Abstract
Objectives. We describe rates and trends in kidney cancer incidence and mortality and identify disparities between American Indian/Alaska Native (AI/AN) and White populations.
Methods. To improve identification of AI/AN race, incidence and mortality data were linked with Indian Health Service (IHS) patient records. Analysis focused on residents of IHS Contract Health Service Delivery Area counties; Hispanics were excluded. We calculated age-adjusted kidney cancer incidence (2001–2009) and death rates (1990–2009) by sex, age, and IHS region.
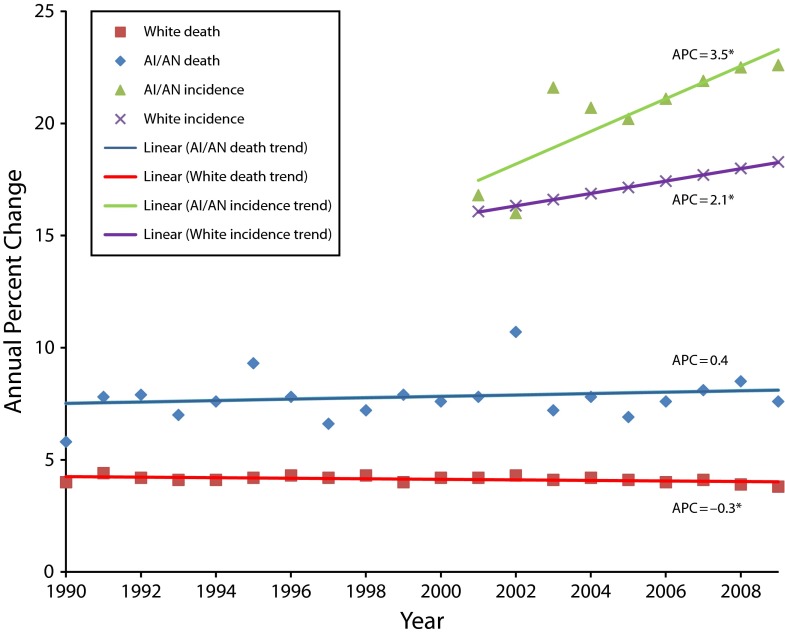
Results. AI/AN persons have a 1.6 times higher kidney cancer incidence and a 1.9 times higher kidney cancer death rate than Whites. Despite a significant decline in kidney cancer death rates for Whites (annual percentage change [APC] = −0.3; 95% confidence interval [CI] = −0.5, 0.0), death rates for AI/AN persons remained stable (APC = 0.4; 95% CI = −0.7, 1.5). Kidney cancer incidence rates rose more rapidly for AI/AN persons (APC = 3.5; 95% CI = 1.2, 5.8) than for Whites (APC = 2.1; 95% CI = 1.4, 2.8).
Conclusions. AI/AN individuals have greater risk of developing and dying of kidney cancers. Incidence rates have increased faster in AI/AN populations than in Whites. Death rates have decreased slightly in Whites but remained stable in AI/AN populations. Racial disparities in kidney cancer are widening.
More than 80% of kidney cancers arise in the renal parenchyma, primarily renal cell carcinoma (RCC), and the remainder originate from the renal pelvis, called renal transitional cell carcinoma (RTCC) or urothelial carcinoma (UC).1 An assessment of Surveillance, Epidemiology, and End Results (SEER) program data revealed that incidence rates of RCC and death rates for kidney cancer increased from 1975 to 1995.2 Recent studies have shown that kidney cancer incidence has continued to increase in the United States for all racial/ethnic groups.3,4 Kidney cancer is an important public health issue for American Indians and Alaska Natives (AI/ANs), ranking among the top 5 cancers for both incidence and mortality.3,5 AI/AN persons are at greater risk for developing and dying of kidney cancers than other racial/ethnic groups.3,5,6
Data on AI/AN persons have not been presented in many population-based studies of kidney cancer2,7,8,9 because sample sizes were too small, even in surveillance systems that collect cancer incidence and mortality for the US population. Available information in the literature that describes demographic and geographic attributes of kidney cancer among AI/AN populations needs to be updated.5,10,11
Accurate cancer incidence and death rates play an important role in identifying areas for etiologic research, prioritizing cancer control resources, and developing cancer control and prevention approaches. Race misclassification of AI/AN cancer cases and deaths, resulting in underestimates of the true cancer burden in this population, is another recognized issue.12–15 To minimize the misclassification of race, the Indian Health Service (IHS) patient registration database was linked to data from the National Death Index, providing an excellent opportunity to generate more accurate cancer mortality statistics for AI/ANs. A previous linkage between IHS patient files and cancer registry data provided more accurate estimations of AI/AN cancer incidence; we present updated results.5,11,12 The purpose of this article was to describe kidney cancer burden in AI/AN populations and characterize racial disparity by demographic, geographic, and temporal factors using Whites as a reference group.
METHODS
Detailed methods for generating the analytic mortality (AI/AN Mortality Database, 1990–2009) and incidence files are described elsewhere.16,17
Data Sources
Population estimates.
Bridged single-race population estimates developed by the US Census Bureau and the Centers for Disease Control and Prevention’s National Center for Health Statistics and adjusted for the population shifts resulting from Hurricanes Katrina and Rita in 2005 were included as denominators in the calculation of death rates.16,18 Bridged single-race data allow for a smoothing of population counts between the single AI/AN race category of the 1990 Census and the 2000 Census expansion to multiple race categories.
During preliminary analyses, it was discovered that the updated bridged intercensal population estimates significantly overestimated AI/AN persons of Hispanic origin.19 Therefore, to avoid underestimating AI/AN deaths because of overinflated denominators, analyses were limited to non-Hispanic AI/AN persons. Fewer than 5% of cancer cases and deaths were identified as Hispanic AI/AN persons and were excluded from the analysis. Non-Hispanic White was chosen as the most homogeneous referent group. Therefore, all analyses are limited to non-Hispanic persons; henceforth, the term “non-Hispanic” is omitted when discussing both groups.
Death data.
