Abstract
Background
Pre-emptive intravenous lidocaine infusion is known to improve postoperative pain in abdominal surgery. We assessed the effect of intravenous lidocaine infusion in patients who underwent subtotal gastrectomy.
Methods
We conducted a double-blind, placebo-controlled study with patients undergoing subtotal gastrectomy for early gastric cancer divided into 2 groups: 1 group received intravenous lidocaine infusion preoperatively and throughout surgery, and the other received normal saline infusion (placebo). We assessed postoperative outcomes, including pain scores on a visual analogue scale (VAS), administration frequency of patient-controlled analgesia (PCA) and the amount of consumed fentanyl. Postoperative nausea and vomiting, length of hospital stay (LOS), time to return to regular diet and patient satisfaction at discharge were evaluated.
Results
There were 36 patients in our study. Demographic characteristics were similar between the groups. The VAS pain scores and administration frequency of PCA were significantly lower in the lidocaine group until 24 hours after surgery, and fentanyl consumption was significantly lower in this group until 12 hours postoperatively compared with the placebo group. The total amount of consumed fentanyl and the total administration frequency of PCA were significantly lower in the lidocaine than the control group. No significant differences were detected in terms of nausea and vomiting, return to regular diet, LOS and patient satisfaction, and there were no reported side-effects of lidocaine.
Conclusion
Intravenous lidocaine infusion reduces pain during the postoperative period after subtotal gastrectomy.
Abstract
Contexte
Administrée à titre préventif, la perfusion intraveineuse de lidocaïne améliorerait la douleur postopératoire dans la chirurgie abdominale. Nous avons mesuré l’effet d’une perfusion intraveineuse de lidocaïne chez des patients soumis à une gastrectomie subtotale.
Méthodes
Nous avons réalisé une étude à double insu avec témoins sous placebo auprès de patients soumis à une gastrectomie subtotale pour un cancer de l’estomac au premier stade. Les patients ont été répartis en 2 groupes : l’un a reçu une perfusion intraveineuse de lidocaïne en préopératoire et tout au long de la chirurgie, tandis que l’autre a reçu une perfusion de solution physiologique (placebo). Nous avons évalué les résultats postopératoires, y compris les scores de douleur sur une échelle analogique visuelle, la fréquence d’administration d’analgésie contrôlée par les patients (ACP) et la quantité de fentanyl utilisée. Les nausées et vomissements postopératoires, la durée du séjour hospitalier, l’intervalle avant la reprise d’une alimentation régulière et la satisfaction du patient au moment de son congé ont aussi été consignés.
Résultats
Notre étude a regroupé 36 patients. Les caractéristiques démographiques étaient similaires entre les groupes. Les scores de douleur à l’échelle analogique visuelle et la fréquence d’administration de l’ACP ont été significativement moindres dans le groupe sous lidocaïne jusqu’à 24 heures après la chirurgie et la prise de fentanyl a aussi été significativement moindre dans ce groupe jusqu’à 12 heures après la chirurgie, comparativement au groupe témoin. La quantité totale de fentanyl utilisée et la fréquence totale d’administration de l’ACP ont été significativement plus faibles dans le groupe sous lidocaïne que dans le groupe témoin. Aucune différence significative n’a été observée pour ce qui est des nausées et vomissements, du retour à une alimentation régulière, de la durée du séjour hospitalier et de la satisfaction des patients et on n’a rapporté aucun effet secondaire associé à la lidocaïne.
Conclusion
La perfusion de lidocaïne intraveineuse atténue la douleur durant la période postopératoire après une gastrectomie subtotale.
Gastric cancer is the fourth most common type of cancer in the world and is the leading cause of cancer-related death in Korea.1,2 Curative treatment of gastric cancer can only be achieved by radical resection of the tumour and regional lymph nodes. Laparoscopic gastrectomy has increasingly been used in the surgical management of early gastric cancer in recent years. Although clinical trials of laparoscopic gastrectomy for advanced gastric cancer are being conducted, the standard surgical procedure for advanced gastric cancer in the middle or lower part of the stomach is subtotal gastrectomy via upper abdominal laparotomy. Compared with laparoscopic gastrectomy, open gastrectomy has been reported to cause sustained operative pain, which leads to the increased consumption of analgesics, delayed bowel function, subsequent complications, longer hospital stay and delayed return to normal activity.3,4 To relieve postoperative pain after major surgeries, such as subtotal gastrectomy, potent narcotics or analgesics have to be used, which can lead to undesirable effects, including respiratory depression, emesis, nausea, vomiting and sedation.5,6
Lidocaine is a local anesthetic that has been shown to have analgesic, antihyperalgesic7 and anti-inflammatory properties,8 which are associated with blockade of sodium channels and of N-methyl-d-aspartate (NMDA) and G protein–coupled receptors.
