Abstract
BACKGROUND:
Adolescents with chronic disease (ACD) must develop independent disease self-management and learn to communicate effectively with their health care team to transition from pediatric to adult-oriented health care systems. Disease-specific interventions have been implemented to aid specific ACD groups through transition. A generic approach might be effective and cost-saving.
METHODS:
Eighty-one ACD, aged 12 to 20 years, were recruited for a randomized clinical trial evaluating an 8-month transition intervention (MD2Me). MD2Me recipients received a 2-month intensive Web-based and text-delivered disease management and skill-based intervention followed by a 6-month review period. MD2Me recipients also had access to a texting algorithm for disease assessment and health care team contact. The intervention was applicable to adolescents with diverse chronic illnesses. Controls received mailed materials on general health topics. Disease management, health-related self-efficacy, and health assessments were performed at baseline and at 2 and 8 months. Frequency of patient-initiated communications was recorded over the study period. Outcomes were analyzed according to assigned treatment group over time.
RESULTS:
MD2Me recipients demonstrated significant improvements in performance of disease management tasks, health-related self-efficacy, and patient-initiated communications compared with controls.
CONCLUSIONS:
Outcomes in ACD improved significantly among recipients of a generic, technology-based intervention. Technology can deliver transition interventions to adolescents with diverse chronic illnesses, and a generic approach offers a cost-effective means of positively influencing transition outcomes. Further research is needed to determine whether improved short-term outcomes translate into an improved transition for ACD.
Keywords: transition to adulthood, adolescents, self-management, chronic disease management
What’s Known on This Subject:
Adolescents with chronic disease are a diverse population with common needs for transition. Disease-specific interventions have shown promise at improving patient outcomes but with substantial personnel and resource costs. Whether a generic approach across diseases may be useful is unknown.
What This Study Adds:
This study is among the first to evaluate a generic (across disease) approach to transition of adolescents to adult care. The approach demonstrated promise and cost savings due to reduced personnel requirement and use of low-cost technology dissemination methods.
Transition is the purposeful, planned transfer of adolescents with chronic medical conditions from child-centered to adult-oriented health care systems. The Institute of Medicine describes the health care transition for adolescents and young adults with chronic disease (ACD) as crucial to future health and psychosocial outcomes.1 Healthy People 2020 identifies transition planning as a major objective for ACD.2 However, there remain notable deficits in the transition experience for many ACD.3
Health care providers and researchers recognize that generic disease management skills are required for and may be effectively and efficiently addressed across all chronic diseases.3 Yet, to date, interventions that prepare adolescents for transition have often been disease-focused and delivered in-person, increasing cost and decreasing availability and efficiency.4 Such clinic-based interventions do not have optimal reach because they do not account for the poor engagement of ACD with the health care system.5
In a randomized clinical trial, we evaluated whether a generic, Internet- and mobile phone–delivered disease management intervention would improve disease management, self-efficacy, and communication outcomes in ACD. Inflammatory bowel disease (IBD), cystic fibrosis (CF), and type 1 diabetes (T1D), with their diversity in clinical course and disease burden, were chosen to represent the broad disease spectrum in ACD. We hypothesized that a generic intervention designed to improve disease management, health-related self-efficacy, and patient-initiated communications would be more effective than a general health intervention in ACD for transition preparation.
Methods
Eighty-one patients with IBD, CF, or T1D and aged 12 to 22 years old without cognitive impairment were recruited (October 2010 to March 2011) from a tertiary care pediatric academic medical center serving ∼1 million youth. The sample size was 80 to account for a 10% attrition rate. The institutional review boards at the University of California, San Diego, and Rady Children’s Hospital approved the study protocol. Informed consent and assent were obtained before the study procedures.
