SUMMARY
Posterior canal benign paroxysmal positional vertigo (BPPV) is the most frequent form of BPPV. It is characterized by a paroxysmal positioning nystagmus evoked through Dix-Hallpike and Semont positioning tests. Anterior canal BPPV (AC) is more rare than posterior canal BPPV; it presents a prevalent down beating positioning nystagmus, with a torsional component clockwise for the left canal, counterclockwise for the right canal. Due to the possible lack of the torsional component, it is sometimes difficult to identify the affected ear. An apogeotropic variant of posterior BPPV (APC) has recently been described, characterised by a paroxysmal positional nystagmus in the opposite direction to the one evoked in posterior canal BPPV: the linear component is down-beating, the torsional component is clockwise for the right canal, counter-clockwise for the left canal, so that a contra-lateral anterior canal BPPV could be simulated. During a 16 month period, of 934 BPPV patients observed, the authors identified 23 (2.5%) cases of apogeotropic posterior canal BPPV and 11 (1.2%) cases of anterior canal BPPV, diagnosed using the specific oculomotor patterns described in the literature. Anterior canal BPPV was treated with the repositioning manoeuvre proposed by Yacovino, which does not require identification of the affected side, whereas apogeotropic posterior canal BPPV was treated with the Quick Liberatory Rotation manoeuvre for the typical posterior canal BPPV, since in the Dix-Hallpike position otoliths are in the same position if they come either from the ampullary arm or from the non-ampullary arm. The direct resolution of BPPV (one step therapy) was obtained in 12/34 patients, 8/23 patients with APC and 4/11 patients with AC; canalar conversion into typical posterior canal BPPV, later treated through Quick Liberatory Rotation (two-step therapy), was obtained in 19 patients,14/23 with APC and 5/11 with AC. Three patients were lost to follow-up. Considering the effects of therapeutic manoeuvres, the authors propose a grading system for diagnosis of AC and APC: "certain" when a canalar conversion in ipsilateral typical posterior canal BPPV is obtained; "probable" when APC or AC are directly resolved; "possible" when disease is not resolved and cerebral neuroimaging is negative for neurological diseases. Our results show that the oculomotor patterns proposed in the literature are effective in diagnosing APC and AC, and that APC is more frequent than AC. Both of these rare forms of vertical canal BPPV can be treated effectively with liberatory manoeuvres.
KEY WORDS: Anterior canal BPPV, Posterior canal BPPV, Apogeotropic posterior canal BPPV, Quick Liberatory Rotation manoeuvre, Yacovino manoeuvre
RIASSUNTO
La VPPB da canalolitiasi posteriore è la forma più frequentemente osservata; essa è caratterizzata da un nistagmo parossistico posizionale evocato dal posizionamento di Dix-Hallpike o di Semont con una componente lineare up-beat ed una componente torsionale oraria per il canale posteriore sinistro, antioraria per il canale posteriore destro. La VPPB da canalolitiasi anteriore è più rara per la posizione più alta del canale anteriore ed è caratterizzata da un nistagmo parossistico evocabile nei posizionamenti Head-Hanging, con una componente lineare down-beating prevalente rispetto ad una incostante componente torsionale, oraria per il canale sinistro, antioraria per quello destro. La incostante presenza della componente torsionale rende talvolta difficile il riconoscimento del lato malato. Recentemente è stata descritta una variante apogeotropa della canalolitiasi posteriore caratterizzata da un quadro nistagmico evocato invertito rispetto alla canalolitiasi posteriore tipica, e cioè con una componente lineare down-beating ed una componente torsionale antioraria per il canale sinistro, oraria per il canale destro, cosicché può essere simulata una canalolitiasi anteriore controlaterale. In un periodo di 16 mesi, applicando come criteri diagnostici i patterns oculomotori descritti in letteratura, gli Autori hanno identificato, su un totale di 934 casi di VPPB, 23 casi di VPPB da canalolitiasi posteriore apogeotropa (2,5%) ed 11 casi di VPPB da canalolitiasi anteriore (1,1%). La VPPB da canalolitiasi anteriore è stata trattata con la manovra di Yacovino, che non necessita dell'individuazione del lato affetto, mentre la VPPB da canalolitiasi posteriore apogeotropa è stata trattata con la manovra di Rotazione Rapida Liberatoria, basandosi sulla considerazione che gli otoconi, sia che provengano dal braccio ampollare che da quello non ampollare del canale posteriore, nella posizione finale dei test diagnostici si trovino nella stessa parte del canale. La risoluzione diretta della VPPB è stata ottenuta con le manovre terapeutiche utilizzate in 8/23 canalolitiasi posteriori apogeotrope ed in 4/11 canalolitiasi anteriori (one-step therapy), mentre la conversione in una canalolitiasi posteriore tipica, trattata con manovra di Rotazione Rapida Liberatoria, è stata osservata in 14/23 canalolitiasi posteriori apogeotrope ed in 5/11 canalolitiasi anteriori (two-step therapy). Tre pazienti sono stati persi al follow-up. Considerando gli effetti delle manovre terapeutiche, gli Autori propongono un sistema di gradazione della diagnosi di VPPB da canalolitiasi posteriore apogeotropa e di VPPB da canalolitiasi anteriore: "grado certo" quando si ottiene una conversione in canalolitiasi posteriore tipica, "grado probabile" quando si ottiene direttamente la risoluzione della malattia,"grado possibile" quando la malattia non si risolve e la RMN cerebrale non evidenzia segni di patologia neurologica. I nostri risultati mostrano come i patterns oculomotori già descritti in letteratura siano efficaci nella diagnosi di VPPB da canalolitiasi posteriore apogeotropa e di VPPB da canalolitiasi anteriore e che la canalolitiasi posteriore apogeotropa sia più frequente rispetto alla canalolitasi anteriore. Entrambe le forme rispondono bene alla terapia liberatoria.
