Abstract
Introduction: The number of mobbing experiences recorded has increased during recent years and it has now been established as global phenomenon among the working population. The goal of our study was to analyze the incidence of certain neurologic and psychiatric diseases as a consequence of mobbing as compared with a control group and to examine the possible influence of previous diseases that occurred within one year before the first mobbing documentation on the incidence of mobbing.
Material & methods: We used a large database (IMS® Disease Analyzer, Germany) to collect data from general practitioners in Germany from 01/2003 until 12/2012. Based on age, gender, and health insurance, patients with experience of mobbing were matched with a control group of patients who had not reported workplace mobbing and who were being treated by the same physicians. At first, diseases that occurred within one year before the bullying experience took place (“index date”) were noted and compared to a control group of similar composition in terms of gender, age, and health insurance. Subsequently, the prevalence of depression, anxiety, somatoform disorders, and sleep disorders following experiences of mobbing were determined. After adjustment to take into account the odds of bullying, the ratios of these diseases were assessed using a logistic regression model.
Results: The study population consisted of n=2,625 patients and n=2,625 controls, of which 33% were men. The number of cases of bullying documented rose continuously from 2003 to 2011 and remained high in 2012. Those who would later become victims of mobbing demonstrated a considerably higher prevalence of diseases in general – these diseases were not confined to the neurologic-psychiatric spectrum. Following experiences of bullying, depression, anxiety, somatoform disorders, and sleep disorders were significantly more prevalent than in the control group (for all, p<0.05). Similarly, odds ratios (OR) representing the risk of suffering from diseases were higher in affected patients, with the highest value (4.28) for depression and the lowest value for sleep disorders (OR=2.4).
Conclusion: Those who will later become the victims of bullying are more prone to suffer from diseases in general, even before this experience of mobbing has occurred, which underlines the importance of supporting (chronically) ill patients to protect them against bullying. Sequelae of mobbing include, in particular, diseases from the neurologic-psychiatric spectrum.
Keywords: mobbing, depression, anxiety, risk factors
Zusammenfassung
Einleitung: Mobbing am Arbeitsplatz hat in den letzten Jahren deutlich zugenommen und ist heutzutage ein weltweites Phänomen in der arbeitenden Bevölkerung. Da es bedeutende sozioökonomische Konsequenzen hat, ist es wichtig, Vorläufer zu kennen, um präventiv tätig werden zu können.
Material & Methoden: Mithilfe einer umfangreichen Datenbank (IMS® Disease Analyzer, IMS Health, Deutschland) haben wir die Daten von Allgemeinmedizinern in Deutschland zwischen Januar 2003 und Dezember 2012 analysiert. Es wurden alle Patienten in die Studie eingeschlossen, die zum ersten Mal mit Mobbing am Arbeitsplatz konfrontiert waren, wobei dieser Zeitpunkt als „Index-Datum“ gesetzt wurde. Zunächst wurden sämtliche Krankheiten notiert, die innerhalb eines Jahres vor dem „Index-Datum“ erstmals aufgetreten sind und mit einer Kontrollgruppe verglichen, die der Untersuchungsgruppe bezüglich Geschlecht, Alter und Versicherungsstatus entsprachen. Danach wurden die Prävalenz von Depressionen, Angst-, somatoformen und Schlafstörungen nach stattgefundenem Mobbing berechnet. Anschließend wurden nach Adjustierung bezüglich Mobbings die Odds Ratio dieser Erkrankungen in einem logistischen Regressionsmodel bestimmt.
Ergebnisse: Die Studiengruppe bestand aus n=2.625 Patienten und derselben Anzahl an Kontrollen, von denen zwei Drittel männlich waren. Die Zahl der dokumentierten Mobbing-Fälle stieg kontinuierlich von 2003 bis 2011 an und blieb auch 2012 auf hohem Niveau. Patienten, die in der Folge Opfer von arbeitsplatzbezogenem Mobbing wurden, hatten generell eine bedeutend höhere Krankheitsprävalenz, wobei diese nicht auf den neurologisch-psychiatrischen Formenkreis beschränkt waren. Nach dem Auftreten von Mobbing war in der Studiengruppe verglichen mit der Kontrollgruppe eine signifikant höhere Prävalenz von Depressionen, Angst-, somatoformen und Schlafstörungen nachzuweisen (für alle Erkrankungen: p<0,05). Ähnliches war im Hinblick auf die Odds Ratio zu sehen, wobei das Risiko an Depressionen zu erkranken mit 4,28 am höchsten und für Schlafstörungen mit 2,4 am niedrigsten war.
Schlussfolgerung: Patienten, die im Verlauf Opfer von arbeitsplatzbezogenem Mobbing wurden, waren bereits vorher häufiger krank als die Kontrollen, was die Wichtigkeit präventiver Maßnahmen bei chronisch kranken Menschen unterstreicht, um sie vor Mobbing zu schützen. Folgeerkrankungen von Mobbing stammen vor allem aus dem psychiatrisch-neurologischen Formenkreis.
