (23.23) | 2.22 (19.90) | NS |
| Expectancy-Valence Model | |||
| Recency parameter | 0.26 (0.35) | 0.30 (0.41) | NS |
| Attention to losses and gains parameter | 0.40 (0.37) | 0.33 (0.36) | NS |
| Choice consistency parameter | 2.77 (3.63) | 2.61 (3.71) | NS |
Abbreviation: NS= nonsignificant.
Given the negative findings of this study and in light of prior positive results, we evaluated our power to detect differences that were reported in a related study that found significantly lower task scores on the Iowa Gambling Task among attempters versus nonattempters.19 Specifically, a significant group difference (P = .005) was reported on trials 41–60, with an effect size equivalent to a small effect (Cohen d = 0.16: attempters, mean ± SD effect size = −2.56 ± 4.69, n = 17; nonattempters, mean ± SD effect size = 3.71 ± 8.72, n = 19). With the current sample size (n = 44), our power to detect the same effect size difference is > 90%, suggesting that we were powered to find even small, statistically significant effects if they were indeed present in our cohort.
DISCUSSION
We investigated clinical, demographic, and neuropsychological variables that may be important in predicting suicide attempts among bipolar disorder patients. Consistent with a subset of recent research, we failed to find significant factors that serve to predict group membership when comparing those patients who have made at least 1 serious suicide attempt to those patients who have never made an attempt.
Interestingly, we found that attempters in our sample were less impulsive than nonattempters by self-report on the BIS-II. Other work yields either equivocal results or statistically significant results in the opposite direction when compared to our findings.7,10 One possible explanation is that we utilized the most stringent of definitions for an attempt, as defined by the Columbia Suicide History Form, while prior studies have used varying definitions. Specifically, an attempt on this scale is coded only if the act was deliberate with a clear intent to die. Indeed, when we examined the relationship between impulsivity and lethality, we found a significant negative correlation. We believe that the use of this stringent definition is a strength, supported by the fact that this scale has been specifically recommended by the US Food and Drug Administration for clinical trials because of its reliability as a suicide measure.39
Overall, our results and the results from a portion of related studies have failed to find reliable predictors of suicidal behavior, making it difficult for clinicians to prospectively predict which patients are at greatest risk. A significant consideration of this research is that our study examined stable trait measures as they relate to suicide attempt rather than measures of mood state or the interplay between trait measures and mood state as a predictor of suicide. A limitation of our study is that we did not assess for several factors that may have tracked with risk for suicidal behaviors, such as stressful life events, medication adherence, and mood state preceding suicide attempts. Indeed, prior research suggests that recent negative life events, lithium discontinuation, and mixed/depressed mood state may increase risk for suicide.40,41 –43
Consistent with our inability to detect significant neuro-psychological predictors of suicide attempt, the handful of existing studies has also yielded few significant results across cognitive domains.8,19,21,22 Our null findings may have been masked by our principal components analysis approach; however, this is unlikely, since each measure was incorporated into 1 of the 4 cognitive factors (ie, no variable was unaccounted for). Furthermore, when we examined individual cognitive tests, we failed to find any measure that significantly distinguished our attempter and nonattempter groups (P > .15). Prior research has examined similar domains of functioning using a different set of neuropsychological tests (n-back test of working memory) and found a significant association with suicide attempts among bipolar disorder patients.21 Negative results could also potentially result from a lack of statistical power. This does not seem to be the case since we demonstrate power > 90% to detect effect sizes in the range that has been previously reported in related research.
In conclusion, the results of our study strongly support the clinician’s dilemma when faced with the task of predicting which patients will attempt suicide and which patients are at a lower risk for acting on suicidal thoughts. It should be highlighted that even when clinical factors and cognition are comprehensively measured using a 4-hour battery, suicidal behavior is highly unpredictable. This study was retrospective, thereby inherently limiting its predictive ability, and its negative findings should not discourage future studies designed to explore quantifiable risk factors for suicide attempts, particularly using prospective analyses. Indeed, a diagnosis of bipolar illness places an individual at among the highest risk for dying by suicide, making ongoing efforts in this research area extremely important and potentially lifesaving.
