Abstract
Objectives. We described death rates and leading causes of death caused by infectious diseases (IDs) in American Indian/Alaska Native (AI/AN) persons.
Methods. We analyzed national mortality data, adjusted for AI/AN race by linkage with Indian Health Service registration records, for all US counties and Contract Health Service Delivery Area (CHSDA) counties. The average annual 1999 to 2009 ID death rates per 100 000 persons for AI/AN persons were compared with corresponding rates for Whites.
Results. The ID death rate in AI/AN populations was significantly higher than that of Whites. A reported 8429 ID deaths (rate 86.2) in CHSDA counties occurred among AI/AN persons; the rate was significantly higher than the rate in Whites (44.0; rate ratio [RR] = 1.96; 95% confidence interval [CI] = 1.91, 2.00). The rates for the top 10 ID underlying causes of death were significantly higher for AI/AN persons than those for Whites. Lower respiratory tract infection and septicemia were the top-ranked causes. The greatest relative rate disparity was for tuberculosis (RR = 13.51; 95% CI = 11.36, 15.93).
Conclusions. Health equity might be furthered by expansion of interventions to reduce IDs among AI/AN communities.
Infectious diseases (IDs) continue to be an important health issue in the United States despite predictions made in the 1970s that by the year 2000 their impact would be minimal.1 Armstrong et al.2 demonstrated that although ID mortality among all races in the United States declined dramatically between 1900 and 1980, ID death rates slowly began to increase in the 1980s, driven primarily by the emergence of HIV and increases in pneumonia and influenza. Furthermore, rates of hospitalization because of IDs were reported to increase from 1998 to 2006.3 Despite overall ID mortality rate declines since 1900, the sudden appearance in 1918 and again in 2009 of the pandemic H1N1 influenza provided a stark reminder of how quickly an infectious agent can affect mortality and morbidity, especially among susceptible populations such as American Indians and Alaska Natives (AI/ANs).4
Among the many disparities affecting AI/AN communities, IDs remain some of the most enduring. A seminal report on the status of AI/AN health in the 1950s noted that the health status of people on many reservations was similar to areas off reservations half a century earlier in 1900.5 This and another early report focusing on Alaska Native health highlighted the tremendous effect of IDs such as tuberculosis, measles, and smallpox on AI/AN morbidity and mortality.5,6 Subsequent studies showed that IDs continued to be significant causes of morbidity among AI/AN persons, with rates typically higher than those for other racial or ethnic groups in the United States.7–11 For example, a recent study found that although the ID hospitalization rate for AI/AN persons declined from 1998 to 2006, the rate among AI/ANs remained higher than the rate for the general US population, especially for the Alaska, Southwest, and Northern Plains West regions.9
Although a study by Pinner et al.12 served to renew interest in overall ID mortality in the United States, to date there have been no similar national studies of ID mortality among AI/AN populations. Despite the ongoing health disparity associated with IDs among AI/AN persons, accurate ID death rates for this group have been difficult to estimate. This difficulty stems, in part, from the use of International Classification of Diseases (ICD) codes, which are not easily related to many infectious causes of mortality.12 An additional complication in determining mortality rates for AI/AN persons is the lack of accuracy in classifying AI/AN race on death certificates.13,14 The accompanying study by Jim et al.14 in this supplement describes, in detail, the effects of misclassification on death rates in the AI/AN population. Studies of ID surveillance data have shown that some reportable ID rates in AI/AN persons may double upon correction for racial misclassification.15 We used national mortality data that, for the first time, were linked with Indian Health Service (IHS) patient registry data, a source of verified AI/AN status with stringent federal rules defining eligibility for health care service.16 This methodology decreased the amount of racial misclassification of AI/AN persons in the national mortality data, and allowed the most complete and accurate view to date of ID mortality among AI/AN populations.
METHODS
We obtained National Vital Statistics System mortality data with IHS patient registration linkage for 1999 to 2009; data included underlying and multiple causes of death, state and county of residence, age, sex, race, and ethnicity. Detailed methods for generating the mortality files used for the present study are described elsewhere in this supplement.17 We selected ID deaths and groups using the ICD-10 codes for ID listed as the underlying cause of death adapted from the ICD-9 codes for ID described in previous articles.7,9,12,18
We conducted analyses of ID mortality among AI/AN persons for Contract Health Service Delivery Area (CHSDA) counties and all US counties (all counties); CHSDA counties, in general, contain federally recognized tribal lands or are adjacent to tribal lands.17 Linkage studies indicated less misclassification of AI/AN race in CHSDA counties.17,19 Although less geographically representative, we presented analyses restricted to CHSDA counties for death rates where indicated.
We conducted further analyses for CHSDA counties and all counties for IHS geographic regions (Alaska, Pacific Coast, Northern Plains, Southern Plains, Southwest, and East).17,20 We used similar overall and regional analyses for other health-related publications focusing on the AI/AN population.21–24 The overall and regional ID deaths were examined by sex, age group (0–19, 20–49, and ≥ 50 years), and ID group. The non-Hispanic White population, assumed to be homogenous across geographic regions, was selected for comparison of ID death rates with those for the AI/AN population.
