Abstract
Introduction:
Thrombocytopenia is highly prevalent among patients with Systemic Lupus Erythematous(SLE) and at the same time it has been reported that a correlation exists between Thrombocytopenia and organ damage. The aim of this study is to highlight the correlation between Thrombocytopenia and the clinical manifestations of SLE.
Objectives:
The objective is to show the clinical manifestations and organ damage of Systemic Lupus Erythematous (SLE) patients who have been found to have Thrombocytopenia.
Methods:
A retrospective study was conducted examining all patient charts diagnosed and treated for SLE at the Rheumatology Service of Mother Teresa Hospital Centre. All the data were collected from discharged patient charts. The data included were Anti DNA,AAN,C3 , thrombocytopenia, leucopenia, and organ damage. Data were taken from 2009 to 2013. The classification criteria of the American College of Rheumatology was used for all patients regarding the diagnosis.
Results:
Out of 330 patients, 12 (3.64%) are men and 318 (96.3%) women. 73 of all patients have thrombocytopenia as cases and 257 patients had SLE without thrombocytopenia, which was considered as the control group. AAN 68(93.1%), Anti DNA 50 (64.3%) , low value of C3 46 (63%), and leucopenia were higher in thrombocytopenic patients compared with control group (p<0.05) 48 (65.7%) of thrombocytopenic patients develop lupus nephritis, 10 (13.6%) were with pulmonary involvement, and 42 (57.5%) had leukopenia.
Conclusion:
Thrombocytopenia is not directly associated with any disease activity, organ damage and mortality, but it should be considered as a prognostic factor which may help identifying a category of patients whose disease course can be aggravated.
Keywords: Thrombocytopenia, upus Nephritis, Anti DNA, AAN, C3
1. INTRODUCTION
Systemic Lupus Erythematous (SLE) is an autoimmune disease with multiple organ involvement (1-5). SLE is characterized by the production of unusual antibodies in the blood which mistakenly attacks healthy tissue. It can affects skin, bone marrow, kidneys, joints, heart, brain and other organs (6-8). Hematologic abnormalities, including anaemia, thrombocytopenia, leukopenia are commonly found in SLE patients. Thrombocytopenia has a reported prevalence ranging from 7 to 30 % in patients of SLE. Thrombocytopenia in SLE result from SLE disease activity, bone marrow suppression from immunosuppressant, co medications The field of pathophysiology is rendered even more intriguing with autoantibodies against platelets, autoantibodies against thrombopoetin and bone marrow abnormalities. Despite the high prevalence of antibodies against platelets among thrombocytopenic patients a number of them display thrombocytopenia without anti-PLT positivity and on the other hand patients with thrombocytopenia are negative against anti-PLT. Antiplatelet antibodies are neither specific nor sensitive in SLE and remain the most important mechanism of platelets destructions. Human TPO is the regulator of PLT production and has an important role in normal hemopoiesis. It acts as a growth factor in differentiated) immature megacaryoblasts, inhibit apoptosis and leads finally to the release of normal platelets. There are elements that include bone marrow as a factor of thrombocytopenia. Anti-TPO antibodies have a persistent but weak effect on plate counts. Faulty hematosis due to the presence of auto reactive lymphocytes and the effect of pro inflammatory cytokines implicate bone marrow as a factor of thrombocytopenia. Bone marrow damage may determine the extend and the severity Thrombocytopenia is generally seen with other cytopenias but with or without is an independent risk factor of disease activity. Although there is an association between anti-ds DNA antibodies, hypocomplementemia , disease activity, involvement of kidneys (lupus nephritis), and increased mortality. Our study indicated that thrombocytopenia is a characteristic of lupus activity. The coexistence of thrombocytopenia and lupus nephritis is an index of worsening disease activity and comorbidity. Episodes of hemorrhagic and thrombocytopenic purpura are fortunately rare in SLE patients with thrombocytopenia.
2. PATIENTS AND METHODS
We retrospectively examined patients from 16 years and older, admitted to Mother Teresa University Hospital Centre. Cases of SLE were identified from databases with the corresponding International Classification of Disease code 710 from July 2009 to December 2013. The classification criteria of the American College of Rheumatology were obtained from all patients at the time of diagnosis. Age, sex, disease activity, disease duration, autoantibody profile, and organ damage were recorded. This retrospective study included patients who were first diagnosed with SLE and other groups were composed from patients with SLE in treatment. At each patient visit, a complete history, routine laboratory testing, and treatment were performed in a systematic fashion. Thrombocytopenia, Anti ds-DNA and serum C3 were measured frequently. Antinuclear antibodies were determined by indirect immunofluorescence, whereas anti-dsDNA and cardiolipin were determined a Standard Enzyme Linked Immunosorbent Assay (ELISA) C3 was determined by nephelometry. Blood test,Anti ds-DNA and serum C3 were measured frequently. Platelet numbers at the onset of thrombocytopenia and hemorrhagic manifestations were recorded for both groups of patients.
