Abstract
Purpose
Educational disparities in health persist after adjustment for income and occupation, suggesting that other purely cognitive and psychosocial mechanisms may be involved. Unlike occupation- or income-mediated effects, effects of cognitive and psychosocial gains—as reflected in academic achievement—may be apparent even before schooling is completed.
Methods
We used data spanning 10 years on a national U.S. cohort of 2,546 children aged 3–14 at baseline to estimate effects of academic achievement, measured by standardized tests of cognitive achievement, on future health. We used marginal structural models to address potential mutual influence of achievement and health on each other over time.
Results
One standard deviation higher academic achievement 1997– 2002 was associated with a lower prevalence of poorer health status in 2007 in girls (prevalence ratio [PR] = 0.87 [(95% confidence interval) 0.78–0.97]) but not in boys (PR = 0.96 [0.86–1.08]). Higher achievement was also weakly associated with lower BMI and less psychological distress among girls only.
Conclusions
Academic achievement may benefit future health but a number of questions remain unanswered, including reasons for the gender differences and how academic-achievement-related health disparities may progress over the life course and interact with other social determinants of health.
Keywords: academic achievement, body mass index, children and adolescents, education, gender, health status, marginal structural models, mental health
It is often hypothesized that education affects health through its effects on occupation and income [1, 2]. However, education-related health disparities persist after adjustment for income and occupation [3]. This suggests that other processes, including purely cognitive and psychosocial benefits of the learning process, may be involved. If these mechanisms are important, students who more successfully make cognitive and psychosocial gains—for example, as reflected in their academic achievement—may enjoy better health even before they complete their schooling and socioeconomic sequelae manifest. Higher academic achievement may reflect cognitive gains that help students better understand and act on information about healthy behaviors such as eating a healthy diet, exercising, not smoking, or hand washing [3, 4]. It may also benefit health through psychosocial mechanisms by fostering higher self-esteem, a greater sense of personal control, the patience and time preference to invest in healthier behaviors, more social integration and social support, or a peer group with more healthful behavioral norms [5–7].
These mechanisms are in contrast to occupation- or income-mediated effects, which would not appear until students enter the workforce. Understanding them could be an important tool for reducing health disparities by fostering educational practices that maximize future health benefits regardless of students’ future economic circumstances. Yet relatively few studies have investigated how academic achievement relates to health, and most have used cross-sectional data or short follow-up times [8–16]. We used three waves of data spanning 10 years on a national cohort of children aged 3–14 at baseline to estimate effects of academic achievement on health during the schooling process.
Our primary health outcome was self-rated global health status, a relevant health measure for young populations among whom serious medical conditions are rare [17–19]. Self-rated health status is correlated in adolescents and young adults with disability, health services use, physical and mental health, and health behaviors [19–22]. In secondary analyses we examined two additional health outcomes, body mass index (BMI) and psychological distress, which might contribute to an association between academic achievement and health status. Low or high BMI and psychological problems have both been associated with poorer self-rated health status in national samples of young people [17, 19, 21], as well as with poorer academic achievement [9, 11, 12, 16].
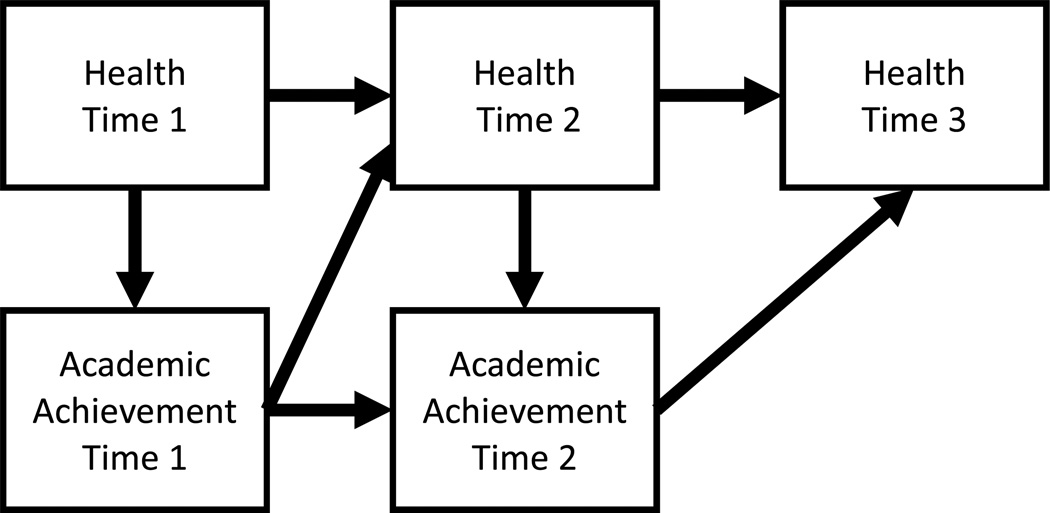
An important challenge is the possibility of reverse causation: students’ health may influence their success in school. Poor health may affect students’ ability to attend school regularly, pay attention in classes, complete assignments, interact with peers and teachers, or invest in long-term educational goals [23–25]. Figure 1 shows this theorized mutual influence of health and academic achievement on each other over time. This presents a methodological challenge in longitudinal analyses because health during follow-up (Health at Time 2 in Figure 1) both mediates the health effect of prior achievement and confounds the effect of future achievement (i.e., is a time-dependent confounder). Therefore, adjusting for health during follow-up may create overadjustment bias while failing to do so may create confounding bias. We addressed potential time-dependent confounding in academic achievement–health associations by using marginal structural models (MSMs) [26].
Figure 1.
Assumed causal structure of health and academic achievement
Academic achievement is assumed to be influenced by health at each time-point, and in turn to influence health at future time-points.
We hypothesized that a history of higher academic achievement decreases the risk of poor health among adolescents and young adults. We also hypothesized that conventional models adjusting for health during follow-up underestimate the effect of academic achievement on health. Finally, based on stronger associations observed among girls in previous studies on this topic [8, 14, 16], we hypothesized that there are sex differences in effects of academic achievement on health.
