Abstract
Objectives. We analyzed cervical cancer incidence and mortality data in American Indian and Alaska Native (AI/AN) women compared with women of other races.
Methods. We improved identification of AI/AN race, cervical cancer incidence, and mortality data using Indian Health Service (IHS) patient records; our analyses focused on residents of IHS Contract Health Service Delivery Area (CHSDA) counties. Age-adjusted incidence and death rates were calculated for AI/AN and White women from 1999 to 2009.
Results. AI/AN women in CHSDA counties had a death rate from cervical cancer of 4.2, which was nearly twice the rate in White women (2.0; rate ratio [RR] = 2.11). AI/AN women also had higher incidence rates of cervical cancer compared with White women (11.0 vs 7.1; RR = 1.55) and were more often diagnosed with later-stage disease (RR = 1.84 for regional stage and RR = 1.74 for distant stage). Death rates decreased for AI/AN women from 1990 to 1993 (−25.8%/year) and remained stable thereafter.
Conclusions. Although rates decreased over time, AI/AN women had disproportionately higher cervical cancer incidence and mortality. The persistently higher rates among AI/AN women compared with White women require continued improvements in identifying and treating cervical cancer and precancerous lesions.
Cervical cancer is the third most common cancer for women, and the fourth most common cause of cancer deaths globally.1 In the United States, cervical cancer is less common because of availability of screening and follow-up treatment, with about 12 000 cases diagnosed and 4000 deaths from the disease annually.2 Cervical cancer screening has resulted in well-documented declines in cervical cancer incidence and mortality, but women who do not receive recommended screening and follow-up are at increased risk for cervical cancer mortality.3
Previous studies have shown higher cervical cancer incidence and mortality among American Indian/Alaska Native (AI/AN) populations, compared with White populations.4–8 Because most cases of invasive cervical cancer are preventable through screening and follow-up, disparities in measures of cervical cancer among AI/AN women are generally attributed to decreased access and additional barriers (such as increased distance to get treatment or cultural differences).3 Programs addressing cervical cancer disparities by increasing screening among AI/AN populations have had positive results, although ongoing regional disparities have been documented.5,9
Observed disparities in incidence rates of cervical cancer between AI/AN and White populations increased after efforts were made to ensure that members of AI/AN populations were properly identified, which increased the number of AI/AN cases and corresponding rates.5 We described the mortality and incidence of cervical cancer among AI/AN women from 1999 to 2009, using techniques to minimize the effect of race misclassification in surveillance data, and to compare rates of cervical cancer among these women to rates among other women living in the same geographic region. Trends for mortality from 1990 to 2009 were also presented.
METHODS
Detailed methods for generating the analytical mortality files are described elsewhere in this supplement.10 Detailed methods describing incidence data and analysis are available in a previous publication.11 Abbreviated methods follow.
Data Sources
Population estimates.
We included bridged single-race population estimates developed by the US Census Bureau and the Centers for Disease Control and Prevention (CDC) National Center for Health Statistics (NCHS) that were adjusted for the population shifts because of Hurricanes Katrina and Rita in 2005 as denominators in the calculations of incidence and death rates.12,13 Bridged single-race data allowed for comparability between the pre- and post-2000 racial/ethnic population estimates during this study period.
Death data.
Death certificate data are compiled by each state. These data are sent to the NCHS, where they are edited for consistency, stripped of personal identifiers, and made available to the general public as part of the National Vital Statistics System (NVSS).14 NCHS applies a bridging algorithm nearly identical to the one used by the Census Bureau to assign a single race to decedents with multiple races reported on the death certificate.15
We linked the Indian Health Service (IHS) patient registration database to the National Death Index (NDI), a tool that allows researchers to link their data with the mortality data in NVSS to identify AI/AN deaths that had been misclassified as non-Native and to determine vital status and cause of death of decedents who had received health care in IHS or tribal facilities.10 About 62% of the AI/AN population has obtained IHS services and is included in the IHS patient registration database.16 Following the linkage of IHS records to the NDI, a flag indicating a positive link to IHS was added as an additional indicator of AI/AN ancestry to the NVSS mortality file. This file was then combined with the census population estimates to create an analytical file in SEER*Stat (version 8.0.4; National Cancer Institute, Bethesda, MD; AI/AN-US Mortality Database [AMD]) which includes all deaths for all races from 1990 to 2009. Race for AI/AN deaths combines race classification by NCHS based on the death certificate and information derived from data linkages between the IHS patient registration database and the NDI.10
During preliminary analyses of the AMD, we discovered that the updated bridged intercensal population estimates significantly overestimated AI/ANs of Hispanic origin.17 Therefore, to avoid underestimating AI/AN deaths because of overinflated denominators, analyses were limited to non-Hispanic AI/AN persons. Fewer than 5% of cancer cases and deaths were identified as Hispanic AI/AN persons and were excluded from the analysis. Non-Hispanic White was chosen as the most homogeneous referent group. Therefore, all analyses were limited to non-Hispanic women. For conciseness, henceforth the term “non-Hispanic” was omitted when discussing both groups.
For 1990 to 1998, the underlying cause of death was coded according to the International Classification of Diseases, Ninth Revision (ICD-9) (code 180, for deaths because of cervical cancer).18 For 1999–2009, the Tenth Revision (ICD-10) was utilized (code C53, for deaths because of cervical cancer).19,20 Trend analyses spanning ICD-9 and ICD-10 reporting years took into account comparability of cause of death recodes between the 2 revisions.20
Incidence data.
