Abstract
Objectives. We characterized estimates of colorectal cancer (CRC) in American Indians/Alaska Natives (AI/ANs) compared with Whites using a linkage methodology to improve AI/AN classification in incidence and mortality data.
Methods. We linked incidence and mortality data to Indian Health Service enrollment records. Our analyses were restricted to Contract Health Services Delivery Area counties. We analyzed death and incidence rates of CRC for AI/AN persons and Whites by 6 regions from 1999 to 2009. Trends were described using linear modeling.
Results. The AI/AN colorectal cancer incidence was 21% higher and mortality 39% higher than in Whites. Although incidence and mortality significantly declined among Whites, AI/AN incidence did not change significantly, and mortality declined only in the Northern Plains. AI/AN persons had a higher incidence of CRC than Whites in all ages and were more often diagnosed with late stage CRC than Whites.
Conclusions. Compared with Whites, AI/AN individuals in many regions had a higher burden of CRC and stable or increasing CRC mortality. An understanding of the factors driving these regional disparities could offer critical insights for prevention and control programs.
Colorectal cancer (CRC) is the second leading cause of cancer death for cancers that affect both men and women in the United States, following lung cancer.1 At current rates, approximately 1 in 17 men and women in the United States will be diagnosed with this disease in their lifetime.2 Understanding the epidemiology of CRC in minority populations is critical to inform cancer prevention and control programs. However, high rates of racial misclassification in medical records and death certificates of American Indian and Alaska Native (AI/AN) people have led to underestimates of their CRC burden.3 As a result, cancer disparities in AI/AN populations have been underappreciated and underserved.
Because Indian Health Service (IHS) and tribal health facilities predominately serve AI/AN individuals, linking IHS and tribal user data to national cancer registry data affords a more accurate determination of CRC epidemiology for the AI/AN population.4 Previously, we applied this approach to cancer incidence data from 1999 to 2004 and found that AI/AN persons were more often diagnosed with CRC at younger ages, and had more advanced stages of disease compared with non-Hispanic White persons.5 The linkage also unveiled significant regional variation in AI/AN colorectal cancer incidence.
Screening can lower CRC incidence and mortality.6 Removing premalignant polyps can prevent the disease, and diagnosing CRC at an earlier stage offers significant survival benefit.7,8 AI/AN screening lags significantly behind that of Whites.9 Although this would portend higher CRC death rates among AI/AN persons than in Whites, more accurate data on CRC mortality differences are needed.
We applied a linkage methodology to both incidence and mortality data to more accurately characterize CRC incidence and mortality for AI/AN persons by region.
METHODS
Detailed methods for generating the analytical mortality files are described elsewhere in this supplement.10 Detailed methods describing incidence data and analysis are available in a previous publication.4 An abbreviated description of our methods follows.
Data Sources
Population estimates.
Bridged single-race population estimates developed by the US Census Bureau and the Centers for Disease Control and Prevention (CDC) National Center for Health Statistics (NCHS), which were adjusted for population shifts because of Hurricanes Katrina and Rita in 2005, are included as denominators in the calculations of death rates.11,12 Bridged single-race data allow for comparability between the pre- and post-2000 race/ethnicity population estimates.
During preliminary analyses, we discovered that the updated bridged intercensal populations estimates significantly overestimated AI/AN persons of Hispanic origin.13 Therefore, to avoid underestimating incidence and mortality in AI/AN populations, our analyses were limited to non-Hispanic AI/AN individuals. We chose Non-Hispanic Whites as the most homogeneous referent group. Henceforth, the qualifying term “non-Hispanic” is omitted when discussing both groups.
Death records.
Death certificate data are compiled by each state and sent to the NCHS, where they are edited for consistency and stripped of personal identifiers. NCHS publishes this information as part of the National Vital Statistics System (NVSS) and includes underlying and multiple cause of death fields, state of residence, age, gender, race, and ethnicity.14 NCHS applies a bridging algorithm nearly identical to that used by the Census Bureau to assign a single race to decedents with multiple races on their death certificates.15a
The IHS patient registration database was linked to death certificate data in the National Death Index to identify AI/AN deaths misclassified as non-Native.10 Following this linkage, a flag indicating a positive link to IHS was added as an indicator of AI/AN ancestry to the NVSS mortality file. This file was combined with the population estimates to create an analytical file in SEER*Stat version 8.0.4 (National Cancer Institute [NCI], Bethesda, Maryland; AI/AN-US Mortality Database [AMD]), which includes all deaths for all races reported to the NCHS from 1990 to 2009. Race for AI/AN deaths in this report were based on criteria described elsewhere in this supplement, combining race classification by NCHS based on the death certificate and information from data linkages between the IHS patient registration database and the National Death Index.10 For deaths between 1990 and 1998, the underlying cause of death was coded according to the International Classification of Diseases, Ninth Revision (ICD-9).15b For 1999 to 2009, the ICD-10 was used.15c
Incidence data.
We identified incidence of CRC cases between 1999 and 2009 from population-based central cancer registries in the CDC National Program of Cancer Registries (NPCR)16 and the NCI Surveillance, Epidemiology, and End Results (SEER) program.17 For data to be included for a given year, registries had to meet data standards developed for the US Cancer Statistics report.16 Participating registries classified tumor histology, tumor behavior, and primary cancer site according to the International Classification of Diseases for Oncology, Third Edition (ICD-O-3).18 To identify CRC cases among AI/ANs misclassified as other races, we linked central cancer registries to cancer registry records with IHS patient registration files as previously described.4,16,19 Stage at diagnosis was based on the SEER summary staging system: localized (confined to colon or rectum); regional (direct extension of the cancer to adjacent organs or tissues, or to regional lymph nodes); distant (metastasis to other areas of the body); and unstaged.20 Stage was then grouped into early (localized) and late (regional or distant) categories.
Geographic coverage.
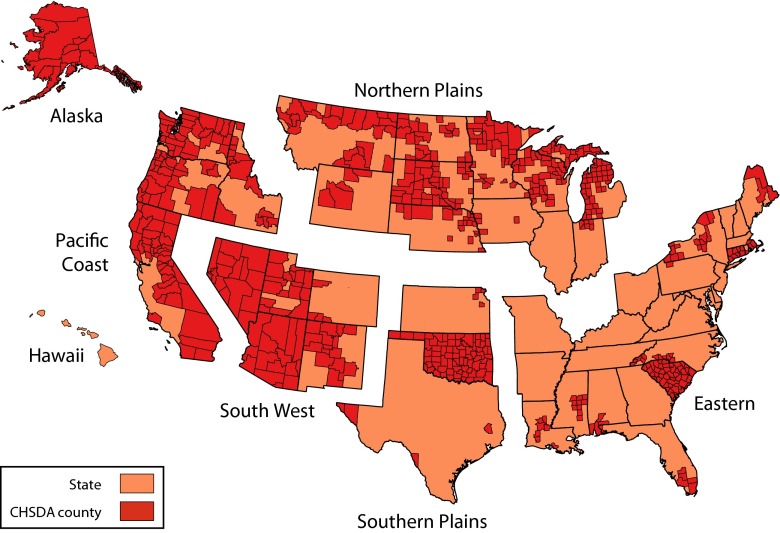
Final analyses were restricted to Contract Health Service Delivery Area (CHSDA) counties that contained federally recognized tribal lands or are adjacent to tribal lands (Figure 1).10 CHSDA residence is used by the IHS to determine eligibility for services not directly available within the IHS. Linkage studies indicate less racial misclassification for AI/AN persons in these counties.10,21 CHSDA counties also have higher proportions of AI/AN persons than do non-CHSDA counties, with 64% of AI/AN individuals residing in the 637 CHSDA counties (representing 20% of the 3141 counties in the United States). Although less geographically representative, we used analyses restricted to CHSDA counties for incidence and death rates to improve accuracy in interpreting AI/AN colorectal cancer statistics.
FIGURE 1—
States and Contract Health Service Delivery Area (CHSDA) Counties by Indian Health Service Region: Colorectal Cancer Mortality and Incidence in American Indian/Alaska Native Persons, 1999–2009.