METHODS
Study population
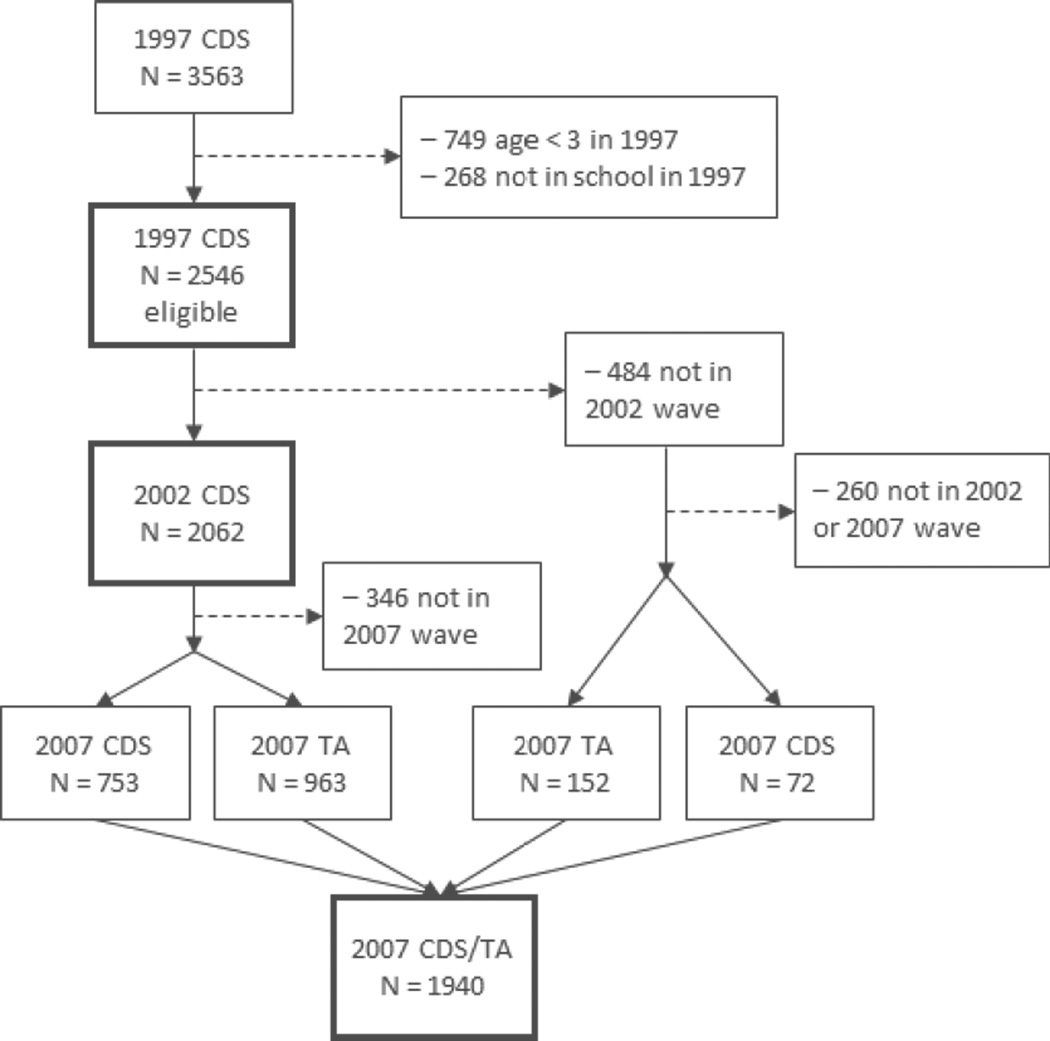
We used publicly available data from two supplementary studies to the Panel Study of Income Dynamics (PSID), a longitudinal study of a representative (after weighting) sample of U.S. families started in 1968 [27]. The Child Development Supplement (CDS) began in 1997 with a sample of 3,563 children drawn from PSID families with a child aged 0–12 in calendar year 1997, with up to two children chosen per family. Black and low-income families were oversampled. Subsequent study waves were conducted in 2002–2003 and 2007–2008. The primary interviewee is the participant’s primary caregiver, in over 90% of cases the child’s biological mother. The children themselves are also interviewed; interview content varies by the child’s age. The Transition Into Adulthood Study (TA), started in 2005, comprises young adults who “aged out” of the CDS by turning 18 and finishing or leaving high school. All questions in the TA are answered by the participants themselves. We combined data from the 1997 CDS, the 2002–2003 CDS (“2002 CDS”), and either the 2007–2008 CDS (“2007 CDS”) or the 2007 TA to create a longitudinal sample with three waves of interviews spanning 10 years. The analysis sample, including only children who were at least 3 years old and enrolled in a childcare center or school at baseline, was 2,546 children aged 3–14 years by the time their baseline interviews were completed and 14–24 years at the third interview (Figure 2).
Figure 2.
Study sample from Child Development Supplement (CDS) and Transition into Adulthood (TA) supplemental studies to the Panel Study of Income Dynamics, 1997–2007
Measures
The primary outcome was 2007 health status, with prior health status treated as a time-dependent confounder (Figure 1). We dichotomized the 5-point scale into “very good” (excellent/very good) and “poorer” (good/fair/poor). We chose this dichotomization instead of excellent/very good/good vs. fair/poor because the number of participants with fair or poor health was very small, particularly in the earlier study waves (e.g., 3% in 1997). Ordinal logistic regression models provided consistent results but the data violated the proportional odds assumption. Because the survey questionnaire content varied depending on the age of the participant, the measure was reported by the participant in 2007 but by the primary caregiver in 1997 and 2002. We also included measures of perinatal health (low birth weight [< 88 ounces] and the primary caregiver’s assessment of the child’s health at birth) as baseline confounders.
As with health status, the outcomes of interest for the secondary analyses of BMI and psychological distress were the 2007 measures, with prior measures treated as time-dependent confounders. BMI (kg/m2) was calculated from height and weight. Baseline height was reported by the participant’s caregiver; baseline weight, 2002 height and weight, and 2007 height and weight for CDS participants were measured by the interviewer; 2007 height and weight for TA participants were self-reported. Psychological distress was measured using the K6 non-specific psychological distress scale developed for use in the U.S. National Health Interview Survey (NHIS) [28]. Because the K6 was administered in the TA but not the CDS, analyses using the K6 were limited to participants aged 18 or over in 2007 (n = 1475). For the same reason, the K6 measure was not available in 2002 to serve as a time-dependent confounder; instead we used the Children’s Depression Inventory (CDI) Short Form, the measure of mental health administered in the 2002 CDS [29]. The correlation between 2002 CDI and 2007 K6 scores was 0.21 (p < .001). No scale of mental health was available at baseline.
The exposure variable was average academic achievement over five years. We characterized academic achievement using the Letter-Word Identification and Applied Problems subtests of the Woodcock-Johnson Psycho-Educational Battery-Revised Achievement Tests (WJ-R ACH), administered in the 1997 and 2002 CDS. These subtests, part of a battery of 39 tests of intellectual processing, test aspects of the test-taker’s stores of acquired knowledge in language and math, respectively [29, 30]. The Letter-Word Identification test asks participants to identify or correctly pronounce letters or words without context; it is not necessary to know the meanings of the words. The Applied Problems test consists of math questions ranging from counting a number of objects to word problems. In both tests, participants complete progressively more difficult questions until they reach a “ceiling” in which they are unable to complete a set number of questions in a row; the raw score equals the number of correct responses, with a possible range of 0–57 for Letter-Word Identification and 0–60 for Applied Problems [29]. The tests have standardized administration and scoring protocols, were norm-referenced to a nationally standardized sample of 6,359 people aged 2–90, and have been widely used in a variety of populations [29, 30]. To create the cumulative measure of average 5-year academic achievement, we averaged each child’s age-standardized Letter-Word Identification and Applied Problems scores to create a measure of overall academic achievement in each wave, then averaged the 1997 and 2002 scores. This measure was normally distributed with a mean of 101.9 and ranged 42.0–169.5; higher scores indicate better achievement.
In addition to the time-dependent confounding effects of prior health, we also considered a range of potential time-invariant and time-varying confounders. We capitalized on the richness of the PSID data to incorporate information from nine broad domains that may influence both schooling and future health in young people: demographic characteristics, family composition, family socioeconomic status, neighborhood characteristics, geographical characteristics, perinatal health, health care use, schooling characteristics, and caregiver academic ability. The variables we used corresponding to these domains are listed in Appendix Table A1.
Analysis
To handle missing information, multiple imputation with 25 imputations was carried out using the sequential regression method with IVEware software, simultaneously including information from all three study waves and including auxiliary variables predictive of analysis variables with large amounts of missing information (Table A1) [31–33].
We contrasted three types of models, each estimating the effect of one standard deviation (approximately 15 points; calculated separately in each imputed data set) higher average achievement 1997–2002 on health in 2007. First, we estimated models adjusted only for baseline confounders. In the presence of time-dependent confounding, these models may produce biased estimates because of confounding by health during follow-up. Second, we estimated “naively time-varying-confounder-adjusted” models that were additionally adjusted for 2002 values of time-varying confounders. These models may produce biased estimates because of inappropriate adjustment for mediators of academic achievement. Third, we estimated marginal structural models (MSMs) that addressed possible time-dependent confounding through inverse-probability-of-exposure weighting rather than adjustment [26]. We tested interactions between academic achievement and sex in all models; in sensitivity analyses, separate sex-specific models produced very similar findings. All models were estimated with robust standard error estimates, which account for correlations between siblings. In sensitivity analyses, models additionally incorporating CDS sampling weights produced nearly identical estimates, as did models using quintiles of academic achievement.
To estimate the MSMs, a stabilized treatment (i.e., exposure) weight swi was constructed for each participant using linear regression and the normal probability density function to estimate probability densities of observed academic achievement conditional on covariates [34] (see Appendix for details). Final marginal structural outcome models of 2007 health with average academic achievement 1997–2002 as the exposure were estimated incorporating the exposure weights and adjusting for baseline characteristics [34, 35].
We used Poisson regression to calculate prevalence ratios for poorer health status and being in the highest quartile of the K6 scale (“serious psychological distress”) in 2007 [36]. We log-transformed the BMI measure because of its skewed distribution and modeled it using linear regression. In a sensitivity analysis, analyses of the BMI outcome excluding observations underweight in 1997 (< 5th percentile according to the Centers for Disease Control & Prevention 2000 growth chart [37]) produced nearly identical results.