Introduction
The topographic classification of benign paroxysmal positional vertigo (BPPV) is based on the position of otoliths in the semicircular canals, which can, hypothetically, be inferred from the oculomotor patterns observed during positioning tests 1. The posterior canal (Fig. 1a) is involved in 80% of cases and the lateral canal with its geotropic and apogeotropic variants in 15%, whereas the rarest forms of BPPV (5%) are anterior canalolithiasis (Fig. 2), described in 1987 by Katsarkas 2, "short arm canalolithiasis" 3 and apogeotropic posterior canalolithiasis (Fig. 1b), recently described by Vannucchi who, on the basis of the pattern of ocular movement induced by positioning tests, hypothesised the presence of debris in the distal part of the non-ampullary arm of the posterior canal 4 5. In 1995, Agus 6 described a "reversed" clinical picture of posterior canalolithiasis with a down-beating paroxysmal nystagmus characterised by torsional components clockwise for the right Dix-Hallpike positioning, and counter-clockwise for left Dix-Hallpike positioning; later, the possible existence of an apogeotropic posterior form was theorised by Giannoni 7.
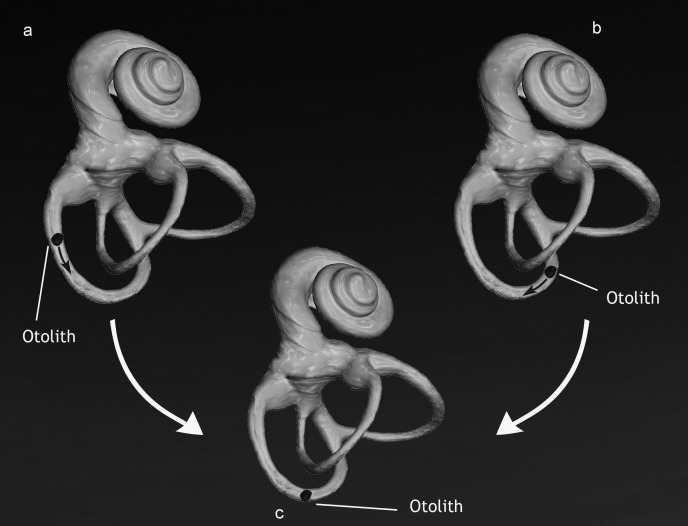
Fig. 1.
Left posterior canal BPPV in sitting position. a: TPC: otoliths are in the ampullary arm of the canal; b: APC: otoliths are in the non-ampullary arm of the canal.
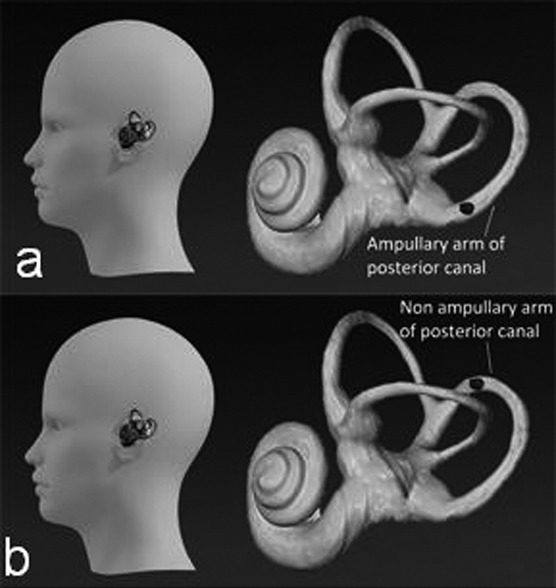
Fig. 2.
Anterior canal BPPV in sitting (a) and in straight-head-hanging positioning (b).
Typical posterior canal BPPV, the most frequent form of BPPV, is characterised by a paroxysmal nystagmus evoked through the Dix-Hallpike test; the nystagmus is torsional clockwise for the left side, counter-clockwise for the right side, with a vertical up-beating component. Anterior canal BPPV (AC) is characterised by an intensity- variable vertical down-beating paroxysmal nystagmus evoked through straight-head hanging and Dix-Hallpike positioning tests, without inversion of the down-beating vertical nystagmus in returning to the sitting position. The torsional component is not always clear and less intense than the vertical one; it is clockwise for the left anterior canal, counter-clockwise for the right anterior canal, regardless of the positioning side; latency is absent or short and nystagmus is sometimes fatigable; positioning usually provokes serious vertiginous symptoms, whereas head hanging position always triggers nystagmus 2 7-21.
Apogeotropic posterior canal BPPV (APC) is characterised by a paroxysmal nystagmus evoked through the Dix-Hallpike test, and sometimes in the straight headhanging position. The nystagmus has a vertical downbeating component and a torsional component, clockwise for the right canal, counter-clockwise for the left canal. Nystagmus is sometimes fatigable and paroxysm is often not intense; when the patient comes back to the sitting position, nystagmus seldom reverses its direction, and when it reverses, its intensity sometimes rises 4 5.
Differential diagnosis between AC and APC therefore assumes a relevant importance: a right AC, for example, is diagnosed through a vertical down-beating paroxysmal nystagmus and a possible counter-clockwise torsional component evoked in straight-head hanging and in Dix- Hallpike positions; however, this oculomotor pattern is similar to a left APC, where, in most cases, the torsional component is more evident than the vertical one. Careful evaluation of differences in intensity and direction of the nystagmus, triggering position or positions, and inversion of the nystagmus in returning to the sitting position in order to identify the affected canal and its side, and adopt the most appropriate therapeutic manoeuvre for each subtype, is fundamental.
The primary scope of the present research is to confirm, through the effects of therapeutic manoeuvres and the resulting gradation of diagnosis, if the oculomotor criteria proposed in the literature are efficient for diagnosis of both anterior and apogeotropic posterior canalolithiasis. The secondary aim is to verify the efficiency of the Yacovino manoeuvre (YM) in treating AC 16 (Fig. 3A), and the Quick Liberatory Rotation manoeuvre (QLR) in treating APC 22 (Fig. 3B).