Systemic lidocaine has been reported to reduce postoperative pain, analgesic consumption, postoperative nausea and vomiting and the length of stay in hospital (LOS).9–11 Furthermore, intravenous lidocaine is easy to administer. The benefits of lidocaine are enhanced by the drug’s low expense, accessibility and safety.
Therefore, we hypothesized that systemic lidocaine would benefit patients with postoperative pain. We designed this study to assess the effect of intraoperative systemic lidocaine infusion in patients who underwent subtotal gastrectomy. The secondary outcome measures were fentanyl consumption and postoperative adverse events.
Methods
Patients
We sought to recruit 40 adult patients (age 18–80 yr) who underwent subtotal gastrectomy between May 2012 and March 2013 for participation in this study. We excluded patients who weighed less than 45 kg or more than 100 kg; had severe underlying respiratory, renal or hepatic disease; or had a history of allergies to local anesthetics. Further exclusion criteria were evidence of previous opioid medication or psychiatric medical history. The decision to exclude patients was made by an investigator (H.K.) who did not otherwise participate in data collection.
The study protocol was approved by the Institutional Review Board from the College of Medicine, Chung-Ang University, and the study was registered in the Australian New Zealand Clinical Trial Records (ACTRN12612000545864). This study was carried out according to the Declaration of Helsinki. We obtained written informed consent from all participants before enrolling them in the trial.
Study design and randomization
The patients were randomly divided into 2 groups: 1 group received intravenous lidocaine and the other received normal saline (placebo). Random assignment was based on a random table generated using PASS software version 11 (NCSS). We used block randomization with a block size of 4 and equal allocation to prevent imbalances in treatment assignments. The randomization sequence was generated by a statistician who was not otherwise involved with the study. The details of the series were unknown to the investigators, and the group assignments were kept in sealed envelopes, each bearing only the case number on the outside. After recruitment, the patients were given a case number, and 1 hour before admitting the patient into the operating room, the numbered envelope was opened and the card inside determined the group into which the patient would be placed. To keep the anesthesiologist blind to the patients’ assigned group, lidocaine or placebo were prepared in a syringe and a bottle labelled only with a case number. The preparations of bolus and continuous infusions were arranged by an additional investigator (H.S.Y.) who read the card. Patients assigned to the lidocaine group received an intravenous bolus infusion of 1.5 mg/kg of lidocaine followed by a continuous infusion of 2 mg/kg/h. Patients in the placebo group received the same amount of normal saline.
General anesthesia
All patients received the same anesthetic protocol. The patients were not premedicated, and anesthesia was induced with 2 mg/kg of propofol and 0.8 mg/kg of rocuronium administered intravenously. Patients were intubated, and mechanical ventilation was adjusted to keep the end-tidal CO2 between 35 and 40 mm Hg. Anesthesia was maintained using 5%–8% desflurane in 1 L/min nitrous oxide and 1 L/min of oxygen. Noninvasive arterial blood pressure, electrocardiography and pulse oximetry were monitored continuously. During surgery, the patients received an intravenous infusion of lactated Ringer solution at a rate of 6–12 mL/kg/h. No additional analgesics were injected during surgery.
Surgical technique
All surgical procedures were carried out identically. A vertical skin incision was made 2 cm above the xyphoid process to the umbilical level with a scalpel and electrocautery device. The laparotomy wound was protected with a surgical pad during the procedure. The surgical field was exposed using a self-retaining retractor. D2 lymph node dissection was routinely performed in all patients. The transection of the stomach and the distal two-thirds of the organ was accomplished using linear staplers. Billroth 2 gastrojejunostomy was performed with hand-sewing anastomosis or stapling methods. One closed suction drain was placed in the liver bed via the foramen of Winslow, and the laparotomy wound was closed layer by layer.
Postoperative pain control
To control postoperative pain, intravenous fentanyl was administered with the use of a patient-controlled analgesia system (PCA; Automed 3300, AceMedical Co.). The mode of PCA was a 0.3 μg/kg bolus with a lockout interval of 15 minutes, continuous infusion and 0.2 μg/kg/h (total regimen of 100 mL) of fentanyl. The patients were instructed to push the button for PCA each time they felt pain. In the case of persistent pain exceeding a visual analogue scale (VAS) pain score of 30 mm, an additional 50 μg of fentanyl (rescue) was intravenously injected by an investigator until the pain was relieved to a level falling below a VAS pain score of 30 mm.
Outcome variables
The primary outcome variables were pain levels measured using a VAS 2, 4, 8, 12, 24 and 48 hours after surgery and at discharge. The VAS scores were collected by 1 blinded investigator (J.H.Y.) with more than 2 years of experience interviewing patients about postoperative pain.
Secondary outcome variables included administration frequency of PCA and the total fentanyl consumption, patients’ satisfaction scores regarding pain control and with the overall recovery process, the incidence of postoperative nausea and vomiting, shivering, tinnitus, return to regular diet and LOS.
