Abstract
Objectives
We examine the dynamics of patient sharing relations within an Italian regional community of 35 hospitals serving approximately 1,300,000 people. We test whether interorganizational relations provide individual patients access to higher quality providers of care.
Methods
We reconstruct the complete temporal sequence of the 3461 consecutive interhospital patient sharing events observed between each pair of hospitals in the community during 2005-2008. We distinguish between transfers occurring between and within different medical specialties. We estimate newly derived models for relational event sequences that allow us to control for the most common forms of network-like dependencies that are known to characterize collaborative relations between hospitals. We use 45 day risk-adjusted readmission rate as a proxy for hospital quality.
Results
After controls (e.g., geographical distance, size, and the existence of prior collaborative relations), we find that patients flow from less to more capable hospitals. We show that this result holds for patient being shared both between as well as within medical specialties. Nonetheless there are strong and persistent other organizational and relational effects driving transfers.
Conclusions
Decentralized patient sharing decisions taken by the 35 hospitals give rise to a system of collaborative interorganizational arrangements that allow patient to access hospitals delivering a higher quality of care. This result is relevant for health care policy because it suggests that collaborative relations between hospitals may produce desirable outcomes both for individual patients, as well as for regional health-care systems.
The rise of Accountable Care Organizations, strategic alliances and collaborative statewide quality agreements has given growing prominence to the role of decentralized coordination between hospitals in the care of patients in the United States.i Yet, such systems have been in place in other advanced medical systems—and other sectors of the economy—for many years. In this article, we approach interhospital transfers of patients as patient sharing relations that constitute an interorganizational network amenable to direct empirical investigationii,iii. Patient sharing requires that partner hospitals commit resources to joint infrastructural investments to support relational coordinationiv,v-- a reliable signal of collaboration between sending and receiving hospitalsvi.
Even as patient-sharing practices diffuse and grow in importance, it remains unclear what drives these colloborations. Do they result in individual patients going to higher quality hospitals? To what extent are do they meeti other organizational, rather than patient-centered goals? Extant research on this issue has produced contrasting results. A recent review of the literature on the transfer of critically ill patients, for example, concludes that the destination of patients is not necessarily chosen on the basis of objective evidence about the performance and capabilities of the receiving hospital5. Yet, it has also been argued that encouraging interhospital patient sharing relations so that appropriate patients could be transferred from lower to higher quality hospitals would be an effective policy for facilitating access to higher quality care2. For example, in the context of critical care medicine studies are available that report how directing trauma victims to centers of excellence may lead to a 25 to 50% improvement in outcomesvii. The conclusion seems to be that interhospital collaboration via patient sharing relations could – at least in principle - facilitate access to higher quality care. In practice, however, this appears not to happen in the U.S. if the decision is left to individual hospitalsviii. As a consequence corrective policy interventions may be needed to realize the full potential of interhospital collaboration. Regionalization, centralization and quality improvement initiatives have been recently proposed as policy instruments to correct potentially undesirable consequences of decentralized interhospital arrangementsix.
The purpose of this paper is, substantively, to widen the discussion by moving outside the U.S. context, with its known insurance-based idiosyncrasies. We collected data on all interhospital transfers during 2005-2008 between all 35 hospitals in a self-contained region in Southern Italy. Modeled after the British NHS, the Italian National Health System (NHS) provides healthcare coverage and uniform access to health care services financed by the government through taxesx. Policies of economic decentralization consistently enacted since the early 1990s have progressively shifted administrative, financial, and managerial control from the central to the regional governments. Today health care in Italy takes the form of a fully federal system with the regions as the relevant organizational units of analysis. Despite considerable regional variation in economic, demographic and social conditions, focusing our analysis on all the hospitals present in a region allows us to examine a representative sub-component of the Italian health care system.
Beyond this substantive motivation, this paper also brings to bear new dynamic statistical models to analyze the temporal sequence of discrete acts of “network-construction” - such as patient transfer events over time - rather than simply presuming the presence of immutable (or slowly changing) network ties between hospitals. Sequences of dyadic patient sharing events link hospitals in the community and give rise to an evolving dynamic network of interorganizational relations which we interpret as the observable traces of collaboration between hospitals. The explicit objectives of the study are to:
Examine how measurable differences in hospital quality affect the direction of interhospital patient flows, net of other organizational relationships. In particular we ask, Q1: do patient sharing-relations allow patients to access better hospitals and hence – presumably – higher quality care?
Understand the micro-mechanisms that facilitate collaborative patient sharing relations between hospitals. In particular we ask, Q2: what organizational and institutional factors affect the propensity of hospitals to collaborate?
Explore how dynamic patterns of interhospital patient sharing relations change for different types of patient sharing events. In particular we ask, Q3: how do different interorganizational collaboration routines affect the structure of patient sharing relations linking the hospitals?