Death certificate data are compiled by each state. These data are sent to the National Center for Health Statistics, where they are edited for consistency, stripped of personal identifiers, and made available to the general public as part of the National Vital Statistics System.19,20 The National Center for Health Statistics applies a bridging algorithm nearly identical to that used by the Census Bureau to assign a single race to decedents with multiple races reported on the death certificate.20,21
The IHS patient registration database was linked to the National Death Index, a tool that allows researchers to link their data with the mortality data in the National Vital Statistics System to identify AI/AN deaths that had been misclassified as non-Native AI/AN deaths and to determine vital status and cause of death of decedents who had received health care in IHS or tribal facilities.16 About 62% of AI/AN populations have obtained IHS services and are included in the IHS patient registration database.21,22 After the linkage of IHS records to the National Death Index, a flag indicating a positive link to IHS was added to the National Vital Statistics System mortality file as an additional indicator of AI/AN ancestry. This file was then combined with the census population estimates to create an analytic file in SEER*Stat (National Cancer Institute, Bethesda, MD; AI/AN Mortality Database) that includes all deaths for all races from 1990 to 2009. Race for AI/AN deaths combines race classification by the National Center for Health Statistics on the basis of the death certificate and information derived from data linkages between the IHS patient registration database and the National Death Index.16
For 1990 to 1998, the underlying cause of death was coded according to the International Classification of Diseases, Ninth Revision (ICD-9; code 189, for deaths resulting from kidney cancer).23 For 1999 to 2009, the International Classification of Diseases, 10th Revision (ICD-10) was used (codes C64 and C65, for deaths resulting from kidney cancer, including renal pelvis).24,25 Trend analyses spanning ICD-9 and ICD-10 reporting years took into account comparability of cause-of-death recodes between the 2 revisions.25 For this study, we excluded the following states and years of data because Hispanic origin was not collected on the death certificate: Louisiana, 1990; New Hampshire, 1990 to 1992; and Oklahoma, 1990 to 1996.
Incidence data.
We identified AI/AN incident kidney cancers diagnosed from 2001 to 2009 from the population-based, central cancer registries that participate in the Centers for Disease Control and Prevention’s National Program of Cancer Registries (NPCR) or the National Cancer Institute’s SEER Program. We excluded the following states and years of data because either data were not collected or US Cancer Statistics publication standards (http://www.cdc.gov/cancer/npcr/uscs) were not met: Mississippi, 2001 to 2002; Tennessee, 2001 to 2002; Virginia, 2001; District of Columbia, 2002; and Wisconsin, 2009. Cancer registries coded primary cancer site and histology according to criteria in the third edition of the International Classification of Diseases for Oncology.26 Initially, we identified 2339 AI/AN kidney cancers using primary site code C64.9 for kidney parenchyma and C65.9 for renal pelvis. We further excluded autopsy or death-certificate-only cases (n = 31) and nonmicroscopically confirmed cases (n = 220). Subsequently, we classified RCC (n = 1974) and RTCC/UC (n = 47) on the basis of the following histology codes: 8140–8575 for RCC and 8052–8130 for RTCC/UC. We did, however, not present data for RTCC/UC as a result of a small number of cases.
Geographic Coverage
To receive care from the IHS, an AI/AN individual must be a member of a federally recognized tribe or AN village and must reside on or near a reservation.15 Contract Health Service Delivery Area (CHSDA) counties are designated by the IHS and consist of 637 counties that, in general, contain or are adjacent to federally recognized tribal lands.16 Evidence has shown that misclassifications of AI/AN persons occur less often in CHSDA counties than in non-CHSDA counties.16,27 Thus, to create most of the tabulations in this article, we restricted the analyses to CHSDA counties, grouped as IHS regions: Northern Plains, Alaska, Southern Plains, Southwest, Pacific Coast, and East. Additional details about CHSDA counties and IHS regions, including population coverage, are provided elsewhere (Table 1).16 Although less geographically representative, we present analyses restricted to CHSDA counties in this article for the purpose of offering improved accuracy in interpreting statistics for AI/AN populations.
TABLE 1—
Kidney Cancer Deaths by IHS Region and Sex for AI/AN Populations and Whites: United States, 1990–2009
| CHSDA |
All Counties |
|||||||||
| IHS Region/Sex | AI/AN Count | AI/AN Rate | White Count | White Rate | AI/AN:White, RR (95% CI) | AI/AN Count | AI/AN Rate | White Count | White Rate | AI/AN: White RR (95% CI) |
| Northern Plains | ||||||||||
| Total | 233 | 9.3 | 7772 | 4.5 | 2.06* (1.78, 2.37) | 305 | 7.7 | 38 103 | 4.6 | 1.69* (1.49, 1.91) |
| Male | 145 | 13.1 | 4795 | 6.4 | 2.06* (1.70, 2.47) | 185 | 10.8 | 23 203 | 6.5 | 1.66* (1.39, 1.95) |
| Female | 88 | 6.3 | 2977 | 3.0 | 2.09* (1.65, 2.60) | 120 | 5.4 | 14 900 | 3.1 | 1.75* (1.43, 2.12) |
| Alaska | ||||||||||
| Total | 96 | 9.8 | 209 | 3.9 | 2.54* (1.94, 3.29) | 96 | 9.8 | 209 | 3.9 | 2.54* (1.94, 3.29) |
| Male | 56 | 12.2 | 149 | 5.6 | 2.17* (1.51, 3.06) | 56 | 12.2 | 149 | 5.6 | 2.17* (1.51, 3.06) |
| Female | 40 | 7.7 | 60 | 2.3 | 3.36* (2.16, 5.16) | 40 | 7.7 | 60 | 2.3 | 3.36* (2.16, 5.16) |
| Southern Plains | ||||||||||
| Total | 272 | 9.2 | 2318 | 4.8 | 1.91* (1.67, 2.17) | 319 | 7.7 | 15 467 | 4.6 | 1.65* (1.47, 1.86) |
| Male | 181 | 13.7 | 1434 | 6.8 | 2.01* (1.70, 2.38) | 217 | 11.7 | 9668 | 6.7 | 1.75* (1.49, 2.03) |
| Female | 91 | 5.7 | 884 | 3.3 | 1.75* (1.39, 2.18) | 102 | 4.6 | 5799 | 3.1 | 1.50* (1.21, 1.83) |
| Southwest | ||||||||||
| Total | 389 | 8.0 | 5196 | 3.7 | 2.16* (1.94, 2.40) | 399 | 7.6 | 8335 | 3.7 | 2.06* (1.85, 2.28) |
| Male | 242 | 11.3 | 3342 | 5.2 | 2.17* (1.88, 2.49) | 250 | 10.8 | 5343 | 5.3 | 2.05* (1.78, 2.34) |
| Female | 147 | 5.4 | 1854 | 2.4 | 2.25* (1.88, 2.67) | 149 | 5.1 | 2992 | 2.4 | 2.13* (1.79, 2.53) |
| Pacific Coast | ||||||||||
| Total | 166 | 5.5 | 12 658 | 4.1 | 1.35* (1.14, 1.59) | 233 | 5.0 | 23 493 | 4.0 | 1.25* (1.08, 1.43) |
| Male | 93 | 7.2 | 8009 | 5.9 | 1.23 (0.96, 1.54) | 140 | 6.9 | 14 828 | 5.7 | 1.21 (0.99, 1.46) |
| Female | 73 | 4.4 | 4649 | 2.7 | 1.63* (1.26, 2.07) | 93 | 3.6 | 8665 | 2.6 | 1.37* (1.09, 1.69) |
| East | ||||||||||
| Total | 59 | 5.1 | 13 800 | 4.1 | 1.24 (0.93, 1.62) | 210 | 3.1 | 107 006 | 4.2 | 0.74 (0.64, 0.86) |
| Male | 34 | 6.5 | 8543 | 6.0 | 1.08 (0.71, 1.56) | 133 | 4.4 | 65 932 | 6.1 | 0.72 (0.59, 0.88) |
| Female | 25 | 4.0 | 5257 | 2.7 | 1.49 (0.95, 2.21) | 77 | 2.1 | 41 074 | 2.8 | 0.76 (0.59, 0.96) |
| Total | 1215 | 7.8 | 41 953 | 4.1 | 1.88* (1.77, 2.00) | 1562 | 6.1 | 192 613 | 4.3 | 1.43* (1.35, 1.50) |