Supplementary Material
Clinical Points.
-
■
The study’s inability to find reliable neuropsychological predictors confirms the difficulty faced by clinicians in identifying which patients are at greatest risk for suicide attempt.
-
■
Despite the failure to find reliable predictors of suicidal behavior, thorough clinical assessment of suicide risk by health care professionals continues to be essential.
Acknowledgments
Funding/support: This study was financially supported by grants from the National Institute of Mental Health (K23MH077807; R03MH079995) to Dr Burdick.
Footnotes
Potential conflicts of interest: Dr Goldberg has consulted for Merck and GlaxoSmithKline over the past year, receives royalties for use of the BACS in clinical trials from Neurocog Trials, and was awarded an investigator-initiated grant from Pfizer. Dr Malhotra has served as a consultant or speaker for Bristol Myers Squibb, Merck, AstraZeneca, Vanda, and Clinical Data; and has received research support from Pfizer, Janssen, Bristol Myers Squibb, and Eli Lilly. Dr Burdick has served on the speakers bureau for Merck. Drs Gilbert, Garno, and Braga and Mr Sliaya report no financial or other conflicts of interest relevant to the subject of this article.
REFERENCES
- 1.Goodwin FK, Jamison KR. Manic Depressive Illness. New York, NY: Oxford; 1990. [Google Scholar]
- 2.Oquendo MA, Waternaux C, Brodsky B, et al. Suicidal behavior in bipolar mood disorder: clinical characteristics of attempters and nonattempters. J Affect Disord. 2000;59(2):107–117. doi: 10.1016/s0165-0327(99)00129-9. [DOI] [PubMed] [Google Scholar]
- 3.Chen YW, Dilsaver SC. Lifetime rates of suicide attempts among subjects with bipolar and unipolar disorders relative to subjects with other Axis I disorders. Biol Psychiatry. 1996;39(10):896–899. doi: 10.1016/0006-3223(95)00295-2. [DOI] [PubMed] [Google Scholar]
- 4.Abreu LN, Lafer B, Baca-Garcia E, et al. Suicidal ideation and suicide attempts in bipolar disorder type 1: an update for the clinician. Rev Bras Psiquiatr. 2009;31(3):271–280. doi: 10.1590/s1516-44462009005000003. [DOI] [PubMed] [Google Scholar]
- 5.Mann JJ, Waternaux C, Haas GL, et al. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156(2):181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 6.Oquendo MA, Galfalvy H, Russo S, et al. Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. Am J Psychiatry. 2004;161(8):1433–1441. doi: 10.1176/appi.ajp.161.8.1433. [DOI] [PubMed] [Google Scholar]
- 7.Swann AC, Dougherty DM, Pazzaglia PJ, et al. Increased impulsivity associated with severity of suicide attempt history in patients with bipolar disorder. Am J Psychiatry. 2005;162(9):1680–1687. doi: 10.1176/appi.ajp.162.9.1680. [DOI] [PubMed] [Google Scholar]
- 8.Swann AC, Lijffijt M, Lane SD, et al. Increased trait-like impulsivity and course of illness in bipolar disorder. Bipolar Disord. 2009;11(3):280–288. doi: 10.1111/j.1399-5618.2009.00678.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brodsky BS, Oquendo M, Ellis SP, et al. The relationship of childhood abuse to impulsivity and suicidal behavior in adults with major depression. Am J Psychiatry. 2001;158(11):1871–1877. doi: 10.1176/appi.ajp.158.11.1871. [DOI] [PubMed] [Google Scholar]
- 10.Galfalvy H, Oquendo MA, Carballo JJ, et al. Clinical predictors of suicidal acts after major depression in bipolar disorder: a prospective study. Bipolar Disord. 2006;8(5 Pt 2):586–595. doi: 10.1111/j.1399-5618.2006.00340.x. [DOI] [PubMed] [Google Scholar]