We completed analyses for all regions combined and by individual IHS regions: Northern Plains, Alaska, Southern Plains, Southwest, Pacific Coast, and East (Figure 1).10 We used identical or similar regional analyses for other health-related publications focusing on AI/AN persons.22–24 We found regional strata to be preferable to using smaller jurisdictions, such as the administrative areas defined by IHS,25 which yielded less stable estimates. Additional details about CHSDA counties and IHS regions are provided elsewhere (Table 1).10
TABLE 1—
Colorectal Cancer Incidence Rates, Death Rates, and Mortality/Incidence Rate Ratios by Indian Health Service Region and Contract Health Service Delivery Area and Gender for American Indian/Alaska Native and White Persons: United States, 2005–2009
| Incidence | Mortality | Mortality/Incidence | ||||||||||||
| IHS Region/Gender | AI/AN Cases, No. | AI/AN Rate | White Cases, No. | White Rate | AI/AN:White RR (95% CI) | AI/AN Deaths, No. | AI/AN Rate | White Deaths, No. | White Rate | AI/AN:White RR (95% CI) | AI/AN RR (95% CI) | AI/AN 1-(M/I) | White RR (95% CI) | White 1-(M/I) |
| CHSDA counties | ||||||||||||||
| Northern Plains | ||||||||||||||
| Both genders | 510 | 67.3 | 19 949 | 44.0 | 1.53* (1.39, 1.68) | 196 | 26.9 | 7784 | 16.1 | 1.65* (1.43, 1.96) | 0.41 (0.34, 0.49) | 0.59 | 0.37 (0.36, 0.38) | 0.63 |
| Men | 275 | 78.5 | 10 124 | 49.8 | 1.58* (1.37, 1.81) | 110 | 34.5 | 3869 | 18.6 | 1.83* (1.46, 2.31) | 0.45 (0.34, 0.58) | 0.55 | 0.38 (0.36, (0.39) | 0.62 |
| Women | 235 | 57.9 | 9825 | 39.2 | 1.48* (1.28, 1.69) | 86 | 21.5 | 3915 | 13.9 | 1.49* (1.21, 1.93) | 0.38 (0.29, 0.50) | 0.62 | 0.36 (0.34, 0.37) | 0.64 |
| Alaska | ||||||||||||||
| Both genders | 325 | 92.7 | 809 | 43.2 | 2.15* (1.86, 2.47) | 106 | 33.0 | 228 | 14.2 | 2.32* (1.80, 2.98) | 0.36 (0.28, 0.45) | 0.64 | 0.33 (0.28, 0.39) | 0.67 |
| Men | 168 | 105.4 | 455 | 47.2 | 2.23* (1.81, 2.73) | 55 | 35.4 | 132 | 16.7 | 2.12* (1.46, 3.03) | 0.34 (0.24, 0.48) | 0.66 | 0.36 (0.29, 0.45) | 0.64 |
| Women | 157 | 83.9 | 354 | 39.1 | 2.14* (1.75, 2.61) | 51 | 30.4 | 96 | 11.8 | 2.58* (1.77, 3.69) | 0.36 (0.26, 0.50) | 0.64 | 0.30 (0.24, 0.38) | 0.70 |
| Southern Plains | ||||||||||||||
| Both genders | 833 | 69.0 | 8312 | 45.8 | 1.51* (1.40, 1.62) | 350 | 30.4 | 3180 | 17.4 | 1.75* (1.55, 1.96) | 0.44 (0.39, 0.50) | 0.56 | 0.38 (0.36, 0.40) | 0.62 |
| Men | 410 | 75.7 | 4340 | 53.5 | 1.42* (1.26, 1.58) | 180 | 35.1 | 1715 | 21.6 | 1.62* (1.36, 1.92) | 0.47 (0.38, 0.57) | 0.53 | 0.40 (0.38, 0.43) | 0.60 |
| Women | 423 | 63.8 | 3972 | 39.5 | 1.61* (1.45, 1.79) | 170 | 26.8 | 1465 | 14.0 | 1.91* (1.61, 2.24) | 0.42 (0.35, 0.51) | 0.58 | 0.35 (0.33, 0.38) | 0.65 |
| Pacific Coast | ||||||||||||||
| Both genders | 482 | 48.6 | 36 949 | 42.8 | 1.14* (1.03, 1.25) | 193 | 21.9 | 13 718 | 15.6 | 1.40* (1.19, 1.63) | 0.45 (0.37, 0.54) | 0.55 | 0.37 (0.36, 0.37) | 0.63 |
| Men | 252 | 53.5 | 19 028 | 48.6 | 1.10 (0.95, 1.27) | 100 | 26.9 | 6985 | 18.1 | 1.48* (1.16, 1.85) | 0.50 (0.38, 0.66) | 0.50 | 0.37 (0.36, 0.38) | 0.63 |
| Women | 230 | 44.3 | 17 921 | 37.7 | 1.17* (1.02, 1.35) | 93 | 18.7 | 6733 | 13.6 | 1.38* (1.10, 1.71) | 0.43 (0.33, 0.55) | 0.57 | 0.36 (0.35, 0.37) | 0.64 |
| East | ||||||||||||||
| Both genders | 149 | 36.4 | 40 734 | 45.4 | 0.80* (0.67, 0.95) | 62 | 17.7 | 14 322 | 15.6 | 1.13 (0.85, 1.47) | 0.48 (0.35, 0.67) | 0.52 | 0.34 (0.34, 0.35) | 0.66 |
| Men | 75 | 38.5 | 20 713 | 52.8 | 0.73* (0.56, 0.93) | 27 | 16.9 | 7173 | 18.6 | 0.90 (0.56, 1.36) | 0.45 (0.26, 0.73) | 0.55 | 0.35 (0.34, 0.36) | 0.65 |
| Women | 74 | 33.7 | 20 021 | 39.5 | 0.85 (0.66, 1.08) | 35 | 18.0 | 7149 | 13.3 | 1.35 (0.93, 1.90) | 0.52 (0.33, 0.80) | 0.48 | 0.33 (0.32, 0.34) | 0.67 |
| Southwest | ||||||||||||||
| Both genders | 520 | 31.0 | 16 879 | 39.1 | 0.79* (0.72, 0.87) | 184 | 12.1 | 6676 | 15.5 | 0.78* (0.67, 0.91) | 0.39 (0.33, 0.47) | 0.61 | 0.40 (0.38, 0.41) | 0.60 |
| Men | 266 | 34.9 | 8979 | 44.5 | 0.78* (0.68, 0.89) | 88 | 12.9 | 3550 | 18.1 | 0.71* (0.56, 0.89) | 0.37 (0.28, 0.48) | 0.63 | 0.41 (0.39, 0.42) | 0.59 |
| Women | 254 | 27.8 | 7900 | 34.3 | 0.81* (0.71, 0.92) | 96 | 11.5 | 3126 | 13.2 | 0.87 (0.69, 1.06) | 0.42 (0.32, (0.53) | 0.58 | 0.39 (0.37, 0.40) | 0.61 |
| All regions | ||||||||||||||
| Both genders | 2819 | 52.5 | 123 632 | 43.4 | 1.21* (1.16, 1.26) | 1091 | 22.0 | 45 908 | 15.8 | 1.39* (1.31, 1.49) | 0.42 (0.39, 0.58) | 0.58 | 0.36 (0.36, 0.37) | 0.64 |
| Men | 1446 | 58.8 | 63 639 | 49.7 | 1.18* (1.12, 1.25) | 560 | 25.3 | 23 424 | 18.6 | 1.37* (1.24, 1.50) | 0.43 (0.39, 0.48) | 0.57 | 0.37 (0.37, 0.38) | 0.63 |
| Women | 1373 | 47.2 | 59 993 | 38.1 | 1.24* (1.17, 1.31) | 531 | 19.4 | 22 484 | 13.5 | 1.44* (1.31, 1.57) | 0.41 (0.37, 0.46) | 0.59 | 0.35 (0.35, 0.36) | 0.65 |
| All counties | ||||||||||||||
| Northern Plains | ||||||||||||||
| Both genders | 661 | 54.4 | 103 728 | 47.5 | 1.15* (1.05, 1.25) | 266 | 22.7 | 38 424 | 16.8 | 1.35* (1.17, 1.54) | ||||
| Men | 358 | 64.3 | 52 385 | 54.7 | 1.18* (1.03, 1.33) | 143 | 28.1 | 19 177 | 20.0 | 1.40* (1.14, 1.70) | ||||
| Women | 303 | 46.6 | 51 343 | 41.6 | 1.12 (0.99, 1.26) | 123 | 18.9 | 19 247 | 14.3 | 1.32* (1.08, 1.59) | ||||
| Alaska | ||||||||||||||
| Both genders | 325 | 97.2 | 809 | 43.2 | 2.15* (1.86, 2.47) | 106 | 33.0 | 228 | 14.2 | 2.32* (1.80, 2.98) | ||||
| Men | 168 | 105.4 | 455 | 47.2 | 2.23 * (1.81, 2.73) | 55 | 35.4 | 132 | 16.7 | 2.12* (1.46, 3.03) | ||||
| Women | 157 | 83.9 | 354 | 39.1 | 2.14 * (1.75, 2.61) | 51 | 30.4 | 96 | 11.8 | 2.58* (1.77, 3.69) | ||||
| Southern Plains | ||||||||||||||
| Both genders | 936 | 57.7 | 43 513 | 44.4 | 1.30* (1.21, 1.39) | 418 | 27.4 | 16 154 | 16.4 | 1.67* (1.50, 1.85) | ||||
| Men | 463 | 62.2 | 23 115 | 52.5 | 1.18* (1.07, 1.31) | 215 | 31.2 | 8580 | 20.1 | 1.55* (1.33, 1.81) | ||||
| Women | 473 | 53.8 | 20 398 | 37.7 | 1.43* (1.30, 1.57) | 203 | 24.5 | 7574 | 13.5 | 1.81* (1.56, 2.09) | ||||
| Pacific Coast | ||||||||||||||
| Both genders | 609 | 41.3 | 70 203 | 43.7 | 0.95 (0.87, 1.03) | 262 | 19.9 | 25 700 | 15.7 | 1.27* (1.11, 1.45) | ||||
| Men | 320 | 46.3 | 36 080 | 49.8 | 0.93 (0.82, 1.05) | 140 | 25.1 | 12 943 | 18.2 | 1.38* (1.13, 1.66) | ||||
| Women | 289 | 37.2 | 34 123 | 38.5 | 0.97 (0.85, 1.09) | 122 | 16.5 | 12 757 | 13.7 | 1.21 (0.99, 1.46) | ||||
| East | ||||||||||||||
| Both genders | 524 | 22.2 | 320 138 | 46.5 | 0.48* (0.43, 0.52) | 239 | 11.0 | 117 497 | 16.8 | 0.65* (0.57, 0.75) | ||||
| Men | 267 | 24.6 | 163 364 | 54.0 | 0.46 * (0.40, 0.52) | 124 | 12.2 | 59 506 | 20.2 | 0.61* (0.49, 0.74) | ||||