RESULTS
There was substantial and nonmotonic case missingness in the data: 67% of participants completed all three study waves, 23% missed either wave 2 or wave 3, and 10% missed both wave 2 and wave 3 (Figure 2). Twenty-nine percent and 27% of participants were missing academic achievement scores in 1997 and 2002, respectively. In 2007, 26% of participants were missing information for health status, 28% for BMI, and 21% for psychological distress.
Variable distributions were very similar in the original and imputed data sets (Appendix table A2). About two-thirds of the participants had a sibling in the sample. At baseline, 21% lived below the Federal poverty line and 18% had no caregiver with a high school degree (Table 1). The majority of participants had good overall health status, were of normal weight, and reported few mental distress symptoms, but over a third were overweight or obese and 43% reported less than excellent or very good health status in 2007 (Table 1). Academic achievement was positively associated with family income and caregiver education, caregiver achievement score, living with two parents, supportiveness of the home environment, neighborhood quality, residence in the Northeast, private school attendance, health status, and normal BMI status; and negatively associated with low birth weight, hospital stays, behavior problems, changing schools, repeating a grade, and mental distress symptoms (Table 1; not all variables shown). Poorer 2007 self-rated health status was associated with female sex, lower family income and caregiver schooling, poorer previous caregiver-rated health status, high BMI in all waves and underweight BMI status in 2007, poorer mental health, more problem behaviors, poorer perinatal health, and more overnight hospital stays (Table 1; not all shown).
Table 1.
Mean academic achievement score and 2007 health status by category of selected predictors (N = 2546)a
| Sample percent |
Mean academic achievement 1997–2002 |
Poorer self-rated health status 2007b |
|||
|---|---|---|---|---|---|
| Mean | pc | Percent | pd | ||
| Total | -- | 101.9 | -- | 43 | -- |
| Sex | 0.28 | 0.05 | |||
| Male | 51 | 102.8 | 40 | ||
| Female | 49 | 103.5 | 46 | ||
| Age at 1997 interview (years) | 0.20 | 0.21 | |||
| 3–5 | 18 | 103.1 | 47 | ||
| 6–8 | 31 | 103.0 | 43 | ||
| 9–11 | 31 | 103.9 | 39 | ||
| 12–14 | 20 | 102.0 | 44 | ||
| Race/Hispanicity | <0.001 | 0.33 | |||
| non-Hispanic white | 46 | 108.4 | 42 | ||
| non-Hispanic black | 42 | 97.7 | 42 | ||
| Hispanic | 8 | 100.5 | 47 | ||
| Other | 5 | 104.4 | 50 | ||
| Number of parent figures live with 1997 | <0.001 | 0.40 | |||
| 0 | 1 | 96.2 | 50 | ||
| 1 | 30 | 98.7 | 45 | ||
| 2 | 69 | 105.1 | 42 | ||
| Primary caregiver achievement score quartile 1997 | <0.001 | 0.59 | |||
| 1 (4.0–26.99) | 23 | 96.3 | 43 | ||
| 2 (27.0–30.99) | 25 | 100.7 | 44 | ||
| 3 (31.0–34.27) | 27 | 105.2 | 43 | ||
| 4 (34.28–43.0) | 25 | 109.6 | 40 | ||
| Family income/poverty ratio 1996 | <0.001 | 0.003 | |||
| 0–0.9 | 21 | 96.8 | 48 | ||
| 1–1.9 | 22 | 99.9 | 46 | ||
| 2–4.9 | 44 | 104.9 | 42 | ||
| ≥5 | 13 | 112.2 | 33 | ||
| Maximum of caregivers' completed years schooling 1997 | <0.001 | 0.03 | |||
| <9 | 3 | 97.1 | 51 | ||
| 9–11 | 9 | 96.0 | 51 | ||
| 12 | 35 | 99.7 | 44 | ||
| 13–15 | 28 | 103.1 | 40 | ||
| ≥16 | 24 | 111.7 | 39 | ||
| Primary caregiver-rated health compared to other babies at birth | <0.001 | 0.34 | |||
| Better | 26 | 105.2 | 41 | ||
| Same | 65 | 102.8 | 43 | ||
| Worse | 9 | 99.6 | 48 | ||
| Low birth weight (<2500 g) | <0.001 | 0.68 | |||
| Yes | 9 | 98.6 | 41 | ||
| No | 91 | 103.6 | 43 | ||
| Primary caregiver-rated health 1997 | <0.001 | 0.03 | |||
| Very good | 81 | 104.1 | 42 | ||
| Poorer | 19 | 99.1 | 48 | ||
| Primary caregiver-rated health 2002 | <0.001 | 0.03 | |||
| Very good | 78 | 104.1 | 41 | ||
| Poorer | 22 | 99.7 | 49 | ||
| Self-rated health 2007 | 0.001 | -- | |||
| Very good | 57 | 104.3 | -- | ||
| Poorer | 43 | 101.6 | -- | ||
| BMI percentile 1997 | <0.001 | 0.008 | |||
| < 5 (underweight) | 13 | 99.8 | 41 | ||
| 5–84.9 (normal) | 52 | 104.6 | 40 | ||
| 85–94.5 (overweight) | 14 | 103.3 | 41 | ||
| ≥ 95 (obese) | 21 | 101.2 | 50 | ||
| BMI percentile 2002 | 0.001 | <0.001 | |||
| < 5 (underweight) | 5 | 101.7 | 38 | ||
| 5–84.9 (normal) | 55 | 104.1 | 37 | ||
| 85–94.5 (overweight) | 17 | 103.6 | 46 | ||
| ≥ 95 (obese) | 23 | 100.7 | 56 | ||
| BMI status 2007 (age ≤ 21/21+) | <0.001 | <0.001 | |||
| < 5th percentile/<18.5 (underweight) | 5 | 102.4 | 45 | ||
| 5–84.9th percentile/18.5–24.9 (normal) | 53 | 104.6 | 36 | ||
| 85–94.5/25–29.9 (overweight) | 22 | 101.8 | 46 | ||
| ≥ 95th percentile/≥ 30 (/obese) | 20 | 100.9 | 57 | ||
| Children's Depression Inventory quartile 2002 (age 12+) | 0.03 | 0.04 | |||
| 1 | 19 | 105.5 | 36 | ||
| 2 | 31 | 103.7 | 39 | ||
| 3 | 24 | 103.0 | 44 | ||
| 4 | 25 | 101.8 | 47 | ||
| K-6 Non-Specific Psychological Distress Scale quartile 2007 (age 18+) | 0.03 | <0.001 | |||
| 1 | 25 | 103.0 | 34 | ||
| 2 | 27 | 104.9 | 40 | ||
| 3 | 23 | 102.6 | 45 | ||
| 4 | 25 | 101.7 | 52 | ||
Uses imputed data.
Good/fair/poor (vs. excellent/very good).
From unadjusted linear regression with clustering by sibling pair.
From unadjusted logistic regression with clustering by sibling pair.
In models, average academic achievement 1997–2002 was inversely associated with poorer health status in 2007 (Table 2) but the overall association was driven by results among girls (p for interaction = 0.12 in the MSM). In the MSM, each standard deviation higher academic achievement was related to a 13% lower prevalence of poorer 2007 health status among girls (prevalence ratio [PR] = 0.87 [95% confidence interval] 0.78–0.97) but negligibly less poorer health status among boys (PR = 0.96 [0.86–1.08]). The MSMs produced only minimally different point estimates than the baseline- and naively time-varying-confounder-adjusted models.
Table 2.