Intervention Groups
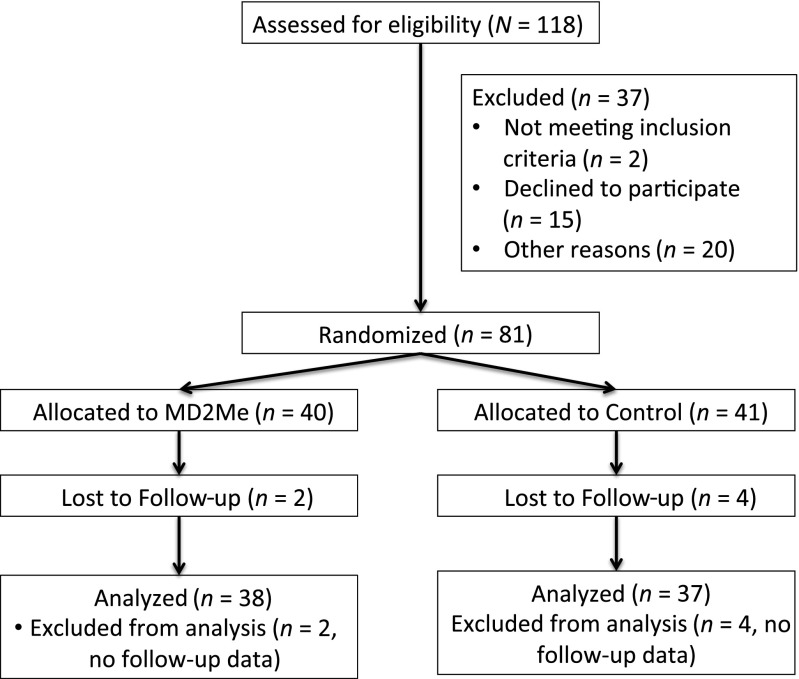
Random assignment to the intervention group (MD2Me) or control groups (Fig 1; by random block assignment stratified by disease and generated by study statistician) occurred after the baseline visit. Participants were not blinded to study group assignment. Cell phones and plans were provided to MD2Me subjects who did not have a cell phone.
FIGURE 1.
CONSORT (Consolidated Standards of Reporting Trials) diagram for the MD2Me randomized controlled clinical trial.
MD2Me
MD2Me subjects received an 8-month technology-based disease management intervention based on Bandura’s Social Cognitive Theory. The intervention targeted the self-management constructs6 of monitoring disease symptoms, responding to monitoring with appropriate treatments, and actively working with health care providers to manage care. For 2 months, subjects were asked to log in to a secure Web site weekly to receive theme-based materials outlining common disease management and communication skills, and lifestyle tips (See Supplementary Materials and Figures for more information). Disease-specific case studies were provided to increase usability. Tailored short message service (SMS) messages and queries were delivered (3–5 messages/week) to ensure that participants received and understood intervention messages. After 2 months, Web site access was provided as a disease management and information resource. Weekly reminder SMS messages were also delivered to reinforce previously introduced concepts and skills.
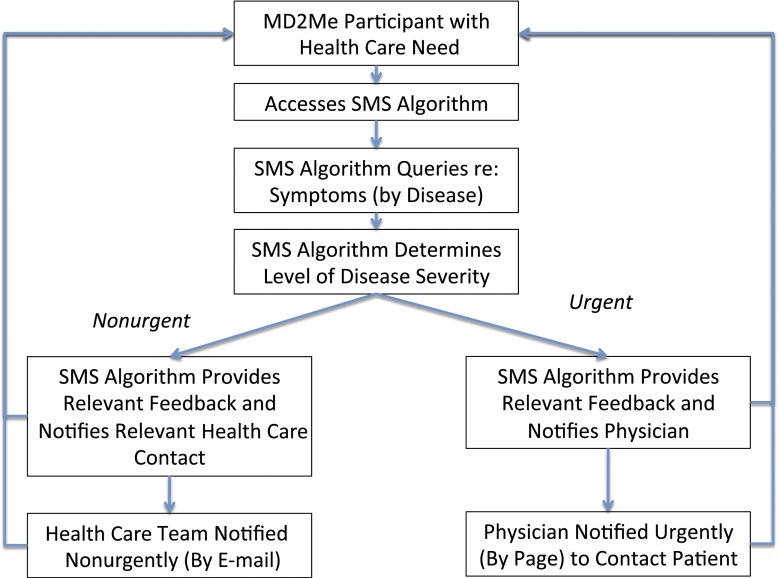
To facilitate patient-initiated communications, MD2Me recipients were given access to an automated SMS algorithm (Fig 2) that provided disease management decision support and a health care team communications portal. Subjects could activate the SMS to report health concerns. According to level of urgency (ie, nonurgent [to be addressed within 48 to 72 hours] or urgent [requiring same-day attention]), subject concerns were relayed to the health care team (by page or e-mail for intervention). Usual health care communication portals (eg, phone) were available to all participants.
FIGURE 2.
MD2Me SMS algorithm decision tree. Nonurgent, requiring intervention within 48 to 72 hours; Urgent, requiring intervention within 24 hours.
