Abstract
Background
Although ischemic stroke is a well-known complication of cardiovascular surgery it has not been extensively studied in patients undergoing noncardiac surgery. The aim of this study was to assess the predictors and outcomes of perioperative acute ischemic stroke (PAIS) in patients undergoing noncardiothoracic, nonvascular surgery (NCS).
Methods
We prospectively evaluated patients undergoing NCS and enrolled patients older than 18 years who underwent an elective, non-daytime, open surgical procedure. Electrocardiography and cardiac biomarkers were obtained 1 day before surgery, and on postoperative days 1, 3 and 7.
Results
Of the 1340 patients undergoing NCS, 31 (2.3%) experienced PAIS. Only age (odds ratio [OR] 2.5, 95% confidence interval [CI] 1.01–3.2, p < 0.001) and preoperative history of stroke (OR 3.6, 95% CI 1.2–4.8, p < 0.001) were independent predictors of PAIS according to multivariate analysis. Patients with PAIS had more cardiovascular (51.6% v. 10.6%, p < 0.001) and noncardiovascular complications (67.7% v. 28.3%, p < 0.001). In-hospital mortality was 19.3% for the PAIS group and 1% for those without PAIS (p < 0.001).
Conclusion
Age and preoperative history of stroke were strong risk factors for PAIS in patients undergoing NCS. Patients with PAIS carry an elevated risk of perioperative morbidity and mortality.
Abstract
Contexte
Même si l’AVC ischémique est une complication bien connue de la chirurgie cardiovasculaire, elle n’a pas fait l’objet d’études approfondies chez les patients soumis à une chirurgie non cardiaque. Le but de cette étude était d’évaluer les prédicteurs et les conséquences de l’AVC ischémique aigu périopératoire (IAPO) chez des patients soumis à une chirurgie non cardiothoracique et non vasculaire (NCNV).
Méthodes
Nous avons évalué de manière prospective les patients soumis à une chirurgie NCNV et inscrit les patients de plus de 18 ans qui subissaient une intervention chirurgicale ouverte non urgente nécessitant une hospitalisation. L’électrocardiogramme et les biomarqueurs cardiaques étaient obtenus 1 jour avant la chirurgie et aux jours 1, 3 et 7 suivant la chirurgie.
Résultats
Parmi les 1340 patients soumis à une chirurgie NCNV, 31 (2,3 %) ont présenté un AVC IAPO. Seuls l’âge (rapport des cotes [RC] 2,5, intervalle de confiance [IC] de 95 % 1,01–3,2, p < 0,001) et des antécédents préopératoires d’AVC (RC 3,6, IC de 95 % 1,2–4,8, p < 0,001) ont été des prédicteurs indépendants de l’AVC IAPO selon l’analyse multivariée. Les patients victimes d’un AVC IAPO avaient davantage de complications cardiovasculaires (51,6 % c. 10,6 %, p < 0,001) et non cardiovasculaires (67,7 % c. 28,3 %, p < 0,001). La mortalité perhospitalière a été de 19,3 % dans le groupe victime d’AVC IAPO et de 1 % chez les patients indemnes d’AVC IAPO (p < 0,001).
Conclusion
L’âge et les antécédents préopératoires d’AVC sont des facteurs de risque importants à l’égard de l’AVC IAPO chez les patients soumis à une chirurgie NCNV. Les patients victimes d’un AVC IAPO sont exposés à un risque élevé de morbidité et de mortalité périopératoires.
Perioperative acute ischemic stroke (PAIS) is devastating to both patients and physicians, particularly when PAIS develops postsurgery in patients with no evidence of cerebrovacsular dysfunction preoperatively. The incidence of PAIS ranges from 0.05% after general surgery to 9% after cardiac surgery and carotid endarterectomy, and PAIS has been associated with substantial perioperative morbidity and mortality.1–10 Cardiopulmonary bypass and carotid endarterectomy induce unique pathophysiology in patients undergoing cardiovascular surgery, and it is inappropriate to assume that the risk factors for PAIS after non-cardiac and nonvascular surgery are the same as those after cardiac or aortic surgery. Several investigators have reported the incidence and risk factors for PAIS among noncardiac surgery patients.11–13 Although PAIS has been reported in approximately 0.08%–3.5% of patients, these figures likely underestimate the true incidence of PAIS owing to inconsistent definition criteria, retrospective study design and the use of an administrative database. A number of risk factors for PAIS, including renal disease, atrial fibrillation, hypertension, prior stroke, valvular disease, congestive heart failure, carotid disease and history of tobacco use, have been identified in these studies. However, relatively few data are available regarding the effect on the cardiac and noncardiac outcome of perioperative PAIS for these surgeries. We performed a prospective study in a cohort of patients undergoing noncardiac and nonvascular surgery to determine incidence, risk factors and outcome of PAIS.
