Abstract
Background
Laparoscopic surgery has become the standard for treating appendicitis. The cosmetic benefits of using single-incision laparoscopy are well known, but its duration, complications and time to recovery have not been well documented. We compared 2 laparoscopic approaches for treating appendicitis and evaluated postoperative pain, complications and time to full recovery.
Methods
We retrospectively reviewed the cases of consecutive patients with appendicitis and compared those who underwent conventional laparoscopic appendectomy (CLA) performed using 3 incisions and those who underwent single-incision laparoscopic appendectomy (SILA). During SILA, the single port was prepared to increase visibility of the operative site.
Results
Our analysis included 688 consecutive patients: 618 who underwent CLA and 70 who underwent SILA. Postsurgical complications occurred more frequently in the CLA than the SILA group (18.1% v. 7.1%, p = 0.018). Patients who underwent SILA returned to oral feeding sooner than those who underwent CLA (median 12 h v. 22 h, p < 0.001). These between-group differences remained significant after controlling for other factors. Direct comparison of only nonperforated cases, which was determined by pathological examination, revealed that SILA was significantly longer than CLA (60 min v. 50 min, p < 0.001). Patients who underwent SILA had longer in-hospital stays than those who underwent CLA (72 v. 55 h, p < 0.001); however, they had significantly fewer complications (3.0% v. 14.4%, p = 0.006).
Conclusion
In addition to its cosmetic advantages, SILA led to rapid recovery and no increase in postsurgical pain or complications.
Abstract
Contexte
La chirurgie laparoscopique est devenue la norme pour le traitement de l’appendicite. Les avantages de la laparoscopie à simple incision au plan esthétique sont bien connus, mais la durée de l’intervention, ses complications et le temps de récupération n’ont pas été adéquatement documentés. Nous avons comparé 2 approches laparoscopiques pour le traitement de l’appendicite et évalué la douleur et les complications postopératoires, de même que le temps de récupération complète.
Méthodes
Nous avons passé en revue de manière rétrospective les dossiers de patients consécutifs atteints d’appendicite et comparé ceux qui ont subi une appendicectomie laparoscopique classique (ALC) à 3 incisions à ceux qui ont subi une appendicectomie laparoscopique à simple incision (ALSI). Durant l’ALSI, l’incision était préparée de manière à améliorer la visibilité du champ opératoire.
Résultats
Notre analyse a inclus 688 patients consécutifs : 618 qui ont subi une ALC et 70, une ALSI. Les complications postopératoires ont été plus nombreuses dans le groupe soumis à l’ALC qu’à l’ALSI (18,1 % c. 7,1 %, p = 0,018). Les patients soumis à l’ALSI ont repris l’alimentation orale plus rapidement que ceux qui avaient subi une ALC (temps médian 12 h c. 22 h, p < 0,001). Ces différences entre les groupes sont demeurées significatives après incorporation d’autres facteurs. La comparaison directe des cas non perforés seulement, révélés par l’examen anatomopathologique, a révélé que l’ALSI a demandé significativement plus de temps que l’ALC (60 min c. 50 min, p < 0,001). Les patients soumis à l’ALSI ont séjourné plus longtemps à l’hôpital que les patients soumis à l’ALC (72 h c. 55 h, p < 0,001); toutefois, ils ont présenté significativement moins de complications (3,0 % c. 14,4 %, p = 0,006).
Conclusion
En plus de ses avantages au plan esthétique, l’ALSI a permis une récupération rapide, sans accroissement de la douleur ou des complications postopératoires.
The benefits of laparoscopic surgery compared with conventional abdominal surgery have been demonstrated, including reduced postoperative pain and morbidity, shorter hospital stays and shorter recovery time for various abdominal surgeries.1–3 Minimally invasive single-port laparoscopic techniques, such as single-incision laparoscopic surgery (SILS) and natural orifice transluminal endoscopic surgery (NOTES) have further improved surgical outcomes, providing virtually scar-free surgery when performed by an experienced surgeon.4 However, several drawbacks have been reported for NOTES, including the need for an additional incision to gain access to the peritoneal cavity, the possibility of perforation leading to serious morbidity, possible longer recovery time and a steep learning curve.4,5
In SILS, all laparoscopic working ports enter the abdominal wall through the same incision. This technique offers a number of advantages in addition to improved cosmetic results, including few complications and rapid patient recovery. Although a review of studies on NOTES procedures found reports of pain and complications equivalent to those of multiport laparoscopic approaches,6 studies have also shown that patients have experienced less pain and fewer complications with SILS,5 including single-port laparoscopic appendectomy (SILA).7 In addition, SILS can be safely converted to conventional laparoscopic surgery at any time during surgery.8
Laparoscopy has become the preferred approach for treating appendicitis, especially in children.9 Appendicitis is one of the most common surgical emergencies, particularly among children, with the risk peaking at the age of 11–12 years, and the lifetime risk is 7%–9%.10 The SILA procedure has been applied in patients of all ages and is increasingly used in a number of surgical centres.11 However, few studies have compared SILA with conventional laparoscopic appendectomy (CLA) using 3 trocars. A recent retrospective study by Chow and colleagues5 reported that SILA is safe and effective. Kim and colleagues8 and Hong and colleagues12 have reported an improvement of SILA that is achieved by creating a single port from a surgical glove, a wound retractor, small trocars and 3-way catheters. We modified this technique to improve surgical site visibility. Our goal was to determine whether SILA had advantages other than cosmetic ones over CLA, including less pain, fewer complications and rapid postsurgical recovery. Our objective was to compare 2 laparoscopic approaches for treating appendicitis and to evaluate postoperative pain, complications and time to full recovery.