| Women | 257 | 20.2 | 156 774 | 40.4 | 0.50* (0.44, 0.57) | 115 | 7.9 | 57 991 | 14.2 | 0.69 (0.56, 0.83) | ||||
| Southwest | ||||||||||||||
| Both genders | 549 | 30.2 | 26 530 | 38.7 | 0.78* (0.71, 0.85) | 203 | 12.5 | 10 225 | 15.0 | 0.83* (0.71, 0.96) | ||||
| Men | 280 | 33.6 | 13 992 | 44.2 | 0.76* (0.67, 0.86) | 96 | 13.0 | 5366 | 17.6 | 0.74* (0.58, 0.92) | ||||
| Women | 269 | 27.2 | 12 538 | 34.0 | 0.80* (0.70, 0.91) | 107 | 12.0 | 4859 | 12.9 | 0.93 (0.75, 1.13) | ||||
| All regions | ||||||||||||||
| Both genders | 3604 | 41.0 | 564 921 | 45.7 | 0.90* (0.87, 0.93) | 1494 | 18.4 | 208 228 | 16.5 | 1.11* (1.05, 1.18) | ||||
| Men | 1856 | 45.8 | 289 391 | 52.9 | 0.87* (0.82, 0.91) | 773 | 21.3 | 105 704 | 19.7 | 1.08 (1.00, 1.17) | ||||
| Women | 1748 | 36.9 | 275 530 | 39.8 | 0.93* (0.88, 0.97) | 721 | 16.2 | 102 524 | 14.0 | 1.16* (1.07, 1.25) | ||||
Note. AI/AN = American Indian/Alaska Native; CHSDA = Contract Health Service Delivery Area; CI = confidence interval; IHS = Indian Health Service; M/I = mortality/incidence rate ratio; RR = rate ratio. Analyses are limited to persons of non-Hispanic origin. AI/AN race for incidence data are reported by National Program of Cancer Registries and Surveillance, Epidemiology, and End Results Registries or through linkage with the IHS patient registration database; AI/AN race for deaths is reported from death certificates or through linkage with the IHS patient registration database. Rates are per 100 000 persons and are age-adjusted to the 2000 US standard population (19 age groups; Census P25-1130). RRs are calculated in SEER*Stat before rounding of rates and may not equal RRs calculated from rates presented in table. IHS regions are defined as follows: Alaskaa; Northern Plains (IL, IN,a IA,a MI,a MN,a MT,a NE,a ND,a SD,a WI,a WYa); Southern Plains (OK,a KS,a TXa); Southwest (AZ,a CO,a NV,a NM,a UTa); Pacific Coast (CA,a ID,a OR,a WA,a HI); East (AL,a AR, CT,a DE, FL,a GA, KY, LA,a ME,a MD, MA,a MS,a MO, NH, NJ, NY,a NC,a OH, PA,a RI,a SC,a TN, VT, VA, WV, DC). Percentage regional coverage of AI/AN persons in CHSDA counties to AI/AN persons in all counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; East = 18.2%; total US = 64.2%.
Source. Mortality data are from the AI/AN Mortality Database (AMD 1990–2009). Incidence data are from population-based cancer registries that participate in the National Program of Cancer Registries or the Surveillance, Epidemiology, and End Results Registries (43 states): AK, AL, AZ, CA, CO, CT, DE, FL, GA, HI, IA, ID, IL, IN, KS, KY, LA, MA, MD, ME, MI, MN, MO, MT, ND, NE, NH, NJ, NM, NV, NY, OH, OK, OR, PA, RI, SC, TX, UT, VT, WA, WV, WY; 1999–2008: WI; 1999–2001 and 2003–2009: DC; 2001–2009: AR, NC, SD; 2002–2009: VA; 2003–2009: MS, TN.
Identifies states with at least 1 county designated as CHSDA.
*P < .05.
Statistical Methods
All rates, expressed per 100 000 population, were directly age-adjusted, using SEER*Stat software, to the 2000 US standard population and should not be compared with published incidence and death rates adjusted using a different standard.
Using age-adjusted incidence and death rates, we calculated standardized rate ratios (RRs) for AI/AN persons compared with Whites. We calculated RRs by SEER*Stat to the fourth decimal place and rounded the RRs for presentation. We calculated confidence intervals (CIs) for age-adjusted rates and RRs using SEER*Stat 8.0.2 based on the methods described by Tiwari et al.26 Temporal changes in annual age-adjusted incidence and death rates, including the annual percent change (APC) for each interval, were assessed with joinpoint regression techniques using statistical software developed by the NCI.27 Statistical significance was set at a P value of less than .05.
We evaluated CRC mortality trends for 1990 to 2009 and reported them as the APC of the age-adjusted rates. If a joinpoint (change in trend) was identified during this period, the average annual percent change (AAPC) for the 10-year period 2000 to 2009 was reported. If no joinpoint was identified, the 20-year APC and the 10-year AAPC would be the same. Subtracting the mortality/incidence ratio from 1 approximated the probability of 5-year survival, and was shown to be reliable for use with CRC rates.28
RESULTS
From 2005 to 2009, 3604 AI/AN persons were diagnosed with CRC; of these, 2819 (78.2%) resided in CHSDA counties (Table 1). During the same period, 1494 AI/AN persons died from CRC; 1091 (73.0%) were CHSDA residents.
The all-counties CRC incidence rate was 10% lower (P < .05) among AI/AN individuals compared with Whites; the death rate was 11% higher (P < .05). For CHSDA counties only, the CRC incidence rate was 21% higher (P < .05) among AI/AN individuals, and the death rate 39% higher, with similar elevations for both men and women. The remainder of the results referred to CHSDA counties only.
AI/AN colorectal cancer incidence varied regionally (Table 1). The rate among AI/AN populations was significantly higher (P < .05) than for Whites in 4 regions (Northern Plains, Alaska, Southern Plains, and Pacific Coast), and significantly lower (P < .05) in 2 regions (East and Southwest). This pattern was seen among both men and women, although it was not always statistically significant. Regional CRC incidence rates for both genders combined varied by 199% among AI/AN populations (31.0 in the Southwest to 92.7 in Alaska), but only by 17% among Whites.
CRC death rates also showed significant regional differences. The risk of dying from CRC was elevated (P < .05) among AI/AN persons in the same 4 regions with elevated incidence (Northern Plains, Alaska, Southern Plains, and Pacific Coast; Table 1). In the other 2 regions AI/AN death RRs were either not statistically significant (East) or lower by a similar magnitude as for incidence (Southwest). Regional CRC death rates for both genders combined varied by 173% among AI/AN persons (12.1 in the Southwest to 33.0 in Alaska) and by only 23% among White CHSDA residents.
The mortality/incidence RR for CHSDA residents as a whole was 0.42 (95% = CI 0.39, 0.58) for AI/AN individuals compared with 0.36 (95% CI = 0.36, 0.37) for Whites; this difference was similar for men and women. The mortality/incidence RR was higher for AI/AN individuals than Whites in each region, except the Southwest. The East, which had a significantly lower CRC incidence rate for AI/AN persons, had the highest mortality/incidence RR among AI/AN persons, and showed the most within region difference from Whites.
