Abstract
Sigmoid volvulus complicating pregnancy is a rare, non-obstetric cause of abdominal pain that requires prompt surgical intervention (decompression) to avoid intestinal ischemia and perforation. We report the case of a 31-week pregnant woman with abdominal pain and subsequent development of constipation. Preoperative diagnosis was achieved using magnetic resonance imaging and ultrasonography: the large bowel distension and a typical whirl sign - near a sigmoid colon transition point - suggested the diagnosis of sigmoid volvulus. The decision to refer the patient for emergency laparotomy was adopted without any ionizing radiation exposure, and the pre-operative diagnosis was confirmed after surgery. Imaging features of sigmoid volvulus and differential diagnosis from other non-obstetric abdominal emergencies in pregnancy are discussed in our report, with special emphasis on the diagnostic capabilities of ultrasonography and magnetic resonance imaging.
Keywords: Volvulus, Pregnancy Complications, Intestinal Diseases, Magnetic Resonance Imaging, Ultrasonography
CASE REPORT
A thirty-one-year-old woman, at 31 weeks’ gestation of her first pregnancy, was admitted to the obstetrics and gynecology unit of our hospital with a three-day history of intermittent lower abdominal pain. She did not report previous medical disease or abdominal surgery; her pregnancy has been uncomplicated thus far. At clinical presentation she had no fever; vital signs were normal. Physical examination showed a diffused tenderness to deep palpation, with distended and painful abdomen; there was no guarding.
Cardiotocography did not show signs of fetal distress, and gynecological examination was not suggestive of threatened preterm labor. Hematological and biochemical tests were unremarkable within normal limits except for neutrophilic predominance (82.8%; normal: 40.0%–74.0%) - with normal white cell count (9.3×10^3 mm3; normal: 4.80–10.80 ×10^3 mm3) - and mildly increased C-reactive protein of 1.64 mg/dl (normal: 0.10–0.80 mg/dl) and Lactate dehydrogenase of 523 U/L (normal: 250–500 U/L); liver function tests, platelet count and urinalysis were normal.
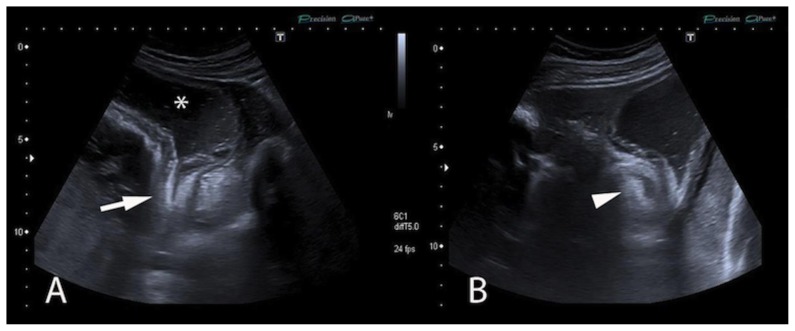
An abdominal US exam was carried out in order to exclude gallstone or kidney disease, revealing only moderate right pelvocaliceal dilatation and small amount of perisplenic fluid (Figure 1). The patient was hospitalized for observation and received conservative analgesic treatment. Nonetheless, in the following 24–48 hours, meteoric distension and abdominal pain worsened with onset of constipation: these clinical signs suggested a bowel obstruction.
Figure 1.
A thirty-one-year-old pregnant woman (31 weeks gestation) with sigmoid volvulus. FINDINGS: US exam shows only mild right pelvocaliceal dilatation (Figure 1A, white arrows) and very small amount of perisplenic fluid (Figure 1B, white arrow). TECHNIQUE: Right and left sagittal scan planes of transabdominal ultrasound (respectively Figures A and B). Ultrasonography was performed using a 3.5 Mhz convex transducer; grayscale images were acquired - Figures A and B (courtesy of Dr. Maria Coronella, Radiodiagnostic and Oncological Radiotherapy Unit, University Hospital “Policlinico-Vittorio Emanuele”, Catania)
In view of the pregnant state, a diagnostic protocol free of ionizing radiation was adopted, and the patient was referred to MRI, to better investigate the clinical suspicion of bowel disease.
MRI and US Findings
The MRI was performed using a 1.5 Tesla scanner (General Electric, Signa HDxt, Milwaukee, USA); unenhanced images were acquired with an eight-channel phased-array coil. Multiplanar single-shot fast spin-echo (SSFSE), steady-state free-precession (SSFP) and three-dimensional fast spoiled gradient echo (3D FSPGR) images showed tortuous, markedly dilated colic loops, extended in the upper and lower abdomen.
