Abstract
Intraosseous pneumatocyst is a gas containing lesion located within a bone. It is a relatively rare condition of unclear etiology and with an undetermined natural course. Gas-density-fluid level pneumatocyst is even rarer. Pneumatocyst is frequently seen in adults but rarely reported in pediatrics. The lesion is usually small and is seen in the vertebral bodies as well as around the sacroiliac joints. Rarely does it occur in other parts of the skeleton. We are reporting a case of large blood signal intensity containing intraosseous pneumatocyst in a 14 year old boy and reviewing other pediatric cases of pneumatocysts as well as those with gas-density-fluid level. The recognition of this incidental rare benign lesion is essential to avoid over investigation and an inappropriate aggressive intervention.
Keywords: Intraosseous pneumatocyst, Gas-density-fluid level, Pediatrics, CT, MRI
CASE REPORT
A 14 year old male arrived at the emergency room with abdominal pain of 12 hours duration. The pain had started in the periumbilical region and then localized in the right iliac fossa. He was also experiencing nausea, anorexia and frequent vomiting. He had no fever, diarrhea or constipation. On examination, he was alert not distressed; his temperature was 37.1°C (normal 36.8° ± 0.4°C); and his other vital signs were within normal limits. Examination of the abdomen revealed right iliac fossa tenderness and positive Rovsing’s sign but without rebound tenderness. A preliminary diagnosis of acute appendicitis was made. His complete blood picture showed a white blood cell count 6.17×1000 cells/mm3 (normal 5,000–10,000 cells/ mm3), neutrophils 28.9% (normal 50%) and lymphocytes 52.1% (normal 25–40%). Urine analysis was normal. Pelvic ultrasound showed a normal appearing appendix and enlarged mesenteric lymph nodes suggestive of mesenteric adenitis.
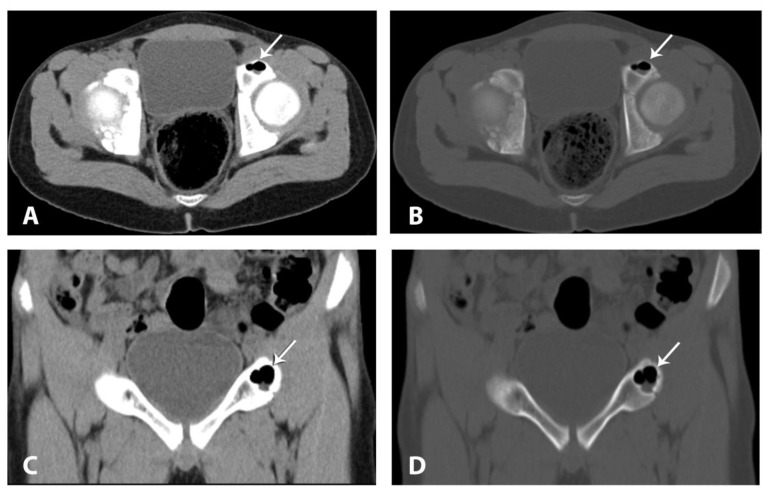
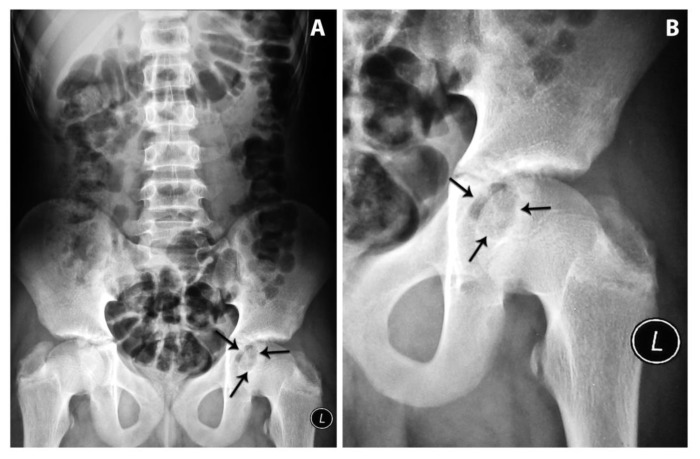
CT (Computed tomography) scan without contrast confirmed ultrasound findings of mesenteric lymph nodes enlargement. Incidentally, a lobulated lesion was noted within the left acetabulum which contains gas with density measuring - 951 HU (Hounsfield unit) and fluid level with density measuring 10 HU. It is surrounded by thin sclerotic rim (Fig. 1). The lesion measured 20×18×10 mm. Multiplanar reformatting failed to detect any cortical breach or connection to the hip joint. The surrounding soft tissue and the hip joint appeared normal. The patient denied any history of trauma or of any complaints related to the hip joint. Reviewing abdominal plain film, a well circumscribed lytic lesion with sclerotic margin at the projection of the left acetabulum was seen (Fig. 2).