Methods
Study group
After institutional ethics approval, we prospectively obtained data on consecutive adult (≥ 18 yr) patients undergoing noncardiothoracic and nonvascular surgery at Haydarpasa Numune Education and Research Hospital between January 2010 and March 2012.
The collection of patient data included patient age, sex, body mass index (BMI), preoperative medications, American Society of Anesthesiologists (ASA) physical status14 and comorbidities. We used the Revised Cardiac Risk Index (RCRI) for prediction of cardiac risk based on 6 prognostic factors: high-risk type of surgery (defined as intraperitoneal, intrathoracic, or suprainguinal vascular procedures), ischemic heart disease, congestive heart failure, history of cerebrovascular disease, insulin therapy for diabetes and preoperative serum creatinine greater than 176.8 μmol/L (2.0 mg/dL).15 Each of the prognostic factors was assigned 1 point. Anesthetic management, monitoring and other aspects of perioperative management were at the discretion of the attending physician. Electrocardiography and cardiac biomarkers (creatine kinase-MB and troponin I) were evaluated 1 day before surgery, immediately after surgery and on postoperative days 1, 3 and 7. Standard transthoracic echocardiography was performed in all patients using Vivid Three System (Vivid 3 pro, GE Vingmed) before surgery. We measured left ventricle ejection fraction using a modified Simpson rule. Standard, 2-dimensional M-mode and Doppler echocardiographic measurements were obtained for all patients.
The left atrial dimension was measured at end-ventricular systole in the parasternal long axis view according to the American Society of Echocardiography (ASE) recommendations.16 The severity of valvular regurgitation and stenosis was also graded according to the ASE recommendations.17,18 Patients who had any type of rheumatic, myxomatous, ischemic or degenerative valve disease with moderate or greater valve regurgitation and/or stenosis were classified as having heart valve disease.
Patients presenting for surgery who required only local or monitored anesthesia care and who were having daytime surgical procedures were excluded from our analysis. Emergent surgical cases, patients with an ASA classification of 5 (moribund, not expected to live 24 h irrespective of operation) and patients with prosthetic heart valves were also excluded. Vascular and intrathoracic surgeries are not performed in our institution. We included patients undergoing major gastrointestinal surgery (i.e., laparotomy, advanced bowel surgery, gastric surgery), major gynecological cancer surgery (i.e., abdominal hysterectomy, oophorectomy), major open or trans-urethral urological surgery (i.e., cystectomy, radical nephrectomy, total prostatectomy), head and neck surgery and hip or knee arthroplasty. Cardiac risk assessment, preoperative preparation, drug therapy and postoperative follow-up were completed according to current American College of Cardiology/American Heart Association guidelines.19 Patients were followed until discharge after surgery.
Study outcomes
The primary outcome evaluated was PAIS. Secondary outcomes included major cardiovascular and noncardiovascular complications, all-cause mortality and length of postoperative stay in hospital. Acute ischemic stroke was defined as rapidly developing clinical signs of focal disturbance of cerebral function lasting more than 24 hours or leading to death with no apparent cause other than that of vascular origin.20 A focal disturbance lasting less than 24 hours was classified as a transient ischemic attack. The perioperative cardiovascular events were defined as the occurrence of severe arrhythmias requiring treatment, acute heart failure, acute coronary syndrome (i.e., nonfatal acute myocardial infarction or unstable angina), pulmonary thromboembolism, peripheral arterial thromboembolism and nonfatal cardiac arrest. Perioperative myocardial infarction was defined according to the universal definition of myocardial infarction.21 The diagnosis of peripheral arterial embolism was based on clinical, laboratory and radiological findings signifying vascular occlusion with renal, intestinal or limb ischemia.
Noncardiovascular complications were lobar pneumonia confirmed by chest radiograph and requiring antibiotic therapy, respiratory failure requiring intubation for more than 2 days or reintubation, wound infection, bacteremia, acute kidney injury and major and minor bleeding. Acute kidney injury was defined based on the RIFLE (risk, injury, failure, loss of function, end-stage kidney disease) criteria using the maximal change in serum creatinine and estimated glomerular filtration rate during the first 7 postoperative days compared with preoperative baseline values.22 We estimated the glomerular filtration rate using the Chronic Kidney Disease Epidemiology Collaboration formula.23
Major bleeding was defined as fatal or life-threatening bleeding at a critical location (i.e., retroperitoneal, intracranial, intraocular, intraspinal), requiring surgical intervention or administration of at least of 2 units of packed red blood cells. Minor bleeding was defined as all other reported bleeding events not meeting the criteria for a major bleed that did not require hospital admission or transfusion.