Coronal SSFP and SSFSE images identified a distended ahaustral sigmoid loop, with an inverted “U configuration”, extended up to the left hemidiaphragm; transverse colon was dilated and displaced to the right side by the U-loop described. On both axial and coronal images, the “U-shaped” colonic loop could be seen, reaching a sigmoid transition point in the left iliac region (Figures 2–5), where a soft-tissue mass with a swirling internal architecture was identified, showing a “whirl sign” (Figures 4–5). The T2-weighted acquisitions showed a diffused mural thickening of the sigma upstream to the transition point - due to edematous imbibition; intestinal downstream segment was collapsed. A new US exam was performed after the MRI acquisition, and confirmed the marked dilatation of the colonic loop and the “whirl sign” in the left iliac region.
Figure 2.
A thirty-one-year-old pregnant woman (31 weeks gestation) with sigmoid volvulus. FINDINGS: The appearance of “coffee bean sign” and “U-shaped distended sigmoid loop” are well depicted. White asterisk and white arrow show the “coffee bean sign”, a common imaging finding typically encountered in sigmoid volvulus, and recognizable between two closed and dilated apposed loops, recalling the appearance of a “coffee bean”. The central cleft of the coffee bean is due to the opposing bowel wall (white arrow). In addition, the “U-shaped distended sigmoid loop” is also well depicted: the coronal image identified a distended ahaustral sigmoid loop (white asterisk), with an inverted “U configuration”, extended up to the left hemidiaphragm; transverse colon was dilated and displaced to the right side by the U-loop described. TECHNIQUE: Coronal SSFSE images obtained using a 1.5 Tesla scanner - Protocol: coronal plane; TR=740.9 ms; TE=91 ms; Thickness 4 mm, Matrix 512×512).
Figure 5.
A thirty-one-year-old pregnant woman (31 weeks gestation) with sigmoid volvulus. FINDINGS: The exam shows the transition point (white arrow) - the obstruction point due to a fusiform tapering of bowel loop; the dilated bowel loop (white asterisk) is well depicted. The white arrowhead partially shows the concentric pattern of twisted intestinal loops. TECHNIQUE: Parasagittal and axial scan planes of transabdominal ultrasound (Figures A and B). Ultrasonography was performed using a 3.5 Mhz convex transducer; grayscale images were acquired (Figures A and B).
Figure 4.
A thirty-one-year-old pregnant woman (31 weeks gestation) with sigmoid volvulus. FINDINGS: The axial images reproduce the “split sign”, thanks to the high contrast resolution of MRI. The images were acquired at the twisting point represented in figure 2 (Figure 4A=cranial level, Figure 4B=caudal level); the intestinal walls of two adjacent segments (white arrows) are separated by adjacent mesenteric fat planes, producing the so called “split sign”; white arrowheads show the mesenteric fat planes and vessels. TECHNIQUE: Axial SSFP images obtained using a 1.5 Tesla scanner - Protocol: axial plane; TR=3.9 ms; TE=1.7 ms; Thickness 4 mm, Matrix 512×512.
Clinical symptoms and imaging findings suggested the diagnosis of a sigmoid volvulus. Meteoric distension and abdominal pain rapidly worsened, so the patient underwent a caesarean operation and subsequent laparotomy. The surgical intervention confirmed the clinical and radiological diagnosis: the large bowel loops were swollen and edematous, with a purple color due to the mild impairment of vascularization (Figure 6); surgical decompression was promptly performed to restore normal blood supply and bowel canalization; the presence of viable tissue allowed a conservative approach, avoiding bowel resection. The preterm infant survived with no complications.
Figure 6.
A thirty-one-year-old pregnant woman with sigmoid volvulus. FINDINGS: The surgical intervention confirmed the clinical and radiological diagnosis: the large bowel loops were dilated (Figure 6A), swollen and edematous (Figure 6B), with purple color due to the mild impairment of vascularization; after surgical decompression, normal vascularization was promptly restored and the bowel recovered its normal appearance and canalization.