Age at Diagnosis
When data from all regions were combined, AI/AN individuals had an increased risk of CRC diagnosis compared with Whites in all age strata. This risk was 45% higher for men and women younger than 50 years, 32% higher among those aged 50 to 64 years, and 13% higher among those aged 65 years or older (all P < 0.05) (Table 2).
TABLE 2—
Colorectal Cancer Incidence by Indian Health Service Region and Age at Diagnosis for American Indian/Alaska Native and White Persons: CHSDA Counties, United States, 2005–2009
| AI/AN | White | ||||
| IHS Region/Age at Diagnosis | Cases, No. (%) | Rate | Cases, No. (%) | Rate | AI/AN:White RR (95% CI) |
| Northern Plains | |||||
| < 50 y | 79 (15.49) | 9.6 | 1514 (7.59) | 5.9 | 1.64* (1.29, 2.05) |
| 50–64 y | 192 (37.65) | 113.2 | 5007 (25.10) | 65.9 | 1.72* (1.48, 1.98) |
| ≥ 65 y | 239 (46.86) | 343 | 13 428 (67.31) | 236.2 | 1.45* (1.26, 1.66) |
| All ages | 510 (100.00) | 67.3 | 19 949 (100.00) | 44.0 | 1.53* (1.39, 1.68) |
| Alaska | |||||
| < 50 y | 54 (16.62) | 15.4 | 109 (13.47) | 6.1 | 2.53* (1.79, 3.54) |
| 50–64 y | 118 (36.31) | 159.2 | 309 (38.20) | 63.2 | 2.52* (2.02, 3.13) |
| ≥ 65 y | 153 (47.08) | 456.5 | 391 (48.33) | 232.0 | 1.97* (1.61, 2.39) |
| All ages | 325 (100.00) | 92.7 | 809 (100.00) | 43.2 | 2.15* (1.86, 2.47) |
| Southern Plains | |||||
| < 50 y | 137 (16.45) | 12.8 | 713 (8.58) | 7.3 | 1.74* (1.44, 2.10) |
| 50–64 y | 274 (32.89) | 110.9 | 2229 (26.82) | 74.3 | 1.49* (1.31, 1.69) |
| ≥ 65 y | 422 (50.66) | 341.4 | 5370 (64.61) | 232.3 | 1.47* (1.32, 1.63) |
| All ages | 833 (100.00) | 69.0 | 8312 (100.00) | 45.8 | 1.51* (1.40, 1.62) |
| Pacific Coast | |||||
| < 50 y | 66 (13.69) | 6.9 | 2942 (7.96) | 6.1 | 1.13 (0.87, 1.44) |
| 50–64 y | 166 (34.44) | 70.9 | 9737 (26.35) | 64.5 | 1.10 (0.94, 1.28) |
| ≥ 65 y | 250 (51.87) | 261.2 | 24 270 (65.69) | 226.8 | 1.15* (1.01, 1.31) |
| All ages | 482 (100.00) | 48.6 | 36 949 (100.00) | 42.8 | 1.14* (1.03, 1.25) |
| East | |||||
| < 50 y | 20 (13.42) | 5.4 | 3431 (8.42) | 7.0 | 0.76 (0.46, 1.18) |
| 50–64 y | 56 (37.58) | 64.2 | 10 469 (25.70) | 72.3 | 0.89 (0.67, 1.15) |
| ≥ 65 y | 73 (48.99) | 181.5 | 26 834 (65.88) | 233.5 | 0.78* (0.60, 0.99) |
| All ages | 149 (100.00) | 36.4 | 40 734 (100.00) | 45.4 | 0.80* (0.67, 0.95) |
| Southwest | |||||
| < 50 y | 121 (23.27) | 7.6 | 1275 (7.55) | 5.7 | 1.34* (1.10, 1.61) |
| 50–64 y | 194 (37.31) | 60.9 | 4346 (25.75) | 59.9 | 1.02 (0.88, 1.17) |
| ≥ 65 y | 205 (39.42) | 129.8 | 11 258 (66.70) | 205.5 | 0.63* (0.55, 0.73) |
| All ages | 520 (100.00) | 31.0 | 16 879 (100.00) | 39.1 | 0.79* (0.72, 0.87) |
| All regions | |||||
| < 50 y | 477 (16.92) | 9.3 | 9984 (8.08) | 6.4 | 1.45* (1.32, 1.59) |
| 50–64 y | 1000 (35.47) | 88.4 | 32 097 (25.96) | 67.0 | 1.32* (1.24, 1.41) |
| ≥ 65 y | 1342 (47.61) | 257.8 | 81 551 (65.96) | 227.5 | 1.13* (1.07, 1.20) |
| All ages | 2819 (100.00) | 52.5 | 123 632 (100.00) | 43.4 | 1.21* (1.16, 1.26) |
Note. AI/AN = American Indian/Alaska Native; CHSDA = Contract Health Service Delivery Area; CI = confidence interval; IHS = Indian Health Service; RR = rate ratio. Analyses are limited to persons of non-Hispanic origin. AI/AN race is reported by National Program of Cancer Registries and Surveillance, Epidemiology, and End Results Registries or through linkage with the IHS patient registration database. Rates are per 100 000 persons and are age-adjusted to the 2000 US standard population (19 age groups; Census P25-1130). Rate ratios are calculated in SEER*Stat before rounding of rates and may not equal RRs calculated from rates presented in table. IHS regions are defined as follows: Alaskaa; Northern Plains (IL, IN,a IA,a MI,a MN,a MT,a NE,a ND,a SD,a WI,a WYa); Southern Plains (OK,a KS,a TXa); Southwest (AZ,a CO,a NV,a NM,a UTa); Pacific Coast (CA,a ID,a OR,a WA,a HI); East (AL,a AR, CT,a DE, FL,a GA, KY, LA,a ME,a MD, MA,a MS,a MO, NH, NJ, NY,a NC,a OH, PA,a RI,a SC,a TN, VT, VA, WV, DC). Percentage regional coverage of AI/AN persons in CHSDA counties to AI/AN persons in all counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; East = 18.2%; total US = 64.2%.
Source: Incidence data are from population-based cancer registries that participate in the National Program of Cancer Registries or the Surveillance, Epidemiology, and End Results Registries (43 states): AK, AL, AZ, CA, CO, CT, DE, FL, GA, HI, IA, ID, IL, IN, KS, KY, LA, MA, MD, ME, MI, MN, MO, MT, ND, NE, NH, NJ, NM, NV, NY, OH, OK, OR, PA, RI, SC, TX, UT, VT, WA, WV, WY; 1999–2008: WI; 1999–2001 and 2003–2009: DC; 2001–2009: AR, NC, SD; 2002–2009: VA; 2003–2009: MS, TN.
Identifies states with at least 1 county designated as CHSDA.
*P < .05.
By region, AI/AN persons in the Northern Plains, Alaska, and the Southern Plains had increased incidence of CRC among all age groups. In the Pacific Coast, there was a significant increased risk among AI/AN persons aged 65 years and older, and nonsignificant increases in other age groups. In the East, there was significantly lower incidence among AI/AN persons aged 65 years and older compared with Whites and a nonsignificant decreased risk in the other age groups, the largest difference being for persons younger than 50 years. In the Southwest, there was a 37% lower incidence of CRC among AI/AN persons aged 65 years and older, whereas AI/AN persons younger than 50 years had a 34% higher incidence compared with Whites.
Stage at Diagnosis
The age-adjusted rate of early stage CRC was 9% higher among AI/AN individuals compared with Whites for both genders combined, whereas the rate of late-stage CRC was 25% higher (Table 3). In the Northern Plains, Alaska, and Southern Plains, the rate of both early- and late-stage CRC were consistently elevated among AI/AN individuals, although the increase in risk was larger for late-stage disease. This was reflected in higher late-to early stage RRs among AI/AN individuals compared with Whites in these regions.