Statistical analysis
Data were analyzed using SPSS for Windows version 15 (SPSS Inc). The continuous variables are expressed as means ± standard deviations, and we compared these variables between the groups using a 2-tailed Student t test. We performed nonparametric tests (Mann–Whitney U test) when appropriate. We used the Fisher exact and χ2 tests to compare categorical variables. We considered results to be significant at p < 0.05.
Results
Preoperative characteristics
A total of 1340 patients (mean age 65.8 ± 14 yr) underwent noncardiothoracic, nonvascular surgery during the study period. The incidence of PAIS in the study cohort was 31 of 1340 (2.3%). Of the 31 patients with PAIS, 23 had a stroke and 8 had a transient ischemic attack. The baseline clinical, demographic, laboratory and echocardiographic characteristics are summarized in Table 1, and perioperative characteristics are presented in Table 2. The 2 groups were comparable in terms of sex, tobacco use, BMI, chronic obstructive pulmonary disease, hypertension, hyperlipidemia, chronic renal failure, preoperative cardiac medication and type of surgical procedure.
Table 1.
Preoperative characteristics of the patients
| Characteristic | Group; no. (%)* | p value | ||
|---|---|---|---|---|
| All patients, n = 1340 | PAIS, n = 31 | No PAIS, n = 1309 | ||
| Age, mean ± SD, yr | 65.81 ± 13.97 | 71.58 ± 12.42 | 65.236 ± 11.73 | < 0.001 |
| Sex, male | 712 (53.1) | 20 (64.5) | 692 (52.9) | 0.20 |
| Body mass index, mean ± SD | 28.28 ± 10.42 | 28.12 ± 11.60 | 27.99 ± 10.81 | 0.77 |
| Medical history | ||||
| Current smoking | 166 (12.4) | 3 (9.7) | 163 (12.6) | 0.41 |
| Diabetes mellitus | 335 (25) | 13 (41.9) | 322 (24.6) | 0.028 |
| Hypertension | 742 (55.4) | 22 (71) | 720 (55) | 0.08 |
| Hyperlipidemia | 498 (37.2) | 12 (38.7) | 486 (37.4) | 0.79 |
| Heart failure | 147 (11) | 14 (45.2) | 133 (10.2) | < 0.001 |
| Coronary artery disease | 358 (26.7) | 12 (38.7) | 346 (26.4) | 0.13 |
| History of cerebrovascular disease | 105 (7.8) | 8 (25.8) | 97 (7.4) | < 0.001 |
| Chronic obstructive pulmonary disease | 151 (11.3) | 3 (9.7) | 148 (11.3) | 0.35 |
| Malignancy | 226 (16.9) | 4 (12.9) | 221 (16.9) | 0.56 |
| Chronic renal failure | 103 (7.7) | 4 (12.9) | 99 (7.6) | 0.27 |
| Atrial fibrillation | 206 (15.4) | 17 (54.8) | 189 (14.4) | < 0.001 |
| New York Heart Association functional class | ||||
| 1 | 825 (61.6) | 13 (41.9) | 812 (62) | |
| 2 | 476 (35.5) | 17 (54.8) | 459 (35.1) | 0.07 |
| 3 | 39 (2.9) | 1 (3.2) | 38 (2.9) | |
| 4 | ||||
| Revised cardiac risk index | ||||
| 0 | 178 (13.3) | 1 (3.2) | 177 (13.5) | |
| 1 | 599 (44.7) | 5 (16.1) | 594 (45.4) | < 0.001 |
| 2 | 380 (28.4) | 10 (32.3) | 370 (28.3) | |
| 3 | 166 (12.3) | 14 (45.2) | 152 (11.6) | |
| 4 | 17 (1.3) | 1 (3.2) | 16 (1.2) | |
| ASA status | ||||
| ASA I | 216 (16.1) | 2 (6.5) | 214 (16.4) | |
| ASA II | 677 (50.5) | 7 (22.6) | 670 (51.2) | < 0.001 |
| ASA III | 334 (24.9) | 13 (41.9) | 321 (24.5) | |
| ASA IV | 113 (8.4) | 9 (29.0) | 104 (7.9) | |
| Laboratory tests, mean ± SD | ||||
| C-reactive protein, nmol/L | 181.9 ± 322.9 | 281.9 ± 376.2 | 181.0 ± 320.0 | 0.06 |