Controls
Controls received monthly messages via mail or e-mail (participant preference) addressing general health issues. Disease-specific information was provided as appropriate (eg, in the healthy nutrition module). Usual health care communication portals were available to controls.
Assessments
Participants’ disease self-management and health-related self-efficacy were assessed at study visits at a clinical research office by measurement staff blinded to group assignment. Patient-initiated communications were assessed as noted below. Health literacy, health status, and demographic data were also collected. All instruments have been used in adolescents and found to be reliable and valid.
Disease Status
Disease status was assessed by using scales developed for each disease. We used the Pediatric Ulcerative Colitis Activity Index (range: 0–85, with 0 indicating no disease and higher scores indicating worse disease)7 for patients with ulcerative/indeterminate colitis and the abbreviated Pediatric Crohn’s Disease Activity Index (range: 0–70, with 0 indicating no disease)8 for patients with Crohn disease. For CF, we used the Cystic Fibrosis Clinical Score (range: 10–50, with 10 indicating no disease)9. The Diabetes Quality of Life Brief Clinical Inventory (range: 60–0, with 60 indicating perfect disease status satisfaction)10 was used for T1D. Baseline predicted forced expiratory volume in 1 second and glycohemoglobin were extracted from the medical record for patients with CF and T1D, respectively.
Global Health Status
The Karnofsky Performance Scale,11 a functional status assessment scale used in chronic disease populations (0–100, where 100 represents perfect health and 0 represents death), was used as a universal functional status measure across all diseases. We also used the Pediatric Quality of Life Scale (PedsQL) to measure quality of life as an indicator of health status.12
Health Literacy Assessments
Health literacy was assessed by using the Test of Functional Health Literacy in Adults.13 The adult version was used to reflect the health information processing needs of patients transitioning to adult health care that was still sensitive to adolescent concerns.14,15 The Test of Functional Health Literacy in Adults provides information on both reading comprehension and numerical ability, with higher scores (0–100 range) indicating better literacy. Scores of <60 represent inadequate literacy.13
Disease Management and Self-efficacy
The Transition Readiness Assessment Questionnaire (TRAQ) 4.116 is a measure of readiness for transition and assesses performance of chronic disease self-management skills. The TRAQ 4.1 was scored by using a 6-point scale where 0 points were given for subjects who felt that the skill was not necessary for their care, 1 point was given for not knowing how to perform the necessary skill, and 5 was given for performing the skill consistently when needed. The TRAQ assumes that subjects can correctly identify when a skill is not necessary for their care. To better capture the inability of subjects to recognize that a particular skill was needed for disease self-management, we scored inability to recognize a skill as needed for chronic disease self-management as −1; the scale was otherwise scored the same. In cases in which a given skill was deemed not necessary for chronic disease self-management for a given patient situation, 0 points was assigned to the question. Because none of our patients was financially independent, all of the financial capability questions in TRAQ 4.1 were scored 0 points. A TRAQ summary score ≥4 is equivalent to respondents reporting that they are starting to perform necessary disease management skills.
The Patient Activation Measure17 gauges participants’ self-efficacy and confidence essential to managing one’s own health and health care on a scale of 0 to 100, with 100 representing functioning as an independently functioning adult with chronic disease). A normalized Patient Activation Measure score ≥68.5 is equivalent to having the self-efficacy and confidence to take charge of one’s own health and care (ie, ready for transition).
Patient-Initiated Health Care Communications
Frequency and mode of communication contacts between adolescent participants only (ie, not those initiated by the parent) and the health care system were recorded as the measures of patient-initiated health care interactions; communication contacts from 8 months before and during the study period were recorded and ultimately compared to determine changes in patient-initiated communications across intervention period by group. Specifically, the numbers of participant-initiated messages to the MD2Me communications portal were recorded, and electronic medical record review ascertained the number of phone conversations between participants and his/her health care team. In the studied electronic medical record, all telephone encounters are recorded and then triaged to the appropriate provider (eg, nurse, scheduler, physician) for action.
Statistical Methods
Demographic and disease variable distributions were analyzed for descriptive purposes. Treatment groups were statistically compared to determine the equality of randomization. To permit comparisons across disease, disease status scores were normalized to a scale of 0 to 100, with 100 representing ideal health. Intervention outcomes (disease management, health-related self-efficacy, and patient-initiated communications) were analyzed by intent-to-treat randomization assignment, using repeated-measures models testing the treatment × time interaction. Variables expected to influence outcomes such as age, specific disease (ie, CF, T1D, and IBD), and literacy status were entered into outcome analyses. Statistical analyses were performed by using JMP statistical software (SAS Institute, Cary, NC); significance was set at P < .05.