Introduction
Within the last few years, mobbing has emerged as an important factor influencing both the working performance and general health status of the population [1], [2]. There is a general consensus in that the terms mobbing, bullying and harassment can be used synonymously, although geographical preferences mean that one or the other term is used more frequently in certain regions [3]. According to the World Health Organization (WHO) or the International Labour Office (ILO), mobbing is defined as “repeated and over time, offensive behavior through vindictive, cruel or malicious attempts to humiliate or undermine an individual or groups of employees” [4]. Typical workplace mobbing actions include social isolation (e.g. exclusion from meetings), intrusion into privacy, verbal attacks or intimidation as well as organizational measures such as deprivation of competencies or allocation of low-order work tasks [5]. To fulfill all the criteria used by Leymann to identify mobbing, this behavior needs to take place on a frequent basis (at least once a week) and over a long period of time (at least 6 months) [1], [6]. It should be noted that bullying crosses all socio-demographic borders and can be observed in all categories of age, gender, ethnicity, academic achievement, and professional environment [7], although it seems to be especially common in the medical sector [8], [9], [10], [11], [12], [13], [14]. Its general prevalence is estimated at between 2% and 15% [15], but a recent study indicated that it is even higher in adolescents, of whom 20–35% reported involvement in mobbing as a victim, a perpetrator or both [16], [17]. A special survey from 2004, initiated by the European Commission, revealed that 10.2% of women and 7.3% of men had been victims of workplace mobbing in the previous 12 months [18]. Tonini and colleagues discovered that women in the age group of 34 to 45 are especially likely to be the subjects of harassment, a phenomenon which can be explained by the increased level of family commitment in this age range, leading to a rise in stress [1]. The sequelae of mobbing are extensive and include social phobia [19], depression [2], [20], [21], [22], suicidality [21], [23], [24], posttraumatic stress disorder [1], [25] as well as substance abuse [7].
The goal of our study was to analyze the incidence of certain neurologic and psychiatric diseases as a consequence of mobbing as compared with a control group and to examine the possible influence of previous diseases that occurred within one year before the bullying took place (“index date”).
Methods and patients
Disease Analyzer database
Disease Analyzer is one of the major European patient databases and allows anonymous access to a selected panel of physicians’ practices and patients. The data are generated directly from the computers in the physicians’ practices via standardized interfaces and provide daily routine information on patients’ diseases and therapies. A practice transmits patient data stored in the physician’s computer to IMS on a monthly basis. Before transmission, the data are encrypted for data protection and contain in similar scope and detail the information in the files of patients in the doctor’s practice [26].
Altogether, the database contains data from approximately 3,000 practices (general practitioners and various specialist groups). The sampling method is based on summary statistics from all doctors in Germany published yearly by the German Medical Association. The panel design is determined according to the following strata: specialist group, German federal state, community size category, and age of physician. To account for natural fluctuation in the practices and an annual check of the summary statistics by the German Medical Association, the panel design is adjusted each year. Whenever a practice ends its collaboration with IMS, it is replaced by a new one [26]. The validity of the Disease Analyzer data was previously evaluated and described [27].
Study population
Overall, the database included 1,072 general practices reporting continuously to IMS HEALTH during the study period (01/2003–12/2012).
First, all patients reporting workplace mobbing for the first time were selected. An additional criterion for inclusion was continuous observation in the same practice (≥1 visit during the 12 months before index date and ≥1 visit during a period of at least 12 months after index date). Mental and neurological disorders were determined based on primary care diagnoses (ICD-10 codes) for depression (F32, F33), anxiety (F41), somatoform disorders (F45) and sleep disorders (G47). Demographic data included age, sex, health insurance (private/statutory) and practice region (East/West Germany).
Statistical analysis
Based on age, gender, and health insurance, patients with experience of mobbing were matched with a control group of patients who had not reported workplace mobbing and who were being treated by the same physicians. A multivariate logistic regression model was applied, with depression, anxiety, somatoform disorder and sleep disorder as dependent variables. Furthermore, potential confounders (practice in West-Germany), diagnoses within one year prior to index date (neoplasms (ICD 10: C00–D48), diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism (ICD 10: D50–D89), endocrine, nutritional and metabolic diseases (ICD 10: E00–E90), diseases of the nervous system (ICD 10: G00–G99), diseases of the ear and the mastoid process (ICD 10: H60–H95), diseases of the circulatory system (ICD 10: I00–I99), diseases of the respiratory system (ICD 10: J00–J99), diseases of the digestive system (ICD 10: K00–K93), diseases of the skin and subcutaneous tissue (ICD 10: L00–L99), diseases of the musculoskeletal system and connective tissue (ICD 10: M00–M99) and diseases of the genitourinary system (ICD 10: N00–N99) were included as independent variables. Two-sided tests were used and a p-value of <0.05 was considered statistically significant. All analyses were carried out using SAS 9.3. (SAS Institute, Cary, USA).