TABLE 3—
Colorectal Cancer Incidence by Indian Health Service Region, Stage at Diagnosis, and Gender for American Indian/Alaska Native and White Persons: CHSDA Counties, United States, 2005–2009
| AI/AN | White | |||||||
| IHS Region/Gender | Stage | Cases, No. (%) | Rate | Late/Early Stage RR (95% CI) | Cases, No. (%) | Rate | Late/Early Stage RR (95% CI) | AI/AN:White RRa |
| Northern Plains | ||||||||
| Both genders | Early | 175 (37.80) | 23.9 | 7638 (44.66) | 16.9 | 1.41 | ||
| Late | 288 (62.20) | 36.4 | 1.52* (1.23, 1.88) | 9465 (55.34) | 21.0 | 1.25* (1.21, 1.28) | 1.73 | |
| Men | Early | 91 (36.11) | 27.3 | 3954 (45.40) | 19.4 | 1.41 | ||
| Late | 161 (63.89) | 43.3 | 1.59* (1.18, 2.15) | 4755 (54.60) | 23.2 | 1.20* (1.15, 1.25) | 1.87 | |
| Women | Early | 84 (39.81) | 21.1 | 3684 (43.89) | 14.7 | 1.44 | ||
| Late | 127 (60.19) | 30.3 | 1.44* (1.06, 1.95) | 4710 (56.11) | 19.1 | 1.30* (1.24, 1.36) | 1.59 | |
| Alaska | ||||||||
| Both genders | Early | 115 (37.10) | 32.3 | 329 (45.63) | 18.0 | 1.79 | ||
| Late | 195 (62.90) | 55.8 | 1.73* (1.35, 2.23) | 392 (54.37) | 20.0 | 1.11 (0.95, 1.31) | 2.79 | |
| Men | Early | 64 (40.25) | 39.4 | 173 (42.30) | 18.0 | 2.19 | ||
| Late | 95 (59.75) | 61.0 | 1.55* (1.08, 2.24) | 236 (57.70) | 23.8 | 1.32* (1.05, 1.67) | 2.56 | |
| Women | Early | 51 (33.77) | 26.5 | 156 (50.00) | 18.0 | 1.47 | ||
| Late | 100 (66.23) | 53.5 | 2.02* (1.41, 2.92) | 156 (50.00) | 16.3 | 0.91 (0.71, 1.15) | 3.28 | |
| Southern Plains | ||||||||
| Both genders | Early | 289 (40.36) | 24.4 | 3259 (43.95) | 17.9 | 1.36 | ||
| Late | 427 (59.64) | 34.7 | 1.42* (1.21, 1.67) | 4157 (56.05) | 23.0 | 1.28* (1.22, 1.34) | 1.51 | |
| Men | Early | 129 (37.61) | 24.7 | 1704 (43.96) | 20.9 | 1.18 | ||
| Late | 214 (62.39) | 38.3 | 1.55* (1.22, 1.99) | 2172 (56.04) | 26.6 | 1.27* (1.19, 1.36) | 1.44 | |
| Women | Early | 160 (42.90) | 24.1 | 1555 (43.93) | 15.4 | 1.56 | ||
| Late | 213 (57.10) | 32.0 | 1.33* (1.07, 1.65) | 1985 (56.07) | 20.0 | 1.29* (1.21, 1.38) | 1.60 | |
| Pacific Coast | ||||||||
| Both Genders | Early | 162 (35.37) | 16.7 | 14 411 (41.38) | 16.7 | 1.00 | ||
| Late | 296 (64.63) | 28.7 | 1.72* (1.39, 2.13) | 20 415 (58.62) | 23.7 | 1.42* (1.39, 1.45) | 1.21 | |
| Men | Early | 88 (36.67) | 18.9 | 7562 (41.95) | 19.3 | 0.98 | ||
| Late | 152 (63.33) | 30.0 | 1.58* (1.17, 2.15) | 10 464 (58.05) | 26.6 | 1.38* (1.34, 1.43) | 1.13 | |
| Women | Early | 74 (33.94) | 14.6 | 6849 (40.77) | 14.5 | 1.01 | ||
| Late | 144 (66.06) | 27.3 | 1.87* (1.39, 2.55) | 9951 (59.23) | 21.1 | 1.46* (1.41, 1.51) | 1.29 | |
| East | ||||||||
| Both genders | Early | 63 (45.32) | 14.3 | 17 039 (45.14) | 19.0 | 0.75 | ||
| Late | 76 (54.68) | 18.9 | 1.31 (0.91, 1.91) | 20 707 (54.86) | 23.2 | 1.22* (1.20, 1.25) | 0.81 | |
| Men | Early | 39 (57.35) | 18.0 | 8848 (45.83) | 22.4 | 0.80 | ||
| Late | 29 (42.65) | 15.2 | 0.84 (0.47, 1.45) | 10 459 (54.17) | 26.6 | 1.19* (1.16, 1.22) | 0.57 | |
| Women | Early | 24 (33.80) | 10.5 | 8191 (44.42) | 16.3 | 0.64 | ||
| Late | 47 (66.20) | 21.6 | 2.06* (1.21, 3.62) | 10 248 (55.58) | 20.4 | 1.26* (1.22, 1.30) | 1.06 | |
| Southwest | ||||||||
| Both genders | Early | 194 (42.73) | 11.8 | 6546 (43.96) | 15.1 | 0.78 | ||
| Late | 260 (57.27) | 15.1 | 1.28* (1.05, 1.56) | 8346 (56.04) | 19.4 | 1.29* (1.24, 1.33) | 0.78 | |
| Men | Early | 107 (45.15) | 14.8 | 3510 (44.48) | 17.2 | 0.86 | ||
| Late | 130 (54.85) | 16.0 | 1.08 (0.82, 1.44) | 4382 (55.52) | 21.7 | 1.26* (1.20, 1.32) | 0.74 | |
| Women | Early | 87 (40.09) | 9.5 | 3036 (43.37) | 13.1 | 0.73 | ||
| Late | 130 (59.91) | 14.1 | 1.49* (1.12, 1.99) | 3964 (56.63) | 17.3 | 1.32* (1.26, 1.38) | 0.82 | |
| All regions | ||||||||
| Both genders | Early | 998 (39.29) | 18.8 | 49 222 (43.67) | 17.3 | 1.09 | ||
| Late | 1542 (60.71) | 28.1 | 1.49* (1.37, 1.62) | 63 482 (56.33) | 22.4 | 1.30* (1.28, 1.31) | 1.25 | |
| Men | Early | 518 (39.88) | 21.6 | 25 751 (44.23) | 20.0 | 1.08 | ||
| Late | 781 (60.12) | 30.5 | 1.41* (1.25, 1.60) | 32 468 (55.77) | 25.3 | 1.26* (1.24, 1.28) | 1.21 | |
| Women | Early | 480 (38.68) | 16.5 | 23 471 (43.08) | 15.0 | 1.10 | ||
| Late | 761 (61.32) | 25.9 | 1.57* (1.39, 1.77) | 31 014 (56.92) | 19.9 | 1.33* (1.31, 1.35) | 1.30 | |
Note. AI/AN = American Indian/Alaska Native; CHSDA = Contract Health Service Delivery Area; CI = confidence interval; IHS = Indian Health Service; RR = rate ratio. Analyses are limited to persons of non-Hispanic origin. AI/AN race is reported by National Program of Cancer Registries and Surveillance, Epidemiology, and End Results registries or through linkage with the IHS patient registration database. Rates are per 100 000 persons and are age-adjusted to the 2000 US standard population (19 age groups; Census P25-1130). Rate ratios are calculated in SEER*Stat before rounding of rates and may not equal RRs calculated from rates presented in table. IHS regions are defined as follows: Alaskab; Northern Plains (IL, IN,b IA,b MI,b MN,b MT,b NE,b ND,b SD,b WI,b WYb); Southern Plains (OK,b KS,b TXb); Southwest (AZ,b CO,b NV,b NM,b UTb); Pacific Coast (CA,b ID,b OR,b WA,b HI); East (AL,b AR, CT,b DE, FL,b GA, KY, LA,b ME,b MD, MA,b MS,b MO, NH, NJ, NY,b NC,b OH, PA,b RI,b SC,b TN, VT, VA, WV, DC). Percentage regional coverage of AI/AN persons in CHSDA counties to AI/AN persons in all counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; East = 18.2%; total US = 64.2%.
Source. Incidence data are from population-based cancer registries that participate in the National Program of Cancer Registries or the Surveillance, Epidemiology, and End Results Registries (43 states): AK, AL, AZ, CA, CO, CT, DE, FL, GA, HI, IA, ID, IL, IN, KS, KY, LA, MA, MD, ME, MI, MN, MO, MT, ND, NE, NH, NJ, NM, NV, NY, OH, OK, OR, PA, RI, SC, TX, UT, VT, WA, WV, WY; 1999–2008: WI; 1999–2001 and 2003–2009: DC; 2001–2009: AR, NC, SD; 2002–2009: VA; 2003–2009: MS, TN.
RRs between rate for AI/AN persons and rate for White persons by stage.
Identifies states with at least 1 county designated as CHSDA.
*P < .05.
Colorectal Cancer Incidence Trends
CRC incidence trends were evaluated for 1999 to 2009 and reported as the APC in the age-adjusted rate (Table 4). The age-adjusted CRC incidence rate among Whites in CHSDA counties significantly decreased (P < .05) in every region from 1999 to 2009, falling 2.1% per year between 1999 and 2003, and accelerating to 3.7% per year between 2003 and 2009 for all regions combined.