Statistical analysis
The statistical analyses was done with SPSS (Statistical Package for Social Sciences) Chicago Illinois version 19.0. The frequencies were done for categorical variables such are organ damage, DNA, C3, etc. Chi square test, OR and confidence interval 95% calculations were performed to see differences between cases and control groups. P value ≤0.05 was considered as statistical significance.
3. RESULTS
Three hundred thirty (330) patients of SLE diagnosis based on the classification criteria of the American College of Rheumatology were included in our study. Out of 330 patients 12/330 are men and 318/330 women. 73 of all patients have thrombocytopenia and 257 patients had SLE without thrombocytopenia. The aim of our study is to evaluate the impact of thrombocytopenia in SLE patients and to explore the correlation of thrombocytopenia with immunologic autoantibodies (AAN, Anti DNA, C3 , C4,) and organ involvement like lupus nephritis, pulmonary involvement etc.
We studied the correlation of thrombocytopenia with clinical signs. Results are shown on Table 1.
Table 1.
Clinical profile among thrombocytopenic group and control group. *OR=odd ratio,**P value ≤0.05 as significant level
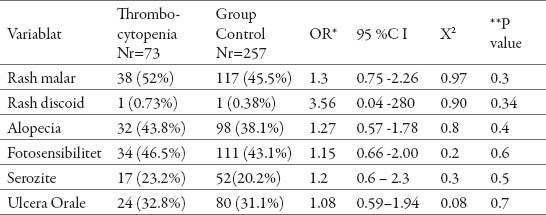
Patients with thrombocytopenia have more expressed clinical signs. Malar rash in thrombocytopenic patients is 38 (52%) higher than control group 117(45.5%) with OR=1.3, and 95 %C I(0.75-2.26) with P value 0.3. Other values of clinical signs that indicate disease activity are more expressed in thrombocytopenic patients than in non-thrombocytopenic patients but there is no statistical significance between these cases and control group. Immunologic findings are very important in Systemic Lupus Erythematous. We evaluate disease activity and organ damage by monitoring immunologic markers. Positivity of AAN and anti -DNA accompanied with low titter of complement C3 are indicators of lupus nephritis.
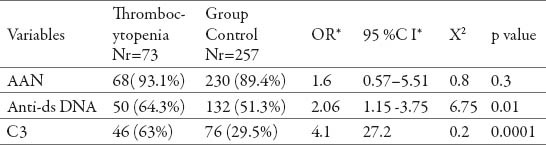
The Table 2 shows that positivity of AAN and anti -DNA are higher than control group. Anti-ds DNA among cases was OR=2.06 higher than control group, 95% CI(1.15 to 3.75) and the difference among two groups was statistically significant (P value= 0.01) Regarding (C3)among patients with Thrombocytopenia accompanied with low titter of complement C3(OR=4.1%, 95% CI 27.2, p=0.0001), and leucopenia (Or=2.13, 95%CI 1.21-3.74 with P value 0.005). The differences for two groups were statistically significant. Base on the results Anti-ds DNA, C3 can be as predictors of lupus nephritis. An analysis of complement activity showed similar results, and patients with low C3 were more likely to be thrombocytopenic indicating a more active disease in thrombocytopenic patients.
Table 2.
Autoimmune profile among thrombocytopenic group and control group. *OR=odd ratio,**P value ≤0.05 as significant level
Organ damage are represented in Table 3
Table 3.
The prevalence of organ damage among cases and control group. *OR=odd ratio,**P value ≤0.05 as significant level
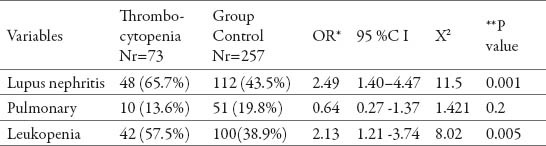
Lupus nephritis 48(65.7%), is the most common complication of patients with thrombocytopenia or 2.49 times higher than controlled group, 95%CI (1.4-4.47) with statistical difference between two groups (P=0.001). Leukopenia 42 (57.5%) OR 2.13, P< 0.005) and pulmonary involvement 10 (13.6%, OR 0.64, P<0.2) are two other more frequently affected in SLE patients compared with control.
