Abstract
Objectives. We used race-corrected data and comprehensive diagnostic codes to better compare HIV and tuberculosis (TB) mortality from 1999 to 2009 between American Indian/Alaska Natives (AI/ANs) and Whites.
Methods. National Vital Statistics Surveillance System mortality data were adjusted for AI/AN racial misclassification through linkage with Indian Health Service registration records. We compared average annual 1990 to 2009 HIV and TB death rates (per 100 000 people) for AI/AN persons with those for Whites; Hispanics were excluded.
Results. Although death rates from HIV in AI/AN persons were significantly lower than those in Whites from 1990 to 1998 (4.2 vs 7.0), they were significantly higher than those in Whites from 1999 to 2009 (3.6 vs 2.0). Death rates from TB in AI/AN persons were significantly higher than those in Whites, with a significant disparity during both 1990 to 1998 (3.3 vs 0.3) and 1999 to 2009 (1.5 vs 0.1).
Conclusions. The decrease in death rates from HIV and TB was greater among Whites, and death rates remained significantly higher among AI/AN individuals. Public health interventions need to be prioritized to reduce the TB and HIV burden and mortality in AI/AN populations.
HIV/AIDS and tuberculosis (TB) are among the top 10 causes of death worldwide and among the top 10 infectious disease causes of death for American Indian/Alaska Natives (AI/ANs).1,2 Fewer deaths from HIV and TB is an important objective of HIV and TB control programs; key international targets include reducing deaths from HIV infection by 10% and halving TB deaths by 2015 compared with 1990 levels.3,4 Monitoring trends in deaths resulting from HIV and TB is important for informing and prioritizing programmatic and research efforts and planning interventions, as well as assessing progress in reducing the burden of premature and preventable deaths.
Since 1981, an estimated 1.7 million people have been infected with HIV in the United States, including more than 600 000 who have died.5,6 Although absolute numbers of HIV infection remain small among AI/AN communities, AI/AN populations continue to feel the impact of the HIV epidemic. Surveillance data from the Centers for Disease Control and Prevention (CDC) have indicated that an estimated 3194 non-Hispanic AI/AN persons were living with HIV at the end of 2010, a rate of 141 per 100 000.5 Although the prevalence of HIV infection among non-Hispanic AI/AN persons is lower than among most other racial and ethnic groups (with the exception of non-Hispanic Whites and Asians), non-Hispanic AI/AN individuals have the shortest survival time from AIDS diagnosis to death.5,7
In 2012, a total of 9945 new TB cases were reported in the United States, an incidence of 3.2 cases per 100 000 population.8 Deaths resulting from TB decreased from 1810 (0.7/100 000) in 1990 to 569 (0.2/100 000) in 2009, the most recent year for which data are available.8 Racial and ethnic minorities, including AI/AN populations, continue to be disproportionately affected by TB in the United States. In 2012, the incidences of TB among AI/ANs and non-Hispanic Whites were 6.3 and 0.8 per 100 000 population, respectively, a decrease from 14 and 3.6 per 100 000, respectively, in 1993.8 Although progress has been made over the past decades in reducing the morbidity and mortality of TB in AI/AN persons, during 2011 and 2012, non-Hispanic AI/AN persons were the only racial/ethnic group that experienced an increase in case rate.7 Furthermore, previous studies have shown that AI/AN individuals are more than twice as likely as other racial/ethnic groups to die during TB treatment,9 highlighting the need for continued and improved TB control efforts in this population.
Reducing HIV-related death in communities at high risk for HIV infection10 and reducing the burden of TB in specific racial/ethnic populations11 are priorities of the US government. Although surveillance data are available to monitor morbidity, mortality estimates among AI/AN populations have been limited, mainly as a result of racial misclassification.12,13 We conducted this study to better document the burden of HIV and TB mortality among AI/AN persons from 1990 to 2009 by using national mortality data linked with Indian Health Service (IHS) patient registration data to improve racial classification of AI/AN individuals.
METHODS
IHS patient registry data were linked to the National Death Index to identify AI/AN decedents misclassified as non-Native. A flag identifying these misclassified decedents was incorporated into the National Vital Statistics System public use mortality data files,14 which include underlying causes of death, state and county of residence, age, sex, race, and ethnicity. The time period for the study was split into 2 subperiods, 1990 to 1998 and 1999 to 2009, on the basis of the transition to International Classification of Diseases, 10th Revision (ICD–10),15 coding for cause of death in 1999. For this study, using the underlying cause of death, we defined a death resulting from HIV as any of the International Classification of Diseases, Ninth Revision (ICD–9),16 codes 042–044 and ICD–10 codes B20–B24 and a death resulting from TB as ICD–9 codes 010–018 and ICD–10 codes A16–A19.