Research Design and Methods
Setting
We used patient-level information on hospital-sharing events from 2005 to 2008 for all 35 hospitals in Abruzzo (Italy) - a region of 1,300,000 inhabitantsxi. Approximately 10% of the population lives in Pescara -the largest urban center in the region. The regional health system is partitioned into six (non-overlapping) Local Health Units (LHUs) designed to ensure availability of and access to homogenous service throughout the region by allocating resources and coordinating the activities of the hospitals. Health care services are provided by 35 hospital organizations of which, 22 are public and 13 are accredited private hospitals. Two of the 22 public providers are teaching hospitals linked to universities. Public hospitals provide specialized tertiary care, and are characterized by managerial autonomy. Private hospitals are investor-owned organizations providing ambulatory, hospital care, and/or diagnostic services that are partially financed by the regional health care service. Hospitals enjoy considerable managerial discretion and management retains full responsibility over the budgeting process and economic outcomes. Patients are free to choose providers operating within the public system of universal coverage which also includes accredited private hospitals. Reimbursements and fees for services provided to hospitalized patients are determined according to a general Diagnosis-Related Group (DRG) system. Patients are asked to contribute to the coverage of part of the cost of service.
Data Collection
Data were provided by the Agency of Public Health, an agency whose institutional mandate is to collect and manage patient discharge data (Schede di demissione ospedaliera, or SDO) for the purpose of assessing regional hospitals' activities and performance. Discharge information is organized into three main databases. The first includes demographics, such as place and date of birth, gender, place of residence and LHU to which patients belong for administrative purposes. The second contains hospitalization-specific data, including the principal diagnosis and intervention (ICD9), the number and type of co-morbidities, the major diagnostic category, and other relevant information such as the date of admission and discharge, the type of admission (e.g., where the patient comes from) and the type of discharge (whether patients are transferred to another hospital or discharged to their residence). Information about the hospital admitting a transferred patient is contained in the third section of the discharge data file.
Data were provided for each and every hospital admission and discharge ever recorded in the region during the period 2005-2008. A patient transferred from a sender hospital to a different receiver hospital within 24 hours from admission in the sender hospital is one observation in the sequence of relational events that we analyze in the empirical part of the study. Patient information was made anonymous through an identification code that the regional agency assigns to admitted patients. The unique identification codes, together with information about the date and nature of discharges/admissions, were used to identify collaborative patient sharing events between hospitals. Specifically, administrative discharge data were matched so that a patient transfer event between two hospitals is recorded when a given patient is discharged and, in the same calendar day, admitted into another hospital3. Information on hospital-specific covariates (staffed beds, occupancy rate, readmission rates etc.) was also provided by the Agency of Public Health.
Statistical approach
The statistical models we estimate are described in detail in the Supplemental Digital Content (SDC). Here we provide a conceptual overview. In brief, we model the dynamics of sequences of relational events connecting a sender and receiver hospital. At each (daily) time point, we estimate the probability that a patient is transferred between every pair of hospitals. We estimate this as a function of characteristics of the particular hospitals, the differences in the measured variables of those hospitals, and of time. Further, the model takes into account the history of past transfers from the sending to the receiving hospital. This is done using a multiplicative Cox function for empirical relational event sequences described in detail in the SDC and used in the existing literature on relational event modelsxii. The resulting hazard ratios can be interpreted as with conventional hazard ratio from survival analysis or converted to predicted probabilities. One feature of this class of models which makes them uniquely useful for our current purposes is their ability to represent directly a variety of local dependencies in temporal sequences of relational events. This allows us to go beyond simple patient-level data and estimate the effect of hospital quality on patient transfer while controlling for a variety of systematic network-like dependencies that are known to characterize data on interorganizational relations iii,vi. More specifically, we examine the extent to which patient sharing relations are affected by the network-like effects summarized in Table 1.
Table 1. Behavioral principles underlying the formation of patient sharing relations and their relation with predicted event sequences.
| Behavioral Principle | Network effect s(i, j, t) | Relational protocols (patient sharing routine) | Predicted event sequence | |
|---|---|---|---|---|
| (t) | (t+Δt) | |||
| Mutuality | Reciprocity | “Share patients preferentially with partners willing to share their patients with you” | i ← j | i → j |
| Specialization | Assortativity | “If I need to send many patients, I send them preferentially to hospitals receiving many patients | j ← k | j ← l |
| Stabilization (Recency) | Repetition | “Share patients preferentially with partners with whom you have shared patients in the past” | i → j | i → j |
| Transitivity | Transitive Closure (“embeddedness”) | “Partners of my partners are my partners” | i → k → j | i → j |
| Generalized exchange | Cyclic closure | “Accept patients from partners of partners even without reciprocity” | i → k → j | i ← k ← j |
| i ← j | i → j | |||
Table 2 summarizes the control variables that we incorporate in our empirical models to control for differences in organizational elements that may affect the flow of patients between hospitals.