Average annual age-specific and age-adjusted ID death rates for 1999 to 2009 were expressed per 100 000 of the corresponding population. We used bridged single-race population estimates developed by the US Census Bureau and the Centers for Disease Control and Prevention’s National Center for Health Statistics, adjusted for the population shifts because of Hurricanes Katrina and Rita in 2005, as population denominators in the calculations of ID death rates for the present study.25,26 We calculated average annual age-adjusted ID rates, directly adjusted to the 2000 US standard population, including those for age groups, using SEER*Stat software (version 8.0.2).27 We calculated standardized rate ratios (RRs) with 95% confidence intervals (CIs) for comparison of AI/AN rates with corresponding non-Hispanic White rates based on methods described by Tiwari et al.28 using SEER*Stat 7.0.9. Statistical significance was considered a P level of less than .05. Further description of the population data and analysis is provided elsewhere in this supplement.17
During preliminary analyses, we discovered that the updated bridged intercensal populations estimates significantly overestimated AI/AN persons of Hispanic origin.29 Therefore, to avoid underestimating mortality in AI/AN populations, we limited analyses to non-Hispanic AI/AN persons. For conciseness, we omitted the term “non-Hispanic” henceforth when discussing both groups.
RESULTS
For 1999 to 2009, AI/AN persons experienced significantly higher average annual age-adjusted ID death rates in CHSDA counties and all counties compared with rates for Whites across sex, age group, and region; the single exception was the East region (for all counties), which was lower than the corresponding White average annual death rate (Table 1). Among both AI/AN and White persons, the higher average annual death rates were found in males than females and with increasing age group.
TABLE 1—
Annual Average Age-Adjusted Infectious Disease Death Rates by Characteristics for American Indians/Alaska Natives Compared With Whites: United States, 1999–2009
| CHSDA Counties |
All Counties |
|||||||
| AI/AN Count | AI/AN Rate | White Rate | AI/AN:White RR (95% CI) | AI/AN Count | AI/AN Rate | White Rate | AI/AN:White RR (95% CI) | |
| Total | 8429 | 86.2 | 44.0 | 1.96* (1.91, 2.00) | 10 930 | 68.5 | 46.8 | 1.46* (1.43, 1.49) |
| Sex | ||||||||
| Male | 4083 | 93.6 | 50.4 | 1.86* (1.79, 1.93) | 5379 | 75.5 | 53.4 | 1.41* (1.37, 1.46) |
| Female | 4346 | 79.1 | 39.4 | 2.01* (1.95, 2.07) | 5551 | 63.0 | 41.8 | 1.51* (1.46, 1.55) |
| Age, y | ||||||||
| 0–19 | 429 | 6.5 | 2.6 | 2.46* (2.22, 2.73) | 518 | 5.6 | 2.7 | 2.07* (1.89, 2.26) |
| 20–49 | 1820 | 27.3 | 9.2 | 2.98* (2.84, 3.13) | 2412 | 21.8 | 8.9 | 2.43* (2.34, 2.54) |
| ≥ 50 | 6180 | 261.9 | 142.1 | 1.84* (1.79, 1.89) | 8000 | 209.6 | 151.7 | 1.38* (1.35, 1.41) |
| IHS region | ||||||||
| Northern Plains | 1307 | 88.2 | 38.6 | 2.29* (2.15, 2.43) | 1805 | 76.6 | 41.9 | 1.83* (1.73, 1.93) |
| Alaska | 506 | 81.5 | 31.4 | 2.60* (2.30, 2.92) | 506 | 81.5 | 31.4 | 2.60* (2.30, 2.92) |
| Southern Plains | 1845 | 82.4 | 53.9 | 1.53* (1.45, 1.61) | 2108 | 71.9 | 49.6 | 1.45* (1.39, 1.52) |
| Southwest | 3006 | 101.8 | 45.7 | 2.23* (2.14, 2.32) | 3150 | 98.7 | 44.2 | 2.23* (2.15, 2.32) |
| Pacific Coast | 1352 | 70.6 | 40.4 | 1.75* (1.64, 1.85) | 1805 | 62.5 | 42.8 | 1.46* (1.39, 1.53) |
| East | 413 | 57.6 | 48.3 | 1.19* (1.07, 1.32) | 1556 | 38.6 | 49.3 | 0.78* (0.74, 0.83) |
Note. AI/AN = American Indian/Alaska Native; CHSDA = Contract Health Service Delivery Area; CI = confidence interval; IHS = Indian Health Service; RR = rate ratio. Analyses used International Classification of Diseases, 10th Revision codes listed as the underlying cause of death adapted from the infectious disease International Classification of Diseases, Ninth Revision codes described in previous articles.12,16 AI/AN race is created using death certificate race and IHS link. Analyses are limited to persons of non-Hispanic origin. Rates are per 100 000 persons; age-adjusted rates are age-adjusted to the 2000 US standard population (11 age groups except total, which used 19 age groups).30 RRs are calculated in SEER*Stat before rounding of rates and may not equal RRs calculated from rates presented in table. Percent of AI/AN persons in CHSDA counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; East = 18.2%; total US = 64.2%.
Source. AI/AN Mortality Database (AMD 1990–2009).
*P < .05.
Regional Infectious Disease Deaths
For CHSDA and all counties, the greatest average annual ID death rate disparities between AI/ANs and Whites were seen in the 0 to 19 and 20 to 49 years age groups, and in the Alaska, Southwest, and Northern Plains regions (Table 1). AI/AN persons of the 0 to 19 and 20 to 49 years age groups in the Alaska region and the 20 to 49 years age group in the Northern Plains had an average annual death rate 4 to 5 times higher than those rates for Whites (Table 2). In all regions, and for AI/AN and White persons, the average annual ID death rate increased with increasing age group. AI/AN populations had higher ID death rates than Whites in all age groups and in all regions, except for the 50 years and older group in all counties in the East region (Table 2).