Incident cancer cases diagnosed from 1999 to 2009 were identified from population-based central cancer registries that participate in the Centers for Disease Control and Prevention’s (CDC) National Program of Cancer Registries (NPCR) or the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program.2,21,22 For data to be included for a given year, registries had to meet data standards developed for United States Cancer Statistics.2 Participating registries classified tumor histology, tumor behavior, and primary cancer site according to the International Classification of Diseases for Oncology, Third Edition (ICD-O-3).19 As with mortality, incidence analyses were limited to non-Hispanic AI/AN and White populations to avoid the previously described complications. Incidence rates were presented for invasive cervical cancer among AI/AN populations nationwide, using the SEER Site recode for cervical cancer.23 Incidence data from 1999 to 2009 were examined by race/ethnicity, age, IHS region, and stage at diagnosis. Stage analysis using Derived SEER Summary Stage 2000 was limited to diagnosis years 2004 to 2009 to ensure consistency, because earlier years used different staging schemas.24
Geographic coverage.
We restricted most of the analyses in this study to IHS Contract Health Service Delivery Area (CHSDA) or Tribal Service Delivery Area counties, which, in general, contain federally recognized tribal reservations or off-reservation trusts or lands that are adjacent to them.10 CHSDA residence is used by the IHS to determine eligibility for services not directly available within the IHS. Linkage studies indicate less misclassification of race for AI/AN populations in these counties.10,25 The CHSDA counties also have higher proportions of AI/AN persons in relation to total population than do non-CHSDA counties, with 64% of the US AI/AN population residing in the 637 counties designated as CHSDA (these counties represent 20% of the 3141 counties in the United States).10 Although less geographically representative, we restricted analyses to CHSDA counties for death and incidence rates in this article for the purpose of offering improved accuracy in interpreting statistics for AI/AN populations. For rates restricted to CHSDA counties, data from 35 states and 6 regions were included.
We completed the analyses for all regions combined and by individual IHS regions: Northern Plains, Alaska, Southern Plains, Southwest, Pacific Coast and East; additional details about IHS regions and CHSDA are provided elsewhere10 (Table 1). Identical or similar regional analyses were used for other health-related publications focusing on AI/AN populations.26–28
TABLE 1—
Cervical Cancer Death Rates by Age and Indian Health Service Region for American Indian/Alaska Native and White Women: United States, 1999–2009
| CHSDA |
All Counties |
|||||
| AI/AN, Count (Rate) | White, Count (Rate) | AI/AN:White RR (95% CI) | AI/AN, Count (Rate) | White, Count (Rate) | AI/AN:White RR (95% CI) | |
| Total | 289 (4.2) | 5972 (2.0) | 2.11* (1.86, 2.38) | 380 (3.3) | 28 547 (2.2) | 1.54* (1.38, 1.71) |
| Age, y | ||||||
| 25–44 | 86 (3.7) | 1183 (1.8) | 2.08* (1.65, 2.59) | 104 (2.8) | 5534 (1.9) | 1.48* (1.21, 1.80) |
| 45–64 | 129 (7.4) | 2598 (3.8) | 1.94* (1.61, 2.31) | 189 (6.3) | 12 346 (4.1) | 1.53* (1.32, 1.77) |
| 65–84 | 58 (10.0) | 1720 (4.7) | 2.14* (1.61, 2.78) | 67 (7.4) | 8415 (5.2) | 1.43* (1.10, 1.82) |
| ≥ 85 | 15 (23.7) | 450 (6.5) | 3.67* (2.03, 6.11) | 18 (17.7) | 2168 (7.0) | 2.52* (1.49, 3.99) |
| IHS Region | ||||||
| Northern Plains | 79 (7.3) | 878 (1.8) | 4.15* (3.23, 5.27) | 99 (5.5) | 4815 (2.0) | 2.78* (2.24, 3.43) |
| Alaska | 14 (3.5) | 43 (1.9) | 1.83 (0.89, 3.48) | 14 (3.5) | 43 (1.9) | 1.83 (0.89, 3.48) |
| Southern Plains | 66 (4.3) | 519 (2.8) | 1.58* (1.20, 2.04) | 73 (3.5) | 2624 (2.5) | 1.40* (1.09, 1.77) |
| Southwest | 81 (4.2) | 857 (2.0) | 2.05* (1.60, 2.59) | 87 (4.1) | 1307 (1.8) | 2.21* (1.74, 2.76) |
| Pacific Coast | 34 (2.4) | 1801 (2.0) | 1.20 (0.82, 1.70) | 48 (2.2) | 3356 (2.0) | 1.11 (0.81, 1.48) |
| East | 15 (3.3) | 1874 (2.0) | 1.69 (0.91, 2.82) | 59 (2.1) | 16 402 (2.3) | 0.93 (0.70, 1.21) |
| Selected IHS regions and age, y | ||||||
| Northern Plains | ||||||
| 25–44 | 18 (4.8) | 175 (1.6) | 3.07* (1.78, 4.99) | 23 (3.7) | 878 (1.6) | 2.35* (1.48, 3.54) |
| 45–64 | 42 (15.5) | 371 (3.3) | 4.71* (3.34, 6.50) | 55 (12.0) | 2062 (3.8) | 3.18* (2.39, 4.16) |
| ≥ 65 | 18 (19.2) | 329 (4.5) | 4.29* (2.48, 7.01) | 20 (13.6) | 1861 (5.3) | 2.58* (1.55, 4.05) |
| Southern Plains | ||||||
| 25–44 | 27 (5.9) | 115 (2.8) | 2.09* (1.32, 3.20) | 30 (4.7) | 568 (2.4) | 2.01* (1.34, 2.90) |
| 45–64 | 26 (7.0) | 208 (4.8) | 1.46 (0.93, 2.20) | 29 (5.5) | 1137 (4.7) | 1.17 (0.78, 1.68) |
| ≥ 65 | 13 (8.3) | 191 (6.6) | 1.27 (0.66, 2.24) | 14 (7.1) | 909 (6.1) | 1.18 (0.64, 2.00) |
| Southwest | ||||||
| 25–44 | 19 (2.7) | 163 (1.8) | 1.50 (0.88, 2.42) | 19 (2.4) | 255 (1.5) | 1.57 (0.93, 2.50) |
| 45–64 | 35 (6.9) | 402 (4.1) | 1.69* (1.16, 2.38) | 40 (7.1) | 613 (3.7) | 1.94* (1.37, 2.68) |
| ≥ 65 | 27 (14.7) | 288 (4.6) | 3.17* (2.04, 4.73) | 27 (13.8) | 433 (4.5) | 3.10* (2.01, 4.60) |
Note. AI/AN = American Indian/Alaska Native; CHSDA = Contract Health Service Delivery Areas; CI = confidence interval; IHS = Indian Health Service. Women of Hispanic origin are excluded from the analyses. AI/AN race is reported from death certificates or through linkage with the IHS patient registration database. Rates are per 100 000 persons and are age-adjusted to the 2000 US standard population (11 age groups; Census P25-1130).29 Rate ratios (RR) are calculated in SEER*Stat before rounding of rates and may not equal RR calculated from rates presented in the table. IHS regions are defined as follows: Northern Plains (IL, IN,b IA,b MA,b MN,b MT,b NE,b ND,b SD,b WI,b WYb); Southern Plains (OK,b KS,b TX); Southwest (AZ,b CO,b NV,b NM,b UTb); Pacific Coast (CA,b ID,b OR,b WA,b HI); East (AL,b AR, CT,b DE, FL,b GA, KY, LA,b ME,b MD, MA,b MS,b MO, NH, NJ, NY,b NC,b OH, PA,b RI,b SC,b TN, VT, VA, WV, DC, IL, IN,b IA,b MIb). Percent regional coverage of AI/AN persons in CHSDA counties to AI/AN persons in all counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; East = 18.2%; total US = 64.2%.