Results
Eighty-one youth with chronic disease were randomly assigned into the study (Fig 1). Demographic data are presented in Table 1. The ages of subjects in each disease group differed (median [interquartile range] for IBD, T1D, and CF: 17 [16–18], 17 [16–18], and 14 [13–16] years, respectively; P = .004). There were no significant ethnic or gender differences. Seventy-five youth completed the study. There were no differences between the 6 dropouts (2 MD2Me subjects and 4 controls) and the main cohort by age (P = .20), disease (P = .10), gender (P = .53), or ethnicity (P = .10). There were no study-related adverse events or confidentiality breaches.
TABLE 1.
Demographic and Other Information on Study Participants
| Characteristic | MD2Me (N = 40) | Control (N = 41) |
|---|---|---|
| Age, median (minimum, maximum), y | 17 (12, 20) | 17 (12, 19) |
| Gender (male:female), n | 17:23 | 20:21 |
| Race/ethnicity, n | ||
| White | 16 | 11 |
| Black | 4 | 4 |
| Hispanic | 18 | 22 |
| American Indian/Alaskan | 1 | 0 |
| Other | 1 | 4 |
| Disease category, n | ||
| IBD | ||
| CD | 11 | 12 |
| UC | 6 | 5 |
| CF | 6 | 7 |
| T1D | 17 | 17 |
| Disease duration, median (IQR), y | 4 (3–9) | 6 (2–10) |
| Disease status, median (IQR) | ||
| UC | ||
| PUCAI | 3 (0–21) | 0 (0–10) |
| CD | ||
| PCDAI | 5 (5–10) | 10 (1–20) |
| CF | ||
| CFCS | 19 (17–24) | 18 (14–25) |
| FEV1% | 87 (69–94) | 81 (72–98) |
| T1D | ||
| DQoL | 47 (44–49) | 45 (35–52) |
| Glycohemoglobin, % | 8.2 (7–9.2) | 8.6 (7.9–9.5) |
| Karnofsky Performance Scale, median (IQR) | 90 (90–100) | 90 (80–100) |
| TOFHLA, median (minimum, maximum) | 82 (74, 88) | 81 (70, 89) |
| PedsQL, median (IQR) | 81 (70–91) | 77 (64–88) |
CD, Crohn disease; CFCS, Cystic Fibrosis Clinical Score; DQoL, Diabetes Quality of Life Brief Clinical Inventory; FEV1%, baseline predicted forced expiratory volume in 1 second by percentage; IBD, inflammatory bowel disease; IQR, interquartile range; PCDAI, Pediatric Crohn’s Disease Activity Index; PedsQL, Pediatric Quality of Life Scale; PUCAI, Pediatric Ulcerative Colitis Activity Index; TOFHLA, Test of Functional Health Literacy in Adults; UC, ulcerative colitis.
Disease Status
Disease status as measured by specific disease scales (P = .18–.86), functional performance (P = .31), and quality of life (P = .17) did not differ according to treatment group assignment (Table 1). Disease severity varied by disease, as expected (Table 1).
Baseline Health Literacy and Readiness for Transition (Disease Management and Health Self-efficacy) Measures
Significant baseline health literacy, disease management, and health-related self-efficacy differences were noted across disease groups (Table 2) but not according to treatment group (Table 3). Most patients demonstrated adequate health literacy (74%). In contrast, only 34% (26% of MD2Me subjects and 41% of controls, P = .13) had begun to perform the necessary disease management skills needed for transition (defined as TRAQ ≥4). Both treatment groups had minimal patient-initiated outside-of-clinic-visit contact with their health care teams at baseline.
TABLE 2.