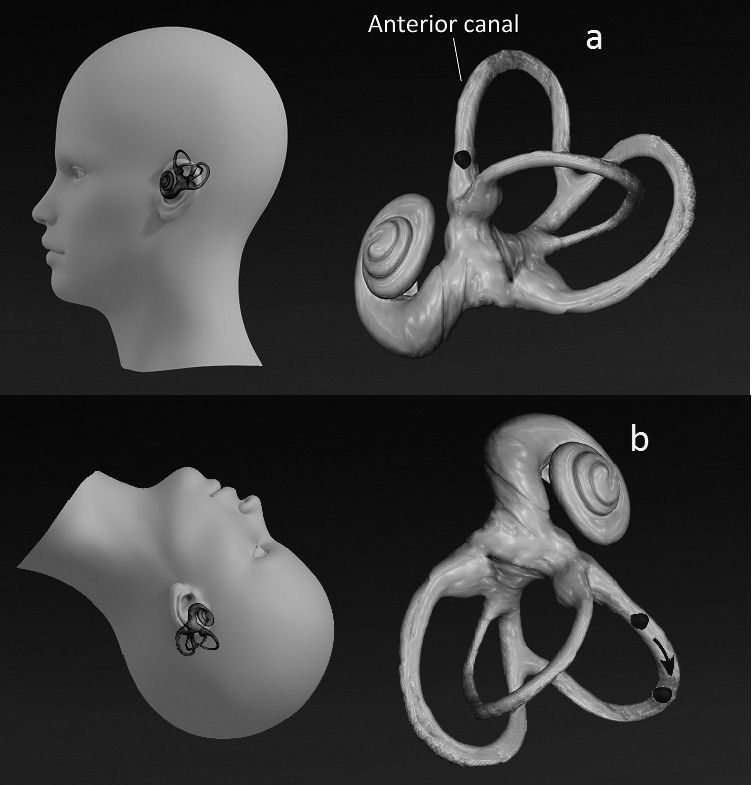
Fig. 3.
Yacovino repositioning manoeuvre for anterior canal BPPV (A): during the manoeuvre otoliths move toward the common crus and the utricle. Head position is the same both for left and right anterior canal BPPV. Quick Liberatory Rotation manoeuvre (B) from the starting position (a) to the final contralateral lying-down position (b) for posterior canal BPPV. The time of execution is about one sec.
Materials and methods
From September 2011 to December 2012, of 934 patients affected by BPPV, we identified 23 patients (2.5%) with presumed APC and 11 patients (1.2%) with presumed AC. There were 16 males and 18 females, with a mean age of 52.3 +/- 10.49 years; patients underwent otomicroscopy, pure tone audiometry and infrared videonystagmoscopy to evaluate spontaneous-positional nystagmus in darkness, in both a seated position – through Head Pitching Test 23 24, Head Shaking Test, Head Thrust Test, Hyperventilation Test, and Gaze Test – and in a supine position via the straight head-hanging positioning, Dix-Hallpike positioning test and supine head roll test (Pagnini-Mc- Clure test) 25-27.
We used the diagnostic oculomotor patterns of APC and AC as reported in the literature 2 4 5 7-21, evoked through the positioning tests (Dix-Hallpike test and straight head hanging positioning) and, according to their presence, we hypothesised a diagnosis of APC or AC. A vertical downbeating nystagmus indicated the involvement of a vertical canal, whereas the torsional component could also indicate the affected side: left AC or right APC for clockwise nystagmus; right AC or left APC for counterclockwise nystagmus. It is important to note that analysis of the nystagmus was performed through infrared videonystagmoscopy, and that different and more sensitive methods (i.e. scleral search coil) could lead to partially different observations.
After diagnosis, all patients signed an informed consent form for treatment.
AC patients were treated with YM, which can be performed regardless of the affected side. The patient is quickly moved from a 30° straight head hanging position to a supine position with a 30° forward inclination of the head for 30 sec, and finally to a sitting position with a 30° forward inclination of the head for 30 sec. APC patients were treated by QLR with a quick rotation of the head and of the body (less than 1 sec) from the Dix-Hallpike positioning on the affected side to a 45° nose-down position on the healthy side, remaining in the final lying-down position for 3 min; finally, they were brought to an upright sitting position.
The expected outcomes of these treatments were either a negative positioning test (one step therapy) or a positional paroxysmal nystagmus, torsional and up-beating, suggesting a canal conversion from AC or APC into TPC. TPC was further treated through QLR until a negative positioning test was observed (two step therapy). Patients were controlled two hours after the first manoeuvre and later every two days, until positioning tests were negative. Success was considered a negative positioning test while failure was the persistence of a positional paroxysmal nystagmus.
If therapeutic manoeuvres failed, the diagnostic work-up was completed by cerebral MRI, searching for central neurological diseases and/or inner ear CT scans to search for semicircular canal dehiscence.
Based on oculomotor criteria and therapeutic results, we elaborated a grading from "certain" to "possible" AC and APC, where therapeutic results confirmed the initial diagnostic hypothesis and the validity of oculomotor patterns reported in literature for APC and AC, depending on the strength of the evidence.
1. Anterior canal BPPV
1a: "certain" AC
Presence of a positional vertical down-beating paroxysmal nystagmus evoked through the straight headhanging positioning and sometimes through the Dix- Hallpike test.
In such positions, possible presence of a clockwise torsional component for the left AC or of a counterclockwise torsional component for the right AC.
Canal conversion in typical posterior canal BPPV (TPC) during or immediately after (no more than two days) the therapeutic manoeuvre, characterised by a vertical up-beating nystagmus, clockwise for the left canal and counter-clockwise for the right canal.
1b: "Probable" AC
As reported in 1a, but with a direct resolution of disease without canalar conversion in TPC.
1c: "Possible" AC
Persistence of symptoms after five cycles of therapeutic manoeuvres.
MRI does not show any neurological disease as a presumed cause of the nystagmus
or
patient lost to follow-up before the resolution of the disease.
2. Apogeotropic Posterior Canal BPPV
2a: "Certain" APC
Presence of a down-beating paroxysmal nystagmus, torsional clockwise for the right canal and counterclockwise for the left canal, evoked through the Dix- Hallpike test and sometimes through the straight headhanging positioning.
Possible presence of a vertical down-beating component in the same positioning tests.
Canalar conversion in TPC during or immediately after (no more than two days) the therapeutic manoeuvre.
2b: "probable" APC
As reported in 2a, but with a direct resolution of disease without canalar conversion in TPC.
2c: "possible" APC
Persistence of symptoms after five cycles of therapeutic manoeuvres.
MRI does not show any neurological disease as a possible cause of nystagmus
or
patient lost to follow-up before resolution of disease.
Statistical analysis was performed using Fisher's exact test to compare the efficacy of QLR in curing APC and TPC and the efficacy of YM in curing AC. These results depend on the accuracy of the initial diagnosis based on the presence of the above-reported diagnostic criteria; therefore, Fisher's exact test was also used to confirm if vertical nystagmus was actually prevalent in presumed AC and torsional nystagmus in presumed APC, basing our analysis on the results of the "certain" grade both of APC and AC, where evidence is stronger than in the "probable" and "possible" grades. A p value ≤ 0.05 was considered statistically significant.
