Abstract
Background and Objectives:
To estimate the effect of surgeon volume on key perioperative outcomes after all modes of hysterectomy.
Methods:
We performed a review of 1914 hysterectomies performed at a large, academic tertiary-care hospital. Women who underwent abdominal, laparoscopic, vaginal, or robotic hysterectomy for benign non-obstetric indications in 2006, 2009, and 2010 were included.
Results:
Gynecologic surgeons were categorized according their average annual hysterectomy case volume: low volume (<11 cases per year), intermediate volume (11–50 cases per year), and high-volume (>51 cases per year). Taking all modes of hysterectomy together, surgeries performed by high-volume surgeons required a shorter operative time (155.11 minutes vs 199.19–203.35 minutes, P < .001) and resulted in less estimated blood loss compared with low- and intermediate-volume surgeons (161.09 mL vs 205.58–237.96 mL, P < .001). The 3 surgical volume groups did not differ from each other significantly in the conversion to laparotomy, readmission rate, or incidence of intraoperative or postoperative complications. These findings were maintained when subgroup analyses were performed by type of hysterectomy, with few exceptions. In the subgroup of vaginal hysterectomies by intermediate-volume surgeons, there were slightly more postoperative complications. There were fewer intraoperative complications in laparoscopic/robotic hysterectomies performed by high-volume surgeons, though not statistically significant.
Conclusions:
Hysterectomies performed by high-volume surgeons at our institution during the 3-year study period were associated with shorter operative times and less estimated blood loss.
Keywords: Hysterectomy, Surgeon volume
INTRODUCTION
Major complications of hysterectomy are rare.1 However, because hysterectomy is one of the most commonly performed surgical procedures in women,2 efforts to decrease risks associated with this procedure have the potential for public health impact. One such effort may include optimizing referral to surgeons with appropriate experience and volumes of major gynecologic cases. In many surgical fields the relationship between surgical volume and operative outcome has been investigated. For example, one study of greater than 470 000 Medicare patients undergoing either cardiovascular procedures or cancer resections found that the operative mortality rate was strongly and inversely related to surgeon volume for each procedure.3 In the field of gynecology, this relationship has been examined with regard to procedures including abdominal myomectomy, hysteroscopic myomectomy, cancer surgery, pubovaginal sling placement, and pelvic reconstruction.4–12 Specifically regarding hysterectomy performed for benign indications, however, the available data are limited and conflicting.
In this study we aim to address two key issues raised by prior work. Most past studies on this subject have used relatively low cutoff values to define high-volume surgical status, equating high volume to approximately one hysterectomy per month. Although the number of cases required to achieve initial skill mastery for hysterectomy has been estimated at 30 cases,13,14 it is not evident how this translates to annual case volume recommendations because maintenance of performance may require frequency and repetition. We aim to stratify surgical volume categories beyond what has previously been done to determine whether there is a greater difference observed between very high-volume surgeons and low- or intermediate-volume surgeons. Second, much of the available data are limited by long periods of data collection and isolated examination of only one route of hysterectomy. This may cause particular difficulty for analysis of laparoscopic hysterectomy because it is characterized by continually evolving technology and more variation in practice patterns. By using the database of all hysterectomies (including abdominal, vaginal, laparoscopic, and robotic) performed at Brigham and Women's Hospital in the years 2006, 2009, and 2010, we hope to gain more insight into patterns of perioperative outcomes.
MATERIALS AND METHODS
Data Source
Internal review board approval from Partner's Healthcare was obtained. All hysterectomies performed in 2006, 2009, and 2010 at Brigham and Women's Hospital were identified by use of data from the billing department. All abdominal, vaginal, laparoscopic, and robotic-assisted laparoscopic hysterectomies were included. To limit confounding variables, cases performed for oncologic or obstetric indications were excluded. Of note, most cases are completed with resident or fellow assistance because the hospital is an academic institution. The creation of this hysterectomy database has been described in detail elsewhere and was used initially to evaluate evolving hysterectomy practice between the years 2006 and 2009.15 The existing hysterectomy database was expanded to include additional data from 2010 for the purposes of this study.