Baseline Health Literacy, Chronic Disease Management, and Health-Related Self-efficacy Assessments by Disease
| Disease Group | Health Literacy (TOFHLA) | Chronic Disease Management (TRAQ) | Health-Related Self-efficacy (PAM) | |||
|---|---|---|---|---|---|---|
| Score | Pa | Score | Pa | Score | Pa | |
| CF | 71 (17) | .01 | 2.9 (0.9) | .01 | 72 (12) | <.01 |
| T1D | 80 (12) | 3.7 (0.8) | 77 (17) | |||
| IBD | 98 (9) | 3.5 (0.7) | 63 (16) | |||
Data are presented as means (SD). PAM, Patient Activation Measure (range: 0 [poor self-efficacy to manage one’s own health] to 100 [fully able to manage one’s own health and health care]); TOFHLA, Test of Functional Health Literacy in Adults (range: 0 [illiterate] to 100 [literate]); TRAQ, Transition Readiness Assessment Questionnaire (range: −1 [not ready to transition] to 5 [ideally ready for transition]).
ANOVA across disease groups.
TABLE 3.
Changes in Main Outcome Measures Over Time According to Treatment Group
| Treatment Group | Chronic Disease Management (TRAQ) | Health-Related Self-efficacy (PAM) | Patient-Initiated Communications (Number of Contacts per Individual per Period) | |||
|---|---|---|---|---|---|---|
| Time and Scores | P | Time and Scores | P | Time and Number | P | |
| MD2Me | Baseline: 3.4 (0.9) | .02 | Baseline: 72 (17) | .02 | 8 months before study participation: 0 (0) | <.0001 |
| 2 months: 3.5 (0.7) | 2 months: 79 (16) | 8-month study period: 2 (2) | ||||
| 8 months: 4.0 (0.8) | 8 months: 81 (17) | |||||
| Control | Baseline: 3.6 (0.7) | Baseline: 69 (17) | 8 months before study participation: 0 (0) | |||
| 2 months: 3.8 (0.9) | 2 months: 69 (16) | 8-month study period: 0 (0) | ||||
| 8 months: 3.8 (0.8) | 8 months: 71 (14) | |||||
Data are presented as means (SD). Comparative analyses between treatment and control groups for each outcome measure used repeated measures models that included treatment group (intent-to-treat), age, disease, and baseline literacy scores. P values presented are from model comparisons of treatment group × time, controlling for the factors listed above. PAM, Patient Activation Measure; TRAQ, Transition Readiness Assessment Questionnaire.
Change in Chronic Disease Management and Patient-Initiated Communications Outcomes Over Time According to Treatment Group
MD2Me recipients demonstrated significant improvements in all targeted outcomes across the study period compared with controls, controlling for age, baseline literacy status, and disease group (Table 3). Specifically, MD2Me participants, compared with controls, demonstrated increases in disease self-management and health-related self-efficacy. In addition, the number of patient-initiated communications between MD2Me participants and their health care team increased significantly compared with the control group. This increase in patient-initiated communications by MD2Me participants primarily occurred via the SMS algorithm (median [minimum, maximum] increased interactions during study period by MD2Me participants: +1 (0, 7) SMS vs. +0 (0, 2) phone).
Baseline health literacy did affect outcomes according to treatment group. Specifically, MD2Me participants with adequate literacy levels demonstrated greater improvements in disease management but not in health-related self-efficacy or patient-initiated communications over the study period compared with MD2Me participants with inadequate literacy levels. In contrast, age and disease group did not significantly affect disease management, health-related self-efficacy, or patient-initiated communications over time.
Health outcomes were not a specific target of the MD2Me program. Disease status, functional performance, and quality of life did not significantly change over the study period by treatment group.
MD2Me: Compliance and Performance
Among MD2Me participants, 79% (63%, 93%) (median [interquartile range]) of curriculum receipt was documented across both Web and SMS modalities. Web visits occurred primarily during the initial 2 months (All but 1 participant visited the Web site during the initial 2 months, whereas only 16 [42%] users visited in the latter 6 months). In contrast, all but 1 user responded to SMS curricula throughout the intervention with 78% (56%, 90%) compliance. Seventy-seven percent of participants used the SMS algorithm, and SMS algorithm users were older than those who did not access the SMS algorithm (mean [SD]: 15 [2] vs 17 [2] years; SMS algorithm non-users v. users, P = .01).
Discussion
We demonstrated the efficacy of a technology-based, transition intervention to improve disease management, health-related self-efficacy, and patient-initiated communications in ACD across 3 disease groups. Our findings suggest that a more resource-intensive disease-specific approach may not be necessary now that a generic approach to aid ACD through transition has been shown to be efficacious. The use of technology in our program offers a low-cost alternative for intervention in this at-risk population, which can be distributed across time and geography and independent of the clinic setting.
