While adefovir dipivoxil (ADV) effectively suppresses the hepatitis B virus, it can cause proximal renal tubular dysfunction leading to phosphate wasting [1, 2]. The safety of low-dose ADV (a dose of 10 mg/day), which does not induce clinically significant nephrotoxicity, is well recognized, but a few cases of hypophosphatemic osteomalacia (HO) caused by low-dose ADV therapy have recently been reported [3–6].
Although HO induced by low-dose ADV therapy is rare, the presence of bone pain in patients treated with ADV should be monitored. Bone scintigraphy can be performed to confirm the occurrence of osteomalacia and to determine the disease extent. Bone scintigraphic and radiological image findings with a brief review of the literature are presented in this article.
We report two cases of HO induced by low-dose ADV therapy that showed multifocal increased radiotracer uptakes in the bilateral bony ribs, spines, pelvic bones and lower extremities on whole-body bone scintigraphy (Figs. 1 and 2). Bone pain gradually improved after phosphate supplementation and by changing the antiviral agent.
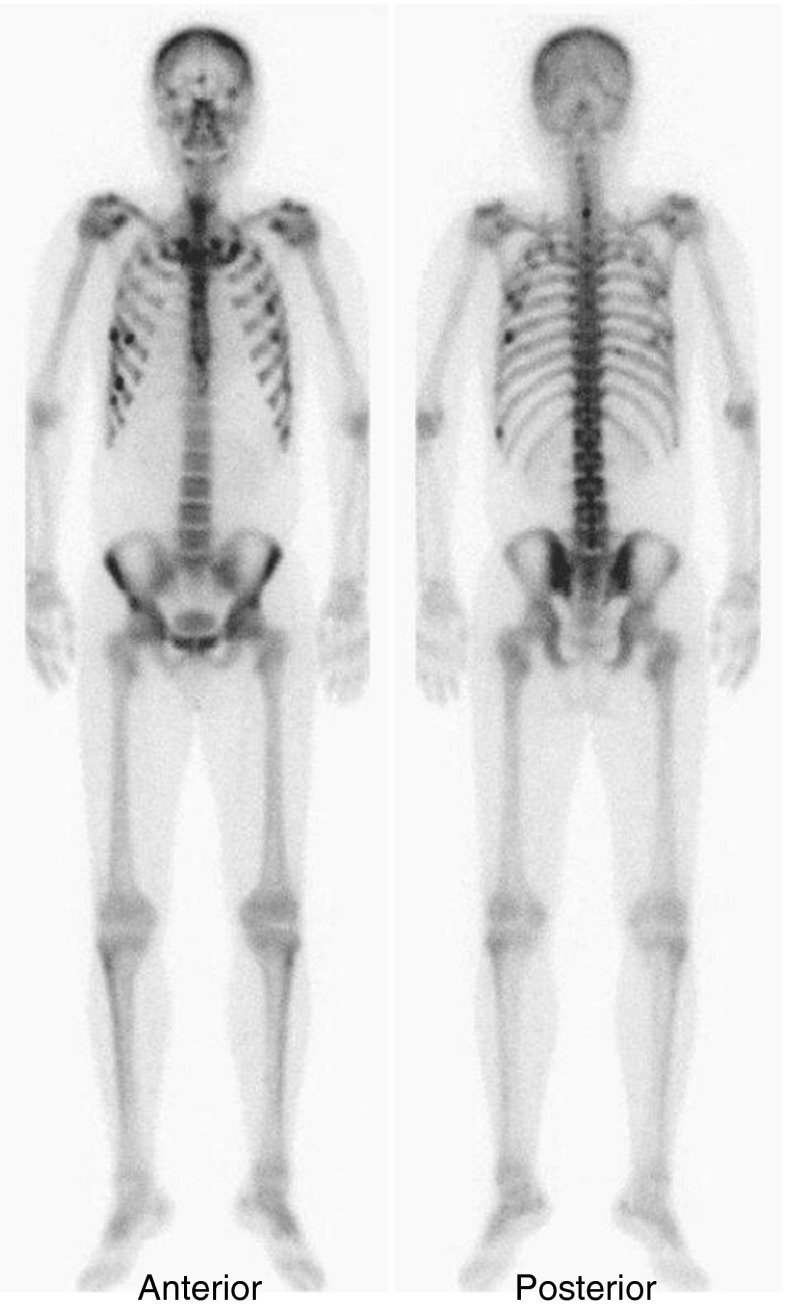
Fig. 1.