Results
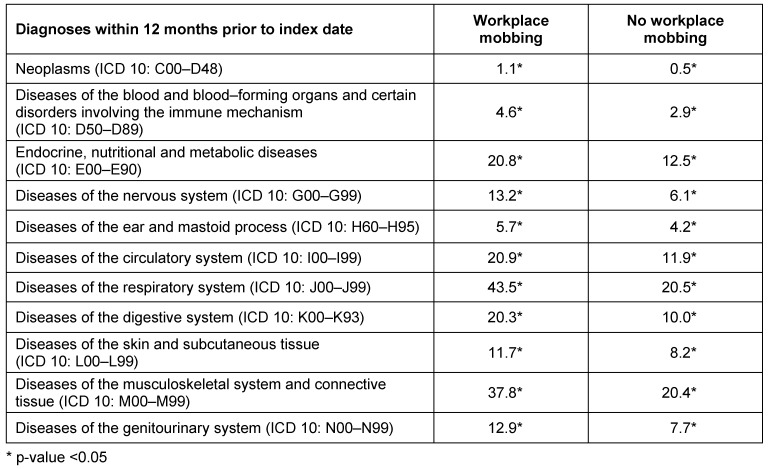
Analysis with the Disease Analyser database revealed that a total of 2,625 patients had consulted their doctors because they were victims of workplace mobbing. This data was collected from 199 general medical practices in Germany over a 10-year-period (from 01/2003 until 12/2012). As can be drawn from Figure 1 (Fig. 1), the number of patients with first documentation of workplace mobbing experience rose continuously from 2003 (n=24) to peak in 2011 (n=441) and remained high in 2012 (n=429).
Figure 1. Development of patient numbers with documentation of workplace mobbing in primary care practices in Germany (Disease Analyzer database).
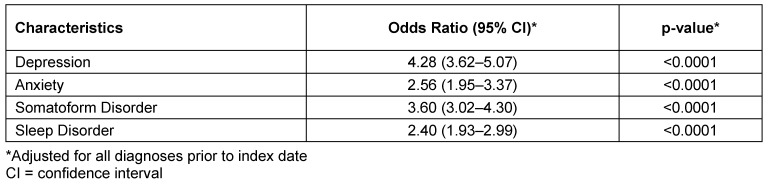
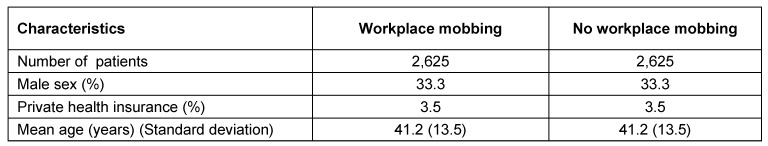
Gender distribution did not change significantly during the observation period (Figure 2 (Fig. 2)); the mean distribution showed that 33% men and 67% women were affected by bullying. Patients had an average age of 41.2 ± 13.5 years of age and the percentage of patients with private health insurance was 5%. These patients were matched with a control group (n=2,625) on the basis of age, gender, and health insurance status and further retrospective analysis was performed. Table 1 (Tab. 1) summarizes the characteristics of the study participants.
Figure 2. Gender distribution of patients with documentation of workplace mobbing (Disease Analyzer database).
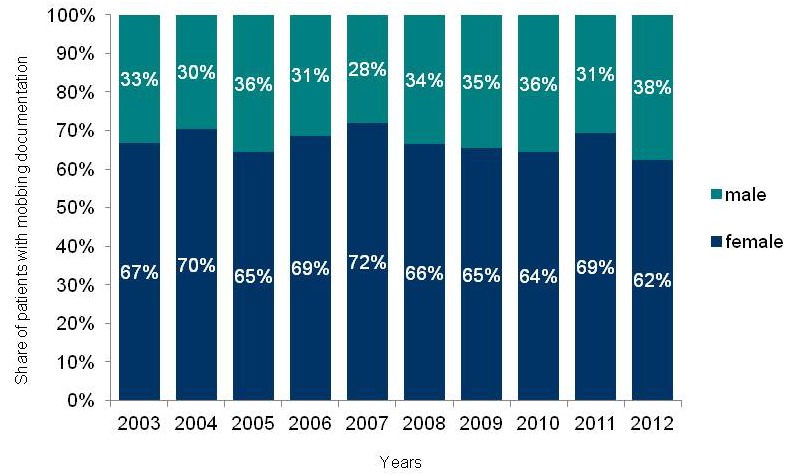
Table 1. Characteristics of patients with and without documentation of workplace mobbing in primary care practices in Germany (Disease Analyser database).