DISCUSSION
Etiology & demographics
Bowel obstruction is an uncommon and rare complication during pregnancy, and varies from 1 in 1500 to 1 in 66000 [1–2]; prompt surgical intervention is necessary to reduce maternal and fetal mortality and morbidity [3–4]. The most common cause is the development of adhesions from previous surgery (60–70% of cases), followed by volvulus (25%) [2, 4–7].
Sigmoid volvulus is an abnormal twisting of the sigmoid colon along its mesenteric axis, producing obstruction of intestinal lumen and mesenteric vessels [8, 9]. The endemic form is extremely common in developing countries (20–54% of all acute intestinal obstructions), with greatest incidence in the II–III decades and male-to-female ratio of 4:1. In western countries sigmoid volvulus represents an unusual condition (male-to-female ratio of 1.1:1), more often observed in elderly patients (V–VI decades), with multiple comorbidities; nevertheless, it is the third most common cause of large bowel obstruction after cancer and diverticulitis [10–11]. In pregnant women sigmoid volvulus occurs rarely; since 1885 only 100 similar cases have been reported [11].
A long redundant sigmoid colon with a narrow mesentery (dolichosigmoid) is considered a prerequisite of volvulus formation [11]; the congenital theory is supported by familial prevalence and sigmoid volvulus occurrence in some ethnical groups. Chronic constipation is associated with increased risk of sigmoid volvulus in western countries’ populations, whereas high fiber diet may increase the risk in developing countries.
During pregnancy, the development of sigmoid volvulus can occur as result of a redundant or abnormally mobile sigmoid colon, displaced and led to twist around its point of fixation by the enlargement of the uterus; the fact that most reported cases occurred during third trimester of pregnancy corroborates this hypothesis [3, 12].
Clinical & imaging findings
The clinical classification of sigmoid volvulus includes typical and atypical presentation of disease. In typical cases the patient shows a sudden onset, with a triad of abdominal distension, pain and constipation; in the atypical form symptoms are misleading and are less suggestive of obstruction.
Intestinal obstruction - if undiagnosed - is associated with significant maternal and perinatal mortality, approaching 25% and 6% respectively [13–14]. Although prompt management to avoid necrosis of the twisted loop is required, intestinal obstruction may be difficult to recognize as a cause of abdominal pain in obstetric patients; symptoms such as mild, crampy pain and constipation are vague and may be regarded as pregnancy-related; furthermore, anatomic and physiologic adaptations of the pregnant state decrease the sensitivity and specificity of the clinical and laboratory data, frequently leading clinicians to rely on imaging to distinguish among an extensive variety of possible diagnoses. The gravid state can obscure common conditions such as appendicitis, cholecystitis, bowel obstruction and adnexal torsion [15]. The delayed diagnosis of volvulus in pregnancies - as observed in our case - has already been reported in literature [3, 10]; the average length of time from the onset of obstructive symptoms until clinical presentation is reported to be 48 hours [3, 16].
Typical imaging findings of sigmoid volvulus - clearly identified in an X-ray of the abdomen or in a scanogram - are the absence of rectal gas and the inverted U-shaped distended sigmoid [8, 17]. The U-loop derives from the progressive accumulation of air in the loops imprisoned by the malrotation; the excessive accumulation of air inside the loops tends to assume the least dependent position. The distended sigmoid loop overlapped with the liver and extended cephalad to the transverse colon, and this appearance is typically described as “northern exposure sign”. The coffee bean sign is another common imaging finding typically encountered in sigmoid volvulus: it is represented by two closed and dilated apposed loops, recalling the appearance of a “coffee bean”; the central cleft of the coffee bean is due to the opposing bowel wall [18].
Levsky et Al.[8] described two novel imaging signs of volvulus: crossing sigmoid transition (called the X-marks-the-spot-sign) and folding of the sigmoid wall by partial twisting (called the split-wall sign) [8]. The split wall sign is a typical imaging finding due to the partial twisting of sigmoid loop: the intestinal walls are separated by adjacent mesenteric fat planes. The transition points, the split sign and the whirl sign are clearly depicted on cross-sectional CT images. In our report, the pregnancy led us to perform an MRI examination to investigate the clinical suspicion of bowel disease. The images acquired allowed us to identify the pathognomonic imaging findings, showing the “coffee bean sign” (Figure 2), the “U-shaped distended sigmoid loops” (Figures 2–3), the “northern exposure sign” (Figure 3) and the twisting of sigmoid loop (Figures 3–4). On axial and coronal acquisitions it is possible to easily identify the split sign: the high contrast resolution of MRI is able to detect the mesenteric planes between the loops (Figures 3–4). US exam identifies the transition point and the sigmoid dilatation, as clearly shown in the figure (Figure 5).
