Abstract
Background
Periprosthetic femoral fracture after total hip arthroplasty (THA) is an increasing clinical problem and a challenging complication to treat surgically. The aim of this retrospective study was to review the treatment of periprosthetic fractures and the complication rate associated with treatment at our institution.
Methods
We reviewed the cases of patients with periprosthetic femoral fractures treated between January 2004 and June 2009. We used the Vancouver classification to assess fracture types, and we identified the surgical interventions used for these fracture types and the associated complications.
Results
We treated 45 patients with periprosthetic femoral fractures during the study period (15 men, 30 women, mean age 78 yr). Based on Vancouver classification, 2 patients had AL fractures, 9 had AG, 15 had B1, 24 had B2, 2 had B3 and 4 had C fractures. Overall, 82% of fractures united with a mean time to union of 15 (range 2–64) months. Fourteen patients (31%) had complications; 11 of them had a reoperation: 6 to treat an infection, 6 for nonunion and 2 for aseptic femoral component loosening.
Conclusion
Periprosthetic fractures are difficult to manage. Careful preoperative planning and appropriate intraoperative management in the hands of experienced surgeons may increase the chances of successful treatment. However, patients should be counselled on the high risk of complications when presenting with this problem.
Abstract
Contexte
La fracture périprothétique du fémur après prothèse totale de la hanche (PTH) est un problème clinique croissant et une complication difficile à traiter chirurgicalement. Le but de cette étude rétrospective était de passer en revue le traitement des fractures périprothétiques et le taux de complications associées à leur traitement dans notre établissement.
Méthodes
Nous avons passé en revue les cas de fractures périprothétiques du fémur traitées entre janvier 2004 et juin 2009. Nous avons utilisé la classification de Vancouver pour évaluer les types de fractures et nous avons recensé les interventions chirurgicales utilisées pour corriger ces types de fractures et leurs complications respectives.
Résultats
Nous avons traité 45 patients victimes de fractures périprothétiques du fémur durant la période de l’étude (15 hommes, 30 femmes, âge moyen de 78 ans). Selon la classification de Vancouver, la répartition des fractures était la suivante : 2 patients avaient une fracture de type AL; 9, un type AG; 15, un type B1; 24, un type B2; 2, un type B3; et 4 un type C. Dans l’ensemble, 82 % des fractures ont repris dans un intervalle de temps moyen de 15 mois (entre 2 et 64 mois). Quatorze patients (31 %) ont présenté des complications; 11 ont dû être réopérés : 6 pour traiter une infection, 6 pour non soudure et 2 pour descellement aseptique de la composante fémorale.
Conclusion
Les fractures périprothétiques sont difficiles à soigner. Une planification préopératoire soigneuse et une prise en charge peropératoire appropriée par des chirurgiens d’expérience peuvent augmenter les chances de succès. Toutefois, il faut informer les patients du risque élevé de complications lorsqu’ils se présentent avec ce type de problème.
Periprosthetic femoral fractures have been classified as occurring either intraoperatively or postoperatively. Intraoperative fractures are an important complication to recognize early.1 Postoperative periprosthetic fractures can occur early or late and are associated with their own set of issues when planning treatment. They may be associated with a loose prosthesis or with bone loss, which can make achieving fixation more difficult. The incidence of periprosthetic fractures is growing and is the third most common reason for reoperation after aseptic loosening and dislocation in patients undergoing total hip arthroplasty (THA).2 The rate of periprosthetic fractures has been estimated to be less than 1% in primary and 4% in revision THAs.3 Cook and colleagues4 assessed 6458 primary cemented THAs from a single unit database and found that the incidence of fracture was 0.8% at 5 years and 3.5% at 10 years. Lindahl and colleagues5 reported an annual incidence of fracture varying from 0.045% to 0.13% for all THAs from the Swedish National Hip Arthroplasty Register between 1979 and 2000; the accumulated incidence was 0.4% for primary and 2.1% for revision THA.5 Risk factors for fracture include age, female sex, osteoporosis, inflammatory arthritis, proximal femoral deformity, longevity of implant, type of implant, revision arthroplasty and implant loosening with associated bone loss.6,7 As the number of patients who undergo THA increases, the burden of disease will continue to increase.