Source. AI/AN Mortality Database (AMD 1990–2009).
Cases aged 0–24 years are included in overall totals, but rows have been suppressed because of few cases.
Identifies states with at least 1 county designated as CHSDA.
*P < .05.
Statistical Methods
All rates, expressed per 100 000 population, were directly age-adjusted to the 2000 US standard population (Census P25-1130),29 using SEER*Stat software (version 8.0.4; National Cancer Institute, Bethesda, MD). Readers should avoid comparison of these data with published death rates adjusted using a different standard population.
Using the age-adjusted incidence and death rates, we calculated standardized rate ratios (RRs) for AI/AN populations using White rates for comparison. We examined data on deaths occurring from 1999 to 2009 by race/ethnicity, age, IHS region, and combined age and IHS region for selected regions. Trends in cervical cancer deaths were examined for 1990 to 2009. We calculated RRs using SEER*Stat to the fourth digit, which were rounded for presentation in the tables. We calculated 95% confidence intervals (CIs) for age-adjusted rates, and RRs were calculated based on methods described by Tiwari et al. using SEER*Stat 8.0.4.30 We assessed temporal changes in annual age-adjusted death rates, including the annual percent change (APC) for each interval, with Joinpoint regression techniques using statistical software developed by the National Cancer Institute; up to 3 joinpoints were allowed in models.31 Statistical significance was set at a P level of less than .05.
RESULTS
Overall, a total of 380 AI/AN women died from cervical cancer from 1999 to 2009; 289 of these women resided in CHSDA counties (Table 1). AI/AN women had a cervical cancer death rate of 3.3, which was higher than the rate of 2.2 for White women (RR = 1.54).
For CHSDA counties only, the death rate from cervical cancer for AI/AN women was 4.2, which was nearly twice the corresponding rate among White women in the same counties (rate 2.0; RR = 2.11). The remaining results about death rates focused on CHSDA counties only.
Age and Indian Health Service Region
Death rates for cervical cancer were higher among AI/AN women compared with White women, for each age group (Table 1). Death rates for those aged 0 to 24 years were suppressed because of small numbers. Rates were highest, and differences were greatest for women aged 85 years or older (RR = 3.67).
Cervical cancer mortality among AI/AN women was highest in the Northern Plains region and was higher than mortality for White women in Northern Plains (RR = 4.15), Southern Plains (RR = 1.58), and the Southwest (RR = 2.05). Death rates comparisons were not statistically significantly different between AI/AN women and White women in Alaska (RR = 1.83), East (RR = 1.69), and Pacific Coast regions (RR = 1.20).
IHS regions with statistically significant AI/AN death rates higher than White death rates (Northern Plains, Southern Plains, and Southwest) were examined further by age to clarify possible reasons for these differences (Table 1). In the Northern Plains, AI/AN women had higher death rates from cervical cancer than White women in all age groups; death rates and disparities between groups (AI/AN vs White) increased with age. In the Southern Plains, AI/AN women aged 25 to 44 years had higher death rates than White women. However, disparities decreased with age, so that differences between women aged 45 to 64 and 65 years and older were not statistically significant. In the Southwest region, AI/AN women aged 40 to 64 and 65 years and older had higher death rates from cervical cancer than White women.
Trends.
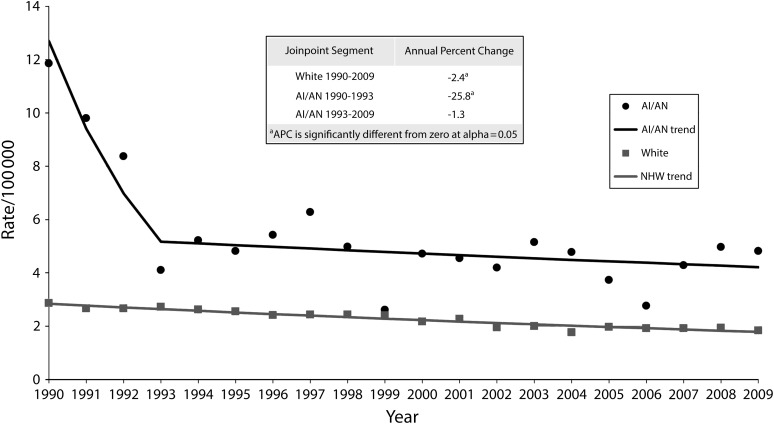
Cervical cancer mortality declined from 1990 to 2009 among both AI/AN women and White women. Declines for AI/AN women occurred primarily from 1990 to 1993 (−25.8% per year; P < .05); death rates remained relatively steady from 1993 to 2009 (APC = −1.3). Declines among White women were more steady and statistically significant (−2.4% per year for 1990–2009; Figure 1).