| Male | 751 | 10.9 | 26 272 | 5.9 | 1.83* (1.69, 1.98) | 981 | 8.7 | 119 123 | 6.1 | 1.41* (1.31, 1.51) |
| Female | 464 | 5.4 | 15 681 | 2.7 | 1.99* (1.81, 2.19) | 581 | 4.1 | 73 490 | 2.8 | 1.46* (1.34, 1.59) |
Note. AI/AN = American Indian/Alaska Native; CHSDA = Contract Health Service Delivery Area; CI = confidence interval; IHS = Indian Health Service; RR = rate ratio. Analyses are limited to persons of non-Hispanic origin. AI/AN race is reported by death certificates, or through linkage with the IHS patient registration database. Rates are per 100 000 persons and were age adjusted to the 2000 US standard population (11 age groups; Census P25-113028). RRs were calculated in SEER*Stat before rounding of rates and may not equal to RRs calculated from rates presented in the table. The following states and years of data were excluded because Hispanic origin was not collected on the death certificate: LA, 1990; NH, 1990–1992; and OK, 1990–1996. IHS regions are defined as follows: AKa; Northern Plains (IL, IN,a IA,a MI,a MN,a MT,a NE,a ND,a SD,a WI,a WYa); Southern Plains (OK,a KS,a TXa); Southwest (AZ,a CO,a NV,a NM,a UTa); Pacific Coast (CA,a ID,a OR,a WA,a HI); and East (AL,a AR, CT,a DE, FL,a GA, KY, LA,a ME,a MD, MA,a MS,a MO, NH, NJ, NY,a NC,a OH, PA,a RI,a SC,a TN, VT, VA, WV, DC).
Source. AI/AN Mortality Database (1990–2009).
Identifies states with ≥ 1 county designated as CHSDA. Percentage regional coverage of AI/AN in CHSDA counties to AI/AN in all counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; East = 18.2%; total United States = 64.2%.
*P < .05.
Statistical Analyses
We calculated kidney cancer death and incidence rates for AI/AN persons by sex, age, and IHS region. To be comparable with previously published results, we categorized age as 20 to 49 years and 50 years and older.11 We also estimated RCC incidence rates by sex and age. All rates are expressed per 100 000 population and were directly age adjusted to the 2000 US standard population (19 age groups Census P25-1130).28 Death rates were directly age adjusted to the 2000 US standard population (11 age groups; Census P25-1130).28 Readers should avoid comparison of these data with published incidence and death rates adjusted using a different standard population. For confidentiality and stability, rates were not reported if the numerator was fewer than 10 cases. We calculated standardized rate ratios (RRs) for the AI/AN population using White rates for comparison. Confidence intervals (CIs) for age-adjusted rates and RRs were calculated on the basis of methods described by Tiwari et al.29
We assessed temporal changes in annual age-adjusted death rates from 1990 to 2009, including the annual percentage change (APC) for each interval, with Joinpoint regression software, version 3.5.4 (National Cancer Institute, Bethesda, MD).30 As many as 3 joinpoints were allowed in the model. Statistical significance was set at a P level of less than .05. As a result of short-term trends of kidney cancer and RCC (2001–2009), we estimated APCs of fixed-interval trend by fitting a straight line to 9 years of data.
RESULTS
From 1990 to 2009, 1215 deaths resulted from kidney cancer among AI/AN persons in CHSDA counties and 1562 total deaths among AI/AN persons in all US counties (Table 1). The overall death rate for AI/AN persons in CHSDA counties was 7.8, higher than the rate for AI/AN persons in all counties combined, which was 6.1. All remaining results about death rates refer to CHSDA counties only. We found that death rates from kidney cancer for AI/AN individuals varied by IHS region: Alaska had the highest death rate (9.8), followed by the Northern Plains (9.3) and Southern Plains (9.2), with the lowest rate in the East (5.1). Compared with Whites, AI/AN individuals had statistically significantly higher kidney cancer death rates for all IHS regions with the exception of the East. AI/AN men had (10.9) almost twice the rate of AI/AN women (5.4).
Table 2 shows that AI/AN adults aged 50 years and older had a much higher death rate (26.2) than AI/AN adults aged 20 to 49 years (1.4). Compared with Whites in the same age group, AI/AN persons had significantly higher death rates: 1.89 times that of the 50 years and older age group and 2.19 times that of the 20 to 49 age group. These patterns held true for each IHS region in which RRs could be calculated, except for the Pacific Coast region, which had a ratio of 1.6.
TABLE 2—
Kidney Cancer Deaths by IHS Region and Age for AI/AN Populations and Whites in CHSDA Counties: United States, 1990–2009
| AI/AN |
White |
||||
| IHS Region/Age, Years | Count | Rate (95% CI) | Count | Rate (95% CI) | AI/AN:White, RR (95% CI) |
| Northern Plains | |||||
| 20–49 | 23 | 1.4 (0.9, 2.0) | 438 | 0.7 (0.6, 0.7) | 2.04* (1.28, 3.09) |
| ≥ 50 | 208 | 31.6* (27.2, 36.5) | 7297 | 15.1 (14.8, 15.5) | 2.09* (1.79, 2.42) |
| Alaska | |||||
| 20–49 | . . . | . . . | 29 | 0.6 (0.4, 0.9) | . . . |
| ≥ 50 | 91 | 34.8* (27.7, 43.2) | 180 | 13.1 (11.1, 15.3) | 2.66* (2.01, 3.50) |
| Southern Plains | |||||
| 20–49 | 34 | 2.2* (1.5, 3.1) | 133 | 0.8 (0.7, 0.9) | 2.80* (1.86, 4.10) |
| ≥ 50 | 235 | 29.9* (26.1, 34.1) | 2177 | 16.1 (15.4, 16.8) | 1.86* (1.61, 2.14) |
| Southwest | |||||
| 20–49 | 52 | 1.7* (1.2, 2.2) | 265 | 0.5 (0.5, 0.6) | 3.11* (2.26, 4.19) |
| ≥ 50 | 334 | 26.4* (23.5, 29.5) | 4909 | 12.4 (12, 12.7) | 2.13* (1.89, 2.39) |
| Pacific Coast | |||||
| 20–49 | 21 | 1.0 (0.6, 1.5) | 755 | 0.6 (0.6, 0.7) | 1.58 (0.97, 2.42) |
| ≥ 50 | 145 | 18.8* (15.7, 22.4) | 11 850 | 13.7 (13.5, 13.9) | 1.37* (1.14, 1.64) |
| East | |||||
| 20–49 | . . . | . . . | 761 | 0.6 (0.6, 0.7) | . . . |
| ≥ 50 | 53 | 17.6* (12.9, 23.3) | 13 002 | 13.7 (13.5, 14.0) | 1.28 (0.94, 1.70) |
| Total | |||||
| 20–49 | 140 | 1.4* (1.2, 1.6) | 2381 | 0.6 (0.6, 0.7) | 2.19* (1.84, 2.60) |
| ≥ 50 | 1066 | 26.2* (24.6, 27.9) | 39 415 | 13.9 (13.7, 14.0) | 1.89* (1.77, 2.01) |
Note. AI/AN = American Indian/Alaska Native; CHSDA = Contract Health Service Delivery Area; CI = confidence interval; IHS = Indian Health Service; RR = rate ratio. Analyses are limited to persons of non-Hispanic origin. Dashes indicate that counts < 10 are suppressed; if no cases reported, then rates and RRs could not be calculated. AI/AN race is reported by death certificates, or through linkage with the IHS patient registration. Rates are per 100 000 persons and were age adjusted to the 2000 US standard population (11 age groups; Census P25-113028). RRs are calculated in SEER*Stat before rounding of rates and may not equal RRs calculated from rates presented in the table. The following states and years of data were excluded because Hispanic origin was not collected on the death certificate: LA, 1990; NH, 1990–1992; and OK, 1990–1996. IHS regions are defined as follows: AKa; Northern Plains (IL, IN,a IA,a MI,a MN,a MT,a NE,a ND,a SD,a WI,a WYa); Southern Plains (OK,a KS,a TXa); Southwest (AZ,a CO,a NV,a NM,a UTa); Pacific Coast (CA,a ID,a OR,a WA,a HI); and East (AL,a AR, CT,a DE, FL,a GA, KY, LA,a ME,a MD, MA,a MS,a MO, NH, NJ, NY,a NC,a OH, PA,a RI,a SC,a TN, VT, VA, WV, DC).