Figure 1.
Fourteen year-old boy with incidental left acetabular intraosseous pneumatocyst. Axial CT scan (a) soft tissue window (b) bone window. Coronal CT scan (c) soft tissue window (d) bone window. It shows a gas density - fluid level well circumscribed lobulated lesion with thin sclerotic margin (arrows) involving pubic bone portion of the left acetabulum. Note the normal appearance of adjacent bone, hip joint and surrounding soft tissue. [Technique CT, 106mAs, 120 KVP, 3mm SL, without contrast].
Figure 2.
Fourteen year-old boy with incidental left acetabular intraosseous pneumatocyst. (A) Abdomen radiograph, anteroposterior view, supine. (B) Magnified view of left hip joint. It shows a well circumscribed, lobulated, expansile, lytic lesion with sclerotic margin and narrow zone of transition. It is seen at the projection of the left hip joint (arrows).
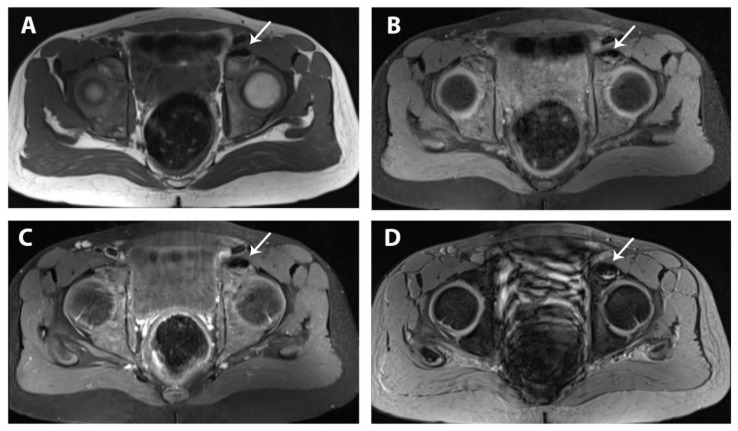
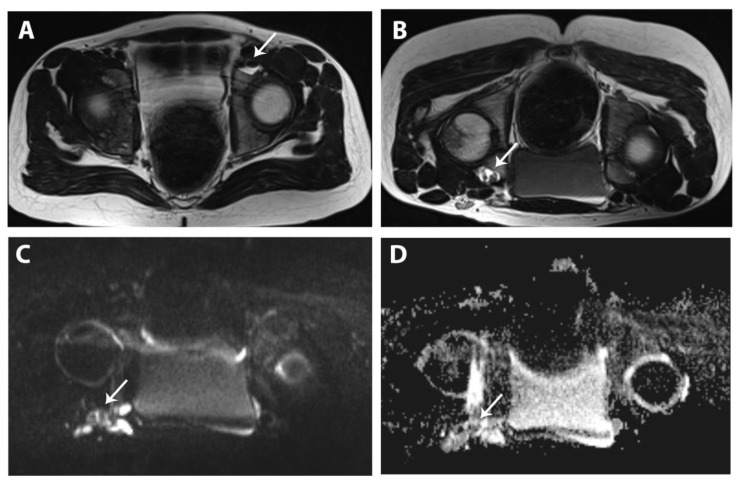
MRI (Magnetic resonance Imaging) was performed using a 3T (3 Tesla) Machine (Magnetom-Vario, Siemens, Erlangen- Germany) for further assessment of the lesion: axial T1WI (T1 weighted images), T1WI FAT SAT (T1 weighted images with fat saturation), T2WI (T2 weighted images), STIR (Short tau inversion recovery), GRE (Gradient recalled echo), DWI (Diffusion weighted images) and T1WI FAT SAT post contrast sequences were obtained in both supine and prone positions. The fluid component demonstrated an intermediate to high signal intensity on T1WI and high signal intensity on T2WI with restriction of diffusion. On GRE images two levels of low signal intensity at its upper part and high signal intensity at its dependant part were apparent. These findings are suggestive of late subacute blood content. The gas component demonstrated a signal void on all sequences (Fig. 3 and 4). Turning the patient to a prone position and waiting for few minutes (Fig. 4) confirmed that the fluid within the lesion was movable, while tracking of the fluid along the cyst wall suggested its thick consistency. The lesion, the surrounding bone, and soft tissue did not enhance on post contrast images. The adjacent hip joint was unremarkable.
