Abstract
Background
One major goal of the Patient-Centered Medical Home (PCMH) is to improve continuity of care between patients and providers and reduce the utilization of non-primary care services like the emergency department (ED).
Objective
To characterize continuity under the Veterans Health Administration’s PCMH model – the Patient Aligned Care Team (PACT), at one large Veterans Affair’s (VA’s) primary care clinic, determine the characteristics associated with high levels of continuity, and assess the association between continuity and ED visits.
Design
Retrospective, observational cohort study of patients at the West Haven VA (WHVA) Primary Care Clinic from March 2011 to February 2012.
Patients
The 13,495 patients with established care at the Clinic, having at least one visit, one year before March 2011.
Main Measures
Our exposure variable was continuity of care –a patient seeing their assigned primary care provider (PCP) at each clinic visit. The outcome of interest was having an ED visit.
Results
The patients encompassed 42,969 total clinic visits, and 3185 (24%) of them had 15,458 ED visits. In a multivariable logistic regression analysis, patients with continuity of care – at least one visit with their assigned PCP – had lower ED utilization compared to individuals without continuity (adjusted odds ratio [AOR] 0.54; 95% CI: 0.41, 0.71), controlling for frequency of primary care visits, comorbidities, insurance, distance from the ED, and having a trainee PCP assigned. Likewise, the adjusted rate of ED visits was 544/1000 person-year (PY) for patients with continuity vs. 784/1000 PY for patients without continuity (p = 0.001). Compared to patients with low continuity (<33% of visits), individuals with medium (33–50%) and high (>50%) continuity were less likely to utilize the ED.
Conclusions
Strong continuity of care is associated with decreased ED utilization in a PCMH model and improving continuity may help reduce the utilization of non-primary care services.
Introduction
The U.S. healthcare system has become disjointed, a challenge for achieving patient-centered care [1]–[3]. The patient-centered medical home (PCMH) model was conceived almost a half-century ago to facilitate greater integration and continuity, but did not gain prominence until a 2007 joint collaborative established a series of principles now used to define the medical home [4]–[6]. After adopting these principles and successfully piloting PCMH care at one Veterans Affairs (VA) primary care clinic, the Veteran’s Health Administration began transitioning all of its primary care clinics towards a PCMH structure under the title, the Patient Aligned Care Team (PACT), in 2008 [7]–[12].
One hallmark goal of PACT involves improved continuity of care between a patient and their primary care provider (PCP), partly because poor continuity is believed to contribute to the inappropriate use of healthcare services like emergency departments (ED) [13]–[17]. As a result, the VA assigned care teams to each patient within PACT and implemented efforts to increase patient access to providers. VA clinics, often serving as training sites for health professionals, face additional challenges towards achieving strong continuity because trainees rotate through inconsistently, making appointment scheduling difficult.
Many observational and pilot studies indicate PCMH models can decrease care fragmentation, reduce utilization of healthcare resources and costs, and decrease ED visits [9]–[12], [18]–[22]. These observations of PCMH implementation, however, do not clearly characterize the degrees of continuity achieved nor do they analyze associations between continuity and ED utilization. Hypothesizing that patients with high continuity of care levels would visit the ED less, we sought to model patient and clinic level factors associated with continuity and assess the association between high levels of continuity and ED visits in the year after the 2011 implementation of PACT at Connecticut’s West Haven VA (WHVA).
Methods
Ethical Review
Institutional review boards at the VA Connecticut Healthcare System (VACHS) and Yale University School of Medicine (New Haven, CT) approved this study. No informed consent was taken. Records and information were anonymous and de-identified prior to analysis.
Cohort
We performed a retrospective analysis of patients who visited the WHVA primary care clinic one year after restructuring under PACT: March 1, 2011 to February 29, 2012. To minimize confounding by different utilization patterns of new WHVA patients, we extracted electronic medical records of patients with established WHVA care, defined as at least one primary care visit one year before restructuring (March 1, 2010 to February 28, 2011). Patient data was extracted from the Veterans Health Information Systems and Technology Architecture and processed by the 2010 Microsoft Structured Query Language Server using Cache Structured Query Language and Open Database Connectivity connections.
Setting
WHVA primary care services consist of routine primary care clinics and a separate women’s clinic allocated for female Veteran care. Though VACHS consists of the WHVA, the Newington campus, and six community-based outpatient clinics (CBOCs) throughout the state, this analysis is limited to the WHVA’s Primary Care Clinic. The exclusion of the Newington campus and CBOCs was deliberate because of the physical distance and clinic level factors that might influence how individuals utilized the WHVA ED, the only VA ED in the VACHS network.
PACT Team Description
Each patient is assigned to a PACT team, which consists of a) a licensed PCP – physician (MD or DO), nurse practitioner (NP), or physician assistant (PA); b) a registered nurse (RN); and c) a medical assistant. Additional on-site staff members include pharmacists, dieticians, social workers, care coordinators, health psychologists, and specialty medical or surgical consultants.
During the study period, over 40 internal medicine resident trainees and two NP fellow trainees were supervised by PCPs and assigned to PACT teams as part of their outpatient training requirements. Moreover, beginning June 2011 and beyond the study period end date, the WHVA had two of its PACT teams participating in the Center of Excellence in Primary Care Education, a training model designed to prepare trainees from different health professions in providing coordinated, interprofessional, outpatient care [23]. The WHVA had 13 clinical, full-time equivalent providers during the study period.
Continuity
We defined continuity as a patient seeing their assigned PCP or trainee (e.g. resident physician or NP).
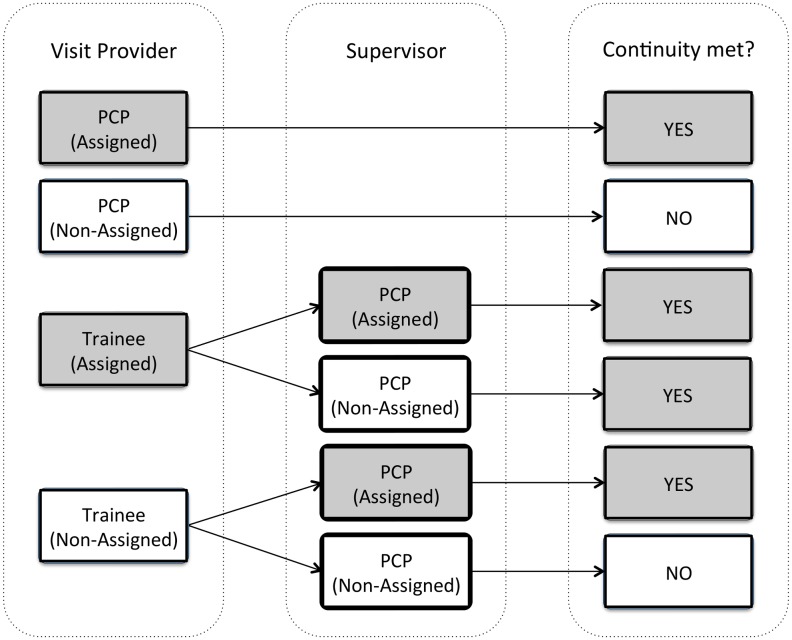
Two assignment scenarios exist for patients – Assignment A: a patient is assigned to a PCP without a trainee also managing their outpatient care or Assignment B: a patient is assigned to a trainee and PCP who supervises that trainee. No patient is ever assigned to a trainee provider without also being assigned to a PCP, since trainees require supervision by a licensed PCP. Patients who are evaluated by trainees require supervision by a PCP during the same visit. Therefore, two visit scenarios exist for patients – a PCP without the additional care of a trainee evaluates the patients or a trainee who is supervised by a PCP evaluates the patient. In the latter scenario, we defined continuity as the patient seeing either their assigned trainee or a separate trainee supervised by the patient’s assigned PCP. When evaluating continuity, we accounted for these various combinations of providers who may see a patient during a given visit ( Figure 1 ); and through the electronic medical record we could account for any patient-PCP or patient-trainee reassignments that might have occurred during the study period.