| Mean platelet volume, fL | 8.55 ± 6.21 | 8.83 ± 5.94 | 8.51 ± 6.38 | 0.76 |
| Hemoglobin, g/L | 123.0 ± 18.0 | 122.0 ± 17.5 | 124.0 ± 19.0 | 0.60 |
| White blood count, ×109/L | 8.55 ± 4.93 | 8.81 ± 3.11 | 8.58 ± 5.11 | 0.83 |
| Fasting glucose, mmol/L | 6.53 ± 2.10 | 7.14 ± 2.17 | 6.15 ± 2.09 | 0.003 |
| Creatinine, μmol/L | 95.47 ± 114.04 | 108.73 ± 122.88 | 91.05 ± 109.62 | 0.43 |
| Albumin, g/L | 38.0 ± 5.9 | 37.3 ± 6.4 | 38.3 ± 5.8 | 0.35 |
| Echocardiography | ||||
| Left ventricle ejection fraction mean ± SD, % | 57.9 ± 9.8 | 50.6 ± 12.9 | 58.7 ± 8.5 | < 0.001 |
| Left atrium diameter, mean ± SD mm | 37.1 ± 4.8 | 39.9 ± 6.1 | 36.8 ± 4.9 | < 0.001 |
| Pulmonary artery systolic pressure, mean ± SD mm Hg | 27.7 ± 9.8 | 29.9 ± 10.5 | 27.2 ± 9.7 | 0.18 |
| Valvular heart disease | 127 (9.5) | 7 (22.6) | 120 (9.2) | < 0.001 |
ASA = American Society of Anesthesiologists; PAIS = perioperative acute ischemic stroke; SD = standard deviation.
Unless otherwise indicated.
Table 2.
Perioperative characteristics
| Characteristic | Group; no. (%) | p value | ||
|---|---|---|---|---|
| All patients, n = 1340 | PAIS, n = 31 | No PAIS, n = 1309 | ||
| Type of surgery | 0.24 | |||
| General | 558 (41.6) | 12 (38.7) | 546 (41.7) | |
| Urological | 273 (20.3) | 6 (19.4) | 267 (20.4) | |
| Plastics | 75 (5.6) | 2 (6.5) | 73 (5.6) | |
| Gynecological | 74 (5.5) | 3 (9.7) | 71 (5.4) | |
| Orthopedic | 306 (22.8) | 6 (19.4) | 300 (22.9) | |
| Neurological | 38 (2.8) | 1 (3.2) | 37 (2.8) | |
| Ear/nose/throat | 16 (1.2) | 1 (3.2) | 15 (1.1) | |
| Preoperative medications | ||||
| Angiotensin-converting enzyme inhibitor | 431 (32.2) | 13 (41.9) | 418 (31.9) | 0.24 |
| β-blocker | 306 (22.8) | 7 (22.6) | 299 (22.8) | 0.97 |
| Statin | 130 (9.7) | 1 (3.2) | 129 (9.9) | 0.22 |
| Aspirin | 348 (25.9) | 11 (35.5) | 337 (25.7) | 0.22 |
| Calcium inhibitor | 199 (14.8) | 4 (12.9) | 195 (14.9) | 0.76 |
| Diuretics | 87 (6.5) | 2 (6.4) | 85 (6.5) | 0.98 |
PAIS = perioperative acute ischemic stroke.
Predictors of PAIS
Compared to patients without PAIS, those with PAIS were older and more often had diabetes (41.9% v. 24.6%, p = 0.028), heart failure (45.2% v. 10.2%, p < 0.001), history of cerebrovascular disease (25.8% v. 7.4%, p < 0.001) and atrial fibrillation (54.8% v. 14.4%, p < 0.001). They also had higher preoperative ASA class and RCRI scores (Table 1). Compared to patients without PAIS, those who had PAIS had higher left atrium dimensions and reduced left ventricle ejection fraction. They were also more likely to have valvular heart disease at presentation. Univariate analysis revealed that the age, atrial fibrillation, diabetes, heart failure, valvular heart disease, history of cerebrovascular disease, higher ASA and RCRI scores, increased fasting glucose levels, lower left ventricle ejection fraction and greater left atrial diameter were significantly associated with PAIS. However, on multivariate logistic regression analysis, only age (odds ratio [OR] 2.5, 95% confidence interval [CI] 1.01–3.2, p < 0.001) and preoperative history of stroke (OR 3.6, 95% CI 1.2–4.8, p < 0.001) were independent predictors of PAIS.