Table 2. Organizational control factors.
| Factor (x) | Unit of measure | Controls for differences in | Predicted effect of difference (Δr,s(x) = xreceiver- xsender)) |
|---|---|---|---|
| Size | Hospital beds | Organizational size | Positive: Larger hospitals tend to attract more patients from smaller hospitals. |
| Revenue per discharged patient | Monetary units (Euros) | Cost absorption computed on the basis of the reimbursement claims made on the basis of the DRG system | Positive: Patients tend to flow toward hospitals offering more sophisticated and hence expensive services; |
| Complexity | Case Mix Index | Capabilities and experience in dealing with complex clinical cases | Positive: Patients tend to flow toward hospitals capable of treating more complex cases |
| Occupancy rate | Dimensionless proportion of beds occupied | Hospital capacity management | Positive: Patients tend to flow toward hospitals that are better able to manage the allocation of their capacity. |
| Level of care | Dimensionless binary indicator variable | Level of care that partner hospitals offer (rehabilitation, secondary, tertiary) | Negative. Patients flows are less likely to be observed between hospitals offering the same levels of care |
| Geographical distance | Kilometers | Distance | Negative. The intensity of patient flows between two hospitals decrease as the distance between them increases. |
| Local Health Unit (LHU) | Dimensionless categorical variable | Membership in the same Local Health Unit | Positive. Hospitals belonging to the same administrative units will find it easier to coordinate patient sharing activities. As a consequence patients flow will be more intense between hospitals in the same LHU. |
| Institutional category | Dimensionless categorical variable | Membership in the same broadly defined institutional category (public vs. private) | Negative. Patients sharing activities are more likely to be observed across the private/public divide. |
Our primary measure of hospital quality is the publicly reported risk-adjusted readmission rate within 45 days; this measure counts as readmissions those for the same primary diagnosis, not all hospitalizations. The risk-adjusted readmission rate takes into account specific patient characteristics that may increase the risk of readmission, such as – for example - patient's age (above 65) and a variety of comorbidities, such as diabetes mellitus, acute coronary syndrome, cancer, and asthma. While readmission rate is an imperfect single measure of quality, xiii,xiv readmission rate is one of the main metrics adopted by regional health supervisory authorities to evaluate hospital quality and allocate resources to hospitals—and as such, is recognized as a quality indicator by the relevant decision-makers in this system. Readmissions impair patients' conditions and frequently imply avoidable costsxv. The 45 day (instead of the more conventional 30 day) cutoff is established end enforced by the regional health authorities with exclusive jurisdiction over the health care services rendered within the community. The publicly reported data at our disposal do not allow us to examine the effects of different definitions of readmission rates.
Throughout our analyses, we estimate separate models for transfers where the patient had the same MDC (Major Diagnostic Category) diagnosis at both the sending and receiving hospitals (calling those “within” a specialty) and cases where the diagnoses at the two hospitals were distinct (calling those patient sharing events “between” specialties). Transfers were categorized as “within” or “between” specialties based on an official classification system of the medical specialties adopted nationally - a system based on the internationally accepted MDC classification. The purpose of disaggregating the overall sequence of relational patient sharing events into “between” and “within” events is to identify and examine two potentially different sets of interhospital relations. The first set (patient sharing “between”) may be driven by a logic of complementarity because one hospital (the sender) may not have the clinical capacity to assist the patient who is being transferred to the partner hospital (the receiver). The second set of relations (patient sharing “within”) may be driven by the recognition that the receiver hospital may be better able to treat the patient. These two logics frequently coexist within public health care systems – and within interorganizational networks more generallyxvi. It is important, therefore, to assess the role that differences in quality between receiver and sender hospitals might play in shaping the interhospital collaboration under these two very different conditions.
Results
We carry out our empirical investigation at two different levels of analysis. The first is aggregate and includes the complete series of patient sharing events recorded during the observation period between the 35 hospitals in the region. The total number of patient sharing events observed was 3461. The daily average was 2.37 (standard deviation = 1.81, range 0-10). The total risk set includes all the 1,490,071 possible edges in the network (event edges + non-event or “control” edges).
The second level involves disaggregation by type of patient sharing event. More specifically, the second level distinguishes between patient sharing events observed “between” and within the various medical specialties, or “discipline” organized by the hospitals in the region. The observed number of “within” events was 603 (daily average = 0.825, standard deviation = 0.661, range 0-5). The observed number of “between” events was 2858 (daily average = 1.956, standard deviation = 1.615, range 0-9).
Table 3 reports maximum likelihood estimates of Cox regression models for series of patient sharing events. The first column reports the estimates for the aggregate series. The second and third columns report the estimates for the series of relational patient sharing events between and within specialties, respectively.