Surgeon Volume
The number of hysterectomies performed annually was determined for each surgeon by review of case statistics from our database. Consideration was given to the fact that surgeons may also practice at outside institutions; therefore the report of hysterectomy volume at all other institutions was also taken into account. Information about operative experience at outside institutions was obtained from the department administration and confirmed with medical records at those institutions. The case load of hysterectomies performed annually over the study period was then averaged to generate the average annual hysterectomy volume for each surgeon. After review of a histogram of the distribution of hysterectomy volumes (Figure 1), surgeons were categorized as low-volume (<11 hysterectomies per year), intermediate-volume (11–50 hysterectomies per year), or high-volume (>50 procedures per year) surgeons.
Figure 1.
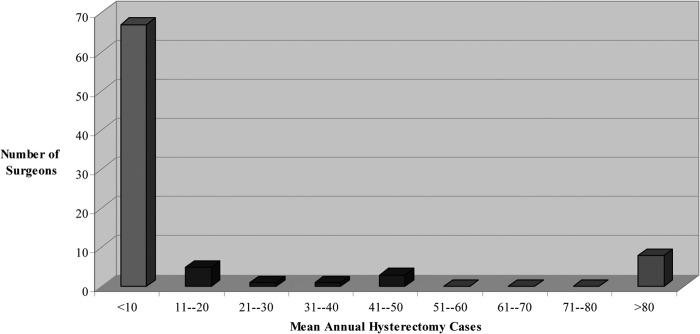
Annual hysterectomy volume of surgeons. The low-volume group was defined as <11 annual hysterectomy cases. The medium-volume group was defined as 11 to 50 annual hysterectomy cases. The high-volume group was defined as >50 annual hysterectomy cases.
Outcomes
Information was abstracted from the medical record regarding age, length of hospital stay, and operative time (reported as time in and time out of the operating room). Patient charts were reviewed for body mass index, parity, prior abdominal surgeries, indication, procedure, estimated blood loss during surgery, pathology report, uterine weight, intraoperative complications, and postoperative complications. Intraoperative complications included estimated blood loss ≥1000 mL, vessel or visceral organ injury, and major cardiac/pulmonary events. By use of a previously reported complication grading scheme,16 major postoperative complications included readmission, reoperation, ileus, and pulmonary embolism; minor postoperative complications included infections (urinary tract, lung, wound, or fever), urinary retention, and deep vein thrombosis.
Statistical Analysis
Baseline characteristics and perioperative outcomes were compared across hysterectomies performed by three distinct categories of operators, classified based on their average annual surgical volume. We used the one-way analysis of variance test to compare continuous variables and the χ2 test or Fisher exact test to compare categorical variables. All comparisons were considered to have reached statistical significance at a value of ≤ .05. We also performed the Bonferroni correction for multiple comparisons where applicable.
RESULTS
A total of 1914 hysterectomies were performed in 2006, 2009, and 2010 for benign non-obstetric indications. Of these cases, 33.7% (n = 644) were abdominal, 20.5% (n = 393) vaginal, and 45.8% (877) laparoscopic or robotic. The number of hysterectomies per year remained stable, with 635 procedures in 2006, 643 procedures in 2009, and 636 procedures in 2010.
Figure 1 shows the breakdown of surgical volume among the 85 gynecologic surgeons who contributed cases to this study. There were 67 surgeons (78.8%) included in the low-volume group (<11 hysterectomies per year), 10 (11.8%) in the intermediate-volume group (11–50 hysterectomies per year), and 8 (9.4%) in the high-volume group (>50 hysterectomies per year). Overall, 43.8% (838) of the hysterectomies were performed by high-volume surgeons, 35.6% (682) by intermediate-volume surgeons, and 20.6% (394) by low-volume surgeons.