Prevalence ratios of poorer self-rated health 2007 for 1-standard-deviationa higher average academic achievement 1997–2002, by sex
| Combined |
Boys |
Girls |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Model Type | Covariates | PR | 95% CI | p | PR | 95% CI | p | PR | 95% CI | p | Interaction p |
| Unweighted | None | 0.90 | (0.84, 0.97) | 0.004 | 0.94 | (0.85, 1.03) | 0.20 | 0.86 | (0.78, 0.95) | 0.002 | 0.17 |
| Unweighted | Baselineb | 0.91 | (0.84, 0.99) | 0.03 | 0.95 | (0.85, 1.06) | 0.35 | 0.87 | (0.79, 0.97) | 0.01 | 0.20 |
| Unweighted | Baseline and time-varyingc | 0.93 | (0.85, 1.01) | 0.08 | 0.96 | (0.86, 1.07) | 0.47 | 0.89 | (0.81, 0.99) | 0.04 | 0.27 |
| MSM | Baselineb | 0.91 | (0.83, 1.00) | 0.05 | 0.96 | (0.86, 1.08) | 0.49 | 0.87 | (0.78, 0.97) | 0.01 | 0.12 |
Standard deviation was calculated separately for each imputation. Values ranged 14.7–15.1, with a mean of 14.9.
Model includes baseline age, sex, race, perinatal health, caregiver education, number of parents in household, HOME scale, household income, region, urbanicity, whether the child had repeated a grade, and the primary caregiver’s achievement score as covariates.
Model includes baseline adjustment variables + time-varying measures of family income, neighborhood rating, health status, overnight hospital stays, BMI percentile, problem behaviors, school type, and whether the child switched schools in the current year.
Models of the other health outcomes produced results generally consistent with the ones for health status. In the MSM, each standard deviation higher academic achievement was weakly associated with a 1.4% lower BMI (Table 3; % difference = −1.36 [−3.12, 0.44]) among girls but a negligible difference among boys (% difference = −0.14 [−1.60, 1.35]). In the combined models and among girls, estimates from the models of BMI were indicative of the pattern we would expect in the presence of time-dependent confounding: the MSM estimates were smaller in magnitude than those from the unweighted baseline-adjusted model but larger than those from the naively time-varying-confounder-adjusted model. Among participants aged 18 and over in 2007, in the MSM, each standard deviation higher achievement was weakly associated with a lower prevalence of serious psychological distress among girls (Table 4; PR = 0.82 [0.64–1.05]) but not among boys (PR = 0.98 [0.79–1.22]). Similar to the models of health status, point estimates were very similar between the different adjusted models.
Table 3.
Percent difference in 2007 BMI associated with 1-standard-deviation higher average academic achievement 1997–2002a, by sex
| Combined |
Boys |
Girls |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Model Type | Covariates | Diff | 95% CI | p | Diff | 95% CI | p | Diff | 95% CI | p | Interaction p |
| Unweighted | None | −1.83 | (−2.89, −0.77) | <0.001 | −1.08 | (−2.51, 0.37) | 0.14 | −2.70 | (−4.13−1.24) | <0.001 | 0.11 |
| Unweighted | Baselineb | −0.88 | (−2.07, 0.31) | 0.15 | −0.26 | (−1.76, 1.25) | 0.73 | −1.58 | (−3.07, −0.07) | 0.04 | 0.16 |
| Unweighted | Baseline and time-varyingc | −0.52 | (−1.51, 0.50) | 0.30 | −0.19 | (−1.35, 0.97) | 0.74 | −0.90 | (−2.13, 0.35) | 0.16 | 0.31 |
| MSM | Baselineb | −0.71 | (−1.98, 0.58) | 0.28 | −0.14 | (−1.60, 1.35) | 0.86 | −1.36 | (−3.12, 0.44) | 0.14 | 0.24 |
Calculated from coefficients and 95% confidence intervals from linear regression of the natural log of BMI using the formula: % difference = 100*(exp(b) − 1)). Standard deviation of average academic achievement was calculated separately for each imputation. Values ranged 14.7–15.1, with a mean of 14.9.
Model includes baseline age, sex, race, perinatal health, caregiver education, number of parents in household, HOME scale, household income, region, urbanicity, whether the child had repeated a grade, and the primary caregiver’s achievement score as covariates.
Model includes baseline adjustment variables + time−varying measures of family income, neighborhood rating, health status, overnight hospital stays, BMI percentile, problem behaviors, school type, and whether the child switched schools in the current year.
Table 4.
Prevalence ratios of serious psychological distress for 1-standard-deviation higher average academic achievement 1997–2002a, by sex
| Combined |
Male |
Female |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Model Type | Covariates | PR | 95% CI | p | PR | 95% CI | p | PR | 95% CI | p | Interaction p |
| Unweighted | None | 0.84 | (0.73, 0.97) | 0.02 | 0.92 | (0.76, 1.12) | 0.39 | 0.77 | (0.61, 0.95) | 0.02 | 0.24 |
| Unweighted | Baselineb | 0.89 | (0.76, 1.05) | 0.16 | 0.95 | (0.77, 1.17) | 0.65 | 0.82 | (0.65, 1.04) | 0.10 | 0.34 |
| Unweighted | Baseline and time-varyingc | 0.91 | (0.77, 1.07) | 0.26 | 0.97 | (0.78, 1.20) | 0.76 | 0.85 | (0.67, 1.07) | 0.17 | 0.40 |
| MSM | Baselineb | 0.91 | (0.76, 1.07) | 0.25 | 0.98 | (0.79, 1.22) | 0.85 | 0.82 | (0.64, 1.05) | 0.12 | 0.28 |
Includes only participants aged at least 18 years in 2007: N = 36,293 in imputed sample, including information for 1475 participants. Standard deviation was calculated separately for each imputation based on the entire sample. Values ranged 14.7–15.1, with a mean of 14.9.
Model includes baseline age, sex, race, perinatal health, caregiver education, number of parents in household, HOME scale, household income, region, urbanicity, whether the child had repeated a grade, and the primary caregiver’s achievement score as covariates.
Model includes baseline adjustment variables + time-varying measures of family income, neighborhood rating, health status, overnight hospital stays, BMI percentile, problem behaviors, childhood depression scale (2002), school type, and whether the child switched schools in the current year.
DISCUSSION
In a national sample of U.S. youth aged 3–14 at baseline, higher average academic achievement 1997–2002 was associated with better health in 2007 (better health status, lower BMI, less serious psychological distress) among girls but consistently less so for boys. The gender pattern we observed mirrors results from studies of similar outcomes in adults, where associations between more schooling and better self-rated health status, less depression, and less obesity have been stronger in women than in men [3, 38, 39]. Studies of gender differences in associations between academic achievement and health among youth are rarer and their evidence is mixed. School performance was slightly more strongly associated with subjective health complaints in girls than boys among Hungarian 9th-graders [8] and school grades were more predictive of depressive symptoms a year later in girls than boys among adolescents in Norway [16]. On the other hand, gender differences were not reported in associations between lower school performance and worse self-rated health among students in Hungary [14] or overweight among American adolescents [12]. Future research examining gender differences in how academic achievement relates to health is needed. These differences may reflect objective mechanistic differences in how schooling influences health, as well as gender differences in how people incorporate information when reporting their health [40].
Contrary to our hypothesis, accounting for mutual influence of academic achievement and health over time with MSMs did not produce meaningfully different results, particularly for the health status and psychological distress outcomes. One explanation is that there may not have been substantial time-dependent confounding in these associations. Appendix Table A3 and Figure A1 list four preconditions for the potential usefulness of MSMs for a given research question and demonstrate how these preconditions apply to our question for the health status outcome [34]. Although our measures met the preconditions when tested in unadjusted models, many of the associations were weak—although in expected directions—after adjustment for relevant covariates.
The reliance on self- and proxy-reported information, a limitation of this analysis, may have resulted in large and/or correlated errors in measurement of different variables. However, exposure information came from validated and interviewer-administered academic achievement tests. In adults, self-rated health status is predictive of morbidity and mortality [41, 42] but it can be unreliable [43] and its predictive power tends to be lower among individuals with lower socioeconomic status [44]. The properties of self-rated health status in adolescents have been less examined but studies have found that the measure is correlated with physical and psychological health conditions, pain, and family socioeconomic status, and is relatively stable over time [21, 22, 45]. Another consideration is that 2007 health status was reported by the participant while the earlier measures were reported by the caregiver; the two sources may have based their assessments on different facets of health. In a sensitivity analysis, restricting the sample to participants aged 5 years or older in 1997 (those old enough to self-report their own health status in 2002) and replacing the 2002 caregiver-reported measure with the self-reported measure in the MSM did not affect our results. Our results may also have been affected by missing data and attrition if missing values were related to unobserved variables, particularly given the large volume of missing exposure and outcome information.