These fractures are challenging, and treatment options vary from nonoperative treatment to component revision with allograft. In addition, a large percentage of these patients are elderly and have multiple medical comorbidities and osteoporotic bone, which can prolong bone healing potential. This makes initial implant stability and subsequent osteointegration less predictable. Surgical management of periprosthetic fractures can result in high complication and reoperation rates.8,9
We performed a retrospective review of patients who sustained a periprosthetic fracture around the femur after THA. This study reports on the results of treatment and complication rates at our institution.
Methods
We retrospectively reviewed the cases of all patients admitted to The Ottawa Hospital with a diagnosis of a periprosthetic femoral fracture between January 2004 and June 2009. Patients with pathological fractures were excluded from the study. We also excluded patients with intraoperative fractures from the data analysis, as they were treated at the time of the primary THA. We collected data for the remaining patients from the patients’ charts, hospital charts and picture archiving and communication system.
We determined the primary indication for joint replacement and the type of fixation used. We determined fracture types using the Vancouver classification. All fractures were treated surgically with either open reduction and internal fixation (ORIF) or a revision prosthesis and ORIF.
Results
Sixty-three patients were treated during our study period (24 men and 39 women with a mean age of 78 [range 46–97] yr). Of these patients, 7 had intraoperative fractures and were excluded from our analysis, 3 passed away within 3 months of surgical treatment and 8 were lost to follow-up, leaving 45 patients (15 men and 30 women with a mean age of 78 [range 46–97] yr) for analysis.
The primary indication for joint replacement was osteoarthritis in 31 patients, hip fracture in 13 patients and rheumatoid arthritis in 1 patient (Table 1). The type of fixation used at the time of primary THA/hemiarthroplasty was cemented in 13 (29%) patients and uncemented in 30 (67%) patients; the remaining 2 (4%) patients experienced fractures of a revision prosthesis.
Table 1.
Primary diagnosis
| Group | Men | Women | Total |
|---|---|---|---|
| OA | 12 | 19 | 31 |
| RA | 1 | 0 | 1 |
| Fracture | 2 | 11 | 13 |
OA = osteoarthritis; RA = rheumatoid arthritis.
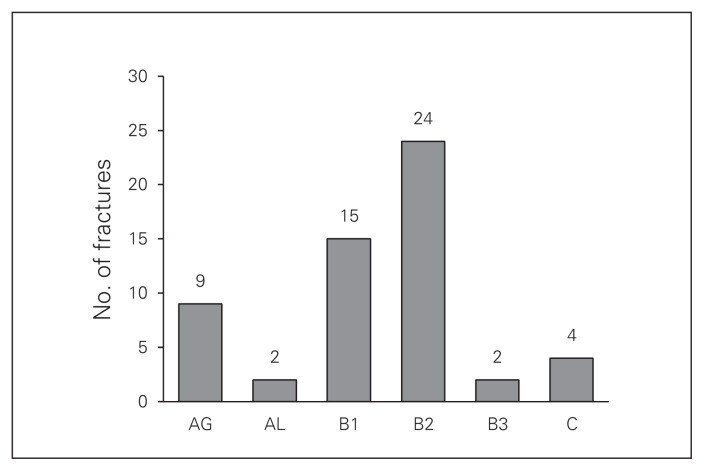
Based on the Vancouver classification, 2 patients had AL fractures, 9 had AG, 15 had B1, 24 had B2, 2 had B3 and 4 had C type fractures (Fig. 1). Revision arthroplasty and ORIF was the treatment of choice for 27 patients, and ORIF alone was used to treat 18 patients. Of the 18 who underwent ORIF, 9 were supplemented with a strut allograft. Autogenous bone graft was used only in the revision arthroplasty setting. Open reduction and internal fixation was the sole treatment in 10 of 11 patients with B1 fractures, whereas 20 of 21 patients with B2 fractures were treated with revision and ORIF. At the time of femoral revision, 24 of the 27 revisions consisted of an un-cemented prosthesis. Type C fractures were treated with ORIF only (Table 2 and Fig. 2). Of the 18 patients whose fractures were treated with ORIF alone, 8 consisted of plate fixation, 6 had been fixed with a plate and strut allograft construct, 3 with cerclage wires and 1 with strut allograft and wires.