Administration frequency of PCA and the total fentanyl consumption (the sum of additional intravenous fentanyl bolus infusions and the fentanyl delivered by the PCA system) were evaluated in the following intervals: up to 2 hours, 2–4 hours, 4–8 hours, 8–12 hours, 12–24 hours and 24–48 hours.
During the preoperative visit, 2 of us (G.J.C. and H.S.Y.) instructed patients on the use of the 100 mm VAS (with 0 indicating “no pain” and 100 indicating “worst pain”) for pain assessment and on the use of the PCA device using a standardized protocol.
We obtained satisfaction scores regarding pain control and the overall recovery process at 48 hours postsurgery (11-point Likert scale, with 0 indicating “very dissatisfied” and 10 indicating “very satisfied”).
We recorded the incidence of postoperative nausea and vomiting reported by each patient. Further, time values that represented the recovery rate were collected from each patient; these included return to regular diet and LOS. All parties involved, including the patients, the surgeon, the anesthesiologists and the investigator (J.H.Y.) collecting the data were unaware of the study drugs or the patients’ group assignment.
Statistical analysis
To estimate group size, we conducted a pilot study measuring the VAS 4 hours after surgery in 8 patients who did not receive any medication. The standard deviation (SD) in the VAS pain score in this group was 20.2 mm. For our power calculation, we assumed an equal SD in the lidocaine group. We wanted to demonstrate a difference of 20 mm in the VAS pain score 2 hours postsurgery between the groups. With a 2-tailed α of 0.05 and a power of 80%, we needed 16 patients in each group. Considering a compliance rate of 80%, we sought to recruit 40 patients to participate in this study.
We used an intention-to-treat strategy — that is, all participants were included in the analysis irrespective of whether they had completed the study. Missing data were completed using a last observation carried forward analysis. The association between VAS, administration frequency of PCA and total fentanyl consumption was analyzed using an as-treated strategy.
For intergroup comparisons, we first evaluated the distribution of the data for normality using the Shapiro–Wilk test. The normally distributed data are presented as means ± SD, and we compared the groups using the Student t test. The non-normally distributed data are expressed as medians and interquartile ranges, and we analyzed the data using the Mann–Whitney U test.
Descriptive variables were subjected to χ2 analysis or the Fisher exact test, as appropriate. As VAS pain score, administration frequency of PCA and total fentanyl consumption were abnormally distributed, we evaluated the associations among these 3 variables at each time interval using the Spearman rank correlation coefficient (ρ). We considered results to be significant at p < 0.05. The data in the figures are reported as means ± standard errors of the mean. We performed our statistical analyses using SPSS software version 18.0 (IBM Corp.).
Results
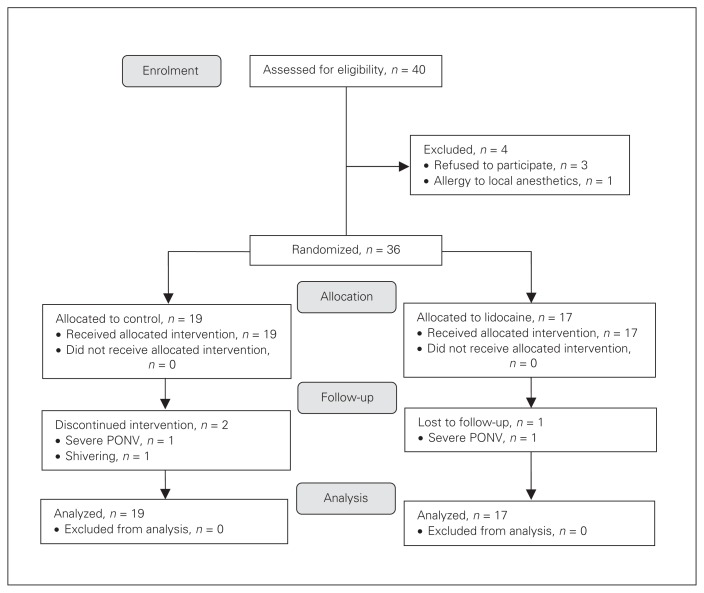
Of the 40 patients who were asked to participate in the study, 3 refused and 1 patient was excluded owing to a history of allergy to local anesthetics. Of the 36 remaining patients, 19 were randomly assigned to the placebo group and 17 were randomly assigned to to the lidocaine group. Figure 1 demonstrates the flow of patients through the trial according to the consolidated standards of reporting trials (CONSORT) statement. There were no significant differences between the groups in terms of age, sex, American Society of Anesthesiologists (ASA) class, height, weight, anesthesia or duration of surgery (Table 1).
Fig. 1.
Flow of patients through the study. PONV = postoperative nausea and vomiting.
Table 1.