Figure 3.
Fourteen year-old boy with incidental left acetabular intraosseous pneumatocyst. pelvic MRI axial cuts (a) T1WI [SL 3, TE 19, TR 778], (b) T1WI FAT SAT [SL 3, TE 19, TR 674], (c) T1WI FAT SAT post Contrast[SL 3, TE 19, TR 674, 4 ml of Gadolinium] and (d) GRE WI [SL 3, TE 9.84, TR 500] in supine position. The fluid component of the lesion (arrows) appears of intermediate signal on T1WI with no suppression upon fat saturation and no post contrast enhancement. On GRE WI the fluid inside the lesion shows two levels of low signal intensity at the upper part and high signal intensity at its dependant part.
Figure 4.
Fourteen year-old boy with incidental left acetabular intraosseous pneumatocyst. Pelvic MRI axial cuts (a) T2WI supine [SL 3, TE 120, TR 5550] shows high T2WI signal intensity of the fluid with clear level (arrow). (b) T2WI prone [SL 3, TE 120, TR 5550] shows free movement of the fluid along the lesion wall (arrow). (c) DWI prone [SL 3, TE 104, TR 5719] and (d) ADC map (Apparent Diffusion Coefficient map) prone [SL 3, TE 104, TR 5719, ep_b0_1000] show restriction of diffusion (arrows).
The patient was followed up by his primary care physician outside our hospital for more than a year; he is doing well without related complaints in this region and with normal growth. Follow up imaging was not needed.
DISCUSSION
True pneumatization in humans is the pneumatization of paranasal sinuses and the middle ear. Besides birds and dinosaurs, pneumatization of other parts of the body is very rare [1]. Ramirez et al [2] in 1984 was the first to describe intraosseous gas containing lesions with thin sclerotic rim, and he proposed a name ‘Pneumatocyst’ to such lesions. Gas- density-fluid level containing cysts are extremely rare and only few adult cases have been reported in the literature (Table 1). The exact nature of this fluid has never been previously discussed. Being familiar with these benign lesions, which are neither tumor-like nor destructive, is important because air within a bone has been combined with some serious bone conditions, including osteomyelitis, osteonecrosis, post traumatic and post intervention (e.g. embolization). Other benign and malignant neoplastic processes may give similar appearance on conventional imaging or MRI [3,4,5]. Review of literature clearly demonstrates male gender predilection with age range between 20–66 years [5,6]; however, the first pediatric case was reported in 2005, and our reported case is the fourth case in a child [3,7,8], and the first that involves the acetabulum and also the first to demonstrate gas-density-fluid level in this age group. It was assessed by plain film, CT scan, and 3T MRI (Table 2).
Table 1.
Gas-density-fluid level containing intraosseous pneumatocyst Review of cases listed in chronological order [F (female), M (male), Rt (right), Lt (left)]
| Reference | Age (years) | Gender | Imaging Modalities | Site | Characterization of the fluid |
|---|---|---|---|---|---|
| Hahn et al 1984 [15] | 19 | M | Plain film CT |
Lt Humerus | Aspiration, yellow clear fluid, negative culture |
| Narvμez et al 1999 [5] | 62 | M | Plain film CT MRI |
Rt Acetabulum | Intermediate T1 and high T2 signal consistent with fluid |
| Nakayama et al 2001 [11] case 1 | 56 | M | Plain Film CT MRI |
L5 vertebral body | Low T1 and High T2 signal consistent with fluid |
| Nakayama et al 2001 [11] case 2 | 57 | M | Plain Film CT MRI |
C5 vertebral body | Low T1 and High T2 signal consistent with fluid |
| Yamamoto et al 2002 [12] | 56 | F | Plain film CT MRI |
C5 vertebral body | CT 30 HU density of the fluid Inhomogeneous low T1 and high T2 signal consistent with fluid |
| This case | 14 | M | Plain film CT MRI |
Lt Acetabulum | CT 10 HU density of the fluid Intermediate to high signal on T1, high signal on T2 and DWI, two level of low and high signal on GRE consistent with late subacute hemorrhage |
Table 2.