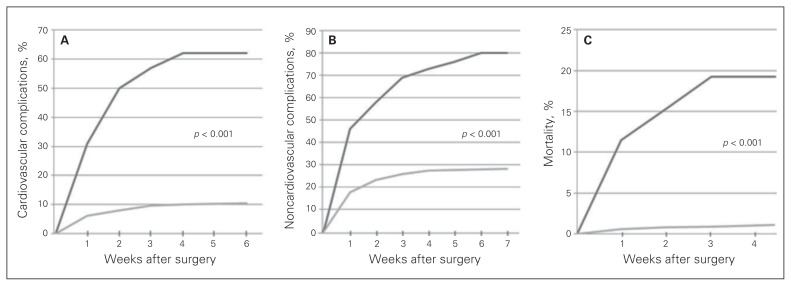
Effect of PAIS on outcome
In-hospital perioperative adverse events and postoperative length of stay data are summarized in Table 3. Postoperative length of stay was prolonged in patients who experienced PAIS (11.4 ± 9.5 v. 8.4 ± 7.7 d, p < 0.001). The most common cardiovascular complications were acute coronary syndrome, acute heart failure and arrhythmia, and the most common noncardiac complications were minor bleeding, wound infection and lobar pneumonia. Patients with PAIS had significantly higher rates of cardiovascular (51.6% v. 10.6%, p < 0.001) and noncardiovascular complications (67.7% v. 28.3%, p < 0.001) than those without PAIS (Fig. 1). Patients with perioperative PAIS also had a greater incidence of in-hospital mortality than those without PAIS (19.3% v. 1%, p < 0.001). After adjustment for age, sex, comorbidities and clinical risk indicators, multivariate analysis showed that PAIS was a significant independent predictor for cardiovascular adverse events (OR 2.87, 95% CI 1.10–5.43, p < 0.001), noncardiovascular complications (OR 1.56, 95% CI 1.15–3.36, p < 0.001), and in-hospital mortality (OR 3.92, 95% CI 1.24–10.40, p < 0.001).
Table 3.
Association of perioperative acute ischemic stroke with adverse perioperative outcomes
| Characteristic | Group; no. (%)* | p value | ||
|---|---|---|---|---|
| All patients, n = 1340 | PAIS, n = 31 | No PAIS, n = 1309 | ||
| Cardiovascular complications | 155 (11.6) | 16 (51.6) | 139 (10.6) | < 0.001 |
| Acute coronary syndrome | 40 (3) | 5 (16.1) | 35 (2.7) | < 0.001 |
| Acute heart failure | 34 (2.5) | 2 (6.5) | 32 (2.4) | 0.23 |
| Severe arrhythmia | 29 (2.2) | 4 (12.9) | 25 (1.9) | < 0.001 |
| Pulmonary embolism | 18 (1.3) | 2 (6.5) | 16 (1.2) | 0.13 |
| Nonfatal cardiac arrest | 12 (0.9) | 2 (6.5) | 10 (0.8) | 0.003 |
| Arterial thromboembolism | 22 (1.6) | 1 (3.2) | 21 (1.6) | 0.22 |
| Noncardiovascular complications | 391 (29.2) | 21 (67.7) | 370 (28.3) | < 0.001 |
| Wound infection | 85 (6.3) | 7 (22.6) | 78 (6) | < 0.001 |
| Respiratory failure | 15 (1.1) | 2 (6.5) | 13 (1) | 0.030 |
| Lobar pneumonia | 24 (1.8) | 3 (9.7) | 21 (1.6) | 0.021 |
| Bacteremia | 14 (1) | 2 (6.5) | 12 (0.9) | 0.024 |
| Minor bleeding | 124 (9.2) | 4 (12.9) | 120 (9.2) | 0.20 |
| Major bleeding | 38 (2.8) | 1 (3.2) | 37 (2.8) | 0.60 |
| Acute kidney injury | 91 (6.8) | 2 (6.5) | 89 (6.8) | 0.72 |
| Length of stay, mean ± SD d | 8.3 ± 8.1 | 11.4 ± 9.5 | 8.4 ± 7.7 | < 0.001 |
| Mortality | 18 (1.4) | 6 (19.3) | 13 (1) | < 0.001 |
PAIS = perioperative acute ischemic stroke; SD = standard deviation.
Unless otherwise indicated.
Fig. 1.
Kaplan–Meier curves for the (A) cardiovascular complications, (B) noncardiovascular complications and (C) in-hospital mortality after noncardiac, nonvascular surgery in patients (black line) with and (grey line) without perioperative acute ischemic stroke.