Demographic and clinical characteristics of study participants
| Characteristic | Group; mean ± SD* | p value | |
|---|---|---|---|
| Control, n = 19 | Lidocaine, n = 17 | ||
| ASA, no. | 0.58 | ||
| 1 | 1 | 2 | |
| 2 | 17 | 13 | |
| 3 | 1 | 2 | |
| Age mean (IQR), yr | 66.00 (59.00–72.00) | 59.00 (57.00–66.50) | 0.12† |
| Sex, male:female | 12:7 | 10:6 | 0.79 |
| Height, cm | 162.77 ± 8.15 | 164.62 ± 10.81 | 0.56 |
| Weight, kg | 61.56 ± 7.83 | 63.56 ± 11.36 | 0.54 |
| Duration of surgery, min. | 291.32 ± 50.47 | 271.47 ± 33.11 | 0.18 |
| Duration of anesthesia, min. | 331.74 ± 56.45 | 316.00 ± 43.58 | 0.39 |
ASA = American Society of Anesthesiologists physical status; IQR = interquartile range; SD = standard deviation.
Unless otherwise indicated.
Mann–Whitney U test.
Data were incomplete for 3 patients. One patient in the lidocaine group and 1 patient in the placebo group were treated with other painkillers for postoperative nausea and vomiting that was unresponsive to antiemetic treatment and likely induced by fentanyl infusion. One patient in the placebo group received meperidine owing to postoperative shivering. Despite incomplete data, these 3 patients were included in our analysis according to the intention-to-treat principle.
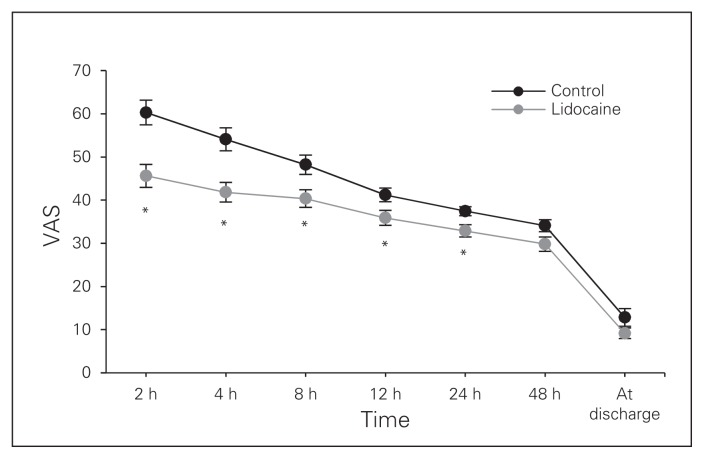
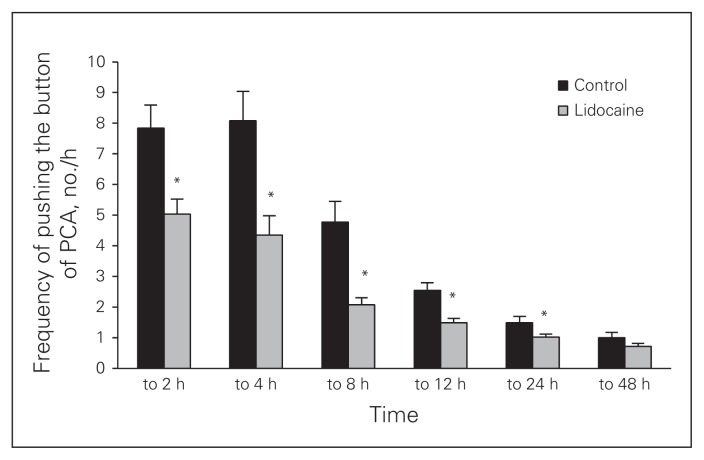
The results of the VAS pain scoring are shown in Figure 2. The highest pain scores were experienced 2 hours postsurgery, and the pain reduced gradually with time. For the first 24 hours postsurgery, the placebo group reported significantly higher VAS scores than the lidocaine group. At discharge, there was no difference with respect to pain between the groups. The administration frequency of PCA was higher in the placebo group than the lidocaine group at every time point for 24 hours postsurgery (Fig. 3). The total administration frequency of PCA in the first 48 hours postsurgery was also higher in the placebo group than the lidocaine group (p = 0.003; Table 2). The VAS scores were moderately correlated with administration frequency of PCA (ρ = 606, p < 0.001).
Fig. 2.
Visual analogue scale (VAS) pain score. Values are expressed as means ± standard errors of the mean. *p < 0.05 compared with the control group.
Fig. 3.
Frequency of pushing the button of patient-controlled analgesia (PCA) system. Values are expressed as means ± standard errors of the mean. *p < 0.05 compared with the control group.
Table 2.
Total amount of fentanyl use and administration frequency of patient-controlled analgesia
| Factor | Group; median (IQR)* | p value | |
|---|---|---|---|
| Control, n = 19 | Lidocaine, n = 17† | ||
| Fentanyl mean ± SD, μg | 2339.26 ± 387.02 | 1931.65 ± 457.03 | 0.007 |
| Administration frequency of PCA, no. | 76.00 (57.00–96.00) | 49.00 (41.00–57.00) | 0.003‡ |
| Satisfaction score, 0–10 | 5.00 (3.00–6.00) | 6.00 (4.50–7.00) | 0.049‡ |
IQR = interquartile ratio; PCA = patient-controlled analgesia; SD = standard deviation.