Methods
Study design and participants
In this prospective observational study, all patients with acute appendicitis admitted to Taipei Medical University Hospital between February 2008 and October 2010 were considered for laparoscopic surgery. We enrolled consecutive patients who underwent either CLA or SILA. The clinical characteristics and operative outcomes of these patients were retrospectively reviewed and compared. Informed consent to participate in the study was obtained before surgery. The study protocol was reviewed and approved by the Internal Review Board of the hospital.
Preoperative, intraoperative and postoperative methods
Preoperative diagnoses were made by taking a thorough history, performing a physical examination and ordering laboratory tests. Ultrasonography and abdominal computed tomography (CT) were performed if necessary. All SILA procedures were performed by a single surgeon (H.-H.L.), who had previously performed 10 SILA procedures. The CLA procedure had been performed in our hospital for more than 10 years, and all procedures were performed by 3 surgeons (H.-H.L. P.-L.W., W.W.), each of whom had previously performed at least 1000 CLA procedures.
Patients were excluded from undergoing SILA if they had a history of major lower abdominal surgery, septic shock or compromised cardiopulmonary function, in which case creating the pneumoperitoneum under general anesthesia was contraindicated. In addition, we excluded patients with complicated appendicitis who had inflammation that lasted for more than 1 week or who had a palpable tumour mass in the right lower quadrant confirmed by CT. Generalized peritonitis was not considered an exclusion criterion for SILA. Patients younger than 12 years and patients undergoing incidental appendectomy were also excluded from this study. Finally, because CLA was free of charge and covered by our national health insurance system, whereas SILA is not covered by health insurance in Taiwan, some patients opted not to undergo SILA. Because patients themselves chose the procedure, assignment was not random.
Main outcome measures
The main outcomes studied included the duration of surgery, time to resuming oral feeding, length of stay in hospital (LOS), complications and pain. The size of the incision was recorded, and was the same as the diameter of the trocar. We evaluated the level of pain by assessing the total dose of analgesics used within the first 24 hours after surgery. The analgesics, which were administered to patients with pain scores greater than 4.0, were converted to an amount equivalent to 50 mg of intravenous meperidine hydrochloride to simplify and clarify comparisons.
Surgical techniques
The CLA procedure was performed in the usual manner. Patients were placed in a supine position, and their feet were not elevated during surgery. During the operation, the surgeon and assistant stood on the left side of the patient, with the monitor placed on the opposite side. The operation was performed using 3 incisions. A 10 mm umbilical wound was made for movement (in and out) of the 10 mm clip and for removal of the appendix, a 5 mm suprapubic incision was made for insertion of the laparoscopic camera, and a 5 mm right lower abdominal wound served as an assistant port for instruments. A clip was used to occlude the stump of the appendix, and a long-tipped grasper was used to occlude the distal end of the appendix. After transection of the appendix, the wounds were closed with 2–0 polyglactin 910 sutures.
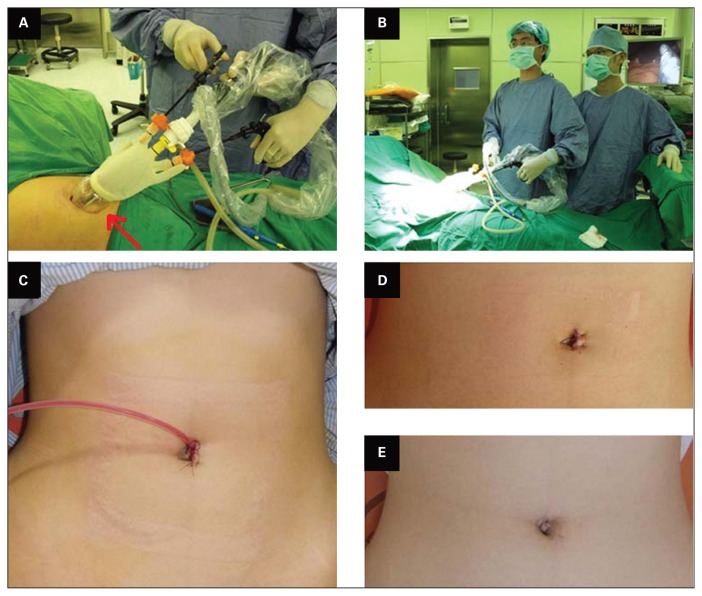
The SILA procedure was performed by applying a modification of a previously described technique.8,12 During the operation, the surgeon and the assistant stood on the left side of the patient, with the monitor placed on the opposite side (Fig. 1B). Under general anesthesia, a port using a 1.5 cm vertical intraumbilical skin incision was created. A surgical glove was used to create a single port, with an extra-small wound retractor (Applied Medical; Fig. 1A). The wound retractor was set up through the 1.5 cm umbilical incision. The surgical glove, attached with 1 trocar and 2 pipes, which served as working channels, was fixed to the outer ring of the wound retractor. The wound retractor and surgical glove were rolled together (Fig. 1A). The transparency between the glove and retractor provided better direct vision of instrument movements, which facilitated the procedure. When abdominal fluid was cloudy or pus-like, a 7 mm Jackson–Pratt drainage tube was inserted through the single umbilical incision in the direction of the pelvic cavity (Fig. 1C).