FIGURE 1—
Trends in cervical cancer death rates for American Indian/Alaska Native and White Women: CHSDA Counties, United States, 1990–2009.
Note. AI/AN = American Indians/Alaska Natives; CHSDA = Contract Health Service Delivery Areas. Women of Hispanic origin were excluded from the analyses. AI/AN race was reported from death certificates or through linkage with the Indian Health Service patient registration database. Rates are age-adjusted to the 2000 US standard population (11 age groups; Census P25-1130).29 States and years of data excluded because Hispanic origin was not collected on the death certificate: LA: 1990; NH: 1990–1992; OK: 1990–1996.
Source. AI/AN Mortality Database (AMD 1990–2009).
Incidence Data
Overall, a total of 1020 AI/AN women were diagnosed with cervical cancer from 1999 to 2009; 799 of these women resided in CHSDA counties (Table 2). AI/AN women had an incidence rate of cervical cancer of 8.7, compared with a rate of 7.5 for White women. However, when restricted to CHSDA areas, the rate for AI/AN women was 11.0, which was higher than that for White women in CHSDA areas (7.1; Table 2). The remaining results about incidence focused on CHSDA areas only.
TABLE 2—
Invasive Cervical Cancer Incidence Rates by Age and Indian Health Service Region for American Indian/Alaska Native and White Women: United States, 1999–2009
| CHSDA |
All Counties |
|||||
| AI/AN,a,b Count (Rate) | White,a Count (Rate) | AI/AN:White RR (95% CI) | AI/AN, Count (Rate) | White, Count (Rate) | AI/AN:White RR (95% CI) | |
| Total | 799 (11.0) | 18 950 (7.1) | 1.55* (1.44, 1.66) | 1020 (8.7) | 87 302 (7.5) | 1.54* (1.32, 1.77) |
| Age, y | ||||||
| < 25 | 27 (0.7) | 271 (0.3) | 2.18* (1.41, 3.23) | 30 (0.5) | 1097 (0.3) | 1.69* (1.13, 2.42) |
| 25–44 | 379 (16.5) | 7473 (11.5) | 1.43* (1.28, 1.58) | 485 (13.1) | 34 054 (11.9) | 1.10* (1.01, 1.21) |
| 45–64 | 283 (16.3) | 7339 (11.0) | 1.48* (1.31, 1.67) | 370 (12.7) | 33 560 (11.7) | 1.08 (0.98, 1.20) |
| 65–84 | 96 (17.2) | 3317 (9.2) | 1.86* (1.50, 2.29) | 118 (13.5) | 15 939 (10.2) | 1.32* (1.09, 1.58) |
| ≥ 85 | 14 (22.3) | 550 (8.0) | 2.80* (1.52, 4.74) | 17 (17.0) | 2652 (8.8) | 1.93* (1.12, 3.10) |
| IHS Region | ||||||
| Northern Plains | 149 (13.3) | 2948 (6.8) | 1.97* (1.65, 2.34) | 206 (11.1) | 15 664 (7.2) | 1.54* (1.32, 1.77) |
| Alaska | 67 (13.1) | 165 (6.8) | 1.94* (1.42, 2.62) | 67 (13.1) | 165 (6.8) | 1.94* (1.42, 2.62) |
| Southern Plains | 234 (15.1) | 1574 (9.2) | 1.64* (1.43, 1.89) | 268 (12.6) | 7907 (8.3) | 1.53* (1.34, 1.73) |
| Southwest | 176 (8.3) | 2659 (7.0) | 1.19* (1.01, 1.39) | 190 (8.1) | 4282 (6.5) | 1.25* (1.07, 1.45) |
| Pacific Coast | 133 (9.6) | 5671 (7.0) | 1.36* (1.13, 1.63) | 167 (8.0) | 10 588 (6.9) | 1.15 (0.98, 1.35) |
| East | 40 (8.4) | 5933 (7.1) | 1.18 (0.83, 1.62) | 122 (4.5) | 48 696 (7.8) | 0.58* (0.48, 0.69) |
| Stage | ||||||
| Localized | 194 (4.5) | 4563 (3.4) | 1.34* (1.15, 1.55) | 259 (3.7) | 21 391 (3.5) | 1.04 (0.92, 1.18) |
| Regional | 166 (4.0) | 3347 (2.2) | 1.84* (1.56, 2.16) | 204 (3.0) | 16 041 (2.4) | 1.27* (1.09, 1.46) |
| Distant | 56 (1.4) | 1274 (0.8) | 1.74* (1.30, 2.28) | 71 (1.1) | 5893 (0.8) | 1.29* (1.00, 1.64) |
| Unstaged | 45 (1.1) | 835 (0.5) | 2.15* (1.53, 2.93) | 59 (0.9) | 3529 (0.5) | 1.78* (1.34, 2.33) |
Note. AI/AN = American Indian/Alaska Native; CHSDA = Contract Health Service Delivery Areas; CI = confidence interval; IHS = Indian Health Service; RR = rate ratio. Women of Hispanic origin are excluded from the analyses. AI/AN race is reported by National Program of Cancer Registries and Surveillance, Epidemiology, and End Results registries or through linkage with the IHS patient registration database. Rates are per 100 000 persons and are age-adjusted to the 2000 US standard population (19 age groups; Census P25-1130).29 RRs are calculated in SEER*Stat before rounding of rates and may not equal RRs calculated from rates presented in the table. IHS regions are defined as follows: Northern Plains (IL, IN,b IA,b MA,b MN,b MT,b NE,b ND,b SD,b WI,b WYb); Southern Plains (OK,b KS,b TXb); Southwest (AZ,b CO,b NV,b NM,b UTb); Pacific Coast (CA,b ID,b OR,b WA,b HI); East (AL,b AR, CT,b DE, FL,b GA, KY, LA,b ME,b MD, MA,b MS,b MO, NH, NJ, NY,b NC,b OH, PA,b RI,b SC,b TN, VT, VA, WV, DC, IL, IN,b IA,b MIb). Percent regional coverage of AI/AN persons in CHSDA counties to AI/AN persons in all counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; East = 18.2%; total US = 64.2%.