Pediatric intraosseous pneumatocyst case review listed in chronological order, [F (female), M (male), Rt (right), Lt (left), SI (sacroiliac)].
| Reference | Age (years) | Gender | Symptoms | Imaging Modalities | Site | Size | Gas-Fluid level |
|---|---|---|---|---|---|---|---|
| Haktanir et al 2005 [8] | 17 | F | Neck pain, Klippel-Feil Syndrome | Plain film CT |
Rt Cervical Rib | 11×11 mm | No |
| Kota et al 2006 [3] | 9 | M | Abdominal pain due to blunt trauma | CT | Lt Ilium adjacent to SI joint | ——— | No |
| Weinberg et al 2011 [7] | 17 | M | Abdominal pain due to Salmonella gastroenteritis | CT | Rt Ilium adjacent to SI joint | 14×0.97×14 mm | No |
| This case | 14 | M | Abdominal pain due to mesenteric lymphadenitis | Plain film CT MRI |
Lt Acetabulum | 20×18×10 mm | Yes |
The pathogenesis of intraosseous pneumatocyst is poorly understood [9,10]. Trapped gas filled spaces within a human body will be eventually reabsorbed [1]. Acquired nature of these cysts has been suggested [2,5]. Vacuum phenomenon is typically found in degenerative disease of intervertebral discs. This phenomenon also can be seen in a normal joints subjected to traction forces, which are caused by creating a negative pressure thereby a gas released from surrounding tissue [4,7]. Some authors proposed the same principle in the development of intraosseous pneumatocyst, but an unknown mechanism causes the release of a mixture of gasses--mainly nitrogen--from surrounding tissue into these cysts [11]. These lesions have been described in some literature as part of degenerative disease based on the fact of their proximity to a joint that shows degenerative changes, other reports have documented the presence of connection between these cysts and joint space, which explains the reason that these lesions may in fact be caused by vacuum phenomenon. However, other lesions have been reported in areas away from a joint or near completely normal joints without evidence of degenerative changes or without a clear connection to the joint space as it was in our case [5,6,7]. This raises the possibility of two similar appearing entities but of different pathogenesis; a primary pneumatocyst without clear underlying pathology and a secondary one associated with degenerative joint disease.
The natural course of pneumatocyst is not clearly established. Some authors documented the progression from air containing cyst to fluid containing cyst over a variable period of time ranging from weeks to months [11]. Yamamoto et al [12] showed clearly the progression of an air filled cyst to a fluid filled cyst that was subsequently replaced by granulation tissue over 40 week period. On the other hand, others suggest the possibility of resorption of fluid and accumulation of gas from a preexisting simple fluid filled cyst, ganglion or synovial cyst [5,12,13,14]. Progression in size has also been described [5,7,12], while other authors documented stable lesions on follow up imaging [1,5,9]. The exact nature of the fluid content inside these lesions has not been clearly established. Hahn et al [15] showed clear yellow fluid which grows no pathogenic organism upon aspiration. Nakayama et al [11] mentioned fluid signal intensity on MRI within both of his two reported cases. In our case the fluid inside the pneumatocyst is bloody according to MRI signal intensity, which may for the first time raise the possibility that spontaneous bleeding within the intraosseous pneumatocyst is one of the stages of its natural course (which is more clearly seen on 3T MRI).
The two cases reported by Ramirez et al [2] were the only cases that underwent excisional biopsy. Histology showed nonspecific fibrous capsule in both cases, in addition microscopic foci of myxoid stroma similar to intraosseous ganglion was seen in one of them. Based on these findings, the lack of endothelial lining in these lesions make the name ‘pneumatocyst’ a misnomer. It is clearly a pseudocyst rather than a cyst.
Intraosseous pneumatocysts are innocuous and are usually discovered incidentally in a patient who has another complaint unrelated to these lesions; however, some patients showed symptoms in a region close to the cyst, but these have been proven to be unrelated to the original complaint [5].