We conducted analyses for Contract Health Service Delivery Area (CHSDA) counties; CHSDA counties, in general, contain federally recognized tribal lands or are adjacent to tribal lands.14 Linkage studies have indicated less misclassification of AI/AN race in CHSDA counties.17,18 The CHSDA counties also have higher proportions of AI/AN persons in relation to total population than do non-CHSDA counties, with 64% of the US AI/AN population residing in the 637 counties designated as CHSDA (these counties represent 20% of the 3141 counties in the United States). Although less geographically representative, analyses restricted to CHSDA counties are presented for death rates in this report for the purpose of offering improved accuracy in interpreting mortality statistics for AI/AN populations. Detailed methods are described elsewhere in this supplement.19
We analyzed death rates by sex, age group, and IHS region (Alaska, Pacific Coast, Northern Plains, Southern Plains, Southwest, and East; Table 1).14,18 Similar regional analyses have been used for other health-related publications focusing on AI/AN populations.12,18,21,22
TABLE 1—
Average Annual HIV Death Rates and Rate Ratios by Age, Sex, and Indian Health Service Region for American Indian/Alaska Native and White People: Contract Health Service Delivery Area Counties, United States, 1990–1998 and 1999–2009
| 1990–1998 |
1999–2009 |
|||||
| Variable | AI/AN Death Rate (per 100 000 Population) | White Death Rate (per 100 000 Population) | AI/AN:White RR (95% CI) | AI/AN Death Rate (per 100 000 Population) | White Death Rate (per 100 000 Population) | AI/AN:White RR (95% CI) |
| Total | 4.2 | 7.0 | 0.60* (0.54, 0.66) | 3.6 | 2.0 | 1.82* (1.67, 1.99) |
| Age group, y | ||||||
| 0–24 | 0.3 | 0.3 | 0.81 (0.41, 1.42) | 0.1 | 0.1 | 1.46 (0.52, 3.32) |
| 25–44 | 10.4 | 16.4 | 0.63* (0.56, 0.71) | 7.2 | 3.6 | 2.01* (1.79, 2.26) |
| 45–64 | 4.4 | 8.6 | 0.51* (0.39, 0.65) | 5.7 | 3.6 | 1.58* (1.36, 1.82) |
| 65–84 | 0.5 | 1.1 | 0.46 (0.10, 1.46) | 1.3 | 0,7 | 1.84 (0.99, 3.16) |
| ≥ 85 | … | … | NA | … | 0.2 | NA |
| Sex | ||||||
| Male | 7.2 | 13.1 | 0.55* (0.49, 0.62) | 5.6 | 3.4 | 1.67* (1.50, 1.85) |
| Female | 1.4 | 1.0 | 1.40* (1.07, 1.80) | 1.7 | 0.6 | 2.92* (2.42, 3.50) |
| IHS region | ||||||
| Alaska | 4.2 | 2.3 | 1.84* (1.19, 2.82) | 4.3 | 0.7 | 6.01* (3.79, 9.49) |
| Male | 6.7 | 3.9 | 1.72* (1.04, 2.80) | 4.9 | 1.2 | 4.11* (2.32, 7.18) |
| Female | 1.8 | 0.5 | 3.77* (1.12, 14.46) | 3.8 | 0.2 | 23.75* (7.35, 105.79) |
| East | 4.0 | 7.9 | 0.50* (0.34, 0.72) | 3.5 | 2.3 | 1.49* (1.07, 2.04) |
| Male | 6.2 | 14.4 | 0.43* (0.27, 0.69) | 6.6 | 3.7 | 1.76* (1.18, 2.56) |
| Female | 1.5 | 1.6 | 0.95 (0.34, 2.20) | 2.2 | 1.0 | 2.26* (1.16, 4.02) |
| Northern Plains | 3.4 | 2.3 | 1.47* (1.10, 1.94) | 2.1 | 0.7 | 2.89* (2.15, 3.85) |
| Male | 5.4 | 4.2 | 1.28 (0.92, 1.78) | 3.2 | 1.3 | 2.56* (1.79, 3.64) |
| Female | 1.5 | 0.4 | 4.18* (2.13, 7.70) | 1.1 | 0.2 | 5.81* (3.04, 10.47) |
| Pacific Coast | 5.8 | 9.0 | 0.64* (0.54, 0.75) | 3.5 | 2.2 | 1.58* (1.33, 1.87) |
| Male | 12.0 | 17.3 | 0.69* (0.57, 0.84) | 7.3 | 3.9 | 1.85* (1.50, 2.27) |
| Female | 1.7 | 0.9 | 1.88* (1.10, 3.08) | 2.3 | 0.5 | 5.12* (3.49, 7.35) |
| Southern Plains | 5.3 | 3.2 | 1.64* (1.31, 2.05) | 3.2 | 2.2 | 1.47* (1.18, 1.81) |
| Male | 5.7 | 3.8 | 1.51* (1.18, 1.91) | 5.7 | 3.8 | 1.51* (1.18, 1.91) |
| Female | 1.0 | 0.7 | 1.43 (0.28, 4.82) | 1.2 | 0.6 | 1.94* (1.14, 3.17) |
| Southwest | 2.8 | 7.2 | 0.39* (0.31, 0.48) | 3.1 | 2.2 | 1.42* (1.20, 1.68) |
| Male | 4.8 | 13.5 | 0.35* (0.28, 0.45) | 5.7 | 3.8 | 1.48* (1.22, 1.79) |
| Female | 1.2 | 0.9 | 1.32 (0.77, 2.13) | 1.4 | 0.5 | 2.96* (1.94, 4.39) |
Note. AI/AN = American Indian/Alaska Native; CHSDA = Contract Health Service Delivery Area; CI = confidence interval; IHS = Indian Health Service; NA = not applicable; RR = rate ratio. The sample size was n = 1096. Dashes indicate that counts < 10 were suppressed; if no cases were reported, then rates and RRs could not be calculated. Cases aged 0–24 y are included in overall totals, but rows have been suppressed as a result of few cases. Analyses are limited to people of non-Hispanic origin. AI/AN race is reported from death certificates or through linkage with the IHS patient registration database. Rates are per 100 000 people and were age adjusted to the 2000 US standard population (11 age groups; Census P25-113020). Rate ratios were calculated in SEER*Stat before rounding of rates and may not equal RRs calculated from rates presented in table. IHS regions are defined as follows: Alaskaa; Northern Plains (IL, IN,a IA,a MI,a MN,a MT,a NE,a ND,a SD,a WI,a WYa); Southern Plains (OK,a KS,a TXa); Southwest (AZ,a CO,a NV,a NM,a UTa); Pacific Coast (CA,a ID,a OR,a WA,a HI); East (AL,a AR, CT,a DE, FL,a GA, KY, LA,a ME,a MD, MA,a MS,a MO, NH, NJ, NY,a NC,a OH, PA,a RI,a SC,a TN, VT, VA, WV, DC). Percentage regional coverage of AI/AN persons in CHSDA counties to AI/AN persons in all counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; East = 18.2%; total US = 64.2%.