Source. Data are from population-based cancer registries that participate in the National Program of Cancer Registries or the Surveillance, Epidemiology, and End Results Program, and meet criteria for high quality data. Years of data and registries used: 1999–2009 (43 states): AK, AL, AZ, CA, CO, CT, DE, FL, GA, HI, IA, ID, IL, IN, KS, KY, LA, MA, MD, ME, MI, MN, MO, MT, ND, NE, NH, NJ, NM, NV, NY, OH, OK, OR, PA, RI, SC, TX, UT, VT, WA, WV, WY; 1999–2008: WI; 1999–2001 and 2003–2009: DC; 2001–2009: AR, NC, SD; 2002–2009: VA; 2003–2009: MS, TN.
Among unstaged cases, 4 women were diagnosed after death (death certificate only).
Identifies states with at least 1 county designated as CHSDA.
*P < .05.
Age.
Incidence rates for cervical cancer were higher among AI/AN women compared with White women for each age group. Differences were greatest for women aged 85 years and older (RR = 2.80).
Region.
Cervical cancer incidence among AI/AN women was highest in the Southern Plains region (rate = 15.1) and was higher than incidence for White women in the Northern Plains (RR = 1.97), Alaska (RR = 1.94), Southern Plains (RR = 1.64), Southwest (RR = 1.19), and Pacific Coast (RR = 1.36) regions (Table 2). Incidence rates were similar for AI/AN women compared with White women in the East region (RR = 1.18).
Stage.
AI/AN women had higher rates of cervical cancer incidence than White women across all stages at diagnosis (Table 2). Disparities between AI/AN and Whites were greater with later stage at diagnosis and were most pronounced among unstaged cases.
DISCUSSION
Our results demonstrated that AI/AN women had significantly higher cervical cancer incidence and mortality compared with White women in the same areas. However, both incidence and mortality decreased over time, documenting improvements in identifying and treating cervical cancer and pre-cancerous lesions. Most cervical cancers could be avoided or diagnosed early through screening and treatment. We noted steep declines in cervical cancer deaths among AI/AN women in the early 1990s. We believed that these declines were likely the result of screening and treatment programs described in our discussion.27 However, our data also underscored the need for further efforts, as noted in CHSDA counties (where identification of AI/AN women was likely to be highest), AI/AN women still died from cervical cancer at twice the rate of White women.
Disparities in death rates between AI/AN women and White women living in the same areas were evident across all age groups and regions; regional differences were only statistically significant in the Northern Plains, Southern Plains, and Southwest regions (possibly because of small numbers in the other areas). To examine these disparities more closely, we analyzed regions with statistically significant disparities in death rates (Northern Plains, Southern Plains, and Southwest) by age group (25–44, 45–64, ≥ 65 years). Overall patterns were unclear, because the Northern Plains region had similar disparities across all age groups, the Southern Plains had the largest disparities among the youngest women, and the Southwest had the largest disparities among the oldest women. These disparities highlighted the need for further outreach to rarely and never-screened AI/AN women of all ages.
Federal programs have been integral in addressing cervical cancer incidence and deaths among AI/AN women. The IHS began providing cervical cancer screening to Native women in the 1960s and 1970s, leading to decreases in cervical cancer incidence and mortality by the 1980s and 1990s, as described in our data.32 In addition to the IHS program, Congress also passed the Breast and Cervical Cancer Mortality Prevention Act of 1990, initiating the CDC’s National Breast and Cervical Cancer Early Detection Program (NBCCEDP), which provides access to breast and cervical cancer screening and diagnostic services to underserved women.33 To address continuing disparities, the 1993 reauthorization of the act included amendments directing the CDC to establish a program with AI/AN tribes and tribal organizations to improve screening in tribal communities.34 A recent study found that 36% of eligible AI/AN women were screened through NBCCEDP, higher than any other group.35 Currently, the NBCCEDP funds 11 AI/AN tribes or tribal organizations to provide screening services for breast and cervical cancer. Collaborations between tribal and state programs have been successful, such as the one between the Oklahoma state, Cherokee Nation, and the Kaw Nation grantees to pass Oklahoma’s Breast and Cervical Cancer Prevention and Treatment Act in 2005, which led to the development of the Oklahoma CARES program.36 In addition to funding screening services, the NBCCEDP also partnered with tribal programs, state partners, and others to increase outreach and education to AI/AN women on the need of preventive care and cervical screening. Such activities were likely related to continued decreases in AI/AN cervical cancer incidence and mortality, as shown in our data.