Figure 3.
A thirty-one-year-old pregnant woman (31 weeks gestation) with sigmoid volvulus. FINDINGS: The distended sigmoid loop - with an inverted “U configuration” (white asterisks) - extended cephalad to the transverse colon (white dotted arrows), up to the left hemidiaphragm. The displacement of the sigmoid colon cephalad to the transverse colon produces “the northern exposure sign”. The figures also show the typical imaging finding due to the partial twisting of sigmoid loop (white arrows): the abnormal malrotation results in dilation and obstruction. TECHNIQUE: Coronal SSFP images obtained using a 1.5 Tesla scanner - Protocol: axial plane; TR=3.9 ms; TE=1.7 ms; Thickness 4 mm, Matrix 512×512.
Treatment & prognosis
The treatment of sigmoid volvulus is related to the disease stage and to the functional state of the patient. In cases with good colonic vascularization - without peritoneal signs or intestinal signs of ischemia - an acceptable treatment could be decompression of the volvulus, to restore canalization and adequate blood supply; detorsion could be effected by endoscopic placement of a soft rectal tube or during laparotomy.
Presence or suspicion of bowel gangrene or perforation, due to prolonged alteration of vascular supply, requires urgent resection [11].
In addition to the vitality of intestinal wall, Alshawi et Al12 proposed the following management options based on the stage of pregnancy: in the first trimester, and in recurrent cases in the second trimester, colonoscopic detorsion and rectal decompression are performed [12]. Sigmoid colectomy is recommended in the second trimester, because endoscopic decompression is associated with high recurrence rate of volvulus, and operating in the second trimester is associated with lower miscarriage rate than the first [12]. In the third trimester, endoscopic decompression is performed until fetal maturity, when elective labor followed by sigmoidectomy provides the final treatment.
However, in later pregnancy, endoscopic derotation could be limited by enlargement of the uterus [3], and surgical derotation or sigmoidectomy are often chosen as treatment: resection could be eventually postponed in the post-partum in cases of viable tissue [2], whereas the presence of non-viable tissue requires bowel resection with a diverting colostomy. Primary anastomosis of edematous large bowel is avoided because it could be hazardous to both mother and foetus [3].
Differential diagnoses
In our patient gynecological examination was not suggestive of threatened preterm labor and cardiotocography did not show signs of fetal distress; in addition, the absence of effacement and/or dilatation of the cervix suggested looking for a different cause of abdominal pain.
In the evaluation of abdominal pain during pregnancy, it is important to look for different pathological processes. Abdominal pain may be related to abdominal emergencies or gynecologic emergencies; in addition, abdominal emergencies are divided into traumatic and non-traumatic types. A post-traumatic condition could be suspected when the patient refers a previous abdominal trauma.
Among non-traumatic emergencies, appendicitis is the most common cause of acute abdomen in the pregnant patient, affecting 1 in 1500 pregnancies [5], with incidence of disease very similar to that observed in the general population (0.05–0.07%) [19]; in addition, it is the most common illness requiring emergency surgery in pregnant patients [19]. Among pregnant patients, perforation seems to be more common, with a percentage of 43%, whereas this complication is less encountered in general population (3–4%). The difference could be explained by the delayed diagnosis: the gravid uterus displaces the appendix superiorly, and the abdominal pain can frequently be referred in the upper portion of the right abdominal flank [19–20]. US examinations can show an intraluminal stump (appendicolith) and periappendiceal fluid. MRI findings include the dilatation of appendix (>6mm), with thickening of its wall and high signal intensity on T2-weighted images due to wall edema; other imaging findings include the increased signal intensity in the pericecal fat and fluid collections; diffusion-weighted images show variable degree of restricted diffusion. The differential diagnosis should include several causes of abdominal pain in the right flank, such as nephrolithiasis or ureteral obstruction.
Intestinal obstruction in pregnancy varies from 1 in 1500 to 1 in 66000 [1–2, 21]; most obstructions are caused by post-surgical adhesions; other causes are volvulus, intussusception and carcinoma. US examinations show bowel dilatation, hypoperistalsis, and multiple air-fluid levels. MR is able to identify the dilatation of bowel and the multiple air-fluid levels. SSFSE sequences are particularly effective for bowel imaging, minimizing artifacts caused by magnetic susceptibility and peristaltic motion [5]. In addition, coronal SSFSE and SSFP images allow very often the location of bowel obstruction transition point.