Fig. 1.
(A) External view of the surgical area during single-incision laparoscopic appendectomy (SILA). The wound retractor is set up through a small umbilical incision. The surgical glove, attached with a reusable trocar and 2 pipes, is fixed to the outer ring of the wound retractor. Note the transparency in the lower portion of the retractor (arrow, bottom left); this aids visibility and placement of the surgical instruments through the small abdominal wound. (B) During SILA, the surgeon and the assistant stand on the left side of the patient with the monitor placed on the opposite side. (C) If drainage is necessary, a drain (Jackson–Pratt drain, 10 mm) can be inserted through the single umbilical incision toward the pelvic cavity. (D) Surgical scar immediately after completion of SILA; this patient had a ruptured appendix, and a drainage tube was inserted. (E)The surgical scar in the same patient 1 year after surgery.
Next, the patient was placed in the Trendelenburg position with the left side of the body rotated down. A clip was used to occlude the stump of the appendix, and a long-tipped grasper was used to occlude the distal end of the appendix. Once the appendix was transected, the surgical glove was detached from the outer ring of the wound retractor. After removing the wound retractor, the umbilical fascia was closed with 2–0 polyglactin 910 sutures. Because the incision was so small and the umbilicus naturally depressed, an additional stitch in the subcutaneous layer was not usually placed (Fig. 1D). To avoid complications after surgery, initially placed drainage tubes were in high proportion among the patients, including some patients in whom 2 drainage tubes were placed in the pelvis and the right side of the abdomen to handle the amount of intra-abdominal pus.
Patients were assessed every 2 hours. If bowel sounds were present postoperatively, the patient was allowed to attempt drinking fluids, and if there was no discomfort solid food was allowed. Patients were discharged once they could resume out-of-bed activities without assistance and if they had no fever or discomfort after eating. Postoperative cosmetic assessment occurred before the patient was discharged. Patient follow-up varied, and we relied on medical records and telephone interviews to determine the occurrence of complications or incision hernias.
Statistical analysis
All statistical assessments were performed using SPSS software version 15.0 (SPSS Inc.). All continuous variables are presented as medians with interquartile ranges (IQRs). We tested the differences between the 2 groups using the nonparametric Mann–Whitney test for non-normal distributions. Categorical variables were summarized as counts with percentages, and we assessed the associations between these variables and the surgical procedure using the Fisher exact test.
To compare the surgeries with adjustment for latent confounders, univariable and multivariable logistic regression models and general linear models were carried out to evaluate complications and oral feeding times, respectively. The results of the logistic regression models are summarized as odds ratios (ORs) with 95% confidence intervals (CIs), and the weight of coefficients (β) with 95% CIs are presented in general linear models. Each variable with results of p < 0.20 in the corresponding univariable model was stepwise-entered into the multivariable model. We considered results to be significant at p < 0.05.
Results
From February 2008 to October 2010, 688 consecutive patients with appendicitis were enrolled in the study. Of these, 70 patients chose SILA and the other 618 patients chose CLA. The demographic and clinical characteristics of participants are summarized in Table 1. Patients in the CLA group were significantly older than those in the SILA group (median 30.5 yr v. 25.0 yr, p = 0.039). The proportion of female patients was significantly higher in the SILA group than in the CLA group (81.4% v. 51.9%, p < 0.001). No significant differences were observed in body mass index between the groups. The time between the appearance of symptoms to hospital admission was longer in the SILA group than the CLA group (median 30 h v. 24 h, p < 0.001). Most patients had no previous major diseases or abdominal surgery; however, 1 patient in the SILA group had glucose-6-phosphate dehydrogenase deficiency and 1 had diabetes mellitus, and 29 patients in the CLA group had cardiovascular disease or other systemic disease. Thus, there was a significant difference in previous major disease histories between the groups (p = 0.012). No patients in the SILA group had previous abdominal surgery, whereas 10% of patients in the CLA group had previous (but not major) abdominal surgery (p = 0.008).
Table 1.