- 11.Leverich GS, Altshuler LL, Frye MA, et al. Factors associated with suicide attempts in 648 patients with bipolar disorder in the Stanley Foundation Bipolar Network. J Clin Psychiatry. 2003;64(5):506–515. doi: 10.4088/jcp.v64n0503. [DOI] [PubMed] [Google Scholar]
- 12.Grunebaum MF, Ramsay SR, Galfalvy HC, et al. Correlates of suicide attempt history in bipolar disorder: a stress-diathesis perspective. Bipolar Disord. 2006;8(5 Pt 2):551–557. doi: 10.1111/j.1399-5618.2006.00304.x. [DOI] [PubMed] [Google Scholar]
- 13.Tondo L, Lepri B, Baldessarini RJ. Suicidal risks among 2826 Sardinian major affective disorder patients. Acta Psychiatr Scand. 2007;116(6):419–428. doi: 10.1111/j.1600-0447.2007.01066.x. [DOI] [PubMed] [Google Scholar]
- 14.Pompili M, Rihmer Z, Innamorati M, et al. Assessment and treatment of suicide risk in bipolar disorders. Expert Rev Neurother. 2009;9(1):109–136. doi: 10.1586/14737175.9.1.109. [Review]. [DOI] [PubMed] [Google Scholar]
- 15.López P, Mosquera F, de León J, et al. Suicide attempts in bipolar patients. Clin Psychiatry. 2001;62(12):963–966. doi: 10.4088/jcp.v62n1208. [DOI] [PubMed] [Google Scholar]
- 16.Keilp JG, Sackeim HA, Brodsky BS, et al. Neuropsychological dysfunction in depressed suicide attempters. Am J Psychiatry. 2001;158(5):735–741. doi: 10.1176/appi.ajp.158.5.735. [DOI] [PubMed] [Google Scholar]
- 17.Jollant F, Bellivier F, Leboyer M, et al. Impaired decision making in suicide attempters. Am J Psychiatry. 2005;162(2):304–310. doi: 10.1176/appi.ajp.162.2.304. [DOI] [PubMed] [Google Scholar]
- 18.Bora E, Yucel M, Pantelis C. Cognitive endophenotypes of bipolar disorder: a meta-analysis of neuropsychological deficits in euthymic patients and their first-degree relatives. J Affect Disord. 2009;113(1–2):1–20. doi: 10.1016/j.jad.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 19.Malloy-Diniz LF, Neves FS, Abrantes SS, et al. Suicide behavior and neuropsychological assessment of type 1 bipolar patients. J Affect Disord. 2009;112(1–3):231–236. doi: 10.1016/j.jad.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 20.Swann AC, Lijffijt M, Lane SD, et al. Severity of bipolar disorder is associated with impairment of response inhibition. J Affect Disord. 2009;116(1–2):30–36. doi: 10.1016/j.jad.2008.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harkavy-Friedman JM, Keilp G, Grunebaum MF, et al. Are BPI and BPII suicide attempters distinct neuropsychologically? J Affect Disord. 2006;94(1–3):255–259. doi: 10.1016/j.jad.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 22.Martinez-Arán A, Vieta E, Reinares M, et al. Cognitive function across manic or hypomanic, depressed, and cuthymic states in bipolar disorder. Am J Psychiatry. 2004;161(2):262–270. doi: 10.1176/appi.ajp.161.2.262. [DOI] [PubMed] [Google Scholar]
- 23.First MB, Spitzer RL, Gibbon M, et al. Research version, Patient Edition (SCID-1/P) Biometrics Research. New York, NY: New York State Psychiatric Institute; 1997. Structured Clinical Interview for the DSMIV Axis 1 Disorders. [Google Scholar]
- 24.Nobler MS, Sackeim HA. Neurobiological correlates of the cognitive side effects of electroconvulsive therapy. J ECT. 2008;24(1):40–45. doi: 10.1097/YCT.0b013e31815d6957. [DOI] [PubMed] [Google Scholar]
- 25.Oquendo MA, Halberstam B, Mann JJ. Risk factors for suicidal behavior: utility and limitations of research instruments. In: First MB, editor. Standardized Evaluation in Clinical Practice. Washington, DC: American Psychiatric Publishing; 2003. pp. 103–130. [Google Scholar]