Source. AI/AN Mortality Database (1990–2009); the following states and years of data were excluded because Hispanic origin was not collected on the death certificate: LA, 1990; NH, 1990–1992; OK, 1990–1996.
Identifies states with more than 1 county designated as CHSDA.
*P < .05.
Average annual age-specific and age-adjusted death rates for 1990 to 2009 are expressed per 100 000 of the corresponding population. Bridged single-race population estimates developed by the US Census Bureau and the CDC’s National Center for HealthStatistics were used as population denominators in the calculation of death rates.23,24 During the development of the analytic file, it was discovered that the updated bridged intercensal population estimates significantly overestimated AI/AN persons of Hispanic origin, as reported elsewhere in this supplement.25 Therefore, to avoid underestimating mortality in AI/AN populations, analyses are limited to non-Hispanic AI/AN persons; non-Hispanic Whites were chosen as the most homogeneous referent group. Henceforth, the term ‘‘non-Hispanic’’ is omitted when discussing both groups.
Average annual age-adjusted death rates directly adjusted to the 2000 US standard population, including those for age groups, were calculated using SEER*Stat software (National Cancer Institute, Rockville, MD).26 We calculated standardized rate ratios with 95% confidence intervals (CIs) to compare AI/AN death rates with White death rates.27 Further description of the population data and analysis is provided elsewhere in this supplement.19 Statistical significance was considered at P < .05.
RESULTS
We present results by disease and time frame, as well as trends and HIV–TB co-infection.
HIV Mortality
1990–1998.
From 1990 to 1998, overall HIV mortality was significantly lower among AI/AN persons than among Whites (Table 1). Although the highest death rates for AI/AN persons occurred in the 25 to 44 and 45 to 64 year age groups, risk ratios were significantly lower than those for Whites. In both AI/AN persons and Whites, death rates among males were much higher than those among females. AI/AN populations in the Alaska, Northern Plains, and Southern Plains regions had significantly higher overall death rates than Whites in those regions. Other regions, including the East, Pacific Coast, and Southwest, had significantly lower death rates among AI/AN persons than among Whites. Both AI/AN males and females had higher death rates than White males and females in the Alaska region, and AI/AN males had significantly lower death rates than White males in the East and Pacific Coast regions. AI/AN females had the greatest disparities overall when compared with White females in the Alaska and Northern Plains regions.
1999–2009.
HIV death rates are characterized by several instances in which death rates for AI/AN populations shifted from being significantly lower than death rates for Whites in 1990 to 1998 to being significantly higher in 1999 to 2009. Overall, HIV death rates were significantly greater among AI/AN populations than among Whites. The highest HIV death rates in AI/AN populations occurred in the 25 to 44 and 45 to 64 year age groups, which were significantly greater than those in Whites. AI/AN males and females had significantly higher death rates than White males and females, a reversal from the significantly lower rate for males between 1990 to 1998. We found higher death rates among AI/AN persons than Whites in each IHS region, although the disparities were greatest between AI/AN and White females. We observed the greatest significant rate ratio for all HIV measures among Alaska females.
Trends.
Although HIV death rates decreased for both AI/AN persons and Whites from 1990–1998 to 1999–2009, the disparity between AI/AN persons and Whites reversed, with death rates among AI/AN individuals moving from being significantly lower to being significantly higher overall (Table 1). These rates changed dramatically in the late 1990s (Figure 1).
FIGURE 1—
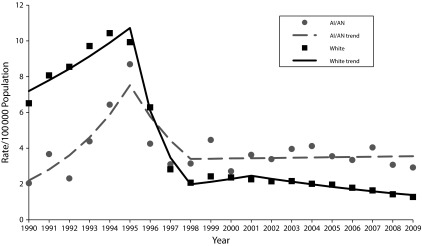
Annual age-adjusted HIV death rates and joinpoint trend lines for American Indian/Alaska Native and White people: Contract Health Service Delivery Area counties, United States, 1990–2009.
Note. AI/AN = American Indian/Alaska Native; IHS = Indian Health Service. Analyses are limited to people of non-Hispanic origin. The following states and years of data were excluded because Hispanic origin was not collected on the death certificate: LA, 1990; NH, 1990–1992; OK, 1990–1996. AI/AN race was reported from death certificates or through linkage with the IHS patient registration database. Rates are per 100 000 people and were age adjusted to the 2000 US standard population (11 age groups; Census P25-113020).
Source. AI/AN Mortality Database (1990–2009).
Tuberculosis Mortality
1990–1998.
Average annual TB death rates among the AI/AN population from 1990 to 1998 are shown in Table 2. From 1990 to 1998, overall TB mortality was significantly higher among AI/AN persons than among Whites (Table 2). During this decade, with the exception of those aged 0 to 24 years, death rates were higher among AI/AN persons of all age groups than among Whites of the same ages. This difference was greatest for those aged 85 and older, with the risk of dying of TB among AI/AN populations being almost 15 times as high as that among Whites. Both AI/AN males and females had a significantly higher death rate than Whites during 1990 to 1998 and, except for females in the East region, this pattern was consistent throughout all regions.