Results
No patient showed significant otomicroscopic or audiometric data. Five cases (#7 and #16 in Table I and #1, #2, #7 in Table II) had already been evaluated for TPC from 9 to 42 months before, and had been treated through QLR. Patient #2 in Table I and patient #8 in Table II had been treated by QLR for a left TPC three and five days before diagnosis, respectively, of APC and AC, which were then considered secondary to treatment. One patient (#10 in Table I) was known to have suffered a recent traumatic brain injury. Three patients had already undergone cerebral MRI before our observation, without signs of central nervous system disease. Vertiginous symptoms had occurred between 1 and 30 days before our visit. No patient regularly used neurotropic drugs or had taken vestibular suppressant drugs for at least 5 days before our visit.
Table I.
Clinical data of apogeotropic posterior canal BPPV patients.
| Patient # | Sex | Age | Right dh nystagmus | Sitting Nystagmus | Left dh nystagmus | Sitting Nystagmus | S-HH-P nystagmus | Diagnosis | Therapeutic manoeuvre | Nr MANs | Outcome | Diagnostic grade |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 50 | CW +++ | CCW+ | CCW++ | CCW++ | CW ++++ | Left APC | QLR from left to right | 2 | Left TPC | Certain |
| 2 | M | 42 | - | - | CCW ++ DB+ |
- | - | Left APC | QLR from left to right | 1 | Left TPC | Certain |
| 3 | M | 48 | CW ++ | - | CCW++ | - | - | Right APC | QLR from right to left | 1 | Right TPC | Certain |
| 4 | M | 43 | CW +++ | - | CCW++ | - | - | Right APC | QLR from right to left | 1 | Right TPC | Certain |
| 5 | M | 60 | CCW++ | CW++ | CCW++ | CW ++ | CCW+ DB+ |
Left APC | QLR from left to right | 2 | Left TPC | Certain |
| 6 | M | 65 | CCW++ | CW + | CCW+ | CW +++ | CCW+ | Left APC | QLR from left to right | 3 | Left TPC | Certain |
| 7 | M | 54 | - | - | CCW++++ DB++ |
CW++++ | DB+++ | Left APC | QLR from left to right | 2 | Left TPC | Certain |
| 8 | M | 40 | CCW + | - | CCW++ | - | DB+ | Left APC | QLR from left to right | 2 | Left TPC | Certain |
| 9 | M | 43 | CW + | - | CW+ | - | - | Right APC | QLR from right to left | 1 | Right TPC | Certain |
| 10 | F | 70 | CW++ | - | CW++ | - | CW ++ | Right APC | QLR from right to left | 3 | Right TPC | Certain |
| 11 | F | 61 | CW ++ DB ++ |
- | CW ++ DB+ |
- | CW ++ DB+ |
Right APC | QLR from right to left | 1 | Right TPC | Certain |
| 12 | F | 62 | CW ++++ DB+++ |
- | CW +++ DB++ |
- | CW + DB ++ |
Right APC | QLR from right to left | 5 | Right TPC | Certain |
| 13 | M | 60 | CCW+++ DB + |
- | CCW++ DB+ |
- | CCW+++ DB+ |
Left APC | QLR from left to right | 2 | Left TPC | Certain |
| 14 | F | 64 | CW + DB+ |
CW+ | CW++ DB++ |
CW++ DB+ |
CW++ DB+ |
Right APC | QLR from right to left | 1 | Right TPC | Certain |
| 15 | M | 66 | CW ++ | - | CW ++ | - | - | Right APC | QLR from right to left | 2 | Direct resolution |
Probable |
| 16 | F | 30 | CW ++ DB++ |
- | CW + | - | CW + | Right APC | QLR from right to left | 1 | Direct resolution |
Probable |
| 17 | F | 51 | CCW ++ | CW+++ | CCW + | - | - | Left APC | QLR from left to right | 2 | Direct resolution |
Probable |
| 18 | F | 60 | CW + DB + |
CCW+ | CW + | - | - | Right APC | QLR from right to left | 2 | Direct resolution |
Probable |
| 19 | M | 59 | CCW ++ | - | CCW + | - | CW ++ DB+ |
Left APC | QLR from left to right | 1 | Direct resolution |
Pprobable |
| 20 | M | 52 | CCW+ | - | CCW++ | - | CCW+ | Left APC | QLR from left to right | 2 | Direct resolution |
Probable |
| 21 | F | 45 | CCW++ DB + |
- | CCW++ DB + |
CCW++ DB + |
CCW++ DB + |
Left APC | QLR from left to right | 3 | Direct resolution |
Probable |
| 22 | F | 55 | CCW+++ DB+ |
CCW+ | CCW+++ DB+ |
CCW+ | CCW+++ DB++ |
Left APC | QLR from left to right | 1 | Direct resolution |
Probable |
| 23 | F | 34 | - | - | CCW++ | CW +++ | CCW++ | Left APC | QLR from right to left | 2 | Lost to follow-up |
Possible |
Legend: DH: Dix-Hallpike positioning test; S-HH-P: Straight Head Hanging Positioning test; Nr Mans: Number of manoeuvres; F: Female; M: Male; CW: Clockwise; CCW: Counter-clockwise; DB: Down-beating; APC: Apogeotropic Posterior Canal BPPV; QLR: Quick Liberatory Rotation Manoeuvre; TPC: Typical Posterior Canal BPPV; Grading of Nystagmus: from + (the least) to +++++ (the greatest)
Table II.
Clinical data of anterior canal BPPV patients.