TABLE 2—
Average Annual Age-Adjusted Infectious Disease Death Rates by Indian Health Service Region and Age Group for American Indians/Alaska Natives and Whites: United States, 1999–2009
| CHSDA Counties |
All Counties |
|||||||||
| IHS Region/Age, y | AI/AN Count | AI/AN Rate | White Count | White Rate | AI/AN:White RR (95% CI) | AI/AN Count | AI/AN Rate | White Count | White Rate | AI/AN:White RR (95% CI) |
| Northern Plains | ||||||||||
| 0–19 | 93 | 6.8 | 556 | 2.6 | 2.60* (2.06, 3.24) | 122 | 6.5 | 2687 | 2.7 | 2.44* (2.02, 2.93) |
| 20–49 | 285 | 26.2 | 1906 | 5.3 | 4.95* (4.35, 5.61) | 408 | 22.4 | 10 753 | 6.1 | 3.69* (3.33, 4.07) |
| ≥ 50 | 929 | 274.7 | 37 636 | 127.6 | 2.15* (2.00, 2.31) | 1275 | 238.2 | 194 877 | 138.2 | 1.72* (1.62, 1.83) |
| Alaska | ||||||||||
| 0–19 | 45 | 9.4 | 27 | 2.0 | 4.67* (2.84, 7.83) | 45 | 9.4 | 27 | 2.0 | 4.67* (2.84, 7.83) |
| 20–49 | 95 | 21.0 | 131 | 5.3 | 3.98* (3.02, 5.22) | 95 | 21.0 | 131 | 5.3 | 3.98* (3.02, 5.22) |
| ≥ 50 | 366 | 255.2 | 772 | 104.1 | 2.45* (2.14, 2.80) | 366 | 255.2 | 772 | 104.1 | 2.45* (2.14, 2.80) |
| Southern Plains | ||||||||||
| 0–19 | 75 | 5.5 | 326 | 4.2 | 1.31* (1.01, 1.69) | 80 | 4.8 | 1387 | 3.1 | 1.53* (1.20, 1.92) |
| 20–49 | 361 | 26.4 | 1710 | 13.1 | 2.02* (1.80, 2.26) | 422 | 22.2 | 8998 | 11.8 | 1.88* (1.70, 2.08) |
| ≥ 50 | 1409 | 252.6 | 18 746 | 169.6 | 1.49* (1.41, 1.58) | 1606 | 222.1 | 90 917 | 156.8 | 1.42* (1.34, 1.49) |
| Southwest | ||||||||||
| 0–19 | 157 | 7.6 | 524 | 3.0 | 2.52* (2.09, 3.02) | 162 | 7.4 | 874 | 2.8 | 2.67* (2.24, 3.16) |
| 20–49 | 656 | 32.6 | 3242 | 11.2 | 2.92* (2.68, 3.17) | 707 | 31.6 | 4961 | 9.5 | 3.33* (3.07, 3.61) |
| ≥ 50 | 2193 | 310.7 | 34 661 | 144.3 | 2.15* (2.06, 2.25) | 2281 | 301.7 | 53 745 | 142.0 | 2.13* (2.03, 2.22) |
| Pacific Coast | ||||||||||
| 0–19 | 37 | 3.9 | 757 | 2.2 | 1.77* (1.23, 2.45) | 39 | 3.1 | 1323 | 2.1 | 1.47* (1.04, 2.01) |
| 20–49 | 338 | 26.6 | 6035 | 9.2 | 2.89* (2.58, 3.22) | 452 | 23.9 | 11 788 | 9.6 | 2.50* (2.27, 2.74) |
| ≥ 50 | 977 | 211.9 | 67 953 | 128.4 | 1.65* (1.54, 1.77) | 1314 | 187.2 | 137 627 | 136.7 | 1.37* (1.29, 1.45) |
| East | ||||||||||
| 0–19 | 22 | 5.7 | 876 | 2.5 | 2.24* (1.39, 3.42) | 70 | 3.9 | 7681 | 2.8 | 1.40* (1.09, 1.77) |
| 20–49 | 85 | 17.9 | 6263 | 9.7 | 1.84* (1.47, 2.29) | 328 | 11.8 | 47 120 | 9.3 | 1.27* (1.13, 1.41) |
| ≥ 50 | 306 | 177.2 | 88 965 | 155.8 | 1.14* (1.01, 1.28) | 1158 | 118.2 | 676 687 | 159.7 | 0.74* (0.70, 0.79) |
Note. AI/AN = American Indian/Alaska Native; CHSDA = Contract Health Service Delivery Area; CI = confidence interval; IHS = Indian Health Service; RR = rate ratio. AI/AN race is created using death certificate race and IHS link. Analyses are limited to persons of non-Hispanic origin. Rates are per 100 000 persons and are age-adjusted to the 2000 US standard population. RRs are calculated in SEER*Stat before rounding of rates and may not equal RRs calculated from rates presented in table. Percent of AI/AN persons in CHSDA counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; East = 18.2%; total US = 64.2%.
Source. AI/AN Mortality Database (AMD 1990–2009).
*P < .05.
Leading Causes of Infectious Disease Deaths
Overall, and in most age groups, the average annual death rates for each of the top 10 ID underlying causes of death in AI/AN persons were significantly higher compared with those for Whites (Table 3); these 10 ID causes of death accounted for 94% of all AI/AN and 96% of all White ID deaths. The top 2 causes, lower respiratory tract infection (LRTI) and septicemia, accounted for 61% of all AI/AN infectious disease deaths and 65% of all White ID deaths; LRTI accounted for the highest proportion of ID deaths (Figure 1). The differences in AI/AN death rates compared with the corresponding White rates for ID causes were similar overall and across age groups, with the exception of the rate for tuberculosis, which was 13 times higher for AI/AN persons than that for Whites. Mycoses, which accounted for 2% of AI/AN infectious disease deaths (Figure 1), also showed a high rate disparity.