Unless otherwise indicated.
p < 0.05 compared with the control group.
Mann–Whitney U test.
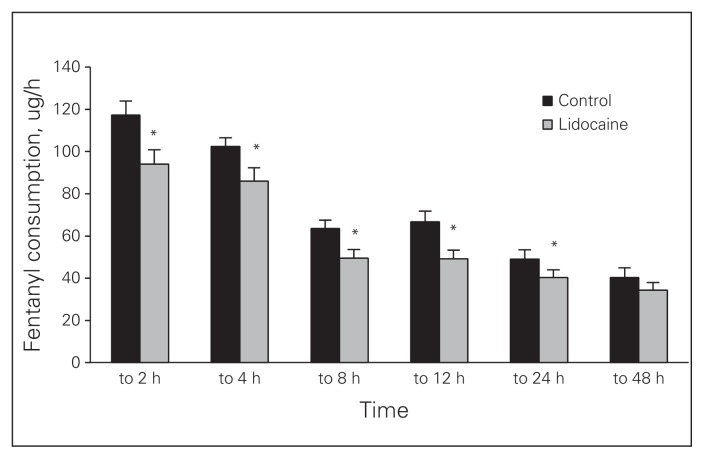
The amount of fentanyl consumption from PCA and rescue analgesia decreased gradually in both groups for 48 hours postsurgery and was higher in the placebo group than the lidocaine group in the first 12 hours (Fig. 4). In terms of total amount of injected fentanyl before discharge, the lidocaine group required significantly less analgesia than the placebo group (p < 0.001; Table 2). The VAS scores were positively correlated with fentanyl consumption (ρ = 0.550, p < 0.001).
Fig. 4.
Fentanyl consumption. Values are expressed as means ± standard errors of the mean. *p < 0.05 compared with the control group.
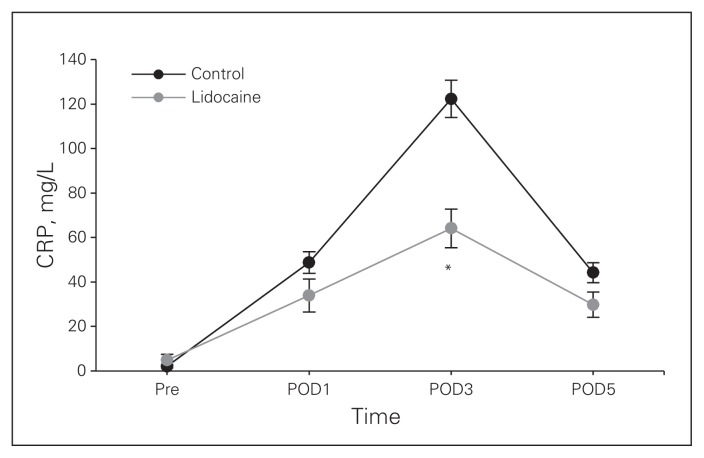
Postoperative C-reactive protein (CRP) was significantly higher in the placebo group than the lidocaine group on postoperative day 3 (p = 0.016; Fig. 5).
Fig. 5.
C-reactive protein (CRP). Values are expressed as means ± standard errors of the mean. *p < 0.05 compared with the control group. POD = postoperative day.
The satisfaction scores regarding pain control and the overall recovery process were higher in the lidocaine group than the placebo group (Table 2). No significant differences were noted between groups for postoperative nausea and vomiting, shivering, tinnitus, LOS or return to regular diet (Table 3).
Table 3.
Adverse events
| Event | Group; median (IQR)* | p value | |
|---|---|---|---|
| Control, n = 19 | Lidocaine, n = 17 | ||
| Nausea | 11 (57.9) | 5 (29.4) | 0.09 |
| Vomiting | 7 (36.8) | 3 (17.6) | 0.20 |
| Shivering | 1 (5.3) | 0 (0) | > 0.99 |
| Tinnitus | 0 (0) | 0 (0) | > 0.99 |
| LOS | 15 (12.0–18.0) | 13 (11.5–15.5) | 0.13 |
| Resume regular diet | 4 (4.0–5.0) | 4 (3.0–5.0) | 0.51 |
IQR = interquartile ratio; LOS = length of stay in hospital.
Mann–Whitney U test.
Discussion
In this prospective study of patients who underwent subtotal gastrectomy, we found that intravenous lidocaine infusion was associated with decreased VAS pain scores, decreased need for postoperative analgesic consumption and decreased administration frequency of PCA. The VAS pain scores and administration frequency of PCA were lower in the lidocaine group than the placebo group for the first 24 hours postsurgery, and fentanyl consumption was lower in the lidocaine group than the placebo group for the first 12 hours postsurgery. The satisfaction scores regarding pain control and the overall recovery process were significantly higher in the lidocaine group than the placebo group.