The patients who underwent hysterectomy by a low-, intermediate-, or high-volume surgeon did not differ from each other significantly in terms of parity or surgical history before undergoing a hysterectomy (Table 1). The participants in the cohort of hysterectomies performed by high-volume surgeons were older and were noted to have a slightly higher body mass index. Although it did not reach statistical significance, the patients on whom high-volume surgeons operated were noted to have a more frequent history of laparotomy (31.7% in both low- and intermediate-volume groups vs 36.75% in high-volume group, P = .061).
Table 1.
Baseline Characteristics of Hysterectomy Cohort by Surgeon Volume Category
| Low Volume (n = 394) | Intermediate Volume (n = 682) | High Volume (n = 838) | P Value | |
|---|---|---|---|---|
| Age (y) | 46.83 ± 7.83 | 48.24 ± 9.26 | 50.95 ± 11.51 | <.001 |
| Parity | 1.88 ± 1.5 | 1.83 ± 1.37 | 1.86 ± 1.5 | .863 |
| BMIa (kg/m2) | 28.57 ± 6.41 | 27.29 ± 5.89 | 28.93 ± 7.6 | .002 |
| Previous laparoscopy | 98 (24.87) | 161 (23.61) | 207 (24.7) | .852 |
| Previous laparotomy | 124 (31.7) | 216 (31.67) | 308 (36.75) | .061 |
| Type of hysterectomy | ||||
| Abdominal | 168 (42.64) | 134 (19.65) | 342 (40.81) | <.001 |
| Vaginal | 80 (20.3) | 144 (21.11) | 169 (20.17) | |
| Laparoscopic | 139 (35.28) | 395 (57.92) | 303 (36.16) | |
| Robotic | 7 (1.78) | 9 (1.32) | 24 (2.86) | |
| Findingsb | ||||
| Fibroids | 254 (64.47) | 475 (69.65) | 414 (49.4) | <.001 |
| Endometriosis | 36 (9.14) | 72 (10.56) | 92 (10.98) | .611 |
| Urogynecologic problems | 72 (18.27) | 140 (20.53) | 156 (18.62) | .556 |
| Adhesions | 115 (29.19) | 169 (24.78) | 236 (28.16) | .202 |
Data are given as mean ± SD or number (percent).
BMI = body mass index.
The total does not add up to 100% because cases may have had >1 finding.
The route of hysterectomy differed significantly by surgical volume category, with abdominal hysterectomy being the most common approach for both the low- and high-volume surgeons (42.64% of low-volume cases, 19.65% of intermediate-volume cases, and 40.81% of high-volume cases; P < .001). The primary mode of hysterectomy for intermediate-volume surgeons was laparoscopic (57.92% of cases), whereas robotic-assisted laparoscopic hysterectomies were performed more frequently by the high-volume surgeons (2.86% of cases). Regarding case mix, low- and intermediate-volume surgeons were predominantly operating on cases of uterine fibroids whereas the high-volume group had more varied indications (fibroids in 64.47% and 69.65% of cases in the low-and intermediate-volume groups vs 49.4% in the high-volume group, P < .001). The operative findings of endometriosis, adhesions, or urogynecologic issues (mainly prolapse) did not differ significantly in the three groups under study.
Perioperative outcomes for all hysterectomies performed by low-, intermediate-, and high-volume surgeons are shown in Table 2. A significant decline in operative time (203.35 minutes in low-volume group, 199.19 minutes in intermediate-volume group, and 155.11 minutes in high-volume group; P < .001) and estimated blood loss (237.96 mL in low-volume group, 205.58 mL in intermediate-volume group, and 161.09 mL in high-volume group; P < .001) was seen as the surgical volume increased. On average, surgeries performed by high-volume operators required 44 to 48 fewer minutes and resulted in 44 to 76 mL less blood loss compared with intermediate- and low-volume surgeons. Interestingly, the mean length of hospital stay was found to be slightly higher in the surgeries performed by high-volume surgeons (1.8 days in low-volume group, 1.35 days in intermediate-volume group, and 2.06 days in high-volume group; P < .001). The three surgical volume groups did not differ from each other significantly with regard to conversion to laparotomy, readmission rate, or incidence of intraoperative or postoperative complications.