TABLE 3—
Leading Underlying Causes of Infectious Disease Mortality by Age Group for American Indians/Alaska Natives Compared With Whites of All Ages: Contract Health Service Delivery Area Counties, United States, 1999–2009
| AI/AN |
White |
||||||
| Age/Cause of Death | Rank | Deaths | Rate | Rank | Rate | Deaths | AI/AN:White RR (95% CI) |
| Total | |||||||
| All infectious diseases | . . . | 8429 | 86.2 | . . . | 44.0 | 271 086 | 1.96* (1.91, 2.00) |
| Lower respiratory tract infection | 1 | 3239 | 37.6 | 1 | 20.0 | 125 764 | 1.88* (1.81, 1.95) |
| Septicemia | 2 | 1928 | 19.1 | 2 | 8.4 | 51 592 | 2.27* (2.16, 2.38) |
| Hepatobiliary disease | 3 | 713 | 5.5 | 5 | 2.4 | 14 171 | 2.27* (2.10, 2.46) |
| Kidney, urinary tract, and bladder infection | 4 | 621 | 7.8 | 3 | 4.6 | 29 338 | 1.68* (1.54, 1.82) |
| HIV/AIDS | 5 | 532 | 3.6 | 6 | 2.0 | 10 036 | 1.82* (1.67, 1.99) |
| Infections of the heart | 6 | 307 | 2.9 | 4 | 2.3 | 14 323 | 1.25* (1.10, 1.41) |
| Tuberculosis | 7 | 186 | 2.0 | 15 | 0.1 | 904 | 13.51* (11.36, 15.93) |
| Enteric infection | 8 | 172 | 1.9 | 7 | 1.5 | 9423 | 1.27* (1.07, 1.48) |
| Mycoses | 9 | 135 | 1.1 | 11 | 0.4 | 2096 | 3.22* (2.65, 3.88) |
| Skin and soft tissue infection | 10 | 131 | 1.3 | 8 | 0.6 | 3533 | 2.23* (1.83, 2.68) |
| 0–19 y | |||||||
| All infectious diseases | . . . | 429 | 6.5 | . . . | 2.6 | 3066 | 2.46* (2.22, 2.73) |
| Lower respiratory tract infection | 1 | 171 | 2.6 | 2 | 0.7 | 821 | 3.72* (3.14, 4.39) |
| Selected perinatal infections | 2 | 105 | 1.6 | 1 | 1.0 | 1091 | 1.64* (1.33, 2.00) |
| Septicemia | 3 | 80 | 1.2 | 3 | 0.4 | 498 | 2.87* (2.23, 3.64) |
| Meningitis | 4 | 24 | 0.4 | 4 | 0.2 | 240 | 1.80* (1.13, 2.74) |
| Viral and central nervous system infection | 5 | 12 | 0.2 | 5 | 0.1 | 83 | 2.59* (1.28, 4.77) |
| Mycoses | 6 | NA | 0.1 | 7 | 0.1 | 64 | 2.54* (1.11, 5.13) |
| Abdominal and rectal infection | 7 | NA | 0.1 | 9 | 0.0 | 37 | 3.04* (1.05, 7.26) |
| Kidney, urinary tract, and bladder infection | 8 | NA | 0.1 | 12 | 0.0 | 22 | 4.11* (1.21, 11.13) |
| Enteric infection | 9 | NA | 0.1 | 8 | 0.0 | 45 | 1.94 (0.60, 4.89) |
| Upper respiratory tract infection | 10 | NA | 0.1 | 6 | 0.1 | 71 | 0.99 (0.26, 2.67) |
| 20–49 y | |||||||
| All infectious diseases | . . . | 1820 | 27.3 | . . . | 9.2 | 19 287 | 2.98* (2.84, 3.13) |
| Lower respiratory tract infection | 1 | 451 | 6.7 | 2 | 1.9 | 3990 | 3.54* (3.20, 3.91) |
| HIV/AIDS | 2 | 418 | 6.4 | 1 | 3.3 | 6741 | 1.94* (1.75, 2.14) |
| Septicemia | 3 | 349 | 5.2 | 4 | 1.2 | 2568 | 4.29* (3.82, 4.80) |
| Hepatobiliary disease | 4 | 262 | 4.0 | 3 | 1.4 | 3150 | 2.81* (2.47, 3.19) |
| Infections of the heart | 5 | 86 | 1.3 | 5 | 0.4 | 857 | 3.20* (2.53, 3.99) |
| Kidney, urinary tract, and bladder infection | 6 | 48 | 0.7 | 6 | 0.2 | 445 | 3.35* (2.43, 4.52) |
| Mycoses | 7 | 36 | 0.5 | 9 | 0.1 | 234 | 4.87* (3.32, 6.93) |
| Tuberculosis | 8 | 33 | 0.5 | 15 | 0.0 | 59 | 18.14* (11.44, 28.23) |
| Skin and soft tissue infection | 9 | 30 | 0.5 | 8 | 0.1 | 237 | 4.08* (2.69, 5.97) |
| Abdominal and rectal infection | 10 | 23 | 0.3 | 10 | 0.1 | 199 | 3.62* (2.24, 5.59) |
| ≥ 50 y | |||||||
| All infectious diseases | . . . | 6180 | 261.9 | . . . | 142.1 | 248 733 | 1.84* (1.79, 1.89) |
| Lower respiratory tract infection | 1 | 2617 | 122.9 | 1 | 68.6 | 120 953 | 1.79* (1.72, 1.86) |
| Septicemia | 2 | 1499 | 59.5 | 2 | 28.0 | 48 526 | 2.12* (2.01, 2.24) |
| Kidney, urinary tract, and bladder infection | 3 | 568 | 26.9 | 3 | 16.4 | 28 871 | 1.64* (1.50, 1.79) |
| Hepatobiliary disease | 4 | 450 | 13.4 | 5 | 6.4 | 11 004 | 2.09* (1.89, 2.31) |
| Infections of the heart | 5 | 218 | 8.3 | 4 | 7.7 | 13 435 | 1.08 (0.93, 1.25) |
| Tuberculosis | 6 | 153 | 6.4 | 14 | 0.5 | 839 | 13.24* (10.99, 15.85) |
| Enteric infection | 7 | 147 | 6.3 | 6 | 5.3 | 9257 | 1.19 (1.00, 1.41) |
| HIV/AIDS | 8 | 111 | 2.9 | 8 | 1.9 | 3266 | 1.51* (1.23, 1.84) |
| Skin and soft tissue infection | 9 | 100 | 3.9 | 7 | 1.9 | 3292 | 2.05* (1.64, 2.53) |
| Mycoses | 10 | 90 | 3.1 | 11 | 1.1 | 1798 | 2.99* (2.35, 3.74) |
Note. AI/AN = American Indian/Alaska Native; CHSDA = Contract Health Service Delivery Areas; CI = confidence interval; IHS = Indian Health Service; RR = rate ratio. NA indicates that counts less than 10 were suppressed; if no cases reported, then rates and RRs could not be calculated. AI/AN race is created using death certificate race and IHS link. Analyses are limited to persons of non-Hispanic origin. Cause of death based on the International Classification of Diseases, 10th Revision.18 Rank is based on number of deaths. Rates are per 100 000 persons and are age-adjusted to the 2000 US standard population. RRs are calculated in SEER*Stat before rounding of rates and may not equal RRs calculated from rates presented in table. Percent of AI/AN in CHSDA counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; East = 18.2%; Total United States = 64.2%.