TABLE 2—
Average Annual TB Death Rates and Rate Ratios by Age, Sex, and Indian Health Service Region for American Indian/Alaska Native and White People: Contract Health Service Delivery Area Counties, United States, 1990–1998 and 1999–2009
| 1990–1998 |
1999–2009 |
|||||
| Variable | AI/AN Death Rate (per 100 000 Population) | White Death Rate (per 100 000 Population) | AI/AN:White RR (95% CI) | AI/AN Death Rate (per 100 000 Population) | White Death Rate (per 100 000 Population) | AI/AN:White RR (95% CI) |
| Total | 3.3 | 0.3 | 11.37* (9.68, 13.28) | 1.5 | 0.1 | 11.50* (10.19, 12.94) |
| Age group, y | ||||||
| 0–24 | < 0.1 | < 0.1 | 8.56 (0.83, 47.16) | … | 0.0 | NA |
| 25–44 | 0.5 | 0.1 | 7.65* (3.87, 13.88) | 0.4 | 0.0 | 20.21* (9.96, 39.94) |
| 45–64 | 3.7 | 0.3 | 13.96* (10.15, 18.90) | 1.4 | 0.1 | 12.70* (8.99, 17.65) |
| 65–84 | 17.2 | 1.4 | 12.00* (9.36, 15.21) | 8.0 | 0.6 | 13.84* (10.60, 17.84) |
| ≥ 85 | 46.7 | 3.2 | 14.78* (9.04, 23.05) | 21.4 | 1.7 | 12.34* (7.36, 19.64) |
| Sex | ||||||
| Male | 4.0 | 0.4 | 9.49* (7.50, 11.83) | 2.0 | 0.2 | 12.10* (9.21, 15.57) |
| Female | 2.8 | 0.2 | 14.47* (11.43, 18.08) | 1.3 | 0.1 | 14.45* (10.94, 18.74) |
| IHS region | ||||||
| Alaska | 3.7 | 0.3 | 13.99* (4.09, 85.73) | 3.9 | 0.1 | 48.51* (13.99, 315.95) |
| Male | 3.8 | 0.3 | 13.97* (4.08, 84.97) | 4.8 | 0.1 | 70.12* (12.01, 665.05) |
| Female | 4.4 | 0.1 | 44.41* (6.72, 14.08) | 3.3 | 0.1 | 42.27* (7.19, 1773.31) |
| East | 1.3 | 0.3 | 4.64* (1.36, 10.79) | … | 0.1 | NA |
| Male | 2.7 | 0.4 | 6.29* (1.13, 17.27) | … | 0.1 | NA |
| Female | 0.5 | 0.2 | 2.81 (0.07, 13.32) | … | 0.1 | NA |
| Northern Plains | 4.4 | 0.2 | 23.10* (15.33, 33.58) | 1.7 | 0.1 | 19.67* (11.88, 30.94) |
| Male | 5.1 | 0.3 | 17.20* (9.18, 29.47) | 1.9 | 0.1 | 19.1* (8.77, 37.51) |
| Female | 3.9 | 0.1 | 33.05* (17.86, 56.93) | 1.6 | 0.1 | 21.65* (10.54, 40.29) |
| Pacific Coast | 1.8 | 0.3 | 5.41* (3.32, 8.26) | 0.7 | 0.1 | 6.14* (3.42, 10.11) |
| Male | 2.5 | 0.4 | 5.56* (2.78, 9.77) | 0.9 | 0.2 | 5.97* (2.85, 11.07) |
| Female | 1.2 | 0.2 | 5.24* (2.27, 10.12) | 0.5 | 0.1 | 5.88* (1.88, 13.44) |
| Southern Plains | 2.4 | 0.3 | 7.66* (4.55, 12.90) | 1.1 | 0.2 | 5.54* (3.31, 8.84) |
| Male | 3.2 | 0.4 | 7.60* (3.59, 16.10) | 1.7 | 0.3 | 5.66* (2.71, 10.52) |
| Female | 2.0 | 0.2 | 8.09* (3.68, 17.86) | 0.7 | 0.1 | 6.49* (2.68, 13.97) |
| Southwest | 4.7 | 0.3 | 13.68* (10.29, 17.95) | 2.3 | 0.1 | 15.56* (11.25, 21.14) |
| Male | 5.4 | 0.5 | 10.66* (7.09, 15.56) | 2.8 | 0.2 | 14.21* (8.84, 21.88) |
| Female | 4.2 | 0.2 | 19.19* (12.52, 28.82) | 2.0 | 0.1 | 19.20* (11.84, 30.08) |
Note. AI/AN = American Indian/Alaska Native; CI = confidence interval; IHS = Indian Health Service; NA = not applicable; RR = rate ratio. The sample size was n = 372. Dashes indicate that counts < 10 were suppressed; if no cases were reported, then rates and RRs could not be calculated. Cases aged 0–24 y are included in overall totals, but rows have been suppressed as a result of few cases. Analyses are limited to people of non-Hispanic origin. AI/AN race is reported from death certificates or through linkage with the IHS patient registration database. Rates are per 100 000 people and were age adjusted to the 2000 US standard population (11 age groups; Census P25-113020). RRs were calculated in SEER*Stat before rounding and may not equal RRs calculated from rates presented in table. IHS regions are defined as follows: Alaskaa; Northern Plains (IL, IN,a IA,a MI,a MN,a MT,a NE,a ND,a SD,a WI,a WYa); Southern Plains (OK,a KS,a TXa); Southwest (AZ,a CO,a NV,a NM,a UTa); Pacific Coast (CA,a ID,a OR,a WA,a HI); East (AL,a AR, CT,a DE, FL,a GA, KY, LA,a ME,a MD, MA,a MS,a MO, NH, NJ, NY,a NC,a OH, PA,a RI,a SC,a TN, VT, VA, WV, DC). Percentage regional coverage of AI/AN persons in CHSDA counties to AI/AN persons in all counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; East = 18.2%; total US = 64.2%.