Demographic and clinical characteristics of study patients, by group
| Characteristic | Group; no. (%)* or median [IQR]† | p value | |
|---|---|---|---|
| SILA, n = 70 | CLA, n = 618 | ||
| Age, yr | 25.0 [18.0–32.0] | 30.5 [20.0–40.0] | 0.039 |
| Sex | |||
| Female | 57 (81.4) | 321 (51.9) | < 0.001 |
| Male | 13 (18.6) | 297 (48.1) | |
| BMI | 20.1 [18.3–22.5] | 20.6 [18.2–24.1] | 0.48 |
| Time from appearance of symptoms to hospital admission, h | 30.0 [24.0–48.0] | 24.0 [10.0–48.0] | < 0.001 |
| White blood cell count, × 109/L | 12.4 [8.7–14.6] | 12.3 [9.6–15.1] | 0.48 |
| Neutrophils | 81.1 [74.2–85.8] | 79.1 [70.0–85.6] | 0.15 |
| Previous major clinical disease | |||
| Nil | 68 (97.1) | 589 (95.3) | 0.012 |
| Cardiovascular | 0 (0) | 11 (1.8) | |
| Systemic disease | 0 (0) | 18 (2.9) | |
| Diabetes mellitus | 1 (1.4) | 0 (0) | |
| G6PD | 1 (1.4) | 0 (0) | |
| Previous abdominal surgery | |||
| Nil | 70 (100) | 550 (89.0) | 0.008 |
| Upper abdomen | 0 (0) | 9 (1.5) | |
| Lower abdomen | 0 (0) | 58 (9.4) | |
| Upper and lower abdomen | 0 (0) | 1 (0.2) | |
| Symptoms | |||
| Fever | 25 (35.7) | 174 (28.2) | 0.21 |
| Gastrointestinal upset | 28 (40.0) | 207 (33.5) | 0.29 |
| Diffuse abdominal pain | 8 (11.4) | 20 (3.2) | 0.005 |
| Right lower quadrant pain | 64 (91.4) | 346 (56.0) | < 0.001 |
| Nausea/vomiting | 40 (57.1) | 10 (1.6) | < 0.001 |
BMI = body mass index; CLA = conventional laparoscopic appendectomy; G6PD = glucose-6-phosphate dehydrogenase; IQR = interquartile range; SILA = single incision laparoscopic appendectomy.
Determined by Fisher exact test.
Determined by Mann–Whitney U test.
The number of drainage tubes required was different between the groups: 17.1% of patients in the SILA group received 1 or 2 drains, compared with 8.1% in the CLA group (p = 0.047; Table 2). Sixty-six (10.7%) patients in the CLA group had ruptured (perforated) appendices compared with no patients in the SILA group (p = 0.001). According to pathology results, 70 (11.3%) and 3 (4.3%) patients in the CLA and SILA groups, respectively, had a perforated appendix (p = 0.037). The duration of surgery in the SILA group was significantly longer than that in the CLA group (60 min v. 55 min, p = 0.001). There were no significant differences between the groups with respect to LOS and the total dosage of analgesics (Table 2).
Table 2.
Surgery-related outcomes by group
| Factor | Group; no. (%) or median [IQR] | p value | |
|---|---|---|---|
| SILA, n = 70 | CLA, n = 618 | ||
| Number of drain tubes | |||
| 0 | 58 (82.9) | 568 (91.9) | 0.047 |
| 1 | 12 (17.1) | 47 (7.6) | |
| 2 | 0 (0.0) | 3 (0.5) | |
| Intraoperative findings | |||
| Inflammation | 56 (80.0) | 438 (70.9) | 0.12 |
| Gangrenous | 12 (17.1) | 91 (14.7) | 0.60 |
| Ruptured/perforated appendix | 0 (0.0) | 66 (10.7) | 0.001 |
| Chylous (pus) ascites | 1 (1.4) | 25 (4.0) | 0.50 |
| Abscess/local abscess | 0 (0.0) | 13 (2.1) | 0.38 |
| Adhesion | 0 (0.0) | 30 (4.9) | 0.06 |
| Total dose of analgesic | |||
| None | 44 (62.9) | 405 (65.5) | 0.69 |
| ≥ 50 mg meperidine | 26 (37.1) | 213 (34.5) | |
| Pathology | |||
| Acute appendix | 39 (55.7) | 363 (58.7) | 0.037 |
| Gangrenous appendix | 13 (18.6) | 118 (19.1) | |
| Perforated appendix | 3 (4.3) | 70 (11.3) | |
| Other | 15 (21.4) | 67 (10.8) | |
| Surgery outcomes | |||
| Duration of surgery, min. | 60.0 [55.0–75.0] | 55.0 [40.0–70.0] | 0.001 |
| LOS, h | 60.0 [36.0–84.0] | 58.0 [42.0–70.0] | 0.30 |
| Time to resuming oral feeding, h | 12.0 [8.0–16.0] | 22.0 [17.0–30.0] | < 0.001 |
| Complications | 5 (7.1) | 112 (18.1) | 0.018 |
| Wound infection | 5 (7.1) | 97 (15.7) | 0.07 |
| Ileus | 0 (0.0) | 3 (0.5) | > 0.99 |
| Intra-abdominal abscess | 0 (0.0) | 6 (1.0) | > 0.99 |
| Incision hernia | 2 (2.9) | 4 (0.6) | 0.12 |
CLA = conventional laparoscopic appendectomy; IQR = interquartile range; LOS = length of stay in hospital; SILA = single incision laparoscopic appendectomy.
Approximately 18% of patients in the CLA group had postsurgical complications compared with 7.1% in the SILA group (p = 0.018). The results of our multivariable logistic regression model to investigate factors that might impact the risk of complications are summarized in Table 3. In univariable models, 11 variables reached statistical significance (see the Appendix, Table S1, available at canjsurg.ca). In the multivariable model, the symptom of right lower quadrant pain was excluded owing to colinearity. Pathology results and surgery group reached significance and were the independent influence factors of complications. After controlling for age, sex and other factors using the same conditions, we found that patients who received CLA had a higher risk of complications than those treated with SILA (OR 2.85, p = 0.043); patients with gangrenous appendices (OR 2.24, p = 0.002) and perforated appendices (OR 6.37, p < 0.001) had a significantly higher risk for complications than those with acute appendices; and patients with gastrointestinal (GI) upset symptoms had a higher risk of complications than those without GI upset symptoms (OR 1.66, p = 0.023; Table 3).