Fig. 1.
Distribution of fracture type, Vancouver classification.
Table 2.
Treatment type and Vancouver classification
| Treatment type | AL, n = 1 | AG, n = 7 | B1, n = 11 | B2, n = 21 | B3, n = 1 | C, n = 4 |
|---|---|---|---|---|---|---|
| Revision and ORIF | 1 | 4 | 1 | 20 | 1 | 0 |
| ORIF | 0 | 3 | 10 | 1 | 0 | 4 |
ORIF = open reduction and internal fixation.
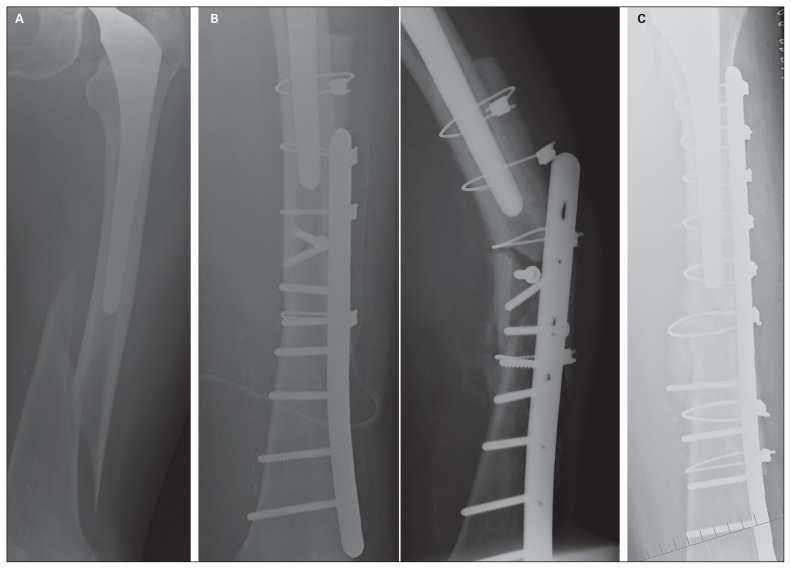
Fig. 2.
(A) Radiograph of an 85-year-old woman 3 years after left total hip arthroplasty with a type C fracture. (B) Postoperative radiographs taken (left) immediately after open reduction and internal fixation with allograft and cerclage plate and (right) after 3 months, showing failure. (C) Revised internal fixation showing proper spanning of the fracture more proximally.
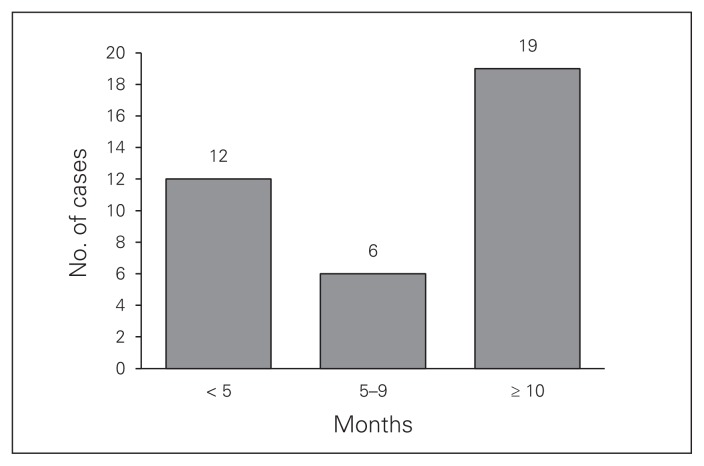
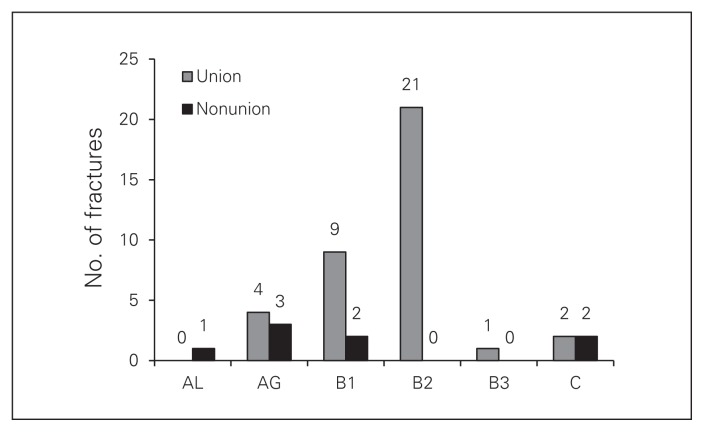
Thirty-seven of the 45 periprosthetic fractures (82%) achieved union with a mean time to union of 15 (range 2–64) months (Fig. 3). All 24 B2 fractures achieved union. The 8 nonunions comprised 4 type A fractures, 2 B1 fractures and 2 C fractures (Fig. 4).