Source. AI/AN Mortality Database (1990–2009); the following states and years of data were excluded because Hispanic origin was not collected on the death certificate: LA, 1990; NH, 1990–1992; OK, 1990–1996.
Identifies states with more than 1 county designated as CHSDA.
*P < .05.
1999–2009.
Average annual TB death rates among AI/AN populations from 1999 to 2009 are shown in Table 2. From 1999 to 2009, overall TB death rates were significantly higher among AI/AN persons compared with those for Whites (Table 2). Death rates were significantly higher among AI/AN individuals in all age groups except for ages 0 to 24 years, compared with Whites of the same age groups. Similar to the previous decade, disparities in death rates were greatest between AI/AN and White women. Except for the East region, in which no AI/AN TB deaths occurred from 1999 to 2009, we found higher death rates among AI/AN persons than among Whites in each IHS region, with the greatest disparity in the Alaska region.
Trends.
TB mortality decreased significantly over time for AI/AN persons and Whites, with specific statistical demographic and geographic comparisons shown in Table 2. From 1990 to 1998 to 1999 to 2009, the death rate declined from 3.3 to 1.5 for AI/AN persons; that for Whites declined from 0.3 to 0.1. Although the rate of decline was similar in both groups, TB death rates were consistently higher among AI/AN individuals. Furthermore, in the Alaska region, the disparity between AI/AN persons and Whites increased between time periods.
Tuberculosis–HIV Coinfection Mortality
Overall, for the entire time period of 1990 to 2009, only 7 death records listed both HIV and TB as a primary or underlying cause of death for AI/AN persons (data not shown).
DISCUSSION
Cause-specific death is an important metric of population health. This study highlights the disparate impact of HIV and TB on AI/AN populations compared with Whites. Although AI/AN populations and Whites have experienced a decline in death rates over time, more recent death rates from HIV and TB are significantly higher among AI/AN populations than among Whites.
We described a marked reversal in HIV death disparities between AI/AN persons and Whites over the 2 time periods studied, roughly coinciding with the advent and increasing availability of antiretroviral therapy in 1998. HIV-infected people on appropriate antiretroviral therapy have reduced or delayed progression to AIDS and significantly reduced mortality. Nationally, antiretroviral therapy has dramatically reduced HIV-related death rates and has changed HIV infection into a manageable chronic disease.28–30 However, the higher HIV death rate and slower decline in death rates among AI/AN persons suggests that the AI/AN population has less access to or use of antiretroviral therapy than Whites. Alternatively, the higher HIV death rate among AI/AN persons may be caused by late diagnosis after development of AIDS. Further investigation of undiagnosed cases, comorbidities, time to diagnosis, and prevalence of antiretroviral therapy use among AI/AN populations in each IHS region is needed to clarify the causes for this reversal in HIV death disparity.
We found that TB death rates in AI/AN persons were consistently elevated throughout the study period and were associated with some of the greatest disparities in rates for all infectious disease causes of death among AI/AN persons.2 TB deaths rates were extremely high among people aged 85 years or older. TB in older adults is often caused by reactivation of latent TB infection as a result of a weakened immune system.31,32 Age; comorbid conditions, such as diabetes; or even certain medications (e.g., corticosteroids) can compromise the immune systems of older adults.31,32 Also, TB in older adults can be difficult to diagnose because TB often presents in atypical ways. Patients may report nonspecific symptoms,33 and comorbid conditions, especially those affecting immune response, may mask TB symptoms and confound diagnosis by reducing the initial response to TB diagnostic tests.31,33 Particularly worrisome is the risk that reactivation of latent TB infection in an older AI/AN individual will result in transmission to younger contacts, thus perpetuating the cycle of TB in this population. Even though older people have a greater overall risk of death from all causes, regardless of TB disease, the disparity between older AI/AN persons and Whites in TB deaths highlights the need to actively target TB diagnostic and treatment efforts toward older AI/AN populations.