Source. AI/AN Mortality Database (AMD 1990–2009).
*P < .05.
FIGURE 1—
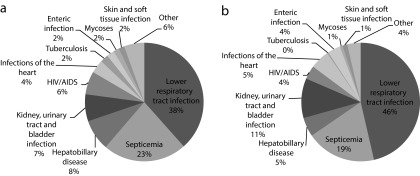
Leading 10 infectious death groups as proportion of total infectious disease deaths for (a) American Indians/Alaska Natives and (b) Whites: Contract Health Service Delivery Area Counties, United States, 1999–2009.
Note. AI/AN = American Indian/Alaska Native; CHSDA = Contract Health Service Delivery Area. AI/AN race is created using death certificate race and Indian Health Service Link. Percentage of AI/AN in CHSDA counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; East = 18.2%; total US = 64.2%.
Source. AI/AN Mortality Database (AMD 1990–2009). Analyses are limited to persons of non-Hispanic origin.
Five percent of all AI/AN infectious disease deaths were among the 0 to 19 years age group, in which LRTI was the leading cause of ID death for AI/AN persons and the second leading ID cause for Whites (Table 3). One of the greatest rate disparities between the 2 populations was for LRTIs. The AI/AN average annual death rates were higher than the rates in Whites among all AI/AN top causes of ID deaths in the 0 to 19 years age group, except for enteric infections and upper respiratory infections, which showed no rate differences.
Twenty-two percent of all AI/AN infectious disease deaths were among the 20 to 49 years age group, in which LRTI and HIV/AIDS were the leading ID causes of death for AI/ANs (25% and 23%, respectively) and Whites (21% and 35%, respectively; Table 3). The average annual death rates of all leading causes of death were significantly higher in AI/AN persons than those for Whites in this age group. The greatest rate disparity between AI/AN and White persons was for tuberculosis deaths, which accounted for 2% of AI/AN deaths in this age group.
The majority of AI/AN infectious disease deaths (73%) occurred among the 50 years and older age group (Table 3). Although the rate disparities were not as great in this age group as those in the other age groups, the AI/AN death rates were significantly higher than those for Whites across all most common causes, with the exception of infections of the heart. Tuberculosis rates showed the greatest rate disparity and accounted for 3% of all AI/AN infectious disease deaths in this age group.
DISCUSSION
We showed significantly higher average annual age-adjusted ID death rates from 1999 to 2009 among AI/AN persons compared with those for Whites. We presented disparities in overall ID and ID group death rates by sex, age group, and region. Although ID death rates were significantly higher for AI/ANs than those for Whites, there were similar ID mortality patterns among the 2 groups, such as higher rates in males and in older age groups. In addition, the leading ID causes of death, LRTI and septicemia, ranked first and second for both AI/ANs and Whites, a finding consistent with previous studies of ID hospitalizations among AI/ANs.7,9,31
In terms of health disparities, the greatest rate disparities in overall ID death rates generally occurred in the AI/AN population that was 50 years old and older in the Alaska, Southwest, and Northern Plains regions. This pattern in ID death rates was consistent with disparities seen in ID hospitalization rates and appeared to be linked with high LRTI rates in AI/AN persons, as shown in other studies.10,32–34 The LRTI group accounted for the highest proportion of deaths among AI/AN and White persons. The greatest rate disparities were for tuberculosis and mycoses, although these causes accounted for relatively few deaths. Rates for tuberculosis were much higher among AI/AN persons, since first recorded in the 1950s, leading to a legacy of many AI/AN elders with latent tuberculosis infection.35 Recent clusters of tuberculosis among AI/AN persons were traced to being spread by middle-aged individuals who often are homeless and alcohol-dependent.36 Relatively little tuberculosis in this group was associated with HIV infection.37 Although HIV in the 20 to 49 years age group was the leading cause of death in Whites and the second leading cause of death in AI/AN person, the disparity in HIV rates was the smallest in the top 10 leading causes of death for this age group. Although we did not examine infant (< 1 year of age) ID mortality rates, examination of infant ID mortality is highly warranted because AI/AN infants have been described as having very high ID mortality and morbidity rates.8 In this supplement, Wong et al.38 specifically address AI/AN infant and pediatric mortality.