Poor transition experiences are commonly reported among ACD3 and have been linked to poor outcomes in this population, including poor mental health and psychosocial outcomes, and negative effects on functional ability, developmental milestone achievement, psychiatric health, employment, and sexual partnering into adulthood.18 The need for ACD to be supported and prepared for transition is well recognized. Consensus statements (both disease-specific19–21 and generic22) on the needs of the adolescent during this period have been published. To prepare for the transition from child-centered to adult-centered care, ACD should learn the skills needed to effectively care for themselves and how to advocate for their own health issues.23 Consensus guidelines suggest that this process should begin by age 14 years among ACD.24
A generic approach to readiness for transition programs has not often been used in pediatrics despite evidence that low-cost disease management training using a generic approach improves health outcomes among adults with chronic disease.25 We demonstrated successful use of a generic approach for transition preparation interventions in ACD. In fact, disease type did not appear to affect the intervention effect on any of the targeted outcomes in our study despite notable differences between disease groups at baseline in disease management, health literacy, and health-related self-efficacy. The approach to transition support tested in this study offers availability and utility across diseases. The technology-based approach offers the possibility of efficient implementation in a clinic setting with modest personnel time and effort.
Recent trends indicate a major shift to incorporate technologies into health behavior interventions. These technologies offer several advantages for health behavioral interventions, such as information and messages tailored to the participant, quick access, increased cultural sensitivity, and anonymity, which may be attractive regarding sensitive health issues. Similarly, mobile technologies can be used to improve health outcomes. The computing power and portability of mobile phones make possible new applications for automatic, timely, and tailored presentation of health messages, and because mobile phones are generally only accessed by a single individual, outreach can be improved for sensitive medical issues. Wireless devices are now ubiquitous, and text messaging is currently the main form of communication by adolescents today.26 We previously demonstrated notable interest among ACD in using technologies in a disease management intervention,27 which has since been validated by others.28 Studies using the Web and SMS for promoting disease self-management among youth have found some success.29 Similarly, we demonstrated efficacy of our Web- and SMS-based intervention for chronic disease management in ACD. Most MD2Me recipients reported that the program was helpful as delivered via text (89%) and Web (91%), with 92% reporting that they would likely recommend the program to their friends or family. Most notably, the SMS communication portal appeared to encourage increased communications between participants and their health care team. Although the absolute increase in number of communications between ACD and their health care team is relatively small, it signified an increase from no communication to some communication. Lack of health care engagement remains a major issue with ACD and the demonstration of ACDs beginning to initiate communications with their health care team is an important step toward autonomy in managing one’s own health. In 1 situation, this communication led to timely intervention in 1 participant who required urgent admission for intensive medical care. Although it is possible that the participant would have contacted his health care team through usual channels had the SMS portal not been available and that this patient’s course was not altered via this SMS-enabled communication, review of past patient-initiated communications revealed no previous participant-initiated communications despite severe disease symptoms.
Suboptimal health literacy has been linked to poorer chronic disease and health outcomes among adults.30,31 Among children, low parental health literacy also appears to adversely affect children’s health outcomes.32 Similarly, we found that adolescent/young adult health literacy status affected the effects of a transition intervention on disease management outcomes in ACD. Apparently, participants with lower health literacy did not accrue all of the benefits of the intervention. This finding may indicate the need for additional modules to bolster the adolescents’ capacity to make use of the program if they screen below a certain threshold in health literacy.
We did not find significant effects of age on disease management, health-related self-efficacy, or patient-initiated communication outcomes. This finding is potentially important because young adolescents are not often given the autonomy to make independent health decisions due to their presumed immaturity. Although many guidelines recommend that transition and disease management training should begin by age 14 years, others promote engaging the child affected by chronic disease at an even younger age33 to set up a culture of learning and engagement throughout what will be a lifetime of health care experiences. Our findings support that benefit can be derived from intervening during early adolescence because self-efficacy and patient-initiated communication improvements were seen independent of age and literacy status in MD2Me-assigned participants.
Limitations of our study include the relatively small sample size, single-institution recruitment, and specific patient populations studied. Nevertheless, we recruited at the main pediatric referral center for a catchment area of ∼1 million persons (<18 years) across a broad variety of ACD. Although we demonstrated success in our generic intervention approach to prepare ACD for the transition process, we only tested it in 3 patient populations. Nevertheless, these patient cohorts together represent a broad range in health status, disease, and disease management burden. Although we would like to attribute improvements in the treatment group to the MD2Me intervention, an alternative explanation for the improvements may have been the increased frequency of intervention interactions in the MD2Me (weekly) compared with the control (monthly) group. The relatively short duration of the intervention and follow-up period likely limited our ability to affect disease and functional status.