This analysis was, to our knowledge, the first to investigate whether academic achievement affects future adolescent and young adult health while accounting for time-dependent confounding. Although small, the associations we observed are consistent with the hypothesis that—at least among girls—schooling may benefit health through mechanisms related to the learning process that are distinct from income-mediated mechanisms associated with educational attainment. A number of questions remain unanswered, including the reasons for the gender differences, the specific mechanisms for these effects and the health outcomes for which they are most important, and how these academic-achievement-related health disparities may progress over the life course and interact with other social determinants of health.
Acknowledgments
The authors thank Bob Schoeni and Brisa Sánchez for their valuable input.
Financial support:
The collection of PSID data used in this study was partly supported by the National Institutes of Health under grant number R01 HD069609 and the National Science Foundation under award number 1157698. The authors thank the Robert Wood Johnson Foundation Health & Society Scholars program at the University of Michigan for its financial support.
Appendix
MULTIPLE IMPUTATION
Table A1.
Variables used in multiple imputation and estimation of treatment weights
| Multiple imputation | Treatment weights | |
|---|---|---|
| Variables | Years used | Years used |
| Demographic | ||
| Sex | 1997 | 1997 |
| Age | 1997, 2002, 2007 | 1997 |
| Race | 1997 | 1997 |
| Family composition | ||
| Family size | 1997, 2002 | |
| Head of household's marital status | 1997 | |
| Number of parent figures/guardians lives with | 1997, 2002, 2007 | 1997, 2002 |
| Lives with a partner (age ≥ 18) | 2007 | |
| Birth order to mother | 1997 | |
| Sibling in 1997 CDS | 1997 | |
| Family socioeconomic status & environment | ||
| Maximum of parents' years schooling at birth | 1997 | |
| Maximum of caregivers' years schooling | 1997, 2002 | 1997 |
| Family poverty threshold | 1996, 2002, 2006 | |
| ln(Family income-to-poverty ratio) | 1996, 2002, 2006 | 1996, 2002 |
| HOME scale | 1997 | 1997 |
| Neighborhood characteristics | ||
| Years lived in current neighborhood | 1997, 2002 | |
| Rating of neighborhood as a place to raise children | 1997, 2002 | 1997, 2002 |
| Neighborhood dangerous to walk around alone after dark | 1997, 2002 | |
| Geographical characteristics | ||
| Urbanicity | 1997, 2001, 2003, 2007 | 1997 |
| Region | 1997, 2001, 2003, 2007 | 1997 |
| Perinatal health | ||
| Birth weight | 1997 | |
| Low birth weight | 1997 | |
| Spent time in neonatal intensive care unit | 1997 | |
| Primary caregiver's rating of health at birth | 1997 | 1997 |
| Current physical health and health care use | ||
| Primary caregiver's rating of health status | 1997, 2002 | 1997, 2002 |
| Self-rated health status | 2002, 2007 | |
| Body mass index | 1997, 2002, 2005 (TA), 2007 | 1997, 2002 |
| Number of overnight hospital stays | 1997, 2002, 2007 | 1997, 2002 |
| Routine physician check-up in past 2 years | 1997, 2002 | 1997, 2002 |
| Primary caregiver’s self-rated health status | 1997, 2002 | |
| Mental health and well-being | ||
| Children's Depression Inventory (age 12+) | 2002, 2007 | 2002 |
| K-6 Nonspecific Psychological Distress Scale (TA only; age 18+) | 2005, 2007 | |
| Physician diagnosis of serious emotional disturbance | 1997, 2002 | |
| Physician diagnosis of depression (TA only; age 18+) | 2007 | |
| Global self-concept (CDS version; age 8+ in 1997, age 10+ in 2002, 2007) | 1997, 2002, 2007 | |
| Global self-concept compared to others (TA version; age 18+) | 2005, 2007 | |
| Emotional well-being subscale (age12+) | 2002, 2007 | |
| Psychological well-being subscale (age 12+) | 2002, 2007 | |
| Social well-being subscale (age 12+) | 2002, 2007 | |
| Behaviors | ||
| Behavior Problems Index (age ≤ 19) | 1997, 2002, 2007 | 1997, 2002 |
| Internalizing Behaviors subscale | 1997, 2002, 2007 | |
| Externalizing Behaviors subscale | 1997, 2002, 2007 | |
| Categories of # arrests (age 12+) | 2002, 2005 (TA),2007 | |
| Drunk driving past 6 mos (age 12+) | 2007 | |
| Rode w/drunk driver past 6 mos (age 12+) | 2007 | |
| How often wear seatbelt (age 10+) | 2002 | |
| Did something dangerous past 6 mos just for thrill (TA only) | 2005, 2007 | |
| Regular smoker (age 11+) | 2002, 2007 | |
| Friend influences (CDS version; 9.5 ≤ age ≤ 19) | 2002, 2007 | |
| Friend influences (TA version; age 18+) | 2005, 2007 | |
| Friend influences (CDS & TA combined) | 2007 | |
| Schooling | ||
| Years completed schooling | 1997, 2002, 2007 | |
| Degrees completed | 2007 | |
| Ever repeated a grade | 1997 | 1997 |
| Whether in school | 2002, 2007 | 2002 |
| Type of school | 1997, 2002 | 1997, 2002 |
| Changed school during current school year | 1997, 2002 | 1997, 2002 |
| Academic achievement | ||
| Academic achievement score | 1997, 2002 | 1997, 2002 |
| Primary caregiver's achievement score | 1997 | 1997 |
Table A2.
Distributions of characteristics in original and imputed samples
| Original sample |
Imputed sample |
||
|---|---|---|---|
| Characteristic | N or range | %a or mean (SEb) |
% or mean (SEb) |
| Total | 2546 | --- | 63,650 |
| Female | 1248 | 51 | 51 |
| Age in years 1997 | 3.0–13.9 | 8.5 (0.059) | 8.5 (0.059) |
| Missing | 0 | 0 | --- |
| Age in years 2002 | 7.8–19.3 | 14.0 (0.068) | 14.0 (0.068) |
| Missing | 679 | 679 | --- |
| Age in years 2007 | 12.8–24.0 | 19.0 (0.068) | 18.9 (0.059) |
| Missing | 671 | 671 | --- |
| Race/Hispanicity | |||
| non-Hispanic white | 1160 | 46 | 46 |
| non-Hispanic black | 1063 | 42 | 42 |
| Hispanic | 193 | 8 | 8 |
| Other race | 127 | 5 | 5 |
| Missing | 3 | <1 | --- |
| Number of parent figures live with 1997 | |||
| 0 | 24 | 1 | 1 |
| 1 | 756 | 30 | 30 |
| 2 | 1762 | 69 | 69 |
| Missing | 4 | <1 | --- |
| Number of parent figures live with 1997 | |||
| 0 | 3 | <1 | 7 |
| 1 | 621 | 30 | 31 |
| 2 | 1438 | 70 | 62 |
| Missing | 484 | 19 | --- |
| Marital status of head of household 1997 | |||
| Married | 1606 | 63 | 63 |
| Never married | 406 | 16 | 16 |
| Divorced/Separated/Widowed | 533 | 21 | 21 |
| Missing | 1 | <1 | --- |
| HOME scale 1997 | 8.8–24.0 | 18.9 (0.058) | 18.7 (0.058) |
| Family income/poverty ratio 1996 | 0–36.9 | 2.9 (0.068) | 2.9 (0.068) |
| Missing | 0 | 0 | --- |
| Family income/poverty ratio 2002 | 0–111.6 | 3.7 (0.13) | 3.4 (0.13) |
| Missing | 186 | 7 | --- |
| Maximum of caregivers' completed years education 1997 | 3–17 | 13.2 (0.062) | 13.2 (0.061) |
| <9 | 84 | 3 | 3 |
| 9–11 | 234 | 9 | 9 |
| 12 | 897 | 36 | 35 |
| 13–15 | 694 | 28 | 28 |
| ≥16 | 613 | 24 | 24 |
| Missing | 24 | 1 | --- |
| Caregiver achievement score | 4–43 | 30.6 (0.16) | 30.4 (0.14) |
| Missing | 631 | 25 | --- |
| Neighborhood as place to raise children 1997 | |||
| Excellent | 427 | 27 | 27 |
| Very good | 481 | 30 | 30 |
| Good | 408 | 26 | 27 |
| Fair/Poor | 263 | 17 | 17 |
| Missing | 967 | 38 | --- |
| Neighborhood as place to raise children 2002 | |||
| Excellent | 621 | 30 | 31 |
| Very good | 633 | 31 | 29 |
| Good | 450 | 22 | 22 |
| Fair/Poor | 345 | 17 | 17 |
| Missing | 497 | 20 | --- |