Subtotal gastrectomy is frequently associated with persistent postoperative discomfort and distress for the patient and, consequently, a late discharge from hospital.3 In our study, despite the use of postoperative PCA and rescue analgesics, the VAS score in the placebo group was elevated during the first 12 hours postsurgery by more than 40 mm, which indicates that postoperative pain after subtotal gastrectomy is substantial.
Perioperative pain has traditionally been managed using opioid analgesics, but opioids are known to increase the incidence of side effects, especially respiratory depression, nausea, vomiting and sedation.5,6 Moreover, development of acute tolerance caused by excessive use of potent opioids may actually increase postoperative pain.12 Therefore, adjuvant therapy to reduce the use of opioids is necessary in patients who have undergone subtotal gastrectomy and experienced extensive tissue trauma and pronounced postoperative pain. These adjuvant therapies include infusion of local anesthetics into the surgical wound, nonsteroidal anti-inflammatory drugs and epidural analgesia using local anesthetics.
Systemic lidocaine may provide an alternative approach to control pain and to reduce opioid consumption for patients after subtotal gastrectomy. Systemic lidocaine has been reported to be as effective as epidural anesthesia in patients undergoing laparoscopic colorectal resection and open colectomy in terms of bowel function.13,14 Intravenous lidocaine infusion also is as effective as intraperitoneal instillation for reducing pain and fentanyl consumption in patients undergoing laparoscopic appendectomy.11
There have been many clinical studies about the use of intraoperative intravenous lidocaine infusion and whether it reduces postoperative pain intensity or the need for analgesic medication; however, the results of these studies have been conflicting for various surgeries.9–11,15,16
Our results are consistent with those of previous studies in which intravenous lidocaine was found to improve postoperative analgesia.9–11,16 Intraoperative lidocaine infusion reduced the postoperative pain and amount of analgesia requested in the postoperative anesthesia care unit in patients who underwent laparoscopic abdominal gynecologic surgery.16
Systemic lidocaine improves postoperative quality of recovery in patients undergoing outpatient laparoscopy. Patients who received lidocaine had less opioid consumption, which translated to a better quality of recovery.9 Similarly, our group reported that intravenous lidocaine reduced postoperative pain intensity, fentanyl consumption and the administration frequency of PCA measured by the number of button pushes in the first 12 hours after inguinal herniorrhaphy.10 Contrary to our findings, some studies have failed to demonstrate a significant analgesic effect of intravenous lidocaine during the postoperative period.15,17,18 Martin and colleagues17 demonstrated that intravenous lidocaine offered no beneficial effect for patients with postoperative analgesia and morphine consumption after total hip arthroplasty. Intravenous lidocaine also did not improve postoperative pain and its related outcomes in patients undergoing laparoscopic renal surgery and abdominal hysterectomy.15,18
The analgesic property of systemic lidocaine can be explained by blockade of neuronal conduction at the surgical wound site, blunting the neurogenic response, and by its anti-inflammatory property.8 Sodium channel blockade of lidocaine causes inhibition of spontaneous and evoked neuronal activity, which reduces neuronal hyperactivity, enhancing postoperative analgesia.19 The analgesic effect of lidocaine can persist even after the reduction of its plasma level. In our study, the reduction of the VAS pain scores, the administration frequency of PCA and the total fentanyl consumption persisted until 12 hours postsurgery. This noticeable prolongation of the analgesic effect beyond the infusion time and plasma half-life20 indicates that systemic lidocaine impacts targets other than voltage-gated sodium channels, which may be related to the prevention of central or peripheral hypersensitivity or the inhibition of the NMDA receptors.21
Lidocaine also has significant anti-inflammatory property, reducing the release of cytokines by inhibiting neutrophil activation. Moreover, lidocaine is known to suppress lymphocyte proliferation and reduce production of both pro- and anti-inflammatory cytokines, which influence acute-phase inflammation reactions.22,23 Our study evaluated the concentration of CRP as an acute phase reactant protein, which shows a positive correlation with the severity of inflammation.24 C-reactive protein increases in the postoperative period, peaks at 2–3 days postsurgery and then returns to normal after 2 weeks.25,26 We noted an increase in CRP after subtotal gastrectomy. In addition, we found that the level of CRP was significantly lower at postoperative day 3 in the lidocaine group than in the placebo group. This significant difference between the groups indicates that systemic lidocaine attenuates the impact of the surgical trauma in terms of anti-inflammatory effect. In contrast to our study, other studies have reported no significant change in CRP values after laparoscopic renal surgery and laparoscopic colectomy.18,27 This lack of significant changes in CRP values may indicate that these types of surgery are less invasive than subtotal gastrectomy, which suggests a benefit from systemic lidocaine in subtotal gastrectomy.