Figure 1. Potential Patient Visit Interactions with a Provider and/or Trainee and the Relationship with Continuity.
PCP: primary care provider. Grey boxes indicate visits with continuity of care and white boxes indicate visits without continuity.
After determining whether each visit had continuity or not, we calculated a continuity index for each patient based on the Usual Provider Continuity (UPC) definition, which calculates the percentage of the number of visits to the assigned provider divided by the total number of visits [24], [25]. Levels of continuity were created based on the index into low (<33% of visits/year had continuity), medium (33–50% of visits/year), and high (>50% of visits/year).
ED Visits
The main outcome of interest was ED visits during the study period by each study patient. We controlled for distance by using the zip code difference between the patient’s address and the WHVA as a proxy. We also determined visit times and day of the week (i.e. weekend versus weekday).
Covariates and Potential Confounders
We examined baseline demographics including age, sex, and race, categorized by the patient as white non-Hispanic, black, Hispanic, or other race. Other covariates of interest were percent service connection – degree of health compensation benefit paid for a designated condition related to injury or illness incurred or aggravated by active military service, period of military service, and presence of outside health insurance. Comorbidity data based on ICD-9 codes were collected, including mental illness (having major depression, bipolar disorder, post-traumatic stress disorder, or schizophrenia), substance abuse (drug abuse or alcohol abuse and dependence), myocardial infarction and coronary artery disease, congestive heart failure, diabetes mellitus, hypertension, peripheral vascular disease, pulmonary diseases, stroke, hyperlipidemia, flu and obesity [15], [16]. Linking particular ICD-9 codes with comorbidity diagnoses have been described previously [26], [27]. We derived smoking prevalence from Veterans Affairs Health Factors database, a computerized clinical provider reminder and reporting system that periodically reminds clinicians to perform assessments of tobacco and alcohol use, then records the results of these structured interviews. Individuals who sparingly visited the WHVA were believed to use the WHVA ED services differently than those who visit routinely; therefore, we tracked the frequency of primary care visits, defining “low” primary care users as less than three primary care visits per year, while “high” primary care users had at least three [15].
Statistical Analysis
We compared demographic characteristics using the student t-test for normally distributed variables, Wilcoxon-Mann Whitney for non-parametric variables, and the chi-square for categorical variables. Bivariate analyses determined the impact demographic data may have on the association between continuity and ED use. For individuals with complete data, multivariable logistic regression models were constructed to assess the relationship between continuity and ED use. In addition, rates of ED visits/1000 person-year (PY) were calculated, adjusted for similar variables as in the multivariable logistic regression. To assess the impact levels of continuity have on ED utilization, models were restricted to individuals who had at least one continuity visit. All models were run unadjusted and then adjusted for the following variables: age, gender, comorbidities, primary care user level, outside insurance, percent service connection, service period, zip-code differences, and having a trainee provider assigned to a patient versus not. In the sensitivity analysis, we calculated stratum-specific odds ratios for the number of primary care visits during the study period instead of categorizing this variable into “low” and “high” primary care users. A p-value of <0.05 was used to determine statistical significance. Statistical analyses were performed using SAS version 9.2 (SAS Institute Inc., North Carolina).
Results
Our cohort included 13,495 individuals who totaled 42,969 unique primary care clinic visits. Among those, 3185 (24%) had an ED visit; accounting for 15,458 ED visits.
The cohort was primarily composed of white, male Veterans with a median age of 69 years ( Table 1 ). The median number of primary care visits was 2 (IQR 1–4). Veterans who had no continuity with their assigned PCPs totaled 364 (3%) individuals. The mean UPC index was 87% (median 1.0; IQR 0.89–1.0). The percentage of low primary care users (<3 visits) was 56% while the percentage of high primary care users (≥3 visits) was 44%. Nineteen percent of patients had a trainee assigned to their care.
Table 1. Patient Demographics by Continuity and Stratification by Continuity of Care Levels.