Discussion
The incidence of PAIS among adult patients undergoing non-cardiac and nonvascular surgery in our study was 2.3%, and PAIS remains a devastating complication following surgery.
The reported incidence of PAIS following noncardiac surgery procedures varies from 0.05% to 7%, depending on the definition of this complication, diagnostic tests, duration of follow-up, study design and the composition of studied populations.24 Previous studies, most of which included a large proportion of cardiac and vascular surgery patients, have identified several risk factors for the development of PAIS after surgery, including advanced age, impaired left ventricular function, long cardiopulmonary bypass time, preoperative renal failure, history of stroke, diabetes and emergent procedures.25–30 However, incidence, predictors and outcome of PAIS in patients undergoing noncardiac and nonvascular surgery are not well studied. Furthermore, most of the previous and current studies are retrospective reviews of administrative databases, and transient ischemic attacks are usually missed owing to inaccurate coding. Kikura and colleagues31 retrospectively evaluated 36 634 consecutive patients after elective noncardiac, noncarotid surgery. Acute stroke occurred in 126 (0.34%) patients during the first 30 days after surgery. Older age and female sex were independent predictors of postoperative stroke. In a retrospective study, Popa and colleagues32 tried to determine the predictors of ischemic stroke in patients aged 65 years and older undergoing hip operations. A total of 1606 patients underwent 1886 hip procedures between 1988 and 2002 and were observed for ischemic stroke for 1 year after their procedure. The rate of stroke at 1 year after hip surgery was 3.9%. In multivariate analysis, history of stroke and hip fracture repair were predictors of postoperative stroke. In another retrospective administrative database study, Bateman and colleagues33 reported an incidence of perioperative stroke of 0.7% after hemicolectomy, 0.2% after hip replacement and 0.6% after lobectomy or segmental lung resection; the incidence increased to 1.0%, 0.3% and 0.8%, respectively, in patients aged 65 years or older. The authors found 4 independent predictors for perioperative stroke: atrial fibrillation, history of stroke, cardiac valvular disease and renal disease. They also showed that PAIS has a profoundly deleterious effect on outcome after surgery, greatly increasing the odds of in-hospital mortality and decreasing the number of hospital-free days. Mashour and colleagues34 presented an analysis of the prospectively collected American College of Surgeons National Surgical Quality Improvement Program database. The authors investigated perioperative stroke in more than 523 000 patients undergoing noncardiac, nonneurologic surgery. They found that the overall incidence of stroke was 0.1% and that perioperative stroke led to an 8-fold increase in 30-day mortality. In another prospective, multicentre study of patients undergoing surgical procedures under general or regional anesthesia in 23 hospitals, Sabaté and colleagues35 investigated major adverse cardiac and cerebrovascular events in 3387 patients and found that the incidence of stroke was 0.4%. The higher PAIS incidence found in the present study versus that reported in the aforementioned studies could be explained by the prospective design of the study, accurate determination of transient ischemic attacks and greater prevalence of comorbidities, such as diabetes, heart failure, atrial fibrillation and history of stroke, in our patients.
A unique finding of our study was that the development of PAIS was associated not only with increased in-hospital mortality and prolonged length of stay in hospital, but also with increased incidence of different types of cardiovascular and noncardiovascular adverse events, such as nonfatal cardiac arrest, acute heart failure, wound infection, lobar pneumonia and respiratory failure. This could be explained in part by the older age and greater prevalence of preoperative comorbidities in patients with PAIS and in part because of the prolonged length of stay for these patients.
Limitations
Although our cohort included a heterogeneous group of patients and procedures, it reflected the practice and outcomes at a single institution and may not be replicable in other settings. Patients undergoing emergent surgery, high-risk surgery (i.e., vascular surgery) and cardiothoracic surgery were not included. Because long-term follow-up after discharge was not performed, the incidence of complications developing after discharge may have been underestimated. Our study cannot establish a causal relation between PAIS and cardiac or noncardiac complications.
Conclusion
Perioperative PAIS is associated with prolonged length of stay in hospital, increased cardiovascular and noncardiovascular adverse events and in-hospital mortality in this cohort of patients undergoing noncardiothoracic, non-vascular surgery. Evaluating the risk:benefit ratio, particularly for elderly patients with a history of stroke or transient ischemic attack, before surgery is essential to optimize care. Physicians must implement diagnostic, therapeutic and procedural measures to modify the peri-operative risk to prevent stroke and minimize morbidity.
Acknowledgements
We thank Fethiye Nihan Demiray for her advice on the statistical analysis section.
Footnotes
Competing interests: None declared.