A 44-year-old man presented with a 6-month history of diffuse musculoskeletal pain in the chest, back and both knees without antecedent trauma. The patient had a history of chronic hepatitis B infection and had received adefovir dipivoxil (ADV) (10 mg/day) for 8 years. Laboratory tests revealed hypophosphatemia (serum phosphorus of 1.6 mg/dl; normal range, 2.5–4.5 mg/dl) and an increased serum ALP level (1,218 U/l; normal range, 104–338 U/l), and the results were otherwise within normal range. Tc-99m whole-body bone scintigraphy (a) showed multiple foci of increased radiotracer uptake in the bilateral bony ribs, costovertebral junctions, lower cervical spine, glenoid process of the right scapula, both sides of the pelvic bone, the distal end of the left femur, the proximal and distal end of the right tibia, and faint uptake in both kidneys. Pelvic MRI (b) reveals fractures in the left anterior acetabular rim, right pubic tubercle and left inferior pubic ramus (arrows) with focal bone marrow edema on the axial plane of T2-weighted images, which corresponded to areas of the bone scan. Also, fractures in the spinous process of C7 and both bony ribs (arrows) were noted on chest CT (c). Symptomatic and biochemical improvements were observed after cessation of ADV and phosphate supplementation. A follow-up bone scan 4 months later showed marked improvement of the previously increased radioactivity in both lower legs and no definite interval change in the rest (not shown here)
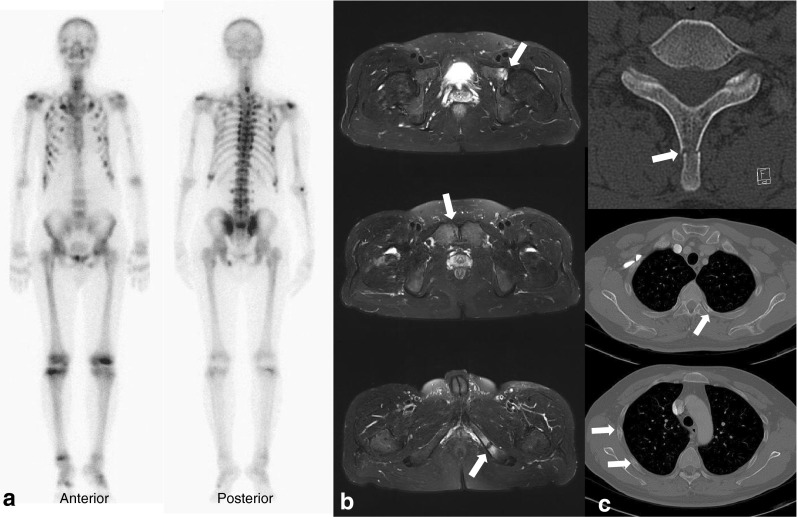
Fig. 2.
A 42-year-old man who had taken adefovir dipivoxil (ADV) (10 mg/day) for 7 years for treatment of chronic hepatitis B complained of a 2-year history of diffuse musculoskeletal pain in the anterior chest area with absence of antecedent trauma. Laboratory investigations showed a decreased serum phosphorus level (1.6 mg/dl, normal range, 2.5–4.5 mg/dl), increased serum ALP level (702 U/l, normal range, 104–338 U/l) with a slightly elevated serum creatinine level (1.6 mg/dl, normal range, 0.7–1.3 mg/dl). Multifocal hot spots were noted on both sides of the rib cage on whole-body bone scintigraphy with faint uptake in both kidneys. On the basis of these findings, the patient was diagnosed as having osteomalacia and pathological fractures associated with ADV therapy. Bone pain was significantly reduced after discontinuation of ADV and correction of the hypophosphatemia
Whole-body bone scintigraphy is a highly sensitive imaging tool and can show disease extent at once in the setting of the wide range of the clinical spectrum with nonspecific radiological findings [5]. Furthermore, frequent involvement of the lower extremities, as a result of maximum weight bearing, could be an additional scintigraphic clue for the diagnosis of HO [6, 7]. These cases could be helpful for both clinicians prescribing ADV and nuclear physicians to prevent delayed diagnosis and plan further appropriate treatment.
Acknowledgments
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
References
- 1.Wong T, Girgis CM, Ngu MC, Chen RC, Emmett L, Archer KA, et al. Hypophosphatemic osteomalacia after low-dose adefovir dipivoxil therapy for hepatitis B. J Clin Endocrinol Metab. 2010;95:479–480. doi: 10.1210/jc.2009-2051. [DOI] [PubMed] [Google Scholar]
- 2.Girgis CM, Wong T, Ngu MC, Emmett L, Archer KA, Chen RC, et al. Hypophosphataemic osteomalacia in patients on adefovir dipivoxil. J Clin Gastroenterol. 2011;45:468–473. doi: 10.1097/MCG.0b013e3181e12ed3. [DOI] [PubMed] [Google Scholar]
- 3.Izzedine H, Hulot JS, Launay-Vacher V, Marcellini P, Hadziyannis SJ, Currie G, et al. Renal safety of adefovir dipivoxil in patients with chronic hepatitis B: two double-blind, randomized, placebo-controlled studies. Kidney Int. 2004;66:1153–1158. doi: 10.1111/j.1523-1755.2004.00866.x. [DOI] [PubMed] [Google Scholar]
- 4.Tanaka M, Setoguchi T, Ishidou Y, Arishima Y, Hirotsu M, Saitoh Y, et al. Pathological femoral fractures due to osteomalacia associated with adefovir dipivoxil treatment for hepatitis B: a case report. Diagn Pathol. 2012;7:108. doi: 10.1186/1746-1596-7-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim DH, Sung DH, Min YK. Hypophosphatemic osteomalacia induced by low-dose adefovir therapy: focus on manifestations in the skeletal system and literature review. J Bone Miner Metab. 2013;31:240–246. doi: 10.1007/s00774-012-0384-y. [DOI] [PubMed] [Google Scholar]
- 6.Kim DH, Lee SW, Kweon YO, Lee J, Ahn BC. Bone scintigraphic findings of hypophosphatemic osteomalacia associated with adefovir therapy. Clin Nucl Med. 2013;38:278–280. doi: 10.1097/RLU.0b013e31828164bd. [DOI] [PubMed] [Google Scholar]
- 7.Seo HJ, Choi YJ, Kim HJ, Jeong YH, Cho A, Lee JH, et al. Using 18F-FDG PET/CT to detect an occult mesenchymal tumor causing oncogenic osteomalacia. Nucl Med Mol Imaging. 2011;45:233–237. doi: 10.1007/s13139-011-0095-7. [DOI] [PMC free article] [PubMed] [Google Scholar]