| Overall (N = 13,495) | Continuity | Among Patients with ≥1 Continuity Visit | ||||||
| Variables | % | No (n = 364) | Yes (n = 13131) | p-value | <33% (n = 307) | 33%–50% (n = 1277) | >50% (n = 11547) | p-value |
| Age, IQR | 69 (61, 80) | 60 (44, 77) | 69 (61, 80) | <0.001 | 64 (51, 74) | 65 (55, 77) | 70 (62, 81) | <0.001 |
| Sex | <0.001 | <0.001 | ||||||
| Female | 5 | 20 | 4 | 10 | 10 | 4 | ||
| Male | 95 | 80 | 96 | 90 | 90 | 96 | ||
| Race a | 0.03 | 0.51 | ||||||
| White | 80 | 71 | 80 | 76 | 79 | 80 | ||
| Black | 15 | 26 | 15 | 19 | 15 | 15 | ||
| Hispanics | 3 | 3 | 3 | 2 | 4 | 3 | ||
| Other | 2 | 0 | 2 | 3 | 2 | 2 | ||
| Smoker | 19 | 26 | 18 | <0.001 | 21 | 23 | 18 | <0.001 |
| Substance use disorder | 8 | 9 | 8 | 0.21 | 11 | 10 | 7 | <0.001 |
| Severe mental iIlness b | 10 | 14 | 10 | 0.01 | 19 | 15 | 9 | <0.001 |
| Service connection (%) | ||||||||
| 0–25 | 11 | 11 | 11 | 1.00 | 11 | 10 | 11 | 0.65 |
| 26–50 | 7 | 9 | 6 | 0.07 | 11 | 9 | 6 | <0.001 |
| 51–75 | 5 | 6 | 5 | 0.27 | 8 | 7 | 4 | <0.001 |
| 76–100 | 7 | 12 | 7 | 0.003 | 15 | 11 | 7 | <0.001 |
| Period of service | <0.001 | <0.001 | ||||||
| Otherc | 2 | 3 | 2 | 3 | 2 | 2 | ||
| Korean | 17 | 9 | 18 | 13 | 15 | 18 | ||
| Persian Gulf | 9 | 27 | 9 | 18 | 13 | 8 | ||
| Post-Korean | 10 | 6 | 10 | 6 | 8 | 10 | ||
| Post-Vietnam | 8 | 15 | 8 | 14 | 14 | 7 | ||
| Vietnam Era | 36 | 24 | 36 | 37 | 37 | 36 | ||
| World War II | 17 | 16 | 17 | 9 | 12 | 18 | ||
| Outside insurance (yes) | 69 | 52 | 70 | <0.001 | 65 | 67 | 70 | 0.01 |
| Primary care user level | <0.001 | <0.001 | ||||||
| Low (<3 visits/year) | 56 | 71 | 55 | 0 | 16 | 61 | ||
| High (≥3 visits/year) | 44 | 29 | 45 | 100 | 84 | 39 | ||
| Comorbidities | ||||||||
| MI/Coronary artery disease | 23 | 13 | 23 | <0.001 | 20 | 21 | 23 | 0.20 |
| Congestive heart failure | 3 | 2 | 3 | 0.08 | 5 | 6 | 3 | <0.001 |
| Diabetes mellitus | 26 | 18 | 26 | <0.001 | 26 | 31 | 25 | <0.001 |
| Hypertension | 64 | 37 | 65 | <0.001 | 57 | 65 | 66 | 0.01 |
| Peripheral vascular disease | 5 | 6 | 5 | 0.78 | 6 | 6 | 5 | 0.26 |
| Pulmonary disorder/COPD | 11 | 9 | 11 | 0.27 | 15 | 16 | 10 | <0.001 |
| Stroke/TIA | 4 | 1 | 4 | <0.001 | 6 | 5 | 4 | 0.08 |
| Alcohol | 6 | 5 | 6 | 0.76 | 8 | 7 | 6 | 0.05 |
| Drug | 3 | 6 | 3 | <0.001 | 5 | 4 | 2 | <0.001 |
| Pneumonia | 0.01 | 0 | 0.01 | 1.00 | 0 | 0 | 0.01 | - |
| Schizophrenia | 1 | 3 | 1 | <0.001 | 2 | 1 | 1 | 0.03 |
| Bipolar disorder | 1 | 1 | 1 | 0.97 | 3 | 2 | 1 | <0.001 |
| Major Depression | 3 | 4 | 3 | 0.07 | 5 | 6 | 2 | <0.001 |
| PTSD | 6 | 6 | 6 | 0.55 | 12 | 8 | 5 | <0.001 |
| Hyperlipidemia | 57 | 30 | 58 | <0.001 | 50 | 54 | 58 | <0.002 |
| Influenza | 33 | 21 | 33 | <0.001 | 43 | 40 | 33 | <0.001 |
| Overweight/obesity | 14 | 10 | 15 | 0.03 | 22 | 21 | 14 | <0.001 |
| ED visits | 24 | 32 | 23 | <0.001 | 50 | 38 | 21 | <0.001 |
| No. of ED visits after hours on a weekday d | 22 | 27 | 23 | 0.34 | 23 | 23 | 23 | 0.99 |
| ED visit day d | 0.15 | 0.07 | ||||||
| Weekday | 78 | 83 | 78 | 73 | 81 | 78 | ||
| Weekend | 22 | 17 | 22 | 27 | 19 | 22 | ||
| No. ED visits d | 0.85 | 0.12 | ||||||
| 1 | 11 | 13 | 11 | 10 | 12 | 11 | ||
| 2 | 24 | 21 | 25 | 21 | 21 | 26 | ||
| 3 | 17 | 16 | 17 | 14 | 16 | 17 | ||
| 4 or more | 47 | 50 | 47 | 55 | 51 | 46 | ||
| Assigned provider(s) | <0.001 | <0.001 | ||||||
| PCP only | 81 | 74 | 82 | 90 | 88 | 81 | ||
| Trainee & PCP | 19 | 26 | 18 | 10 | 12 | 19 | ||
| Zip code distance from ED | 0.11 | <0.001 | ||||||
| ≤2 | 15 | 14 | 15 | 19 | 17 | 15 | ||
| 3–5 | 11 | 10 | 11 | 12 | 13 | 11 | ||
| 6–10 | 1 | 0.3 | 1 | 2 | 1 | 1 | ||
| 11–50 | 18 | 15 | 18 | 14 | 16 | 19 | ||
| >50 | 55 | 60 | 55 | 53 | 52 | 55 | ||
Abbreviations: IQR, interquartile range; MI, myocardial infarction; COPD, chronic obstructive pulmonary disease; TIA, transient ischemic attack; PTSD, post-traumatic stress disorder; ED, emergency department.
Sixty-nine percent were missing this variable.
Composite of major depression, bipolar, schizophrenia and PTSD.
Because of the small number of veterans in these groups, they were combined: active military personnel, CAV/NPS, ChampVA spouse and children, non-Veteran humanitarian groups, merchant marines, and Tricare.
Among ED visits that took place between Monday and Friday.
Individuals having at least one continuity visit were less likely to visit the ED compared to those lacking a single continuity visit (23% vs. 32%, p<0.001) ( Table 1 ). They were less likely to actively smoke, have higher service connection, have severe mental illness, and abuse drugs. They were more likely to be white, have outside insurance, visit the primary care clinic more than three times in the year, served in Korea or Vietnam, have a diagnosis of coronary artery disease or a myocardial infarction, diabetes, hypertension, stroke or transient ischemic attack, hyperlipidemia, or obesity. Patients assigned to trainees were less likely to have continuity of care.
Unadjusted Predictors of ED Utilization
Compared with individuals who did not use the ED ( Table 2 ), ED users were significantly (p<0.05 for all variables) younger, female, smoke, use substances, have a severe mental illness, have a high degree of service connection, more frequently visited the primary care clinic, and have the following comorbidities: congestive heart failure, a pulmonary disorder, stroke, flu, and obesity. In contrast, ED users were less likely to have outside insurance. In the unadjusted logistic regression model, having at least one primary care visit with continuity was associated with a 36% reduction in visits to the ED (odds ratio [OR] 0.64; 95% confidence interval [CI]: 0.51, 0.80). The unadjusted rate of ED visits for patients with continuity vs. none was 204/1000 PY (95% CI: 141, 294) vs. 266/1000 PY (95% CI: 222, 319) (p = 0.004).