Table 3.
Maximum likelihood estimates of proportional hazard models for relational patient sharing events between 35 hospitals in a regional community. Standard errors in parentheses.
| M1 (all events, N = 3461) |
M2 (Between events only, N = 2858) |
M3 (within events only, N = 603) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Estimate (s.e.) | Pr>Chisq | Hazard ratio | Estimate (s.e.) | Pr>Chisq | Hazard ratio | Estimate (s.e.) | Pr>Chisq | Hazard ratio | |
| Propensity to collaborate (outdegree) | 0.1895 *(0.0140) | <.0001 | 1.209 | 0.1712 *(0.0160) | <.0001 | 1.187 | 0.3293 *(0.0510) | <.0001 | 1.39 |
| Propensity to initiate patient sharing events (weighted outdegree) | 0.4310 *(0.0752) | <.0001 | 1.539 | 0.6080 *(0.0805) | <.0001 | 1.837 | 0.1608(0.2790) | 0.5644 | 1.174 |
| Propensity to be selected as partner (indegree) | 0.1131*(0.0082) | <.0001 | 1.12 | 0.0975 *(0.0083) | <.0001 | 1.102 | 0.1669 *(0.0255) | <.0001 | 1.182 |
| Propensity to receive patient sharing events (weighted indegree) | 0.3010 *(0.1018) | 0.0031 | 1.351 | 0.5983 *(0.1090) | <.0001 | 1.819 | 0.5967(0.3416) | 0.0807 | 1.816 |
| Recent sending | -0.0014 *(0.0002) | <.0001 | 0.999 | -0.0014 *(0.0002) | <.0001 | 0.999 | -0.0011 *(0.0003) | 0.0004 | 0.999 |
| Recent receiving | -0.0031 *(0.0002) | <.0001 | 0.997 | -0.0028 *(0.0002) | <.0001 | 0.997 | -0.0029 *(0.0003) | <.0001 | 0.997 |
| Quality of care (45 day R-Rate) | -0.0996 *(0.009) | <.0001 | 0.905 | -0.0888 *(0.0095) | <.0001 | 0.915 | -0.1094 *(0.0261) | <.0001 | 0.896 |
| Geographical distance (Km) | -0.0255 *(0.0012) | <.0001 | 0.975 | -0.0271 *(0.0014) | <.0001 | 0.973 | -0.0201 *(0.0029) | <.0001 | 0.98 |
| Institutional category | -1.3674 *(0.0856) | <.0001 | 0.255 | -1.2617 *(0.0877) | <.0001 | 0.283 | -2.7813 *(0.4848) | <.0001 | 0.062 |
| LHU membership | 1.4445 *(0.0530) | <.0001 | 4.24 | 1.5260 *(0.0575) | <.0001 | 4.6 | 1.0029 *(0.1098) | <.0001 | 2.726 |
| Level of care provided | 0.2723 *(0.0481) | <.0001 | 1.313 | 0.2405 *(0.0547) | <.0001 | 1.272 | 0.3561(0.1403) | 0.0111 | 1.428 |
| Size (number of staffed beds) | 0.0007 *(0.0002) | <.0001 | 1.001 | 0.00074 *(0.0002) | 0.0001 | 1.001 | 0.00073(0.0005) | 0.1161 | 1.001 |
| Occupancy rate | 0.0177 *(0.0015) | <.0001 | 1.018 | 0.0155 *(0.0016) | <.0001 | 1.016 | 0.0112(0.0053) | 0.0328 | 1.011 |
| Revenue per discharged patient | 0.0002 *(2.6E-05) | <.0001 | 1 | 0.0002 *(2.7E-05) | <.0001 | 1 | 0.0003 *(9.2E-05) | 0.0003 | 1 |
| Complexity (Case mix) | 0.6549 *(0.1433) | <.0001 | 1.925 | 0.5968 *(0.1478) | <.0001 | 1.816 | 1.1879(0.4733) | 0.0121 | 3.28 |
| Reciprocity | 0.0402 *(0.0107) | 0.0002 | 1.041 | 0.0322 *(0.0112) | 0.0039 | 1.033 | 0.2374(0.0997) | 0.0172 | 1.268 |
| Assortativity (by degree) | -0.0045 *(0.0011) | <.0001 | 0.995 | -0.0045 *(0.0013) | 0.0004 | 0.995 | -0.0207 *(0.0056) | 0.0002 | 0.979 |
| Assortativity (by intensity) | -0.0877(0.0722) | 0.2249 | 0.916 | -0.3519 *(0.0907) | 0.0001 | 0.703 | -0.1458(0.4079) | 0.7208 | 0.864 |
| Event Recurrence | 0.1886 *(0.0089) | <.0001 | 1.208 | 0.1912 *(0.0118) | <.0001 | 1.211 | 0.6569 *(0.0604) | <.0001 | 1.929 |
| Transitive closure | 0.0721 *(0.0215) | 0.0008 | 1.075 | 0.1196 *(0.0246) | <.0001 | 1.127 | -0.0054(0.0834) | 0.9481 | 0.995 |
| Cyclic closure | 0.0352 *(0.0126) | 0.0052 | 1.036 | 0.0542 *(0.0146) | 0.0002 | 1.056 | 0.1128 *(0.0486) | 0.0202 | 1.119 |
|
| |||||||||
| Goodness of fit (GoF; Pr>Chi-Sq) | L.Rat. = 18114.2249 (21; <.0001) | L.Rat. = 14936.0144 (21; <.0001) | L.Rat. = 3744.089 (21; <.0001) | ||||||
| Score = 119197.084 (21; <.0001) | Score = 111928.51 (21; <.0001) | Score = 44530.026 (21; <.0001) | |||||||
| (Global null hypothesis B=0) | Wald = 11009.4902 (21; <.0001) | Wald = 9351.5354 (21; <.0001) | Wald = 2299.3437 (21; <.0001) | ||||||
Legend:
= p<0.01
Across all the models we estimated, the effect of Readmission rate within 45 days is negative and significant. According to these estimates our answer to Q1 is that patient sharing relations between hospitals systematically increase the mobility of patients towards more capable hospitals (i.e., hospitals with a lower readmission rate). The estimate of the hazard ratio (or odds) corresponding to our measure of hospital quality in the aggregate model is (0.475/0.525-)= 0.905.