Table 2.
Perioperative Outcomes of Hysterectomy Cohort by Surgeon Volume Category
| Low Volume (n = 394) | Intermediate Volume (n = 682) | High Volume (n = 838) | P Value | |
|---|---|---|---|---|
| Operating time (min) | 203.35 ± 64.34 | 199.19 ± 69.41 | 155.11 ± 53.98 | <.001 |
| Length of hospital stay (d) | 1.8 ± 1.32 | 1.35 ± 1.39 | 2.06 ± 1.67 | <.001 |
| Uterine weight (g) | 305.39 ± 346.88 | 312.12 ± 398.75 | 300.95 ± 469.99 | .877 |
| EBLa (mL) | 237.96 ± 254.29 | 205.58 ± 238.9 | 161.09 ± 255.46 | <.001 |
| Conversionb | 9 (3.98) | 15 (2.74) | 10 (2.02) | .314 |
| Readmission | 19 (4.82) | 18 (2.64) | 36 (4.3) | .123 |
| Intraoperative complications | 14 (3.55) | 23 (3.37) | 15 (1.79) | .087 |
| Postoperative complications | 44 (11.17) | 73 (10.7) | 104 (12.41) | .565 |
| Total complications | 55 (13.96) | 88 (12.9) | 114 (13.6) | .87 |
Data are given as mean ± SD or number (percent).
EBL = estimated blood loss.
For conversion outcome, total eligible cases equals 1270 (excluding abdominal).
To better appreciate the potential differences among surgical volume groups, the perioperative characteristics were analyzed separately for each mode of hysterectomy (Tables 3–5). When we looked at abdominal hysterectomies alone (Table 3), the relationship of shorter operative time (202.54 minutes in low-volume group, 184.39 minutes in intermediate-volume group, and 164.27 minutes in high-volume group; P < .001) and lower estimated blood loss (321.96 mL in low-volume group, 379.54 mL in intermediate-volume group, and 253.89 mL in high-volume group; P < .001) among high-volume surgeons is maintained. The length of stay is also longer in the high-volume abdominal hysterectomy group; however, no differences are seen regarding readmission or intraoperative or postoperative complications.
Table 3.
Perioperative Outcomes by Surgeon Volume Category for Abdominal Hysterectomy
| Low Volume (n = 168) | Intermediate Volume (n = 134) | High Volume (n = 342) | P Value | |
|---|---|---|---|---|
| Operating time (min) | 202.54 ± 57.26 | 184.39 ± 52.07 | 164.27 ± 53.16 | <.001 |
| Length of hospital stay (d) | 2.55 ± 1.35 | 2.57 ± 1.63 | 3.28 ± 1.85 | <.001 |
| Uterine weight (g) | 438.13 ± 440.42 | 733.30 ± 659.47 | 455.39 ± 631.45 | <.001 |
| EBLa (mL) | 321.96 ± 262.63 | 379.54 ± 291.54 | 253.89 ± 331.46 | <.001 |
| Conversionb | NA | NA | NA | NA |
| Readmission | 7 (4.17) | 3 (2.24) | 19 (5.56) | .283 |
| Intraoperative complications | 4 (2.38) | 3 (2.24) | 8 (2.34) | .997 |
| Postoperative complications | 22 (13.10) | 20 (14.93) | 63 (18.42) | .276 |
| Total complications | 26 (15.48) | 23 (17.16) | 68 (19.88) | .452 |
Data are given as mean ± SD or number (percent).
EBL = estimated blood loss; NA = Not Applicable.
For conversion outcome, total eligible cases equals 1270 (excluding abdominal).
Table 4.