Contributors: All authors designed the study. M. Biteker acquired and analyzed the data, which K. Kayatas, F.M. Türkmen and C.H. Misirli also analzed. M. Biteker wrote the article, which all authors reviewed and approved for publication.
References
- 1.Hart R, Hindman B. Mechanisms of perioperative cerebral infarction. Stroke. 1982;13:766–73. doi: 10.1161/01.str.13.6.766. [DOI] [PubMed] [Google Scholar]
- 2.Wolman RL, Nussmeier NA, Aggarwal A, et al. Cerebral injury after cardiac surgery: identification of a group at extraordinary risk. Multicenter Study of Perioperative Ischemia Research Group (McSPI) and the Ischemia Research Education Foundation (IREF) Stroke. 1999;30:514–22. doi: 10.1161/01.str.30.3.514. [DOI] [PubMed] [Google Scholar]
- 3.Bull DA, Neumayer LA, Hunter GC, et al. Risk factors for stroke in patients undergoing coronary artery bypass grafting. Cardiovasc Surg. 1993;1:182–5. [PubMed] [Google Scholar]
- 4.Bendszus M, Reents W, Franke D, et al. Brain damage after coronary artery bypass grafting. Arch Neurol. 2002;59:1090–5. doi: 10.1001/archneur.59.7.1090. [DOI] [PubMed] [Google Scholar]
- 5.Hogue CW, Jr, Murphy SF, Schechtman KB, et al. Risk factors for early or delayed stroke after cardiac surgery. Circulation. 1999;100:642–7. doi: 10.1161/01.cir.100.6.642. [DOI] [PubMed] [Google Scholar]
- 6.Stamou SC, Hill PC, Dangas G, et al. Stroke after coronary artery bypass: incidence, predictors, and clinical outcome. Stroke. 2001;32:1508–13. doi: 10.1161/01.str.32.7.1508. [DOI] [PubMed] [Google Scholar]
- 7.Rothwell PM, Slattery J, Warlow CP. A systematic comparison of the risks of stroke and death due to carotid endarterectomy for symptomatic and asymptomatic stenosis. Stroke. 1996;27:266–9. doi: 10.1161/01.str.27.2.266. [DOI] [PubMed] [Google Scholar]
- 8.Bond R, Narayan SK, Rothwell PM, et al. Clinical and radiographic risk factors for operative stroke and death in the European carotid surgery trial. Eur J Vasc Endovasc Surg. 2002;23:108–16. doi: 10.1053/ejvs.2001.1541. [DOI] [PubMed] [Google Scholar]
- 9.Tu JV, Wang H, Bowyer B, et al. Risk factors for death or stroke after carotid endarterectomy: observations from the Ontario Carotid Endarterectomy Registry. Stroke. 2003;34:2568–73. doi: 10.1161/01.STR.0000092491.45227.0F. [DOI] [PubMed] [Google Scholar]
- 10.Cunningham EJ, Bond R, Mehta Z, et al. Long-term durability of carotid endarterectomy for symptomatic stenosis and risk factors for late postoperative stroke. Stroke. 2002;33:2658–63. doi: 10.1161/01.str.0000034397.72390.d3. [DOI] [PubMed] [Google Scholar]
- 11.Landercasper J, Merz BJ, Cogbill TH, et al. Perioperative stroke risk in 173 consecutive patients with a past history of stroke. Arch Surg. 1990;125:986–9. doi: 10.1001/archsurg.1990.01410200044006. [DOI] [PubMed] [Google Scholar]
- 12.Parikh S, Cohen JR. Perioperative stroke after general surgical procedures. N Y State J Med. 1993;93:162–5. [PubMed] [Google Scholar]
- 13.Limburg M, Wijdicks EF, Li H. Ischemic stroke after surgical procedures: clinical features, neuroimaging, and risk factors. Neurology. 1998;50:895–901. doi: 10.1212/wnl.50.4.895. [DOI] [PubMed] [Google Scholar]
- 14.American Society of Anesthesiologists. New classification of physical status. Anesthesiology. 1963;24:111. [Google Scholar]
- 15.Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100:1043–9. doi: 10.1161/01.cir.100.10.1043. [DOI] [PubMed] [Google Scholar]
- 16.Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 17.Zoghbi WA, Enriquez-Sarano M, Foster E, et al. American Society of Echocardiography: recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003;16:777–802. doi: 10.1016/S0894-7317(03)00335-3. [DOI] [PubMed] [Google Scholar]
- 18.Baumgartner H, Hung J, Bermejo J, et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. J Am Soc Echocardiogr. 2009;22:1–23. doi: 10.1016/j.echo.2008.11.029. [DOI] [PubMed] [Google Scholar]