Yet, measured quality differences between hospitals are not the only factor driving the destination of patients. To address question Q2 we estimated models that incorporate a number of institutional and organizational differences between the hospitals in our sample. The probability of observing patients sharing events is significantly reduced by geographical distance between hospitals. The probability of observing a patient sharing event connecting two hospitals in the sample that are maximally far apart (146 km) is approximately 97% lower than the probability of observing patient sharing relations between hospitals that are minimally distant (2 km). Hospitals within the same administrative area (LHU) are significantly more likely to collaborate by sharing patients, even conditional on distance between the hospitals. Hospitals are more likely to collaborate across broadly defined Institutional categories defined in terms of ownership (Public-Private) rather than across such categories. Collaborative relations between hospitals tend to move patients from less sophisticated sender to more sophisticated receiver hospitals (as measured by Revenue per discharged patient), from less complex sender to more complex receiver hospitals (as measured by the Case Mix Index), from hospitals less capable to hospitals more capable of managing their capacity (as measured by the Occupancy rate), and from smaller to larger hospitals (in terms of Number of beds). The role played by the case mix is particularly noteworthy. In the aggregate model, the odds are approximately 2:1 to observe a patient transfer event toward hospitals. The parameter estimate in the aggregate model (0.6549) implies that as the interhospital difference in case mix increases from its minimum (0) to its observed maximum (0.76) the probability of observing a patient transfer event from a less to a more complex hospital increases 84%.
Importantly, the longitudinal models also control for the heterogeneous unobserved propensities of hospitals in the community to collaborate (Propensity to Collaborate – or outdegree: number of partners) and to share patients with partner hospitals (Propensity to initiate patient sharing events- or weighted outdegree: number of patients shared with partners). In the aggregate model the hazard ratio associated with the propensity to collaborate is 1.209 (see M1 in Table 1). This estimate implies that, on average, the conditional probability of observing a patient sharing event originating from a hospital experiencing a unit increase in the number of partner hospitals (the “outdegree”) is approximately 0.55. By a similar reasoning, a unit increase in the number of shared patients between hospitals i and j corresponds to a probability of observing a new patient sharing event between i and j of approximately 0.61. Similar qualitative implications may be associated with the other two general controls the Propensity to be selected as partner (or the “indegree”) and the Propensity to receive patient sharing events. The estimates of these important effects are fairly stable across models. The recency effects (Recent sending, Recent receiving) are significantly negative indicating that activities of sending and receiving patients in the past, respectively, are associated with shorter time between successive events.
Prior studies have argued that the selection of patient sharing partners is affected by routinized procedures and consolidated hospital practices that may be unrelated to quality considerations7. As the figures reported in Table 3 clearly show the effect of interhospital patient transfer routines is significant, answering Q3. In general we find that patient sharing relations are more likely to be observed between reciprocating hospitals (Reciprocity). We also find a significant tendency against assortativity (Assortativity by degree): hospitals sending patients to many others tend not to select as partners hospitals that receive patient from many others. This may be interpreted as a relative lack of interorganizational division of labor between hospitals in the community. Interestingly, there is no evidence of assortativity in numbers (Assortativity by Intensity): hospitals sharing many patients do not necessarily share them with hospitals accepting many patients. In in Table 3, the significantly positive estimate of the parameter associated to event Recurrence tells that hospitals have the tendency to reinforce their collaboration over time. Finally, we find that patient sharing is more likely between hospitals sharing common partners (Transitive closure), and between hospitals embedded in cyclic relations (Cyclic closure) even after controlling for geographic proximity in terms of distance and membership in the same territorial/administrative units (LHU).