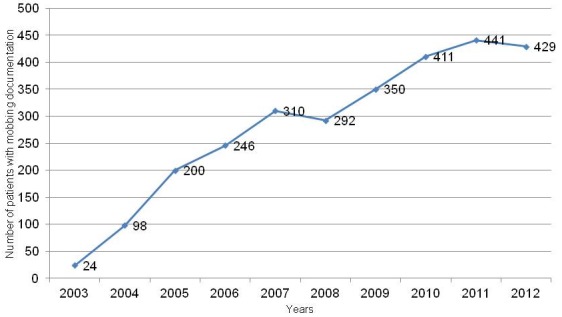
Certain diseases (indicated using their ICD-10-codes) that occurred within one year before mobbing was reported (“index date”) are listed in Table 2 (Tab. 2). Results are separated for subjects with (second column) and without (third column) a history of workplace mobbing and an asterisk indicates statistical significance (p<0.05).
Table 2. Prevalence of diseases occurring within 1 year before the mobbing experience, separated for patients with (second column) and without (third column) victimization.
As can be seen from this information, the most common disorders by far in mobbing patients were diseases of the respiratory system (ICD 10: J00–J99) and of the musculoskeletal system and connective tissue (ICD 10:M00–M99); both were almost twice as prevalent in these patients as in patients who did not subsequently report mobbing (prevalence: 43.5% vs. 20.5% and 37.8% vs. 20.4%, respectively). Other diseases such as disorders of the digestive system (ICD 10: K00–K93) or of the circulatory system (ICD 10: I00–I99) were considerably less prevalent (in mobbing patients: 20.3% and 20.9% respectively; in control group patients: 10.0% and 11.9%, respectively), but still detected significantly more often in those who would later become victims of mobbing. Indeed, all of the diseases listed occurred considerably more frequently in patients who later became subjects of mobbing.
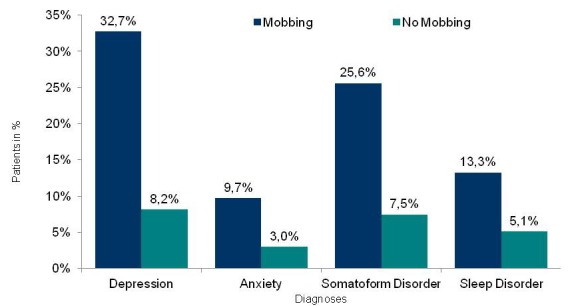
After adjustment for all diagnoses prior to index date (“diagnosis of mobbing”) using a regression model so as to ensure that mobbing was indeed the contributing factor, analysis displayed the highest odds ratio of 4.28 (95% confidence interval (CI), 3.62–5.07) for depression (Table 3 (Tab. 3)) (p<0.0001). The lowest value detected was that for sleep disorders; however, the incidence of this disease was still more than twice as high as that in patients without mobbing experience (odds ratio, 2.4; 95% CI, 1.93–2.99; p<0.0001). Other diseases with a considerably higher incidence included anxiety and somatoform disorders (both p<0.0001). Figure 3 (Fig. 3) compares disease prevalence in affected and non-affected patients. Again, the biggest difference detected was with regard to depression, which had a prevalence of 32.7% in mobbing victims compared to 8.2% in unaffected peers. Concerning anxiety, prevalence was three times higher in bullying victims (9.7% versus 3%, respectively).
Table 3. Impact of workplace mobbing experience on prevalence of psychiatric and neurological diseases (logistic regression analysis).
Figure 3. Incidence of defined psychiatric and neurological diseases in patients with and without documentation of workplace mobbing.
Discussion
Mobbing has emerged as a global phenomenon in the working population within the last years and our study also revealed a continuous rise over a 10-year observation period. Consequently, it now has significant socioeconomic consequences in the form of deteriorating workplace performance, long absences from work or the need to replace affected staff [14]. In the present study, we not only analyzed the incidence of diseases that occurred after mobbing took place (after adjustment for all diagnoses prior to index date, so that mobbing can be regarded as the disease-causing factor), but also examined the prevalence of diseases that were diagnosed within one year before the mobbing experience. We found that diseases in general were considerably more prevalent in patients who later became victims of mobbing as compared with a control group, encompassing diseases of the respiratory, circulatory and digestive system as well as of the musculoskeletal system and connective tissue. Thus, it can be stated that subsequent mobbing victims are more prone to diseases even before their experience of mobbing, which may trigger the bullying since these subjects appear more vulnerable than others. Other reasons may include long periods of workplace absenteeism due to illness, possibly leading to overwork for colleagues, who become mobbing perpetrators as a consequence and isolate the member of staff who is ill. The fact that higher prevalence is not confined to neurologic-psychiatric disorders is in contrast to the findings presented previously in the existing literature, which referred in particular to the higher prevalence of diseases of the neurologic-psychiatric spectrum (e.g. emotional exhaustion, psychological distress) in subsequent mobbing victims [9], [28], [29]. Moreover, it underlines that victimization does not necessarily require psychiatric, personality or coping problems as underlying factors, although Kreiner et al. reported a tendency towards higher levels of stress and symptoms of depression, and a lower quality of life in mobbing victims with a pre-existing psychiatric disease [25], [28].