TABLE 4—
Incidence Rate (1999–2009) and Death Rate (1990–2009) Trends for Colorectal Cancer With Joinpoint Analyses for American Indian/Alaska Native Persons Compared With Whites: CHSDA Counties, United States
| Trend 1 | Trend 2 | Trend 3 | Trend 4 | |||||
| IHS Region/Race | Years | APCa | Years | APCa | Years | APCa | Years | APCa |
| Incidence rate joinpoint analysisb | ||||||||
| Northern Plains | ||||||||
| Whitec | 1999–2003 | −1.8 | 2003–2009 | −4.4* | ||||
| AI/ANc,d | 1999–2009 | −1.8 | ||||||
| Alaska | ||||||||
| White | 1999–2009 | −3.4* | ||||||
| AI/AN | 1999–2009 | −3.1* | ||||||
| Southern Plains | ||||||||
| White | 1999–2001 | 0.2 | 2001–2009 | −2.6* | ||||
| AI/AN | 1999–2009 | 0.3 | ||||||
| Pacific Coast | ||||||||
| White | 1999–2009 | −2.4* | ||||||
| AI/AN | 1999–2009 | −1.9* | ||||||
| East | ||||||||
| White | 1999–2003 | −2.2* | 2003–2009 | −4.6* | ||||
| AI/AN | 1999–2009 | −1.6 | ||||||
| Southwest | ||||||||
| White | 1999–2002 | −0.9 | 2002–2009 | −3.6* | ||||
| AI/AN | 1999–2005 | 7.7* | 2005–2009 | −3.2 | ||||
| All regions | ||||||||
| White | 1999–2003 | −2.1* | 2003–2009 | −3.7* | ||||
| AI/AN | 1999–2009 | −0.7 | ||||||
| Death rate joinpoint analyses | ||||||||
| Northern Plains | ||||||||
| White | 1990–2000 | −2.0* | 2000–2009 | −2.9* | ||||
| AI/AN | 1990–2009 | −1.6* | ||||||
| Alaska | ||||||||
| White | 1990–2009 | −3.0* | ||||||
| AI/AN | 1990–2009 | −1.6 | ||||||
| Southern Plainsc | ||||||||
| White | 1997–2009 | −1.6* | ||||||
| AI/AN | 1997–2009 | 1.8 | ||||||
| Pacific Coast | ||||||||
| White | 1990–2001 | −1.5* | 2001–2009 | −2.6* | ||||
| AI/AN | 1990–2009 | 1.5* | ||||||
| East | ||||||||
| White | 1990–2000 | −1.8* | 2000–2009 | −3.8* | ||||
| AI/AN | 1990–2009 | 1.7 | ||||||
| Southwest | ||||||||
| White | 1990–2003 | −1.0* | 2003–2009 | −3.5* | ||||
| AI/AN | 1990–2009 | 1.3 | ||||||
| All regions | ||||||||
| White | 1990–1994 | −1.1* | 1994–1997 | −2.9* | 1997–2000 | −0.6 | 2000–2009 | −3.1* |
| AI/AN | 1990–2009 | 0.8 | ||||||
Note. AI/AN = American Indian/Alaska Native; APC = annual percent change; CHSDA = Contract Health Service Delivery Area; IHS = Indian Health Service. Analyses are limited to persons of non-Hispanic origin. AI/AN race for incidence data are reported by National Program of Cancer Registries and Surveillance, Epidemiology, and End Results registries or through linkage with the IHS patient registration database. AI/AN race for deaths is reported from death certificates or through linkage with the IHS patient registration database. IHS regions are defined as follows: Alaskad; Northern Plains (IL, IN,d IA,d MI,d MN,d MT,d NE,d ND,d SD,d WI,d WYd); Southern Plains (OK,d KS,d TXd); Southwest (AZ,d CO,d NV,d NM,d UTd); Pacific Coast (CA,d ID,d OR,d WA,d HI); East (AL,d AR, CT,d DE, FL,d GA, KY, LA,d ME,d MD, MA,d MS,d MO, NH, NJ, NY,d NC,d OH, PA,d RI,d SC,d TN, VT, VA, WV, DC). Percentage regional coverage of AI/AN persons in CHSDA counties to AI/AN persons in all counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; East = 18.2%; total US = 64.2%.
Source. Incidence data are from population-based cancer registries that participate in the National Program of Cancer Registries or the Surveillance, Epidemiology, and End Results Registries (43 states): AK, AL, AZ, CA, CO, CT, DE, FL, GA, HI, IA, ID, IL, IN, KS, KY, LA, MA, MD, ME, MI, MN, MO, MT, ND, NE, NH, NJ, NM, NV, NY, OH, OK, OR, PA, RI, SC, TX, UT, VT, WA, WV, WY; 1999–2008: WI; 1999–2001 and 2003–2009: DC; 2001–2009: AR, NC, SD; 2002–2009: VA; 2003–2009: MS, TN.
APC is based on rates that were age-adjusted to the 2000 US standard population (11 age groups; Census P25-1130).
Joinpoint analyses with up to 3 joinpoints that are based on rates per 100 000 persons and are age-adjusted to the 2000 US standard population (11 age groups; Census P25-1130).
Mortality trend is calculated only for 1997–2009.
Identifies states with at least 1 county designated as CHSDA.
*P < .05.
When all CHSDA counties were combined, there was no significant change in CRC incidence rate among AI/AN populations between 1999 and 2009. Only Alaska (3.1% per year) and the Pacific Coast (1.9% per year) had a significant decrease in AI/AN colorectal cancer incidence rate during this period. In the Southwest, CRC incidence rates among AI/AN populations significantly increased at 7.7% per year from 1999 to 2005, but had no significant change from 2005 to 2009.
Mortality Trends
The age-adjusted CRC death rate among Whites significantly (P < .05) decreased in every region from 1990 to 2009 (Table 4). In most regions, the decrease in death rates accelerated in the latest decade, with a combined decline of 3.1% per year between 2000 and 2009.
Conversely, CRC death rates among AI/AN persons showed no statistically significant change when regional data were combined. Only the Northern Plains region experienced a decline in death rate among AI/AN persons, falling 1.6% per year between 1990 and 2009, whereas the rate among White persons in this region fell at a rate of 2.0% per year between 1999 and 2000 and 2.9% between 2000 and 2009. The AI/AN colorectal cancer death rate increased in the Pacific Coast at a rate of 1.5% per year between 1990 and 2009. No significant death rate change was seen in the other regions during the analysis period.
DISCUSSION
The purpose of our study was to characterize estimates of CRC incidence and mortality in AI/AN persons by region compared with Whites using a linkage methodology to improve AI/AN classification in the incidence and mortality data. Restricting the study population to CHSDA counties unveiled significantly higher incidence and death rates among AI/AN persons compared with those for all US counties. The difference between the CHSDA and all counties rates was likely driven by higher rates of misclassification in the cancer registries and death records for AI/AN persons living in urban and other non-CHSDA areas.3
Our previous application of this method examined incidence from 1999 to 2004.5 In that analysis, the overall CHSDA CRC incidence was 9% lower among all AI/AN populations than Whites; however, the AI/AN rate varied approximately 5-fold regionally, from 21.0 in the Southwest to 102.6 in Alaska. Over the subsequent 5 years covered in this report, CRC incidence among AI/AN persons increased from 46.3 to 52.5, whereas it decreased among Whites from 50.8 to 43.4. Hence, although rates decreased steadily in Whites across regions, the incidence in AI/AN individuals fell in only Alaska and the Pacific Coast, albeit at a slower rate. Meanwhile, incidence did not significantly change in the other regions from 2005 to 2009.
Others reported a steady decline in the US CRC incidence rate, driven primarily by downward trends among Whites.29 The accelerated decline in recent years was primarily attributed to the efficacy of removing precancerous polyps during screening colonoscopy.30 Significant disparities existed between Whites and AI/ANs in the use of CRC screening, especially with endoscopic screening.31 Reasons for these disparities were multifactorial, but included a lack of endoscopic services at most IHS and tribal facilities, underfunded referral systems, and fecal occult blood testing (with either guaiac or fecal immunochemical methods) as the primary CRC screening modality employed by the majority of IHS and tribal facilities. Although effective at finding CRC before symptoms arise, fecal testing does not remove precancerous polyps, which can be removed during endoscopic screening.6 Data from the 2010 National Health Interview Survey reported 59.8% of Whites to be current with screening guidelines compared with 49.5% of AI/AN persons.9 The Government Performance Results Act requires IHS-funded facilities to submit CRC screening data. In 2010, 37% of AI/AN men and women served by the IHS were current with screening guidelines, although rates ranged from 24% in the IHS Phoenix area to 55% in the IHS Alaska area.32 Because screening rates significantly rose over the last decade, as has the use of endoscopic screening, more time might be needed to see an effect on incidence and mortality.32
Between 2005 and 2009, AI/AN persons in Alaska had a 115% greater CRC incidence rate and a 132% greater death rate than Whites. The Alaska Area program has been responding to this disparity with innovative programs designed to increase screening, including the deployment of itinerant colonoscopy teams who travel to regional health centers.33 The Northern Plains had the second highest CRC incidence and death rate, but was distinguished by being the only region with a significantly declining death rate. Innovative community-based programs such as Minnesota’s Intertribal Colorectal Cancer Council, which brings together tribal health champions to improve screening, and the Wisdom Steps program, which rewards elders for meeting preventative health measures, might be affecting this change.34,35
By comparison, between 2005 and 2009, the incidence of CRC among Southwest AI/AN persons was more than 21% lower than Whites. Despite lower CRC burden, the incidence of CRC among Southwest AI/AN persons increased at an alarming rate of 7.7% per year between 1999 and 2005, whereas mortality increased at 1.3% per year. Work is needed to identify the factors behind these concerning trends.
