Abstract
When given a choice, how do people decide which physician to select? Although significant research has demonstrated that how people actually feel (their “actual affect”) influences their health care preferences, how people ideally want to feel (their “ideal affect”) may play an even greater role. Specifically, we predicted that people trust physicians whose affective characteristics match their ideal affect, which leads people to prefer those physicians more. Consistent with this prediction, the more participants wanted to feel high arousal positive states on average ([ideal HAP]; e.g., excited), the more likely they were to select a HAP-focused physician. Similarly, the more people wanted to feel low arousal positive states on average ([ideal LAP]; e.g., calm), the more likely they were to select a LAP-focused physician. Also as predicted, these links were mediated by perceived physician trustworthiness. Notably, while participants’ ideal affect predicted physician preference, actual affect (how much people actually felt HAP and LAP on average) did not. These findings suggest that people base even serious decisions on how they want to feel and highlight the importance of considering ideal affect in models of decision making, person perception, and patient physician communication.
Keywords: Ideal Affect, Health, Decision Making, Emotion, Patient Physician Communication, Person Perception, Trust
Imagine that you need to choose a new primary care physician. You read about two available physicians. Both have similar credentials, but one aims to “increase patients’ vitality,” whereas the other aims to “ensure patients’ peace of mind.” Whom do you choose, and why? Alongside credentials, physicians’ interpersonal rapport is one of the most important factors in selecting a physician (e.g., Mercado, Mercado, Myers, Hewit, & Haller, 2012), suggesting that physicians’ affective characteristics matter. Indeed, patients often respond better to physicians who express more affect (e.g., concern, pleasantness; for reviews, see Beck, Daughtridge, & Sloane, 2002; Blasi, Harkness, Ernst, Georgiou, & Kleijnen, 2001; DiMatteo, 1979; Levine & Ambady, in press). Further, providers who express more positive affect have patients who feel more satisfied (Griffith, Wilson, Langer, & Haist, 2003), have better health outcomes (Ambady, Koo, Rosenthal, & Winograd, 2002), and are more likely to keep follow-up appointments (Hall, Roter, & Rand, 1981). Patients’ affective traits also seem to play a role (e.g., trait anxiety predicts medication non-adherence [Wroe, 2002]), although this work mostly focuses on negative affect. None of these studies, however, have examined how physicians’ affective expressions interact with patients’ affective characteristics to influence how patients respond to physicians. Based on Affect Valuation Theory (AVT), we argue that people more positively evaluate and prefer physicians who express the affective states that people value and ideally want to feel.
AVT (Tsai, 2007) posits that people's “ideal affect” (i.e., how people ideally want to feel typically) is distinct from their “actual affect” (i.e., how they actually feel typically). Whereas temperamental traits (e.g., extraversion) are more related to actual than ideal affect, sociocultural values (e.g., wanting to influence others) are more related to ideal than actual affect. Although both are important to emotional life, they serve different functions: actual affect represents how someone is feeling (“I feel good”); ideal affect provides a way of interpreting that feeling (“Does this feel right?”). While a significant literature demonstrates that actual affect plays an instrumental role in health-related decision-making (for reviews see Peters, Lipkus, & Diefenbach, 2006; Power, Swartzman, & Robinson, 2011), the role of ideal affect is largely unexplored, despite evidence that people base decisions on how they want to feel (Löckenhoff & Carstensen, 2007; Mikels et al., 2010; see Tsai, Chim, & Sims, in press, for review).
While most people want to feel positive, people vary in the types of positive states they want to feel, with some valuing high arousal positive [HAP] states more, and others valuing low arousal positive [LAP] states more (Tsai, Knutson, & Fung, 2006; Tsai, Louie, Chen, & Uchida, 2007; Tsai, Miao, & Seppala, 2007; Tsai, Miao, Seppala, Fung, & Yeung, 2007). Moreover, these individual differences in ideal affect influence people's preferences. For example, the more people value HAP states, the more they prefer exciting (vs. calming) consumer products, and the more people value LAP states, the more they prefer calming (vs. exciting) products (e.g., music CDs, tea; Mogilner, Aaker, & Kamvar, 2012; Tsai, 2007). While these findings may not be surprising, given the clear role of hedonics in these types of decisions, here we propose that people also base serious choices like which physician to see on how they want to feel (“ideal affect match hypothesis”). In these cases, it may be even more important that people choose a physician who feels “right.”