Several causes of death continue to drive the disparities in ID death rates between AI/AN and White populations. Some higher ID death rates might be because of historically higher ID rates that continue to manifest as incident cases among younger generations, as might be the situation with tuberculosis.35 By contrast with other minority populations in the United States, access to affordable care might not play as important a role for the AI/AN populations described in this study because of the health care coverage provided through the IHS. For example, AI/AN persons were the racial group in the United States most likely to receive primarily directly observed therapy for tuberculosis, presumably because of coordination of care by IHS.34 Many urban AI/AN individuals who are not enrolled in the IHS, however, might experience significant difficulties accessing care.39 A more likely economic factor contributing to reduced access to health care among AI/AN persons who benefit from IHS was the remoteness and isolation of homes of many AI/AN persons living on or near tribal reservations. In addition, AI/AN individuals who are IHS beneficiaries but live in urban locations that are not included in their tribe’s CHSDA were not eligible to receive contract health care through IHS. As a result, they might have limited access to care for financial reasons, similar to nonenrolled urban AI/AN persons.17,40 Some of the greatest ID death rate disparities were found in some of the most remote and isolated regions of the United States, namely, the Alaska, Northern Plains, and Southwest regions, which supported our hypothesis that remoteness and isolation were important factors, and was similar to other studies. 9–11,33 Another contributing factor, particularly in these regions, might be the lack of adequate sanitation, including in-home water service, which was found to be associated with increased ID hospitalization rates, including respiratory and skin infections rates in Alaska.41 The IHS regions with the largest proportion of homes without adequate water and sewage treatment are the Alaska and Southwest regions.42
Study Limitations
Our limitations in the present study included the use of ICD codes to determine ID causes of death and the uncorrected racial misclassification of AI/ANs. The problems of using ICD codes to determine ID causes of death were previously described, although using the underlying cause of death in our study provided a conservative approach to selection of ID deaths.2,12 As for the problem of AI/AN racial misclassification, our study provided the least biased view of AI/AN infectious disease mortality to date because we used mortality data with corrected misclassified AI/AN race from information in the IHS patient registration database. Such linkage, however, corrected only for persons listed in the IHS patient registration database, which contained roughly half of all self-reported AI/AN persons from the US census.14 Furthermore, IHS and tribes only provided health care to members of the 566 federally recognized tribes.16 AI/AN individuals were not included in the IHS/tribal health care system if they were members of the 64 tribes that are not federally recognized.43 Of the regions examined, the East had the smallest population served by IHS, and as a result, had the fewest AI/AN persons identified through the linkage process and correctly classified using this method.20 Uncorrected misclassification might account for some of that region’s characteristics, such as the lower overall average annual death rate compared with Whites. Finally, although the exclusion of Hispanic AI/AN individuals from the analyses reduced the overall count of deaths among AI/AN persons by less than 5%, it might have disproportionately affected some states along the US–Mexico border and elsewhere.
Conclusions
Although much progress has been made since the 1950s, many significant disparities remain for ID causes of death among AI/AN populations. Many of these ID death rates, in particular, rates of LRTIs and sepsis, might improve over time as living conditions improve and more AI/AN persons acquire modern water and sewer treatment, as well as improved transportation. In many ways, the continued lack of basic sanitation and transportation in some AI/AN communities and households harks back to the observation made in 1957 regarding AI/AN communities of the day that appeared to be unchanged from 1900.5 Implementation of the improvements thought to be responsible for the bulk of the reduction in ID mortality in the United States between 1900 and 1980, such as improved sanitation, use of immunizations, and prompt access to antimicrobial therapy, might lead to similar substantial reductions in ID mortality among this population. Based on the ID death rate differences observed in our study, if health equity had been achieved with Whites, almost half of the AI/AN infectious disease deaths might have been avoided between 1999 and 2009. Rapid and dramatic improvements in AI/AN infectious disease rates are possible, as seen with the tremendous decline in cases of hepatitis A among AI/AN persons.44,45 Rates of hepatitis A infection in AI/AN persons from Centers for Disease Control and Prevention surveillance in the 1980s were approximately 8-fold higher than the overall US population, but since the implementation of hepatitis A immunization in the 1990s, AI/ANs rates have fallen below the rates for the overall US population. Further studies of ID mortality and morbidity among AI/AN persons are needed to monitor trends, and to identify high-risk groups and diseases for specific intervention strategies. This would include analyses to investigate the burden of IDs among children, especially infants. Health equity might be achieved by supporting and sustaining expansion of proven methods and the development of new interventions to reduce IDs among AI/AN communities.
Acknowledgments
We would like to thank David Espey and Melissa Jim for their technical contributions to this study.