Table 3.
Multivariable analyses of factors of complications and time to resuming oral feeding, by logistic regression and general linear models
| Factor | Occurring complications | Oral feeding time | ||
|---|---|---|---|---|
|
|
|
|||
| OR (95% CI) | p value | β (95% CI) | p value | |
| Surgery group, CLA v. SILA | 2.85 (1.03 to 7.87) | 0.043 | 12.83 (9.749 to 15.91) | < 0.001 |
|
| ||||
| Age, yr | 1.00 (0.99 to 1.01) | 0.93 | 0.06 (–0.004 to 0.11) | 0.07 |
|
| ||||
| Sex, male v. female | 0.98 (0.63 to 1.52) | 0.93 | –0.37 (–2.201 to 1.46) | 0.69 |
|
| ||||
| Symptoms of gastrointestinal upset | 1.66 (1.07 to 2.57) | 0.023 | — | — |
|
| ||||
| Symptoms of diffuse abdominal pain | 2.48 (0.95 to 6.46) | 0.06 | 7.64 (3.009 to 12.26) | 0.001 |
|
| ||||
| Pathology | ||||
|
| ||||
| Acute appendix | — | — | — | — |
|
| ||||
| Gangrenous appendix | 2.24 (1.34 to 3.74) | 0.002 | — | — |
|
| ||||
| Perforated appendix | 6.37 (3.58 to 11.34) | < 0.001 | — | — |
|
| ||||
| Other | 0.19 (0.05 to 0.81) | 0.024 | — | — |
|
| ||||
| Neutrophil counts | — | — | 5.46 (0.828 to 10.09) | 0.021 |
|
| ||||
| Operation finding of ruptured appendix (perforated) | — | — | 8.64 (5.362 to 11.92) | < 0.001 |
|
| ||||
| No. of drain tubes | ||||
|
| ||||
| 0 | — | — | — | — |
|
| ||||
| 1 | — | — | 5.13 (1.671 to 8.59) | 0.004 |
|
| ||||
| 2 | — | — | 63.26 (49.590 to 76.92) | < 0.001 |
CI = confidence interval; CLA = conventional laparoscopic appendectomy; OR = odds ratio; SILA = single incision laparoscopic appendectomy.
Patients in the SILA group had a significantly shorter time to resuming oral feeding than those in the CLA group (median 12 h v. 22 h, p < 0.001; Table 2). The differences remained significant in multivariable analysis. The results of the multivariable general linear model to investigate factors that might impact the time to resuming oral feeding are summarized in Table 3. In the univariable model, 11 variables reached statistical significance (see the Appendix, Table S1). The symptom of right lower quadrant pain was excluded from the multivariable model owing to colinearity. Neutrophil counts, diffuse abdominal pain, number of drainage tubes, ruptured/perforated appendicitis and surgery group reached statistical significance and were the independent influence factors of time to resuming oral feeding. After controlling for age, sex and other factors, we found that patients treated with CLA had significantly longer time to resuming oral feeding than those treated with SILA; the difference was estimated as 12.83 hours (p < 0.001); oral feeding time was increased by every unit increase in neutrophil count, with an estimated difference of 5.46 hours (p = 0.021). Patients with diffuse abdominal pain took much longer to reach the first oral feeding than those without diffuse abdominal pain, and the difference was estimated to be 7.64 hours (p = 0.001). Patients with 1 or 2 drains had a significantly longer time to resuming oral feeding than those without drains, and the estimated differences were 5.13 hours (p = 0.004) and 63.26 hours (p < 0.001), respectively. Patients with ruptured (perforated) appendices had significantly longer time to resuming oral feeding than those without, and the estimated difference was 8.64 hours (p < 0.001; Table 3).
Patients in the SILA group with any symptoms had fewer complications than those in the CLA group (Table 4), although there were no significant differences among those with GI upset, diffuse abdominal pain and right lower quadrant pain. Patients with acute appendicitis and gangrenous appendicitis in the SILA group had fewer complications than patients in the CLA group, but the difference was not significant. All 3 patients with perforated appendices in the SILA group experienced only mild wound infections, but 47.1% of patients in the CLA group experienced complications.
Table 4.