We predict that when people evaluate a physician, they base that evaluation on how much they trust that physician in general and perhaps more specifically, how much they trust that physician to help them feel how they want to feel. Consequently, people are more likely to select a physician whose affective expressions match their ideal affect. For instance, people who value HAP more should evaluate physicians based on how much HAP they express and promote, and therefore, trust and ultimately choose the physician who expresses and promotes HAP states the most.
Our predictions are consistent with previous research indicating that people trust physicians whose values are more aligned with their own (Street, O’Malley, Cooper, & Haidet, 2008), are more satisfied with physicians who interact with them in a manner consistent with their information preferences (e.g., Cousin, Schmid Mast, Roter, & Hall, 2012; Krupat, Yeager, & Putnam, 2000), and are more motivated by health messages framed in line with their goals (Higgins, 2005; Mann, Sherman, & Updegraff, 2004; Rothman & Salovey, 1997; Shen & Dillard, 2007). None of these studies, however, have examined affective values or goals. Unlike other values (e.g., religious, shared decision making), people may be less aware that their affective values influence their health decisions. Instead, options that match patients’ ideal affect may be perceived as “better” or “feel right,” even when they are in all other ways comparable.
An alternative hypothesis is that choice depends on a match between physicians’ affective expressions and people's actual affect (“actual affect match hypothesis”). People may prefer physicians who express states that are consistent with how they actually feel because people may feel more similar to these physicians.
The Present Study
To test our hypotheses, we presented participants with a hypothetical scenario and asked them to rate a HAP-focused, LAP-focused, and Neutral primary care provider. We matched physicians’ education and training, as is often the case in managed health care plans. We presented different positively-framed (vs. neutral) options because the scenario focused on preventive care rather than treatment, and because few studies have examined how people's positive affective characteristics shape health decisions. We used hypothetical scenarios because they are commonly used to assess medical preferences; they allow us to standardize information presented; and they mimic many medical decisions in everyday life (e.g., choosing a physician based on their online directory profile).
We hypothesized that: (1) ideal HAP would predict higher likelihood of choosing the HAP physician, whereas ideal LAP would predict higher likelihood of choosing the LAP physician, and (2) the effect of ideal affect on physician choice would be mediated by perceived trustworthiness. We also tested the alternative hypothesis that actual HAP and actual LAP would predict physician preference.
Method
Participants
For course credit, 185 undergraduate students (65% Female, 35% Male; 46.8% White, 29.4% Asian/Pacific Islander, 2.1% Black, 9.4% Hispanic, 1.6% Native American, 8.1% Multiracial) participated in a larger online survey that included measures of actual affect, ideal affect, and physician preference.
Instruments
Physician Scenario
Using a hypothetical scenario, participants were asked to imagine their current physician was no longer available, and they needed to choose a new primary care physician (see Appendix). Participants read descriptions of three physicians, modeled after real descriptions on a large health maintenance organization's website. Physicians were similar in age, education, and record of service, but differed in their views of patient care: the HAP physician focused on increasing patients’ overall vitality; the LAP physician focused on promoting a relaxed life-style; the Neutral physician focused on administering medical care. For each physician, participants indicated how much they agreed with “I would choose this physician as my health care provider,” “I would trust this physician,” “This physician is positive,” “This physician is stimulating,” using a seven-point scale from 1 (strongly disagree) to 7 (strongly agree). Choice and trust items were significantly correlated (HAP r=0.70, LAP r=0.63, Neutral r=0.75). As intended, repeated measures analyses revealed that the Neutral physician was rated less positive (M=5.32, SE=0.09) than the HAP (M=5.70, SE=0.08) and LAP (M=5.70, SE=0.07) physicians, F(1, 184) = 15.49, p<0.001; and the HAP physician was rated as more stimulating (M=5.65, SE=0.09) than the LAP (M=4.69, SE=0.10) and Neutral (M=4.82, SE=0.10) physicians, F(1, 184) = 54.94, p<0.001.