Source. AI/AN Mortality Database (1990–2009).
Identifies states with ≥ 1 county designated as CHSDA. Percentage regional coverage of AI/AN persons in CHSDA counties to AI/AN persons in all counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; East = 18.2%; and total US = 64.2%.
*P < .05.
Joinpoint regression analyses revealed that kidney cancer death rates decreased slightly for Whites (APC = −0.3; 95% CI = −0.5, 0.0; P < .05) from 1990 to 2009, whereas the death rates for AI/AN persons remained stable during the same time period (Figure 1). Larger decreasing trends occurred in White men from 2002 to 2009 (APC = −1.3; 95% CI = −2.2, −0.4) and White women from 1990 to 2009 (APC = −0.4; 95% CI = −0.8, −0.1). We observed stable death trends for both AI/AN males (APC = 0.5; 95% = −1.1, 2.1) and females (APC = −0.4; 95% CI = −2.6, 1.7; data not shown).
FIGURE 1—
Annual age-adjusted kidney cancer incidence and death rates and trend lines among AI/AN persons and Whites in CHSDA counties.
Note. AI/AN = American Indian/Alaska Native; APC = annual percentage change; CHSDA = Contract Health Service Delivery Areas. Analyses are limited to persons of non-Hispanic origin. AI/AN race is reported by NPCR and SEER registries, death certificates, or through linkage with the IHS patient registration database. APCs for death rates were based on rates that were age-adjusted to the 2000 US standard population (11 age groups, Census P25-113028) and estimated using joinpoint regression. APCs for incidence were based on rates that were age-adjusted to the 2000 US standard population (19 age groups, Census P25-1130) and were calculated with SEER*Stat. The following states and years of data were excluded because Hispanic origin was not collected on the death certificate: LA, 1990; NH, 1990–1992; and OK, 1990–1996. The following states and years of data were excluded because data were not collected or US Cancer Statistics standards were not met: MS, 2001–2002; TN, 2001–2002; VA, 2001; DC, 2002; and WI, 2009. Percentage regional coverage of AI/AN persons in CHSDA counties to AI/AN persons in all counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; and East = 18.2%; total US = 64.2%.
Source. For mortality, AI/AN Mortality Database (1990–2009). For incidence, cancer registries in the Centers for Disease Control and Prevention’s NPCR, the National Cancer Institute’s SEER, or both.
*P < .05 (2-tailed).
From 2001 to 2009, 2088 AI/AN kidney cancer cases were diagnosed in CHSDA counties, with an incidence rate of 20.5 per 100 000 (Table 3). All remaining results regarding incidence rates refer to CHSDA counties only. Of these cases, 95% were RCC (1974 cases). AI/AN men had significantly higher incidence rates of kidney cancer (26.3) and RCC (24.8) than AI/AN women (15.7 for kidney cancer and 14.9 for RCC). The Northern Plains had the highest kidney cancer incidence rate (26.8), followed by the Southern Plains (24.4) and Alaska (21.4), with the lowest incidence rate in the East (15.0). Compared with Whites, AI/AN persons had statistically significantly higher kidney cancer incidence rates in all IHS regions except the East. Among AI/AN individuals, incidence rates of kidney cancer and RCC in older adults (≥ 50 years) were 7 times the rates in younger adults (20–49 years). Compared with Whites in the same age group, AI/AN adults had significantly higher kidney cancer incidence rates: 1.57 times that for the 50 years and older age group and 1.89 times that for the 20 to 49 age group. These patterns held true for most IHS regions. The fixed-interval trend analysis showed that incidence rates for kidney cancer significantly increased for AI/AN persons (APC = 3.5; 95% CI = 1.2, 5.8) and Whites (APC = 2.1; 95% CI = 1.4, 2.8) from 2001 to 2009 (Figure 1). More rapid increases were observed for RCC: 3.8% per year for AI/AN individuals and 2.5% per year for Whites (Table 3).