In addressing question Q3 it is particularly interesting to note how the effects of interorganizational patient sharing routines vary across different types of patient sharing event. Patients sharing events occurring across hospitals but “within” the same clinical specialty (for example, patients leaving a coronary unit in the sender hospital to arrive at a coronary unit in the receiving hospital) are not affected by tendencies toward triadic closure. Patients sharing events occurring across hospitals and “between” different clinical specialties (for example, patients leaving a neonatal unit in the sender hospital and arriving at an intensive care unit in the receiving hospital) are significantly affected by tendencies toward transitive closure. Differences in patterns of triadic closure across event types suggest that patient transfer events embedded in transitive sequences are unlikely to be observed when hospitals are better able to assess directly the value of the partners because they share common knowledge bases and operational experiences (“within” transfers).
Unlike inter-specialty patient sharing, the number of past intra-specialty patient sharing events does not help to predict future relational events of this kind. However, once an intra-specialty transfer event connects two hospitals this relation tends to be repeated and hence to become more stable over time (see Event Recurrence). Conditional on the rest of the model, the estimated odds are roughly 2:1 to observe the recurrence of an intra-specialty transfer event between the same partner hospitals, as compared to any two other hospitals which have not yet shared patients.
Discussion
Hospitals are embedded in complex interorganizational networks of relations emerging from decentralized patient sharing decisions, activities, and arrangements. The results we have reported in the context of Italian health care clearly demonstrate that these relationships matter for the ability of patients to access higher quality care. Beyond these ongoing relationships, we show that decentralized patient sharing decisions systematically tend move patients from less to more capable hospitals. This is the case also after controlling for organization-centered rather than patient-centered considerations10. More specifically, we have shown that tendencies toward reciprocation, transitivity, assortativity and the tendency to rely on prior relations in the aggregate event sequence are also and at the same time significant among the hospitals in our sample. These organizational relationships extend beyond simple dyads of senders and receivers; sharing multiple partners – or “embeddedness” - makes two hospitals more likely to collaborate in the case of patients transferred between different specialties. Thus “embedded ties” are ties that are part of closed triadsxvii.
For readers who may be less familiar with the institutional features of the national healthcare system in the background to our study, it is important to understand that patient sharing decisions should be considered as organizational decisions taken jointly by the sending and the receiving hospital. Patients are free to decide what hospital to use but – in the typical case – they have no control over transfer decisions. Of course, patients can refuse transfer in the same way as they can refuse treatment. In such cases there will be no transfer and patients will be free to leave the hospital under their own responsibility. There are no particular constraints related to health insurance policies as long as the hospitals involved are accredited hospitals and hence recognized as legitimate participants to the system of public health (all the hospitals in our sample were either public or private accredited hospitals). Insurance is public and universal and there are no uninsured patients. Costs of care are computed on the basis of the DRG system. Documented costs of treatment are reimbursed by a single payer – occasionally with a direct contribution of the patient.
Patient outcomes may be improved if collaboration between hospitals allows patients to access more capable hospitals. This issue is important because patients would clearly like to trust that hospital collaboration effectively facilitates their access to better care. Similarly, policy makers would like to support collaboration between (possibly competing) hospitals if it leads to desirable outcomes without increasing the costs of care. Our analysis of patient sharing relations within a regional community of hospitals supports the view that decentralized collaboration between hospitals may give rise to a network of interorganizational relations that systematically helps patients to access more capable hospitals. This result is valuable because extant U.S.-centric research on interhospital patient transfer has argued that patient transfer decisions may be driven more by organizational concerns, bed availability, and established routines - and less by considerations of partner quality and capabilities. Despite the recent interest in the analysis of relational coordination between hospitals 8, xviii, to the best of our knowledge this is the first study of patient sharing relations based on newly derived relational event models that allow representing relations between hospitals in terms of sequences of individual patient sharing events.
There contextual elements that may result in differences between Italian and American hospital behavior—but that may increase the generalizability of these findings outside of the U.S. First, Italian hospitals are members neither of superordinate multihospital systems, nor of insurance groups, such as HMO (health maintenance organizations) or PPO (private public organizations). Patient sharing decisions are therefore more decentralized and less constrained by corporate boundaries or insurance policies than similar decisions that may be taken by American hospitals. Second, the general DRG-based prospective payment system typical of European countries (including Italy) is a second factor that is likely to affect the empirical scope of our findings; there may be less perceived opportunity for using transfers in order to take advantage of differential payment systems. Third, and finally, the Italian National Health Service provides universal coverage and general access to health services. In this context, hospitals are mainly public and competition is limited. In such systems competition is frequently implicit and balanced by the network of institutional relations in which public hospitals are embedded. This institutional feature of many European public health systems may be more supportive of inter-hospital collaboration strategies from which patients may benefit.