Conclusions
We demonstrated efficacy of a generic intervention approach to improve disease management skills, health-related self-efficacy, and patient-initiated communications in ACD. The use of a common approach and available technologies offers a potentially low-cost option for a population that is sparse and widely distributed. Further study is required to determine whether demonstrated improvements translate into an improved transition experience for ACD.
Supplementary Material
Acknowledgments
We thank Dr Meerana Lim for her contributions as safety officer for the project. We also thank all of our research participants for their help.
Glossary
- ACD
adolescents and young adults with chronic disease
- CF
cystic fibrosis
- IBD
inflammatory bowel disease
- SMS
short message service
- T1D
type 1 diabetes
- TRAQ
Transition Readiness Assessment Questionnaire
Footnotes
Dr Huang conceptualized and designed the study, obtained funding for the study, drafted the initial manuscript, and oversaw the entire project; Drs Gottschalk, Pian, and Norman reviewed the initial analyses and reviewed and revised the manuscript; Ms Terrones, Mr Tompane, and Ms Dillon designed the data collection instruments, coordinated data collection, and critically reviewed the manuscript; Dr Bartholomew worked with Dr Huang to conceptualize and develop the intervention and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
This trial has been registered at www.clinicaltrials.gov (identifier NCT01253733).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by National Institutes of Health grant 1 RC1 MD004721. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Committee on Adolescent Health Care Services National Research Council, Institute of Medicine Challenges in Adolescent Health Care. Washington, DC: National Academies Press; 2007 [Google Scholar]
- 2.US Department of Health and Human Services. Healthy People 2020. Available at: www.healthypeople.gov/2020/topicsobjectives2020/pdfs/HP2020objectives.pdf. Accessed March 21, 2011
- 3.Department of Health/Child Health and Maternity Services Branch Transition: Getting It Right for Young People. Improving the Transition of Young People With Long Term Conditions From Children's to Adult Health Services. London, United Kingdom: Department of Health; 2006 [Google Scholar]
- 4.Rettig P, Athreya BH. Adolescents with chronic disease: transition to adult health care. Arthritis Care Res. 1991;4(4):174–180 [DOI] [PubMed] [Google Scholar]
- 5.Ford CA, Bearman PS, Moody J. Foregone health care among adolescents. JAMA. 1999;282(23):2227–2234 [DOI] [PubMed] [Google Scholar]
- 6.Bandura A. Self-efficacy: The Exercise of Control. New York, NY: WH Freeman and Co; 1997 [Google Scholar]
- 7.Turner D, Otley AR, Mack D, et al. Development, validation, and evaluation of a pediatric ulcerative colitis activity index: a prospective multicenter study. Gastroenterology. 2007;133(2):423–432 [DOI] [PubMed] [Google Scholar]
- 8.Shepanski MA, Markowitz JE, Mamula P, Hurd LB, Baldassano RN. Is an abbreviated Pediatric Crohn’s Disease Activity Index better than the original? J Pediatr Gastroenterol Nutr. 2004;39(1):68–72 [DOI] [PubMed] [Google Scholar]
- 9.Kanga J, Kuhn R, Craigmyle L, Haverstock D, Church D. Cystic fibrosis clinical score: a new scoring system to evaluate acute pulmonary exacerbation. Clin Ther. 1999;21(8):1343–1356 [DOI] [PubMed] [Google Scholar]
- 10.Burroughs TE, Desikan R, Waterman BM, Gilin D, McGill J. (2004). Development and Validation of the Diabetes Quality of Life Brief Clinical Inventory. Diabetes Spectrum. 17(1):41–49 [Google Scholar]
- 11.Karnofsky DA, Burchenal JH. The clinical evaluation of chemotherapeutic agents in cancer. In: MacLeod CM, ed. Evaluation of Chemotherapeutic Agents. New York, NY: Columbia University Press; 1949:196 [Google Scholar]
- 12.Varni JW, Limbers CA, Burwinkle TM. Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5:43–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10(10):537–541. Available at: www.peppercornbooks.com/. Accessed March 31, 2014 [DOI] [PubMed] [Google Scholar]