Perioperative Outcomes by Surgeon Volume Category for Vaginal Hysterectomy
| Low Volume (n = 80) | Intermediate Volume (n = 144) | High Volume (n = 169) | P Value | |
|---|---|---|---|---|
| Operating time (min) | 178.64 ± 62.83 | 194.12 ± 46.67 | 114.09 ± 31.84 | <.001 |
| Length of hospital stay (d) | 1.51 ± .69 | 1.66 ± .84 | 1.30 ± .64 | .004 |
| Uterine weight (g) | 123.05 ± 110.75 | 88.81 ± 59.31 | 107.11 ± 108.69 | .028 |
| EBLa (mL) | 218.37 ± 233.2 | 215.36 ± 264.22 | 106.83 ± 155.65 | <.001 |
| Conversionb | 1 (1.25) | 1 (.69) | 2 (1.18) | .888 |
| Readmission | 4 (5) | 4 (2.78) | 5 (2.96) | .635 |
| Intraoperative complications | 2 (2.5) | 5 (3.47) | 1 (.59) | .188 |
| Postoperative complications | 5 (6.25) | 28 (19.44) | 14 (8.28) | .002 |
| Total complications | 7 (8.75) | 31 (21.53) | 15 (8.88) | .003 |
Data are given as mean ± SD or number (percent).
EBL = estimated blood loss.
For conversion outcome, total eligible cases equals 1270 (excluding abdominal).
Table 5.
Perioperative Outcomes by Surgeon Volume Category for Laparoscopic and Robotic Hysterectomy
| Low Volume (n = 146) | Intermediate Volume (n = 404) | High Volume (n = 327) | P Value | |
|---|---|---|---|---|
| Operating time (min) | 217.8 ± 68.86 | 205.9 ± 79.66 | 166.83 ± 53.91 | <.001 |
| Length of hospital stay (d) | 1 ± 1.02 | .77 ± 1.04 | 1.15 ± .83 | <.001 |
| Uterine weight (g) | 252.57 ± 233.43 | 252.02 ± 208.54 | 239.61 ± 309.38 | .779 |
| EBLa (mL) | 152.56 ± 225.25 | 144.06 ± 172.37 | 92.05 ± 157.60 | <.001 |
| Conversionb | 8 (5.48) | 14 (3.47) | 8 (2.45) | .254 |
| Readmission | 8 (5.48) | 11 (2.72) | 12 (3.67) | .299 |
| Intraoperative complications | 8 (5.48) | 15 (3.71) | 6 (1.83) | .101 |
| Postoperative complications | 17 (11.64) | 25 (6.19) | 27 (8.26) | .105 |
| Total complications | 22 (15.07) | 34 (8.42) | 31 (9.48) | .066 |
Data are given as mean ± SD or number (percent).
EBL = estimated blood loss.
For conversion outcome, total eligible cases equals 1270 (excluding abdominal).
For the subgroup of vaginal hysterectomy (Table 4), the high-volume surgeons had a faster operative time (178.64 minutes in low-volume group, 194.12 minutes in intermediate-volume group, and 114.09 minutes in high-volume group; P < .001), lower estimated blood loss (218.37 mL in low-volume group, 215.36 mL in intermediate-volume group, and 106.83 mL in high-volume group; P < .001), and shorter hospital stay. Of note, postoperative complications from vaginal hysterectomy were highest in the intermediate-volume group (6.25% in low-volume group, 19.44% in intermediate-volume group, and 9.28% in high-volume group; P = .002). Conversion to laparotomy, readmission rate, and intraoperative complications did not differ by surgical volume cohort.
Analysis of solely laparoscopic and robot-assisted laparoscopic hysterectomies also showed a faster operative time (217.8 minutes in low-volume group, 205.9 minutes in intermediate-volume group, and 166.83 minutes in high-volume group; P < .001) and decreased blood loss (152.56 mL in low-volume group, 144.06 mL in intermediate-volume group, and 92.05 mL in high-volume group; P < .001) in the high-volume group. In addition, the length of hospital stay was highest in the high-volume group, although no difference was seen in readmissions. The difference in total complications neared statistical significance, with fewer intraoperative complications seen in the intermediate- and high-volume groups (15.07% in low-volume group, 8.42% in intermediate-volume group, and 9.48% in high-volume group; P = .066).