After appendicitis and bowel obstruction, cholecystitis and cholelithiasis represent the third cause of non-obstetric surgical emergencies in pregnancy, occurring in 1 to 8 in 10000 pregnancies. US is accurate in the diagnosis of choledocholithiasis, showing the stone in the bile duct lumen and the dilatation of biliary tree; however, bowel gas limits the evaluation, and MRI allows diagnosis. In the diagnosis of cholecystitis, US scans show gallbladder wall thickening and pericholecystic fluid collection; in some cases US images allow to detect intraluminal debris or associated stones.
Inflammatory bowel diseases have to be differentiated from other acute abdominal diseases in pregnancy; an accurate gathering of clinical history is necessary to make the diagnosis of an exacerbation of inflammatory disease. US examinations reveal narrowing of distal ileum, with bowel wall thickening and enlarged mesenteric lymph nodes; in addition to these mentioned signs, MR diffusion images may show restricted diffusion of the involved loops.
Acute pyelonephritis occurs in 1% to 2% of pregnancies; the clinical presentation is similar to the general population (acute pain, fever, leukocytosis) [5]. Generally, imaging findings observed are renal enlargement (kidneys may appear asymmetrical), areas of edema (seen as hypointensity on T1-weighted images and hyperintensity on T2-weighted images) and dilatation of collecting system.
In conclusion, our case report shows how MRI findings allowed for the diagnosis of a rare disease complicating pregnancy, avoiding ionizing radiation exposure; in accordance with recent articles in literature, we emphasize the role of MRI in the diagnosis and management of acute nontraumatic abdominal pain in pregnancy [22, 23].
TEACHING POINT
During pregnancy, the development of sigmoid volvulus can occur as result of a redundant or abnormally mobile sigmoid colon, displaced and led to twist around its point of fixation by the enlargement of the uterus. The coffee bean sign is a common imaging finding typically encountered in sigmoid volvulus: it is represented by two closed and dilated apposed loops, recalling the appearance of a “coffee bean”; the central cleft of the coffee bean is due to the opposing bowel wall. Transition points, split sign and whirl sign are other common imaging findings depicted on cross-sectional images: the high contrast resolution of MRI is able to detect the mesenteric planes between the intestinal walls of two adjacent segments - identifying the whirl sign and the split sign. These MRI findings suggest the diagnosis of volvulus in pregnancy.
Table 1.
Summary table for sigmoid volvulus in pregnancy
| SUMMARY TABLE | |
|---|---|
| Etiology |
|
| Incidence |
|
| Gender Ratio |
|
| Age Predilection |
|
| Risk Factors |
|
| Treatment |
|
| Prognosis | |
| Findings on imaging |
|
Table 2.
Differential table for sigmoid volvulus
| LESION | X-ray | US | CT | MRI | Pattern of contrast enhancement | Scintigraphy | PET |
|---|---|---|---|---|---|---|---|
| Sigmoid volvulus | Absence of rectal gas; inverted U-shaped distended sigmoid; coffee bean sign; northern exposure sign | Transition point; split sign; bowel loop dilatation | Distended ahaustral sigmoid loop in a U-inverted configuration Transition point; split sign; bowel loop dilatation | MR - T1: U-inverted sigmoid loop configuration; bowel dilatation MR - T2: U-inverted sigmoid loop configuration; bowel dilatation; MR- DWI: possible restricted diffusion |
Variable contrast enhancement; prolonged volvulus may produce ischemic wall changes (low enhancement) | Increased uptake | Increased uptake |
| Appendicitis | Air-fluid levels localised to the caecum; adynamic ileus; appendicoliths; deformity of caecum | Wall thickening; appendicoliths; periappendiceal fluid | Enlargement of the appendix (>6 mm); wall thickening; periappendiceal fat stranding | MR - T1: enlargement of the appendix MR - T2: high signal intensity that filled lumen; wall edema MR - DWI: restricted diffusion |
