Abstract
Venocaval anomalies are uncommon in the general population and often go unrecognized, but physicians should be aware of their significance. Duplicate superior vena cava should be identified during cardiac imaging, surgery, and catheter insertions. While interrupted inferior vena cava can predispose to thrombus formation, they protect against pulmonary embolism from lower extremity deep vein thrombosis. We describe a unique case of a patient in which combined superior vena cava and inferior vena cava anomalies were found incidentally. This is the first reported case of a duplicate superior vena cava and interrupted inferior vena cava in a single patient in English literature. This article also provides a literature review on the topic.
Keywords: Venocaval anomaly, vena cava embryology, duplicate SVC, interrupted IVC
CASE REPORT
Imaging Findings
A 49 year old man presented initially with a testicular mass. A workup revealed metastatic testicular tumor. For chemotherapy access, a tunneled catheter with a subcutaneous port was placed and a chest x-ray following placement revealed the catheter tracing from the left internal jugular vein through a suspected left superior vena cava (SVC) (Figure 1). A non-contrast CT scan, performed during the workup of the testicular mass, confirmed the presence of duplicate superior vena cava (Figure 2). He had no known cardiac or vascular anomalies before this presentation.
Figure 1.
49 year old male with a duplicate SVC and interrupted IVC. FINDINGS: Portable AP chest X-ray after PORT-A-CATH placement in left internal jugular vein demonstrates catheter positioned in left superior vena cava (arrow). TECHNIQUE: GE Portable machine kVp 85, mAs 8, 72 inches distance from the patient.
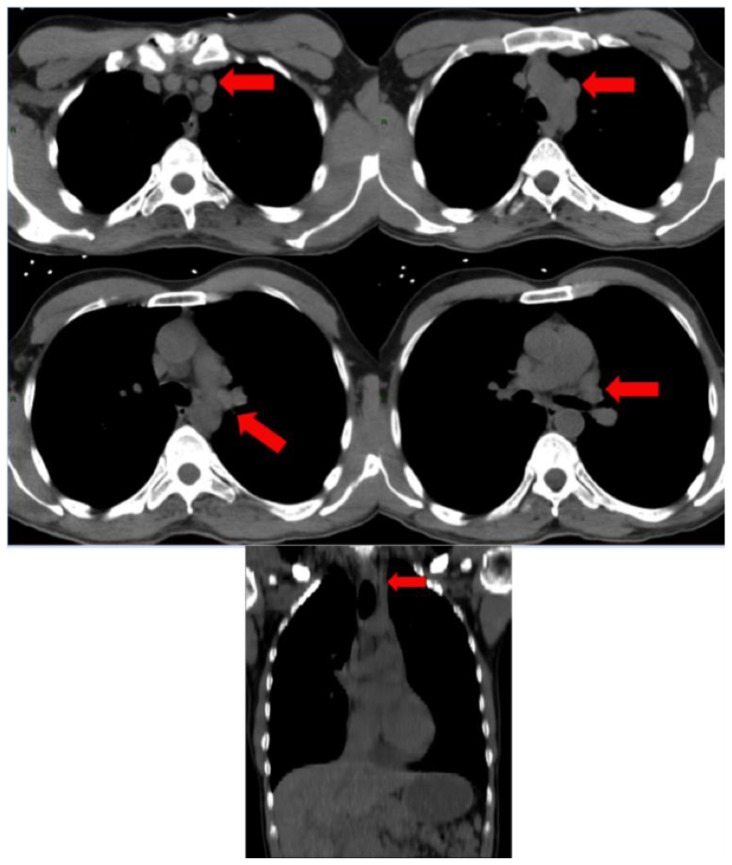
Figure 2.
49 year old male with a duplicate SVC and interrupted IVC. FINDINGS: (A–E) CT scan of the chest without PO or IV contrast. This series shows the formation of the left brachiocephalic vein, which remains separate from the right brachiocephalic vein at the level of the aortic arch. The left brachiocephalic vein continues as a separate left superior vena cava (arrows) inferiorly alongside the left side of the heart. The drainage path of the left superior vena cava cannot be confirmed, as this scan did not use IV contrast. Analyzing the anatomy of the great vessels was not the intent of performing this scan. (F) This coronal reconstruction of the above CT scan shows the presence of a persistent left superior vena cava (arrow). TECHNIQUE: Computer tomography of the chest was performed without intravenous or oral contrast using Philips Briliance 64 CT machine (Cleveland, OH) with slice thickness 5mm 120 kVp, 106–228 mAs.