Table 2. Patient Demographics by Emergency Department Visits.
| ED Visits | |||
| Variables | No, n = 10310 | Yes, n = 3185 | p-value |
| Age, IQR | 70 (62, 80) | 65 (56, 78) | <0.001 |
| Sex | <0.001 | ||
| Female | 4 | 7 | |
| Male | 96 | 93 | |
| Race a | <0.001 | ||
| White | 81 | 77 | |
| Black | 14 | 19 | |
| Hispanics | 3 | 3 | |
| Other | 2 | 2 | |
| Smoker (yes) | 16 | 25 | <0.001 |
| Substance use disorder (yes) | 6 | 14 | <0.001 |
| Severe mental illness b (yes) | 8 | 16 | <0.001 |
| Service connection (%) | |||
| 0–25 | 11 | 11 | 0.67 |
| 26–50 | 6 | 8 | <0.001 |
| 51–75 | 4 | 6 | <0.001 |
| 76–100 | 6 | 12 | <0.001 |
| Period of service | <0.001 | ||
| Otherc | 2 | 2 | |
| Korean | 19 | 13 | |
| Persian Gulf War | 9 | 11 | |
| Post-Korean War Period | 10 | 7 | |
| Post-Vietnam War Period | 7 | 13 | |
| Vietnam War | 35 | 39 | |
| World War II | 17 | 15 | |
| Outside insurance status (yes) | 72 | 61 | <0.001 |
| Primary care user level | <0.001 | ||
| Low (<3 visits/year) | 64 | 30 | |
| High (≥3 visits/year) | 36 | 70 | |
| Continuity | 98 | 96 | <0.001 |
| <33% | 2 | 5 | <0.001 |
| 33%–50% | 8 | 16 | |
| >50% | 91 | 79 | |
| Comorbidities | |||
| Coronary artery disease/MI | 23 | 23 | 0.91 |
| Congestive heart failure | 2 | 6 | <0.001 |
| Diabetes mellitus | 24 | 29 | <0.001 |
| Hypertension | 65 | 63 | 0.15 |
| Peripheral vascular disease | 5 | 6 | 0.004 |
| Pulmonary disorder/COPD | 9 | 17 | <0.001 |
| Stroke/TIA | 4 | 6 | <0.001 |
| Alcohol | 5 | 10 | <0.001 |
| Drug | 2 | 6 | <0.001 |
| Pneumonia | 0 | 0.03 | 0.24 |
| Schizophrenia | 1 | 2 | <0.001 |
| Bipolar disorder | 1 | 3 | <0.001 |
| Major Depression | 2 | 5 | <0.001 |
| PTSD | 5 | 8 | <0.001 |
| Hyperlipidemia | 58 | 52 | <0.001 |
| Influenza | 31 | 41 | <0.001 |
| Overweight/obesity | 14 | 17 | <0.001 |
| Primary care visits, IQR | 2 (1, 3) | 4 (2, 6) | <0.001 |
| Continuity visits, IQR | 2 (1, 3) | 3 (2, 4) | <0.001 |
| Assigned provider(s) | <0.001 | ||
| PCP only | 82 | 79 | |
| Trainee & PCP | 18 | 21 | |
| Zip code distance from ED | <0.001 | ||
| ≤2 | 13 | 20 | |
| 3–5 | 9 | 16 | |
| 6–10 | 1 | 2 | |
| 11–50 | 20 | 14 | |
| >50 | 57 | 49 | |
Abbreviations: IQR, interquartile range; MI, myocardial infarction; COPD, chronic obstructive pulmonary disease; TIA, transient ischemic attack; PTSD, post-traumatic stress disorder; PCP, primary care provider.
Sixty-nine percent (69%) were missing this variable.
Composite of major depression, bipolar, schizophrenia and PTSD.
Because of the small number of veterans in these groups, they were combined: active military personnel, CAV/NPS, ChampVA spouse and children, non-Veteran humanitarian groups, merchant marines, and Tricare.
Adjusted Predictors of ED Utilization
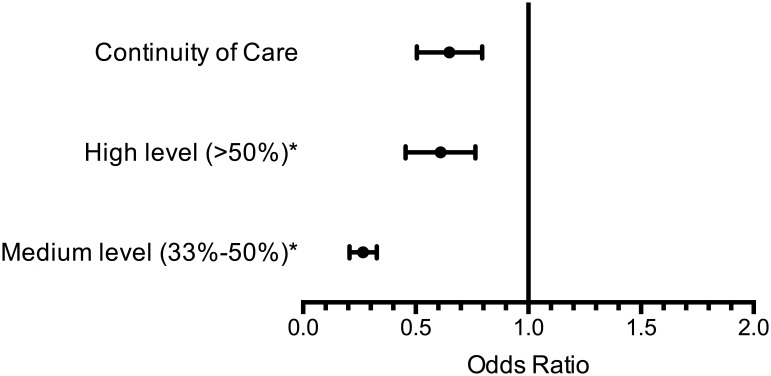
In the adjusted multivariable logistic regression ( Table 3 & Figure 2 ), continuity reduced ED utilization by 46% (adjusted odds ratio [AOR] 0.54; 95% CI: 0.41, 0.71). Likewise, the rate of ED visits for patients with continuity, 544/1000 PY (95% CI: 277, 1106), was lower compared to the patients without continuity, 784/1000 PY (95% CI: 484, 1272) (p = 0.001). Older age (AOR 0.91; 95% CI: 0.84, 0.98), low primary care clinic use (AOR 0.27; 95% CI: 0.24, 0.29), lower (<50%) service connection level (AOR 0.68; 95% CI: 0.58, 0.80), living far from the WHVA (>11 zip codes: AOR 0.53; 95% CI: 0.48, 0.59), and having a trainee provider assigned (AOR 0.78; 95% CI: 0.69, 0.89) were associated with lower ED utilization. Predictive factors included comorbidities such as smoking (AOR 1.22; 95% CI: 1.09, 1.37), substance abuse disorder (AOR 1.73; 95% CI: 1.47, 2.03), severe mental illness (AOR 1.31; 95% CI: 1.13, 1.51), coronary artery disease (AOR 1.19; 95% CI: 1.06, 1.34), congestive heart failure (AOR 2.38; 95% CI: 1.91, 2.97), diabetes (AOR 1.17; 1.05, 1.31), pulmonary disorders (AOR 1.68; 95% CI: 1.47, 1.92), and stroke (AOR 1.55; 95% CI: 1.26, 1.91); and compared with Vietnam era Veterans, serving during the post-Vietnam era (AOR 1.36; 95% CI: 1.13, 1.64) or World War II (AOR 1.40; 95% CI: 1.11, 1.75).