We identified very few deaths with TB–HIV coinfection. In the United States, among people with TB with a known HIV status aged 25 to 44 years, 7.7% were reported as HIV-positive8; among AI/AN persons, this percentage was approximately 3%.34 HIV infection significantly increases the risk of developing and dying from TB.35,36 Among people with latent TB infection, HIV infection is the strongest known risk factor for progressing to TB. TB is associated with faster AIDS progression and is 1 of the leading causes of death among HIV-infected people.37 The reasons for not finding more deaths resulting from TB–HIV coinfection among AI/AN persons in this study are unknown but may reflect a failure to ascertain deaths related to coinfection. No method of assessing causes of death is completely reliable.38 In-depth mortality reviews can help improve the accuracy of cause-of-death data.38
The results from this study highlight several groups that should be targeted to reduce mortality caused by HIV and TB in AI/AN persons. For example, disparities in HIV and TB deaths between AI/AN and White females were seen in both study periods and were greater than disparities seen among AI/AN and White males. For HIV deaths, the disparity was marginally significant for 1990 to 1998 and increased greatly for 1999 to 2009. The disparity remained consistently elevated over time for TB deaths. The disparity in HIV deaths follows a similar pattern seen among women in other small populations; in 2010, the CDC estimated that Hispanic women and non-Hispanic Black women had 15 times the TB death rate and more than twice the HIV death rate of non-Hispanic White women.39,40
Both HIV and TB require lengthy and sometimes complicated treatment regimens. Access and adherence to appropriate therapy is essential for the successful management and reduction of death resulting from HIV infection and TB disease. However, access to care can be complicated for AI/AN patients because of factors such as remote rural residence (which necessitates traveling long distances for care), lower rates of health insurance, and high rates of poverty.41–44 Substance abuse program support may need special attention; 1 recent study demonstrated that alcohol abuse in an American Indian HIV-positive population had a negative impact on HIV viral loads.45
In rural settings with low population density, practitioners with training and experience in caring for people with HIV or complicated forms of TB are often less available. Rural programs may need to make additional use of alternative service delivery methods such as telemedicine and home care programs and need additional resources to reach hard-to-reach populations. Additional variables that merit further investigation on access to care and outcomes include coinfection such as HCV–HIV,46 culturally appropriate care, and stigma of TB or HIV diagnosis. In addition, HIV-specific variables of importance include transmission via sexual contact and injection drug use. These factors may have specific dynamics within AI/AN communities that may greatly affect disease incidence, diagnosis, and adherence to care.47–52
Limitations
The primary limitations of this study include the use of ICD–9 and ICD–10 codes to determine infectious disease causes of death53,54 and the uncorrected racial misclassification of AI/AN persons.55 Federally recognized tribes vary substantially in the proportion of Native ancestry required for tribal membership and therefore for eligibility for IHS services. Whether and how this discrepancy in tribal membership requirements influenced some of our findings is unclear, although our findings are consistent with prior reports. In addition, the findings from CHSDA counties in this study do not represent all AI/AN populations in the United States or individual IHS regions. Furthermore, the analyses based on CHSDA designation exclude many AI/AN decedents in urban areas that are not part of a CHSDA county, and AI/AN persons who reside in rural areas have higher levels of poverty and less access to health care, which may influence mortality trends,56,57 although health disparities and presence of risk factors for disease transmission are present in the AI/AN population that has migrated to urban areas.58 Finally, although the exclusion of Hispanic AI/AN persons from the analyses reduces the overall count of deaths among AI/AN persons by less than 5%, it may disproportionately affect some states.
Conclusions
Lower TB and HIV death rates in the United States have not translated to equal reductions in death rates among AI/AN individuals compared with Whites, and significant disparities persist. AI/AN populations must be prioritized and resources allocated for greater TB and HIV control, using both risk-based testing and screening as per national recommendations,59,60 as well as linkages and adherence to care.
Acknowledgments
We would like to thank David Espey, Melissa Jim, Diana Roberts, and Don Haverkamp for their technical contributions to this study.
Human Participant Protection
The Centers for Disease Control and Prevention and the Indian Health Service determined this project constituted public health practice and not research; therefore, no formal institutional review board approvals were required.
References
- 1.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL. Global Burden of Disease and Risk Factors. Washington, DC: World Bank; 2006. [PubMed] [Google Scholar]
- 2. Cheek JE, Holman RC, MS, Redd JT, Haberling D, Hennessy TW. Infectious disease mortality among American Indians and Alaska Natives, 1999–2009. Am J Public Health. 2014;104(6 suppl 3):S446–S452. [DOI] [PMC free article] [PubMed]
- 3.US Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2020. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/pdfs/HIV.pdf. Accessed May 16, 2013.
- 4.Dye C, Maher D, Weil D, Espinal M, Raviglione M. Targets for global tuberculosis control. Int J Tuberc Lung Dis. 2006;10(4):460–462. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. HIV Surveillance Report, 2011; vol. 23. 2013. Available at: http://www.cdc.gov/hiv/topics/surveillance/resources/reports. Accessed July 2, 2013.
- 6.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 US Dependent Areas—2010. HIV Surveillance Supplemental Report 2012, Vol. 17, No. 3 (Part A); 2012. Available at: http://www.cdc.gov/hiv/library/reports/surveillance/2010/surveillance_Report_vol_17_no_3.html. Accessed March 20, 2013.
- 7.Martin LJ, Houston S, Yasui Y, Wild TC, Saunders LD. All-cause and HIV-related mortality rates among HIV-infected patients after initiating highly active antiretroviral therapy: the impact of aboriginal ethnicity and injection drug use. Can J Public Health. 2011;102(2):90–96. doi: 10.1007/BF03404154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Reported tuberculosis in the United States, 2012. Available at: http://www.cdc.gov/tb/statistics/reports/2012/pdf/report2012.pdf. Accessed August 15, 2013.
- 9.Marks SM, Magee E, Robison V. Patients diagnosed with tuberculosis at death or who died during therapy: association with the human immunodeficiency virus. Int J Tuberc Lung Dis. 2011;15(4):465–470. doi: 10.5588/ijtld.10.0259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.White House Office of National AIDS Policy. National HIV/AIDS strategy for the United States. 2010. Available at: http://aids.gov/federal-resources/national-hiv-aids-strategy/nhas.pdf. Accessed March 20, 2013.
- 11.Centers for Disease Control and Prevention. Strategic planning for tuberculosis (TB) elimination in the United States and prevention and control of TB globally. Available at: http://www.cdc.gov/tb/about/strategicplan.htm. Accessed May 16, 2013.