Ideal and Actual Affect
We administered the Affect Valuation Index (AVI; Tsai et al., 2006) to assess trait ideal and actual affect. The HAP aggregate consisted of excited, enthusiastic, elated, and euphoric. The LAP aggregate consisted of calm, peaceful, relaxed, and serene. Internal consistencies of aggregates were high (ideal HAP α=0.83, actual HAP α=0.82, ideal LAP α=0.86, actual LAP α=0.86).
Procedure
Participants completed the AVI and physician scenario, which were separated by several questionnaires not relevant to this study. We counterbalanced the presentation order of ideal and actual affect as well as the HAP, LAP, and Neutral physicians.
Results
To assess whether ideal affect predicted physician choice, we regressed participants’ physician choice rating onto ideal HAP, ideal LAP, actual HAP, and actual LAP. We included ratings of the other two physicians as covariates in each model. We removed 3 outliers for ratings of actual HAP (z=3.09) and 2 outliers for ratings of the Neutral (z=-3.47) and HAP (z=-3.19) physicians.1 Table 1 shows means and regression results. Correlations between all variables in model ranged from .01-.37 (available upon request).
Table 1.
Summary of means and linear regression results for ideal and actual affect predicting preference for HAP, LAP, and Neutral physicians.
| HAP Physician M=5.28, SD=1.31 | LAP Physician M=4.76, SD=1.40 | Neutral Physician M=5.37, SD=1.21 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| b (se) | β | t | b (se) | β | t | b (se) | β | t | |
| Ideal HAP M=3.74, SD=.81 | 0.37 (0.14) | .23 | 2.68** | −0.03 (0.15) | −.02 | −0.22 | 0.03 (0.13) | .02 | 0.21 |
| Ideal LAP M=4.07, SD=.75 | −0.14 (0.15) | −.08 | −0.92 | 0.33 (0.16) | .17 | 2.02* | 0.06 (0.14) | .04 | 0.40 |
| Actual HAP M=2.71, SD=.67 | 0.00 (0.17) | .00 | 0.01 | 0.08 (0.18) | .04 | 0.41 | 0.11 (0.16) | .06 | 0.71 |
| Actual LAP M=2.82, SD=.73 | 0.01 (0.15) | .01 | 0.09 | −0.13 (0.16) | −.07 | −0.83 | −0.02 (0.014) | −.01 | −0.14 |
| Intercept | 3.47 (0.85) | 4.08** | 2.68 (0.94) | 2.86** | 4.42 (0.78) | 5.65** | |||
Note. High Arousal Positive; LAP = Low Arousal Positive; Ratings of the other two physicians are included as covariates in each model.
p < 0.01
p < 0.05.
Consistent with Hypothesis 1 and the “ideal affect match hypothesis,” ideal HAP significantly predicted HAP physician choice, whereas ideal LAP did not, and ideal LAP significantly predicted LAP physician choice, whereas ideal HAP did not. Further, neither actual nor ideal HAP or LAP predicted Neutral physician choice, suggesting that ideal affect is more relevant for evaluating affectively-framed options. Contrary to the “actual affect match hypothesis,” neither actual HAP nor actual LAP predicted HAP or LAP physician choice, suggesting that our findings are specific to ideal affect and not due to demand to endorse HAP or LAP. Finally, ideal affect did not predict aversion to physicians who did not match people's ideal affect (i.e., ideal LAP was not negatively associated with HAP physician choice and vice-versa), indicating that ideal affect is associated only with ideal affect-relevant preferences.