Limitations
In its current stage of development our study suffers from three main limitations - each indicating clear directions for future research. First, the period covered by the study is limited. While sample size is defined in terms of number of events – rather than calendar years – it may be useful to collect additional data in order to verify the robustness of our conclusions. We note that computational requirements increase steeply with the number of events, as possible non-events also need to be considered. For example, in the current analysis we considered all possible non-events, but larger risk sets may require sampling of non-events. Second, the value of the hospital-specific covariates is updated at yearly interval. Consequently we had to assume that the effect of covariates was piecewise constant. The extent to which this assumption actually affects the results we have reported needs to be determined using data containing information on finer grained time variation in the relevant hospital-specific covariates. Third, the measure that we adopted is generally considered as a reliable indicator of the quality of care that hospitals effectively deliver. Yet, the hospital readmission rate captures only selected aspects of quality which may be correlated with others that we have not observed directly in our studyxix. Further research is needed to assess the extent to which collaborative interhospital patient sharing relations allow patients to access better care when quality of care is evaluated on different metrics.
Conclusions
In this study we applied newly derived statistical models for the analysis of relational events to assess the extent to which interorganizational collaboration allows patients to access more capable hospitals. Our empirical analysis supports the view that this is indeed the case in the regional community of hospitals that we have examined. We have found that this result holds when we control for the main sources of hospital-level heterogeneity. The tendency of patient to flow from less to more capable hospitals continues to be detectable when we control for the main sources of relational dependencies that shape patient transfer event sequences connecting the hospital in our sample. If replicated in different institutional contexts, the results reported in this study could inspire public health care policies that better utilize decentralized collaboration and partnership between hospitals as a way to reduce costs of care and improve patient access better care. While our sample may be characterized by a number of institutional idiosyncrasies that could limit the external generalizability of our results, the problem that we have addressed remains of general interest and relevance for policy. Similarly general are the analytic solutions that we have provided.
Supplementary Material
Figure 1.
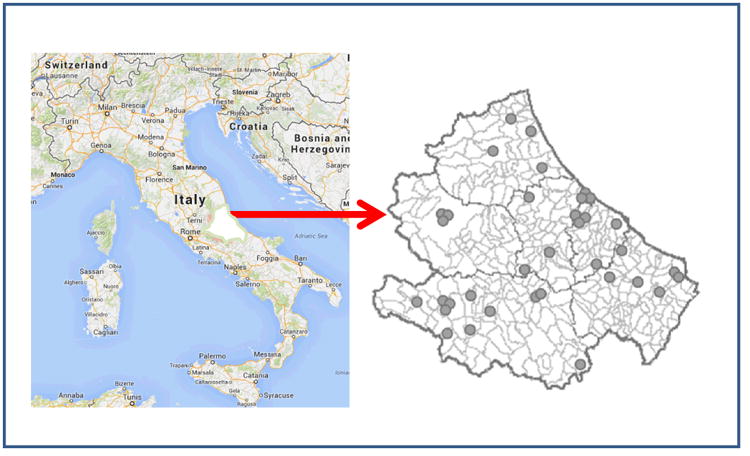
Map of Abruzzo and its location in Italy. Grey circles represent the geographical location of the hospitals in the region.
Acknowledgments
The research leading to this paper was supported in part by the European Science Foundation, European Collaborative Research Project in the Social Sciences Program (ECRP VI), by the Swiss National Science Foundation (Grant number 133273: Social Influence in Dynamic Networks) and by the NIH (NHLBI K08: HL091249)
Contributor Information
Alessandro Lomi, Email: alessandro.lomi@usi.ch, Faculty of Economics, University of Italian Switzerland, Via Buffi 13. 6900 – Lugano. Switzerland.
Daniele Mascia, Email: dmascia@rm.unicatt.it, Catholic University of the Sacred Heart, Department of Management, Largo F. Vito 1, 00199 - Rome (Italy).
Duy Quang Vu, Email: duy.vu@unimelb.edu.au, Department of Mathematics and Statistics, Richard Berry Building 111, University of Melbourne, Victoria, 3010. Australia.
Francesca Pallotti, Email: f.pallotti@gre.ac.uk, Department of International Business and Economics, Centre for Business Network Analysis, University of Greenwich, Old Royal Naval College, Park Row, London SE10 9LS (UK).