Table 3. Association Between Continuity of Care and Emergency Department Utilization.
| Rates of ED Utilization | ||||||
| Unadjusted | Adjusted a , b | |||||
| Variables | Visits/1000 PY (95% CI) | p-value | Visits/1000 PY (95% CI) | p-value | ||
| No Continuity c | 266 (222, 319) | - | 784 (484, 1272) | - | ||
| Continuity | 204 (141, 294) | 0.004 | 544 (277, 1106) | <0.001 | ||
| Odds of ED Utilization | ||||||
| Unadjusted | Adjusted a , b | |||||
| Variables | OR (95% CI) | p-value | AOR (95% CI) | p-value | ||
| Continuity | 0.64 (0.51, 0.80) | 0.001 | 0.54 (0.41, 0.71) | <0.001 | ||
| Continuity of care level | ||||||
| Low (<33%)c | 1.00 | - | - | - | ||
| Medium (33–50%) | 0.60 (0.46, 0.77) | <0.001 | - | - | ||
| High (>50%) | 0.26 (0.21, 0.33) | <0.001 | - | - | ||
| Age/10 | 0.85 (0.83, 0.88) | <0.001 | 0.91 (0.84, 0.98) | 0.02 | ||
| Male | 0.64 (0.53, 0.76) | <0.001 | 0.93 (0.75, 1.15) | 0.49 | ||
| Comorbidities | ||||||
| Smoker | 1.75 (1.59, 1.92) | <0.001 | 1.22 (1.09, 1.38) | 0.001 | ||
| Substance use disorder | 2.83 (2.49, 3.23) | <0.001 | 1.73 (1.47, 2.04) | <0.001 | ||
| Severe mental illness | 2.16 (1.92, 2.43) | <0.001 | 1.31 (1.13, 1.52) | <0.001 | ||
| MI/Coronary artery disease | 1.01 (0.91, 1.11) | 0.91 | 1.19 (1.06, 1.34) | 0.003 | ||
| Congestive heart failure | 2.92 (2.41, 3.54) | <0.001 | 2.38 (1.91, 2.97) | <0.001 | ||
| Diabetes mellitus | 1.27 (1.17, 1.39) | <0.001 | 1.17 (1.05, 1.31) | 0.004 | ||
| Hypertension | 0.94 (0.87, 1.02) | 0.15 | 1.02 (0.91, 1.14) | 0.71 | ||
| Peripheral vascular disease | 1.28 (1.08, 1.51) | 0.004 | 1.09 (0.90, 1.32) | 0.40 | ||
| Pulmonary disorder/COPD | 2.03 (1.81, 2.28) | <0.001 | 1.69 (1.48, 1.93) | <0.001 | ||
| Stroke/TIA | 1.61 (1.35, 1.94) | <0.001 | 1.55 (1.26, 1.91) | <0.001 | ||
| Hyperlipidemia | 0.76 (0.70, 0.82) | <0.001 | 0.82 (0.75, 0.91) | <0.001 | ||
| Flu | 1.56 (1.44, 1.70) | <0.001 | 1.08 (0.98, 1.20) | 0.10 | ||
| Obesity | 1.25 (1.12, 1.39) | <0.001 | 0.97 (0.85, 1.10) | 0.61 | ||
| Primary care user level | ||||||
| High (≥3 visits/year)c | 1.00 | - | 1.00 | - | ||
| Low (<3 visits/year) | 0.24 (0.22, 0.26) | <0.001 | 0.27 (0.24, 0.29) | <0.001 | ||
| Outside insurance | 0.62 (0.57, 0.67) | <0.001 | 0.87 (0.77, 0.99) | 0.03 | ||
| Service connection (%) | ||||||
| >75c | 1.00 | - | 1.00 | - | ||
| 51–75 | 0.78 (0.63, 0.96) | 0.02 | 0.83 (0.65, 1.04) | 0.10 | ||
| <50 | 0.48 (0.42, 0.55) | <0.001 | 0.68 (0.58, 0.80) | <0.001 | ||
| Service period | ||||||
| Vietnam Warc | 1.00 | - | 1.00 | - | ||
| Otherd | 0.93 (0.70, 1.24) | 0.62 | 1.14 (0.83, 1.57) | 0.43 | ||
| Korean War | 0.62 (0.54, 0.71) | <0.001 | 1.01 (0.84, 1.22) | 0.89 | ||
| Persian Gulf War | 1.13 (0.98, 1.31) | 0.09 | 0.99 (0.76, 1.28) | 0.92 | ||
| Post-Korean War Period | 0.59 (0.50, 0.70) | <0.001 | 0.89 (0.73, 1.09) | 0.27 | ||
| Post-Vietnam Period | 1.68 (1.45, 1.94) | <0.001 | 1.36 (1.13, 1.64) | <0.001 | ||
| World War II | 0.77 (0.68, 0.88) | <0.001 | 1.39 (1.11, 1.75) | 0.004 | ||
| Assigned provider(s) | ||||||
| PCP onlyc | 1.00 | - | 1.00 | - | ||
| Trainee & PCP | 1.24 (1.13, 1.37) | <0.001 | 0.78 (0.69, 0.89) | <0.001 | ||
| Zip code distance from ED | ||||||
| ≤2c | 1.00 | - | 1.00 | - | ||
| 3–5 | 1.10 (0.95, 1.27) | 0.19 | 1.06 (0.90, 1.25) | 0.49 | ||
| 6–10 | 0.87 (0.62, 1.24) | 0.45 | 1.10 (0.75, 1.61) | 0.63 | ||
| ≥11 | 0.53 (0.48, 0.59) | <0.001 | 0.58 (0.51, 0.65) | <0.001 | ||
Abbreviations: ED, emergency department; PY, per-year; CI, confidence interval; IQR, interquartile range; OR, odds ratio; AOR, adjusted odds ratio; COPD, chronic obstructive pulmonary disease; TIA, transient ischemic attack; PTSD, post-traumatic stress disorder; ED, emergency department; PCP, primary care provider.
The adjusted model excluded 1289 (9.6%) patients because they were missing one or more variables in the model.
Continuity of care levels were excluded because of potential for colinearity with the main outcome of interest, overall continuity.
Reference value.
Because of the small number of veterans in these groups, they were combined: active military personnel, CAV/NPS, ChampVA spouse and children, non-Veteran humanitarian groups, merchant marines, and Tricare.
Figure 2. Adjusted Odds Ratio of Association Between ED Visit and Continuity of Care and Levels of Continuity.
The first row illustrates the adjusted odds ratio between ED visits and continuity of care for individuals with at least one visit having continuity with their primary care provider. The second and third rows are the adjusted odds ratio for individuals who had high and medium levels of continuity and are compared to individuals with low levels of continuity, indicated by the asterisk (*).