- 12.Espey D, Paisano R, Cobb N. Regional patterns and trends in cancer mortality among American Indians and Alaska Natives, 1990-2001. Cancer. 2005;103(5):1045–1053. doi: 10.1002/cncr.20876. [DOI] [PubMed] [Google Scholar]
- 13.Rhoades DA. Racial misclassification and disparities in cardiovascular disease among American Indians and Alaska Natives. Circulation. 2005;111(10):1250–1256. doi: 10.1161/01.CIR.0000157735.25005.3F. [DOI] [PubMed] [Google Scholar]
- 14.National Center for Health Statistics, Division of Vital Statistics. National Vital Statistics System. Available at: http://www.cdc.gov/nchs/nvss.htm. Accessed May 2, 2012.
- 15.International Classification of Diseases, 10th Revision. . Geneva, Switzerland: World Health Organization; 1990. [Google Scholar]
- 16.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980. [Google Scholar]
- 17.Arias E, Schauman W, Eschbach K, Sorlie P. The validity of race and Hispanic origin reporting on death certificates in the United States. Vital Health Stat 2. 2008;148:1–23. [PubMed] [Google Scholar]
- 18.Indian Health Service. Indian Health Service areas. Available at: http://www.ihs.gov/locations. Accessed Febuary 5, 2012.
- 19.Espey DK, Jim MA, Richards T, Begay C, Haverkamp D, Roberts D. Methods for improving the quality and completeness of mortality data for American Indians and Alaska Natives. Am J Public Health. 2014;104(6 suppl 3):S286–S294. doi: 10.2105/AJPH.2013.301716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Day JC. Population Projections of the United States by Age, Sex, Race, and Hispanic Origin: 1995 to 2050. US Bureau of the Census, Current Population Reports, P25-1130. Washington, DC: US Government Printing Office; 1996. [Google Scholar]
- 21.Denny CH, Taylor TL. American Indian and Alaska Native health behavior: findings from the Behavioral Risk Factor Surveillance System, 1992-1995. Ethn Dis. 1999;9(3):403–409. [PubMed] [Google Scholar]
- 22.Wiggins CL, Espey DK, Wingo PA et al. Cancer among American Indians and Alaska Natives in the United States, 1999-2004. Cancer. 2008;113(5 suppl):1142–1152. doi: 10.1002/cncr.23734. [DOI] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics. U.S. Census populations with bridge race categories. 2012. http://www.cdc.gov/nchs/nvss/bridged_race.htm . Accessed August, 2012.
- 24.National Vital Statistics System. Adjusted populations for the counties/parishes affected by Hurricanes Katrina and Rita. Available at: http://seer.cancer.gov/popdata/hurricane_adj.html. Accessed March 18, 2013.
- 25.Edwards BK, Noone AM, Mariotto AB et al. Annual Report to the Nation on the status of cancer, 1975-2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. 2013 doi: 10.1002/cncr.28509. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. SEER*Stat [computer program]. Version 8.0.2. 2013. Available at: http://seer.cancer.gov/seerstat. Accessed April 10, 2013.
- 27.Tiwari RC, Clegg LX, Zou Z. Efficient interval estimation for age-adjusted cancer rates. Stat Methods Med Res. 2006;15(6):547–569. doi: 10.1177/0962280206070621. [DOI] [PubMed] [Google Scholar]
- 28.Antiretroviral Therapy Cohort Collaboration. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;372(9635):293–299. doi: 10.1016/S0140-6736(08)61113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.HIV-CAUSAL Collaboration. Ray M, Logan R et al. The effect of combined antiretroviral therapy on the overall mortality of HIV-infected individuals. AIDS. 2010;24(1):123–137. doi: 10.1097/QAD.0b013e3283324283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kitahata MM, Gange SJ, Abraham AG et al. Effect of early versus deferred antiretroviral therapy for HIV on survival. N Engl J Med. 2009;360(18):1815–1826. doi: 10.1056/NEJMoa0807252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zevallos M, Justman JE. Tuberculosis in the elderly. Clin Geriatr Med. 2003;19(1):121–138. doi: 10.1016/s0749-0690(02)00057-5. [DOI] [PubMed] [Google Scholar]
- 32.Dutt AK, Stead WW. Tuberculosis in the elderly. Med Clin North Am. 1993;77(6):1353–1368. doi: 10.1016/s0025-7125(16)30198-5. [DOI] [PubMed] [Google Scholar]
- 33.Pratt RH, Winston CA, Kammerer JS, Armstrong LR. Tuberculosis in older adults in the United States, 1993-2008. J Am Geriatr Soc. 2011;59(5):851–857. doi: 10.1111/j.1532-5415.2011.03369.x. [DOI] [PubMed] [Google Scholar]
- 34.Bloss E, Holtz TH, Jereb J et al. Tuberculosis in indigenous peoples in the US, 2003–2008. Public Health Rep. 2011;126(5):677–689. doi: 10.1177/003335491112600510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gray JM, Cohn DL. Tuberculosis and HIV coinfection. Semin Respir Crit Care Med. 2013;34(1):32–43. doi: 10.1055/s-0032-1333469. [DOI] [PubMed] [Google Scholar]
- 36.Badri M, Ehrlich R, Wood R, Pulerwitz T, Maartens G. Association between tuberculosis and HIV disease progression in a high tuberculosis prevalence area. Int J Tuberc Lung Dis. 2001;5(3):225–232. [PubMed] [Google Scholar]
- 37.World Health Organization. Frequently asked questions about TB and HIV. Available at: http://www.who.int/tb/challenges/hiv/faq/en. Accessed August 16, 2013.
