Abstract
In-utero exposure to endocrine-disrupting compounds, including dichlorodiphenyltrichloroethane (DDT) and its metabolite dichlorodiphenylethylene (DDE), has been hypothesized to increase the risk of obesity later in life. We examined the associations of maternal serum concentrations of DDT and DDE during pregnancy with body mass index, obesity, waist circumference, and percentage of body fat in 9-year-old children (n = 261) in the Center for the Health Assessment of Mothers and Children of Salinas (CHAMACOS) Study, a longitudinal birth cohort study in the Salinas Valley, California (2000–2010). We found associations between prenatal exposure to DDT and DDE and several measures of obesity at 9 years of age in boys but not in girls. For example, among boys, 10-fold increases in prenatal DDT and DDE concentrations were associated with increased odds of becoming overweight or obese (for o,p′-DDT, adjusted odds ratio (OR) = 2.5, 95% confidence interval (CI): 1.0, 6.3; for p,p′-DDT, adjusted OR = 2.1, 95% CI: 1.0, 4.5; and for p,p′-DDE, adjusted OR = 1.97, 95% CI: 0.94, 4.13). The odds ratios for girls were nonsignificant. Results were similar for body mass index z score, waist circumference z score, and odds of increased waist circumference but were less consistent for percentage of body fat. The difference by sex persisted after considering pubertal status. These results provide support for the chemical obesogen hypothesis.
Keywords: body mass index, children, dichlorodiphenyldichloroethylene, dichlorodiphenyltrichloroethane, obesity, prenatal exposure
In-utero exposure to endocrine-disrupting compounds has been hypothesized to increase the risk of obesity later in life (1–4). Increasing evidence from studies in animals supports a potential role for endocrine-disrupting compounds, either directly or indirectly, in the pathogenesis of obesity (4–9). Early-life exposure might alter development of adipose tissue by affecting the number, size, and distribution of adipocytes or the larger regulatory systems involved in weight homeostasis (10).
Dichlorodiphenyltrichloroethane (DDT) and its breakdown product dichlorodiphenyldichloroethylene (DDE) are persistent organic pollutants and known endocrine disruptors (11). Experimental studies have shown a link between exposure DDT and DDE and adipose dysfunction. In vitro, p,p′-DDT has been shown to alter adipocyte differentiation, and the effects correlate with changes in expression of CCAAT-enhancer binding protein-α and peroxisome proliferator–activated receptor-γ, transcription factors that are thought to play an important role in adipogenesis (12). Likewise, p,p′-DDE has been shown to increase basal free fatty acid uptake (13). In animal studies, rats fed DDE-contaminated salmon oil in combination with a high-fat diet developed abdominal obesity and insulin resistance (14, 15).
Several longitudinal birth cohort studies have examined the relationship of prenatal exposure to DDT and DDE with child growth (16–22). Positive associations between prenatal DDT and DDE exposure and body mass index (BMI; weight (kg)/height (m)2) z score or overweight status have been reported in birth cohorts in Europe (17–19) in which the follow-up ages ranged from 1 to 7 years, but these associations were not found in the United States (21, 22) or Mexico (16, 20).
In Spain, elevated maternal serum DDE concentration was associated with an increased risk of being overweight (BMI z score ≥85th percentile) in 518 children at 14 months of age (19). DDT was measured but not analyzed because of the low detection frequency. Additionally, in 138 Belgian children, higher cord blood DDE levels were associated with an increased BMI standard deviation score at 3 years of age; DDT was not measured (17). Among 344 children in Spain, higher cord blood p,p′-DDT and p,p-DDE levels were nonmonotonically associated with increased BMI z score and odds of being overweight (≥85th percentile) at 6.5 years of age, but associations with p,p′-DDT were limited to boys (18).
In Mexico, no association was found between maternal serum DDT or DDE concentrations at delivery and BMI standard deviation score in 788 male children aged 5–38 months from Chiapas, where DDT was recently used (16); there was also no association between maternal serum DDE concentration and BMI z score at 12 months of age in 253 children from Morelos (20). In the Collaborative Perinatal Project birth cohort, which included births that occurred before DDT was banned in the United States, there was no clear association between maternal serum DDT and DDE concentrations and overweight (BMI >90th percentile) or obesity (BMI >97th percentile) status at 7 years of age, although estimates were more strongly positive for boys (21).
Using data from the Center for the Health Assessment of Mothers and Children of Salinas (CHAMACOS) Study, a longitudinal birth cohort study in a California agricultural community, we previously reported no association between prenatal DDT and DDE exposure and child obesity between the ages 2 and 7 years, but we did observe a significant trend toward a positive association as the children aged (22). Here, we report results from a subsequent follow-up of the cohort. Specifically, we examined the relationships of maternal serum concentrations of o,p′-DDT, p,p′-DDT, and p,p′-DDE (DDT and DDE) during pregnancy with child body size at 9 years of age, including BMI, waist circumference, percentage of body fat, and overweight or obese status. We also examined whether these relationships were modified by child sex or the onset of puberty.
METHODS
Study participants
The CHAMACOS Study is a longitudinal birth cohort study of environmental exposures and childhood growth and development. Pregnant women were recruited from prenatal clinics serving the farmworker population in the Salinas Valley, California, between October 1999 and October 2000. Eligible women were at least 18 years of age, at less than 20 weeks of gestation, and English or Spanish speakers who qualified for government-sponsored health insurance and planned to deliver at the county hospital. The study was approved by the institutional review boards at participating institutions. Before participation, we obtained written informed consent from all mothers and oral assent from all children who were 7 years of age or older.
Of the 601 women who were initially enrolled, 527 were followed through delivery of a singleton live birth that survived the neonatal period, and 417 provided a serum sample during pregnancy for DDT and DDE analysis. Complete follow-up interview and anthropometric measurements were available for 261 children at 9 years of age.
Procedure
Details of the study have been published previously (23). Briefly, women were interviewed in English or Spanish using structured questionnaires twice during pregnancy, after delivery, and when their children were 0.5, 1, 2, 3.5, 5, 7, and 9 years old. During each interview, we collected information about family sociodemographic characteristics, maternal characteristics, and pregnancy and medical histories, as well as child-based developmental milestone, diet, and behavioral information. At the 9-year visit, clinical Tanner staging was conducted by trained research staff. Children were considered to have entered puberty if they were stage 2+ for breast development for girls or stage 2+ for pubic hair or genital development for boys.