| Urbanicity 1997 | |||
| Central county, metropolitan area ≥1M | 754 | 30 | 30 |
| County, metropolitan area ≥250K | 1044 | 41 | 41 |
| Area <250K | 748 | 29 | 29 |
| Region 1997 | |||
| Northeast | 362 | 14 | 14 |
| North Central | 624 | 25 | 25 |
| South | 1152 | 45 | 45 |
| West | 407 | 16 | 16 |
| Missing | 1 | <1 | --- |
| Primary caregiver-rated health compared to other babies at birth | |||
| Same | 1633 | 65 | 65 |
| Better | 662 | 26 | 26 |
| Worse | 225 | 9 | 9 |
| Missing | 26 | 1 | --- |
| Low birth weight (<2500 g) | 219 | 9 | 9 |
| Missing | 62 | 2 | --- |
| Spent time in NICU after birth | 313 | 12 | 12 |
| Missing | 38 | 1 | --- |
| Number overnight hospital stays birth–1997 | |||
| 0 | 1912 | 75 | 75 |
| 1–2 | 519 | 20 | 20 |
| ≥3 | 107 | 4 | 4 |
| Missing | 8 | <1 | --- |
| Number overnight hospital stays 1997–2002 | |||
| 0 | 1859 | 90 | 89 |
| 1–2 | 171 | 8 | 9 |
| ≥3 | 31 | 2 | 2 |
| Missing | 485 | 19 | --- |
| Routine physician check-up 1996–1997 | 1952 | 78 | 78 |
| Missing | 40 | 2 | --- |
| Routine physician check-up in 2001–2002 | 1713 | 84 | 83 |
| Missing | 507 | 20 | --- |
| Primary caregiver-rated health 1997 | |||
| Excellent | 1237 | 49 | 49 |
| Very good | 814 | 32 | 32 |
| Good | 410 | 16 | 16 |
| Fair | 65 | 3 | 3 |
| Poor | 5 | <1 | <1 |
| Missing | 15 | <1 | --- |
| Primary caregiver-rated health 2002 | |||
| Excellent | 1090 | 53 | 47 |
| Very good | 653 | 32 | 32 |
| Good | 257 | 12 | 13 |
| Fair | 56 | 3 | 3 |
| Poor | 6 | <1 | 5 |
| Missing | 484 | 19 | --- |
| Self-rated health 2007 | |||
| Excellent | 464 | 25 | 25 |
| Very good | 725 | 39 | 32 |
| Good | 518 | 28 | 28 |
| Fair | 152 | 8 | 10 |
| Poor | 14 | 1 | 5 |
| Missing | 673 | 26 | --- |
| BMI percentile 1997 | 0–100 | 59 (0.78) | 59 (0.78) |
| <5 (underweight) | 271 | 12 | 13 |
| 5–84.9 (normal) | 1238 | 54 | 52 |
| 85–94.5 (overweight) | 325 | 14 | 14 |
| ≥95 (obese) | 459 | 20 | 21 |
| Missing | 253 | 10 | --- |
| BMI percentile 2002 | 0–100 | 66 (0.75) | 66 (0.79) |
| < 5 (underweight) | 49 | 3 | 5 |
| 5–84.9 (normal) | 1102 | 60 | 55 |
| 85–94.5 (overweight) | 288 | 16 | 17 |
| ≥95 (obese) | 399 | 22 | 23 |
| Missing | 708 | 28 | --- |
| BMI status 2007 (age < 21/age 21+) | |||
| < 5th percentile/<18.5 (underweight) | 60 | 3 | 5 |
| 5–84.9th percentile/18.5–24.9 (normal) | 1035 | 56 | 53 |
| 85–94.5th percentile/25–29.9 (overweight) | 394 | 21 | 22 |
| ≥ 95th percentile/≥ 30 (obese) | 347 | 19 | 20 |
| Missing | 710 | 28 | --- |
| Children's Depression Inventory 2002 (age 12+) | 0–18 | 3.0 (0.092) | 3.5 (1.27) |
| Missing | 566 | 22 | --- |
| Too young to be asked questionc | 725 | 28 | 21 |
| K-6 Non-Specific Psychological Distress Scale 2007 (age 18+) | 0–23 | 5.2 (0.11) | 5.2 (0.17) |
| Missing | 522 | 21 | --- |
| Too young to be asked questionc | 911 | 36 | 35 |
| Behavior Problems Index 1997 | 0–27 | 8.0 (0.13) | 8.0 (0.13) |
| Missing | 102 | 4 | --- |
| Behavior Problems Index 2002 | 0–30 | 8.7 (0.16) | 8.7 (0.15) |
| Missing | 509 | 20 | --- |
| Ever repeated a grade 1997 | 159 | 6 | 7 |
| Missing | 67 | 3 | --- |
| Changed school during current school year 1997 | 129 | 5 | 5 |
| Missing | 49 | 2 | --- |
| Changed school during current school year 2002 | 122 | 6 | 6 |
| Not in school | 29 | 1 | 8 |
| Missing | 513 | 20 | --- |
| Type of school 1997 | |||
| Public | 1867 | 90 | 81 |
| Private | 188 | 9 | 8 |
| Home | 17 | 1 | 11 |
| Missing | 474 | 19 | --- |
| Type of school 2002 | |||
| Public | 1784 | 91 | 78 |
| Private | 126 | 6 | 5 |
| Home | 28 | 1 | 9 |
| Not in school | 29 | 1 | 8 |
| Missing | 579 | 23 | --- |
| Academic achievement 1997 | 40.5–163.0 | 104.3 (0.42) | 104.4 (0.40) |
| Missing | 745 | 29 | --- |
| Academic achievement 2002 | 42.0–169.5 | 102.2 (0.42) | 101.9 (0.39) |
| Missing | 691 | 27 | --- |
| Mean academic achievement 1997–2002 | 42.0–169.5 | 103.1 (0.37) | 103.1 (0.36) |
| Missing | 316 | 12 | --- |
| Change in academic achievement 1997–2002 | −48.0–72.5 | −2.6 (0.35) | −2.5 (0.32) |
| Missing | 1120 | 44 | --- |
To facilitate comparison with the imputed sample, the denominators for percents for nonmissing categories include only observations with nonmissing information. To facilitate interpretation,denominators also exclude participants ineligible to be asked the question because of age.
Standard error of the mean.
Estimated from age in 1997 for participants missing from this wave
CONSTRUCTION OF TREATMENT WEIGHTS
To estimate the marginal structural models, each participant was assigned a treatment weight swi that was constructed using the equation:
where each term’s numerator f(A(t) = ai(t)|A(t − 1) = ai(t − 1), V = vi) is the probability density of participant i’s academic achievement score at time-point t, conditional on his or her history of academic achievement through time-point t − 1 (so A(1) was 1997 academic achievement and A(0) was set to zero) and values of time-invariant baseline covariates V. In the denominator, V is replaced by L(t), the history of both baseline and time-varying covariates through time t (V is included in L(1) [26, 35].
Included in V were sex, race, baseline age, perinatal health (whether the child was low birth weight [< 88 ounces] and the primary caregiver’s assessment of the child’s health at birth), an interviewer-assessed scale of cognitive stimulation and emotional support provided in the participant’s home at baseline (using selected items from Caldwell and Bradley’s Home Observation for the Measurement of The Environment [HOME] scale) [46], whether the participant had ever repeated a grade in school, and the primary caregiver’s achievement score. In addition, the following variables with time-varying information but very high correlation or agreement between 1997 and 2002 were treated as time invariant and therefore also included in V: the maximum of the child’s caregivers’ years of schooling, geographical region, and urbanicity. In addition to the variables included in V, L(t) also included time-varying information on family income (measured as a family income-to-poverty-level ratio in which the annual household income was divided by the corresponding annual U.S. Census Bureau poverty threshold, which takes into account family size and the ages of family members [47]), whether the child lived with two parent figures, a caregiver-rated measure of how good a place the neighborhood where the family resided was to raise children, health (global health status, body mass index [BMI], number of overnight hospital stays), whether the child had a routine physician check-up in the previous two years, a scale of the caregiver’s report of problem behaviors (including both aggressive and withdrawn or sad behaviors), school type (public, private, home, not in school), and whether the child changed schools during the current school year. In models of psychological distress, the log of the 2002 CDI score was additionally included as a time-dependent confounder. Since academic achievement was a normally distributed continuous measure, the conditional numerator and denominator probability densities were estimated using linear regression and the normal probability density function [26, 34].