Fig. 3.
Distribution of patients according to time of radiographic union (mo).
Fig. 4.
Fracture type versus outcome (union/nonunion).
Fourteen (31%) patients experienced complications: 6 had deep infections, 6 had nonunions and 2 had aseptic femoral loosening. Eleven of the 14 complications were treated with reoperation. Of the 6 patients with deep infections, 4 were successfully treated with irrigation débridement and IV antibiotics, 2 went on to nonunion and 1 required an amputation. Of the nonseptic failures, 6 patients experienced nonunions and 2 had aseptic loosening of femoral prostheses; 5 of these patients proceeded to revision surgery at a mean time of 3 months (range 2 wk to 10 mo). Three patients did not have reoperations owing to medical comorbidities.
Discussion
Patients presenting with a periprosthetic fracture after THA is a difficult clinical problem to manage. The incidence of these fractures is rising given the increasing number of patients undergoing THA, the rise in the number of revision THAs performed, the increasing life expectancy and the increased risk of falls in the elderly population. Therefore, orthopedic surgeons will probably encounter more patients presenting with this problem in the future.
Patients with periprosthetic fractures carry significant risks once they present to hospital. In one study, 1-year mortality in patients with periprosthetic fractures is similar to that in patients with hip fractures (11%).10 In a study from New Zealand,11 232 patients underwent revision for periprosthetic femur fractures and were compared with a similar group undergoing revision for aseptic loosening. The periprosthetic group had higher mortality and lower functional outcome scores than those in the aseptic loosening group.11
The use of the Vancouver classification system offers a good approach to the treatment of these fractures.12–14 This system aims to provide a guide to treatment based on the fracture pattern, implant stability and associated bone loss. We follow this treatment algorithm set out by previous authors.15 Based on this classification, treatment most commonly involves either ORIF or revision THA. It is important to distinguish between B1 and B2 fractures, as failure to recognize a loose implant increases the chance of failure of fixation and leads to revision surgery. In our series, patients with B2 fractures treated with revision arthroplasty had the best chance of avoiding reoperation and had the lowest complication rate. This should be carefully scrutinized both preoperatively and intraoperatively. There are now many options of revision modular prostheses available to help the surgeon.
Similar to other series, we treated most B1 and C fractures (14 of 15) with ORIF alone. We were able to achieve union with our index surgery in only 11 of 15 patients (73%). Of these 15 patients who underwent ORIF alone, 12 had adequate fixation. The 3 patients whose fractures failed did not adhere to the principles of periprosthetic fracture management. A C-type fracture failed because the plate did not span the prosthesis, which led to a stress riser between the stem tip and the proximal plate (Fig. 2). Extensive periosteal stripping and anterior plating with insufficient cortical purchase was the cause of failure in 1 patient with a B1 fracture. In another patient with a B1 fracture, a lateral based plate was used; however, it did not have bicortical fixation distally, and this led to the formation of a pseudarthrosis. In 1 patient with a C fracture, fixation was adequate but the patient’s postoperative course was complicated by an extensive infection, and the decision to perform an above-knee amputation was made given the medical comorbidities and rehabilitation goals.