- 19.Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the ACC/AHA Task Force on Practice Guidelines (Writing Committee) Circulation. 2007;116:e418–99. [Google Scholar]
- 20.The World Health Organization. MONICA Project (monitoring of trends and determinants in cardiovascular disease): a major international collaboration. J Clin Epidemiol. 1988;41:105–14. doi: 10.1016/0895-4356(88)90084-4. [DOI] [PubMed] [Google Scholar]
- 21.Thygesen K, Alpert JS, White HD. Universal definition of myocardial infarction. Eur Heart J. 2007;28:2525–38. doi: 10.1093/eurheartj/ehm355. [DOI] [PubMed] [Google Scholar]
- 22.Bellomo R, Ronco C, Kellum JA, et al. Acute renal failure — definition, outcome measures, animal models, fluid therapy and information technology needs. The second international consensus conference of Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204–12. doi: 10.1186/cc2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levey AS, Stevens LA, Schmid CH, et al. CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ng JL, Chan MT, Gelb AW. Perioperative stroke in noncardiac, non-neurosurgical surgery. Anesthesiology. 2011;115:879–90. doi: 10.1097/ALN.0b013e31822e9499. [DOI] [PubMed] [Google Scholar]
- 25.Hedberg M, Boivie P, Engström KG. Early and delayed stroke after coronary surgery — an analysis of risk factors and the impact on short-and long-term survival. Eur J Cardiothorac Surg. 2011;40:379–87. doi: 10.1016/j.ejcts.2010.11.060. [DOI] [PubMed] [Google Scholar]
- 26.Melissano G, Tshomba Y, Bertoglio L, et al. Analysis of stroke after TEVAR involving the aortic arch. Eur J Vasc Endovasc Surg. 2012;43:269–75. doi: 10.1016/j.ejvs.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 27.Dacey LJ, Likosky DS, Leavitt BJ, et al. Perioperative stroke and long-term survival after coronary bypass graft surgery. Ann Thorac Surg. 2005;79:532–6. doi: 10.1016/j.athoracsur.2004.07.027. [DOI] [PubMed] [Google Scholar]
- 28.Karkouti K, Djaiani G, Borger MA, et al. Low hematocrit during cardiopulmonary bypass is associated with increased risk of perioperative stroke in cardiac surgery. Ann Thorac Surg. 2005;80:1381–7. doi: 10.1016/j.athoracsur.2005.03.137. [DOI] [PubMed] [Google Scholar]
- 29.Roach GW, Kanchuger M, Mangano CM, et al. Adverse cerebral outcomes after coronary bypass surgery. Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. N Engl J Med. 1996;335:1857–63. doi: 10.1056/NEJM199612193352501. [DOI] [PubMed] [Google Scholar]
- 30.Stamou SC, Hill PC, Dangas G, et al. Stroke after coronary artery bypass: incidence, predictors, and clinical outcome. Stroke. 2001;32:1508–13. doi: 10.1161/01.str.32.7.1508. [DOI] [PubMed] [Google Scholar]
- 31.Kikura M, Oikawa F, Yamamoto K, et al. Myocardial infarction and cerebrovascular accident following non-cardiac surgery: differences in postoperative temporal distribution and risk factors. J Thromb Haemost. 2008;6:742–8. doi: 10.1111/j.1538-7836.2008.02948.x. [DOI] [PubMed] [Google Scholar]
- 32.Popa AS, Rabinstein AA, Huddleston PM, et al. Predictors of ischemic stroke after hip operation: a population-based study. J Hosp Med. 2009;4:298–303. doi: 10.1002/jhm.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bateman BT, Schumacher HC, Wang S, et al. Perioperative acute ischemic stroke in noncardiac and nonvascular surgery: incidence, risk factors, and outcomes. Anesthesiology. 2009;110:231–8. doi: 10.1097/ALN.0b013e318194b5ff. [DOI] [PubMed] [Google Scholar]
- 34.Mashour GA, Shanks AM, Kheterpal S. Perioperative stroke and associated mortality after noncardiac, nonneurologic surgery. Anesthesiology. 2011;114:1289–96. doi: 10.1097/ALN.0b013e318216e7f4. [DOI] [PubMed] [Google Scholar]
- 35.Sabaté S, Mases A, Guilera N, et al. Incidence and predictors of major perioperative adverse cardiac and cerebrovascular events in non-cardiac surgery. Br J Anaesth. 2011;107:879–90. doi: 10.1093/bja/aer268. [DOI] [PubMed] [Google Scholar]