During the same hospital admission the patient was found to have lower extremity swelling suspicious of deep vein thrombosis (DVT) (Figure 3). The patient underwent venous duplex ultrasound of the left leg that revealed an acute DVT in the left common iliac, external iliac, left common femoral and left deep femoral veins.
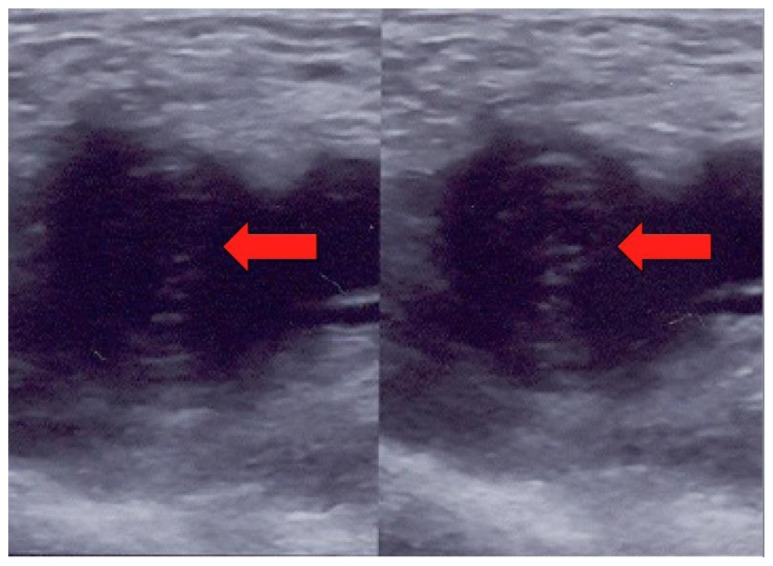
Figure 3.
49 year old man with duplicate SVC, interrupted IVC and lower extremity DVT. FINDINGS: Compression ultrasound images of the left lower extremity show a thrombus (arrows) in the left common femoral vein (left) that is non-compressible upon pressure (right). TECHNIQUE: GE LOGIQ 5 ultrasound machine with normal pressure (right) and attempted compressed (left).
Management
Due to the size of the thrombus and concern of potential future pulmonary embolism (PE), inferior vena cava (IVC) filter placement was attempted; however, the patient was found to have IVC interruption which was confirmed by venogram (Figure 4).
Figure 4.
49 year old male with a duplicate SVC and interrupted IVC. FINDINGS: Venogram performed during IVC filter placement showing interrupted IVC. Injection of the contrast showed a 3 cm segment of interruption in the inferior vena cava with numerous large collaterals formed in lieu of a continuous IVC. TECHNIQUE: Omnipaque 140 – 50 ml was used for venogram.
Follow-up
As duplicated SVCs are benign and an interrupted IVC is natural protection against PE, no further treatment was needed.
DISCUSSION
Introduction
Anomalies of the great vessels are not uncommon in the general population and can have significant implications during diagnostic evaluation and surgery. We presented a unique case of combined IVC and SVC anomalies in one patient. This case report described a patient with a duplicate superior vena cava and an interrupted IVC, both discovered incidentally. To our knowledge this is the first reported case in English literature of a duplicate SVC and interrupted IVC in a single patient.
Etiology and Demographics
Duplicate left superior vena cava have an incidence of 0.3% in the general population and 10% in patients with congenital heart disease [1]. Inferior vena cava interruption is a relatively uncommon anomaly. However, because this anomaly was previously discovered on autopsy and is now being discovered through radiologic imaging, there is not a clear consensus on its incidence [2]. Although the incidence is unclear, many studies cite an increased incidence with cardiac comorbidities.