We evaluated the association of different continuity levels and ED utilization amongst individuals having at least one primary care visit with continuity – low (2%), medium (10%), and high (88%). Those with low continuity had an ED visit rate of 662/1000 PY (95% CI: 407, 1076), compared to patients with medium continuity at 585/1000 PY (95% CI: 298, 1148; p = 0.20) and high continuity at 533/1000 PY (95% CI: 276, 1031; p = 0.01) ( Table 4 ). Analyzing odds ratios, individuals with medium and high levels of continuity were 31% less likely (AOR 0.69; 95% CI: 0.54, 0.92) and 41% less likely (AOR 0.59; 95% CI: 0.25, 0.76) to go to the ED compared to those with low continuity. Evaluating those individuals with low (<3 visits/year) versus high (≥3 visits/year) primary care users, those with low usage were 73% less likely (AOR 0.27; 95% CI: 0.24, 0.29) to use the ED.
Table 4. Association Between Levels of Continuity of Care and Emergency Department Utilization for Patients with ≥1 Continuity Visit.
| Adjusted Rates of ED Utilizationa | ||
| Variables | Visits/1000 PY (95% CI) | p-value |
| Continuity of care level | ||
| Low (<33%)b | 662 (407, 1076) | - |
| Medium (33–50%) | 585 (298, 1148) | 0.20 |
| High (>50%) | 533 (276, 1031) | 0.01 |
| Adjusted Odds of ED Utilization a | ||
| Variables | AOR (95% CI) | p-value |
| Continuity of care level | ||
| Low (<33%)b | 1.00 | |
| Medium (33–50%) | 0.70 (0.54, 0.92) | <0.001 |
| High (>50%) | 0.59 (0.25, 0.76) | <0.001 |
| Age/10 | 0.91 (0.84, 0.99) | 0.02 |
| Male | 0.96 (0.78, 1.20) | 0.74 |
| Comorbidities | ||
| Smoker | 1.24 (1.10, 1.39) | <0.001 |
| Substance use disorder | 1.74 (1.48, 2.04) | <0.001 |
| Severe mental illness | 1.30 (1.12, 1.51) | <0.001 |
| MI/Coronary artery disease | 1.19 (1.06, 1.34) | 0.003 |
| Congestive heart failure | 2.36 (1.89, 2.95) | <0.001 |
| Diabetes mellitus | 1.18 (1.06, 1.31) | 0.003 |
| Hypertension | 1.03 (0.92, 1.15) | 0.63 |
| Peripheral vascular disease | 1.08 (0.89, 1.31) | 0.41 |
| Pulmonary disorder/COPD | 1.68 (1.47, 1.92) | <0.001 |
| Stroke/TIA | 1.54 (1.26, 1.90) | <0.001 |
| Hyperlipidemia | 0.83 (0.75, 0.92) | <0.001 |
| Flu | 1.09 (0.99, 1.20) | 0.08 |
| Obesity | 0.96 (0.84, 1.09) | 0.49 |
| Primary care user level | ||
| High (≥3 visits/year)b | 1.00 | |
| Low (<3 visits/year) | 0.28 (0.26, 0.32) | <0.001 |
| Outside insurance | 0.87 (0.77, 0.98) | 0.02 |
| Service connection (%) | ||
| >75%b | 1.00 | |
| 51–75% | 0.82 (0.65, 1.04) | 0.10 |
| <50% | 0.69 (0.59, 0.80) | <0.001 |
| Service Period | ||
| Vietnam Warb | 1.00 | |
| Otherc | 1.14 (0.82, 1.57) | 0.44 |
| Korean War | 1.00 (0.83, 1.21) | 0.97 |
| Persian Gulf War | 0.97 (0.75, 1.26) | 0.85 |
| Post-Korean War Period | 0.89 (0.73, 1.09) | 0.25 |
| Post-Vietnam Period | 1.34 (1.12, 1.61) | 0.002 |
| World War II | 1.39 (1.10, 1.74) | 0.005 |
| Assigned provider(s) | ||
| PCP onlyb | 1.00 | |
| Trainee & PCP | 0.82 (0.72, 0.93) | 0.002 |
| Zip code distance from ED | ||
| ≤2b | 1.00 | |
| 3–5 | 1.06 (0.90, 1.25) | 0.48 |
| 6–10 | 1.09 (0.74, 1.59) | 0.67 |
| 11–50 | 0.55 (0.47, 0.64) | <0.001 |
| >50 | 0.59 (0.52, 0.66) | <0.001 |
Abbreviations: ED, emergency department; PY, person-year; CI, confidence interval; IQR, interquartile range; OR, odds ratio; AOR, adjusted odds ratio; COPD, chronic obstructive pulmonary disease; TIA, transient ischemic attack; PTSD, post-traumatic stress disorder; ED, emergency department; PCP, primary care provider.
The adjusted model excluded 1289 (9.6%) patients because they were missing one or more variables in the model.
Reference value.
Because of the small number of veterans in these groups, they were combined: active military personnel, CAV/NPS, ChampVA spouse and children, non-Veteran humanitarian groups, merchant marines, and Tricare.
Stratified Analysis, Sensitivity Analysis, Interactions
To further evaluate the independence of the association between continuity and ED utilization, we calculated stratum-specific odds ratios for the number of primary care clinic visits during the study period instead of dichotomizing the population into “low” and “high” primary care users. These models, adjusted for the same covariates in Table 3, found a similar association between continuity and ED visits ( Table 5 ) for patients who had one visit (AOR 0.41; 95% CI: 0.24, 0.68) and two visits (AOR 0.39; 95% CI: 0.25, 0.61) in the year. However, the association between continuity on ED utilization did not reach statistical significance when looking at individuals with three, four, or five or more visits in the year.
Table 5. Association Between Continuity and Emergency Department Utilization, Stratified by Total Number of Primary Care Visits.
| No. of Primary Care Visits | AOR (95% CI)* | p-value |
| 1 | 0.41 (0.24, 0.68) | <0.001 |
| 2 | 0.39 (0.25, 0.61) | <0.001 |
| 3 | 1.08 (0.52, 2.23) | 0.84 |
| 4 | 1.54 (0.55, 4.35) | 0.41 |
| 5+ | 1.09 (0.49, 2.40) | 0.84 |
AOR, adjusted odds ratio; CI, confidence interval.
*The adjusted odds ratio is the association between continuity and emergency department utilization based on the same covariates used in the model as outlined in Table 3.
Because of the high proportion of patients with >50% of their visits with continuity of care, the high continuity individuals were further categorized into patients with >75% of their visits having continuity with their assigned PCP (data not shown). These patients were 51% less likely to utilize the ED compared to patients with low continuity (AOR 0.49; 95% CI: 0.38, 0.64).