Associations between surgeries and complications and surgery-related outcomes, stratified by symptoms and pathology
| Symptom or pathology; group | No. | Complications | Duration of surgery, min. | ||
|---|---|---|---|---|---|
|
|
|
||||
| No. (%)* | p value | Median (IQR)† | p value | ||
| Fever | 0.019 | 0.028 | |||
|
| |||||
| SILA | 25 | 1 (4.0) | 60.0 (55.0–75.0) | ||
|
| |||||
| CLA | 174 | 42 (24.1) | 55.0 (45.0–70.0) | ||
|
| |||||
| Gastrointestinal upset | 0.46 | 0.19 | |||
|
| |||||
| SILA | 28 | 4 (14.3) | 60.0 (52.5–67.5) | ||
|
| |||||
| CLA | 207 | 47 (22.7) | 55.0 (45.0–70.0) | ||
|
| |||||
| Diffuse abdominal pain | 0.42 | 0.049 | |||
|
| |||||
| SILA | 8 | 2 (25.0) | 47.5 (40.0–62.5) | ||
|
| |||||
| CLA | 20 | 9 (45.0) | 75.0 (52.5–81.0) | ||
|
| |||||
| RLQ pain | 0.23 | < 0.001 | |||
|
| |||||
| SILA | 64 | 5 (7.8) | 60.0 (55.0–75.0) | ||
|
| |||||
| CLA | 346 | 50 (14.5) | 52.5 (40.0–65.0) | ||
|
| |||||
| Nausea/vomiting | 0.011 | 0.71 | |||
|
| |||||
| SILA | 40 | 2 (5.0) | 60.0 (50.0–72.5) | ||
|
| |||||
| CLA | 10 | 4 (40.0) | 62.5 (35.0–75.0) | ||
|
| |||||
| Acute appendix | 0.07 | 0.009 | |||
|
| |||||
| SILA | 39 | 1 (2.6) | 60.0 (50.0–60.0) | ||
|
| |||||
| CLA | 363 | 47 (12.9) | 50.0 (40.0–60.0) | ||
|
| |||||
| Gangrenous appendix | 0.30 | 0.035 | |||
|
| |||||
| SILA | 13 | 1 (7.7) | 90.0 (65.0–105.0) | ||
|
| |||||
| CLA | 118 | 30 (25.4) | 60.0 (50.0–80.0) | ||
|
| |||||
| Perforated appendix | 0.12 | 0.39 | |||
|
| |||||
| SILA | 3 | 3 (100) | 55.0 (25.0–95.0) | ||
|
| |||||
| CLA | 70 | 33 (47.1) | 70.0 (60.0–90.0) | ||
CLA = conventional laparoscopic appendectomy; IQR = interquartile range; RLQ = right lower quadrant; SILA = single incision laparoscopic appendectomy.
Determined by Fisher exact test.
Determined by the Mann–Whitney U test.
Incision wounds, 3 for CLA procedures and a single navel wound for SILA procedures, were evaluated postoperatively before discharge by a member of the surgical team (H.-H.L.). All wounds in all patients healed well with good cosmetic results. Lower abdominal and suprapubic surgical wounds were seen more obviously in patients who underwent CLA, whereas the 1 SILA incision scar was well hidden in the skin folds of the navel. The duration of surgery in both groups was affected by symptoms and pathology. Patients in the SILA group who had fever and right lower quadrant pain had slightly longer surgeries than those in the CLA group who had the same symptoms. However, this changed with the degree of abdominal pain: those with diffuse abdominal pain in the CLA group had longer surgeries than patients with diffuse abdominal pain in the SILA group (75.0 min v. 47.5 min, p < 0.05). The duration of surgery for patients with acute appendicitis was significantly longer in the SILA group than in the CLA group (p < 0.01). The median duration of surgery for patients with gangrenous appendices was 90 minutes in the SILA group compared with 60 minutes in the CLA group (p < 0.05).
Further direct comparisons made between nonperforated appendices in the 2 groups (n = 615), are shown in Table 5. After excluding 73 patients (3 in SILA group, 70 in CLA group) with perforated appendices, as determined by pathological examination, significant associations were observed between the groups in the number of drain tubes, duration of surgery, LOS, time to resuming oral feeding and the complication of wound infection (all p < 0.05).
Table 5.
Surgery-related outcomes by group for patients with nonperforated appendices
| Factor | Group; no. (%)* or median [IQR]† | p value | |
|---|---|---|---|
| SILA, n = 67 | CLA, n = 548 | ||
| No. of drain tubes | |||
| 0 | 58 (86.6) | 524 (95.6) | 0.008 |
| 1 | 9 (13.4) | 23 (4.2) | |
| 2 | 0 (0) | 1 (0.2) | |
| Intraoperative findings | |||
| Inflammation | 56 (83.6) | 434 (79.2) | 0.52 |
| Gangrenous appendix | 10 (14.9) | 84 (15.3) | > 0.99 |
| Ruptured appendix (perforated) | 0 (0) | 13 (2.4) | 0.38 |
| Chylous (pus) ascites | 0 (0) | 8 (1.5) | > 0.99 |
| Abscess/local abscess | 0 (0) | 3 (0.5) | > 0.99 |
| Adhesion | 0 (0) | 23 (4.2) | 0.16 |
| Total dose of analgesic | |||
| None | 44 (65.7) | 373 (68.1) | 0.68 |
| ≥ 50 mg meperidine | 23 (34.3) | 175 (31.9) | |
| Surgery outcomes | |||
| Duration of surgery, min. | 60.0 [55.0–75.0] | 50.0 [40.0–65.0] | < 0.001 |
| LOS, h | 72.0 [48.0–96.0] | 55.0 [41.0–68.0] | < 0.001 |
| Time to resuming oral feeding, h | 12.0 [8.0–16.0] | 22.0 [16.0–28.0] | < 0.001 |
| Complications | 2 (3.0) | 79 (14.4) | 0.006 |
| Wound infection | 2 (3.0) | 71 (13.0) | 0.015 |
| Ileus | 0 (0) | 2 (0.4) | > 0.99 |
| Intra-abdominal abscess | 0 (0) | 2 (0.4) | > 0.99 |
| Incision hernia | 1 (1.5) | 3 (0.5) | 0.37 |
CLA = conventional laparoscopic appendectomy; IQR = interquartile range; LOS = length of stay in hospital; SILA = single-incision laparoscopic appendectomy.
Determined by Fisher exact test.
Determined by Mann–Whitney U test.