In order to produce a reasonable distribution of weights for the MSMs of global health status and BMI, (i.e., mean approximately 1 and reasonable range), we trimmed the weights separately for each imputation at their 3rd-highest and 3rd-lowest values, resulting in a total range of 0.07–32.97 and imputation-specific means ranging 1.00–1.05. Because the distribution of weights for the psychological distress models was more unstable, we trimmed them at the 1st and 99th percentiles, resulting in imputation-specific means ranging 0.99–1.01 and a total range 0.25–2.73. Further trimming the weights produced nearly identical estimates.
Table A3.
Tests of preconditions for the outcome of 2007 poorer self-rated health status
| Precondition | In This Case | Tests | Conclusions |
|---|---|---|---|
| Key time-varying covariates predict exposure | Does health predict academic achievement? | Adjusted linear regression of 1997 academic achievement on perinatal health (low birth weight, spent time in NICU, caregiver-rated health compared to other babies) & 1997 health (caregiver-rated health status, nights spent in hospital birth-1997). | In general, poorer health predicts lower academic achievement. For 1997 achievement, point estimates are driven by NICU and are stronger for perinatal health than 1997 health. For 2002 achievement, perinatal health is stronger predictor than 1997 or 2002 health. |
| Adjusted linear regression of 2002 academic achievement on perinatal health, 1997 health, and 2002 health (caregiver-rated health status, nights spent in hospital 1997- 2002). | |||
| Exposure predicts key time-varying covariates | Does academic achievement predict future health? | Adjusted logistic regression of 2002 poorer caregiver-rated health status on 1997 academic achievement. | In general, higher academic achievement predicts lower odds of poorer health. Stronger evidence for 2007 self-rated health status than 2002 caregiverrated health status. |
| Adjusted logistic regression of 2007 poorer self-rated health status on 1997 and 2002 academic achievement. | |||
| Key time-varying covariates predict outcome independent of exposure | Does past health predict 2007 health independent of academic achievement? | Adjusted logistic regression of 2007 poorer self-rated health status on perinatal, 1997, and 2002 health measures, with average 1997–2002 academic achievement included as a covariate | Poorer previous health weakly predicts 2007 poorer self-rated health independent of academic achievement. |
| Exposure and key time-varying covariates vary over time | Do academic achievement and health vary over time? | Correlation between 1997 and 2002 academic achievement. | Academic achievement and health status do vary over time. |
| Agreement between 1997, 2002, and 2007 poorer health status measures. |
Figure A1. Empirical support for hypothesized causal paths linking academic achievement and health status
Results are from tests described in Table A3 and describe the direction and strength of associations. Parentheses indicate weak associations.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Félice Lê-Scherban, Department of Epidemiology, University of Michigan.
Ana V. Diez Roux, Department of Epidemiology, University of Michigan.
Yun Li, Department of Biostatistics, University of Michigan.
Hal Morgenstern, Departments of Epidemiology and Environmental Health Sciences, University of Michigan.
REFERENCES
- 1.Julian T, Kominski R. Educational Resources Information Center (U.S.), US Census Bureau. Education and Synthetic Work-Life Earnings Estimates. American Community Survey Reports. ACS-14 [Numeric (Numerical Quantitative Data) Text (Reports, Research)]. [S.l.]: Distributed by ERIC Clearinghouse. 2011 Available from: http://www.eric.ed.gov/contentdelivery/servlet/ERICServlet?accno=ED523770.
- 2.Kawachi I, Adler NE, Dow WH. Money, schooling, and health: mechanisms and causal evidence. Ann N Y Acad Sci. 2010 Feb;1186:56–68. doi: 10.1111/j.1749-6632.2009.05340.x. PubMed PMID: 20201868. Epub 2010/03/06. eng. [DOI] [PubMed] [Google Scholar]
- 3.Cutler DM, Lleras-Muney A. Education and Health: Evaluating Theories and Evidence. Cambridge, MA: National Bureau of Economic Research; 2006. Jun, Report No.: Contract No.: 12352. [Google Scholar]
- 4.Grossman M. On the concept of health capital and the demand for health. The Journal of Political Economy. 1972;80(2):223–255. [Google Scholar]
- 5.Cutler DM, Lleras-Muney A. Understanding differences in health behaviors by education. Journal of Health Economics. 2010;29:1–28. doi: 10.1016/j.jhealeco.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ross CE, Wu C-L. The links between education and health. Am Sociol Rev. 1995;60(5):719–745. [Google Scholar]
- 7.Feinstein L, Sabates R, Anderson TM, Sorhaindo A, Hammond C. What are the effects of education on health? In: Desjardins R, Schuller T, editors. Measuring the Effects of Education on Health and Civic Engagement: Proceedings of the Copenhagen Symposium. Copenhagen: Organisation for Economic Co-operation and Development; 2006. pp. 171–353. [Google Scholar]
- 8.Brolin Laftman S, Modin B. School-performance indicators and subjective health complaints: are there gender differences? Sociology of health & illness. 2012 May;34(4):608–625. doi: 10.1111/j.1467-9566.2011.01395.x. PubMed PMID: 22103817. [DOI] [PubMed] [Google Scholar]
- 9.Crosnoe R, Muller C. Body mass index, academic achievement, and school context: examining the educational experiences of adolescents at risk of obesity. J Health Soc Behav. 2004 Dec;45(4):393–407. doi: 10.1177/002214650404500403. PubMed PMID: 15869112. Epub 2005/05/05. eng. [DOI] [PubMed] [Google Scholar]
- 10.Crosnoe R, Riegle-Crumb C. A life course model of education and alcohol use. J Health Soc Behav. 2007 Sep;48(3):267–282. doi: 10.1177/002214650704800305. PubMed PMID: 17982868. Pubmed Central PMCID: 2843392. Epub 2007/11/07. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eide ER, Showalter MH, Goldhaber DD. The relation between children's health and academic achievement. Children and Youth Services Review. 2010;32:231–238. [Google Scholar]
- 12.Florin TA, Shults J, Stettler N. Perception of overweight is associated with poor academic performance in US adolescents. J Sch Health. 2011 Nov;81(11):663–670. doi: 10.1111/j.1746-1561.2011.00642.x. PubMed PMID: 21972986. [DOI] [PubMed] [Google Scholar]
- 13.Frojd SA, Nissinen ES, Pelkonen MU, Marttunen MJ, Koivisto AM, Kaltiala-Heino R. Depression and school performance in middle adolescent boys and girls. Journal of adolescence. 2008 Aug;31(4):485–498. doi: 10.1016/j.adolescence.2007.08.006. PubMed PMID: 17949806. [DOI] [PubMed] [Google Scholar]
- 14.Piko BF. Self-perceived health among adolescents: the role of gender and psychosocial factors. European journal of pediatrics. 2007 Jul;166(7):701–708. doi: 10.1007/s00431-006-0311-0. PubMed PMID: 17120041. [DOI] [PubMed] [Google Scholar]
- 15.Tucker JS, Martinez JF, Ellickson PL, Edelen MO. Temporal associations of cigarette smoking with social influences, academic performance, and delinquency: a four-wave longitudinal study from ages 13–23. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors. 2008 Mar;22(1):1–11. doi: 10.1037/0893-164X.22.1.1. PubMed PMID: 18298226. [DOI] [PubMed] [Google Scholar]
- 16.Undheim AM, Sund AM. School factors and the emergence of depressive symptoms among young Norwegian adolescents. European child & adolescent psychiatry. 2005 Dec;14(8):446–453. doi: 10.1007/s00787-005-0496-1. PubMed PMID: 16341501. [DOI] [PubMed] [Google Scholar]