| Patient # | Sex | Age | Right DH nystagmus | Sitting nystagmus | Left dh nystagmus | Sitting Nystagmus | S-HH-P nystagmus | Diagnosis | Therapeutic manoeuvre | Nr MANs | Outcome | Diagnostic grade |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 56 | DB++ | DB+ CCW+ | DB +++ CCW++ | - | DB+++++ | Right AC | Yacovino | 1 | Right TPC | Certain |
| 2 | M | 60 | DB+++++ | DB++ | DB+++++ | DB+ | DB+++++ | AC | Yacovino | 3 | Right TPC | Certain |
| 3 | F | 46 | DB+++ | DB++ | DB+++ | DB+ + CW+ | DB+++ | (left?)AC | Yacovino | 3 | Left TPC | Certain |
| 4 | F | 47 | DB+++ | - | DB+++ | - | DB++ | AC | Yacovino | 2 | Right TPC | Certain |
| 5 | M | 63 | DB++++ | - | DB++++ | - | DB++++ | AC | Yacovino | 2 | Right TPC | Certain |
| 6 | F | 39 | DB+ | - | DB++ | - | DB++ | AC | Yacovino | 1 | Direct resolution |
Probable |
| 7 | F | 72 | DB+ | - | DB++ | - | DB+ | AC | Yacovino | 1 | Direct resolution |
Probable |
| 8 | F | 48 | DB+ CW+ |
DB+ CW+ |
DB++ | - | DB+++ | Left AC | Yacovino | 2 | Direct resolution |
Probable |
| 9 | F | 66 | DB++ CCW+ |
- | DB++ CCW+ |
- | DB++ CCW+ |
Right AC | Yacovino | 1 | Direct resolution |
Probable |
| 10 | F | 45 | DB+ CW + |
DB+ CW + |
DB++ | - | DB++ | Left AC | Yacovino | 2 | Lost to follow-up |
Possible |
| 11 | M | 49 | DB++ CW + |
DB+ CW + |
DB++ | - | DB+++ | Left AC | Yacovino | 1 | Lost to follow-up |
Possible |
Legend: DH: Dix-Hallpike positioning test; S-HH-P: Straight Head Hanging Positioning test; Nr Mans: Number of manoeuvres; F: Female; M: Male; CW: Clockwise; CCW: Counter-clockwise; DB: Down-beating; AC: Anterior Canal BPPV; TPC: Typical Posterior Canal BPPV; Grading of Nystagmus: from + (the least) to +++++ (the greatest)
The results of positioning tests and therapeutic manoeuvres are reported in Tables I and II.
Final diagnosis of APC and AC was made according to the above-mentioned criteria and grading system ("certain", "probable" and "possible").
Both AC and APC were characterised by paroxysmal nystagmus evoked in different positions and rarely inverting when returning to the sitting position. Paroxysmal nystagmus was usually more intense in frequency, amplitude and/or duration in AC than in APC, lasting in both forms from 1 to 4 min. In 3 patients with APC, the reverted nystagmus in returning to the sitting position was more intense than the nystagmus in Dix-Hallpike positioning. Only in 5 of the 11 patients with AC were we able to identify the affected side through a slight clockwise torsional component for the left canal, counter-clockwise for the right canal, regardless of the side of the head hanging positioning (Tables I and II). According to literature data, a torsional component of nystagmus was present in all 23 cases of presumed APC and in 5/11 cases of presumed AC; a down-beating component of nystagmus was present in 13/23 cases of presumed APC and in all 11 cases of presumed AC.
In APC, all patients presented nystagmus in Dix-Hallpike positioning, 4/23 only on the supposed affected side and 19/23 on both sides. In the head-hanging positioning, nystagmus was present in 16/23 patients; in 14 cases it presented a torsional component, in 8 of these cases the torsional component was associated with a down-beating component and in 2 cases only the down-beating component was present.
In AC, all patients presented nystagmus on both sides in either positioning, with different intensity. The straight head hanging position usually evoked the strongest nystagmus.
Therapeutic manoeuvre caused a canalar conversion to TPC in 19 cases (14 from the APC group and 5 from the AC group), and cured 12 patients in one step (8 in the APC group and 4 in the AC group).
Analysing the presence of a prevalent torsional nystagmus vs. a prevalent down beating vertical nystagmus in the "certain" APC group (14 patients) and in the "certain" AC group (5 patients), it emerged that torsional nystagmus was more frequent in the presumed APC group, whereas vertical down-beating nystagmus was more frequent in the presumed AC group (p = 0.03 at Fisher's exact test).
All patients with canal conversion in TPC were successfully treated with QLR, performed from 1 to 3 times (Tables III and IV). A significant difference at Fisher's exact test (p < 0.0001) was found in QLR efficacy in curing in one step APC (8/22 cases) vs. TPC (19/19 cases).
Table III.
Clinical data after the conversion from apogeotropic posterior canal to typical posterior canal BPPV.
| Patient # | Sex | Age' | Right DH nystagmus | Sitting nystagmus | Left dh nystagmus | Sitting Nystagmus | S-HH-P nystagmus | Diagnosis | Therapeutic manoeuvre | Nr MANs | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 50 | - | - | CW+++ | CCW+ | Left TPC | QLR from left to right | 2 | Resolution | |
| 2 | M | 42 | - | - | CW+++ | CCW+ | CW+ | Left TPC | QLR from left to right | 1 | Resolution |
| 3 | M | 48 | CCW++ | CW+ | - | - | - | Right TPC | QLR from right to left | 1 | Resolution |
| 4 | M | 43 | CCW+++ | CW+ | - | - | - | Right TPC | QLR from right to left | 1 | Resolution |
| 5 | M | 60 | CW++++ | CCW+ | - | Left TPC | QLR from left to right | 2 | Resolution | ||
| 6 | M | 65 | - | - | CW+++ | CCW+ | - | Left TPC | QLR from left to right | 3 | Resolution |
| 7 | M | 54 | - | - | CW+++ | CCW+ | - | Left TPC | QLR from left to right | 2 | Resolution |
| 8 | M | 40 | - | - | CW+++ | CCW+ | - | Left TPC | QLR from left to right | 1 | Resolution |
| 9 | M | 43 | CCW+++ | CW+ | - | - | - | Right TPC | QLR from right to left | 1 | Resolution |
| 10 | F | 70 | CCW+++ | CW+ | - | - | - | Right TPC | QLR from right to left | 2 | Resolution |
| 11 | F | 61 | CCW+++ | CW+ | - | - | - | Right TPC | QLR from right to left | 1 | Resolution |
| 12 | F | 62 | CCW++++ | CW+ | - | - | CCW++ | Right TPC | QLR from right to left | 2 | Resolution |
| 13 | M | 60 | - | - | CW+++ | CCW+ | - | Left TPC | QLR from left to right | 3 | Resolution |
| 14 | F | 64 | CCW++++ | CW ++ | - | - | CCW+ | Right TPC | QLR from right to left | 1 | Resolution |
Legend: DH: Dix-Hallpike positioning test; S-HH-P: Straight Head Hanging Positioning test; Nr Mans: Number of manoeuvres; F: Female; M: Males; CW: Clockwise; CCW: Counter-clockwise; DB: Down-beating; APC: Apogeotropic Posterior Canal BPPV; QLR: Quick Liberatory Rotation Manoeuvre; TPC: Typical Posterior Canal BPPV; Grading of Nystagmus: from + (the least) to +++++ (the greatest)
Table IV.