DISCUSSION
Concerning hospital-level data for abdominal hysterectomy, it has been suggested that academic status or hospital volume may not be as important a modifier of surgical outcomes for this common procedure of relatively lower risk as compared with more complex operations.17 Similar conclusions were reached when surgeon-level data were analyzed in a retrospective cohort study of greater than 8000 women who underwent abdominal hysterectomy at one institution between 1995 and 2005.18 In that study the authors asserted that although high-volume surgeons (defined by completion of greater than 10 hysterectomies per year) have fewer complications and shorter operative times, the overall rate of complications is low enough to deem hysterectomy safely performed by both groups. The relationship between surgeon volume and perioperative outcomes from vaginal hysterectomy has been assessed through an analysis of greater than 77 000 cases taken from a national database for the years 2003–2007.19 Findings included both lower perioperative complications and resource use in the high-volume vaginal surgeon group (defined by completion of greater than 13 vaginal hysterectomies per year). Volume-related outcomes from laparoscopic hysterectomy have also been examined in a retrospective analysis of 1000 procedures from a single institution during the years 1999–2008.13 This study did not find any differences between the high- and low-volume surgeon groups aside from a shorter operative time for high-volume surgeons (loosely defined as completion of greater than 30 cases, not specific to laparoscopic hysterectomy or annual case volume). However, a large database analysis of 124 615 benign laparoscopic hysterectomies performed during the years 2000–2010 found significantly decreased risk of overall morbidity, complications, prolonged hospitalization, and resource utilization in high-volume surgeons (defined as greater than 14.1 operations per year).20 Finally, a more recent prospective cohort study of 1534 laparoscopic hysterectomies performed over a 1-year study period showed no effect of annual hysterectomy surgical volume on blood loss, operative time, or adverse events.21 Interestingly, the authors did identify an intangible surgical skills factor that was associated with procedure success and noted that increasing cumulative surgical experience (up to 125 procedures) was also associated with improved outcomes.
With the benefit of a large hysterectomy database and expanded categorization of surgeon volume, we confirm a strong relationship between operator surgical volume and both shorter operative time and lower estimated blood loss. These outcomes were strikingly maintained for all modes of hysterectomy, building on prior findings.13,18,19 Interestingly, the incidence of conversion to laparotomy and readmission rate did not differ among surgical volume cohorts for any of the modes of hysterectomy. Few differences were seen in the occurrence of complications, with the highest occurrence of postoperative complications from vaginal hysterectomy for the intermediate-volume cohort and highest occurrence of total complications from laparoscopic/robotic-assisted laparoscopic hysterectomy in the low-volume cohort.
The findings regarding length of stay are inconsistent among modes of hysterectomy, with decreased hospital stay after vaginal hysterectomy by high-volume surgeons but increased hospital stay after abdominal or laparoscopic/robotic hysterectomy by high-volume surgeons. One possible explanation for the increased length of stay in selected high-volume cohorts is a greater complexity of cases undertaken by the more referral-based high-volume surgeons, although this was not reflected in terms of higher uterine weights for this group. Arguably, uterine weight is an imperfect predictor of case complexity, and other unmitigated clinical factors may be at play, such as surgeon specialization. For example, many of the surgeons in the high-volume group are gynecologic oncologists who perform predominantly abdominal or laparoscopic/robotic cases; even when one analyzes only their benign hysterectomies, these surgeons are likely dealing with a more challenging case mix. In addition, hospital stay may reflect physician preference or practice patterns.