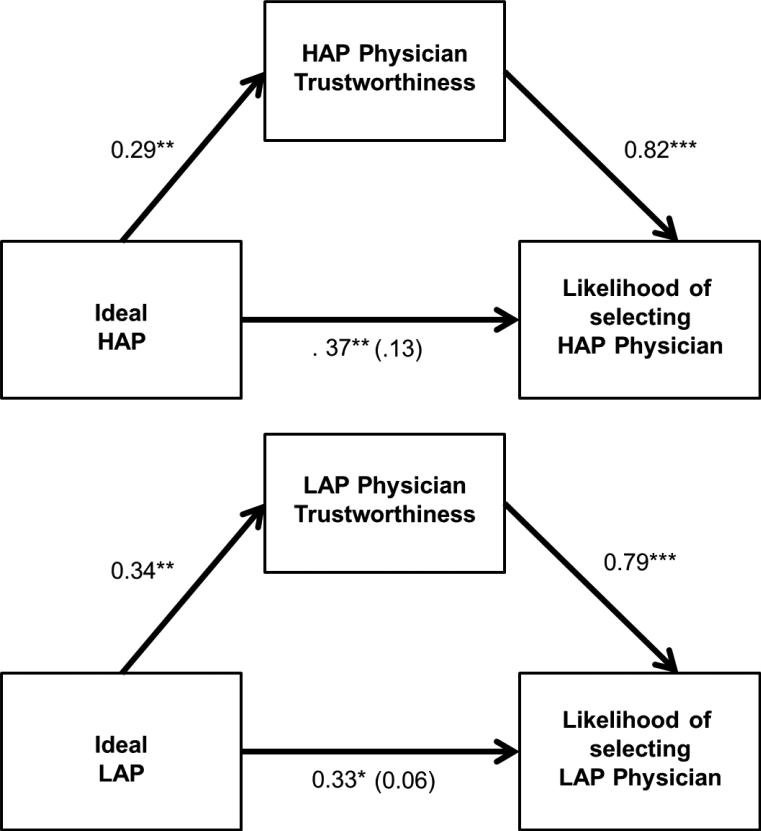
To test Hypothesis 2, we added perceived physician trustworthiness to each model to assess mediation of the relationship between ideal affect and physician choice (see Figure 1). When estimating the effect of ideal HAP on physician trustworthiness (path a), we found the more people valued HAP states, the more trustworthy they perceived the HAP physician, Ba=0.29, SE=0.11, t=2.71, p<0.01. Next, we regressed HAP physician choice onto physician trustworthiness and ideal HAP (path b). Above and beyond ideal HAP, HAP physician trustworthiness significantly predicted HAP physician preference, Bb=0.82, SE=0.07, t=11.24, p<0.001. As described above, the more people valued HAP, the more they preferred the HAP physician (path c). When including physician trustworthiness in this model (path c’), the effect of ideal HAP was no longer significant, Bc'=0.13, SE=0.11, t=1.18, p=0.24, but the indirect effect of ideal HAP on physician choice through physician trustworthiness was significant, indirect effect=0.24, SE=0.09, Sobel's z=2.63, p<0.01.
Figure 1.
Effect of ideal affect on likelihood of choosing physician mediated by perceived trustworthiness. Top: Ideal HAP indirect effect through perceived trustworthiness = 0.24 (SE = 0.09), p < 0.01; R2 = 0.47, F (7, 172) = 21.44, p < 0.001; Bottom: Ideal LAP indirect effect through perceived trustworthiness = 0.27 (SE = 0.11), p = 0.01; R2 = 0.44, F (7, 172) = 19.01, p < 0.001 . All analyses controlled for actual affect and likelihood of choosing other physicians; **p < 0.01, p < 0.05. HAP = High arousal positive states; LAP = Low arousal positive states.
When estimating the effect of ideal LAP on perceived trustworthiness of the LAP physician (path a), we found the more people valued LAP states, the more trustworthy they perceived the LAP physician, Ba=0.34, SE=0.13, t=2.60, p=0.01. When regressing LAP physician choice onto LAP physician trustworthiness and ideal LAP (path b), LAP physician trustworthiness significantly predicted LAP physician preference, Bb=0.79, SE=0.07, t=10.80, p<0.001. When including LAP physician trustworthiness in the model (path c’), the effect of ideal LAP was no longer significant, Bc'=0.06, SE=0.13, t=0.46, p=0.64, but the indirect effect of ideal LAP through physician trustworthiness was significant, indirect effect=0.27, SE=0.11, Sobel's z=2.52, p=0.01. Thus, consistent with Hypothesis 2, the relationship between ideal affect and physician choice was mediated by perceived trustworthiness.
Discussion
How do people choose physicians? Our findings suggest that people choose physicians based on whether the affective states a physician promotes matches how they ideally want to feel. The more people valued HAP, the more they trusted and preferred the HAP-focused physician,2 and the more people valued LAP, the more they trusted and preferred the LAP-focused physician. Ideal affect did not predict neutral physician preference, suggesting that ideal affect matters more for affective vs. non-affective options.