Appropriate screening and follow-up treatment of abnormalities could reduce cervical cancer incidence and mortality (screening guidelines can be found at http://www.cdc.gov/cancer/cervical/pdf/guidelines.pdf). Self-reported screening data from the Behavioral Risk Factor Surveillance System (BRFSS) showed that 82% of eligible AI/AN women reported having had a Pap test recently (within 3 years), nearly as high as that for White women (85%).37 However, Government Performance and Results Act data from the IHS on cervical screening, which are based on medical records rather than self-report, showed lower rates of screening and slight declines in recent years. In 2012, only 57% of eligible women in the IHS system were recently screened (within 3 years), down from 62% in 2002.38
Despite these screening efforts by federal programs to reach AI/AN women, disparities remained, as demonstrated by the higher incidence, later stage of disease, and mortality of cervical cancer in the Northern and Southern Plains. Barriers to screening among AI/AN women might stem from lack of transportation or childcare, negative perception of medical providers, long waits for appointments, and patient–provider communication.39 Provider time pressures, health systems designed primarily for acute and episodic care, and an underfunded health system are other potential barriers IHS and tribal providers might face.5 In addition, cultural reluctance to access Western medicine for nonacute health problems and transportation difficulties were factors commonly cited as barriers to cancer screening by AI/AN individuals.40–43
Human papillomavirus (HPV) is the primary cause of nearly all cervical cancer.44 AI/AN populations generally have lower rates of HPV-associated cancers than Whites, except for cervical cancer.45 Vaccines are available that protect against infection with the types of HPV that most commonly cause cervical cancer. Rates of HPV vaccination were lower than for other childhood and adolescent vaccines, but AI/AN vaccination rates were similar to those of other races and ethnicities, and providers frequently serving AI/AN populations generally adopted recommendations for HPV vaccination.46,47 A recent study found that AI/AN women in the Northern Plains were less likely to vaccinate children against HPV than White women in the same area, but differences were because of knowledge about the vaccine, suggesting that improving education could improve vaccine uptake.48 As with screening, local and culturally tailored interventions are important to improving vaccination rates.
The 2004 US surgeon general’s report indicated that smoking increases the risk of cervical cancer, and data in this supplement showed that the highest prevalence of female AI/AN current smokers was in the Northern Plains and Alaska.37,49 Comprehensive cancer control programs in tribal communities, such as the Cherokee Nation Comprehensive Cancer Control program funded by the CDC, implemented programs to help reduce tobacco use that might be helpful in reducing cervical cancer incidence.50
There were several limitations to consider when interpreting the results presented in this article. First, although linkage with the IHS patient registration database improved the classification of race for AI/AN decedents, the issue was not completely resolved because AI/AN persons who were not members of the federally recognized tribes were not eligible for IHS services and not represented in the IHS database. Additionally, some decedents might have been eligible for, but never used, IHS services, and therefore, were not included in the IHS registration database. Approximately 38% of AI/AN persons might be eligible for IHS services, but never used them. Second, the findings from CHSDA counties highlighted in this supplement did not represent all AI/AN populations in the United States or in individual IHS regions.10 In particular, the East region included only 18.2% of the total AI/AN population for that region. Furthermore, the analyses based on CHSDA designation excluded many AI/AN decedents in urban areas that were not part of a CHSDA county. AI/AN residents of urban areas differed from all AI/ANs in poverty level, health care access, and other factors that may influence mortality trends.51,52 Third, these analyses revealed less variation for White women than for AI/AN women by IHS regions using data from CHSDA counties only. Alternative groupings of states or counties might reveal a different level of variation for non-Hispanic White women. In addition, there was substantial variation between federally recognized tribes in the proportion of Native ancestry required for tribal membership, and therefore, for eligibility for IHS services. Whether and how this discrepancy in tribal membership requirements might influence some of our findings was unclear, although our findings were consistent with previous reports. Moreover, although the exclusion of Hispanic AI/ANs from the analyses reduced the overall number of AI/AN deaths by less than 5%, it might disproportionately exclude some tribal members in states along the US–Mexico border and elsewhere who had Hispanic surnames and might be coded as Hispanic at death. Finally, some rates were based on relatively small numbers.
Despite these limitations, this study added to the existing literature on cervical cancer incidence and mortality of AI/AN women by improving identification of AI/AN populations. Death certificates and cancer incidence data frequently misclassified race of AI/AN decedents and patients.11,53 Linkage with the IHS patient registration database identified 203 cases and 40 deaths among AI/AN women that would not otherwise have been identified, adding approximately 20% of incident cases and 10% of deaths to our analysis. This was the first time data linkages between the IHS patient registration database and the NDI were used for mortality, making these the most accurate data available to calculate mortality statistics.10,53 By providing analysis of CHSDA counties and all US counties, and by using linked data to improve identification of AI/AN cases and deaths, this study provided the most comprehensive picture to date of cervical cancer mortality among AI/AN women. Previous analyses of cervical cancer incidence among AI/AN populations used similarly linked data sets, but our study extended those findings by adding information on cervical cancer mortality.5
The substantial strides made in cervical cancer control for AI/AN women over the last 20 years have clearly played a role in reducing the incidence and mortality of this disease. However, findings from this study and previous reports indicated that these rates were higher than those for White women, and that there was a wide regional variation.5,54 The regional variations in the rates might reflect, in part, geographic variations in screening and other factors. Future progress in decreasing the cervical cancer burden in AI/AN populations is necessary and achievable with implementation of intervention programs that are targeted to these specific populations and address the barriers to appropriate screening and follow-up.
Human Participant Protection
CDC and IHS determined this project to constitute public health practice and not research; therefore, no formal institutional review board approvals were required.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.US Cancer Statistics Working Group. United States Cancer Statistics: 1999–2009 Incidence and Mortality Web-based Report. 2013. Available at: http://apps.nccd.cdc.gov/uscs. Accessed May 5, 2013.