Human Participant Protection
This project was determined to be exempt from institutional review board approval as determined by the CDC and IHS institutional review boards.
References
- 1.Omran AR. The epidemiologic transition. A theory of the epidemiology of population change. Milbank Mem Fund Q. 1971;49(4):509–538. [PubMed] [Google Scholar]
- 2.Armstrong GL, Conn LA, Pinner RW. Trends in infectious disease mortality in the United States during the 20th century. JAMA. 1999;281(1):61–66. doi: 10.1001/jama.281.1.61. [DOI] [PubMed] [Google Scholar]
- 3.Christensen KL, Holman RC, Steiner CA, Sejvar JJ, Stoll BJ, Schonberger LB. Infectious disease hospitalizations in the United States. Clin Infect Dis. 2009;49(7):1025–1035. doi: 10.1086/605562. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Deaths related to 2009 pandemic influenza A (H1N1) among American Indian/Alaska Natives—12 states, 2009. MMWR Morb Mortal Wkly Rep. 2009;58(48):1341–1344. [PubMed] [Google Scholar]
- 5.US Public Health Service Office of the Surgeon General. Health Services for American Indians. Washington, DC: PHS Publications; 1957. [Google Scholar]
- 6.Ciocco A, Crabtree JA, McNerney WJ . Alaska’s Health: A Survey Report to the United States Department of the Interior. Pittsburgh, PA: Graduate School of Public Health, University of Pittsburgh; 1954. [Google Scholar]
- 7.Holman RC, Curns AT, Kaufman SF, Cheek JE, Pinner RW, Schonberger LB. Trends in infectious disease hospitalizations among American Indians and Alaska Natives. Am J Public Health. 2001;91(3):425–431. doi: 10.2105/ajph.91.3.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holman RC, Curns AT, Cheek JE, Singleton RJ, Anderson LJ, Pinner RW. Infectious disease hospitalizations among American Indian and Alaska native infants. Pediatrics. 2003;111(2):E176–E182. doi: 10.1542/peds.111.2.e176. [DOI] [PubMed] [Google Scholar]
- 9.Holman RC, Folkema AM, Singleton RJ et al. Disparities in infectious disease hospitalizations for American Indian/Alaska Native people. Public Health Rep. 2011;126(4):508–521. doi: 10.1177/003335491112600407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singleton RJ, Holman RC, Folkema AM, Wenger JD, Steiner CA, Redd JT. Trends in lower respiratory tract infection hospitalizations among American Indian/Alaska Native children and the general US child population. J Pediatr. 2012;161(2):296–302.e2. doi: 10.1016/j.jpeds.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 11.Holman RC, Hennessy TW, Haberling DL et al. Increasing trend in the rate of infectious disease hospitalisation among Alaska Native people. Int J Circumpolar Health. 2013;Aug;5:72. doi: 10.3402/ijch.v72i0.20994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pinner RW, Teutsch SM, Simonsen L et al. Trends in infectious diseases mortality in the United States. JAMA. 1996;275(3):189–193. [PubMed] [Google Scholar]
- 13.Arias E, Eschbach K, Schauman WS, Backlund EL, Sorlie PD. The Hispanic mortality advantage and ethnic misclassification on US death certificates. Am J Public Health. 2010;100(suppl 1):S171–S177. doi: 10.2105/AJPH.2008.135863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jim MA, Arias E, Seneca DS et al. Racial misclassification of American Indians and Alaska Natives by Indian Health Service Contract Health Service Delivery Area. Am J Public Health. 2014;104(6 suppl 3):S295–S302. doi: 10.2105/AJPH.2014.301933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thoroughman DA, Frederickson D, Cameron HD, Shelby LK, Cheek JE. Racial misclassification of American Indians in Oklahoma State surveillance data for sexually transmitted diseases. Am J Epidemiol. 2002;155(12):1137–1141. doi: 10.1093/aje/155.12.1137. [DOI] [PubMed] [Google Scholar]
- 16.Black MS. Indian entities recognized and eligible to receive services from the Bureau of Indian Affairs. Federal Register. 2012:47868–47873. [Google Scholar]
- 17.Espey DK, Jim MA, Richards T, Begay C, Haverkamp D, Roberts D. Methods for improving the quality and completeness of mortality data for American Indians and Alaska Natives. Am J Public Health. 2014;104(6 suppl 3):S286–S294. doi: 10.2105/AJPH.2013.301716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.International Statistical Classification of Diseases and Related Health Problems. 10th ed. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 19.Arias E, Schauman W, Eschbach K, Sorlie P. The validity of race and Hispanic origin reporting on death certificates in the United States. Vital Health Stat 2. 2008;148:1–23. [PubMed] [Google Scholar]
- 20. Indian Health Service Areas. 2012. Available at: http://www.ihs.gov/index.cfm?module=AreaOffices. Accessed April 2, 2012.
- 21.Denny CH, Taylor TL. American Indian and Alaska Native health behavior: findings from the Behavioral Risk Factor Surveillance System, 1992–1995. Ethn Dis. 1999;9(3):403–409. [PubMed] [Google Scholar]
- 22.Wiggins CL, Espey DK, Wingo PA et al. Cancer among American Indians and Alaska Natives in the United States, 1999–2004. Cancer. 2008;113(5 suppl):1142–1152. doi: 10.1002/cncr.23734. [DOI] [PubMed] [Google Scholar]
- 23.Espey D, Paisano R, Cobb N. Regional patterns and trends in cancer mortality among American Indians and Alaska Natives, 1990–2001. Cancer. 2005;103(5):1045–1053. doi: 10.1002/cncr.20876. [DOI] [PubMed] [Google Scholar]
- 24. Indian Health Service Areas. Indian Health Service, 2012. Available at: http://www.ihs.gov/aboutihs/organizationalstructure. Accessed April 2, 2012.