When compared with a healthy control group that matched on the basis of age, gender and insurance status, mobbing victims in our study had a significantly higher risk of suffering from depression, anxiety, somatoform disorders or sleep disorders. Moreover, these diseases were demonstrated to be considerably more prevalent in bullying victims. Some of these results have been described in literature before, in which a reciprocal association of mobbing victimization with low self-esteem [30], anxiety [13], [31], sleep disturbances [32] and depression [22], [33], [34], [35] was demonstrated, but our study is the first to directly compare mobbing victims with non-affected matches. Recently, Dobry et al. [7] described as the worst-case outcome of bullying an increased likelihood of psychiatric disorders including depression, posttraumatic stress disorder, anxiety disorders, substance abuse and suicidal behavior. Interestingly, this finding applied to both the victims and the perpetrators of mobbing. In addition to the aforementioned sequelae of bullying, victimization was shown to negatively influence health security and confidence in ability [12] and may increase the risk of developing psychotic experiences [36] or chronic diseases [11].
Several studies have assessed the risk of experiencing verbal, physical, and relational victimization and detected a positive relationship with increased body mass index (BMI) in cross-sectional [11], [37] and longitudinal studies [38]. These studies also mediated the coincidence of BMI with social phobia, depression, suicidality, and low self-esteem in adolescents [21], for example by raising adolecents’ levels of anticipatory anxiety of being bullied again in situations of social interaction or by conveying a sense of helplessness and hopelessness to them [21].
However, it is not only the BMI but also the gender that places people at risk of becoming victims of mobbing. Although Ortega et al. [39] and Kivimäki et al. [11] did not find significant age- or gender-related differences, most other publications reported that women were at a higher risk of getting bullied at work [1], [2], [28], [40], which is in line with the findings of our own study, which revealed that two-thirds of mobbing victims were female. While mobbing mainly focuses on criticisms and rumors concerning the private life in women, it often concentrates on work performance in men [1]. Other authors described risk factors for workplace mobbing such as occupational status (people with higher levels of education tend to have lower alert thresholds to negative situations [1]), long working hours, job insecurity, and night shift work [39], [41]. As found by Klomek at al. [34], [42] adolescents who were both a bullies and victims of bullying were at the highest risk with regard to substance abuse, violent or physically aggressive behavior, and suicidal tendencies, whereby substance abuse may further increase an adolescent’s risk of suicidal tendencies [40], [43], [44].
We recognize the following limitations of our study: firstly, perceived victimization of mobbing was measured using a single, self-labeling question and no survey of peers, parents and/or marriage partners was conducted, although it is well known that data collection from different sources is the most suitable way to evaluate the real causal relationship. Thus, instances of mobbing are determined based on subjective data as doctors are not able to directly verify the occurrence of the instance of bullying reported [1]. In addition, data may be biased by the fact that women are known to more readily report work problems, while men, in line with the stereotype, tend to neglect such problems due to the fact that they see themselves as the breadwinner of the family, managing the family through their work. Thirdly, we did not separate data for patients in terms of their working environment (e.g. healthcare sector) or job position, although, as mentioned before, well-established differences exist in this context. However, we aimed to carry out a survey on mobbing victimization that would include as many participants as possible and therefore did not use sub-segmentation. Moreover, the control group was matched with the mobbing victim group only on the basis of age, gender, and health insurance status but not workplace environment, which might also have influenced our analysis.
To sum up, our study was the first that demonstrated a general susceptibility to diseases in people even before they had experienced mobbing. These diseases included disorders of the respiratory, circulatory, and musculoskeletal systems. After their experiences of bullying, these people have demonstrated considerably higher levels of depression, anxiety, somatoform disorders and sleep disorders as compared with peers who have not been victims of mobbing. Thus, our study underlines the importance of supporting (chronically) ill staff in order to prevent them from becoming victims of mobbing and suffering from psychiatric disorders later on, which may create a vicious cycle. As suggested previously by other authors [1], such preventive measures for the individual should include a personal training that teaches the person concerned in dealing with conflict using verbal self-defense and behavioral techniques.
Notes
Competing interests
The authors declare that they have no competing interests.
Data protection
In connection with data/figures used terms, such as “patient, doctor, medical practice, prescriber or pharmacy”, do not designate any personal data but exclusively anonymous information (in accordance with § 3 Abs. 6 “Bundesdatenschutzgesetz” – German Federal Data Protection Act).