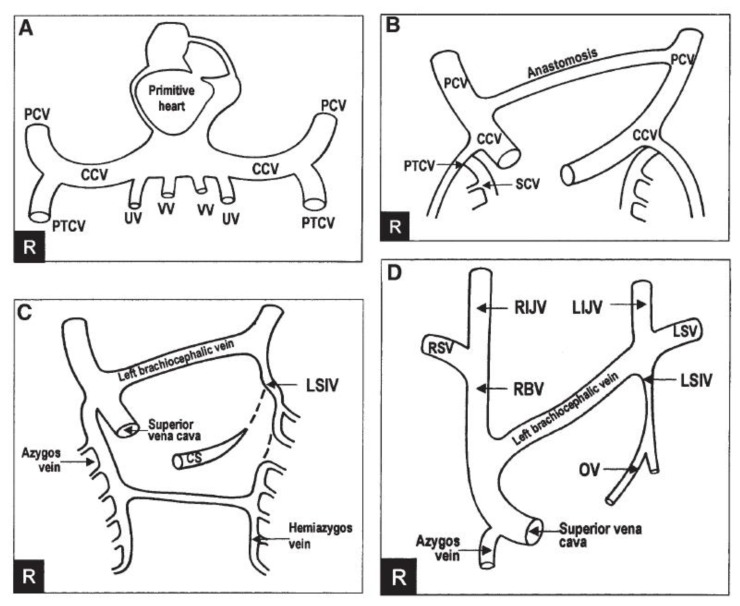
Embryologically, the right SVC originates from the junction of the right precardinal vein and the right common cardinal vein. An oblique anastomosis develops, connecting with the precardinal veins to become the left brachiocephalic vein (Figure 5). Typically, the left precardinal vein and the left common cardinal vein undergo atrophy [3, 4]. In patients with duplicate SVC, this atrophy does not occur and the left SVC remains patent, usually draining into the coronary sinus and then into the right atrium. In approximately 10% of patients the left duplicate SVC attaches to the left atrium and may cause hemodynamic compromise [5, 6, 7].
Figure 5.
Diagram illustrating normal SVC embryogenesis. (A) Initial presence of common cardinal veins. (B) Anastomosis forms creating the (C) left brachiocephalic vein. (D) Left common cardinal vein undergoes atrophy to form normal adult vasculature. CCV: common cardinal vein, CS: coronary sinus, LIJV: left internal jugular vein, LSIV: left superior intercostal vein, LSV: left subclavian vein, OV: oblique vein of the left atrium, PCV: precardinal vein, PTCV: postcardinal vein, RBV: right brachiocephalic vein, RIJV: right internal jugular vein, RSV: right subclavian vein, SCV: supracardinal vein, UV: umbilical vein, VV: vitelline vein. Image reproduced with permission from ref [4].
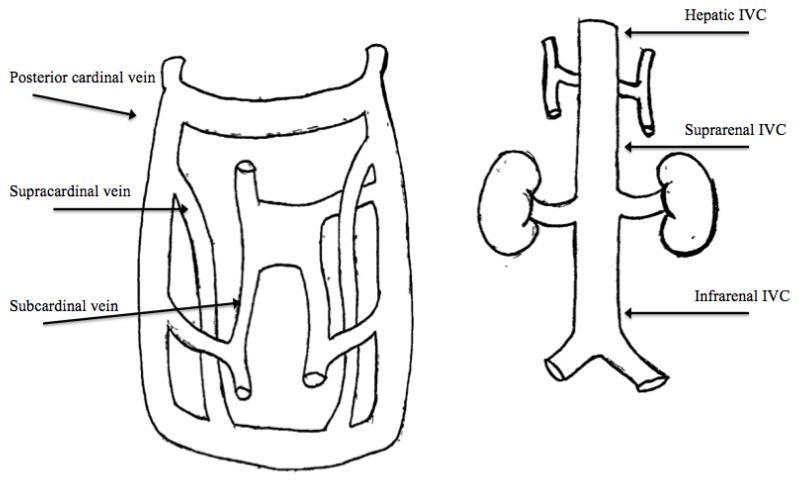
The IVC is formed embryologically from the formation, regression, and then fusion of three pairs of veins: the supracardinal, subcardinal and posterior cardinal veins (figure 6) [8, 9].
Figure 6.
Diagram illustrating normal IVC embryogenesis. (A) Development of IVC at 6–8 weeks. (B) Normal adult IVC anatomy after fusion of the supracardinal, subcardinal and posterior cardinal veins. IVC: Inferior vena cava. Illustrations by Stephanie L. Clymer, B.A.