Children were weighed and measured by trained research staff at each visit. At the 9-year visit, we measured barefoot standing height to the nearest 0.1 cm using a stadiometer and standing weight to the nearest 0.1 kg using a bioimpedence scale (Tanita TBF-300A Body Composition Analyzer, Tanita Corporation of America, Inc., Arlington Heights, Illinois) that also measured percentage of body fat using “foot-to-foot” bioimpedance technology. The scale was set to child mode and the manufacturer's algorithm was used for calculation of percentage of body fat. We measured waist circumference to the nearest 0.1 cm by placing a measuring tape around the abdomen at the level of the iliac crest, parallel to the floor. Height and waist circumference were measured in triplicate and averaged for analysis.
Laboratory analysis
Maternal serum samples were collected using venipuncture at approximately 26 weeks of gestation (n = 242) or delivery (n = 19). Serum levels of o,p′-DDT, p,p′-DDT, and p,p′-DDE were measured using isotope dilution gas chromatography-high resolution mass spectrometry methods (24) and reported on a whole-weight basis (pg/g). Mean levels of detection for o,p′-DDT, p,p′-DDT, and p,p′-DDE were 1.3 (standard deviation (SD), 0.7), 1.5 (SD, 0.8), and 2.9 (SD, 1.5) pg/g serum, respectively. For nondetectable values, a serum level of one-half the detection limit was assigned (25). Lipid-adjusted values (ng/g) were calculated by dividing o,p′-DDT, p,p′-DDT, and p,p′-DDE on a whole-weight basis by total serum lipid content, estimated by enzymatic determination of triglycerides and total cholesterol (26).
Statistical analysis
Lipid-adjusted levels of o,p′-DDT, p,p′-DDT, and p,p′-DDE were log10-transformed and analyzed as continuous variables. We calculated age- and sex-specific BMI z scores and percentiles for each child using 2000 Centers for Disease Control and Prevention growth charts (27). Children who were in the 85th percentile of BMI or higher but lower than the 95th percentile were classified as overweight, and children who were in the 95th percentile or higher were classified as obese. We calculated age- and sex-specific waist circumference z scores and percentiles for each child using the National Health and Nutrition Examination Survey III reference data for Mexican-American children provided by Stephen Cook (Stephen Cook, MD, written communication, 2013) (28). Children who were in the 90th percentile or higher were classified as having increased waist circumference and were considered to be at risk for metabolic syndrome (29).
All statistical analyses were performed using Stata, version 11.2 (30). For all outcomes, we used generalized additive models with a 3-degrees-of-freedom cubic spline to evaluate the shape of the exposure-response curves in the full sample and in boys and girls separately. None of the digression from linearity tests were significant (P = 0.15), suggesting that the relationships were linear. We examined the relation of maternal serum DDT and DDE concentrations with continuous outcomes (BMI z score, waist circumference z score, and percentage of body fat) using multivariable linear regression and with categorical outcomes (overweight/obese (≥85th vs. <85th percentile) and increased waist circumference (≥90th vs. <90th percentile)) using multivariable logistic regression. We used multinomial logistic regression to examine the relation of maternal serum DDT and DDE concentrations with the 3-category weight outcome (obese, overweight, normal weight).
We considered the following variables as potential covariates. Maternal variables included socioeconomic status, educational level, marital status, country of birth, years in the United States at childbirth, age at pregnancy (years), prepregnancy BMI (determined using self-reported weight and measured height), weight gain during pregnancy (from medical records), smoking during pregnancy, and household food insecurity at the 9-year visit. Child variables included birthweight, birth order, breastfeeding (any or none), and behaviors at 9 years of age, including intakes of soda, sweetened beverages, and fast food and time spent watching television or playing outside. Covariates were included in the final models if they changed the coefficient for exposure (log10DDT or log10DDE) by more than 10%. Final models were adjusted for maternal time in the United States at birth and prepregnancy BMI. We considered effect modification by child sex in all analyses by including a cross-product term between exposure and sex. To assess the influence of pubertal status on the sex-stratified relationship between DDT and DDE exposure and child body size, we analyzed sex-specific models that included a cross-product term between exposure and pubertal status. Interaction P values <0.2 were considered significant.
We reanalyzed the final models first excluding 20 children who had a low birth weight (n = 8) and/or were preterm (n = 19) and then excluded 1 outlier with standardized residuals greater than 3 or less than −3. We also reran the final models using inverse probability weights to account for potential bias due to loss to follow-up (31).
RESULTS
Tables 1 and 2 present maternal and child characteristics by child BMI status at 9 years of age. Mothers were on average 26.3 (SD, 5.1) years of age at delivery, and most were Latina (98.1%), had lived in the United States for 5 years or less at birth (52.1%), had not completed high school (79.3%), and were living at or below the federal poverty line (69.3%). Nearly two-thirds (64.8%) of mothers were overweight or obese before pregnancy.
Table 1.