- 14.Chisolm DJ, Buchanan L. Measuring adolescent functional health literacy: a pilot validation of the Test of Functional Health Literacy in Adults. J Adolesc Health. 2007;41(3):312–314 [DOI] [PubMed] [Google Scholar]
- 15.Julian TW, Kelleher K, Julian DA, Chisolm D. Using technology to enhance prevention services for children in primary care. J Prim Prev. 2007;28(2):155–165 [DOI] [PubMed] [Google Scholar]
- 16.Sawicki GS, Lukens-Bull K, Yin X, et al. Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ—Transition Readiness Assessment Questionnaire. J Pediatr Psychol. 2011;36(2):160–171. Available at: www.dragonflyheartcamp.org/retreat%20facts/assets/transitionreadinessquestionaire.pdf. Accessed March 31, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4 pt 1):1005–1026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stam H, Hartman EE, Deurloo JA, Groothoff J, Grootenhuis MA. Young adult patients with a history of pediatric disease: impact on course of life and transition into adulthood. J Adolesc Health. 2006;39(1):4–13 [DOI] [PubMed] [Google Scholar]
- 19.Yankaskas JR, Marshall BC, Sufian B, Simon RH, Rodman D. Cystic fibrosis adult care: consensus conference report. Chest. 2004;125(1 suppl):1S–39S [DOI] [PubMed] [Google Scholar]
- 20.Baldassano R, Ferry G, Griffiths A, Mack D, Markowitz J, Winter H. Transition of the patient with inflammatory bowel disease from pediatric to adult care: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2002;34(3):245–248 [DOI] [PubMed] [Google Scholar]
- 21.Court JM, Cameron FJ, Bert-Kelly K, Swift, PGF. Diabetes in Adolescence. Pediatric Diabetes. 2009;10:185–194 [DOI] [PubMed] [Google Scholar]
- 22.Cooley WC, Sagerman PJ, American Academy of Pediatrics. American Academy of Family Physicians. American College of Physicians. Transitions Clinical Report Authoring Group . Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128(1):182–200 [DOI] [PubMed] [Google Scholar]
- 23.Callahan ST, Winitzer RF, Keenan P. Transition from pediatric to adult-oriented health care: a challenge for patients with chronic disease. Curr Opin Pediatr. 2001;13(4):310–316 [DOI] [PubMed] [Google Scholar]
- 24.American Academy of Pediatrics. American Academy of Family Physicians. American College of Physicians-American Society of Internal Medicine . A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110(6 pt 2):1304–1306 [PubMed] [Google Scholar]
- 25.Lorig KR, Ritter PL, Dost A, Plant K, Laurent DD, McNeil I. The Expert Patients Programme online, a 1-year study of an Internet-based self-management programme for people with long-term conditions. Chronic Illn. 2008;4(4):247–256 [DOI] [PubMed] [Google Scholar]
- 26.Nielsen Telecom Practice Group. The Mobile Media Report: state of the media Q3 2011. Available at: www.nielsen.com. Accessed March 31, 2014
- 27.Huang JS, Gottschalk M, Pian M, Dillon L, Barajas D, Bartholomew LK. Transition to adult care: systematic assessment of adolescents with chronic illnesses and their medical teams. J Pediatr. 2011;159(6):994–998, e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Applebaum MA, Lawson EF, von Scheven E. Perception of transition readiness and preferences for use of technology in transition programs: teens’ ideas for the future. Int J Adolesc Med Health. 2013;25(2):119–125 [DOI] [PubMed] [Google Scholar]
- 29.van der Meer V, van Stel HF, Detmar SB, Otten W, Sterk PJ, Sont JK. Internet-based self-management offers an opportunity to achieve better asthma control in adolescents. Chest. 2007;132(1):112–119 [DOI] [PubMed] [Google Scholar]
- 30.Omachi TA, Sarkar U, Yelin EH, Blanc PD, Katz PP. Lower health literacy is associated with poorer health status and outcomes in chronic obstructive pulmonary disease. J Gen Intern Med. 2013;28(1):74–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155(2):97–107 [DOI] [PubMed] [Google Scholar]
- 32.DeWalt DA, Hink A. Health literacy and child health outcomes: a systematic review of the literature. Pediatrics. 2009;124(suppl 3):S265–S274 [DOI] [PubMed] [Google Scholar]
- 33.Borzekowski DL. Considering children and health literacy: a theoretical approach. Pediatrics. 2009;124(suppl 3):S282–S288 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.