Contrary to the “actual affect match hypothesis,” how often people actually felt HAP or LAP states did not predict physician preference, suggesting that at least in our scenarios, people's ideal affect mattered more than their actual affect. These findings suggest that physician choice depends more on a match to patients’ goals than a general matching or similarity to the physician. Indeed, post-hoc analyses revealed that the association between ideal affect and physician choice was not mediated by perceived similarity. One potential criticism may be that ideal affect was more relevant because participants viewed the physicians as promoting but not actually experiencing HAP and LAP states. However, participants’ ratings indicated they viewed the HAP-focused physician as more stimulating than (but equally positive as) the LAP-focused physician. Further, in earlier work, we find similar effects even when physicians are presented with HAP and LAP smiles and as engaging in HAP and LAP hobbies (see online supplemental materials).
The lack of association between actual affect and physician preference may have been due to the nature of the decision. Because the scenarios were hypothetical, participants may have placed less emphasis on how they actually feel and focused more on how they want to feel. It would be important to examine how our findings translate to patient preferences in actual clinical settings, especially when people are making critical health decisions in the context of illness. Because we were interested in how people's affective tendencies influenced their physician preferences, we did not assess people's state actual or ideal affect. Future studies are needed to assess whether state ideal affect also predicts physician preference more than state actual affect.
Future work should also examine how ideal affect shapes other medical choices, such as medications (e.g., stimulant vs. sedative) and how ideal affect interacts with other factors that influence medical choices, such as the objective qualities of the options (e.g., cost, accessibility). Given cultural variation in ideal affect (e.g., Ruby et al., 2012; Tsai et al., 2006; Tsai, 2007, Tsai et al., 2007abc), future work should also examine whether ideal affect may explain ethnic variation in patients’ preferences for physicians. In this study, participants were the least likely to select the LAP physician. It would be important to examine whether this finding is specific to our American college student sample. Finally, it is unclear whether the observed associations are specific to physician choice. Indeed, current work in our lab suggests that similar processes may occur for choosing leaders and friends (Chim, Tsai, & Ang, 2013).
Implications
These results highlight the importance of including ideal affect in models of decision-making, person perception, and patient preferences. Our work suggests that knowing how someone ideally wants to feel may be as important as knowing how someone actually feels when predicting their decisions. How people are perceived (e.g., how trustworthy they are) seems to depend not only on their affective expressions, but also whether the perceiver values those states. And how physicians are evaluated depends on both the type of affect expressed and promoted by the physician and the type of affect valued by the patient. Consequently, physicians who promote the states that their patients value may be ultimately more effective at treating them.
Supplementary Material
Acknowledgments
Research reported in this publication was supported by the National Institute on Aging P03AG024957 awarded to the first and second authors, R03AG023302 awarded to the second author, and National Institute of Mental Health R01MH068879 awarded to the second author. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the Department of Veterans Affairs, or other affiliated organizations. The authors thank the Stanford Culture and Emotion Lab, Culture Collaboratory and Life Span Lab for their helpful suggestions; Alexia Charles, Michael To, and Henry Young for their research assistance.
Appendix
Choosing A Physician Scenario
Imagine that your current physician is no longer available, and you now have to choose a physician from the two individuals described below to provide your regular health care. Both have similar educational backgrounds, are accredited by the American Medical Association, and have been recognized by their medical center as providing outstanding care. Please read their descriptions carefully and respond to the questions that follow.
Dr. H
Specialty: Internal Medicine Facility: Bay Area Medical Center
Education: Doctor of Medicine, University of California San Francisco, 1991
Award for Outstanding Healthcare Provider, Bay Area Medical Center
Views on Patient Care: “My primary objective is to enhance my patients’ well-being by increasing their activity levels and overall vitality so my patients can lead healthy, dynamic lifestyles.”
Outside interests: “I volunteer in a youth home where we help adolescents discover a passion for educational goals.”