References
- 1.Tonini S, Lanfranco A, Dellabianca A, Lumelli D, Giorgi I, Mazzacane F, Fusi C, Scafa F, Candura SM. Work-related stress and bullying: gender differences and forensic medicine issues in the diagnostic procedure. J Occup Med Toxicol. 2011;6(1):29. doi: 10.1186/1745-6673-6-29. Available from: http://dx.doi.org/10.1186/1745-6673-6-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Figueiredo-Ferraz H, Gil-Monte PR, Olivares-Faúndez VE. Influence of mobbing (workplace bullying) on depressive symptoms: a longitudinal study among employees working with people with intellectual disabilities. J Intellect Disabil Res. 2013 Aug 6; doi: 10.1111/jir.12084. Available from: http://dx.doi.org/10.1111/jir.12084. [DOI] [PubMed] [Google Scholar]
- 3.Sperry L. Mobbing and bullying: the influence of individual, work group, and organizational dynamics on abusive workplace behavior. Consult Psychol J Pract Res. 2009;61(3):190–201. doi: 10.1037/a0016938. Available from: http://dx.doi.org/10.1037/a0016938. [DOI] [Google Scholar]
- 4.Takaki J, Tsutsumi A, Fujii Y, Taniguchi T, Hirokawa K, Hibino Y, Lemmer RJ, Nashiwa H, Wang DH, Ogino K. Assessment of workplace bullying and harassment: reliability and validity of a Japanese version of the negative acts questionnaire. J Occup Health. 2010;52(1):74–81. doi: 10.1539/joh.O9011. Available from: http://dx.doi.org/10.1539/joh.O9011. [DOI] [PubMed] [Google Scholar]
- 5.Ostendorf GM. Mobbing: Arbeitsunfähigkeit oder nur "ArbeitsplatzunverträgIichkeit"? [Mobbing: bullying or just "workplace acceptability"?]. Versicherungsmedizin. 2013 Jun 1;65(2):101. (Ger). [PubMed] [Google Scholar]
- 6.Leymann H. The content and development of mobbing at work. Eur J Work Organ Psychol. 1996;5(2):165–184. doi: 10.1080/13594329608414853. Available from: http://dx.doi.org/10.1080/13594329608414853. [DOI] [Google Scholar]
- 7.Dobry Y, Braquehais MD, Sher L. Bullying, psychiatric pathology and suicidal behavior. Int J Adolesc Med Health. 2013;25(3):295–299. doi: 10.1515/ijamh-2013-0065. Available from: http://dx.doi.org/10.1515/ijamh-2013-0065. [DOI] [PubMed] [Google Scholar]
- 8.Simons S, Sauer P. An exploration of the workplace bullying experience: coping strategies used by nurses. J Nurses Prof Dev. 2013 Sep-Oct;29(5):228–232. doi: 10.1097/01.NND.0000433147.33631.c9. Available from: http://dx.doi.org/10.1097/01.NND.0000433147.33631.c9. [DOI] [PubMed] [Google Scholar]
- 9.Chipps E, Stelmaschuk S, Albert NM, Bernhard L, Holloman C. Workplace bullying in the OR: Results of a descriptive study. AORN J. 2013 Nov;98(5):479–493. doi: 10.1016/j.aorn.2013.08.015. Available from: http://dx.doi.org/10.1016/j.aorn.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 10.Hutchinson M, Jackson D. Hostile clinician behaviours in the nursing work environment and implications for patient care: a mixed-methods systematic review. BMC Nurs. 2013;12(1):25. doi: 10.1186/1472-6955-12-25. Available from: http://dx.doi.org/10.1186/1472-6955-12-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kivimäki M, Elovainio M, Vahtera J. Workplace bullying and sickness absence in hospital staff. Occup Environ Med. 2000 Oct;57(10):656–660. doi: 10.1136/oem.57.10.656. Available from: http://dx.doi.org/10.1136/oem.57.10.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whiteside D, Stubbs B, Soundy A. Physiotherapy students' experiences of bullying on clinical internships: a qualitative study. Physiotherapy. 2014 Mar;100(1):41–46. doi: 10.1016/j.physio.2013.06.005. Available from: http://dx.doi.org/10.1016/j.physio.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 13.Reknes I, Pallesen S, Magerøy N, Moen BE, Bjorvatn B, Einarsen S. Exposure to bullying behaviors as a predictor of mental health problems among Norwegian nurses: results from the prospective SUSSH-survey. Int J Nurs Stud. 2014 Mar;51(3):479–487. doi: 10.1016/j.ijnurstu.2013.06.017. Available from: http://dx.doi.org/10.1016/j.ijnurstu.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 14.Stagg SJ, Sheridan DJ, Jones RA, Speroni KG. Workplace bullying: the effectiveness of a workplace program. Workplace Health Saf. 2013 Aug;61(8):333–338. doi: 10.3928/21650799-20130716-03. Available from: http://dx.doi.org/10.3928/21650799-20130716-03. [DOI] [PubMed] [Google Scholar]
- 15.Tuckey MR, Dollard MF, Hosking PJ, Winefield AH. Workplace bullying: the role of psychosocial environment factors. Int J Stress Manag. 2009;16(3):215–232. doi: 10.1037/a0016841. Available from: http://dx.doi.org/10.1037/a0016841. [DOI] [Google Scholar]