Clinical and Imaging Findings
SVC is rarely symptomatic in patients without congenital heart disease, however during cardiac catheterization, angiography, echocardiography, and open heart surgery, it is important to be aware of anomalies of the great thoracic veins, including duplicate SVC [10]. SVC can be suspected on chest x-ray if a catheter or line is in the left paramediastinal area and can be diagnosed on CT scan by tracking the anomalous vessel from the left jugular and subclavian veins to the coronary sinus (figures 1, 2).
The complex development of the IVC lends itself to the formation of anomalies. In IVC interruption, lower extremity venous drainage occurs through collaterals developed in lieu of a continuous IVC. This can readily be seen on venogram (figure 4). IVC interruption is clinically relevant. Studies show that IVC interruption can predispose to the development of lower extremity DVTs; however it is protective against pulmonary emboli as the thrombus is unable to reach the lung and remains lodged in the interrupted segment of IVC. It is possible, however rare, to develop a pulmonary embolism from the upper extremity or jugular veins through the SVC [11, 12, 13, 14].
Treatment and Prognosis
In the absence of congenital heart disease, duplicate SVC is benign and no treatment is necessary. Thus, the prognosis is excellent. As interrupted IVC is protective against pulmonary emboli, no treatment is necessary and the prognosis is also excellent [15].
Differential Diagnoses
On chest x-ray, the differential diagnosis of a left paramediastinal catheter includes a duplicate left superior vena cava and location of the catheter in the left internal mammary vein, left superior intercostal vein or left pericardiophrenic vein. The diagnosis can be confirmed by CT scan by tracking the anomalous vessel from the left jugular and subclavian veins to the coronary sinus.
Differential diagnosis of an interrupted IVC as seen on venogram includes an acute obstruction of the IVC, such as a thrombosis, and congenital interruption. Congenital interruptions will have collateral formation joining the inferior and superior segments of the IVC while acute obstruction will not have collaterals.
TEACHING POINT
Venocaval anomalies are uncommon in the general population and often go unrecognized, but physicians should be aware of their significance. Duplicate SVC should be identified during cardiac imaging, surgery, and catheter insertions and while interrupted inferior vena cava can predispose to thrombus formation, they protect against pulmonary embolism from lower extremity deep vein thrombosis.
Table 1.
Summary table of key findings in both duplicate SVC and interrupted IVC
| Duplicate Superior Vena Cava (SVC) | Interrupted Inferior Vena Cava (IVC) | |
|---|---|---|
| Etiology | Absence of atrophy of left common cardinal vein | Alteration in the formation, regression and fusion of the supracardinal, subcardinal and posterior cardinal veins |
| Incidence |
|
|
| Gender Ratio | Unknown | Unknown |
| Age predilection | Congenital | Congenital |
| Risk Factors | Congenital heart disease | Unknown |
| Treatment | None necessary | None necessary |
| Prognosis | Excellent | Excellent |
| Findings on Imaging | Chest X-ray: suspected when catheter or line is in the left paramediastinal area Computed tomography scan: Anomalous vessel tracks from the left jugular and subclavian veins to the coronary sinus | Venogram: Interruption of IVC and presence of large collaterals connecting inferior and superior IVC portions |
Table 2.
Differential diagnosis table of a left paramediastinal catheter on chest X-ray
| Chest X-ray | Computed Tomography Scan | |
|---|---|---|
| Duplicate Superior Vena Cava | Left paramediastinal catheter | Anomalous vessel tracks from the left jugular and subclavian veins to the coronary sinus |
| Catheter in left internal mammary vein | Left paramediastinal catheter | Catheter visualized in left internal mammary vein |
| Catheter in left superior intercostal vein | Left paramediastinal catheter | Catheter visualized in left superior intercostal vein |
| Catheter in left pericardiophrenic vein | Left paramediastinal catheter | Catheter visualized in left pericardiophrenic vein |
Table 3.
Differential Diagnosis table of IVC interruption
| Venogram | |
|---|---|
| Congenital or chronic interrupted IVC | Discontinuous IVC with the formation of collaterals |
| Acute IVC obstruction | Discontinuous IVC with no collateral formation |
ACKNOWLEDGEMENTS
The authors would like to thank Dr. Bhugwan Singh for permission to use his diagram and Stephanie L. Clymer, B.A. for her illustrations.