Guido Conaldi, Email: conaldi@gmail.com, Department of International Business and Economics, Centre for Business Network Analysis, University of Greenwich Old Royal Naval College, Park Row, London SE10 9LS (UK).
Theodore J. Iwashyna, Email: tiwashyn@umich.edu, University of Michigan, 2800 Plymouth Road, Bldg 16, Room 332W, Ann Arbor, MI (USA), (734) 936-5047; fax: (734) 936-5048.
References
- i.Landon BE, Keating NL, Barnett ML, MD, Onnela JP, Paul S, PhD, O'Malley AJ, Keegan T, Christakis NA. Variation in Patient-Sharing Networks of Physicians across the United States. JAMA. 2012;308(3):265–273. doi: 10.1001/jama.2012.7615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ii.Iwashyna TJ, Christie JD, Moody J, Kahn JM, Asch DA. The structure of critical care transfer networks. Medical Care. 2009;47(7):787–793. doi: 10.1097/MLR.0b013e318197b1f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- iii.Lee BY, McGlone SM, Song Y, et al. Social Network Analysis of Patient Sharing Among Hospitals in Orange County, California. American journal of Public Health. 2011;101(4):708–713. doi: 10.2105/AJPH.2010.202754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- iv.Gittell JH, Fairfield KM, Bierbaum B, Head W, et al. Impact of Relational Coordination on Quality of Care, Postoperative Pain and Functioning, and Length of Stay: A Nine-Hospital Study of Surgical Patients. Medical Care. 2000;38(8):807–819. doi: 10.1097/00005650-200008000-00005. [DOI] [PubMed] [Google Scholar]
- v.Iwashyna TJ. The incomplete infrastructure for interhospital patient transfer. Critical Care Medicine. 2012;40(8):2470–2478. doi: 10.1097/CCM.0b013e318254516f. [DOI] [PubMed] [Google Scholar]
- vi.Lomi A, Pallotti F. Relational collaboration among spatial multipoint competitors. Social Networks. 2012;34(1):101–11. [Google Scholar]
- vii.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. New England Journal of Medicine. 2006;(354):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- viii.Veinot TC, Bosk EA, Unnikrishnan KP, Iwashyna TJ. Revenue, relationships and routines: The social organization of acute myocardial infarction patient transfers in the United States. Social Science & Medicine. 2012;75:1800–1810. doi: 10.1016/j.socscimed.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ix.Iwashyna TJ, Kahn JM. Uncharted paths: Hospital networks in critical care. Chest. 2009;135(3):827–833. doi: 10.1378/chest.08-1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- x.Nuti S, Seghieri C, Vainieri M, Zett S. Assessment and improvement of the Italian healthcare system: first evidence from a pilot national performance evaluation system. J Healthc Manag. 2012;57(3):182–98. [PubMed] [Google Scholar]
- xi.Mascia D, Di Vincenzo F. Understanding hospital performance: The role of network ties and patterns of competition. Health Care Management Review. 2011;36(4):327–337. doi: 10.1097/HMR.0b013e31821fa519. [DOI] [PubMed] [Google Scholar]
- xii.Vu DQ, Asuncion AU, Hunter DR, Smyth P. Continuous-Time Regression Models for Longitudinal Networks. Proceedings of the 24th International Conference on Neural Information Processing Systems. 2011:2492–2500. [Google Scholar]
- xiii.Coffey RM, Misra A, Barrett M, Andrews RM, Mutter R, Moy E. Congestive Heart Failure: Who Is Likely to Be Readmitted? Med Care Res Rev. 2012;69:602–616. doi: 10.1177/1077558712448467. [DOI] [PubMed] [Google Scholar]
- xiv.Kiefe C, Allison JJ, de Lissovoy G. Predicting hospital readmission: different approaches raise new questions about old issues. Medical Care. 2013;51(1):11–12. doi: 10.1097/MLR.0b013e3182780afb. [DOI] [PubMed] [Google Scholar]
- xv.Pfizer SD. Should hospital readmissions be reduced through payment penalties? Medical Care. 2013;51(1):20–22. doi: 10.1097/MLR.0b013e318277eb92. [DOI] [PubMed] [Google Scholar]
- xvi.Gulati R, Gargiulo M. Where do interorganizational networks come from? American Journal of Sociology. 104(5):1439–93. [Google Scholar]
- xvii.Uzzi B. Embeddedness in the making of financial capital: how social relations and networks benefit firms seeking financing. Am Sociol Rev. 1999;64:481–505. [Google Scholar]
- xviii.Gibbons DE. Interorganizational network structures and diffusion of information through a health system. Am J Public Health. 2007;97(9):1684–1692. doi: 10.2105/AJPH.2005.063669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- xix.Laudicella M, Li Donni P, Smith PC. Discussion paper number 2012/02. Imperial College Business School; London: Hospital readmission rates: Signal of failure or success? [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