- 16.Litwiller BJ, Brausch AM. Cyber bullying and physical bullying in adolescent suicide: the role of violent behavior and substance use. J Youth Adolesc. 2013 May;42(5):675–684. doi: 10.1007/s10964-013-9925-5. Available from: http://dx.doi.org/10.1007/s10964-013-9925-5. [DOI] [PubMed] [Google Scholar]
- 17.Levy N, Cortesi S, Gasser U, Crowley E, Beaton M, Casey J, Nolan C. Bullying in a Networked Era: A Literature Review. Berkman Center Research Publication. 2012 doi: 10.2139/ssrn.2146877. Available from: http://dx.doi.org/10.2139/ssrn.2146877. [DOI] [Google Scholar]
- 18.European Commission, DG for Employment, Social Affairs, and Equal Opportunities. Report on equality between women and men, 2004. Luxembourg: Office for Official Publications of the European Communities; 2005. [Google Scholar]
- 19.McCabe RE, Antony MM, Summerfeldt LJ, Liss A, Swinson RP. Preliminary examination of the relationship between anxiety disorders in adults and self-reported history of teasing or bullying experiences. Cogn Behav Ther. 2003;32(4):187–193. doi: 10.1080/16506070310005051. Available from: http://dx.doi.org/10.1080/16506070310005051. [DOI] [PubMed] [Google Scholar]
- 20.Nansel TR, Craig W, Overpeck MD, Saluja G, Ruan WJ Health Behaviour in School-aged Children Bullying Analyses Working Group. Cross-national consistency in the relationship between bullying behaviors and psychosocial adjustment. Arch Pediatr Adolesc Med. 2004 Aug;158(8):730–736. doi: 10.1001/archpedi.158.8.730. Available from: http://dx.doi.org/10.1001/archpedi.158.8.730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yen CF, Liu TL, Ko CH, Wu YY, Cheng CP. Mediating effects of bullying involvement on the relationship of body mass index with social phobia, depression, suicidality, and self-esteem and sex differences in adolescents in Taiwan. Child Abuse Negl. 2014 Mar;38(3):517–526. doi: 10.1016/j.chiabu.2013.07.015. Available from: http://dx.doi.org/10.1016/j.chiabu.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 22.Niedhammer I, David S, Degioanni S. Association between workplace bullying and depressive symptoms in the French working population. J Psychosom Res. 2006 Aug;61(2):251–259. doi: 10.1016/j.jpsychores.2006.03.051. Available from: http://dx.doi.org/10.1016/j.jpsychores.2006.03.051. [DOI] [PubMed] [Google Scholar]
- 23.Kim YS, Leventhal B. Bullying and suicide. A review. Int J Adolesc Med Health. 2008 Apr-Jun;20(2):133–154. doi: 10.1515/IJAMH.2008.20.2.133. Available from: http://dx.doi.org/10.1515/IJAMH.2008.20.2.133. [DOI] [PubMed] [Google Scholar]
- 24.Kim YS, Leventhal BL, Koh YJ, Boyce WT. Bullying increased suicide risk: prospective study of Korean adolescents. Arch Suicide Res. 2009;13(1):15–30. doi: 10.1080/13811110802572098. Available from: http://dx.doi.org/10.1080/13811110802572098. [DOI] [PubMed] [Google Scholar]
- 25.Kreiner B, Sulyok C, Rothenhäusler HB. Führt Mobbing zur posttraumatischen Belastungsstörung? Implikationen von Stressverarbeitung und Persönlichkeit. [Does mobbing cause posttraumatic stress disorder? Impact of coping and personality]. Neuropsychiatr. 2008;22(2):112–123. (Ger). [PubMed] [Google Scholar]
- 26.Ogdie A, Langan SM, Parkinson J, Dattani H, Kostev K, Gelfand JM. Medical Record Databases. In: Strom BL, Kimmel SE, Hennessy S, editors. Pharmacoepidemiology. 5th ed. Oxford: Wiley-Blackwell; 2012. pp. 224–243. Available from: http://dx.doi.org/10.1002/9781119959946.ch15. [DOI] [Google Scholar]
- 27.Becher H, Kostev K, Schröder-Bernhardi D. Validity and representativeness of the "Disease Analyzer" patient database for use in pharmacoepidemiological and pharmacoeconomic studies. Int J Clin Pharmacol Ther. 2009 Oct;47(10):617–626. doi: 10.5414/CPP47617. Available from: http://dx.doi.org/10.5414/CPP47617. [DOI] [PubMed] [Google Scholar]
- 28.Drabek M, Merecz D. Job stress, occupational position and gender as factors differentiating workplace bullying experience. Med Pr. 2013;64(3):283–296. [PubMed] [Google Scholar]
- 29.Nielsen MB, Hetland J, Matthiesen SB, Einarsen S. Longitudinal relationships between workplace bullying and psychological distress. Scand J Work Environ Health. 2012 Jan;38(1):38–46. doi: 10.5271/sjweh.3178. Available from: http://dx.doi.org/10.5271/sjweh.3178. [DOI] [PubMed] [Google Scholar]
- 30.Juvonen J, Nishina A, Graham S. Peer harassment, psychological adjustment, and school functioning in early adolescence. J Educ Psychol. 2000;92(2):349–59. doi: 10.1037/0022-0663.92.2.349. Available from: http://dx.doi.org/10.1037/0022-0663.92.2.349. [DOI] [Google Scholar]