The reasons for the substantial interregional variation in AI/AN colorectal cancer incidence and mortality were unclear, but were likely multifactorial. Genetic differentiation might play a role in these diverse, often isolated communities.36 AI/AN populations also vary widely in their diets, environments, and access to care. Many Alaskan AI/AN persons maintain subsistence diets high in animal fats and low in fresh fruits and vegetables.37 The high cigarette smoking rate and high prevalence of vitamin D deficiency because of low dietary intake and low ultraviolet B exposure could also play a role.38,39 By comparison, AI/AN persons in the Southwest have lower cigarette smoking use,40 whereas year-round ultraviolet B exposure results in lower rates of vitamin D deficiency.38 Given the dramatic regional CRC differences among AI/AN populations, these populations might be ideally suited for further research into the influence of risk factors, such as diet, environment, genetics, and screening on CRC mortality. Such findings might have important implications for all populations.
Understanding the relationship between CRC incidence and age at diagnosis is critical for informing screening guidelines. The rationale for when to begin screening is based on the benefit of early stage diagnoses in terms of added life-years, attenuated by the risk of screening.6 In this study, the incidence rate of CRC cases occurring in AI/AN individuals younger than age 50 years ranged from 5.4 in the East to 15.4 in Alaska. By comparison, the rate among Whites ranged from 5.7 in the Southwest to 7.3 in the Southern Plains. Although the American College of Gastroenterology recommends CRC screening beginning at age 50 years in average-risk persons, it recommends that African Americans begin screening at age 45 years because they were shown to acquire a survival benefit from screening at a younger age.41 Given our data, modeling the risks and benefits of earlier age CRC screening in AI/AN individuals might be warranted.
Based on the mortality/incidence ratio, AI/ANs diagnosed with CRC had a lower 5-year survival probability than Whites in all IHS regions, with exception of the Southwest, where it was the same. A major predictor of CRC mortality odds was stage at diagnosis. Five-year survival was more than 90% for CRC diagnosed at an early, localized stage, but decreased precipitously to 70% with localized spread or lymph node involvement, and to 12% with metastatic disease.42 In our analysis, 61% of incident cases occurring in AI/AN persons were late stage versus 56% in Whites. Pacific Coast, East, and Alaska women had the highest proportion of late-stage CRC diagnosis (66% of cases in each region), whereas men in the Northern Plains were diagnosed at advanced stages 64% of the time. These proportions were from 7% to 11% higher than those seen in Whites, and likely represented inequities in CRC screening. Continued efforts to improve screening uptake among AI/AN populations are therefore needed.
Additional factors likely played a role in survival disparities. Proximity to a cancer center, the availability of resources to pay for care, patient comorbidities, and patient acceptance of treatment could all affect cancer outcomes.43,44 A better understanding of how these factors affected AI/AN colorectal cancer survival disparities is needed.
Our results must be considered in light of several limitations. Although we approximated survival probability, making inferences about the relationship between incidence and mortality based on 5 years of data was problematic. Incident cases might die from CRC after the catchment period, whereas mortality cases might have been diagnosed before catchment. Linking incidence and mortality so case–fatality ratios might be discerned would better characterize survival disparities.
It was also probable that our reported incidence and death rates for CRC in AI/AN populations were still underestimates. The IHS provides care to 2.2 million of the estimated 3.4 million AI/AN persons in the United States.45 Individuals who self-identified as AI/AN persons on census records, but did not have direct tribal ties, were from non-federally recognized tribes, lived long distances from IHS and tribal health facilities, were multiracial, were less likely to access the IHS.46 AI/AN residents of urban areas might also differ from all AI/AN persons in poverty level, health care access, and other factors that might influence mortality.47,48 Our approach could not correct racial misclassification in these cases. Furthermore, there was substantial variation between federally recognized tribes in the proportion of Native ancestry required for tribal membership, and therefore, for eligibility for IHS services. Whether and how this discrepancy in tribal membership requirements might influence some of our findings was unclear, although our findings were consistent with previous reports. Finally, although the exclusion of Hispanic AI/AN persons from the analyses reduced the overall count of deaths in AI/AN persons by less than 5%, it might disproportionately exclude some tribal members in some states.
This study found dramatic geographic variations in AI/AN colorectal cancer incidence and mortality compared with Whites. Future presentations of AI/AN cancer data should consider the effects of racial misclassification and regional variations might have on summary statistics. The higher prevalence of advanced disease at diagnosis and corresponding mortality disparities among AI/AN populations call for more attention to improve access to and utilization of CRC screening programs. An understanding of the factors driving these regional disparities could offer critical insights for prevention and control programs.
Human Participant Protection
Human participant protection was not required because no human participants were involved.
References
- 1.Centers for Disease Control and Prevention. Vital signs: colorectal cancer screening, incidence, and mortality—United States, 2002–2010. MMWR Morb Mortal Wkly Rep. 2011;60(26):884–889. [PubMed] [Google Scholar]
- 2. Lifetime Risk (Percent) of Being Diagnosed with Cancer by Site and Race/Ethnicity: Males, 18 SEER Areas, 2007-2009 (Table 1.15) and Females, 18 SEER Areas, 2007-2009 (Table 1.16). 2012. Available at: http://seer.cancer.gov/csr/1975_2009_pops09/results_merged/topic_lifetime_risk.pdf. Accessed January 17, 2014.
- 3.Arias E, Schauman WS, Eschbach K, Sorlie PD, Backlund E. The validity of race and Hispanic origin reporting on death certificates in the United States. Vital Health Stat 2. 2008;148:1–23. [PubMed] [Google Scholar]
- 4.Espey DK, Wiggins CL, Becker TM, Johnson C, Miller BA. Methods for improving cancer surveillance data in American Indian and Alaska Native populations. Cancer. 2008;113(5 suppl):1120–1130. doi: 10.1002/cncr.23724. [DOI] [PubMed] [Google Scholar]
- 5.Perdue DG, Perkins C, Jackson-Thompson J et al. Regional differences in colorectal cancer incidence, stage, and subsite among American Indians and Alaska Natives, 1999-2004. Cancer. 2008;113(5 suppl):1179–1190. doi: 10.1002/cncr.23726. [DOI] [PubMed] [Google Scholar]
- 6.US Preventive Services Task Force. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;149(9):627–637. doi: 10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- 7.Winawer SJ, Zauber AG, Ho MN et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329(27):1977–1981. doi: 10.1056/NEJM199312303292701. [DOI] [PubMed] [Google Scholar]
- 8.Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009;150(1):1–8. doi: 10.7326/0003-4819-150-1-200901060-00306. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Cancer screening. MMWR Morb Mortal Wkly Rep. 2012;61(3):41–45. [PubMed] [Google Scholar]
- 10.Espey DK, Jim MA, Richards T, Begay C, Haverkamp D, Roberts D. Methods for improving the quality and completeness of mortality data for American Indians and Alaska Natives. Am J Public Health. 2014;104(6 suppl 3):S286–S294. doi: 10.2105/AJPH.2013.301716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. US census populations with bridged race categories. Available at: http://www.cdc.gov/nchs/nvss/bridged_race.htm. Accessed March 13, 2013.
- 12.National Cancer Institute. Adjusted populations for the counties/parishes affected by Hurricanes Katrina and Rita. 2012. Available at: http://seer.cancer.gov/popdata/hurricane_adj.html. Accessed March 18, 2013.
- 13.Edwards BK, Noone AM, Mariotto AB et al. Annual Report to the Nation on the status of cancer, 1975–2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. 2013 doi: 10.1002/cncr.28509. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. National Vital Statistics System. Available at: http://www.cdc.gov/nchs/nvss.htm. Accessed May 2, 2012.