It is difficult to report objective observations of subjective expression of pain, which is an intensely personal experience. Because VAS scores are estimated by patients, objective evaluation of pain may be ambiguous. Therefore, we used computerized PCA for more accurate evaluations of pain. We instructed the patients to press the button of the PCA device to express pain, which increases the objectivity in evaluating pain. In our study, the total administration frequency of PCA derived from the computerized PCA device was 36% less in the lidocaine group than the placebo group, which indicates objectively that the group receiving intraoperative intravenous lidocaine experienced better patient satisfaction in terms of pain control.10
Limitations
Our study had some limitations. We did not measure the concentration of lidocaine. The measurement of the concentration of lidocaine in the blood would be a safe procedure contributing to the understanding of the pharma-cokinetics of lidocaine and its systemic effects. However, we used a smaller amount and a shorter duration of lidocaine than that used in previous studies in which the lidocaine did not reach a toxic concentration and in which there were no side effects reported. In addition, plasma cytokine levels of proinflammatory and anti-inflammatory interleukins were not measured in this study; these markers of inflammatory response might have been more sensitive.
Some advantages of the present study are worth highlighting. All surgeries were performed by the same surgical team to minimize the differences in tissue handling. Furthermore, all the observations were performed by a single observer to eliminate any interobserver variability. Thus, we can assume that the difference in pain relief reflects only the effectiveness of the antinociceptive measures.
Conclusion
Lidocaine infusion is not only effective, but it is also feasible and safe when administered in appropriate dosages.
Acknowledgements
This work was supported by the 2012 Inje University research grant. Trial registration: ACTRN12612000545864.
Footnotes
Competing interests: None declared.
Contributors: J.H. Yon, H. Kang, J.M. Park and H.S. Yang designed the study. J.H. Yon and H. Kang acquired the data, which J.H. Yon, H. Kang, G.J. Choi and J.M. Park analyzed. J.H. Yon, H. Kang and G.J. Choi wrote the article, which G.J. Choi, H. Kang, J.M. Park and H.S. Yang reviewed. All authors approved the final version for publication.
References
- 1.Bae JM, Jung KW, Won YJ. Estimation of cancer deaths in Korea for the upcoming years. J Korean Med Sci. 2002;17:611–5. doi: 10.3346/jkms.2002.17.5.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bellows CF, Berger DH. Infiltration of suture sites with local anesthesia for management of pain following laparoscopic ventral hernia repairs: a prospective randomized trial. JSLS. 2006;10:345–50. [PMC free article] [PubMed] [Google Scholar]
- 3.Hwang SI, Kim HO, Yoo CH, et al. Laparoscopic-assisted distal gastrectomy versus open distal gastrectomy for advanced gastric cancer. Surg Endosc. 2009;23:1252–8. doi: 10.1007/s00464-008-0140-5. [DOI] [PubMed] [Google Scholar]
- 4.Yano H, Monden T, Kinuta M, et al. The usefulness of laparoscopy-assisted distal gastrectomy in comparison with that of open distal gastrectomy for early gastric cancer. Gastric cancer. 2001;4:93–7. doi: 10.1007/pl00011730. [DOI] [PubMed] [Google Scholar]
- 5.Junger A, Klasen J, Benson M, et al. Factors determining length of stay of surgical day-case patients. Eur J Anaesthesiol. 2001;18:314–21. doi: 10.1046/j.0265-0215.2000.00837.x. [DOI] [PubMed] [Google Scholar]
- 6.Pavlin DJ, Rapp SE, Polissar NL, et al. Factors affecting discharge time in adult outpatients. Anesth Analg. 1998;87:816–26. doi: 10.1097/00000539-199810000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Koppert W, Ostermeier N, Sittl R, et al. Low-dose lidocaine reduces secondary hyperalgesia by a central mode of action. Pain. 2000;85:217–24. doi: 10.1016/s0304-3959(99)00268-7. [DOI] [PubMed] [Google Scholar]
- 8.Hollmann MW, Durieux ME. Local anesthetics and the inflammatory response: A new therapeutic indication? Anesthesiology. 2000;93:858–75. doi: 10.1097/00000542-200009000-00038. [DOI] [PubMed] [Google Scholar]
- 9.De Oliveira GS, Jr, Fitzgerald P, Streicher LF, et al. Systemic lidocaine to improve postoperative quality of recovery after ambulatory laparoscopic surgery. Anesth Analg. 2012;115:262–7. doi: 10.1213/ANE.0b013e318257a380. [DOI] [PubMed] [Google Scholar]