Dr. L
Specialty: Internal Medicine Facility: Bay Area Medical Center
Education: Doctor of Medicine, University of California San Francisco, 1991
Distinguished Service in Health Award, Bay Area Medical Center
Views on Patient Care: “My goal as a physician is to ensure that my patients have peace of mind when it comes to their health by promoting a stress-free (calm and relaxed) lifestyle.” Outside interests: “I spend time at a facility where I teach young people to feel more at ease with school.”
Footnotes
We identified outliers based on ratings of the independent and dependent variables in the models with z-scores exceeding +/- 3 as well as regression outliers with extremely large Cook's D values (i.e., > 0.4). Results are similar when including outliers except that the effect of ideal LAP is marginal, p=0.09
We replicated the association between ideal HAP and HAP physician preference in two additional studies using different physician stimuli (e.g., photographs). See online supplementary materials.
Contributor Information
Tamara Sims, Department of Psychology, Stanford University.
Jeanne L. Tsai, Department of Psychology, Stanford University
Birgit Koopmann-Holm, Department of Psychology, Stanford University.
Ewart A.C. Thomas, Department of Psychology, Stanford University
Mary K. Goldstein, Stanford Health Policy, Stanford University and VA Palo Alto Health Care System.
References
- Ambady N, Koo J, Rosenthal R, Winograd CH. Physical therapists' nonverbal communication predicts geriatric patients' health outcomes. Psychology and aging. 2002;17(3):443. doi: 10.1037/0882-7974.17.3.443. [DOI] [PubMed] [Google Scholar]
- Beck RS, Daughtridge R, Sloane PD. Physician-patient communication in the primary care office: a systematic review. The Journal of the American Board of Family Practice. 2002;15(1):25–38. [PubMed] [Google Scholar]
- Blasi ZD, Harkness E, Ernst E, Georgiou A, Kleijnen J. Influence of context effects on health outcomes: a systematic review. The Lancet. 2001;357(9258):757–762. doi: 10.1016/s0140-6736(00)04169-6. [DOI] [PubMed] [Google Scholar]
- Chim L, Tsai JL, Ang J, Fung HH. Cultural differences in perceptions of leadership: The role of ideal affect. 2013. Manuscript in preparation.
- Cousin G, Schmid Mast M, Roter DL, Hall JA. Concordance between physician communication style and patient attitudes predicts patient satisfaction. Patient Education and Counseling. 2012;87(2):193–197. doi: 10.1016/j.pec.2011.08.004. doi: 10.1016/j.pec.2011.08.004. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR. A social psychological analysis of physician patient rapport: Toward a science of the art of medicine. Journal of Social Issues. 1979;35(1):12–33. [Google Scholar]
- Griffith CH, Wilson JF, Langer S, Haist SA. House staff nonverbal communication skills and standardized patient satisfaction. Journal of General Internal Medicine. 2003;18(3):170–174. doi: 10.1046/j.1525-1497.2003.10506.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall JA, Roter DL, Rand CS. Communication of affect between patient and physician. Journal of Health and Social Behavior. 1981;22(1):18–30. [PubMed] [Google Scholar]
- Higgins ET. Value from regulatory fit. Current Directions in Psychological Science. 2005;14(4):209–213. [Google Scholar]
- Krupat E, Yeager CM, Putnam S. Patient role orientations, doctor-patient fit, and visit satisfaction. Psychology and Health. 2000;15(5):707–719. [Google Scholar]
- Levine CS, Ambady N. Nonverbal behavior's role in racial gaps in healthcare: Implications and solutions. . Medical Education. doi: 10.1111/medu.12216. in press. [DOI] [PubMed] [Google Scholar]
- Löckenhoff CE, Carstensen LL. Aging, emotion, and health-related decision strategies: motivational manipulations can reduce age differences. Psychology and aging. 2007;22(1):134. doi: 10.1037/0882-7974.22.1.134. [DOI] [PubMed] [Google Scholar]