- 3.Freeman H, Wingrove B. Excess Cervical Cancer Mortality: A Marker for Low Access to Health Care in Poor Communities. Bethesda, MD: National Cancer Institute; 2005. [Google Scholar]
- 4.Baquet CR. Native Americans’ cancer rates in comparison with other peoples of color. Cancer. 1996;78(7 suppl):1538–1544. [PubMed] [Google Scholar]
- 5.Becker TM, Espey DK, Lawson HW, Saraiya M, Jim MA, Waxman AG. Regional differences in cervical cancer incidence among American Indians and Alaska Natives, 1999–2004. Cancer. 2008;113(5 suppl):1234–1243. doi: 10.1002/cncr.23736. [DOI] [PubMed] [Google Scholar]
- 6.Chu KC, Miller BA, Springfield SA. Measures of racial/ethnic health disparities in cancer mortality rates and the influence of socioeconomic status. J Natl Med Assoc. 2007;99(10):1092–1100. 1102–1104. [PMC free article] [PubMed] [Google Scholar]
- 7.Cobb N, Paisano RE. Patterns of cancer mortality among Native Americans. Cancer. 1998;83(11):2377–2383. doi: 10.1002/(sici)1097-0142(19981201)83:11<2377::aid-cncr18>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 8.Paltoo DN, Chu KC. Patterns in cancer incidence among American Indians/Alaska Natives, United States, 1992–1999. Public Health Rep. 2004;119(4):443–451. doi: 10.1016/j.phr.2004.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. The National Breast and Cervical Cancer Early Detection Program (NBCCEDP): Screening Program Data. 2012. Available at: http://www.cdc.gov/cancer/nbccedp/data/index.htm. Accessed March 6, 2013.
- 10.Espey DK, Jim MA, Richards T, Begay C, Haverkamp D, Roberts D. Methods for improving the quality and completeness of mortality data for American Indians and Alaska Natives. Am J Public Health. 2014;104(6 suppl 3):S286–S294. doi: 10.2105/AJPH.2013.301716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Espey DK, Wiggins CL, Jim MA, Miller BA, Johnson CJ, Becker TM. Methods for improving cancer surveillance data in American Indian and Alaska Native populations. Cancer. 2008;113(5 suppl):1120–1130. doi: 10.1002/cncr.23724. [DOI] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics. US census populations with bridged race categories. 2012. Available at: http://www.cdc.gov/nchs/nvss/bridged_race.htm. Accessed April 9, 2012.
- 13.National Cancer Institute. Surveillance epidemiology and end results. Adjusted populations for the counties/parishes affected by Hurricanes Katrina and Rita. 2012. Available at: http://seer.cancer.gov/popdata/hurricane_adj.html. Accessed April 5, 2013.
- 14.National Center for Health Statistics, Division of Vital Statistics. National Vital Statistics System. 2012. Available at: http://www.cdc.gov/nchs/nvss.htm. Accessed May 2, 2012.
- 15.National Center for Health Statistics, Division of Vital Statistics. NCHS procedures for multiple-race and Hispanic origin data: collection, coding, editing, and transmitting. 2004. Available at: http://www.cdc.gov/nchs/data/dvs/Multiple_race_documentation_5-10-04.pdf. Accessed May 8, 2013.
- 16.Indian Health Service. Indian Health Service: a quick look. 2013. Available at: http://www.ihs.gov/newsroom/includes/themes/newihstheme/display_objects/documents/factsheets/QuickLook_2013.pdf. Accessed May 8, 2013.
- 17.Edwards BK, Noone AM, Mariotto AB et al. Annual report to the nation on the status of cancer, 1975–2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. 2013 doi: 10.1002/cncr.28509. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention (CDC) International Classification of Diseases. Ninth Revision (ICD-9) Geneva, Switzerland: World Health Organization; 1980. [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC) International Classification of Diseases. Tenth Revision (ICD-10) Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 20.Anderson RN, Minino AM, Hoyert DL, Rosenberg HM. Comparability of cause of death between ICD-9 and ICD-10: preliminary estimates. National Vital Stat Rep. 2001;49(2):1–32. [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. National Program of Cancer Registries (NPCR). About the Program. Available at: http://www.cdc.gov/cancer/npcr/about.htm. Accessed May 8, 2013.
- 22.Hankey BF, Ries LA, Edwards BK. The surveillance, epidemiology, and end results program: a national resource. Cancer Epidemiol Biomarkers Prev. 1999;8(12):1117–1121. [PubMed] [Google Scholar]
- 23.National Cancer Institute. SEER site recode ICD-O-3 (1/27/2003) definition. Surveillance Epidemiology and End Results. 2010. Available at: http://seer.cancer.gov/siterecode/icdo3_d01272003. Accessed March 2, 2010.
- 24.Young JL Jr, Roffers SD, Ries LAG, Fritz AG, editors. HA. SEER Summary Staging Manual - 2000: Codes and Coding Instructions. Bethesda, MD: National Cancer Institute; 2001. [Google Scholar]
- 25.Arias E, Schauman W, Eschbach K, Sorlie P. The validity of race and Hispanic origin reporting on death certificates in the United States. Vital Health Stat 2. 2008;(148):1–23. [PubMed] [Google Scholar]
- 26.Denny CH, Taylor TL. American Indian and Alaska Native health behavior: findings from the Behavioral Risk Factor Surveillance System, 1992-1995. Ethn Dis. 1999;9(3):403–409. [PubMed] [Google Scholar]
- 27.Espey D, Paisano R, Cobb N. Regional patterns and trends in cancer mortality among American Indians and Alaska Natives, 1990-2001. Cancer. 2005;103(5):1045–1053. doi: 10.1002/cncr.20876. [DOI] [PubMed] [Google Scholar]
- 28.Wiggins CL, Espey DK, Wingo PA et al. Cancer among American Indians and Alaska Natives in the United States, 1999-2004. Cancer. 2008;113(5 suppl):1142–1152. doi: 10.1002/cncr.23734. [DOI] [PubMed] [Google Scholar]
- 29. Day JC, Population Projections of the United States by Age, Sex, Race, and Hispanic Origin: 1995 to 2050, US Bureau of the Census, Current Population Reports, P25-1130, Washington, DC: US Government Printing Office; 1996.