Maternal Characteristics by Child BMI Status at 9 Years of Age, Center for the Health Assessment of Mothers and Children of Salinas Study, 2000–2010
| Characteristic | No. | % | Child BMI Category at 9 Years of Agea |
|||||
|---|---|---|---|---|---|---|---|---|
| Normal |
Overweight |
Obese |
||||||
| No. | % | No. | % | No. | % | |||
| Total | 261 | 100.0 | 115 | 44.1 | 42 | 16.1 | 104 | 39.9 |
| Race/ethnicity | ||||||||
| Latina | 256 | 98.1 | 114 | 44.5 | 41 | 16.0 | 101 | 39.5 |
| Non-Latina | 5 | 1.9 | 1 | 20.0 | 1 | 20.0 | 3 | 60.0 |
| Years of residence in the United States | ||||||||
| ≤1 | 60 | 23.0 | 26 | 43.3 | 14 | 23.3 | 20 | 33.3 |
| 2–5 | 76 | 29.1 | 41 | 54.0 | 11 | 14.5 | 24 | 31.6 |
| 6–10 | 67 | 25.7 | 23 | 34.3 | 11 | 16.4 | 33 | 49.3 |
| ≥11 | 58 | 22.2 | 25 | 43.1 | 6 | 10.3 | 27 | 46.6 |
| Educational level | ||||||||
| ≤6th grade | 117 | 44.8 | 50 | 42.7 | 17 | 14.5 | 50 | 42.7 |
| 7th–12th grade | 90 | 34.5 | 39 | 43.3 | 17 | 18.9 | 34 | 37.8 |
| ≥High school | 54 | 20.7 | 26 | 48.2 | 8 | 14.8 | 20 | 37.0 |
| Household income | ||||||||
| At or below the poverty level | 181 | 69.3 | 79 | 43.7 | 31 | 17.1 | 71 | 39.2 |
| Above the poverty level | 80 | 30.7 | 36 | 45.0 | 11 | 13.8 | 33 | 41.3 |
| Prepregnancy BMIb | ||||||||
| Underweight/normal | 92 | 35.3 | 52 | 56.5 | 18 | 19.6 | 22 | 23.9 |
| Overweight | 101 | 38.7 | 50 | 49.5 | 14 | 13.9 | 37 | 36.6 |
| Obese | 68 | 26.1 | 13 | 19.1 | 10 | 14.7 | 45 | 66.2 |
| Weight gain during pregnancy, lbsc | 28.5 (12.2) | 27.7 (10.1) | 31.5 (12.7) | 28.1 (13.9) | ||||
| Smoking during pregnancyb | ||||||||
| No | 252 | 96.6 | 114 | 45.2 | 41 | 16.3 | 97 | 38.5 |
| Yes | 9 | 3.5 | 1 | 11.1 | 1 | 11.1 | 7 | 77.8 |
| Age at delivery, years | ||||||||
| <25 | 105 | 40.2 | 48 | 45.7 | 16 | 15.2 | 41 | 39.1 |
| 25–34 | 133 | 51.0 | 60 | 45.1 | 22 | 16.5 | 51 | 38.4 |
| >34 | 23 | 8.8 | 7 | 30.4 | 4 | 17.4 | 12 | 52.2 |
| Breastfeeding duration, months | ||||||||
| 0–2 | 63 | 24.1 | 32 | 50.8 | 9 | 14.3 | 22 | 34.9 |
| >2–6 | 66 | 25.3 | 28 | 42.4 | 13 | 19.7 | 25 | 37.9 |
| >6–12 | 57 | 21.8 | 28 | 49.1 | 10 | 17.5 | 19 | 33.3 |
| >12 | 75 | 28.7 | 27 | 36.0 | 10 | 13.3 | 38 | 50.7 |
Abbreviation: BMI, body mass index.
a Weight (kg)/height (m)2. Normal indicates a BMI below the 85th percentile of sex-specific BMI for age; overweight, BMI in the 85th percentile or higher but below the 95th percentile of sex-specific BMI for age; and obese, BMI in the 95th percentile or higher of sex-specific BMI for age.
b P < 0.05 on χ2 test (for variables with cell frequencies >5) or Fisher's exact test (for variables with at least one cell frequency ≤5).
c Values are presented as mean (SD).
Table 2.
Child Characteristics by Child BMI Status at 9 Years of Age, Center for the Health Assessment of Mothers and Children of Salinas Study, 2000–2010
| Characteristic | No. | % | Mean (SD) | Child BMI Category at 9 Years of Agea |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal |
Overweight |
Obese |
||||||||||
| No. | % | Mean (SD) | No. | % | Mean (SD) | No. | % | Mean (SD) | ||||
| Total | 261 | 100.0 | 115 | 44.1 | 42 | 16.1 | 104 | 39.9 | ||||
| Sex | ||||||||||||
| Male | 118 | 45.2 | 48 | 40.7 | 24 | 20.3 | 46 | 39.0 | ||||
| Female | 143 | 54.8 | 67 | 46.9 | 18 | 12.6 | 58 | 40.6 | ||||
| Birthweight, gb | 3,458 (492) | 3,350 (449) | 3,499 (549) | 3,560 (492) | ||||||||
| Age at 9-year follow-up, years | 9.1 (0.2) | 9.1 (0.2) | 9.1 (0.1) | 9.2 (0.3) | ||||||||
| Onset of puberty by 9 years of age | ||||||||||||
| Boys | ||||||||||||
| No | 101 | 85.6 | 43 | 42.6 | 18 | 17.8 | 40 | 39.6 | ||||
| Yes | 13 | 11.0 | 4 | 30.8 | 5 | 38.5 | 4 | 30.8 | ||||
| Missing | 4 | 3.4 | 1 | 25.0 | 1 | 25.0 | 2 | 50.0 | ||||
| Girlsb | ||||||||||||
| No | 82 | 57.3 | 47 | 57.3 | 9 | 11.0 | 26 | 31.7 | ||||
| Yes | 54 | 37.8 | 19 | 35.2 | 8 | 14.8 | 27 | 50.0 | ||||
| Missing | 7 | 4.9 | 1 | 14.3 | 1 | 14.3 | 5 | 71.4 | ||||
| Time per day spent watching television at 9 years of agec | ||||||||||||
| <1 hour | 38 | 14.7 | 14 | 36.8 | 9 | 23.7 | 15 | 39.5 | ||||
| 1–2 hours | 82 | 31.7 | 41 | 50.0 | 13 | 15.9 | 28 | 34.2 | ||||
| >2 hours | 139 | 53.7 | 59 | 42.5 | 19 | 13.7 | 61 | 43.9 | ||||
| Time per day spent playing outside at 9 years of agec | ||||||||||||
| <1 hour | 36 | 13.9 | 17 | 47.2 | 5 | 13.9 | 14 | 38.9 | ||||
| 1–2 hours | 143 | 55.0 | 64 | 44.8 | 24 | 16.8 | 55 | 38.5 | ||||
| >2 hours | 81 | 31.2 | 33 | 40.7 | 13 | 16.1 | 35 | 43.2 | ||||
| No. of sodas consumed at 9 years of age | ||||||||||||
| <1 per week | 107 | 41.0 | 47 | 43.9 | 20 | 18.7 | 40 | 37.4 | ||||
| 1–6 per week | 127 | 48.7 | 56 | 44.1 | 21 | 16.5 | 50 | 39.4 | ||||
| ≥1 per day | 27 | 10.3 | 12 | 44.4 | 1 | 3.7 | 14 | 51.9 | ||||
| No. of sugar-sweetened beverages consumed per day at 9 years of age | ||||||||||||
| <1 | 59 | 22.6 | 21 | 35.6 | 9 | 15.3 | 29 | 49.2 | ||||
| 1 | 139 | 53.3 | 65 | 46.8 | 23 | 16.6 | 51 | 36.7 | ||||
| ≥1 | 63 | 24.1 | 29 | 46.0 | 10 | 15.9 | 24 | 38.1 | ||||
| No. of fast food meals consumed per week at 9 years of agec | ||||||||||||
| <1 | 102 | 39.2 | 38 | 37.3 | 20 | 19.6 | 44 | 43.1 | ||||
| 1–2 | 150 | 57.7 | 75 | 50.0 | 20 | 13.3 | 55 | 36.7 | ||||
| ≥3 | 8 | 3.1 | 1 | 12.5 | 2 | 25.0 | 5 | 62.5 | ||||
| Body mass indexb | 1.09 (1.09) | 0.02 (0.69) | 1.41 (0.17) | 2.13 (0.28) | ||||||||
| Percentile of waist circumferenceb | 1.08 (0.91) | 0.25 (0.58) | 1.26 (0.35) | 1.92 (0.40) | ||||||||
| <90th | 139 | 53.3 | 113 | 81.3 | 21 | 15.1 | 5 | 3.6 | ||||
| ≥90th | 122 | 46.7 | 2 | 1.6 | 21 | 17.2 | 99 | 81.2 | ||||
| Body fat percentaged | 27.7 (10.3) | 18.3 (5.6) | 27.9 (4.4) | 37.2 (6.1) | ||||||||
| o,p′-DDT, ng/ge | 1.2 (0.7–3.3) | 1.0 (0.6–2.7) | 1.5 (0.8–3.5) | 1.5 (0.8–4.3) | ||||||||
| p,p′-DDT, ng/ge | 12.1 (7.6–42.6) | 10.8 (7.6–24.9) | 17.9 (7.0–158.0) | 14.2 (7.6–53.4) | ||||||||
| p,p′-DDE, ng/ge | 1,104 (613–2,710) | 982 (548–2,153) | 1,638 (706–6,957) | 1,152 (649–2,886) | ||||||||
Abbreviations: BMI, body mass index; DDE, dichlorodiphenyldichloroethylene; DDT, dichlorodiphenyltrichloroethane; SD, standard deviation.