TABLE 3—
Kidney Cancer Incidence by IHS Region, Sex, and Age for AI/AN Populations and Whites in CHSDA Counties: United States, 2001–2009
| AI/AN |
White |
||||||
| IHS Region | Count | Rate (95% CI) | APC (95% CI) | Count | Rate (95% CI) | APC (95% CI) | AI/AN: White RR (95% CI) |
| By Sex | |||||||
| Northern Plains | |||||||
| Total | 423 | 26.8 (24.1, 29.6) | 10 077 | 12.7 (12.5, 13.0) | 2.10* (1.89, 2.33) | ||
| Male | 238 | 31.4 (27.2, 36.0) | 6278 | 16.9 (16.5, 17.3) | 1.85* (1.60, 2.14) | ||
| Female | 185 | 22.4 (19.2, 26.1) | 3799 | 9.1 (8.8, 9.4) | 2.47* (2.10, 2.89) | ||
| Alaska | |||||||
| Total | 135 | 21.4 (17.7, 25.5) | 468 | 13.0 (11.7, 14.3) | 1.64* (1.33, 2.02) | ||
| Male | 86 | 28.6 (22.5, 35.8) | 308 | 16.8 (14.7, 19.0) | 1.71* (1.30, 2.22) | ||
| Female | 49 | 14.6 (10.7, 19.5) | 160 | 9.3 (7.8, 10.9) | 1.58* (1.10, 2.22) | ||
| Southern Plains | |||||||
| Total | 552 | 24.4 (22.3, 26.6) | 4272 | 13.5 (13.1, 13.9) | 1.81* (1.65, 1.99) | ||
| Male | 319 | 30.1 (26.7, 33.8) | 2639 | 17.9 (17.3, 18.7) | 1.68* (1.48, 1.90) | ||
| Female | 233 | 19.3 (16.9, 22.0) | 1633 | 9.7 (9.2, 10.2) | 2.00* (1.73, 2.30) | ||
| Southwest | |||||||
| Total | 548 | 18.3 (16.7, 20.0) | 8531 | 11.6 (11.4, 11.9) | 1.58* (1.44, 1.73) | ||
| Male | 339 | 26.0 (23.1, 29.1) | 5360 | 15.2 (14.8, 15.6) | 1.71* (1.51, 1.92) | ||
| Female | 209 | 12.4 (10.8, 14.3) | 3171 | 8.4 (8.1, 8.7) | 1.49* (1.28, 1.72) | ||
| Pacific Coast | |||||||
| Total | 321 | 16.6 (14.7, 18.6) | 18 216 | 12.2 (12.1, 12.4) | 1.35* (1.20, 1.52) | ||
| Male | 188 | 21.0 (17.8, 24.6) | 11 690 | 16.7 (16.4, 17.0) | 1.26* (1.06, 1.48) | ||
| Female | 133 | 12.9 (10.7, 15.5) | 6526 | 8.3 (8.1, 8.6) | 1.55* (1.28, 1.86) | ||
| East | |||||||
| Total | 109 | 15.0 (12.2, 18.3) | 20 779 | 13.6 (13.4, 13.8) | 1.10 (0.90, 1.35) | ||
| Male | 57 | 17.1 (12.6, 22.6) | 13 013 | 18.6 (18.2, 18.9) | 0.92 (0.68, 1.22) | ||
| Female | 52 | 13.4 (9.9, 17.8) | 7766 | 9.4 (9.2, 9.7) | 1.42* (1.05, 1.88) | ||
| Total | 2088 | 20.5 (19.6, 21.5) | 3.5* (1.2, 5.8) | 62 343 | 12.7 (12.6, 12.8) | 2.1* (1.4, 2.8) | 1.61* (1.54, 1.69) |
| Male | 1227 | 26.3 (24.7, 27.9) | 4.9* (2.1, 7.8) | 39 288 | 17.1 (17.0, 17.3) | 1.6 (0.9, 2.4) | 1.53* (1.44, 1.63) |
| Female | 861 | 15.7 (14.7, 16.9) | 1.5 (−2.3, 5.5) | 23 055 | 8.9 (8.8, 9.0) | 2.7* (1.8, 3.6) | 1.77* (1.65, 1.90) |
| Total RCC | |||||||
| Total | 1974 | 19.4 (18.5, 20.3) | 3.8* (1.3, 6.3) | 55 000 | 11.2 (11.1, 11.3) | 2.5* (1.8, 3.3) | 1.73* (1.65, 1.81) |
| Male | 1160 | 24.8 (23.3, 26.4) | 5.0* (2.5, 7.6) | 35 071 | 15.2 (15.0, 15.4) | 2.1* (1.3, 2.8) | 1.63* (1.53, 1.74) |
| Female | 814 | 14.9 (13.8, 15.9) | 1.9 (−2.3, 6.3) | 19 929 | 7.7 (7.6, 7.8) | 3.1* (2.0, 4.1) | 1.93* (1.79, 2.07) |
| By Age | |||||||
| Northern Plains | |||||||
| 20–49 | 116 | 13.0 (10.8, 15.6) | 1347 | 4.6 (4.4, 4.9) | 2.8* (2.3, 3.4) | ||
| ≥ 50 | 301 | 75.7 (66.8, 85.5) | 8604 | 38.0 (37.2, 38.8) | 2.0* (1.8, 2.3) | ||
| Alaska | |||||||
| 20–49 | 20 | 5.3 (3.3, 8.2) | 71 | 3.6 (2.8, 4.5) | 1.5 (0.9, 2.5) | ||
| ≥ 50 | 112 | 68.0 (55.3, 82.8) | 391 | 40.8 (36.4, 45.5) | 1.7* (1.3, 2.1) | ||
| Southern Plains | |||||||
| 20–49 | 129 | 11.6 (9.7, 13.8) | 507 | 4.7 (4.3, 5.1) | 2.5* (2.0, 3.0) | ||
| ≥ 50 | 416 | 69.3 (62.6, 76.6) | 3712 | 40.4 (39.1, 41.8) | 1.7* (1.5, 1.9) | ||
| Southwest | |||||||
| 20–49 | 117 | 7.1 (5.9, 8.5) | 1038 | 4.3 (4.0, 4.6) | 1.7* (1.4, 2.0) | ||
| ≥ 50 | 421 | 54.4 (49.1, 60.0) | 7401 | 34.5 (33.7, 35.3) | 1.6* (1.4, 1.7) | ||
| Pacific Coast | |||||||
| 20–49 | 74 | 7.1 (5.6, 9.0) | 2336 | 4.3 (4.2, 4.5) | 1.7* (1.3, 2.1) | ||
| ≥ 50 | 236 | 47.2 (40.9, 54.2) | 15 658 | 36.6 (36.1, 37.2) | 1.3* (1.1, 1.5) | ||
| East | |||||||
| 20–49 | 21 | 5.2 (3.2, 8.0) | 2740 | 5.1 (4.9, 5.3) | 1.0 (0.6, 1.6) | ||
| ≥ 50 | 87 | 45.8 (36.2, 57.3) | 17 846 | 40.4 (39.8, 41.0) | 1.1 (0.9, 1.4) | ||
| Total | |||||||
| 20–49 | 477 | 8.7 (8.0, 9.6) | 7.3* (2.7, 12.1) | 8039 | 4.6 (4.5, 4.7) | 5.0* (3.8, 6.1) | 1.9* (1.7, 2.1) |
| ≥ 50 | 1573 | 59.7 (56.6, 62.9) | 2.6 (0.2, 5.0) | 53 612 | 38.0 (37.7, 38.3) | 1.6 (0.7, 2.4) | 1.6* (1.5, 1.7) |
| Total RCC | |||||||
| 20–49 | 464 | 8.5 (7.7, 9.3) | 7.2* (2.6, 1.2) | 7722 | 4.4 (4.4, 4.6) | 5.2* (4.1, 6.3) | 1.9* (1.7, 2.1) |
| ≥ 50 | 1504 | 56.5 (53.5, 59.6) | 2.8 (0.3, 5.5) | 47 235 | 33.4 (33.1, 33.7) | 1.9* (1.0, 2.9) | 1.7* (1.6, 1.8) |
Note. AI/AN = American Indian/Alaska Native; APC = annual percentage change; CHSDA = Contract Health Service Delivery Area; CI = confidence interval; IHS = Indian Health Service; RCC = renal cell carcinoma; RR = rate ratio. Analyses are limited to persons of non-Hispanic origin. AI/AN race is reported by NPCR and SEER registries, or through linkage with the IHS patient registration database. Rates are per 100 000 persons and were age adjusted to the 2000 US standard population (19 age groups; Census P25-113028). Rate ratios were calculated in SEER*Stat before rounding of rates and may not equal RRs calculated from rates presented in the table. APCs and their corresponding 95% CIs were calculated with SEER*Stat. Years of data and registries used in the analyses: 1999–2009 (43 states): AK, AL, AZ, CA, CO, CT, DE, FL, GA, HI, IA, ID, IL, IN, KS, KY, LA, MA, MD, ME, MI, MN, MO, MT, ND, NE, NH, NJ, NM, NV, NY, OH, OK, OR, PA, RI, SC, TX, UT, VT, WA, WV, WY; 1999–2008: WI; 1999–2001 and 2003–2009: DC; 2001–2009: AR, NC, SD; 2002–2009: VA; and 2003–2009: MS, TN. IHS regions are defined as follows: AKa; Northern Plains (IL, IN,a IA,a MI,a MN,a MT,a NE,a ND,a SD,a WI,a WYa); Southern Plains (OK,a KS,a TXa); Southwest (AZ,a CO,a NV,a NM,a UTa); Pacific Coast (CA,a ID,a OR,a WA,a HI); and East (AL,a AR, CT,a DE, FL,a GA, KY, LA,a ME,a MD, MA,a MS,a MO, NH, NJ, NY,a NC,a OH, PA,a RI,a SC,a TN, VT, VA, WV, DC).