Clinical data after the conversion from anterior canal to typical posterior canal BPPV.
| Patient # | Sex | Age | Right DH nystagmus | Sitting nystagmus | Left dh nystagmus | Sitting Nystagmus | S-HH-P nystagmus | Diagnosis | Therapeutic manoeuvre | Nr MANs | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 56 | CCW++ | CW+ | - | - | - | right TPC | QLR from right to left | 5 | Resolution |
| 2 | M | 60 | CCW+++++ | CW++ | - | - | - | right TPC | QLR from right to left | 1 | Resolution |
| 3 | F | 46 | - | - | CW+++ | CCW+ | CW+ | left TPC | QLR from left to right | 2 | Resolution |
| 4 | F | 47 | CCW++ | CW+ | - | - | - | right TPC | QLR from right to left | 1 | Resolution |
| 5 | M | 63 | CCW+++++ | CW++ | - | - | - | right TPC | QLR from right to left | 1 | Resolution |
Legend: DH: Dix-Hallpike positioning test; S-HH-P: Straight Head Hanging Positioning test; Nr Mans: Number of manoeuvres; F: Female; M: Males; CW: Clockwise; CCW: Counter-clockwise; QLR: Quick Liberatory Rotation Manoeuvre; TPC: Typical Posterior Canal BPPV; Grading of Nystagmus: from + (the least) to +++++ (the greatest)
Neuroimaging was never performed because 31 patients were disease-free after therapeutic manoeuvre and 3 patients, one with APC and two with AC, were lost to follow-up.
Discussion
Anterior canal BBPV is considered rare for anatomic considerations because the anterior canal is higher than both the posterior and lateral ones; furthermore, the fact that the posterior arm of the anterior canal descends directly into the common crus and vestibule should cause a continuous self clearing of otoliths from the canal 28. To explain AC, changes in the diameter of the common crus, stenosis of membranous duct and changes in the position of the canal have been proposed 10 17 28 29. As reported by Giannoni 7 and Korres 17, AC can induce ambiguous nystagmus, depending on the position of otoconial debris; the most common clinical picture is characterised by vertical down-beating paroxysmal nystagmus in the Dix-Hallpike test, as well as in the straight head hanging positioning, with clockwise (or counter- clockwise) torsional components, due to a left anterior (or right anterior) canal involvement, without inversion of the nystagmus when coming back to the sitting position.
AC is believed to be more frequent in post-traumatic BPPV 13 20. A down-beating vertical nystagmus with a clockwise (or counter-clockwise) torsional component for left (or right) canal is coherent with Flourens law, because it respects the plane of the interested canal, whereas according to Zapala 15, an anterior bilateral canalolithiasis can be supposed for the presence of a pure vertical down-beating nystagmus. Nevertheless, a unilateral form of AC can also cause a vertical down-beating nystagmus, due to the orientation of the anterior canal which is closer to the sagittal plane (usually by a 41° angle) than the posterior canal (usually by a 56°angle); these considerations are enough to justify the frequent occurrence of a purely vertical down-beating nystagmus on both sides even in unilateral forms 28. The prevalence of down-beating components can be caused by the fact that vestibulo-oculomotor torsional gain reflex is smaller than horizontal and vertical components gain 30.
Down-beating nystagmus syndrome can be associated witb cerebellar diseases, and in such cases it is mandatory to exclude these from peripheral down beating nystagmus syndrome. Bertholon 28 reported 50 consecutive cases of positional down-beating nystagmus, 12 of which presented without central neurological symptoms or signs and a clinical picture of an anterior canal BPPV. Cambi 31 recently showed that the natural course of most cases of down-beating nystagmus syndrome is towards a spontaneous resolution, and that it is sometimes associated with BPPV, so that the frequency of peripheral down-beating nystagmus syndrome appears to be more frequent than previously suggested: our data confirmed this possibility. Our diagnostic algorithm gives substantial importance to this aspect of the problem, but we decided to search for central neurological disease as a possible cause of positional vertical down-beating nystagmus not associated with other neurological signs and symptoms, only in the case of failure of therapeutic manoeuvres: in this situation, we included cerebral MRI in our diagnostic workup. However, the frequent conversion of a down-beating nystagmus syndrome in a posterior canal BPPV or its direct resolution confirmed that, in these cases, as reported by Cambi 31, a peripheral cause, i.e. anterior canal BPPV, is very probable.
Recently, Vannucchi described a new form of BPPV which he called "Apogeotropic Posterior Canal BPPV" that is characterised by a torsional down-beating nystagmus clockwise for the right posterior canal and counterclockwise for the left posterior canal. He explained the oculomotor pattern of APC is caused by ampullopetal stimulation of the posterior semicircular canal due to free-floating otoconial debris in the non-ampullary arm, perhaps because putative alterations of posterior canal morphology can cause otolith entrapment in that zone 4 5. The less severe paroxysm could be due to the reduced movement of the otoconial mass and to the weaker inhibitory ampullopetal endolymphatic flow (III Ewald's law) caused by otoliths on diagnostic positioning tests 32.
Differential diagnosis between APC and AC is possible due to the prevalence of the torsional component compared with the vertical one in APC, whereas differential diagnosis between APC and TPC is possible because of the inverted characteristics of the nystagmus, which in APC is downbeating, clockwise in the right Dix-Hallpike position and counter-clockwise in the left Dix-Hallpike position.
The above-mentioned criteria let us identify two populations in our cohort: the first composed of 23 patients affected by presumed APC (2.5%) and the second of 11 patients affected by presumed AC (1.2%) (Tabs. I and II). Therefore, AC appears to be rarer than reported in the literature, because we have diagnosed some cases as APC which otherwise may have been classified as AC. All patients we included in the APC group showed the oculomotor pattern described by Vannucchi 4 5. In three APC patients, nystagmus reversed its direction with higher intensity in returning to the sitting position, probably because of the stronger excitatory ampullophugal endolymphatic flow (III Ewald's law).