Discussion
In this study, using a single incision and a novel port approach provided several advantages over CLA: mainly better cosmetic effects (Fig. 1E v. Fig. 1D), and no increase in postsurgical pain or complications in a relatively large group of patients.
Although many surgeons consider SILA to be a difficult procedure with a challenging learning curve, increasing experience is making this surgery far more available to patients. It is important to note that the patients in this study were not randomly assigned to the 2 groups. When patients presented with an advanced stage of the disease, such as ruptured or perforated appendicitis, they were treated with CLA. Perhaps because of the cosmetic benefits of SILA, younger patients and a greater percentage of women selected SILA despite the procedure being more costly. The novel technique using a surgical glove improved the visibility of the procedure outside the belly (Fig. 1A). As Hayashi and colleagues13 reported, the cost of new port-related devices can be an important factor. The use of a standard surgical glove for the single port provided a simple and cost-effective method.
During SILA, instrument crowding can increase the difficulty of the surgery. Our technique used a transparent glove, which allowed a better view of the operation and less chance of instrument crossover. All SILA procedures were successful, and there was no need to convert to CLA or to open appendectomy. Hong and colleagues12 performed transumbilical SILA in 33 patients, and 2 patients required conversion to conventional 3-port laparoscopic appendectomy owing to gangrenous changes and 1 patient needed additional drainage. Oltmann and colleagues14 reported that 2 of 39 pediatric patients required conversion from SILA to CLA. A review of the literature by Ahmed and colleagues15 in 2011 reported that the conversion rate from SILA to CLA in published studies ranged from 0 to 41%.
Our results showed that the duration of surgery was associated with symptoms and pathology, especially among patients with diffuse abdominal pain (duration was shorter in the SILA group) and gangrenous appendicitis (duration was longer in the SILA group). When we directly compared cases of nonperforated appendicitis determined by pathological examination, we observed significant differences between the groups in the number of drain tubes, duration of surgery, LOS, time to resuming oral feeding and the rate of wound infection. With this direct comparison, SILA surgeries were significantly longer than CLA surgeries, and those in the SILA group had longer LOS than those in the CLA group. However, the SILA group had significantly fewer complications and resumed oral feeding more quickly than the CLA group, still demonstrating the advantages of SILA over CLA for most patients. Notably, a recent prospective study comparing SILA and CLA in 102 patients reported that SILA was feasible and safe even in patients with perforated appendices.16
In the present study, when all patients were included in analysis, the median duration of surgery was 5 minutes longer for patients in the SILA group (median 60.0 min, mean 65.2 min) than the CLA group (median 55.0 min, mean 58.5 min). Our results are similar to those of Kim and colleagues,8 who reported a mean duration of 61.3 (range 24–120) minutes for SILA, and those of Hong and colleagues,12 who reported a mean duration of 40.8 (range 15–90) minutes.
In the present study, there was little difference in LOS between the groups. The median LOS was 60.0 (mean 59.7) hours for those treated with SILA and 58.0 (mean 62.9) hours for those treated with CLA, which is comparable to the mean LOS of 2.5 (range 1–11) days reported by Hong and colleagues.12
The rate of complications was significantly different between the 2 groups in the present study. A number of factors can influence the occurrence of complications, including wound size, bowel injury and leakage of the appendiceal stump. In our study, during SILA, a drainage tube was commonly placed through the 10 mm umbilical incision, which was a larger incision than that used for CLA (5 mm, right lower quadrant wound). While some studies with larger patient samples12,13 have indicated that the complication rate with SILA was low, a 2001 literature review suggested that SILA was applied only to restricted groups of patients, notably premenopausal women in whom, after explorative laparoscopy, the level of inflammation of the appendix was not so high and not complicated by generalized peritonitis, abscess, gangrene or perforation.17 Otherwise, trends seem to evidence an increase in complications, especially in complicated appendicitis.
Another advantage that we noted among the SILA group patients was that they returned to oral intake more quickly after surgery. In the SILA group, patients had their first oral feeding 12.0 hours after surgery compared with 22.0 hours in the CLA group. The patients in the SILA group could be fed independent of symptoms and pathology, indicating a quick and full physical recovery from surgery. Among the factors that can influence time to resuming oral feeding is the presence of drainage tubes. A larger number of drainage tubes are used with more severe disease, such as ruptured appendicitis and peritonitis, which can lead to a slower recovery. The use of drainage tubes may also be associated with increased pain. In our study, there was no difference in analgesic use between the groups. A study by Kang and colleagues,18 however, showed that patients who received SILA experienced more postoperative pain.
Limitations
The primary limitations of this study are that patients were not randomly assigned to the surgical procedure they received, and that the number of patients was significantly different between the groups. This indicates potential selection bias and population bias, and results cannot be generalized to all patients receiving these surgeries. Additional prospective studies are needed to confirm our results.
Conclusion
Our results indicate that SILA has acceptable safety and effectiveness as a minimally invasive approach for treating appendicitis. In addition to offering cosmetic advantages, it leads to rapid recovery and no significant increases in postsurgical pain or complications. The duration of surgery for SILA is somewhat longer than that for CLA, and SILA may not be appropriate for patients with complicated appendicitis, such as appendicitis with perforation or tumour formation.
Footnotes
Competing interests: None declared.