Patients with these injuries are often not ideal, healthy candidates for surgery. Many factors, including medical comorbidities, osteoporotic bone, tissue that has previously undergone operative treatment, achievement of proximal fixation around a well-fixed femoral stem, poor biology and decreased healing potential, can make treatment more difficult. Modern treatment options can help but do not guarantee success. Locking plate technology and hybrid plate and cable systems are now available from several implant companies. Cortical onlay strut grafts and osteobiologics can help with bone healing.16 Some authors have reported promising results with surgery.17,18 Despite these modern techniques, failure rates remain relatively high in most series.9 In particular, periprosthetic fractures (B1 and C) treated with ORIF still have significant failure rates (18%–33%).9,19
In our study, the fracture patterns that were most likely to require revision or even multiple revisions were B1 and C fractures. Failures in these patients were either due to unrecognized prosthetic loosening and/or suboptimal internal fixation. These findings are somewhat similar to those of Lindahl and colleagues,6 who reported a higher risk of failure, with B1 fractures representing 44% of their failures in a series of 1049 patients. The need for specialized care is also reflected by our failures in C type fractures, which were mainly due to poor implant fixation technique (Fig. 2). Similarly, others have recommended that these patients be referred for subspecialty care (arthroplasty or trauma) to minimize the risk of reoperation.8
Unlike typical femur fractures, time to union of periprosthetic fractures will often be prolonged; our average time to radiographic union was 15.3 months, and 19 of 37 periprosthetic fractures took more than 10 months to unite. In another study on periprosthetic fractures treated with ORIF, 20 of 66 patients had no great signs of fracture union 6 months postoperatively.9 This is in sharp contrast to nonprosthetic femur fractures, which have been reported to unite by 3 months.20 When managing patients with delayed union and minimal pain who show no signs of implant failure, the risks associated with reoperation must be weighed against those associated with close observation.
Although our overall complication rate of 31% (14 of 45) is high, it is consistent with that reported in the literature (26%–43%).9,21 Infection and nonunion were the most common complications in our series. When infections were adequately eradicated, the fractures usually went on to attain union. However, patients often had to have multiple operations, and 1 patient with an infected nonunion ultimately needed an above-knee amputation.
Conclusion
Patients presenting with periprosthetic fractures are at high risk for complications associated with surgical treatment. These fractures should be assessed individually, and the optimal treatment plan should be made in accordance with the bone stock quality, stem stability, location of the fracture and patient expectations. The complication rate remains high in our institution despite modern treatment options.
Footnotes
This work was previously presented in poster format at the Canadian Orthopaedic Association Annual Meeting, 2011.
Competing interests: None declared.
Contributors: All authors designed the study. N. Holder acquired the data, which all authors analyzed. N. Holder, S. Papp and P.E. Beaulé wrote the article, which all authors reviewed and approved for publication.
References
- 1.Davidson D, Pike J, Garbuz D, et al. Intraoperative periprosthetic fractures during total hip arthroplasty. Evaluation and management. J Bone Joint Surg Am. 2008;90:2000–12. doi: 10.2106/JBJS.H.00331. [DOI] [PubMed] [Google Scholar]
- 2.Lindahl H, Garellick G, Regnér H, et al. Three hundred and twenty-one periprosthetic femoral fractures. J Bone Joint Surg Am. 2006;88:1215–22. doi: 10.2106/JBJS.E.00457. [DOI] [PubMed] [Google Scholar]
- 3.Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am. 1999;30:183–90. doi: 10.1016/s0030-5898(05)70073-0. [DOI] [PubMed] [Google Scholar]