- 17.Power C, Matthews S, Manor O. Inequalities in self-rated health: explanations from different stages of life. Lancet. 1998 Apr 4;351(9108):1009–1014. doi: 10.1016/S0140-6736(97)11082-0. PubMed PMID: 9546506. [DOI] [PubMed] [Google Scholar]
- 18.Crosnoe R, Elder GH., Jr Life course transitions, the generational stake, and grandparent-grandchild relationships. Journal of Marriage and Family. 2002;64(4):1089–1096. [Google Scholar]
- 19.Bauldry S, Shanahan MJ, Boardman JD, Miech RA, Macmillan R. A life course model of self-rated health through adolescence and young adulthood. Soc Sci Med. 2012 Oct;75(7):1311–1320. doi: 10.1016/j.socscimed.2012.05.017. PubMed PMID: 22726620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Breidablik HJ, Meland E, Lydersen S. Self-rated health during adolescence: stability and predictors of change (Young-HUNT study, Norway) Eur J Public Health. 2009 Jan;19(1):73–78. doi: 10.1093/eurpub/ckn111. PubMed PMID: 19022851. Pubmed Central PMCID: 2639013. Epub 2008/11/22. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fosse NE, Haas SA. Validity and stability of self-reported health among adolescents in a longitudinal, nationally representative survey. Pediatrics. 2009 Mar;123(3):e496–e501. doi: 10.1542/peds.2008-1552. PubMed PMID: 19254984. Epub 2009/03/04. eng. [DOI] [PubMed] [Google Scholar]
- 22.Vingilis ER, Wade TJ, Seeley JS. Predictors of adolescent self-rated health. Analysis of the National Population Health Survey. Can J Public Health. 2002 May-Jun;93(3):193–197. doi: 10.1007/BF03404999. PubMed PMID: 12050986. Epub 2002/06/08. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fowler MG, Johnson MP, Atkinson SS. School achievement and absence in children with chronic health conditions. J Pediatr. 1985 Apr;106(4):683–687. doi: 10.1016/s0022-3476(85)80103-7. PubMed PMID: 3981326. Epub 1985/04/01. eng. [DOI] [PubMed] [Google Scholar]
- 24.Taras H, Potts-Datema W. Chronic health conditions and student performance at school. J Sch Health. 2005 Sep;75(7):255–266. doi: 10.1111/j.1746-1561.2005.00034.x. PubMed PMID: 16102088. Epub 2005/08/17. eng. [DOI] [PubMed] [Google Scholar]
- 25.Jackson MI. Understanding links between adolescent health and educational attainment. Demography. 2009 Nov;46(4):671–694. doi: 10.1353/dem.0.0078. PubMed PMID: 20084824. Pubmed Central PMCID: 2831357. Epub 2010/01/21. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000 Sep;11(5):550–560. doi: 10.1097/00001648-200009000-00011. PubMed PMID: 10955408. Epub 2000/08/24. eng. [DOI] [PubMed] [Google Scholar]
- 27.The Panel Study of Income Dynamics [Internet] University of Michigan. [cited 2011]. Available from: http://psidonline.isr.umich.edu/default.aspx.
- 28.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002 Aug;32(6):959–976. doi: 10.1017/s0033291702006074. PubMed PMID: 12214795. Epub 2002/09/07. eng. [DOI] [PubMed] [Google Scholar]
- 29.Institute for Social Research. The Panel Study of Income Dynamics Child Development Supplement: User Guide for CDS-II. Ann Arbor, MI: Institute for Social Research, Survey Research Center, University of Michigan; 2010. Jul 30, Report No. [Google Scholar]
- 30.Dean RS, Woodcock RW. The WJ-R and Bateria-R in Neuropsychological Assessment: Report Number 3. Rolling Meadows, IL: Riverside Publishing; 1999. Contract No. 3. [Google Scholar]
- 31.Raghunathan TE, Lepkowski J, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology. 2001 Jun;27(1):85–95. [Google Scholar]
- 32.Institute for Social Research. IVEware: Imputation and Variance Estimation Software. Ann Arbor, MI: University of Michigan; 2002. [updated October 11, 2011; cited 2011 December 8]. Available from: http://www.isr.umich.edu/src/smp/ive/. [Google Scholar]
- 33.Spratt M, Carpenter J, Sterne JA, Carlin JB, Heron J, Henderson J, et al. Strategies for multiple imputation in longitudinal studies. Am J Epidemiol. 2010 Aug 15;172(4):478–487. doi: 10.1093/aje/kwq137. PubMed PMID: 20616200. Epub 2010/07/10. eng. [DOI] [PubMed] [Google Scholar]
- 34.Cerda M, Diez-Roux AV, Tchetgen ET, Gordon-Larsen P, Kiefe C. The relationship between neighborhood poverty and alcohol use: estimation by marginal structural models. Epidemiology. Jul;21(4):482–489. doi: 10.1097/EDE.0b013e3181e13539. PubMed PMID: 20498603. Epub 2010/05/26. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hernan MA, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology. 2000 Sep;11(5):561–570. doi: 10.1097/00001648-200009000-00012. PubMed PMID: 10955409. Epub 2000/08/24. eng. [DOI] [PubMed] [Google Scholar]
- 36.Zou G, Donner A. Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat Methods Med Res. 2011;0(0) doi: 10.1177/0962280211427759. Epub November 8, 2011. [DOI] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention. A SAS Program for the CDC Growth Charts. Atlanta, GA: Centers for Disease Control and Prevention; 2011. [updated June 27, 2011; cited 2012 August 1]. Available from: http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. [Google Scholar]
- 38.Ross CE, Masters RK, Hummer RA. Education and the gender gaps in health and mortality. Demography. 2012 Nov;49(4):1157–1183. doi: 10.1007/s13524-012-0130-z. PubMed PMID: 22886759. Pubmed Central PMCID: 3496041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu H, Hummer RA. Are educational differences in U.S. self-rated health increasing?: an examination by gender and race. Soc Sci Med. 2008 Dec;67(11):1898–1906. doi: 10.1016/j.socscimed.2008.09.021. PubMed PMID: 18930339. Pubmed Central PMCID: 2656569. Epub 2008/10/22. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Benyamini Y, Leventhal EA, Leventhal H. Gender differences in processing information for making self-assessments of health. Psychosom Med. 2000 May-Jun;62(3):354–364. doi: 10.1097/00006842-200005000-00009. PubMed PMID: 10845349. [DOI] [PubMed] [Google Scholar]
- 41.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- 42.Idler EL, Kasl SV. Self-ratings of health: do they also predict change in functional ability? J Gerontol B Psychol Sci Soc Sci. 1995 Nov;50(6):S344–S353. doi: 10.1093/geronb/50b.6.s344. PubMed PMID: 7583813. Epub 1995/11/01. eng. [DOI] [PubMed] [Google Scholar]
- 43.Zajacova A, Dowd JB. Reliability of self-rated health in US adults. Am J Epidemiol. 2011 Oct 15;174(8):977–83. doi: 10.1093/aje/kwr204. PubMed PMID: 21890836. Pubmed Central PMCID: 3218632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dowd J, Zajacova A. Does the predictive power of self-rated health for subsequent mortality risk vary by socioeconomic status in the US? Int J Epidemiol. 2007;36:1214–1221. doi: 10.1093/ije/dym214. [DOI] [PubMed] [Google Scholar]
- 45.Boardman JD. Self-rated health among U.S. adolescents. J Adolesc Health. 2006 Apr;38(4):401–408. doi: 10.1016/j.jadohealth.2005.01.006. PubMed PMID: 16549301. Epub 2006/03/22. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baker PC, Keck CK, Mott FL, Quinlan SV. NLSY Child Handbook: A Guide to the 1986–1990 National Longitudinal Survey of Youth Child Data. Revised Edition. Columbus, OH: Center for Human Resource Research, The Ohio State University; 1993. Oct, Report No. [Google Scholar]
- 47.Grieger LD, Schoeni RF, Danziger S. Accurately measuring the trend in poverty in the United States using the Panel Study of Income Dynamics. Ann Arbor, MI: Institute for Social Research; 2008. Contract No.: 08-04. [Google Scholar]