ABBREVIATIONS
- CT
Computed Tomography
- DVT
Deep Vein Thrombosis
- IVC
Inferior Vena Cava
- SVC
Superior Vena Cava
REFERENCES
- 1.Iimura A, Oguchi T, Shibata M, Matsuo M, Takahashi T. Double superior vena cava and anomaly of cardiovascular system with a review of the literature. Okajimas Folia Anatomica Japonica. 2011 May;88(1):37–42. doi: 10.2535/ofaj.88.37. [DOI] [PubMed] [Google Scholar]
- 2.Nichols JL, Gonzalez SC, Bellino PJ, Bieber EJ. Venous thrombosis and congenital absence of inferior vena cava in a patient with menorrhagia and pelvic pain. Journal Pediatric Adolescent Gynecology. 2010 Feb;23(1):e17–21. doi: 10.1016/j.jpag.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 3.Melluso C, Raffa S, Di Bella G, et al. Double superior and inferior vena cava: unusual venous anomaly. Journal of Cardiovascular Medicine. 2008 Mar;9(3):289–92. doi: 10.2459/JCM.0b013e3282058bcd. [DOI] [PubMed] [Google Scholar]
- 4.Singh B, Ramsaroop L, Maharaj J, Reddi A. Case of Double Superior Vena Cava. Clinical Anatomy. 2005;18:366–369. doi: 10.1002/ca.20116. [DOI] [PubMed] [Google Scholar]
- 5.Arslan G, Ozkaynak C, Cubuk M, Sindel T, Luleci E. Absence of the azygous vein associated with double superior vena cava. The Journal of Vascular Diseases. 1999 Jan;50(1):81–4. doi: 10.1177/000331979905000111. [DOI] [PubMed] [Google Scholar]
- 6.Albay S, Cankal F, Kocabiyik N, Yalcin B, Ozan H. Double superior vena cava. Morphologie. 2006 Mar;288:39–42. doi: 10.1016/s1286-0115(06)74317-x. [DOI] [PubMed] [Google Scholar]
- 7.Freedom RM, Culham JAG, Moes CAF. Angiography of Congenital Heart Disease. New York: Macmillan; 1984. [Google Scholar]
- 8.Gayer G, Luboshitz J, Hertz M, et al. Congenital anomalies of the inferior vena cava revealed on CT in patients with deep vein thrombosis. American Journal of Roentgenology. 2003 Mar;180(3):729–32. doi: 10.2214/ajr.180.3.1800729. [DOI] [PubMed] [Google Scholar]
- 9.Malaki M, Willis AP, Jones RG. Congenital anomalies of the inferior vena cava. Clinical Radiology. 2012 Feb;67(3):165–171. doi: 10.1016/j.crad.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Ying Z, Ma J, Geng X, Chen M. Double superior vena cava with a persistent left superior vena cava. Internal Medicine. 2008:679–680. doi: 10.2169/internalmedicine.47.0840. [DOI] [PubMed] [Google Scholar]
- 11.Baeshko A, Zhuk G, Orlovskii I, et al. Congenital anomalies of the inferior vena cava: diagnosis and medical treatment. Angiology and Vascular Surgery. 2007;13(1):91–5. [PubMed] [Google Scholar]
- 12.Bass J, Redwine M, Kramer L, Huynh P, Harris J. Spectrum of congenital anomalies of the inferior vena cava: cross-sectional imaging findings. Radiographics. 2000 May-Jun;20(3):639–52. doi: 10.1148/radiographics.20.3.g00ma09639. [DOI] [PubMed] [Google Scholar]
- 13.Vucicevic Z, Degoricija V, Alfirevic Z, Sharma M. Inferior vena cava agenesia and a massive bilateral iliofemoral venous thrombosis. Angiology. 2008 Aug-Sep;59(4):510–3. doi: 10.1177/0003319707305350. [DOI] [PubMed] [Google Scholar]
- 14.Lambert M, Marboeuf P, Midulla M, et al. Inferior vena cava agenesis and deep vein thrombosis: 10 patients and review of the literature. Vascular Medicine. 2010 Dec;15(6):451–459. doi: 10.1177/1358863X10391355. [DOI] [PubMed] [Google Scholar]
- 15.Broshtein M, Khatib N, Blemfeld Z. Prenatal diagnosis and outcome of isolated interrupted inferior vena cava. American Journal of Obstetrics and Gynecology. 2010 Apr;202(4):398. doi: 10.1016/j.ajog.2009.11.014. [DOI] [PubMed] [Google Scholar]