4. DISCUSSION
Thrombocytopenia, leukopenia and anaemia in Systemic Lupus erythematous are included in the criteria of diagnosing SLE. Haemopoietic abnormalities in SLE are evident and different studies (1, 2, 3) show the correlation of leucopenia and anaemia with severe disease activity. As it is seen in our study, there is an association between disease activity and the coexistence of thrombocytopenia. Different authors identified thrombocytopenia as an important prognostic (4, 5, 6) feature and that it should be evaluated not only for the risk of hemorrhagic manifestations. General causes of thrombocytopenia are: increased peripheral destruction of plates, associated with the presence of anti-plated antibodies and antitrombopoetin (7) (TPO) antibodies (the TPO receptor c-MpL and CD40L (1). These are the most likely pathogenic mechanisms. The presence of severe and resistant of thrombocytopenia is usually related to disease activity, and these patients tend to be (Corticosteroids) CS less responsive (7). Thrombocytopenia may also occur as a complication of drug therapy with, for example, immunosuppressant such as Azathioprine and rarely Hydroxichlorochina (8). Thrombotic micro angiopathic hemolytic anaemia is also reported in association with SLE, characterized by thrombocytopenia, hemolytic anaemia, fever, neurological symptoms and kidney involvement. In most patients thrombocytopenia follows a benign course, and only a few patients had severe bleeding. Complement is used as a single estimate of kidney involvement, thrombocytopenia itself does not influence in overall morbidity , but in correlation with AAN, Anti DNA and C3, C4 indicate lupus nephritis (6, 8), pulmonary or/and nervous system involvement. Differences of outcome in different studies may be attributed to different treatments, population, and the database study design. This is a retrospective study but all patients included have been followed up in regular intervals at Mother Teresa University Hospital”. There are evident differences between the two groups with or without thrombocytopenia in disease activity and morbidity. That makes the thrombocytopenic factor a very important one in the evaluation of organ damage (8). However there is no correlation between the time that any organ will be damaged. Thrombocytopenia should be considered as a prognostic factor, identifying a category of patients whose disease course can be aggravated.
5. CONCLUSION
Our results showed that thrombocytopenic factors, and especially Ant DNA, AAN, C3 and Leucopenia, are very useful indicators in evaluation of organ damage. Thrombocytopenia should be recommended as a diagnostic and prognostic factor in systemic lupus erythematous.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Mok CC, Lee KW, Ho CT, Lau CS, Wong RW. A prospective study of survival and prognostic indicators of systemic lupus erythematous in a southern Chinese population. Rheumatology (Oxford) 2000;39:399–406. doi: 10.1093/rheumatology/39.4.399. [DOI] [PubMed] [Google Scholar]
- 2.Ziakas PD, Giannouli S, Zintzaras E, Tzioufas AG, Voulgarelis M. Lupus thrombocytopenia: clinical implications and prognostic significance. Ann Rheum Dis. 2005;64:1366–1369. doi: 10.1136/ard.2004.033100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ziakas PD, Dafni UG, Giannouli S, Tzioufas AG, Voulgarelis M. Thrombocytopaenia in lupus as a marker of adverse outcome–seeking Ariadne’s thread. Rheumatology (Oxford) 2006;45:1261–1265. doi: 10.1093/rheumatology/kel101. [DOI] [PubMed] [Google Scholar]
- 4.Ziakas PD, Poulou LS, Giannouli S, Tzioufas AG, Voulgarelis M. Thrombocytopenia in lupus: baseline C3 as an independent risk factor for relapse. Ann Rheum Dis. 2007;66:130–13I. doi: 10.1136/ard.2006.059758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fossati G, Bucknall RC, Edwards SW. Fcgamma receptors in auto- immune diseases. Eur J Clin Invest. 2001;31:821–831. doi: 10.1046/j.1365-2362.2001.00881.x. [DOI] [PubMed] [Google Scholar]
- 6.Ziakas PD, Routsias JG, Giannouli S, Tasidou A, Tzioufas AG, Voulgarelis M. Suspects in the tale of lupus-associated thrombocytopenia. Clin Exp Immunol. 2006;145:71–80. doi: 10.1111/j.1365-2249.2006.03122.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ziakas PD, Papadaki H, Psyllaki M, Voulgarelis M. Anti-Thrombopoietin antibodies suppress megakaryocytic colony formation in vitro in patients with systemic lupus erythematous. Ann Rheum Dis. 2008;67:1643–1644. doi: 10.1136/ard.2007.087478. [DOI] [PubMed] [Google Scholar]
- 8.Bhatt AS, Berliner N. Hematologic Manifestations of SLE In Lupus Erythematous: Clinical Evaluation and Treatment. In: Schur P, Massarotti E, editors. New York: Springer; 2012. pp. 127–140. [Google Scholar]