- 10.Kang H, Kim BG. Intravenous lidocaine for effective pain relief after inguinal herniorrhaphy: a prospective, randomized, double-blind, placebo-controlled study. J Int Med Res. 2011;39:435–45. doi: 10.1177/147323001103900211. [DOI] [PubMed] [Google Scholar]
- 11.Kim TH, Kang H, Hong JH, et al. Intraperitoneal and intravenous lidocaine for effective pain relief after laparoscopic appendectomy: a prospective, randomized, double-blind, placebo-controlled study. Surg Endosc. 2011;25:3183–90. doi: 10.1007/s00464-011-1684-3. [DOI] [PubMed] [Google Scholar]
- 12.Jin FL, Chung F. Postoperative pain — a challenge for anaesthetists in ambulatory surgery. Can J Anaesth. 1998;45:293–6. doi: 10.1007/BF03012017. [DOI] [PubMed] [Google Scholar]
- 13.Swenson BR, Gottschalk A, Wells LT, et al. Intravenous lidocaine is as effective as epidural bupivacaine in reducing ileus duration, hospital stay, and pain after open colon resection: a randomized clinical trial. Reg Anesth Pain Med. 2010;35:370–6. doi: 10.1097/AAP.0b013e3181e8d5da. [DOI] [PubMed] [Google Scholar]
- 14.Wongyingsinn M, Baldini G, Charlebois P, et al. Intravenous lidocaine versus thoracic epidural analgesia: a randomized controlled trial in patients undergoing laparoscopic colorectal surgery using an enhanced recovery program. Reg Anesth Pain Med. 2011;36:241–8. doi: 10.1097/AAP.0b013e31820d4362. [DOI] [PubMed] [Google Scholar]
- 15.Bryson GL, Charapov I, Krolczyk G, et al. Intravenous lidocaine does not reduce length of hospital stay following abdominal hysterectomy. Can J Anaesth. 2010;57:759–66. doi: 10.1007/s12630-010-9332-2. [DOI] [PubMed] [Google Scholar]
- 16.Grady P, Clark N, Lenahan J, et al. Effect of intraoperative intravenous lidocaine on postoperative pain and return of bowel function after laparoscopic abdominal gynecologic procedures. AANA J. 2012;80:282–8. [PubMed] [Google Scholar]
- 17.Martin F, Cherif K, Gentili ME, et al. Lack of impact of intravenous lidocaine on analgesia, functional recovery, and nociceptive pain threshold after total hip arthroplasty. Anesthesiology. 2008;109:118–23. doi: 10.1097/ALN.0b013e31817b5a9b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wuethrich PY, Romero J, Burkhard FC, et al. No benefit from perioperative intravenous lidocaine in laparoscopic renal surgery: a randomised, placebo-controlled study. Eur J Anaesthesiol. 2012;29:537–43. doi: 10.1097/EJA.0b013e328356bad6. [DOI] [PubMed] [Google Scholar]
- 19.Amir R, Argoff CE, Bennett GJ, et al. The role of sodium channels in chronic inflammatory and neuropathic pain. J Pain. 2006;7(5 Suppl 3):S1–29. doi: 10.1016/j.jpain.2006.01.444. [DOI] [PubMed] [Google Scholar]
- 20.Rowland M, Thomson PD, Guichard A, et al. Disposition kinetics of lidocaine in normal subjects. Ann N Y Acad Sci. 1971;179:383–98. doi: 10.1111/j.1749-6632.1971.tb46915.x. [DOI] [PubMed] [Google Scholar]
- 21.Petrenko AB, Yamakura T, Baba H, et al. The role of N-methyl-D-aspartate (NMDA) receptors in pain: a review. Anesth Analg. 2003;97:1108–16. doi: 10.1213/01.ANE.0000081061.12235.55. [DOI] [PubMed] [Google Scholar]
- 22.MacGregor RR. The effect of anti-inflammatory agents and inflammation on granulocyte adherence. Evidence for regulation by plasma factors. Am J Med. 1976;61:597–607. doi: 10.1016/0002-9343(76)90137-6. [DOI] [PubMed] [Google Scholar]
- 23.MacGregor RR, Thorner RE, Wright DM. Lidocaine inhibits granulocyte adherence and prevents granulocyte delivery to inflammatory sites. Blood. 1980;56:203–9. [PubMed] [Google Scholar]
- 24.Cole DS, Watts A, Scott-Coombes D, et al. Clinical utility of perioperative C-reactive protein testing in general surgery. Ann R Coll Surg Engl. 2008;90:317–21. doi: 10.1308/003588408X285865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aronsen KF, Ekelund G, Kindmark CO, et al. Sequential changes of plasma proteins after surgical trauma. Scand J Clin Lab Invest Suppl. 1972;124:127–36. doi: 10.3109/00365517209102760. [DOI] [PubMed] [Google Scholar]
- 26.Halevy A, Lin G, Gold-Deutsch R, et al. Comparison of serum C-reactive protein concentrations for laparoscopic versus open cholecystectomy. Surg Endosc. 1995;9:280–2. doi: 10.1007/BF00187768. [DOI] [PubMed] [Google Scholar]
- 27.Kaba A, Laurent SR, Detroz BJ, et al. Intravenous lidocaine infusion facilitates acute rehabilitation after laparoscopic colectomy. Anesthesiology. 2007;106:11–8. doi: 10.1097/00000542-200701000-00007. discussion 15–6. [DOI] [PubMed] [Google Scholar]