- 4.Cook RE, Jenkins PJ, Walmsley PJ, et al. Risk factors for periprosthetic fractures of the hip: a survivorship analysis. Clin Orthop Relat Res. 2008;466:1652–6. doi: 10.1007/s11999-008-0289-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lindahl H, Malchau H, Herberts P, et al. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty. 2005;20:857–65. doi: 10.1016/j.arth.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 6.Lindahl H, Malchau H, Odén A, et al. Risk factors for failure after treatment of a periprosthetic fracture of the femur. J Bone Joint Surg Br. 2006;88:26–30. doi: 10.1302/0301-620X.88B1.17029. [DOI] [PubMed] [Google Scholar]
- 7.Franklin J, Malchau H. Risk factors for periprosthetic femoral fracture. Injury. 2007;38:655–60. doi: 10.1016/j.injury.2007.02.049. [DOI] [PubMed] [Google Scholar]
- 8.Matharu GS, Pynsent PB, Dunlop DJ, et al. Clinical outcome following surgical intervention for periprosthetic hip fractures at a tertiary referral centre. Hip Int. 2012;22:494–9. doi: 10.5301/HIP.2012.9760. [DOI] [PubMed] [Google Scholar]
- 9.Zuurmond RG, van Wijhe W, van Raay JJAM, et al. High incidence of complications and poor clinical outcome in the operative treatment of periprosthetic femoral fractures: an analysis of 71 cases. Injury. 2010;41:629–33. doi: 10.1016/j.injury.2010.01.102. [DOI] [PubMed] [Google Scholar]
- 10.Bhattacharyya T, Chang D, Meigs JB, et al. Mortality after periprosthetic fracture of the femur. J Bone Joint Surg Am. 2007;89:2658–62. doi: 10.2106/JBJS.F.01538. [DOI] [PubMed] [Google Scholar]
- 11.Young SW, Walker CG, Pitto RP. Functional outcome of femoral periprosthetic fracture and revision hip arthroplasty: a matched-pair study from the New Zealand Registry. Acta Orthop. 2008;79:483–8. doi: 10.1080/17453670710015463. [DOI] [PubMed] [Google Scholar]
- 12.Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 13.Masri BA, Meek RMD, Duncan CP. Periprosthetic fractures evaluation and treatment. Clin Orthop Relat Res. 2004;(420):80–95. doi: 10.1097/00003086-200403000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Brady OH, Garbuz DS, Masri BA, et al. The reliability and validity of the Vancouver classification of femoral fractures after hip replacement. J Arthroplasty. 2000;15:59–62. doi: 10.1016/s0883-5403(00)91181-1. [DOI] [PubMed] [Google Scholar]
- 15.Pike J, Davidson D, Garbuz D, et al. Principles of treatment for periprosthetic femoral shaft fractures around well-fixed total hip arthroplasty. J Am Acad Orthop Surg. 2009;17:677–88. doi: 10.5435/00124635-200911000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Buttaro MA, Farfalli G, Paredes Núñez M, et al. Locking compression plate fixation of Vancouver type-B1 periprosthetic femoral fractures. J Bone Joint Surg Am. 2007;89:1964–9. doi: 10.2106/JBJS.F.01224. [DOI] [PubMed] [Google Scholar]
- 17.Ricci WM, Bolhofner BR, Loftus T, et al. Indirect reduction and plate fixation, without grafting, for periprosthetic femoral shaft fractures about a stable intramedullary implant. Surgical technique. J Bone Joint Surg Am. 2006;88(Suppl 1 Pt 2):275–82. doi: 10.2106/JBJS.F.00327. [DOI] [PubMed] [Google Scholar]
- 18.Chakravarthy J, Bansal R, Cooper J. Locking plate osteosynthesis for Vancouver Type B1 and Type C periprosthetic fractures of femur: a report on 12 patients. Injury. 2007;38:725–33. doi: 10.1016/j.injury.2007.02.038. [DOI] [PubMed] [Google Scholar]
- 19.Froberg L, Troelsen A, Brix M. Periprosthetic Vancouver type B1 and C fractures treated by locking-plate osteosynthesis: fracture union and reoperations in 60 consecutive fractures. Acta Orthop. 2012;83:648–52. doi: 10.3109/17453674.2012.747925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Winquist RA, Hansen ST, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am. 1984;66:529–39. [PubMed] [Google Scholar]
- 21.Corten K, Vanrykel F, Bellemans J, et al. An algorithm for the surgical treatment of periprosthetic fractures of the femur around a well-fixed femoral component. J Bone Joint Surg Br. 2009;91:1424–30. doi: 10.1302/0301-620X.91B11.22292. [DOI] [PubMed] [Google Scholar]