a Weight (kg)/height (m)2. Normal indicates a BMI below the 85th percentile of sex-specific BMI for age; overweight, BMI in the 85th percentile or higher but below the 95th percentile of sex-specific BMI for age; and obese, BMI in the 95th percentile or higher of sex-specific BMI for age.
b P < 0.05 on χ2 test (for variables with cell frequencies >5) or Fisher's exact test (for variables with at least one cell frequency ≤5).
c Numbers do not add to the total because of missing data for time spent watching television at 9 years of age (n = 2), outside play time at 9 years of age (n = 1), and fast food consumption at 9 years of age (n = 1).
d Body fat percentages were available for 224 children.
e Median (interquartile range) are presented for o,p′-DDT, p,p′-DDT, and p,p′-DDE rather than mean (SD).
Children were assessed close to their 9th birthday (mean age = 9.1 (SD, 0.2) years,) and 54.8% were female (Table 2). At 9 years of age, 37.8% of girls and 11.0% of boys had entered puberty. Children watched television an average of 2.1 (SD, 1.2) hours per day and played outside an average of 2.1 (SD, 1.5) hours per day. More than 10% of children consumed 1 or more sodas per day, 77.4% consumed at least 1 sugar-sweetened beverage per day, and 60.8% consumed at least 1 fast food meal per week.
At 9 years of age, the mean BMI z score was 1.09 (SD, 1.09), with 16.1% of children classified as overweight and 39.9% classified as obese. Mean waist circumference z score and percentage of body fat for the group were 1.08 (SD, 0.91) and 27.7% (SD, 10.3), respectively. A total of 122 (46.7%) children had increased waist circumference, and of these, 120 (98%) were also overweight or obese.
As presented in Tables 1 and 2, overweight or obese children were more likely to have a mother who was obese before pregnancy (P < 0.01), a mother who smoked during pregnancy (P = 0.05), and a higher birth weight (P < 0.01). There was no significant difference in obesity status of children by maternal sociodemographic indicators. The association with covariates was similar when other obesity measures were considered (data not shown).
Maternal serum levels of o,p′-DDT, p,p′-DDT, and p,p′-DDE at pregnancy were above the detection limit in 96%, 100%, and 100% of samples, respectively. The median serum levels were 1.2 (interquartile range, 0.7–3.3) ng/g lipid for o,p′-DDT, 12.1 (interquartile range, 7.6–42.6) ng/g lipid for p,p′-DDT, and 1,103.6 (interquartile range, 612.6–2,709.8) ng/g lipid for p,p′-DDE. As reported previously (32), maternal DDT and DDE concentrations were higher in women who were Latina, Mexican-born, less educated, and more recent immigrants to the United States.
In the full sample, maternal serum DDT and DDE concentrations were not associated with BMI z score, waist circumference z score, or percentage of body fat at 9 years of age (Table 3). However, we observed statistically significant interactions by sex for several models. Ten-fold increases in o,p′-DDT and p,p′-DDT concentrations were significantly positively associated with BMI z score in boys (for o,p′-DDT, adjusted β = 0.34, 95% confidence interval (CI): 0.08, 0.60; for p,p′-DDT, adjusted β = 0.23, 95% CI: 0.03, 0.43) but not in girls (for o,p′-DDT, adjusted β = −0.13, 95% CI: −0.42, 0.16; for p,p′-DDT, adjusted β = −0.12, 95% CI: −0.38, 0.15) (P for interaction = 0.02 and 0.03, respectively). A similar pattern was observed with p,p-DDE, but the association in boys did not reach significance (P for interaction = 0.15).
Table 3.