Contributors: H.-H. Liang, C.-S. Hung, W. Wang and P.-L. Wei designed the study. C.-S. Hung, W. Wang, K.-W. Tam, C.-C. Chang, H.-H. Liu and K.-L. Yen acquired and analyzed the data. H.-H. Liang, H.-H. Liu and K.-L. Yen wrote the article, which all authors reviewed and approved for publication.
References
- 1.Keus F, de Jong JA, Gooszen HG, et al. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev. 2006:CD006231. doi: 10.1002/14651858.CD006231. [DOI] [PubMed] [Google Scholar]
- 2.Stocchi L, Nelson H, Young-Fadok TM, et al. Safety and advantages of laparoscopic vs. open colectomy in the elderly: matched-control study. Dis Colon Rectum. 2000;43:326–32. doi: 10.1007/BF02258297. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen KT, Marsh JW, Tsung A, et al. Comparative benefits of laparoscopic vs. open hepatic resection: a critical appraisal. Arch Surg. 2011;146:348–56. doi: 10.1001/archsurg.2010.248. [DOI] [PubMed] [Google Scholar]
- 4.Froghi F, Sodergren MH, Darzi A, et al. Single-incision laparoscopic surgery (SILA) in general surgery. A review of current practice. Surg Laparosc Endosc Percutan Tech. 2010;20:191–204. doi: 10.1097/SLE.0b013e3181ed86c6. [DOI] [PubMed] [Google Scholar]
- 5.Chow A, Purkayastha S, Nehme J, et al. Single incision laparoscopic surgery for appendectomy: a retrospective comparative analysis. Surg Endosc. 2010;24:2567–74. doi: 10.1007/s00464-010-1004-3. [DOI] [PubMed] [Google Scholar]
- 6.Sodergren MH, Clark J, Athanasiou T, et al. Natural orifice translumenal endoscopic surgery: critical appraisal of applications in clinical practice. Surg Endosc. 2009;23:680–7. doi: 10.1007/s00464-008-0278-1. [DOI] [PubMed] [Google Scholar]
- 7.Nguyen NT, Reavis KM, Hinojosa MW, et al. A single-port technique for laparoscopic extended stapled appendectomy. Surg Innov. 2009;16:78–81. doi: 10.1177/1553350608330528. [DOI] [PubMed] [Google Scholar]
- 8.Kim HJ, Lee JI, Lee YS, et al. Single-port transumbilical laparoscopic appendectomy: 43 consecutive cases. Surg Endosc. 2010;24:2765–9. doi: 10.1007/s00464-010-1043-9. [DOI] [PubMed] [Google Scholar]
- 9.Jen HC, Shew SB. Laparoscopic versus open appendectomy in children: outcomes comparison based on a statewide analysis. J Surg Res. 2010;161:13–7. doi: 10.1016/j.jss.2009.06.033. [DOI] [PubMed] [Google Scholar]
- 10.Dunn JC, Grosfeld JL, O’Neill JA, et al. Pediatric surgery. 6th ed. Philadelphia (PA): Mosby Elsevier; 2006. Appendicitis; p. 1501. [Google Scholar]
- 11.Cho MS, Min BS, Hong YK, et al. Single-site versus conventional laparoscopic appendectomy: comparison of short-term operative outcomes. Surg Endosc. 2011;25:36–40. doi: 10.1007/s00464-010-1124-9. [DOI] [PubMed] [Google Scholar]
- 12.Hong TH, Kim HL, Lee YS, et al. Transumbilical single-port laparoscopic appendectomy (TUSPLA): scarless intracorporeal appendectomy. J Laparoendosc Adv Surg Tech A. 2009;19:75–8. doi: 10.1089/lap.2008.0338. [DOI] [PubMed] [Google Scholar]
- 13.Hayashi M, Asakuma M, Komeda K, et al. Effectiveness of a surgical glove port for single port surgery. World J Surg. 2010;34:2487–9. doi: 10.1007/s00268-010-0649-3. [DOI] [PubMed] [Google Scholar]
- 14.Oltmann SC, Garcia NM, Ventura B, et al. Single-incision laparoscopic surgery: feasibility for pediatric appendectomies. J Pediatr Surg. 2010;45:1208–12. doi: 10.1016/j.jpedsurg.2010.02.088. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed K, Wang TT, Patel VM, et al. The role of single-incision laparoscopic surgery in abdominal and pelvic surgery: a systematic review. Surg Endosc. 2011;25:378–96. doi: 10.1007/s00464-010-1208-6. [DOI] [PubMed] [Google Scholar]
- 16.Kye BH, Lee J, Kim W, et al. Comparative study between single-incision and three-port laparoscopic appendectomy: a prospective randomized trial. J Laparoendosc Adv Surg Tech A. 2013;23:431–6. doi: 10.1089/lap.2012.0284. [DOI] [PubMed] [Google Scholar]
- 17.Vettoretto N, Mandalà V. Single port laparoscopic appendectomy: Are we pursuing real advantages? World J Emerg Surg. 2011;6:25. doi: 10.1186/1749-7922-6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kang KC, Lee SY, Kang DB, et al. Application of single-incision laparoscopic surgery for appendectomies in patients with complicated appendicitis. J Korean Soc Coloproctol. 2010;26:388–94. doi: 10.3393/jksc.2010.26.6.388. [DOI] [PMC free article] [PubMed] [Google Scholar]