Source. Data are from population-based cancer registries that participate in the NPCR, the SEER, or both and meet criteria for high data quality.
Identifies states with ≥ 1 county designated as CHSDA. Percentage regional coverage of AI/AN persons in CHSDA counties to AI/AN persons in all counties: Northern Plains = 64.8%; Alaska = 100%; Southern Plains = 76.3%; Southwest = 91.3%; Pacific Coast = 71.3%; East = 18.2%; and total US = 64.2%.
*P < .05.
DISCUSSION
Analyses of population-based cancer incidence and mortality data revealed that kidney cancer incidence and death rates in AI/AN men and women were higher than those of Whites. From 2001 to 2009, incidence rates of kidney cancer, especially RCC, continued to rise for both AI/AN persons and Whites, but more rapidly for AI/AN individuals. Although a decreasing trend of kidney cancer deaths was observed for Whites, death rates remained unchanged in AI/AN persons from 1990 to 2009, resulting in an increase in disparity. The increasing burden of kidney cancer in AI/AN populations varies by IHS region, with the Northern Plains, Alaska, and Southern Plains having the highest incidence and death rates.
These results are consistent with 2 previous studies.5,11 In 2007, Espey et al.5 reported that, in CHSDA counties, AI/AN populations had the highest kidney cancer death rates among all races (9.3 for males and 4.3 for females). Espey et al.’s study5 also revealed that AI/ANs had higher kidney cancer incidence rates than other races (22.7 for males and 13.9 for females), and rates were highest in the Northern Plains, Alaska, and the Southern Plains. Wilson et al.11 examined kidney cancer incidence data and found that kidney parenchyma cancer incidence rates of AI/AN persons varied by region, sex, and age, similar to what we observed. They also found that the incidence of kidney parenchyma cancer increased from 1999 to 2004 for younger and older White adults, respectively, but not for AI/AN adults. Overall kidney cancer incidence has consistently been documented to be rising over recent decades.2,31 In our study, we observed a significant increase of kidney cancer incidence in White and AI/AN younger and older adults from 2001 to 2009. One explanation from Wilson et al.11 about this nonsignificant trend for AI/AN persons was that the time period of 6 years was too brief. Our study revealed stable kidney cancer death trends for both male and female AI/AN persons from 1990 to 2009, which were consistent with a previously reported study using 1995 to 2004 National Vital Statistics System data.5
RCC is the most common kidney cancer.1,2 Our study shows that, for AI/AN adults, RCC accounts for approximately 95% of kidney cancers in this population. Rising incidence of RCC may only partially be attributable to improvement and widespread use of diagnostic imaging because better detection cannot explain the continued increase in advanced tumors.8,31,32 Higher prevalence estimates for obesity, smoking, and hypertension among AI/AN persons, which are all known risk factors for kidney cancer, may also contribute to the increase. Epidemiological research has shown associations of excess body weight and smoking with risk for RCC.11,33 It has been estimated that more than 40% of RCC in the United States may be attributable to overweight and obesity34; obesity alone accounts for 25% of kidney cancers.11 Two Behavioral Risk Factor Surveillance System surveys for 1999 to 2006 have shown that AI/AN adults were 1.5 times more likely to be obese or current smokers than White adults.5,35 A higher prevalence of obesity in AI/AN persons was also observed among preschool- and school-age children in late 1980s.36 The prevalence of smoking over the past several decades has consistently been reported as higher among AI/AN populations than Whites.5,35,37–39 Despite overall declines in cigarette smoking, smoking prevalence among AI/AN populations remains high. Hypertension and its treatments have been shown to be risk factors for RCC independent of obesity and smoking.8,31 An analysis of 2003 Behavioral Risk Factor Surveillance System data showed that the prevalence of hypertension in AI/AN persons was 23% higher than that in Whites.40 Interestingly, several studies have also suggested that AI/AN persons have less leisure time and physical activity than Whites, and this finding correlates with RCC risk difference by race.5,35,38 Physical inactivity may increase kidney cancer risk by increasing obesity and blood pressure.41,42 However, a recent meta-analysis suggested that physical inactivity may play an independent role in conferring kidney cancer risk.43 Researchers have reported that physical activity may independently reduce kidney cancer risk by lowering lipid peroxidation levels.44
The East, Pacific Coast, and Southwest regions had lower kidney cancer incidence rates than the remaining regions. Regional analyses showed that, among all IHS regions, the East had the lowest prevalence of obesity, the Southwest and Pacific Coast had the lowest smoking prevalence, and the Pacific Coast had the lowest hypertension prevalence, suggesting that regional variations in kidney cancer incidence may be attributable to regional variation in cancer risk factors.5,35,45 However, the high prevalence of smoking and hypertension in the East cannot explain the low incidence rate of kidney cancer. Regional differences in AI/AN population sizes and misclassification, health insurance, and proximity to health care facilities should also be considered in interpreting the geographic variations of cancer burden.