Adjusteda Linear Regression Models of the Associations of Prenatal DDT and DDE Exposure Outcomes at 9 Years of Age, Overall and by Child Sex, Center for the Health Assessment of Mothers and Children of Salinas Study, 2000–2010
| Exposure by Outcome | No.b | Adjusted βc | 95% CI | Child Sex |
P for Interaction | |||
|---|---|---|---|---|---|---|---|---|
| Male |
Female |
|||||||
| Adjusted βc | 95% CI | Adjusted βc | 95% CI | |||||
| BMId z score | ||||||||
| o,p′-DDT | 260 | 0.07 | −0.15, 0.30 | 0.34 | 0.08, 0.60 | −0.13 | −0.42, 0.16 | 0.02 |
| p,p′-DDT | 261 | 0.05 | −0.14, 0.24 | 0.23 | 0.03, 0.43 | −0.12 | −0.38, 0.15 | 0.03 |
| p,p′-DDE | 261 | 0.05 | −0.18, 0.29 | 0.19 | −0.06, 0.45 | −0.13 | −0.50, 0.24 | 0.15 |
| Waist circumference z score |
||||||||
| o,p′-DDT | 260 | 0.07 | −0.12, 0.25 | 0.30 | 0.08, 0.52 | −0.08 | −0.35, 0.19 | 0.03 |
| p,p′-DDT | 261 | 0.07 | −0.09, 0.22 | 0.23 | 0.07, 0.39 | −0.07 | −0.31, 0.17 | 0.04 |
| p,p′-DDE | 261 | 0.07 | −0.12, 0.25 | 0.20 | −0.01, 0.41 | −0.09 | −0.41, 0.23 | 0.13 |
| Body fat, % | ||||||||
| o,p′-DDT | 223 | −0.22 | −2.21, 1.76 | 1.36 | −1.20, 3.91 | −1.60 | −4.21, 1.01 | 0.10 |
| p,p′-DDT | 224 | −0.27 | −1.90, 1.36 | 1.04 | −0.98, 3.06 | −1.58 | −3.89, 0.72 | 0.08 |
| p,p′-DDE | 224 | −0.30 | −2.49, 1.89 | 0.44 | −2.19, 3.06 | −1.19 | −4.82, 2.45 | 0.47 |
Abbreviations: BMI, body mass index; CI, confidence interval; DDE, dichlorodiphenyldichloroethylene; DDT, dichlorodiphenyltrichloroethane.
a Adjusted for maternal prepregnancy BMI and time in the United States at birth.
b There were 118 boys and 143 girls for whom we had BMI z score and waist circumference data and 106 boys and 118 girls for whom we had body fat data.
c β is for a 10-fold increase in exposure.
d Weight (kg)/height (m)2.
DDT was also significantly positively associated with waist circumference z scores in boys (for o,p′-DDT, adjusted β = 0.30, 95% CI: 0.08, 0.52; for p,p′-DDT, adjusted β = 0.23, 95% CI: 0.07, 0.39), but in girls, the β coefficients were nonsignificant (P for interaction = 0.03 and 0.04, respectively). The estimate for p,p′-DDE did not reach significance in boys, but there was still evidence of effect modification by sex (P for interaction = 0.13).
For percentage of body fat, there was some evidence of effect modification by sex for o,p′-DDT and p,p′-DDT (P for interaction = 0.10 and 0.08, respectively), with nonsignificant positive associations in boys but not girls (Table 3). Similarly, maternal serum DDT and DDE concentrations were not associated with overweight/obese status or increased waist circumference in the full sample, but we observed statistically significant interaction by sex (Table 4). The association with overweight/obese status was significant for DDT in boys (for o,p′-DDT, adjusted OR = 2.51, 95% CI: 1.00, 6.28; for p,p′-DDT, adjusted OR = 2.11, 95% CI: 1.00, 4.46) but not girls (P for interaction = 0.02 and 0.03, respectively). The estimate for p,p′-DDE did not reach significance in boys, but there was still evidence of effect modification by sex (P for interaction = 0.04). When we examined the association of maternal serum DDT and DDE concentrations with the 3-category weight outcome (obese, overweight, normal weight), the results were similar to the dichotomous outcomes (data not shown). In boys, DDT was also associated with odds of increased waist circumference (for o,p′-DDT, adjusted OR = 1.98, 95% CI: 0.95, 4.11; for p,p′-DDT, adjusted OR = 2.05, 95% CI: 1.10, 3.82), but this was not the case in girls (P for interaction = 0.07 and 0.04, respectively).
Table 4.
Results of Adjusteda Logistic Regression Models for Associations of Prenatal DDT and DDE Exposure With Overweight/Obese Status and Increased Waist Circumference at 9 Years of Age, Overall and by Child Sex, Center for the Health Assessment of Mothers and Children of Salinas Study, 2000–2010
| Outcome | Casesb | Total | Adjusted ORc | 95% CI | Child Sex |
P for Interaction | |||
|---|---|---|---|---|---|---|---|---|---|
| Male |
Female |
||||||||
| Adjusted ORc | 95% CI | Adjusted ORc | 95% CI | ||||||
| Overweight/ obesity |
|||||||||
| o,p′-DDT | 145 | 260 | 1.20 | 0.75, 1.92 | 2.51 | 1.00, 6.28 | 0.76 | 0.46, 1.25 | 0.02 |
| p,p′-DDT | 146 | 261 | 1.20 | 0.79, 1.81 | 2.11 | 1.00, 4.46 | 0.80 | 0.50, 1.27 | 0.03 |
| p,p′-DDE | 146 | 261 | 1.19 | 0.72, 1.99 | 1.97 | 0.94, 4.13 | 0.69 | 0.35, 1.37 | 0.04 |
| Increased waist circumference |
|||||||||
| o,p′-DDT | 121 | 260 | 1.20 | 0.77, 1.86 | 1.98 | 0.95, 4.11 | 0.88 | 0.53, 1.44 | 0.07 |
| p,p′-DDT | 122 | 261 | 1.31 | 0.88, 1.93 | 2.05 | 1.10, 3.82 | 0.92 | 0.58, 1.47 | 0.04 |
| p,p′-DDE | 122 | 261 | 1.31 | 0.79, 2.16 | 1.98 | 0.97, 4.04 | 0.83 | 0.43, 1.62 | 0.08 |
Abbreviations: CI, confidence interval; DDE, dichlorodiphenyldichloroethylene; DDT, dichlorodiphenyltrichloroethane; OR, odds ratio.
a All models were adjusted for maternal prepregnancy body mass index (weight (kg)/height (m)2) and time in the United States at birth.
b There were 70 male and 76 female overweight/obese cases and 48 male and 73 female cases with increased waist circumference.
c OR is for a 10-fold increase in exposure.