Discussion
This study found continuity of care had an independent association with lower ED utilization after controlling for age, gender, patient comorbidities, primary care user levels, having outside insurance, service connection status, military service period, distance from the VA, and having an associate provider. Having a trainee manage the outpatient care of a patient was associated with higher ED utilization in the unadjusted model (AOR 1.24; 95% CI: 1.13, 1.37), but was then associated with lower ED utilization in the adjusted model (AOR 0.78; 95% CI: 0.69–0.89), illustrating there was confounding.
To our knowledge, this is the first detailed description of PCMH continuity of care and an analysis of the association between continuity and ED utilization within this model, an important downstream outcome for PCMH care [14]. A Canadian study has evaluated the association between continuity and ED utilization within the large integrated Canadian health system, which showed that no continuity was associated with a 27 to 49% increase in ED usage [15]. These results are difficult to extrapolate, however, given the multiple differences between the VA and the Canadian health system that may confound the effects of continuity. Gill et al. measured continuity prior to the widespread uptake of PCMH models, evaluating Delaware’s Medicaid data from 1993–1994 using multivariable analyses, showing an 18% decrease in the odds of having a single ED visit and a 35% decreased odds of having multiple ED visits in a year among individuals with 3 or more primary care visits in a year [16].
To date, most reports evaluating the impact of PCMH models have focused on studying the methodology of implementing and integrating PCMH models into pre-existing medical practices [18], [28], [29]. Some studies suggest that PCMH models might improve continuity, but conclusions are based on perceptions of continuity, not continuity indices [30]–[32]. One study by Rosland et al. does report significantly improved continuity from 80% in December 2009 to 83% in June 2012 across all VA’s nationally after the implementation of PACT [12]. However, because the implementation of PACT is not expected to be complete at all VA’s until 2014, this analysis cannot fully characterize continuity across all centers and it does not analyze the association between continuity and ED use. Moreover, our methodology and dataset allows us to evaluate the impact of trainees. Large analyses have not been able to delineate continuity at the level of the trainee, while studies of trainees working within PCMH models describe qualitative experiences, not quantitative outcomes such as continuity or healthcare utilization patterns [12], [30], [31], [33]. Understanding the impact of trainees is also important because corollaries exist between residency outpatient clinics and non-training, interprofessional clinics where a physician supervises NP’s and PA’s.
Our study has limitations, notably unmeasured confounders that are inherent limitations to retrospective, observational studies. First of all, we cannot fully account for all the PACT-related components implemented in the years prior to the formalized implementation of PACT teams in 2011 at the WHVA because of the irregular nature and timing of systems-based changes required for PACT implementation. Additionally, given the VA’s work-environment culture of enhancing system performance, continuous quality improvement cycles were occurring throughout the study period affecting our ability to isolate and characterize systems changes that were fluid in nature. We can report that during the study period, major interventions for improving continuity, for example open-access scheduling or weekend clinic days, were not implemented at the WHVA. Moreover, we attempted to control for variability in PACT implementation by isolating our study to the WHVA, while an analysis of multiple facilities or large regional health systems might not be able to control for accurately. Secondly, our study design did not allow us to address the quality of a visit or account for education provided to patients on how to appropriately use the primary care clinic or the ED. Thirdly, we did not capture visits to other members of the health teams as defined in other PCMH models – pharmacists, physical therapists, social workers, mental health providers, medical or surgical specialty services, or medical assistants, who might have contributed to patient care and potentially prevented ED visits. The frequency of patient encounters with registered nurses, a key component of PACT teams, was recorded but not included in the analysis because only two percent of primary care clinic visits were exclusively with registered nurses (data not shown) and were therefore unlikely to alter our conclusions. Fourth, we cannot account for ED visits outside of the WHVA system or for patient preference to go to the WHVA ED or not. We attempted to control for factors known to influence a patient’s selection to visit one ED over another by accounting for the presence of outside insurance, the level of service connection to the VA, and the distance that a patient lived from the WHVA ED [34], [35]. Fifth, our analysis does not explore how PACT changed continuity at the WHVA and whether or not changing continuity, as PCMH aims to improve, altered ED utilization. Sixth, though we controlled for patient-level data in the adjusted model, there might be other unmeasured variables that are unavailable for a dataset such as ours. For example, individuals with less than three visits in a year, “low” primary care users, were less likely to visit the ED. Patients using the primary care clinic less might have more flexible personal schedules to see their provider because they were less sick. In contrast, those who visited the clinic three or more times in the year might have needed to be seen more urgently because of their comorbidities. Therefore, they might be inclined to see any available provider, not their assigned PCP; equivalently, they might be more likely to utilize the ED to receive care. We attempted to control for these patient-level characteristics by accounting for comorbidities, but could not account for exacerbations of their comorbid conditions prompting more frequent visits. Finally, the association between higher continuity of care levels and lower risk of ED visits cannot be used to conclude that this is a causal relationship.
In conclusion, higher continuity of care within a PCMH model was associated with decreased ED utilization. Further analyses of PCMH should evaluate the magnitude of PCMH’s impact on continuity of care, how changes in continuity might alter ED utilization, and explore other arenas of healthcare utilization, including hospitalization and readmissions. Moreover, as the volume of studies on PCMH models grows, emphasis should be placed on understanding individual components or features of PCMH, allowing clinics and integrated healthcare networks to focus on specific PCMH components shown to improve the efficient use of healthcare services by patients which may potentially save costs to the US health system.
Funding Statement
This publication was supported by the Office of Academic Affiliations and the VA Connecticut Health System Center of Excellence in Primary Care Education. Neither funding source had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation or review of the manuscript. The Office of Academic Affiliation did approve the manuscript for publication, but no modifications were made to the manuscript. Evergreen Design provided support in the form of a salary for author WL, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. Iora Health provided support in the form of a salary for author AK, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘author contributions’ section.
References
- 1.(2007) Joint Principles of the Patient Centered Medical Home | Patient Centered Primary Care Collaborative.