Racial disparities in kidney cancer continue to widen because kidney cancer death rates have declined among Whites but remained stable among AI/AN populations for the past 2 decades. Studies have suggested that higher death rates from kidney cancer for AI/AN populations may be associated with lower socioeconomic status, no or less health care access, poor health coverage, lack of appropriate medical care, and later stage at cancer diagnosis.5,11,15 Espey et al.5 reported that compared with Whites, AI/AN persons had higher prevalence of poverty, less than 9th-grade education, no health care coverage, and no regular source of medical care. The Southwest has higher prevalence of almost all of these socioeconomic status and health care access factors when compared with other IHS regions.5 For stage at cancer diagnosis, Wilson et al.11 concluded that AI/AN persons were significantly more likely to have been diagnosed with late-stage kidney cancer than Whites. These less favorable socioeconomic status and health care access factors may lead to a later stage at diagnosis. Combined with higher overall prevalence of smoking, obesity, and physical inactivity, these less favorable factors may contribute to the higher death rates in AI/AN populations compared with Whites.
This study provides the most recent kidney cancer incidence and death rates and trends by IHS region in AI/AN populations. Misclassification of AI/AN race was reduced by linking cancer registry and National Death Index databases to the IHS patient registration files and restricting analyses to CHSDA counties. Our study is subject to several limitations: First, although data linkages improved the race classification for AI/AN persons, the problem may still exist and likely varies by IHS region. Also, restricting the majority of analyses to CHSDA counties, in which only 64.2% of AI/AN persons live and which tend to be in Western states and more rural areas, limits the generalizability to all AI/AN populations in the United States. The percentage of AI/AN persons living in the CHSDA counties varies substantially by IHS region, ranging from 100% in Alaska and about 18.2% in the East. Additionally, the proportion of Native ancestry required for tribal membership and therefore eligibility for IHS services varies substantially between federally recognized tribes. Whether and how this discrepancy in tribal membership requirements may influence some of our findings is unclear, although our findings are consistent with prior reports. Although the exclusion of Hispanic AI/AN persons from the analyses reduces the overall AI/AN deaths by less than 5%, it may disproportionately affect some states. We excluded mortality data from several states and years because Hispanic origin was not collected on the death certificate. Finally, the 2 major types of kidney cancer, RCC and RTCC/UC, have distinct etiology, risk factors, rates, and trends. We could not separate RCC and RTCC/UC deaths because this information was not available in the mortality file.
AI/AN persons are at greater risk of developing and dying of kidney cancers than Whites. Only a few modifiable risk factors for kidney cancer are known, and these factors cannot fully explain the geographic patterns in kidney cancer incidence and mortality in AI/AN individuals. Because of the more rapid increase of kidney cancer incidence in AI/AN persons and the less favorable mortality trend compared with Whites, additional studies are needed to explain the differences in incidence and mortality that would reduce and eliminate racial disparities for this disease. Continued monitoring of kidney cancer patterns through surveillance is warranted to track progress in eliminating racial disparity in kidney cancer. Given the high prevalence of obesity, smoking, and hypertension, more public health interventions are needed such as healthy diet and physical activity promotion, tobacco cessation, and early detection and control of hypertension.
References
- 1.Chow WH, Dong LM, Devesa SS. Epidemiology and risk factors for kidney cancer. Nat Rev Urol. 2010;7(5):245–257. doi: 10.1038/nrurol.2010.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chow WH, Devesa SS, Warren JL, Fraumeni JF., Jr Rising incidence of renal cell cancer in the United States. JAMA. 1999;281(17):1628–1631. doi: 10.1001/jama.281.17.1628. [DOI] [PubMed] [Google Scholar]
- 3.Jemal A, Simard EP, Dorell C et al. Annual report to the nation on the status of cancer, 1975–2009, featuring the burden and trends in human papillomavirus (HPV)-associated cancers and HPV vaccination coverage levels. J Natl Cancer Inst. 2013;105(3):175–201. doi: 10.1093/jnci/djs491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cho E, Adami HO, Lindblad P. Epidemiology of renal cell cancer. Hematol Oncol Clin North Am. 2011;25(4):651–665. doi: 10.1016/j.hoc.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Espey DK, Wu XC, Swan J et al. Annual report to the nation on the status of cancer, 1975–2004, featuring cancer in American Indians and Alaska Natives. Cancer. 2007;110(10):2119–2152. doi: 10.1002/cncr.23044. [DOI] [PubMed] [Google Scholar]
- 6.Weir HK, Jim MA, Marrett LD, Fairley T. Cancer in American Indian and Alaska Native young adults (ages 20–44 years): US, 1999-2004. Cancer. 2008;113(5 suppl):1153–1167. doi: 10.1002/cncr.23731. [DOI] [PubMed] [Google Scholar]
- 7.Vaishampayan UN, Do H, Hussain M, Schwartz K. Racial disparity in incidence patterns and outcome of kidney cancer. Urology. 2003;62(6):1012–1017. doi: 10.1016/j.urology.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 8.Chow WH, Devesa SS. Contemporary epidemiology of renal cell cancer. Cancer J. 2008;14(5):288–301. doi: 10.1097/PPO.0b013e3181867628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nepple KG, Yang L, Grubb RL, 3rd, Strope SA. Population based analysis of the increasing incidence of kidney cancer in the United States: evaluation of age specific trends from 1975 to 2006. J Urol. 2012;187(1):32–38. doi: 10.1016/j.juro.2011.09.028. [DOI] [PubMed] [Google Scholar]
- 10.Watson RA. Kidney cancer in American Indian and Native Alaskan men and women—time to notice, time to care. Urology. 2008;72(4):726–730. doi: 10.1016/j.urology.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Wilson RT, Richardson LC, Kelly JJ, Kaur J, Jim MA, Lanier AP. Cancers of the urinary tract among American Indians and Alaska Natives in the United States, 1999–2004. Cancer. 2008;113(5 suppl):1213–1224. doi: 10.1002/cncr.23733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wiggins CL, Espey DK, Wingo PA et al. Cancer among American Indians and Alaska Natives in the United States, 1999-2004. Cancer. 2008;113(5 suppl):1142–1152. doi: 10.1002/cncr.23734. [DOI] [PubMed] [Google Scholar]
- 13.Harwell TS, Miller SH, Lemons DL, Helgerson SD, Gohdes D. Cancer incidence in Montana: rates for American Indians exceed those for Whites. Am J Prev Med. 2006;30(6):493–497. doi: 10.1016/j.amepre.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 14.Becker TM, Bettles J, Lapidus J et al. Improving cancer incidence estimates for American Indians and Alaska Natives in the Pacific Northwest. Am J Public Health. 2002;92(9):1469–1471. doi: 10.2105/ajph.92.9.1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Espey D, Paisano R, Cobb N. Regional patterns and trends in cancer mortality among American Indians and Alaska Natives, 1990-2001. Cancer. 2005;103(5):1045–1053. doi: 10.1002/cncr.20876. [DOI] [PubMed] [Google Scholar]
- 16.Espey DK, Jim MA, Richards T, Begay C, Haverkamp D, Roberts D. Methods for improving the quality and completeness of mortality data for American Indians and Alaska Natives. Am J Public Health. 2014;104(6 suppl 3):S286–S294. doi: 10.2105/AJPH.2013.301716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Espey DK, Wiggins CL, Jim MA, Miller BA, Johnson CJ, Becker TM. Methods for improving cancer surveillance data in American Indian and Alaska Native populations. Cancer. 2008;113(5 suppl):1120–1130. doi: 10.1002/cncr.23724. [DOI] [PubMed] [Google Scholar]
- 18.National Cancer Institute, Surveillance, Epidemiology, and End Results Program. Adjusted populations for the counties/parishes affected by Hurricanes Katrina and Rita. Available at: http://seer.cancer.gov/popdata/hurricane_adj.html. Accessed April 5, 2013.