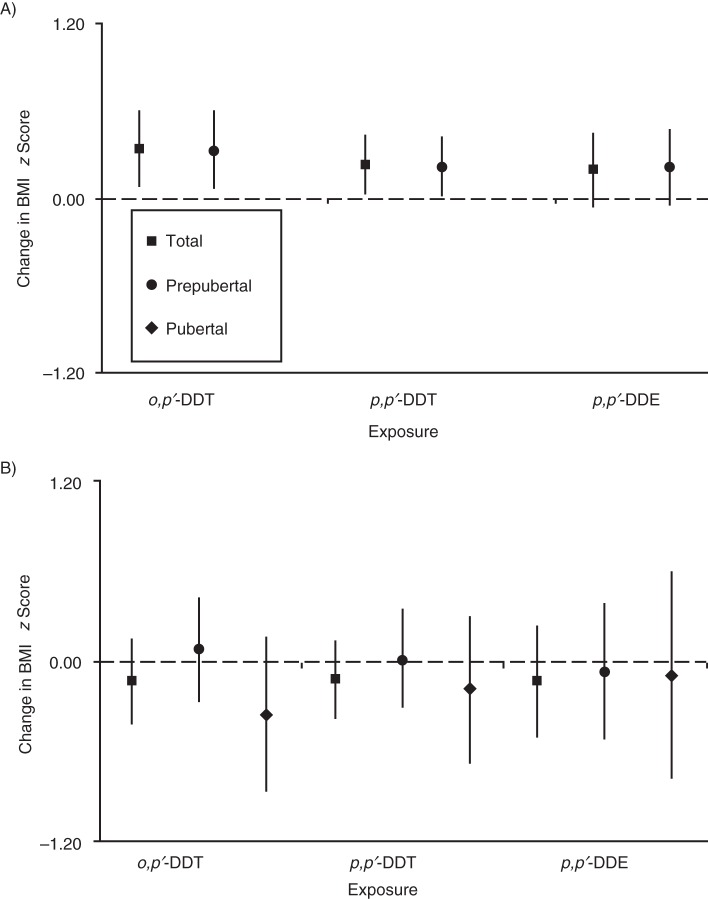
Figure 1A and 1B show the puberty-stratified relationship between DDT and DDE exposure and BMI z score in boys and girls, respectively (see Web Tables 1 and 2, available at http://aje.oxfordjournals.org/, for adjusted β coefficients and 95% confidence intervals). In boys, the associations persisted among boys who had not yet entered puberty; the number of boys who had entered puberty (n = 13) was too small to give meaningful results (data not shown). In girls, regardless of pubertal status, DDT and DDE concentrations were not associated with any measure of obesity.
Figure 1.
Associations of prenatal dichlorodiphenyltrichloroethane (DDT) and dichlorodiphenyldichloroethylene (DDE) exposure with body mass index (BMI) z score at 9 years of age stratified by pubertal status in A) boys and B) girls, Center for the Health Assessment of Mothers and Children of Salinas Study, 2000–2010. All models were adjusted for maternal prepregnancy BMI and maternal time in the United States at birth. Results are shown for a 10-fold increase in exposure. Bars, 95% confidence intervals.
In sensitivity analyses, when we repeated the final models excluding preterm children and/or those with a low birth weight, excluding 1 outlier, or adjusting for potential bias due to loss to follow-up, the results did not change materially (data not shown). The children included in the analysis did not differ significantly from those who were excluded because of missing maternal serum DDT and DDE levels or 9-year anthropometric data (data not shown).
DISCUSSION
This longitudinal birth cohort study of predominantly Mexican-American children residing in a California agricultural community provides evidence that in utero exposure to DDT and DDE may alter the risk for later obesity among boys. Specifically, we found that higher prenatal DDT concentrations were significantly associated with increased BMI z scores, odds of being overweight, waist circumference z scores, and odds of increased waist circumference at 9 years of age, but only in boys. Higher prenatal DDE concentrations were also nonsignificantly associated with increased odds of being overweight, waist circumference z scores, and odds of increased waist circumference in boys. Associations with body fat percentage were less clear. In contrast, prenatal DDT and DDE concentrations were not associated with any measure of obesity in girls. These findings persisted after considering pubertal status.
Our findings of associations in boys only are consistent with most (18, 19, 21), but not all (20), studies that have assessed effect modification by sex. Valvi et al. (18) reported a nonmonotonic increase in the risk of being overweight at 6.5 years of age and cord blood DDT concentration that was limited to boys. The association was statistically significant for the second (269–576 ng/g lipid) but not third tertile of exposure. Mendez et al. (19) reported that maternal DDE levels (mean 125 ng/g lipid) were more strongly associated with rapid growth at 14 months of age in boys, although the sex differences were not statistically significant. In a more highly exposed population, Cupul-Uicab et al. (21) reported that the association of maternal p,p′-DDT concentration (median, 1,170 ng/g lipid) with BMI at age 7 years was stronger in boys than in girls (P for interaction = 0.20). In contrast, Garced et al. (20) reported no evidence of sex interaction at 12 months of age; however, exposure levels were lower in their study.
The International Diabetes Federation does not recommend diagnosing metabolic syndrome in children younger than 10 years of age, but those who are 6–10 years of age and in the 90th percentile or higher of waist circumference for their age and sex are considered at risk for metabolic syndrome (29). In the CHAMACOS Study, we found positive associations between prenatal DDT and DDE concentrations and increased waist circumference in boys at 9 years of age. This suggests that exposure to DDT and DDE may be associated with future risk of metabolic syndrome. To our knowledge, no other epidemiologic studies have investigated the relation of prenatal DDT and DDE exposure with increased waist circumference, metabolic syndrome, or its individual components. However, recent cross-sectional studies in adults suggested a positive association of DDE with metabolic syndrome (33, 34). We plan to examine this association in future follow-up studies of the CHAMACOS cohort.
Although both DDT congeners are estrogenic, o,p′-DDT has stronger estrogenic activity (11). Only 2 other studies have examined prenatal o,p′-DDT and p,p′-DDT separately (35, 36). Prenatal levels of o,p′-DDT, p,p′-DDT, and p,p′-DDE were not associated with child weight or height z scores at age 5 years, and there was no evidence of heterogeneity by sex in the Child Health and Development Studies (36). There was also no association with BMI at 10–20 years of age in boys from the Collaborative Perinatal Project (35). However, levels in those studies were considerably higher than in the present study, and a standardized measure of BMI was not used. In the CHAMACOS cohort, we observed similar associations between o,p-DDT and p,p′-DDT concentrations and child obesity status at 9 years of age, but estimates for o,p′-DDT were stronger in most cases. Given the high correlation in the present study between DDT and DDE (r = 0.9), it is difficult to separate out the individual associations of each compound with confidence.
Both DDT and DDE have been associated with adipose dysfunction in experimental studies (12, 13), and given that DDT, an estrogen agonist, is metabolized into DDE, an androgen antagonist, multiple mechanisms may be involved. The sex-specific associations observed seem plausible given that both estrogenic and antiandrogenic activity play a key role in adipogenesis during development (2, 37). Early developmental exposure to DDT and DDE could impact weight by affecting normal weight homeostasis either directly by acting on adipose cells through differentiation and proliferation or indirectly via disruption of the endocrine feedback loop (2, 37).