- 25. National Vital Statistics System. US census populations with bridged race categories. 2013. Available at: http://www.cdc.gov/nchs/nvss/bridged_race.htm. Accessed March 13, 2013.
- 26. National Cancer Institute. Adjusted populations for the counties/parishes affected by Hurricanes Katrina and Rita. 2012. Available at: http://seer.cancer.gov/popdata/hurricane_adj.html. Accessed March 18, 2013.
- 27.Bethesda, MD: National Cancer Institute; 2013. SEER*Stat Software. Version 8.0.2. [Google Scholar]
- 28.Tiwari RC, Clegg LX, Zou Z. Efficient interval estimation for age-adjusted cancer rates. Stat Methods Med Res. 2006;15(6):547–569. doi: 10.1177/0962280206070621. [DOI] [PubMed] [Google Scholar]
- 29.Edwards BK, Noone AM, Mariotto AB et al. Annual report to the nation on the status of cancer, 1975–2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. 2013 doi: 10.1002/cncr.28509. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. National Cancer Institute. 2000 US Standard Population—19 Age Groups. Available at: http://seer.cancer.gov/stdpopulations/stdpop.19ages.html. Accessed March 8, 2014.
- 31.Armstrong GL, Pinner RW. Outpatient visits for infectious diseases in the United States, 1980 through 1996. Arch Intern Med. 1999;159(21):2531–2536. doi: 10.1001/archinte.159.21.2531. [DOI] [PubMed] [Google Scholar]
- 32.Groom AV, Hennessy TW, Singleton RJ, Butler JC, Holve S, Cheek JE. Pneumonia and influenza mortality among American Indian and Alaska Native People, 1990–2009. Am J Public Health. 2014;104(6 suppl 3):S460–S469. doi: 10.2105/AJPH.2013.301740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singleton RJ, Wirsing EA, Haberling DL et al. Risk factors for lower respiratory tract infection death among infants in the United States, 1999–2004. Pediatrics. 2009;124(4):e768–e776. doi: 10.1542/peds.2009-0109. [DOI] [PubMed] [Google Scholar]
- 34.Peck AJ, Holman RC, Curns AT et al. Lower respiratory tract infections among American Indian and Alaska Native children and the general population of US children. Pediatr Infect Dis J. 2005;24(4):342–351. doi: 10.1097/01.inf.0000157250.95880.91. [DOI] [PubMed] [Google Scholar]
- 35.Bloss E, Holtz TH, Jereb J et al. Tuberculosis in indigenous peoples in the US, 2003–2008. Public Health Rep. 2011;126(5):677–689. doi: 10.1177/003335491112600510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention. Tuberculosis outbreak on an American Indian reservation–Montana, 2000–2001. MMWR Morb Mortal Wkly Rep. 2002;51(11):232–234. [PubMed] [Google Scholar]
- 37.Reilley B, Bloss E, Byrd KK, Iralu J, Neel L, Cheek J. Death rates from human immunodeficiency virus and tuberculosis among American Indians/Alaska Natives in the United States, 1990–2009. Am J Public Health. 2014;104(6 suppl 3):S453–S459. doi: 10.2105/AJPH.2013.301746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wong CA, Gachupin FC, Holman RC et al. American Indian and Alaska Native infant and pediatric mortality, United States, 1999–2009. Am J Public Health. 2014;104(6 suppl 3):S320–S328. doi: 10.2105/AJPH.2013.301598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Castor ML, Smyser MS, Taualii MM, Park AN, Lawson SA, Forquera RA. A nationwide population-based study identifying health disparities between American Indians/Alaska Natives and the general populations living in select urban counties. Am J Public Health. 2006;96(8):1478–1484. doi: 10.2105/AJPH.2004.053942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Urban Indian Health Commission. Invisible Tribes: Urban Indians and Their Health in a Changing World. Seattle, WA: Urban Indian Health Commission; 2007. [Google Scholar]
- 41.Hennessy TW, Ritter T, Holman RC et al. The relationship between in-home water service and the risk of respiratory tract, skin, and gastrointestinal tract infections among rural Alaska natives. Am J Public Health. 2008;98(11):2072–2078. doi: 10.2105/AJPH.2007.115618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rogers CL. The Sanitation Facilities Construction Program of the Indian Health Service-Public Law 86-121 Annual Report for 2010. Rockville, MD: Indian Health Service; 2010. [Google Scholar]
- 43. Federally and State Recognized Tribes. National Conference of State Legislatures, 2013. Available at: http://www.ncsl.org/research/state-tribal-institute/list-of-federal-and-state-recognized-tribes.aspx. Accessed March 8, 2014.
- 44.Bialek SR, Thoroughman DA, Hu D et al. Hepatitis A incidence and hepatitis A vaccination among American Indians and Alaska Natives, 1990–2001. Am J Public Health. 2004;94(6):996–1001. doi: 10.2105/ajph.94.6.996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Byrd KK, Redd JT, Holman RC, Haberling DL, Cheek JE. Changing trends in viral hepatitis-associated hospitalizations in the American Indian/Alaska Native population, 1995–2007. Public Health Rep. 2011;126:816–825. doi: 10.1177/003335491112600607. [DOI] [PMC free article] [PubMed] [Google Scholar]