Strengths of this study include the variety of gynecologic surgeons included, with a selection of subspecialists and generalists. By limiting analysis to a 5-year time frame (2006, 2009, and 2010) at one institution, the effect of extrinsic factors on perioperative outcomes is diminished. We have also stratified surgical volume categories more finely than previous work on the subject in an attempt to observe the breakdown of operator experience. Limitations of this study include its retrospective nature and inherent potential for errors in data collection. In addition, one of our main outcomes measures, estimated blood loss, is a subjectively reported value (surgeon's estimated blood loss as listed in the operative note) as opposed to being objectively verified. Although we attempted to accurately code each physician's average annual hysterectomy case volume, we did not account for cumulative years of experience or other factors such as learning curve or fellowship training. This variety of providers and types of cases is a benefit but also may introduce confounding factors that are not entirely accounted for in our study design. In addition, we may have an incomplete sample size to detect rare outcomes such as major complications and conversion to laparotomy.
CONCLUSION
We have established that high-volume surgeons have shorter operative times and less blood loss for all modes of hysterectomy. Prior work from our institution has shown that charges based on operating room time account for the vast majority of total operative charges for hysterectomy (unpublished data, presented in abstract form at 2010 American Association of Gynecologic Laparoscopists AAGL meeting by K.N. Wright). Given the current focus on containing health care costs, the importance of operative time savings cannot be overlooked. It is uncertain, however, whether the benefits of operator experience extend to other perioperative outcomes. This may in part reflect practices already in place at our institution that allow for accurate referral of cases to the appropriate surgical provider, thereby mitigating gradients in perioperative complications. At our hospital, we have seen a trend of low- and intermediate-volume surgeons transitioning to minimally invasive modes of access, which highlights the need for continued training to maintain optimal patient outcomes, in addition to appropriate surgical referral networks as needed.
Contributor Information
Florentien E. M. Vree, Department of Obstetrics and Gynecology, Academic Medical Center, Amsterdam, the Netherlands.; Division of Minimally Invasive Gynecologic Surgery, Department of Obstetrics and Gynecology, Brigham and Women's Hospital, Boston, MA, USA.
Sarah L. Cohen, Division of Minimally Invasive Gynecologic Surgery, Department of Obstetrics and Gynecology, Brigham and Women's Hospital, Boston, MA, USA..
Niraj Chavan, Department of Obstetrics and Gynecology, Flushing Hospital Medical Center, Queens, NY, USA..
Jon I. Einarsson, Division of Minimally Invasive Gynecologic Surgery, Department of Obstetrics and Gynecology, Brigham and Women's Hospital, Boston, MA, USA..
References:
- 1. McPherson K, Metcalfe MA, Herbert A, et al. Severe complications of hysterectomy: the VALUE study. BJOG. 2004;111:688–694 [DOI] [PubMed] [Google Scholar]
- 2. Whiteman MK, Hillis SD, Jamieson DJ, et al. Inpatient hysterectomy surveillance in the United States, 2000–2004. Am J Obstet Gynecol. 2008;198(1):34.e1–34.e7 [DOI] [PubMed] [Google Scholar]
- 3. Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117–2127 [DOI] [PubMed] [Google Scholar]
- 4. Anger JT, Rodriguez LV, Wang Q, Pashos CL, Litwin MS. The role of provider volume on outcomes after sling surgery for stress urinary incontinence. J Urol. 2007;177:1457–62 [DOI] [PubMed] [Google Scholar]