It is unlikely that our finding of sex-specific associations between prenatal DDT and DDE concentrations and obesity outcomes is due to differences in pubertal timing. Among girls, prenatal DDT and DDE concentrations were not associated with any measure of obesity, regardless of pubertal status; among boys, DDT and DDE were associated with measures of obesity even when restricting the sample to those who were prepubescent. However, given the small number of boys who had entered puberty, it will be important to follow the CHAMACOS cohort through puberty to continue to examine the longitudinal trends in obesity with regard to in-utero exposure to DDT and DDE while considering the impact of exposure on the adrenal hormone–mediated increase in weight and the sex steroid–induced pubertal growth spurt.
The present study has several strengths. The CHAMACOS study is a longitudinal birth cohort study with a long follow-up period for which considerable information was collected about potential confounders. The study population is relatively homogenous with regard to factors such as diet, breastfeeding, country of origin, and socioeconomic status, which can reduce uncontrolled confounding. We were able to measure exposure to o,p′-DDT, p,p′-DDT, and p,p′-DDE in maternal serum collected during pregnancy. Exposure levels were high relative to other Mexican Americans, likely because of the mothers’ recent immigration from Mexico (38), but there was a wide range of exposure. We were able to measure percentage of body fat using bioelectrical impedance, which is a more direct measure of adiposity, and used a standardized measure of overweight based on BMI z score, which facilitates comparison across studies. In addition, we have measures of pubertal onset using state-of-the-art Tanner staging.
The present study has some limitations. There were 417 mothers who had maternal serum DDT and DDE measurements during pregnancy, but we had complete anthropometric data at age 9 years for only 261 children. However, the prenatal DDT and DDE exposure levels of those with and without 9-year anthropometric data were not significantly different. In addition, predictors of maternal levels of o,p′-DDT, p,p′-DDT, and p,p′-DDE were similar to those reported previously in the larger group (32), and adjustment for loss to follow-up using inverse probability weighting did not change the results substantially. Finally, unlike the other outcome measures, data on percentage of body fat were not standardized for age or sex, which may have limited our ability to observe significant associations.
In summary, we examined the associations of in utero exposure to o,p′-DDT, p,p′-DDT, and p,p′-DDE with several measures of obesity in the CHAMACOS cohort at 9 years of age. We found that higher prenatal DDT and DDE concentrations were significantly positively associated with BMI, waist circumference, and overweight or obese status, but only in boys. In contrast, DDT and DDE were not associated with any measure of obesity in girls, even after considering pubertal status. Our results support the hypothesis that in-utero exposure to endocrine-disrupting compounds may increase risk of obesity later in life.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Center for Environmental Research and Children's Health, School of Public Health, University of California at Berkeley, Berkeley, California (Marcella Warner, Amelia Wesselink, Kim G. Harley, Asa Bradman, Katherine Kogut, Brenda Eskenazi).
This work was supported by grants from the National Institute of Environmental Health Sciences at the National Institutes of Health (grants PO1 ES009605 and R01 ES017054), the National Institute for Occupational Safety and Health (grant RO1 OH007400), and the US Environmental Protection Agency (grants R82670901 and RD83451301).
Conflict of interest: none declared.
REFERENCES
- 1.Baillie-Hamilton PF. Chemical toxins: a hypothesis to explain the global obesity epidemic. J Altern Complement Med. 2002;8(2):185–192. doi: 10.1089/107555302317371479. [DOI] [PubMed] [Google Scholar]
- 2.Diamanti-Kandarakis E, Bourguignon JP, Giudice LC, et al. Endocrine-disrupting chemicals: an Endocrine Society scientific statement. Endocrine Rev. 2009;30(4):293–342. doi: 10.1210/er.2009-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heindel JJ. Endocrine disruptors and the obesity epidemic. Toxicol Sci. 2003;76(2):247–249. doi: 10.1093/toxsci/kfg255. [DOI] [PubMed] [Google Scholar]
- 4.Heindel JJ, vom Saal FS. Role of nutrition and environmental endocrine disrupting chemicals during the perinatal period on the aetiology of obesity. Mol Cell Endocrinol. 2009;304(1-2):90–96. doi: 10.1016/j.mce.2009.02.025. [DOI] [PubMed] [Google Scholar]
- 5.Grün F, Blumberg B. Environmental obesogens: organotins and endocrine disruption via nuclear receptor signaling. Endocrinology. 2006;147(6 suppl):S50–S55. doi: 10.1210/en.2005-1129. [DOI] [PubMed] [Google Scholar]
- 6.Newbold RR, Padilla-Banks E, Snyder RJ, et al. Developmental exposure to endocrine disruptors and the obesity epidemic. Reprod Toxicol. 2007;23(3):290–296. doi: 10.1016/j.reprotox.2006.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Newbold RR, Padilla-Banks E, Jefferson WN. Environmental estrogens and obesity. Mol Cell Endocrinol. 2009;304(1-2):84–89. doi: 10.1016/j.mce.2009.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Casals-Casas C, Desvergne B. Endocrine disruptors: from endocrine to metabolic disruption. Annu Rev Physiol. 2011;73:135–162. doi: 10.1146/annurev-physiol-012110-142200. [DOI] [PubMed] [Google Scholar]
- 9.Swedenborg E, Ruegg J, Makela S, et al. Endocrine disruptive chemicals: mechanisms of action and involvement in metabolic disorders. J Mol Endocrinol. 2009;43(1):1–10. doi: 10.1677/JME-08-0132. [DOI] [PubMed] [Google Scholar]
- 10.Grün F, Blumberg B. Endocrine disrupters as obesogens. Mol Cell Endocrinol. 2009;304(1-2):19–29. doi: 10.1016/j.mce.2009.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agency for Toxic Substances and Disease Registry. Toxicological Profile for DDT, DDE and DDD. Atlanta, GA: US Department of Health and Human Services, Public Health Service; 2002. [PubMed] [Google Scholar]
- 12.Moreno-Aliaga MJ, Matsumura F. Effects of 1,1,1-trichloro-2,2-bis(p-chlorophenyl)-ethane (p,p′-DDT) on 3T3-L1 and 3T3-F442A adipocyte differentiation. Biochem Pharmacol. 2002;63(5):997–1007. doi: 10.1016/s0006-2952(01)00933-9. [DOI] [PubMed] [Google Scholar]