- 38.Sprinson J, Bahl M, Benjamin R et al. TB death assessment tool in California: development and pilot test. TB Notes Newsletter. 2008:4. [Google Scholar]
- 39.Centers for Disease Control and Prevention, National Center for Health Statistics. The autopsy, medicine, and mortality statistics. Vital Health Stat 3. 2001;32:1–42. [PubMed] [Google Scholar]
- 40.Steele CB, Richmond-Reese V, Lomax S. Report from the CDC: racial and ethnic disparities in HIV/AIDS, sexually transmitted diseases, and tuberculosis among women. J Womens Health (Larchmt) 2006;15(2):116–122. doi: 10.1089/jwh.2006.15.116. [DOI] [PubMed] [Google Scholar]
- 41.US Census Bureau. The American community—American Indians and Alaska Natives: 2004. American Community Survey Reports. Available at: http://www.census.gov/prod/2007pubs/acs-07.pdf. Accessed May 16, 2013.
- 42.Miller CL, Spittal PM, Wood E et al. Inadequacies in antiretroviral therapy use among aboriginal and other Canadian populations. AIDS Care. 2006;18(8):968–976. doi: 10.1080/09540120500481480. [DOI] [PubMed] [Google Scholar]
- 43.Zuckerman S, Haley J, Roubideaux Y, Lillie-Blanton M. Health service access, use, and insurance coverage among American Indians/Alaska Natives and Whites: what role does the Indian Health Service play? Am J Public Health. 2004;94(1):53–59. doi: 10.2105/ajph.94.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Probst JC, Moore CG, Glover SH, Samuels ME. Person and place: the compounding effects of race/ethnicity and rurality on health. Am J Public Health. 2004;94(10):1695–1703. doi: 10.2105/ajph.94.10.1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Iralu J, Duran B, Pearson C, Jiang Y, Foley K, Harrison M. Risk factors for HIV disease progression in a rural Southwest American Indian population. Public Health Rep. 2010;125(suppl 4):43–50. doi: 10.1177/00333549101250S408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Braitstein P, Montessori V, Chan K et al. Quality of life, depression and fatigue among persons co-infected with HIV and hepatitis C: outcomes from a population-based cohort. AIDS Care. 2005;17(4):505–515. doi: 10.1080/09540120412331291733. [DOI] [PubMed] [Google Scholar]
- 47.Vernon I, Jumper-Thurman P. The changing face of HIV/AIDS among native populations. J Psychoactive Drugs. 2005;37(3):247–255. doi: 10.1080/02791072.2005.10400516. [DOI] [PubMed] [Google Scholar]
- 48.Bertolli J, McNaghten AD, Campsmith M et al. Surveillance systems monitoring HIV/AIDS and HIV risk behaviors among American Indians and Alaska Natives. AIDS Educ Prev. 2004;16(3):218–237. doi: 10.1521/aeap.16.3.218.35442. [DOI] [PubMed] [Google Scholar]
- 49.McNaghten AD, Neal JJ, Li J, Fleming PL. Epidemiologic profile of HIV and AIDS among American Indians/Alaska natives in the USA through 2000. Ethn Health. 2005;10(1):57–71. doi: 10.1080/1355785052000323038. [DOI] [PubMed] [Google Scholar]
- 50.Wood E, Lloyd-Smith E, Li K et al. Frequent needle exchange use and HIV incidence in Vancouver, Canada. Am J Med. 2007;120(2):172–179. doi: 10.1016/j.amjmed.2006.02.030. [DOI] [PubMed] [Google Scholar]
- 51.Craib KJ, Spittal PM, Wood E et al. Risk factors for elevated HIV incidence among aboriginal injection drug users in Vancouver. CMAJ. 2003;168(1):19–24. [PMC free article] [PubMed] [Google Scholar]
- 52.Saylors K, Jim N, Plasencia AV, Smith D. Faces of HIV/AIDS and substance abuse in Native American communities. J Psychoactive Drugs. 2005;37(3):241–246. doi: 10.1080/02791072.2005.10400515. [DOI] [PubMed] [Google Scholar]
- 53.Pinner RW, Teutsch SM, Simonsen L et al. Trends in infectious diseases mortality in the United States. JAMA. 1996;275(3):189–193. [PubMed] [Google Scholar]
- 54.Armstrong GL, Conn LA, Pinner RW. Trends in infectious disease mortality in the United States during the 20th century. JAMA. 1999;281(1):61–66. doi: 10.1001/jama.281.1.61. [DOI] [PubMed] [Google Scholar]
- 55.Jim MA, Arias E, Seneca DS et al. Racial misclassification of American Indians and Alaska Natives by Indian Health Service Contract Health Service Delivery Area. Am J Public Health. 2014;104(6 suppl 3):S295–S302. doi: 10.2105/AJPH.2014.301933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Urban Indian Health Institute, Seattle Indian Health Board. Reported health and health-influencing behaviors among urban American Indians and Alaska Natives: an analysis of data collected by the Behavioral Risk Factor Surveillance System. 2008. Available at: http://www.uihi.org/wp-content/uploads/2009/01/health_health-influencing_behaviors_among_urban_indiansupdate-121020081.pdf. Accessed April 20, 2012.
- 57.Urban Indian Health Commission. Invisible Tribes: Urban Indians and Their Health in a Changing World. 2007 Seattle, WA. [Google Scholar]
- 58.Burhansstipanov L. Urban Native American health issues. Cancer. 2000;88(5 suppl):1207–1213. doi: 10.1002/(sici)1097-0142(20000301)88:5+<1207::aid-cncr5>3.3.co;2-k. [DOI] [PubMed] [Google Scholar]
- 59.US Preventive Services Task Force. Screening for HIV. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspshivi.htm. Accessed May 15, 2013.
- 60.US Preventive Services Task Force. Screening for tuberculosis infection. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspstubr.htm. Accessed May 15, 2013.