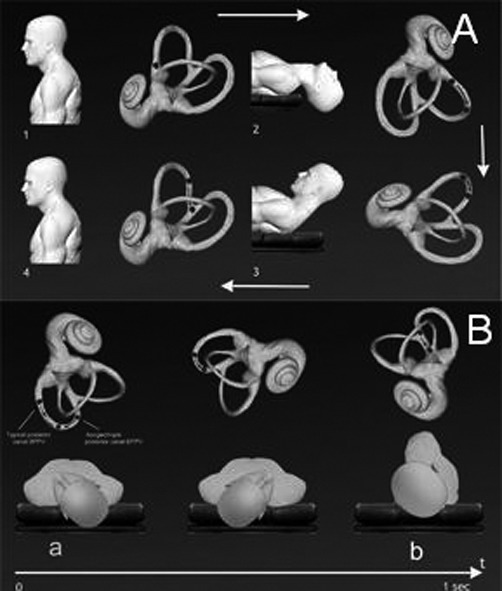
APC was treated through QLR, a manoeuvre usually used in TPC, because in the Dix-Hallpike test on the affected side, the otoconial mass in the posterior canal always moves towards the most sloping part of the canal, regardless of its initial positioning, in both the ampullary and non-ampullary arm (Fig. 4). The canalar conversion from APC to TPC occurred in 14 cases (ranked "certain" in the diagnostic grade), and the direct resolution of APC occurred in 8 cases ("probable" diagnostic grade). One patient was lost to follow up ("possible" diagnostic grade). In conclusion, 22 of 23 patients affected by APC were successfully treated by QLR in a one-step or a two-step therapy, and one was lost to follow up. AC (Table 4) was treated with YM which caused canalar conversion in TPC in 5 patients ("certain" diagnostic grade) and was then cured through QLR (two-step therapy), whereas the direct resolution (one-step therapy) was obtained in 4 patients ("probable" diagnostic grade). Two patients were lost to follow-up ("possible" diagnostic grade) (Table II). The affected side was confirmed in only one patient with "certain" AC where the conversion into an ipsilateral TPC confirmed our diagnostic hypothesis.
Fig. 4.
Left typical (a) and apogeotropic (b) posterior canal BPPV: the final position of otoliths in the Dix-Hallpike positioning test is the same, in the sloping part of the canal (c).
QLR appeared more effective (p < 0.0001) in curing TPC (19/19 cases, 14 from the APC group, 5 from the AC group) than in curing APC, where a two-step therapy was frequently required (Table III). This result could be explained if an obstacle (i.e. a stenosis) was blocking the exit of otoliths from the non-ampullary arm toward the utricle in case of APC, a situation which could cause, at a later stage, a shift of otoliths toward the ampullary arm of the canal, the most frequent site of entrapment. The efficacy in two steps could be explained by hypothesising a fragmentation of otholits during the first manoeuvre and their exit through the later manoeuvres.
On a speculative basis, this finding and the analogous finding of the conversion of AC into TPC through YM could further confirm that otoliths floating in semicircular canals could be the pathophysiological mechanism in BPPV even in rare forms of vertical canal BPPV.
Conclusions
Our data, based on the efficacy of therapeutic manoeuvres in the form of canalar conversion or direct resolution of the disease, confirmed that oculomotor patterns reported in the literature allow correct identification of both AC and APC; analysis of positioning-evoked nystagmus through infrared videonystagmoscopy permits differential diagnosis between AC, characterised by a prevalent vertical down-beating nystagmus and APC, in which the torsional component is prevalent and reverted compared to TPC. The diagnostic grading we propose could be useful in the management of these forms of BPPV.
The clinical evolution of our cases showed that the peripheral type of positional down-beating nystagmus is not uncommon, and that it is often the sign of an anterior canal BPPV, characterised by a benign evolution, always keeping in mind that the presence of a positional downbeat nystagmus needs careful follow-up, particularly if nystagmus persists or reappears: in these cases, cerebral imaging through MRI is mandatory.
Correct differential diagnosis is of significant importance to identify the affected ear and to adopt the most appropriate therapeutic manoeuvre to obtain a good therapeutic outcome in these rare and atypical forms of BPPV. For APC, a specific liberatory manoeuvre can be considered, albeit in our experience based on a limited number of patients, QLR gives good results.
Acknowledgments
The authors acknowledge Dr. Genoveffa Errico for the original figures of the paper.
References
- 1.Leigh RJ, Zee DS. The neurology of eye movements. 4th ed. New York: Oxford University Press Inc; 2006. pp. 559–597. [Google Scholar]
- 2.Katsarkas A. Nystagmus of paroxysmal positional vertigo: some new insights. Ann Otol Rhinol Laryngol. 1987;96:305–308. doi: 10.1177/000348948709600313. [DOI] [PubMed] [Google Scholar]
- 3.Oas JG. Benign Paroxysmal positional vertigo. A clinician's perspective. Annals New York Academy of Science. 2001;942:201–209. doi: 10.1111/j.1749-6632.2001.tb03746.x. [DOI] [PubMed] [Google Scholar]
- 4.Vannucchi P, Giannoni B, Giustino F, et al. Atti XXXIII Congresso Nazionale della Società Italiana di Audiologia e Foniatria "Audiologia, Foniatria e Scienze correlate". 2011. La variante apogeotropa della VPP del CSP; pp. 69–70. Bari. [Google Scholar]
- 5.Vannucchi P, Pecci R, Giannoni B. Posterior semicircular canal benign paroxysmal positional vertigo presenting with torsional downbeating nystagmus: an apogeotropic variant. Int J Otolaryngol. 2012;2012:413603–413603. doi: 10.1155/2012/413603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agus G. Atypical "reversed" paroxysmal positioning nystagmus in benign paroxysmal positional vertigo. Acta Otolaryngol. 1995;520(Suppl.):143–147. doi: 10.3109/00016489509125213. [DOI] [PubMed] [Google Scholar]
- 7.Giannoni B. Vertical canal lithiasis. In: Guidetti VG, Pagnini P, editors. Labyrintholithiasis-Related Paroxysmal Positional. Excerpta Medica: 2002. pp. 157–170. [Google Scholar]
- 8.Korres S, Balatsouras DG, Kaberos A, et al. Occurrence of semicircular canal involvement in benign paroxysmal positional vertigo. Otol Neurotol. 2002;23:926–932. doi: 10.1097/00129492-200211000-00019. [DOI] [PubMed] [Google Scholar]