On plain radiography, pneumatocyst appears as a well-defined area of lucency surrounded by a thin sclerotic margin suggesting a long standing process; however, the exact nature of these lesions and their gas content can not be appreciated based on plain films only, and further evaluation is required. Small lesions can not be identified either because of inherit density of the bone, or because they are obscured by overlying gas shadows from the bowel. [2]. CT scan is the diagnostic modality of choice for these lesions because it can depict the content of these lesions precisely, can assess if the density is consistent with gas. It can also identify small lesions and determine gas-density or the gas-density-fluid level. CT scan clearly identifies the sclerotic thin border of these lesions and the presence or absence of surrounding bone or soft tissue abnormalities [1,7]. These lesions are usually solitary and small in size measuring 2–5 mm; however, multiple lesions have also been reported. These lesions are typically rounded or oval in shape, while in our case the lesion was solitary, large and lobulated [4]. Only few adult cases have undergone MRI [1,5,10,11,12], which showed pure gas cysts as areas of signal void, mimicking susceptibility artifact or hypersclerotic lesion, but with normal signal intensity of adjacent bone and with no contrast enhancement. In a pneumatocyst with gas-density-fluid level, characterization of the nature of the fluid can be identified according to its signal intensity, which could be simple fluid [5, 11] or free bloody fluid that changes with patient position as in our case. These lesions don’t demonstrate uptake on 99m Tc-MDP bone scan [6,12].
Conclusion, intraosseous pneumatocysts are rare bony lesions of benign nature and are very rare in children. They may appear as solely gas containing cysts or, very rarely, they can show a gas-density-fluid level that may be of blood content. These lesions may in reality be more common than expected; their asymptomatic nature may limit their identification. The awareness of the benignity of these incidental lesions and their different appearances in all modalities are of extreme importance, as they do not require follow up, biopsy or surgical intervention.
TEACHING POINT
Intraosseous pneumatocyst is a gas-density or a gas-density- fluid level bone cyst; a rare benign incidental lesion that may be seen in all age groups without associated clinical symptoms. CT is the modality of choice to identify the gas content; otherwise they can easily be mistaken as lytic lesions on plain film and sclerotic or susceptibility artifact on MRI.
Table 3.
Summary table for key aspects and imaging findings associated with intraosseous pneumatocyst.
| Etiology | Unknown |
| Incidence | Exact incidence is unknown. |
| Gender ratio | Male predilection [5,6] |
| Age predilection | 20–66 years [5,6]. four pediatric cases were reported to date including ours, age ranged from 9–17 years |
| Risk factor | No known risk factor. Degenerative joint or disc disease was postulated if the intraosseous pneumatocyst is seen in vicinity. |
| Treatment | None |
| Prognosis | Benign lesion |
| Findings on imaging |
Plain film: well defined areas of lucency surrounded by thin sclerotic margins CT: The diagnostic modality of choice. Well defined gas-density or gas-density-fluid level containing intraosseous lesions, sclerotic rim, normal surrounding bone and soft tissue. Adjacent joints may be normal or degenerated. Small lesion can be seen MRI: signal void mimicking susceptibility artifact or hypersclerotic lesion, normal signal intensity of adjacent bone and no contrast enhancement. Pneumatocyst with gas-fluid level, characterization of the nature of the fluid can be identified according to its signal intensity which could be simple fluid or free bloody fluid that changes with patient position as in our case Bone scan: 99m Tc-MDP scan show no uptake |
Table 4.
Differential diagnosis of intraosseous pneumatocyst.