Increased wall enhancement | Increased uptake | Increased uptake |
| Bowel obstruction | Multiple air-fluid levels; (large and/or small) bowel distension | Bowel dilatation; bowel wall thickening; hypoperistalsis; presence of air-fluid levels; free fluid collection | Multiple air-fluid levels; identification of the transition points; CT demonstrates the cause of stenosis (tumor, etc.) | MR - T1: multiple air-fluid levels; bowel dilatation MR - T2: increased signal intensity due to wall edema MR- DWI: variable degree of restricted diffusion |
Variable degree of enhancement | Not applicable in acute bowel obstructions | Not applicable in acute bowel obstructions |
| Cholecystitis | Presence of stone in the right hypochondrium | Gallbladder wall thickening; pericholecystic fluid collection; presence of stone | Wall thickening, sometimes with intramural hypodensity (edema); pericholecystic fluid collection | MR - T1: high signal intensity of the lumen (debris) MR - T2: hyperintensity of the wall (edema) MR- DWI: variable degree of restricted diffusion |
Enhancement of the gallbladder wall | Increased uptake, hot rim sign | Ring-like radiotracer uptake |
| Cholelithiasis | Presence of stone in the right hypochondrium | Stone in the bile duct; dilatation of biliary tree | Hyperdensity (stone) inside the biliary duct; presence of rim sign; extra-hepatic and intrahepatic biliary ectasia | MR - T1: high signal intensity of the lumen (debris) MR - T2: hyperintensity of the wall (edema); sludge or stones MR- DWI: variable degree of restricted diffusion |
Absence or mild enhancement of biliary tree (in cases of infection) | Generally not performed | Generally not performed |
| Inflammatory bowel disease | Narrowing (stenosis) of distal ileum; bowel wall ulcerations; fistulae, bowel distension | Narrowing (stenosis) of distal ileum; bowel wall thickening; enlarged mesenterial nodes | Wall thickening; stenosis of distal ileum; enlargement of nodes | MR - T1: wall thickening; narrowing of distal ileum MR - T2: hyperintensity of the wall (edema); fluid collection; enlargement of nodes MR- DWI: variable degree of restricted diffusion |
Increased wall enhancement | Increased uptake | Increased uptake |
| Acute pyelonephritis | Kidneys may appear asymmetrical; kidney stones | Edema (hypoechoic area); abscess | Renal enlargement; hypodensity areas | MR - T1: hypointensity areas in the kidney MR - T2: dilatation of collecting system MR- DWI: restricted diffusion |
Delayed caliceal appearance time; delayed or striated nephrogram | Delayed nephrogram | Delayed nephrogram |
ABBREVIATIONS
- FSPGR
Fast-Spoiled-Gradient-Echo
- MDCT
MultiDetector Computed Tomography
- MPR
MultiPlanar Reconstructions
- MRI
Magnetic Resonance Imaging
- SSFP
Steady-State-Free-Precession
- SSFSE
Single-Shot-Fast-Spin-Echo
- TE
Echo Time
- TR
Repetition Time
- US
UltraSonography
REFERENCES
- 1.Augustin G, Majerovic M. Non-obstetrical acute abdomen during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2007;131(1):4–12. doi: 10.1016/j.ejogrb.2006.07.052. [DOI] [PubMed] [Google Scholar]
- 2.Machado NO, Machado LS. Sigmoid Volvulus Complicating Pregnancy Managed by Resection and Primary Anastomosis: Case report with literature review. Sultan Qaboos Univ Med J. 2009;9(1):84–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Connoly MM, Unti JA, Nora PF. Bowel obstruction in pregnancy. Surg Clin North Am. 1995;75:101–113. doi: 10.1016/s0039-6109(16)46537-0. [DOI] [PubMed] [Google Scholar]
- 4.De U, De KK. Sigmoid volvulus complicating pregnancy. Indian J Med Sci. 2005;59(7):317–9. [PubMed] [Google Scholar]
- 5.Wolfe G, Oto A. MRI evaluation of acute abdominal pain in pregnant patients. Applied Radiology. 2007;36(9) http://www.appliedradiology.com [Google Scholar]