- 15a.Centers for Disease Control and Prevention. NCHS procedures for multiple-race and Hispanic origin data: collection, coding, editing, and transmitting. Available at: http://www.cdc.gov/nchs/data/dvs/Multiple_race_documentation_5-10-04.pdf. Access April 12, 2012.
- 15b.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980. [Google Scholar]
- 15c.International Classification of Diseases, 10th Revision. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 16.US Cancer Statistics Working Group. United States Cancer Statistics: 1999-2009 Incidence and Mortality Web-based Report. Department of Health and Human Services. Atlanta, GA: Centers for Disease Control and Prevention and National Cancer Institute; 2013. [Google Scholar]
- 17.Hankey BF, Ries LA, Edwards BK. The surveillance, epidemiology, and end results program: a national resource. Cancer Epidemiol Biomarkers Prev. 1999;8(12):1117–1121. [PubMed] [Google Scholar]
- 18.Fritz A, Percy C, Jack A. International Classification of Diseases of Oncology. Geneva, Switzerland: World Health Organization; 2000. [Google Scholar]
- 19.White MC, Espey DK, Swan J, Wiggins C, Eheman C, Kaur JS. Disparities in cancer mortality and incidence among American Indians and Alaska Natives in the United States. Am J Public Health. 2014;104(6 suppl 3):S377–S387. doi: 10.2105/AJPH.2013.301673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Young JL, Roffers SD, Ries LAG, Fritz AG, Hurlbut AA, editors. SEER Summary Staging Manual - 2000: Codes and Coding Instructions. Bethesda, MD: National Cancer Institute; 2001. [Google Scholar]
- 21.Arias E, Schauman WS, Eschbach K, Sorlie PD. The validity of race and Hispanic origin reporting on death certificates in the United States. Vital Health Stat 2. 2008;(148):1–23. [PubMed] [Google Scholar]
- 22.Denny CH, Taylor TL. American Indian and Alaska Native health behavior: findings from the Behavioral Risk Factor Surveillance System, 1992-1995. Ethn Dis. 1999;9(3):403–409. [PubMed] [Google Scholar]
- 23.Wiggins CL, Espey DK, Wingo PA et al. Cancer among American Indians and Alaska Natives in the United States, 1999-2004. Cancer. 2008;113(5 suppl):1142–1152. doi: 10.1002/cncr.23734. [DOI] [PubMed] [Google Scholar]
- 24.Espey D, Paisano R, Cobb N. Regional patterns and trends in cancer mortality among American Indians and Alaska Natives, 1990-2001. Cancer. 2005;103(5):1045–1053. doi: 10.1002/cncr.20876. [DOI] [PubMed] [Google Scholar]
- 25.US Department of Health and Human Services. Indian Health Service Areas. 2012. Available at: http://www.ihs.gov/index.cfm?module=AreaOffices. Accessed April 2, 2012.
- 26.Tiwari RC, Clegg LX, Zou Z. Efficient interval estimation for age-adjusted cancer rates. Stat Methods Med Res. 2006;15(6):547–569. doi: 10.1177/0962280206070621. [DOI] [PubMed] [Google Scholar]
- 27.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 28.Asadzadeh Vostakolaei F, Karim-Kos HE, Janssen-Heijnen ML, Visser O, Verbeek AL, Kiemeney LA. The validity of the mortality to incidence ratio as a proxy for site-specific cancer survival. Eur J Public Health. 2011;21(5):573–577. doi: 10.1093/eurpub/ckq120. [DOI] [PubMed] [Google Scholar]
- 29.Jemal A, Simard EP, Dorell C et al. Annual report to the nation on the status of cancer, 1975-2009, featuring the burden and trends in human papillomavirus (HPV)-associated cancers and HPV vaccination coverage levels. J Natl Cancer Inst. 2013;105(3):175–201. doi: 10.1093/jnci/djs491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Edwards BK, Ward E, Kohler BA et al. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010;116(3):544–573. doi: 10.1002/cncr.24760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Day LW, Espey DK, Madden E, Segal M, Terdiman JP. Screening prevalence and incidence of colorectal cancer among American Indian/Alaskan natives in the Indian Health Service. Dig Dis Sci. 2011;56(7):2104–2113. doi: 10.1007/s10620-010-1528-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Indian Health Service. Area summary report. Government Performance and Results Act (GPRA) 2012. Available at: http://www.ihs.gov/crs/documents/gpra/201012AreaReport.pdf. Accessed April 15, 2013.
- 33.Redwood D, Provost E, Perdue D, Haverkamp D, Espey D. The last frontier: innovative efforts to reduce colorectal cancer disparities among the remote Alaska Native population. Gastrointest Endosc. 2012;75:474–480. doi: 10.1016/j.gie.2011.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Minnesota Intertribal Colorectal Cancer Council. Colorectal cancer in Minnesota American Indians; an intertribal dialogue for action. Available at: http://preventcancer.org/files/education/digest-eleven.pdf. Accessed May 17, 2013.
- 35. Wisdom steps: preventative health for American Indian elders. Available at: http://www.wisdomsteps.org. Accessed May 17, 2013.
- 36.Wang S, Lewis CM, Jakobsson M et al. Genetic variation and population structure in Native Americans. PLoS Genet. 2007;3(11):e185. doi: 10.1371/journal.pgen.0030185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Johnson JS, Nobmann ED, Asay E, Lanier AP. Dietary intake of Alaska Native people in two regions and implications for health: the Alaska Native Dietary and Subsistence Food Assessment Project. Int J Circumpolar Health. 2009;68(2):109–122. doi: 10.3402/ijch.v68i2.18320. [DOI] [PubMed] [Google Scholar]
- 38.Redwood D, Lanier AP, Renner C, Smith J, Tom-Orme L, Slattery ML. Differences in cigarette and smokeless tobacco use among American Indian and Alaska Native people living in Alaska and the Southwest United States. Nicotine Tob Res. 2010;12(7):791–796. doi: 10.1093/ntr/ntq087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Frost JT, Hill L. Vitamin D deficiency in a nonrandom sample of southeast Alaska Natives. J Am Diet Assoc. 2008;108(9):1508–1511. doi: 10.1016/j.jada.2008.06.427. [DOI] [PubMed] [Google Scholar]
- 40.Steele CB, Cardinez CJ, Richardson LC, Tom-Orme L, Shaw KM. Surveillance for health behaviors of American Indians and Alaska Natives-findings from the Behavioral Risk Factor Surveillance System, 2000-2006. Cancer. 2008;113(5 suppl):1131–1141. doi: 10.1002/cncr.23727. [DOI] [PubMed] [Google Scholar]
- 41.Rex DK, Johnson DA, Anderson JC, Schoenfeld PS, Burke CA, Inadomi JM. American College of Gastroenterology guidelines for colorectal cancer screening 2009. Am J Gastroenterol. 2009;104(3):739–750. doi: 10.1038/ajg.2009.104. erratum 2009;104(6):1613. [DOI] [PubMed] [Google Scholar]
- 42.Howlader N, Noone AM, Krapcho M . SEER Cancer Statistics Review, 1975-2010. Bethesda, MD: National Cancer Institute; 2012. [Google Scholar]
- 43.Lamont EB, Hayreh D, Pickett KE et al. Is patient travel distance associated with survival on phase II clinical trials in oncology? J Natl Cancer Inst. 2003;95(18):1370–1375. doi: 10.1093/jnci/djg035. [DOI] [PubMed] [Google Scholar]
- 44.Lee W, Nelson R, Mailey B, Duldulao MP, Garcia-Aguilar J, Kim J. Socioeconomic factors impact colon cancer outcomes in diverse patient populations. J Gastrointest Surg. 2012;16(4):692–704. doi: 10.1007/s11605-011-1809-y. [DOI] [PubMed] [Google Scholar]
- 45. Indian Health Service A Quick Look. Available at: http://www.ihs.gov/newsroom/includes/themes/newihstheme/display_objects/documents/factsheets/QuickLook.pdf. Accessed January 17, 2014.
- 46.Cunningham PJ. Access to care in the Indian Health Service. Health Aff (Millwood) 1993;12:224–233. doi: 10.1377/hlthaff.12.3.224. [DOI] [PubMed] [Google Scholar]
- 47.Urban Indian Health Institute, Seattle Indian Health Board. Reported Health and Health-influencing behaviors among Urban American Indians and Alaska Natives: An Analysis of Data Collected by the Behavioral Risk Factor Surveillance System. 2008. Available at: http://www.uihi.org/wp-content/uploads/2009/01/health_health-influencing_behaviors_among_urban_indiansupdate-121020081.pdf. Accessed January 17, 2014.
- 48.Invisible Tribes: Urban Indians and Their Health in a Changing World. Seattle, WA: Urban Indian Health Commission; 2007. [Google Scholar]