| Modality | Differential Diagnosis | Description |
|---|---|---|
| Plain Film |
|
|
|
|
|
|
|
|
| CT |
|
|
|
|
|
| MRI |
|
|
|
|
|
|
|
ABBREVIATIONS
- ADC
Apparent Diffusion Coefficient
- CT
Computed tomography
- DWI
Diffusion weighted images
- F
female
- GRE
Gradient recalled weighted images
- HU
Hounsfield unit
- Lt
left
- M
male
- MRI
Magnetic resonance Imaging
- Rt
right
- SI
sacroiliac
- STIR
Short tau inversion recovery
- T1 FAT SAT
T1 fat saturation
- T1WI
T1 weighted images
- T2WI
T2 weighted images
REFERENCES
- 1.Fitzek S, Engelmann C, Fitzek C. Vertebral Pneumatization. Clin Neuroradiol. 2011;21:27–30. doi: 10.1007/s00062-010-0034-5. [DOI] [PubMed] [Google Scholar]
- 2.Ramirez H, Blatt ES, Cable HF, McComb BL, Zornoza J, Hibri NS. Intraosseous Pneumatocyst of the ilium findings on radiographs and CT scans. Radiology. 1984;150:503–505. doi: 10.1148/radiology.150.2.6691108. [DOI] [PubMed] [Google Scholar]
- 3.Kota G, Coleman L. Air in bone: intraosseous pneumatocyst in a child. Pediatr Radiol. 2006;36:999. doi: 10.1007/s00247-006-0237-8. [DOI] [PubMed] [Google Scholar]
- 4.Steingruber IE, Bach CM, Wimmer C, Nogler M, Buchberger W. Multisegmental pneumatocysts of lumbar spine mimic osteolytic lesions. Eur Radiol. 2001;11:845–848. doi: 10.1007/s003300000490. [DOI] [PubMed] [Google Scholar]
- 5.Narvμez JA, Narvμez J, Rodríguez-Mijarro1 M, Quintero JC. Acetabular pneumatocyst containing air-fluid level. Eur Radiol. 1999;9:1647–1649. doi: 10.1007/s003300050902. [DOI] [PubMed] [Google Scholar]
- 6.Catalano O, De Rosa F, Muto M. Intraosseous pneumatocyst of the ilium: CT findings in two cases and literature review. Eur. Radiol. 1997;7:1449–1451. doi: 10.1007/s003300050315. [DOI] [PubMed] [Google Scholar]
- 7.Weinberg B, Sharma R, Maldjian C. Abdominal Pain, Vomiting, and Nausea in a 17-Year-Old Patient. The Journal of Musculoskeletal Medicine. 2011;28(9) Available at: http://www.musculoskeletalnetwork.com/display/article/1145622/1939927. [Google Scholar]
- 8.Haktanir A, Degirmenci B, Albayrak R, Acar M, Yucel A. Klippel-Feil Syndrome Associated With Pneumatocyst of the Right Cervical Rib. South Med J. 2005;98(11):1132–1134. doi: 10.1097/01.smj.0000184788.50353.83. [DOI] [PubMed] [Google Scholar]
- 9.Cosar M, Eser O, Aslan A, et al. Vertebral Body Pneumatocyst in the Cervical Spine and Review of the Literature. Turkish Neurosurgery. 2008;18(2):197–199. [PubMed] [Google Scholar]
- 10.Haithcock JA, Layton KF, Opatowsky MJ. Vertebral pneumatocysts: uncommon lesions with pathognomonic imaging characteristics. Proc (Bayl Univ Med Cent) 2006;19:423–424. doi: 10.1080/08998280.2006.11928216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nakayama T, Ehara S, Hama H. Spontaneous progression of vertebral intraosseous pneumatocysts to fluid -fluid cyst. Skeletal Radiol. 2001;30:523–526. doi: 10.1007/s002560100367. [DOI] [PubMed] [Google Scholar]
- 12.Yamamoto T, Yoshiya S, Kurosaka M, et al. Natural Course of an Intraosseous Pneumatocyst of the Cervical Spine. AJR. 2002;179:667–669. doi: 10.2214/ajr.179.3.1790667. 0361-803X/02/1793-667. [DOI] [PubMed] [Google Scholar]
- 13.Master M, Keshava S. Incidental intraosseous pneumatocyst. Applied Radiology. Jan-Feb. 2010. p. 30. Available at: http://www.appliedradiology.com/uploadedFiles/Issues/2010/01/Cases/AR_01-02-10_MasterRC.pdf.
- 14.Kamba M, Ohuchi Y, Ogawa T, Ohata R. Intraosseous pneumatocyst of the scapula. The British Journal of Radiology. 2000;73:658–60. doi: 10.1259/bjr.73.870.10911791. [DOI] [PubMed] [Google Scholar]
- 15.Hahn PF, Rosenthalm DI, Ehrkich MG. Case Report 286. Skeletal Radiol. 1984;12(3):214–7. doi: 10.1007/BF00361091. [DOI] [PubMed] [Google Scholar]