- 31.Kumpulainen K, Räsänen E, Henttonen I, Almqvist F, Kresanov K, Linna SL, Moilanen I, Piha J, Puura K, Tamminen T. Bullying and psychiatric symptoms among elementary school-age children. Child Abuse Negl. 1998 Jul;22(7):705–717. doi: 10.1016/S0145-2134(98)00049-0. Available from: http://dx.doi.org/10.1016/S0145-2134(98)00049-0. [DOI] [PubMed] [Google Scholar]
- 32.Niedhammer I, David S, Degioanni S, Drummond A, Philip P, Acquarone D, Aicardi F, André-Mazeaud P, Arsento M, Astier R, Baille H, Bajon-Thery F, Barre E, Basire C, Battu JL, et al. Workplace bullying and sleep disturbances: findings from a large scale cross-sectional survey in the French working population. Sleep. 2009 Sep;32(9):1211–1219. doi: 10.1093/sleep/32.9.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fekkes M, Pijpers FI, Verloove-Vanhorick SP. Bullying behavior and associations with psychosomatic complaints and depression in victims. J Pediatr. 2004 Jan;144(1):17–22. doi: 10.1016/j.jpeds.2003.09.025. Available from: http://dx.doi.org/10.1016/j.jpeds.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 34.Klomek AB, Kleinman M, Altschuler E, Marrocco F, Amakawa L, Gould MS. High school bullying as a risk for later depression and suicidality. Suicide Life Threat Behav. 2011 Oct;41(5):501–516. doi: 10.1111/j.1943-278X.2011.00046.x. Available from: http://dx.doi.org/10.1111/j.1943-278X.2011.00046.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stock SR, Tissot F. Are there health effects of harassment in the workplace? A gender-sensitive study of the relationships between work and neck pain. Ergonomics. 2012;55(2):147–159. doi: 10.1080/00140139.2011.598243. Available from: http://dx.doi.org/10.1080/00140139.2011.598243. [DOI] [PubMed] [Google Scholar]
- 36.Wolke D, Copeland WE, Angold A, Costello EJ. Impact of bullying in childhood on adult health, wealth, crime, and social outcomes. Psychol Sci. 2013 Oct;24(10):1958–1970. doi: 10.1177/0956797613481608. Available from: http://dx.doi.org/10.1177/0956797613481608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.BeLue R, Francis LA, Colaco B. Mental health problems and overweight in a nationally representative sample of adolescents: effects of race and ethnicity. Pediatrics. 2009 Feb;123(2):697–702. doi: 10.1542/peds.2008-0687. Available from: http://dx.doi.org/10.1542/peds.2008-0687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Griffiths LJ, Wolke D, Page AS, Horwood JP ALSPAC Study Team. Obesity and bullying: different effects for boys and girls. Arch Dis Child. 2006 Feb;91(2):121–125. doi: 10.1136/adc.2005.072314. Available from: http://dx.doi.org/10.1136/adc.2005.072314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ortega A, Høgh A, Pejtersen JH, Feveile H, Olsen O. Prevalence of workplace bullying and risk groups: a representative population study. Int Arch Occup Environ Health. 2009 Feb;82(3):417–426. doi: 10.1007/s00420-008-0339-8. Available from: http://dx.doi.org/10.1007/s00420-008-0339-8. [DOI] [PubMed] [Google Scholar]
- 40.Smith PK, Singer M, Hoel H, Cooper CL. Victimization in the school and the workplace: are there any links? Br J Psychol. 2003 May;94(Pt 2):175–188. doi: 10.1348/000712603321661868. Available from: http://dx.doi.org/10.1348/000712603321661868. [DOI] [PubMed] [Google Scholar]
- 41.Lee HE, Kim HR, Park JS. Work-related Risk Factors for Workplace Violence among Korean Employees. J Occup Health. 2014 Apr 17;56(1):12–20. doi: 10.1539/joh.13-0082-oa. [DOI] [PubMed] [Google Scholar]
- 42.Klomek AB, Kleinman M, Altschuler E, Marrocco F, Amakawa L, Gould MS. Suicidal adolescents' experiences with bullying perpetration and victimization during high school as risk factors for later depression and suicidality. J Adolesc Health. 2013 Jul;53(1 Suppl):S37–S42. doi: 10.1016/j.jadohealth.2012.12.008. Available from: http://dx.doi.org/10.1016/j.jadohealth.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 43.Deykin EY, Buka SL. Suicidal ideation and attempts among chemically dependent adolescents. Am J Public Health. 1994 Apr;84(4):634–639. doi: 10.2105/AJPH.84.4.634. Available from: http://dx.doi.org/10.2105/AJPH.84.4.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bolognini M, Plancherel B, Laget J, Halfon O. Adolescent's suicide attempts: populations at risk, vulnerability, and substance use. Subst Use Misuse. 2003 Sep-Nov;38(11-13):1651–1669. doi: 10.1081/JA-120024235. Available from: http://dx.doi.org/10.1081/JA-120024235. [DOI] [PubMed] [Google Scholar]