- 13.Howell G, 3rd, Mangum L. Exposure to bioaccumulative organochlorine compounds alters adipogenesis, fatty acid uptake, and adipokine production in NIH3T3-L1 cells. Toxicol In Vitro. 2011;25(1):394–402. doi: 10.1016/j.tiv.2010.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ruzzin J, Petersen R, Meugnier E, et al. Persistent organic pollutant exposure leads to insulin resistance syndrome. Environ Health Perspect. 2010;118(4):465–471. doi: 10.1289/ehp.0901321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ibrahim MM, Fjære E, Lock EJ, et al. Chronic consumption of farmed salmon containing persistent organic pollutants causes insulin resistance and obesity in mice. PLoS One. 2011;6(9):e25170. doi: 10.1371/journal.pone.0025170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cupul-Uicab LA, Hernández-Avila M, Terrazas-Medina EA, et al. Prenatal exposure to the major DDT metabolite 1,1-dichloro-2,2-bis(p-chlorophenyl)ethylene (DDE) and growth in boys from Mexico. Environ Res. 2010;110(6):595–603. doi: 10.1016/j.envres.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Verhulst SL, Nelen V, Hond ED, et al. Intrauterine exposure to environmental pollutants and body mass index during the first 3 years of life. Environ Health Perspect. 2009;117(1):122–126. doi: 10.1289/ehp.0800003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Valvi D, Mendez MA, Martinez D, et al. Prenatal concentrations of polychlorinated biphenyls, DDE, and DDT and overweight in children: a prospective birth cohort study. Environ Health Perspect. 2012;120(3):451–457. doi: 10.1289/ehp.1103862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mendez MA, Garcia-Esteban R, Guxens M, et al. Prenatal organochlorine compound exposure, rapid weight gain, and overweight in infancy. Environ Health Perspect. 2011;119(2):272–278. doi: 10.1289/ehp.1002169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garced S, Torres-Sánchez L, Cebrián ME, et al. Prenatal dichlorodiphenyldichloroethylene (DDE) exposure and child growth during the first year of life. Environ Res. 2012;113:58–62. doi: 10.1016/j.envres.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cupul-Uicab LA, Klebanoff MA, Brock JW, et al. Prenatal exposure to persistent organochlorines and childhood obesity in the US Collaborative Perinatal Project. Environ Health Perspect. 2013;121(9):1103–1109. doi: 10.1289/ehp.1205901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Warner M, Aguilar Schall R, Harley KG, et al. In utero DDT and DDE exposure and obesity status of 7-year-old Mexican-American children in the CHAMACOS cohort. Environ Health Perspect. 2013;121(5):631–636. doi: 10.1289/ehp.1205656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eskenazi B, Bradman A, Gladstone EA, et al. CHAMACOS, A longitudinal birth cohort study: lessons from the fields. J Child Health. 2003;1(1):3–27. [Google Scholar]
- 24.Barr JR, Maggio VL, Barr DB, et al. New high-resolution mass spectrometric approach for the measurement of polychlorinated biphenyls and organochlorine pesticides in human serum. J Chromatogr B Analyt Technol Biomed Life Sci. 2003;794(1):137–148. doi: 10.1016/s1570-0232(03)00451-3. [DOI] [PubMed] [Google Scholar]
- 25.Hornung RW, Reed LD. Estimation of average concentration in the presence of nondetectable values. Appl Occup Environ Hyg. 1990;5(1):48–51. [Google Scholar]
- 26.Phillips DL, Pirkle JL, Burse VW, et al. Chlorinated hydrocarbon levels in human serum: effects of fasting and feeding. Arch Environ Contam Toxicol. 1989;18(4):495–500. doi: 10.1007/BF01055015. [DOI] [PubMed] [Google Scholar]
- 27.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002;(246):1–190. [PubMed] [Google Scholar]
- 28.Cook S, Auinger P, Huang TT. Growth curves for cardio-metabolic risk factors in children and adolescents. J Pediatr. 2009;155(3):S6.e15–S6.e26. doi: 10.1016/j.jpeds.2009.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zimmet P, Alberti G, Kaufman F, et al. The metabolic syndrome in children and adolescents. Lancet. 2007;369(9579):2059–2061. doi: 10.1016/S0140-6736(07)60958-1. [DOI] [PubMed] [Google Scholar]
- 30.Stata Corporation. Stata statistical software, release 11. College Station, TX: Stata Corporation; 2009. [Google Scholar]
- 31.Hernán MA, Hernández-Díaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004;15(5):615–625. doi: 10.1097/01.ede.0000135174.63482.43. [DOI] [PubMed] [Google Scholar]
- 32.Bradman AS, Schwartz JM, Fenster L, et al. Factors predicting organochlorine pesticide levels in pregnant Latina women living in a United States agricultural area. J Expo Sci Environ Epidemiol. 2007;17(4):388–399. doi: 10.1038/sj.jes.7500525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee DH, Steffes MW, Sjödin A, et al. Low dose organochlorine pesticides and polychlorinated biphenyls predict obesity, dyslipidemia, and insulin resistance among people free of diabetes. PLoS One. 2011;6(1):e15977. doi: 10.1371/journal.pone.0015977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee DH, Lee IK, Porta M, et al. Relationship between serum concentrations of persistent organic pollutants and the prevalence of metabolic syndrome among non-diabetic adults: results from the National Health and Nutrition Examination Survey 1999–2002. Diabetologia. 2007;50(9):1841–1851. doi: 10.1007/s00125-007-0755-4. [DOI] [PubMed] [Google Scholar]
- 35.Jusko TA, Koepsell TD, Baker RJ, et al. Maternal DDT exposures in relation to fetal and 5-year growth. Epidemiology. 2006;17(6):692–700. doi: 10.1097/01.ede.0000232226.06807.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gladen BC, Klebanoff MA, Hediger ML, et al. Prenatal DDT exposure in relation to anthropometric and pubertal measures in adolescent males. Environ Health Perspect. 2004;112(17):1761–1767. doi: 10.1289/ehp.7287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cooke PS, Naaz A. Role of estrogens in adipocyte development and function. Exp Biol Med (Maywood) 2004;229(11):1127–1135. doi: 10.1177/153537020422901107. [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. Atlanta, GA: National Center for Health Statistics; 2004. 2001–2002 National Health and Nutrition Examination Survey (NHANES) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.