- 6.Wanetick LH, Roschen FP, Dunn JM. Volvolus of the small bowel complicating pregnancy. J Reprod Med. 1975;14(2):82–3. [PubMed] [Google Scholar]
- 7.Sharp HT. The acute abdomen during pregnancy. Clin Obstet Gynecol. 2002;45(2):405–13. doi: 10.1097/00003081-200206000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Levsky JM, Den EI, DuBrow RA, Wolf EL, Rozenblit AM. CT findings of sigmoid volvulus. AJR Am J Roentgenol. 2010;194(1):136–43. doi: 10.2214/AJR.09.2580. [DOI] [PubMed] [Google Scholar]
- 9.Cirocchi R, Farinella E, La Mura F, Morelli U, Trastulli S, Milani D, Di Patrizi MS, Rossetti B, Spizzirri A, Galanou I, Kopanakis K, Mecarelli V, Sciannameo F. The sigmoid volvulus: surgical timing and mortality for different clinical types. World J Emerg Surg. 2010;5:1. doi: 10.1186/1749-7922-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weingrow D, McCague A, Shah R, Laiezarzadeh F. Delayed presentation of sigmoid volvulus in a young woman. West J Emerg Med. 2012;13(1):100–2. doi: 10.5811/westjem.2011.4.6720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raveenthiram V, Matiba TE, Atamanalp SS, De U. Volvolus of the sigmoid colon. Colorectal Dis. 2010;12(7):e1–17. doi: 10.1111/j.1463-1318.2010.02262.x. [DOI] [PubMed] [Google Scholar]
- 12.Alshawi JS. Recurrent sigmoid volvulus in pregnancy: report of a case and review of the literature. Dis Colon Rectum. 2005;48(9):1811–3. doi: 10.1007/s10350-005-0118-5. [DOI] [PubMed] [Google Scholar]
- 13.Sharp HT. Gastrointestinal surgical conditions during pregnancy. Clin Obstet Gynecol. 1994;37:306–315. doi: 10.1097/00003081-199406000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Ballantyne GH, Brandner MD, Beart RW, Jr, Illstrup DM. Volvulus of the colon. Incidence and mortality. Ann Surg. 1985;202:83–92. doi: 10.1097/00000658-198507000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Challoner K, Incerpi M. Nontraumatic abdominal surgical emergencies in the pregnant patient. Emerg Med Clin North Am. 2003;21(4):971–85. doi: 10.1016/s0733-8627(03)00071-3. [DOI] [PubMed] [Google Scholar]
- 16.Perdue PW, Johnson HW, Jr, Stafford PW. Intestinal obstruction complicating pregnancy. Am J Surg. 1992;164(4):384–8. doi: 10.1016/s0002-9610(05)80910-9. [DOI] [PubMed] [Google Scholar]
- 17.Lepage-Saucier M, Tang A, Billiard JS, Murphy-Lavallée J, Lepanto L. Smal and large bowel volvulus: Clues to early recognition and complications. Eu J Radiol. 2010;74:60–66. doi: 10.1016/j.ejrad.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 18.Feldman D. The coffee bean sign. Radiology. 2000;216(1):178–9. doi: 10.1148/radiology.216.1.r00jl17178. [DOI] [PubMed] [Google Scholar]
- 19.Eyvazzadeh AD, Pedrosa I, Rofsky NM, Siewert B, Farrar N, Abbott J, Levine D. MRI of right-sided abdominal pain in pregnancy. AJR Am J Roentgenol. 2004;183(4):907–14. doi: 10.2214/ajr.183.4.1830907. [DOI] [PubMed] [Google Scholar]
- 20.Spalluto LB, Woodfield CA, DeBenedectis CM, Lazarus E. MR imaging evaluation of abdominal pain during pregnancy: appendicitis and other nonobstetric causes. Radiographics. 2012;32(2):317–34. doi: 10.1148/rg.322115057. [DOI] [PubMed] [Google Scholar]
- 21.Mirza MS, Mulla M, Hall RI. Large bowel obstruction in pregnancy: a rare entity, an unusual cause. Arch Gynecol Obstet. 2009;279(2):177–8. doi: 10.1007/s00404-008-0656-x. [DOI] [PubMed] [Google Scholar]
- 22.Masselli G, Brunelli R, Casciani E, Polettini E, Bertini L, Laghi F, Anceschi M, Gualdi G. Acute abdominal and pelvic pain in pregnancy: MR imaging as a valuable adjunct to ultrasound? Abdominal Imaging. 2011;36(5):596–603. doi: 10.1007/s00261-010-9654-0. [DOI] [PubMed] [Google Scholar]
- 23.Oto A, Ernst RD, Ghulmiyyah LM, Nishino TK, Hughes D, Chaljub G, Saade G. MR imaging in the triage of pregnant patients with acute abdominal and pelvic pain. Abdom Imaging. 2009;34(2):243–50. doi: 10.1007/s00261-008-9381-y. [DOI] [PubMed] [Google Scholar]