- 9.Califano L, Montanaro SC, Capparuccia PG, et al. Case report: associazione ipsilaterale di canalolitiasi anteriore e posteriore. Acta Otorhinolaryngol Ital. 2002;22:376–379. [PubMed] [Google Scholar]
- 10.Crevits L. Treatment of anterior canal benign paroxysmal positionale vertigo by a prolonged forced position procedure. J Neurol Neurosurg Psychiatry. 200;75:779–781. doi: 10.1136/jnnp.2003.025478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim YK, Shin JE, Chung JW. The effect of canalith repositioning for anterior semicircular canal canalithiasis. ORL J Otorhinolaryngol Relat Spec. 2005;67:56–60. doi: 10.1159/000084336. [DOI] [PubMed] [Google Scholar]
- 12.Lopez-Escamez JA, Molina MI, Gamiz MJ. Anterior semicircular canal benign paroxysmal positional vertigo and positional downbeating nystagmus. Am J Otolaryngol. 2006;27:173–178. doi: 10.1016/j.amjoto.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 13.Jackson LE, Morgan B, Fletcher JC, Jr, et al. Anterior canal benign paroxysmal positional vertigo: an underappreciated entity. Otol Neurotol. 2007;28:218–222. doi: 10.1097/01.mao.0000247825.90774.6b. [DOI] [PubMed] [Google Scholar]
- 14.Lorin P. Treatment of anterior semi-circular canalithiasis by a sedimentation procedure in a vertical rotatory chair. Ann Otolaryngol Chir Cervicofac. 2007;124:184–188. doi: 10.1016/j.aorl.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 15.Zapala DA. Down-Beating Nystagmus in anterior canal benign paroxysmal positional vertigo. J Am Acad Audiol. 2008;19:257–266. doi: 10.3766/jaaa.19.3.10. [DOI] [PubMed] [Google Scholar]
- 16.Yacovino DA, Hain T, Gualtieri F. New therapeutic maneuver for anterior canal benign paroxysmal positional vertigo. J Neurol. 2009;256:1851–1855. doi: 10.1007/s00415-009-5208-1. [DOI] [PubMed] [Google Scholar]
- 17.Korres S, Riga M, Sandris V, et al. Canalolithiasis of the anterior semicircular canal (ASC): Treatment options based on the possible underlying pathogenetic mechanisms. Int J Audiol. 2010;49:606–612. doi: 10.3109/14992021003753490. [DOI] [PubMed] [Google Scholar]
- 18.Casani AP, Cerchiai N, Dallan I, et al. Anterior canal lithiasis: diagnosis and treatment. Otolaryngol Head Neck Surg. 2011;144:412–418. doi: 10.1177/0194599810393879. [DOI] [PubMed] [Google Scholar]
- 19.Heidenreich KD, Kerber KA, Carender WJ, et al. Persistent positional nystagmus: a case of superior semicircular canal benign paroxysmal positional vertigo? Laryngoscope. 2011;121:1818–1820. doi: 10.1002/lary.21848. [DOI] [PubMed] [Google Scholar]
- 20.Dlugaiczyk J, Siebert S, Hecker DJ, et al. Involvement of the anterior semicircular canal in posttraumatic benign paroxysmal positional vertigo. Otol Neurotol. 2011;32:1825–1890. doi: 10.1097/MAO.0b013e31822e94d9. [DOI] [PubMed] [Google Scholar]
- 21.Adamec I, Habek M. Anterior semicircular canal BPPV with positional downbeat nystagmus without latency, habituation and adaption. Neurol Sci. 2012;33:955–956. doi: 10.1007/s10072-011-0843-6. [DOI] [PubMed] [Google Scholar]
- 22.Califano L, Capparuccia PG, Maria D, et al. Treatment of benign paroxysmal positional vertigo of posterior semicircular canal by "Quick Liberatory Rotation Manoeuvre". Acta Otorhinolaryngol Ital. 2003;23:161–167. [PubMed] [Google Scholar]
- 23.Choung Y-H, Shin YR, Kahng H, et al. "Bow and Lean test" to determine the affected ear of horizontal canal benign paroxysmal positional vertigo. Laryngoscope. 2006;116:1776–1781. doi: 10.1097/01.mlg.0000231291.44818.be. [DOI] [PubMed] [Google Scholar]
- 24.Asprella-Libonati G. Pseudo-spontaneous nystagmus: a new sign to diagnose the affected side in lateral semicircular canal benign paroxysmal positional vertigo. Acta Otorhinolaryngol Ital. 2008;28:73–78. [PMC free article] [PubMed] [Google Scholar]
- 25.Cipparrone L, Corridi G, Pagnini P. V Giornata Italiana di Nistagmografia Clinica. Milano: Ed. Boots-Formenti; 1985. Cupulolitiasi; pp. 36–53. [Google Scholar]
- 26.McClure JA. Horizontal canal BPV. J Otolaryngol. 1985;14:30–35. [PubMed] [Google Scholar]
- 27.Fife TD, Iverson DJ, Lempert TJ, et al. Practice parameter: therapies for benign paroxysmal positional vertigo (an evidence- based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2008;70:2067–2074. doi: 10.1212/01.wnl.0000313378.77444.ac. [DOI] [PubMed] [Google Scholar]
- 28.Bertholon P, Bronstein AM, Davies RA, et al. Positional down beating nystagmus in 50 patients: cerebellar disorders and possible anterior semicircular canalolithiasis. J Neurol Neurosurg Psychiatry. 2002;72:366–372. doi: 10.1136/jnnp.72.3.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schratzenstaller B, Wagner-Manslau C, Strasser G, et al. Canalolithiasis of the superior semicircular canal: An anomaly in benign paroxysmal vertigo. Acta Otolaryngol. 2005;125:1055–1062. doi: 10.1080/00016480510037023. [DOI] [PubMed] [Google Scholar]
- 30.Aw ST, Todd MJ, Aw GE, et al. Benign positional nystagmus: a study of its three-dimensional spatio-temporal characteristics. Neurology. 2005;64:1897–1905. doi: 10.1212/01.WNL.0000163545.57134.3D. [DOI] [PubMed] [Google Scholar]
- 31.Cambi J, Astore S, Mandalà M, et al. Natural course of positional down-beating nystagmus of peripheral origin. J Neurol. 2013;260:1489–1496. doi: 10.1007/s00415-012-6815-9. [DOI] [PubMed] [Google Scholar]
- 32.Ichijo H, et al. Asymmetry of positioning nystagmus in posterior canalolithiasis. Acta Otolaryngol. 2013;133:159–164. doi: 10.3109/00016489.2012.728293. [DOI] [PubMed] [Google Scholar]