- 26.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicidal Ideation. Consult Clin Psychol. 1979;47(2):343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 27.Hamilton M. A rating scale for depression. Neural Neurosurg Psychiatry. 1960;23(1):56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Altman EG, Hedeker DR, Janicak PG, et al. The Clinician-Administered Rating Scale for Mania (CARS-M): development, reliability, and validity. Biol Psychiatry. 1994;36(2):124–134. doi: 10.1016/0006-3223(94)91193-2. [DOI] [PubMed] [Google Scholar]
- 29.Bernstein DP, Fink L. Childhood Trauma Questionnaire: A Retrospective Self-Report Manual. San Antonio, TX: The Psychological Corporation; 1998. [Google Scholar]
- 30.Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51(6):768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 31.Buss AH, Perry M. The aggression questionnaire. J Pers Soc Psychol. 1992;63(3):452–459. doi: 10.1037//0022-3514.63.3.452. [DOI] [PubMed] [Google Scholar]
- 32.Linehan MM. Skills Training Manual for Treatment of Borderline Personality Disorder. New York, NY: Guilford Press; 1993. [Google Scholar]
- 33.Bartfai A, Winborg l-M, Nordström P, et al. Suicidal behavior and cognitive flexibility: design and verbal fluency after attempted suicide. Suicide Life Threat Behav. 1990;20(3):254–266. [PubMed] [Google Scholar]
- 34.Marzuk PM, Hartwell N, Leon AC, et al. Executive functioning in depressed patients with suicidal ideation. Acta Psychiatr Scand. 2005;112(4):294–301. doi: 10.1111/j.1600-0447.2005.00585.x. [DOI] [PubMed] [Google Scholar]
- 35.Bechara A, Damasio AR, Damasio H, et al. Insensilivity to future con sequences following damage to human prefrontal cortex. Cognition. 1994;50(1–3):7–15. doi: 10.1016/0010-0277(94)90018-3. [DOI] [PubMed] [Google Scholar]
- 36.Sevy S, Burdick KE, Visweswaraiah H, et al. Iowa gambling task in schizophrenia: a review and new data in patients with schizophrenia and co-occurring cannabis use disorders. Schizophr Res. 2007;92(1–3):74–84. doi: 10.1016/j.schres.2007.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Busemeyer JR, Stout JC. A contribution of cognitive decision models to clinical assessment: decomposing performance on the Bechara gambling task. Psychol Assess. 2002;14(3):253–262. doi: 10.1037//1040-3590.14.3.253. [DOI] [PubMed] [Google Scholar]
- 38.Yechiam E, Busemeyer JR, Stout JC, et al. Using cognitive models to map relations between neuropsychological disorders and human decision-making deficits. Psychol Sci. 2005;16(12):973–978. doi: 10.1111/j.1467-9280.2005.01646.x. [DOI] [PubMed] [Google Scholar]
- 39.Posncr K, Oquendo MA, Gould M, et al. Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA's pediatric suicidal risk analysis of antidepressants. Am J Psychiatry. 2007;164(7):1035–1043. doi: 10.1176/appi.ajp.164.7.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Valtonen HM. Suicidal Behavior in Bipolar Disorder. Helsinki, Finland: National Public Health Institute; 2007. [Google Scholar]
- 41.Azorin JM, Kaladjian A, Adida M, et al. Risk factors associated with lifetime suicide attempts in bipolar I patients: findings from a French National Cohort. Compr Psychiatry. 2009;50(2):115–120. doi: 10.1016/j.comppsych.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 42.Baldessarini RJ, Tondo L, Davis P, et al. Decreased risk of suicides and attempts during long-term lithium treatment: a meta-analytic review. Bipolar Disord. 2006;8(5, Pt 2):625–639. doi: 10.1111/j.1399-5618.2006.00344.x. [DOI] [PubMed] [Google Scholar]
- 43.Valtonen HM, Suominen K, Haukka J, et al. Differences in incidence of suicide attempts during phases of bipolar I and II disorders. Bipolar Disord. 2008;10(5):588–596. doi: 10.1111/j.1399-5618.2007.00553.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.