- 2. Parekh AK, Barton MB (2010) The challenge of multiple comorbidity for the US health care system. JAMA 303: 1303–1304. [DOI] [PubMed] [Google Scholar]
- 3. Lee TA, Shields AE, Vogeli C, Gibson TB, Woong-Sohn M, et al. (2007) Mortality rate in veterans with multiple chronic conditions. J Gen Intern Med 22 Suppl 3403–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dewing S, Mathews C, Schaay N, Cloete A, Louw J, et al. (2012) Behaviour change counselling for ARV adherence support within primary health care facilities in the Western Cape, South Africa. AIDS and Behavior 16: 1286–1294. [DOI] [PubMed] [Google Scholar]
- 5. Bodenheimer T (2006) Primary care–will it survive? N Engl J Med 355: 861–864. [DOI] [PubMed] [Google Scholar]
- 6. Sia C, Tonniges TF, Osterhus E, Taba S (2004) History of the medical home concept. Pediatrics 113: 1473–1478. [PubMed] [Google Scholar]
- 7. Duncan LG, Moskowitz JT, Neilands TB, Dilworth SE, Hecht FM, et al. (2012) Mindfulness-based stress reduction for HIV treatment side effects: a randomized, wait-list controlled trial. J Pain Symptom Manage 43: 161–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kuehn BM (2012) Veterans health system cited by experts as a model for patient-centered care. JAMA 307: 442–443. [DOI] [PubMed] [Google Scholar]
- 9. Dewan NA, Rice KL, Caldwell M, Hilleman DE (2011) Economic evaluation of a disease management program for chronic obstructive pulmonary disease. COPD 8: 153–159. [DOI] [PubMed] [Google Scholar]
- 10. Ishani A, Greer N, Taylor BC, Kubes L, Cole P, et al. (2011) Effect of nurse case management compared with usual care on controlling cardiovascular risk factors in patients with diabetes: a randomized controlled trial. Diabetes Care 34: 1689–1694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rice KL, Dewan N, Bloomfield HE, Grill J, Schult TM, et al. (2010) Disease management program for chronic obstructive pulmonary disease: a randomized controlled trial. Am J Respir Crit Care Med 182: 890–896. [DOI] [PubMed] [Google Scholar]
- 12. Rosland AM, Nelson K, Sun H, Dolan ED, Maynard C, et al. (2013) The patient-centered medical home in the Veterans Health Administration. Am J Manag Care 19: e263–272. [PubMed] [Google Scholar]
- 13. McCusker J, Tousignant P, Borges Da Silva R, Ciampi A, Levesque JF, et al. (2012) Factors predicting patient use of the emergency department: a retrospective cohort study. CMAJ 184: E307–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Flores-Mateo G, Violan-Fors C, Carrillo-Santisteve P, Peiro S, Argimon JM (2012) Effectiveness of organizational interventions to reduce emergency department utilization: a systematic review. PLoS One 7: e35903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ionescu-Ittu R, McCusker J, Ciampi A, Vadeboncoeur AM, Roberge D, et al. (2007) Continuity of primary care and emergency department utilization among elderly people. CMAJ 177: 1362–1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gill JM, Mainous AG 3rd, Nsereko M (2000) The effect of continuity of care on emergency department use. Arch Fam Med 9: 333–338. [DOI] [PubMed] [Google Scholar]
- 17. Burge F, Lawson B, Johnston G (2003) Family physician continuity of care and emergency department use in end-of-life cancer care. Med Care 41: 992–1001. [DOI] [PubMed] [Google Scholar]
- 18. Reid RJ, Fishman PA, Yu O, Ross TR, Tufano JT, et al. (2009) Patient-centered medical home demonstration: a prospective, quasi-experimental, before and after evaluation. Am J Manag Care 15: e71–87. [PubMed] [Google Scholar]
- 19. Harbrecht MG, Latts LM (2012) Colorado’s Patient-Centered Medical Home Pilot met numerous obstacles, yet saw results such as reduced hospital admissions. Health Aff (Millwood) 31: 2010–2017. [DOI] [PubMed] [Google Scholar]
- 20.Grumbach K, Grundy P (2010) Outcomes of implementing patient-centered medical home interventions: a review of the evidence from prospective evaluation studies in the United States. Washington, DC: Patient-Centered Primary Care Collaborative.
- 21. Roby DH, Pourat N, Pirritano MJ, Vrungos SM, Dajee H, et al. (2010) Impact of patient-centered medical home assignment on emergency room visits among uninsured patients in a county health system. Med Care Res Rev 67: 412–430. [DOI] [PubMed] [Google Scholar]
- 22. Fields D, Leshen E, Patel K (2010) Analysis & commentary. Driving quality gains and cost savings through adoption of medical homes. Health Aff (Millwood) 29: 819–826. [DOI] [PubMed] [Google Scholar]
- 23.(2011) Office of Academic Affiliations. VA Centers of Excellence in Primary Care Education.
- 24. Magill MK, Senf J (1987) A new method for measuring continuity of care in family practice residencies. J Fam Pract 24: 165–168. [PubMed] [Google Scholar]
- 25. Bice TW, Boxerman SB (1977) A quantitative measure of continuity of care. Med Care 15: 347–349. [DOI] [PubMed] [Google Scholar]
- 26. Justice AC, Lasky E, McGinnis KA, Skanderson M, Conigliaro J, et al. (2006) Medical disease and alcohol use among veterans with human immunodeficiency infection: A comparison of disease measurement strategies. Med Care 44: S52–60. [DOI] [PubMed] [Google Scholar]
- 27. Westover AN, McBride S, Haley RW (2007) Stroke in young adults who abuse amphetamines or cocaine: a population-based study of hospitalized patients. Arch Gen Psychiatry 64: 495–502. [DOI] [PubMed] [Google Scholar]
- 28. Sidorov JE (2008) The patient-centered medical home for chronic illness: is it ready for prime time? Health Aff (Millwood) 27: 1231–1234. [DOI] [PubMed] [Google Scholar]
- 29. Nutting PA, Crabtree BF, Miller WL, Stange KC, Stewart E, et al. (2011) Transforming physician practices to patient-centered medical homes: lessons from the national demonstration project. Health Aff (Millwood) 30: 439–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Markova T, Mateo M, Roth LM (2012) Implementing teams in a patient-centered medical home residency practice: lessons learned. J Am Board Fam Med 25: 224–231. [DOI] [PubMed] [Google Scholar]
- 31.Chang A, Bowen JL, Buranosky RA, Frankel RM, Ghosh N, et al.. (2012) Transforming Primary Care Training-Patient-Centered Medical Home Entrustable Professional Activities for Internal Medicine Residents. J Gen Intern Med. [DOI] [PMC free article] [PubMed]
- 32.Henschen BL, Garcia P, Jacobson B, Ryan ER, Woods DM, et al.. (2013) The Patient Centered Medical Home as Curricular Model: Perceived Impact of the “Education-Centered Medical Home”. J Gen Intern Med. [DOI] [PMC free article] [PubMed]
- 33.Hochman ME, Asch S, Jibilian A, Chaudry B, Ben-Ari R, et al.. (2013) Patient-Centered Medical Home Intervention at an Internal Medicine Resident Safety-Net Clinic. JAMA Intern Med. [DOI] [PMC free article] [PubMed]
- 34. Grafstein E, Wilson D, Stenstrom R, Jones C, Tolson M, et al. (2013) A regional survey to determine factors influencing patient choices in selecting a particular emergency department for care. Acad Emerg Med 20: 63–70. [DOI] [PubMed] [Google Scholar]
- 35. Wharam JF, Zhang F, Landon BE, Soumerai SB, Ross-Degnan D (2013) Low-socioeconomic-status enrollees in high-deductible plans reduced high-severity emergency care. Health Aff (Millwood) 32: 1398–1406. [DOI] [PubMed] [Google Scholar]