- 30.Tiwari RC, Clegg LX, Zou Z. Efficient interval estimation for age-adjusted cancer rates. Stat Methods Med Res. 2006;15(6):547–569. doi: 10.1177/0962280206070621. [DOI] [PubMed] [Google Scholar]
- 31.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 32.Chao A, Becker TM, Jordan SW, Darling R, Gilliland FD, Key CR. Decreasing rates of cervical cancer among American Indians and Hispanics in New Mexico (United States) Cancer Causes Control. 1996;7(2):205–213. doi: 10.1007/BF00051296. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention The National Breast and Cervical Cancer Early Detection Program (NBCCEDP). 2012Available at: http://www.cdc.gov/cancer/nbccedp/index.htm. Accessed March 8, 2013
- 34.Henson RM, Wyatt SW, Lee NC. The National Breast and Cervical Cancer Early Detection Program: a comprehensive public health response to two major health issues for women. J Public Health Manag Pract. 1996;2(2):36–47. [PubMed] [Google Scholar]
- 35.Tangka FK, O’Hara B, Gardner JG et al. Meeting the cervical cancer screening needs of underserved women: the National Breast and Cervical Cancer Early Detection Program, 2004-2006. Cancer Causes Control. 2010;21(7):1081–1090. doi: 10.1007/s10552-010-9536-3. [DOI] [PubMed] [Google Scholar]
- 36.Oklahoma State Department of Health. Oklahoma CARES Program. Available at: http://www.ok.gov/health/Disease,_Prevention,_Preparedness/Chronic_Disease_Service/Cancer_Prevention_Programs_/Oklahoma_Breast_and_Cervical_Cancer_Treatment_Program.html. Accessed March 13, 2013.
- 37.Cobb N, Espey D, King J. Health behaviors and risk factors among American Indians and Alaska Natives, 2000–2010. Am J Public Health. 2014;104(6 suppl 3):S481–S489. doi: 10.2105/AJPH.2014.301879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Indian Health Service. Quality of IHS Health Care: Performance Measures: Cancer Screening-Cervical (Pap Smear) 2013. Available at: http://www.ihs.gov/qualityofcare/index.cfm?module=chart&rpt_type=gpra&measure=15. Accessed March 11, 2013.
- 39.Smith AJ, Christopher S, LaFromboise VR, Letiecq BL, McCormick AK. Apsaalooke women’s experiences with Pap test screening. Cancer. 2008;15(2):166–173. doi: 10.1177/107327480801500209. [DOI] [PubMed] [Google Scholar]
- 40.Coe K, Martin L, Nuvayestewa L et al. Predictors of Pap test use among women living on the Hopi reservation. Health Care Women Int. 2007;28(9):764–781. doi: 10.1080/07399330701562956. [DOI] [PubMed] [Google Scholar]
- 41.Michalek AM, Mahoney MC, Papas M, Tenney M, Burhansstipanov L. Tribal-based cancer control activities among Alaska Natives: services and perceptions. Alaska Med. 1996;38(2):59–64. [PubMed] [Google Scholar]
- 42.Canales M. Taking care of self: health care decision making of American Indian women. Health Care Women Int. 2004;25(5):411–435. doi: 10.1080/07399330490438323. [DOI] [PubMed] [Google Scholar]
- 43.Novins D, Beals J, Moore L, Spicer P, Manson S. Use of biomedical services and traditional healing options among American Indians: sociodemographic correlates, spirituality, and ethnic identity. Med Care. 2004;42(7):670–679. doi: 10.1097/01.mlr.0000129902.29132.a6. [DOI] [PubMed] [Google Scholar]
- 44.Walboomers JM, Jacobs MV, Manos MM et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12–19. doi: 10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 45.Jemal A, Simard EP, Dorell C et al. Annual report to the nation on the status of cancer, 1975-2009, featuring the burden and trends in HPV-associated cancers and HPV vaccination coverage levels. J Natl Cancer Inst. 2013;105(3):175–201. doi: 10.1093/jnci/djs491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Centers for Disease Control and Prevention. National and state vaccination coverage among adolescents aged 13-17 years–United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(34):671–677. [PubMed] [Google Scholar]
- 47.Jim CC, Lee JW, Groom AV et al. Human papillomavirus vaccination practices among providers in Indian health service, tribal and urban Indian healthcare facilities. J Womens Health (Larchmt) 2012;21(4):372–378. doi: 10.1089/jwh.2011.3417. [DOI] [PubMed] [Google Scholar]
- 48.Buchwald D, Muller C, Bell M, Schmidt-Grimminger D. Attitudes toward HPV vaccination among rural American Indian women and urban White women in the northern plains. Health Educ Behav. 2013;40(6):704–711. doi: 10.1177/1090198113477111. [DOI] [PubMed] [Google Scholar]
- 49.US Department of Health and Human Services. The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, CDC; 2004. [Google Scholar]
- 50.Centers for Disease Control and Prevention. Stories of Success: National Comprehensive Cancer Control Program: Comprehensive Cancer Control in Action. Atlanta, GA: Centers for Disease Control and Prevention, National Comprehensive Cancer Control Program; 2012. [Google Scholar]
- 51.Urban Indian Health Institute, Seattle Indian Health Board. Seattle, WA: Urban Health Institute; 2004. The Health Status of Urban American Indians and Alaska Natives: An Analysis of Select Vital Records and Census Data Sources. [Google Scholar]
- 52.Urban Indian Health Commission. Seattle, WA: Urban Indian Health Commission; 2007. Invisible Tribes: Urban Indians and Their Health in a Changing World. Available at: http://www.uihi.org/wp-content/uploads/2009/09/UIHC_Report_FINAL.pdf. Accessed February 2, 2014. [Google Scholar]
- 53.Jim MA, Arias E, Seneca DSet al. Racial misclassification of American Indians and Alaska Natives by Indian Health Service Contract Health Service Delivery Area Am J Public Health 20141046 suppl 3)S295–S302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Espey DK, Wu XC, Swan J et al. Annual report to the nation on the status of cancer, 1975-2004, featuring cancer in American Indians and Alaska Natives. Cancer. 2007;110(10):2119–2152. doi: 10.1002/cncr.23044. [DOI] [PubMed] [Google Scholar]