- 19.Edwards BK, Noone AM, Mariotto AB et al. Annual Report to the Nation on the status of cancer, 1975–2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. 2013 doi: 10.1002/cncr.28509. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Center for Health Statistics, Division of Vital Statistics. National Vital Statistics System. Available at: http://www.cdc.gov/nchs/nvss.htm. Accessed May 2, 2012.
- 21.National Center for Health Statistics, Division of Vital Statistics. NCHS procedures for multiple-race and Hispanic origin data: collection, coding, editing, and transmitting. Available at: http://www.cdc.gov/nchs/data/dvs/Multiple_race_documentation_5-10-04.pdf. Accessed June 15, 2013.
- 22.Indian Health Service. Indian Health Service: A quick look. Available at: http://www.ihs.gov/factsheets/index.cfm?module=dsp_fact_quicklook. Accessed May 8, 2013.
- 23.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980. [Google Scholar]
- 24.International Classification of Diseases, 10th Revision. Geneva, Switzerland: World Health Organization; 1990. [Google Scholar]
- 25.Anderson RN, Minino AM, Hoyert DL, Rosenberg HM. Comparability of cause of death between ICD-9 and ICD-10: preliminary estimates. Natl Vital Stat Rep. 2001;49(2):1–32. [PubMed] [Google Scholar]
- 26.Fritz A, Percy C, Jack A, editors. International Classification of Diseases for Oncology. 3rd ed. Geneva, Switzerland: World Health Organization; 2000. [Google Scholar]
- 27.Arias E, Schauman WS, Eschbach K, Sorlie PD, Backlund E. The validity of race and Hispanic origin reporting on death certificates in the United States. Vital Health Stat 2. 2008;2(148):1–23. [PubMed] [Google Scholar]
- 28. Day JC, Population Projections of the United States by Age, Sex, Race, and Hispanic Origin: 1995 to 2050, U.S. Bureau of the Census, Current Population Reports, P25-1130, Washington, DC: US Government Printing Office; 1996.
- 29.Tiwari RC, Clegg LX, Zou Z. Efficient interval estimation for age-adjusted cancer rates. Stat Methods Med Res. 2006;15(6):547–569. doi: 10.1177/0962280206070621. [DOI] [PubMed] [Google Scholar]
- 30.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 31.Weikert S, Ljungberg B. Contemporary epidemiology of renal cell carcinoma: perspectives of primary prevention. World J Urol. 2010;28(3):247–252. doi: 10.1007/s00345-010-0555-1. [DOI] [PubMed] [Google Scholar]
- 32.Hollingsworth JM, Miller DC, Daignault S, Hollenbeck BK. Rising incidence of small renal masses: a need to reassess treatment effect. J Natl Cancer Inst. 2006;98(18):1331–1334. doi: 10.1093/jnci/djj362. [DOI] [PubMed] [Google Scholar]
- 33.Moore LE, Wilson RT, Campleman SL. Lifestyle factors, exposures, genetic susceptibility, and renal cell cancer risk: a review. Cancer Invest. 2005;23(3):240–255. doi: 10.1081/cnv-200055962. [DOI] [PubMed] [Google Scholar]
- 34.Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer. 2004;4(8):579–591. doi: 10.1038/nrc1408. [DOI] [PubMed] [Google Scholar]
- 35.Steele CB, Cardinez CJ, Richardson LC, Tom-Orme L, Shaw KM. Surveillance for health behaviors of American Indians and Alaska Natives—findings from the Behavioral Risk Factor Surveillance System, 2000–2006. Cancer. 2008;113(5 suppl):1131–1141. doi: 10.1002/cncr.23727. [DOI] [PubMed] [Google Scholar]
- 36.Broussard BA, Johnson A, Himes JH et al. Prevalence of obesity in American Indians and Alaska Natives. Am J Clin Nutr. 1991;53(6 suppl):1535S–1542S. doi: 10.1093/ajcn/53.6.1535S. [DOI] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention. Cigarette smoking among American Indians, Alaskan Natives–behavioral risk factor surveillance system, 1987–1991. J Am Med Assoc. 1992;268(21):3052–3055. [PubMed] [Google Scholar]
- 38.Denny CH, Holtzman D, Cobb N. Surveillance for health behaviors of American Indians and Alaska Natives: findings from the Behavioral Risk Factor Surveillance System, 1997–2000. MMWR Surveill Summ. 2003;52(7):1–13. [PubMed] [Google Scholar]
- 39.Frieden TR Centers for Disease Control and Prevention. CDC health disparities and inequalities report—United States, 2011. MMWR Surveill Summ. 2011;60(suppl):1–2. [PubMed] [Google Scholar]
- 40.Zhao G, Ford ES, Mokdad AH. Racial/ethnic variation in hypertension-related lifestyle behaviours among US women with self-reported hypertension. J Hum Hypertens. 2008;22(9):608–616. doi: 10.1038/jhh.2008.52. [DOI] [PubMed] [Google Scholar]
- 41.Wing RR. Physical activity in the treatment of the adulthood overweight and obesity: current evidence and research issues. Med Sci Sports Exerc. 1999;31(11 suppl):S547–S552. doi: 10.1097/00005768-199911001-00010. [DOI] [PubMed] [Google Scholar]
- 42.Blair SN, Goodyear NN, Gibbons LW, Cooper KH. Physical fitness and incidence of hypertension in healthy normotensive men and women. JAMA. 1984;252(4):487–490. [PubMed] [Google Scholar]
- 43.Behrens G, Leitzmann MF. The association between physical activity and renal cancer: systematic review and meta-analysis. Br J Cancer. 2013;108(4):798–811. doi: 10.1038/bjc.2013.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vincent KR, Vincent HK, Braith RW, Lennon SL, Lowenthal DT. Resistance exercise training attenuates exercise-induced lipid peroxidation in the elderly. Eur J Appl Physiol. 2002;87(4–5):416–423. doi: 10.1007/s00421-002-0640-2. [DOI] [PubMed] [Google Scholar]
- 45.Jernigan VBB, Duran B, Ahn D, Winkleby M. Changing patterns in health behaviors and risk factors related to cardiovascular disease among American Indians and Alaska Natives. Am J Public Health. 2010;100(4):677–683. doi: 10.2105/AJPH.2009.164285. [DOI] [PMC free article] [PubMed] [Google Scholar]