- 5. Bristow RE, Zahurak ML, Diaz-Montes TP, Giuntoli RL, Armstrong DK. Impact of surgeon and hospital ovarian cancer surgical case volume on in-hospital mortality and related short-term outcomes. Gynecol Oncol. 2009;115:334–338 [DOI] [PubMed] [Google Scholar]
- 6. Hanstede MM, Emanuel MH, Stewart EA. Outcomes for abdominal myomectomies among high-volume surgeons. J Reprod Med. 2008;53:941–946 [PubMed] [Google Scholar]
- 7. Sung VW, Rogers ML, Myers DL, Clark MA. Impact of hospital and surgeon volumes on outcomes following pelvic reconstructive surgery in the United States. Am J Obstet Gynecol. 2006;195:1778–1783 [DOI] [PubMed] [Google Scholar]
- 8. Wright JD, Lewin SN, Deutsch I, Burke WM, Sun X, Herzog TJ. The influence of surgical volume on morbidity and mortality of radical hysterectomy for cervical cancer. Am J Obstet Gynecol. 2011;205(3):225.e1–225.e7 [DOI] [PubMed] [Google Scholar]
- 9. Wright JD, Hershman DL, Burke WM, et al. Influence of surgical volume on outcome for laparoscopic hysterectomy for endometrial cancer. Ann Surg Oncol. 2012;19(3):948–958 [DOI] [PubMed] [Google Scholar]
- 10. Yasunaga H, Nishii O, Hirai Y, Ochiai K, Matsuyama Y, Ohe K. Impact of surgeon and hospital volumes on short-term postoperative complications after radical hysterectomy for cervical cancer. J Obstet Gynaecol Res. 2009;35:699–705 [DOI] [PubMed] [Google Scholar]
- 11. Betjes HE, Hanstede MM, Emanuel MH, Stewart EA. Hysteroscopic myomectomy and case volume hysteroscopic myomectomy performed by high- and low-volume surgeons. J Reprod Med. 2009;54(7):425–428 [PubMed] [Google Scholar]
- 12. Díaz-Montes TP, Zahurak ML, Giuntoli RL, II, Gardner GJ, Bristow RE. Uterine cancer in Maryland: impact of surgeon case volume and other prognostic factors on short-term mortality. Gynecol Oncol. 2006;103(3):1043–1047 [DOI] [PubMed] [Google Scholar]
- 13. Tunitsky E, Citil A, Ayaz R, Esin S, Knee A, Harmanli O. Does surgical volume influence short-term outcomes of laparoscopic hysterectomy? Am J Obstet Gynecol. 2010;203:24.e1–24.e6 [DOI] [PubMed] [Google Scholar]
- 14. Altgassen C, Michels W, Schneider A. Learning laparoscopic-assisted hysterectomy. Obstet Gynecol. 2004;104:308–313 [DOI] [PubMed] [Google Scholar]
- 15. Jonsdottir GM, Jorgensen S, Cohen SL, et al. Increasing minimally invasive hysterectomy: effect on cost and complications. Obstet Gynecol. 2011;117:1142–1149 [DOI] [PubMed] [Google Scholar]
- 16. Garry R, Fountain J, Mason S, et al. The eVALuate study: two parallel randomised trials, one comparing laparoscopic with abdominal hysterectomy, the other comparing laparoscopic with vaginal hysterectomy. BMJ. 2004;328(7432):129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Juillard C, Lashoher A, Sewell CA, Uddin S, Griffith JG, Chang DC. A national analysis of the relationship between hospital volume, academic center status, and surgical outcomes for abdominal hysterectomy done for leiomyoma. J Am Coll Surg. 2009;208:599–606 [DOI] [PubMed] [Google Scholar]
- 18. Hanstede MM, Wise LA, Stewart EA, Feldman S. The relation of annual surgeon case volume to clinical outcomes and resource utilization in abdominal hysterectomy. J Reprod Med. 2009;54:193–202 [PubMed] [Google Scholar]
- 19. Rogo-Gupta LJ, Lewin SN, Kim JH, et al. The effect of surgeon volume on outcomes and resource use for vaginal hysterectomy. Obstet Gynecol. 2010;116:1341–1347 [DOI] [PubMed] [Google Scholar]
- 20. Wallenstein MR, Ananth CV, Kim JH, et al. Effect of surgical volume on outcomes for laparoscopic hysterectomy for benign indications. Obstet Gynecol. 2012;119(4):709–716 [DOI] [PubMed] [Google Scholar]
- 21. Twijnstra AR, Blikkendaal MD, van Zwet EW, van Kesteren PJ, de Kroon CD, Jansen FW. Predictors of successful surgical outcome in laparoscopic hysterectomy. Obstet Gynecol 2012;119(4):700–708 [DOI] [PubMed] [Google Scholar]