- Mann T, Sherman D, Updegraff J. Dispositional motivations and message framing: a test of the congruency hypothesis in college students. Health Psychology. 2004;23(3):330. doi: 10.1037/0278-6133.23.3.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercado F, Mercado M, Myers N, Hewit M, Haller NA. Patient Preferences in Choosing a Primary Care Physician. Journal of Primary Care & Community Health. 2012;3(2):125–131. doi: 10.1177/2150131911421802. [DOI] [PubMed] [Google Scholar]
- Mikels JA, Löckenhoff CE, Maglio SJ, Carstensen LL, Goldstein MK, Garber A. Following your heart or your head: Focusing on emotions versus information differentially influences the decisions of younger and older adults. Journal of Experimental Psychology: Applied;Journal of Experimental Psychology: Applied. 2010;16(1):87–95. doi: 10.1037/a0018500. doi: 10.1037/a0018500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogilner C, Aaker J, Kamvar SD. How Happiness Affects Choice. Journal of Consumer Research. 2012;39(2):429–443. [Google Scholar]
- Peters E, Lipkus I, Diefenbach MA. The functions of affect in health communications and in the construction of health preferences. Journal of Communication. 2006;56(s1):S140–S162. [Google Scholar]
- Power TE, Swartzman LC, Robinson JW. Cognitive-emotional decision making (CEDM): A framework of patient medical decision making. Patient Education and Counseling. 2011;83(2):163–169. doi: 10.1016/j.pec.2010.05.021. [DOI] [PubMed] [Google Scholar]
- Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behavior: the role of message framing. Psychological bulletin. 1997;121(1):3. doi: 10.1037/0033-2909.121.1.3. [DOI] [PubMed] [Google Scholar]
- Ruby MB, Falk CF, Heine SJ, Villa C, Silberstein O. Not All Collectivisms Are Equal: Opposing Preferences for Ideal Affect Between East Asians and Mexicans. 2012. [DOI] [PubMed]
- Shen L, Dillard JP. The influence of behavioral inhibition/approach systems and message framing on the processing of persuasive health messages. Communication Research. 2007;34(4):433–467. [Google Scholar]
- Street RL, O'Malley KJ, Cooper LA, Haidet P. Understanding Concordance in Patient-Physician Relationships: Personal and Ethnic Dimensions of Shared Identity. The Annals of Family Medicine. 2008;6(3):198–205. doi: 10.1370/afm.821. doi: 10.1370/afm.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai JL. Ideal Affect: Cultural Causes and Behavioral Consequences. Perspectives on Psychological Science. 2007;2(3):242–259. doi: 10.1111/j.1745-6916.2007.00043.x. doi: 10.1111/j.1745-6916.2007.00043.x. [DOI] [PubMed] [Google Scholar]
- Tsai JL, Chim L, Sims TL. Understanding Affect and Consumer Behavior Across Cultures: The Role of Ideal Affect. In: Lee AY, Ng S, editors. Handbook of Culture and Consumer Behavior. in press. [Google Scholar]
- Tsai JL, Knutson B, Fung HH. Cultural variation in affect valuation. Journal of Personality and Social Psychology. 2006;90(2):288–307. doi: 10.1037/0022-3514.90.2.288. doi: 10.1037/0022-3514.90.2.288. [DOI] [PubMed] [Google Scholar]
- Tsai JL, Louie JY, Chen EE, Uchida Y. Learning What Feelings to Desire: Socialization of Ideal Affect Through Children's Storybooks. Personality and Social Psychology Bulletin. 2007;33(1):17–30. doi: 10.1177/0146167206292749. doi: 10.1177/0146167206292749. [DOI] [PubMed] [Google Scholar]
- Tsai JL, Miao FF, Seppala E. Good Feelings in Christianity and Buddhism: Religious Differences in Ideal Affect. Personality and Social Psychology Bulletin. 2007;33(3):409–421. doi: 10.1177/0146167206296107. doi: 10.1177/0146167206296107. [DOI] [PubMed] [Google Scholar]
- Tsai JL, Miao FF, Seppala E, Fung HH, Yeung DY. Influence and adjustment goals: sources of cultural differences in ideal affect. Journal of Personality and Social Psychology. 2007;92(6):1102. doi: 10.1037/0022-3514.92.6.1102. [DOI] [PubMed] [Google Scholar]
- Wroe A. Intentional and Unintentional Nonadherence: A Study of Decision Making. Journal of Behavioral Medicine. 2002;25(4):355–372. doi: 10.1023/a:1015866415552. doi: 10.1023/a:1015866415552. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.